Abstract
Rationale:
Albeit it is rare, the authors report a stage 3 Kummell disease case. It is diagnosed by dynamic thoracic magnetic resonance imaging (MRI). Because there is no established strategy on stage 3 Kummell disease, we performed percutaneous kyphoplasty at first, but unfortunately made a revision surgery to remove the polymethylmethacrylate (PMMA) cement after the failure of percutaneous kyphoplasty.
Patient concerns:
A 73-year-old lady with severe back pain due to osteoporosis vertebral fracture was admitted to our hospital on June 23, 2016. She underwent percutaneous kyphoplasty with the back pain improved shortly. Unfortunately, she went back to our hospital due to aggravated back pain and partial paralysis on July 25, 2016.
Diagnoses:
Kummell disease, lumbar stenosis, lacunar infarction.
Outcomes:
Specially, the compression of spinal cord was obvious in the hyperflexion position on dynamic MRI. Even though there was no improvement in muscle strength, the patient was satisfied with the back pain relief after percutaneous kyphoplasty. But, the same back pain reappeared after about 1 month. Then, we took out the PMMA cement and performed posterior vertebral column resection. At last, the back pain was relieved again but the muscle strength was improved not obviously after operation. At the same time, the kyphosis was corrected and the intravertebral stability was achieved.
Lessons:
Dynamic MRI is helpful in Kummell disease with neurologic symptoms, even if there is no obvious compression in the neutral position. Furthermore, the intravertebral instability is probably the main reason of the neurologic symptoms in this case. Percutaneous kyphoplasty could not reconstruct the intravertebral stability. Stage 3 Kummell disease with obvious intravertebral instability should be treated by open surgery.
Keywords: intravertebral instability, Kummell disease, percutaneous kyphoplasty, therapy
1. Introduction
Kummell disease was first raised as delayed post-traumatic vertebral collapse by Dr. Hermann Kummell in 1891. It is a clinical phenomenon that patients with a minor trauma tend to develop a symptomatic and progressive angular kyphosis after a short asymptomatic period.[1]
Kummell disease was once divided into 5 stages according to the development of symptoms by Dr. Steel in 1951. Stage 1 is the initial insult with no abnormality on the x-ray. Stage 2 means the post-traumatic period of minor back pain. The patient is still able to work in this stage. Stage 3 represents the latent interval of relative well-being. Patients in this stage usually experience asymptomatic period lasting from months to years. Stage 4 is the recrudescent stage. Patients may feel progressive pain at the fracture position. Stage 5 signifies the terminal stage. A permanent kyphosis or compression of roots and spinal cord may be formed in this stage.[1]
Kummell disease was also divided into three stages based on different manifestations on magnetic resonance imaging (MRI). Stage 1 has a body height loss <20% with no adjacent degenerative disc disease (DDD). Stage 2 has a body height loss >20% usually with adjacent DDD. Dynamic mobile fracture is the main characteristic in this stage. Stage 3 has a posterior breakage with cord compression.[2]
Two main pathogenesis of Kummell disease include the avascular osteonecrosis[3–6] and formation of pseudarthrosis.[7] Prabhu et al point out that the distribution of vertebral artery is closely related to ischemic necrosis. The rear of 2 adjacent vertebral bodies can be supplied by its collateral circulation, whereas anterior 1/3 of it can only be supplied by the terminal blood vessels, which may increase the risk of ischemic necrosis of the anterior 1/3 of the vertebral bodies.[8] The intravertebral vacuum of Kummell disease mostly locates at the center of the vertebra or the side close to the vertebral endplate.[6]
MRI plays an important role in the diagnosis of Kummell disease. The manifestations of MRI depend on the components of the intravertebral vacuum cleft (IVC). When filled with fluid, the cleft has a reduced signal on T1-weighted images and an increased signal on T2-weighted images, which may reveal the early stage of the disease. When filled with gas, the cleft has both reduced signal on T1 and T2 weighted images, which may indicate the severe necrosis of the vertebra.[9] However, the cleft filled with both gas and fluid which accounts for 21.5% of all was not unusual.[10]
Kummell disease can cause great damage to the patients. So it is necessary to be suspicious of the occurrence of Kummell disease and make interventions right away.
2. Case presentation and analysis
2.1. Consent
This study was approved by the Medical Ethics Committee of Shandong Provincial Hospital affiliated to Shandong University. Informed consent was obtained.
2.2. General information (first visit)
A 73-year-old lady complaining of severe back pain was admitted to our department of Shandong Provincial Hospital on June 23, 2016. The visual analogue scale (VAS) for back pain was 9 points. Physical examination showed hypoesthesia on her 2 feet and weakness of hallux dorsiflexion (muscle strength, left, grade 3 and right, grade 4). Both of foot plantar flexion were weak (muscle strength, left, grade 4 and right, grade 4−).The knee jerk reflex was increased on both sides (right ++, left +++). The ankle jerk reflex was absent on both sides (−). Pathologic reflex was detected (Babinski +).
2.3. Medical history review
The patient felt slight back pain after falling down on March 15, 2016. She could walk without intermittent claudication before the injury. Also, muscle strength was normal before the injury. She received no treatment after the injury. Unfortunately, the back pain got worse and the muscle strength was decreased 3 months after the injury. Numbness of both feet was also aggravated gradually. At last, she was persuaded to go to our department to seek help.
2.4. Imaging characteristics
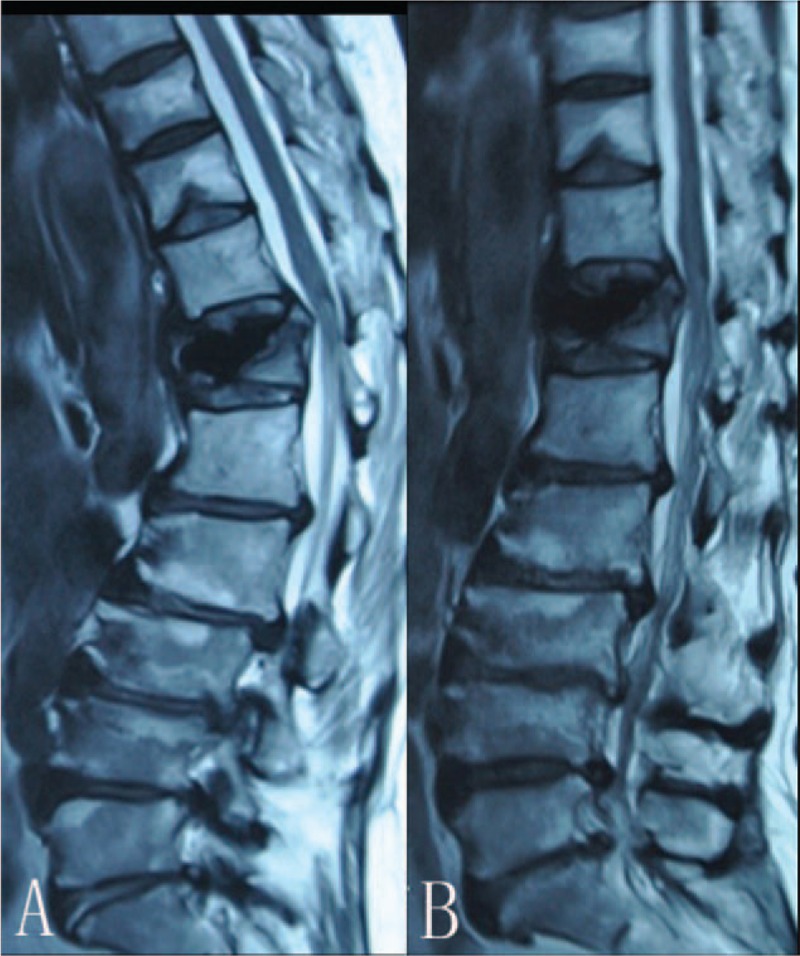
We thought that the injury lesion was in the thoracolumbar area based on previous medical history. Then, we performed thoracic MRI at first. The twelfth thoracic vertebra (T12) Kummell disease was detected on MRI. However, there was not a compression on the spinal cord. So we continued to perform a dynamic thoracic MRI for the patient. Interestingly, we found an obvious compression in the hyperflexion position (Fig. 1).
Figure 1.
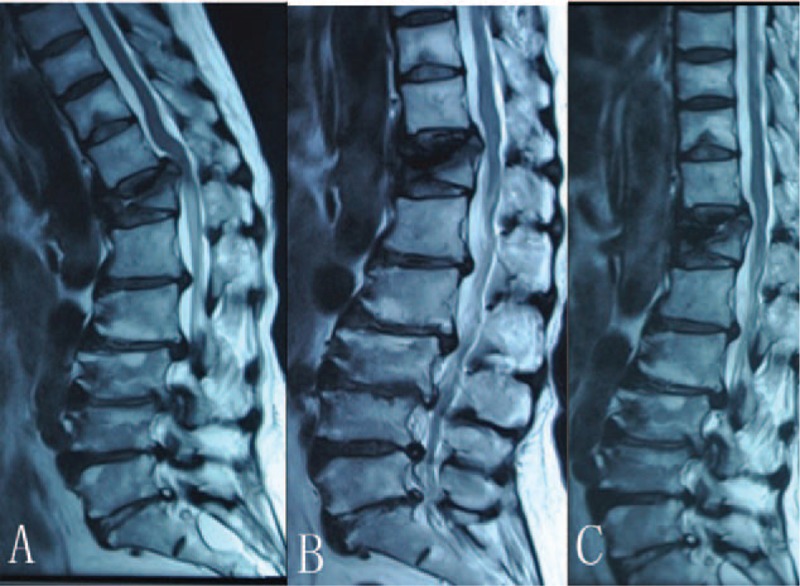
Magnetic resonance imaging (MRI) shows (B) the twelfth thoracic vertebra (T12) Kummell disease and no obvious compression on the spinal cord. Hyperflexion lateral MRI demonstrates (A) an obvious compression. Hyperextension lateral MRI reveals (C) height restoration of the T12 vertebra and no compression.
X-ray showed IVC which ensured the diagnosis of Kummell disease (Fig. 2).Obvious spinal stenosis in the hyperflexion position was detected on dynamic computer tomography (CT; Fig. 3). Notably, intravertebral instability could be found on CT and MRI (Figs. 1 and 3).
Figure 2.
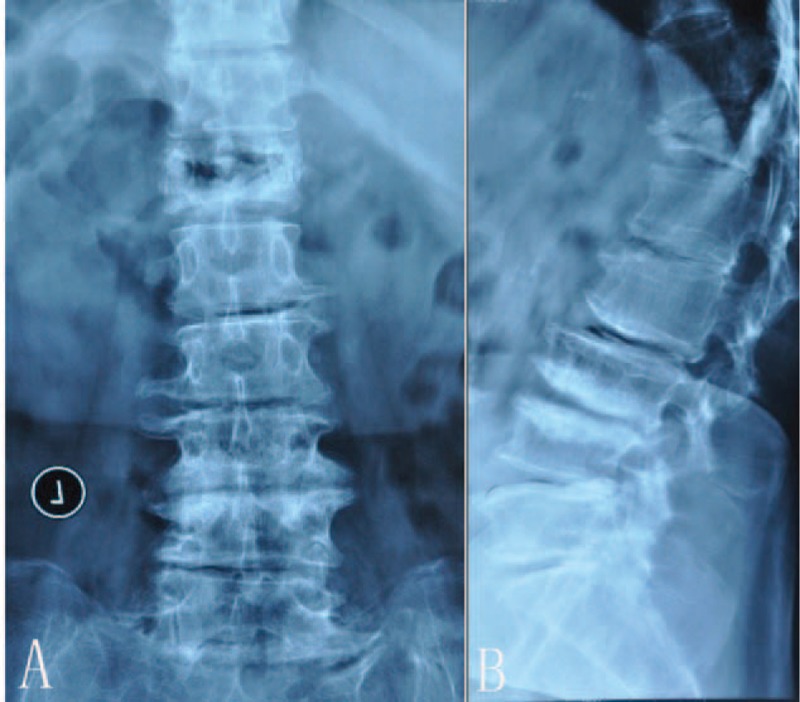
Positive and lateral x-ray show (A and B) obvious intravertebral vacuum cleft (IVC) of the twelfth thoracic vertebra (T12).
Figure 3.
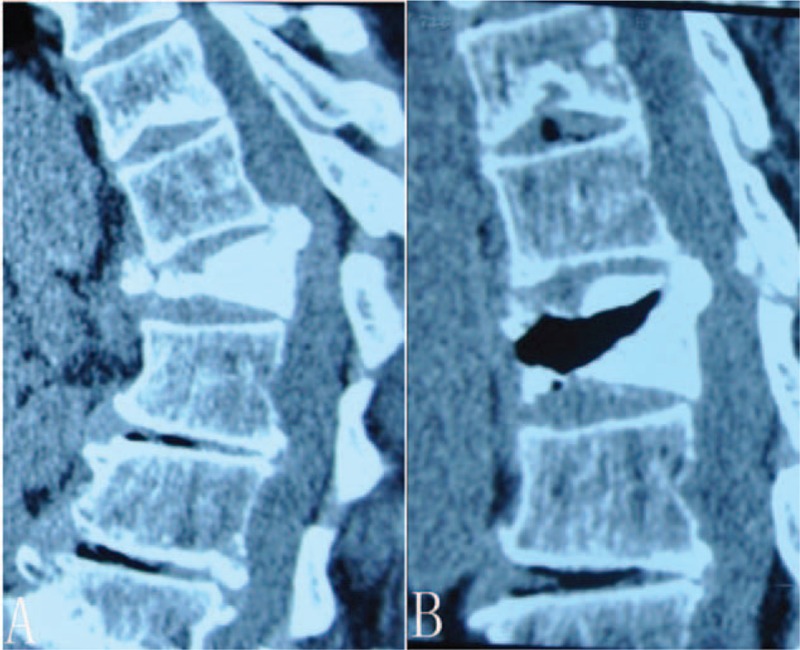
Hyperflexion lateral computer tomography (CT) detects (A) obvious spinal stenosis. Hyperextension lateral CT reveals (B) intravertebral vacuum cleft (IVC).
We guessed that the spinal cord was injured in the hyperflexion position. T12 Kummell disease was probably the main reason of the neurologic symptoms instead of lumbar stenosis. So, we performed percutaneous kyphoplasty for the patient.
2.5. Surgical procedure (percutaneous kyphoplasty)
At first, the patient was placed in a prone, lordotic position, with pillows under the upper chest and pelvis to get a reduction of the T12-fractured vertebral body. Also, we pressed the injured T12 vertebra to get a manual reduction. Using C-arm fluoroscopy visualization, unilateral transpedicular puncture was performed. Approximately 10 mL of polymethylmethacrylate (PMMA) cement was injected through a kyphoplasty needle. The injection was halted if the PMMA cement leaked into the foraminal vein, disc space, or epidural space. We injected the PMMA cement slowly to achieve a sufficient filling of T12 vertebra. Through the anteroposterior and lateral position of C-arm, height restoration and kyphosis correction were achieved.
2.6. Outcome (percutaneous kyphoplasty)
Even though there was no improvement in muscle strength, the patient was satisfied with the back pain relief after percutaneous kyphoplasty. The VAS for back pain was 2 points. We were also satisfied with the postoperative dynamic x-ray and MRI. Dynamic x-ray showed the T12 vertebral stability (Fig. 4). The spinal cord was far away from the compression on dynamic MRI (Fig. 5).
Figure 4.
Dynamic x-ray (A and B) shows the twelfth thoracic vertebra (T12) vertebra stability.
Figure 5.
Dynamic magnetic resonance imaging (MRI) demonstrates (A and B) the spinal cord far away from the compression after percutaneous kyphoplasty.
2.7. General information (second visit)
Unfortunately, she went back to our hospital due to aggravated back pain and partial paralysis on July 25, 2016. The back pain was as serious as before the percutaneous kyphoplasty. But, both of hallux dorsiflexion were weaker than before (muscle strength, left, grade 1 and right, grade 1). Both of foot plantar flexion were also weaker (muscle strength, left grade 3, and right grade 4−).
2.8. Imaging characteristics
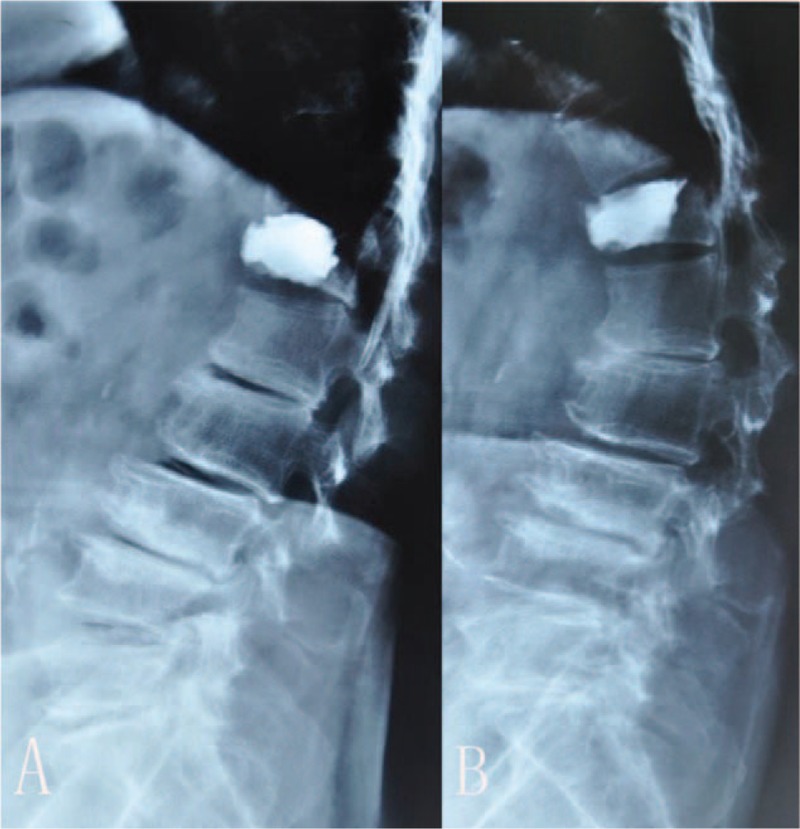
We performed a dynamic thoracic MRI again. Then, we found a new compression. Intravertebral instability could be detected obviously again on dynamic MRI (Fig. 6). X-ray and CT revealed dislocation of PMMA cement (Fig. 7).
Figure 6.
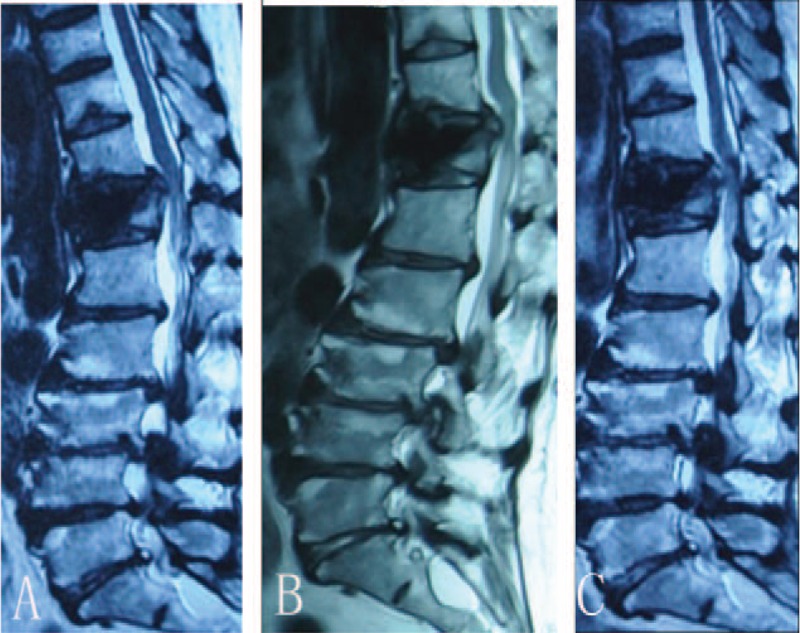
Magnetic resonance imaging (MRI) shows (A, B, and C) a new compression on the spinal cord. Intravertebral instability could be detected obviously again on dynamic MRI (A and C).
Figure 7.

X-ray (A) and computer tomography (CT) (B) revealed the dislocation of polymethylmethacrylate (PMMA) cement.
We discussed that percutaneous kyphoplasty could not reconstruct the intravertebral stability. In order to acquire full decompression and intravertebral stability, we decided to take out PMMA cement and performed posterior vertebral column resection (PVCR) for the patient.
2.9. Surgical procedure (posterior vertebral column resection)
The patient was placed prone position to avoid compression of the vena cava and to decrease thoracolumbar kyphosis. A posterior midline incision was made ranging from 2 upper vertebral segments to 2 lower segments as the center of the T12-injured vertebra. Eight screws with PMMA cement reinforcement were implanted through the pedicles with 4 on each side. Spinous process, lamina process, and articular process were removed. The fractured vertebra were dissected at first and the pedicles were then removed with a high-speed diamond bur. We took out PMMA cement from the vertebra (Fig. 8). The collapsed vertebral body was drilled laterally and anteriorly from the base of the bilateral pedicles to produce an egg-like shell. The adjacent discs were removed and the cartilaginous endplates were peeled off. The freed burst fragment with posterior longitudinal ligament was gently detached from the ventral surface of the dura mater, and then the area around the spinal cord was decompressed circumferentially. With nerve roots and dura mater being gently retracted, one large-sized special cage filled with milled autogenous bone was inserted into the cavity. One drilled autogenous bone was also inserted to act as another anterior support. After the cage and bone were placed properly on the endplates, rods were applied to the pedicle screws, then the cage and bone were fixed with compressive strength to correct angular deformity. Finally, we made man-made allograft bone to act as lamina (Fig. 8). The remaining milled autogenous bone then was embedded around the lamina to achieve bony fusion.
Figure 8.
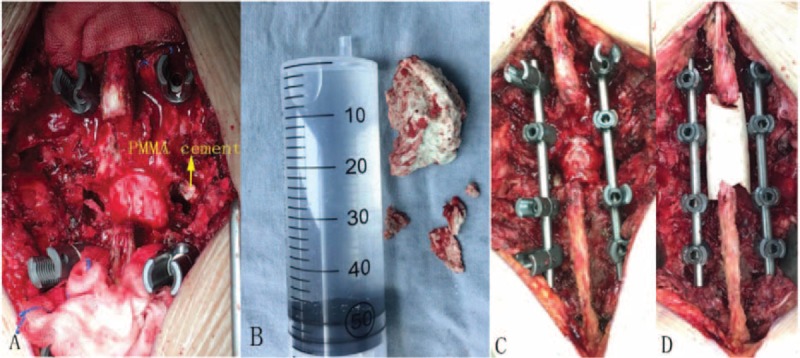
Intraoperative photo (A) shows the polymethylmethacrylate (PMMA) cement. B, PMMA cement removed from the twelfth thoracic vertebra (T12) vertebra. C, VCR osteotomy. D, Man-made allograft bone acting as lamina.
2.10. Outcome (posterior vertebral column resection)
The back pain was relieved again after operation. C-arm fluoroscopy visualization showed that kyphosis correction and intravertebral stability were both achieved. (Fig. 9).
Figure 9.
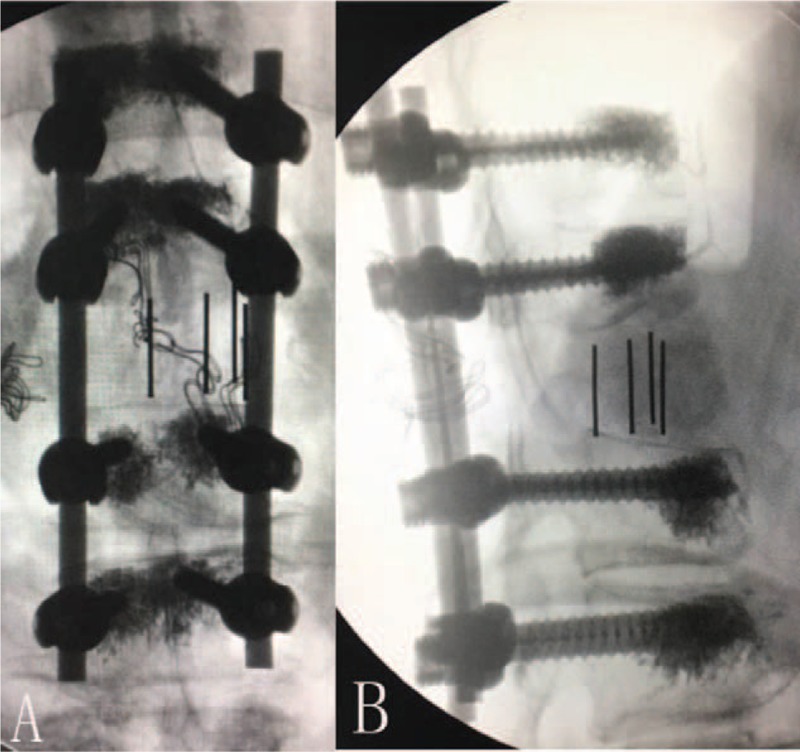
Intraoperative fluoroscopy shows (A and B) achievements of kyphosis correction and intravertebral stability.
2.11. Follow-up
After a 1-year follow-up, the back pain was relieved greatly. The VAS for back pain was 1 point. But the muscle strength was improved not obviously. The kyphosis was corrected and the intravertebral stability was reconstructed. Late subsidence of the cage was not seen. No instrumentation failure was found. Solid bony fusion was achieved (Fig. 10).
Figure 10.

Positive and lateral x-ray of 1-year follow-up show (A and B) solid bone fusion.
3. Discussion
As we all know, Kummell disease could not be treated by conservative treatment such as lying in bed or bracing. If no surgery intervention, the vertebra tend to collapse and kyphosis will be formed. A variety of therapies have been reported to treat Kummell disease. For stages 1 and 2 Kummell disease, percutaneous kyphoplasty can be an efficient treatment choice. Many scholars advocate percutaneous kyphoplasty for treating Kummell disease. Percutaneous kyphoplasty has the advantages of simple surgical method, minor trauma, less operation time, less blood loss, and acceptable postoperative outcome. Peh et al[11] report that percutaneous kyphoplasty is a safe procedure that provides pain relief and vertebral stabilization in most patients with painful fractured vertebra. Wang et al support that there is no difference between percutaneous kyphoplasty and percutaneous vertebroplasty in pain relief. But, percutaneous kyphoplasty is better in vertebral height recovery and kyphosis correction.[12] Percutaneous kyphoplasty can recover the height of the anterior volume of vertebra, correct the kyphosis, relieve the pain instantly, and achieve the vertebral stability.
But for stage 3 Kummell disease, there is no established strategy. So we performed percutaneous kyphoplasty at first, but unfortunately made a revision surgery to remove the PMMA cement after the failure of percutaneous kyphoplasty. Most scholars choose open surgery to decompress neural components, stabilize segments, allow rapid mobilization, and prevent development of kyphotic deformity for stage 3 Kummell disease. Open therapies have the advantages of sufficient decompression, better correction of kyphosis and achievements of intravertebral stability.
Uchida et al state that anterior expandable strut cage can be transplanted to support the osteoporotic vertebral collapse. They claim that anterior surgery may be an efficient way. Because the main reasons of neural compromises are present not in the posterior column but in the middle and anterior columns.[13] Some studies have gained favorable outcomes after anterior surgery.[13–15] But anterior surgery also has obvious disadvantages, such as the risk of postoperative atelectasis, progression of postoperative kyphosis, and requirement for posterior reinstrengthment.[15] Bak et al put up with pedicle subtraction wedge osteotomy to treat stage 3 Kummell disease. They report that pedicle subtraction osteotomy provides both sagittal correction of kyphotic deformity and decompression of spinal cord.[16]
Saita et al pronounce that posterior spinal shortening osteotomy can be a choice for treating the delayed paraplegia after osteoporotic vertebral fracture. By changing the spinal curvature, the surgery can control the direction of strength applying to the implant. In this way, instrumentation failure may be less seen.[17] Suzuki et al report that posterior-approach vertebral replacement with rectangular parallelepiped cages (PAVREC) may be a treatment option for stage 3 Kummell disease. They put 2 large-sized rectangular parallelepiped cages on the peripheral regions of the endplate to get a greater resistance to subsidence. PAVREC can be an alternative procedure to anterior-approach reconstruction surgery or single posterior-approach reconstruction using a cylindrical mesh cage.[18]
Zhang et al suggest that modified transpedicular subtraction and disc osteotomy combined with long-segment fixation may be an efficient treatment for stage 3 Kummell disease. They removed the upper disc of the injured vertebra. It may result in a better bony union. Furthermore, this approach can create a larger interspace, permitting a greater correction angle for the kyphotic deformity than a regular pedicle subtraction wedge osteotomy.[19] Da-Long et al come up with modified PVCR for stage 3 Kummell disease. They regard it as an effective and safe surgical method to treat Kummell disease, especially for patients with kyphotic deformity and obvious nerve-oppressed symptoms.[20]
We finally adopted PVCR for this patient to acquire full decompression and intravertebral stability. After a 1-year follow-up, the back pain was relieved greatly. The VAS for back pain was 1 point. But the muscle strength was improved not obviously after operation. We got some experiences from this case. Firstly, the main reason of the neurologic symptoms in this case was difficult to find. Specially, the compression on the spinal cord was obvious in the hyperflexion position on the dynamic MRI. The neurologic deficit mainly resulted from the intravertebral instability instead of lumbar stenosis. Secondly, we performed percutaneous kyphoplasty for this patient to stabilize vertebra. Although the vertebra was filled with PMMA cement sufficiently, the intravertebral stability could not be reconstructed by percutaneous kyphoplasty. Stage 3 Kummell disease with obvious intravertebral instability should be treated by open surgery.
4. Conclusion
Dynamic MRI is helpful in Kummell disease with neurologic symptoms, even if there is no obvious compression in the neutral position. Furthermore, the intravertebral instability is probably the main reason of the neurologic symptoms in this case. Percutaneous kyphoplasty could not reconstruct the intravertebra stability. Stage 3 Kummell disease with obvious intravertebra instability should be treated by open surgery. However, this is only a case report, more cases should be accumulated to identify this finding.
Footnotes
Abbreviations: CT = computer tomography, DDD = degenerative disc disease, IVC = intravertebral vacuum cleft, MRI = magnetic resonance imaging, PAVREC = posterior-approach vertebral replacement with rectangular parallelepiped cages, PMMA = polymethylmethacrylate, PVCR = posterior vertebral column resection, T12 = the twelfth thoracic vertebra, VAS = visual analogue scale.
The authors report no conflicts of interest.
References
- [1].Steel HH. Kummell's disease. Am J Surg 1951;81:161–7. [DOI] [PubMed] [Google Scholar]
- [2].KungChia L, TakUee W, FuChi K, et al. Staging of Kummell's disease. J Musculoskelet Res 2004;8:43–55. [Google Scholar]
- [3].Young WF, Brown D, Kendler A, et al. Delayed post-traumatic osteonecrosis of a vertebral body (Kummell's disease). Acta Orthop Belg 2002;68:13–9. [PubMed] [Google Scholar]
- [4].Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology 1978;129:23–9. [DOI] [PubMed] [Google Scholar]
- [5].Benedek TG, Nicholas JJ. Delayed traumatic vertebral body compression fracture; part II: pathologic features. Semin Arthritis Rheum 1981;10:271–7. [DOI] [PubMed] [Google Scholar]
- [6].Yu CW, Hsu CY, Shih TT, et al. Vertebral osteonecrosis: MRI imaging findings and related changes on adjacent levels. AJNR Am J Neuroradiol 2007;28:42–7. [PMC free article] [PubMed] [Google Scholar]
- [7].Kim DY, Lee SH, Jang JS, et al. Intravertebral vacuum phenomenon in osteoporotic compression fracture: report of 67 cases with quantitative evaluation of intravertebral instability. J Neurosurg 2004;100:24–31. [DOI] [PubMed] [Google Scholar]
- [8].Prakash, Prabhu LV, Saralaya VV, et al. Vertebral body integrity: a review of various anatomical factors involved in the lumbar region. Osteoporos Int 2007;18:891–903. [DOI] [PubMed] [Google Scholar]
- [9].Baur A, Stabler A, Arbogast S, et al. Acute osteoporotic and neoplastic vertebral compression fractures: fluid sign at MRI imaging. Radiology 2002;225:730–5. [DOI] [PubMed] [Google Scholar]
- [10].Zhang K, Hong D, Zhou X, et al. Surgical technique and clinical results for scapular allograft reconstruction following resection of scapular tumors. J Exp Clin Cancer Res 2009;28:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Peh WC, Gelbart MS, Gilula LA, et al. Percutaneous vertebroplasty: treatment of painful vertebral compression fractures with intraosseous vacuum phenomena. AJR Am J Roentgenol 2003;180:1411–7. [DOI] [PubMed] [Google Scholar]
- [12].Wang G, Yang H, Chen K. Osteoporotic vertebral compression fractures with an intravertebral cleft treated by percutaneous balloon kyphoplasty. J Bone Joint Surg Br 2010;92:1553–7. [DOI] [PubMed] [Google Scholar]
- [13].Uchida K, Kobayashi S, Nakajima H, et al. Anterior expandable strut cage replacement for osteoporotic thoracolumbar vertebral collapse. J Neurosurg Spine 2006;4:454–62. [DOI] [PubMed] [Google Scholar]
- [14].Kanayama M, Ishida T, Hashimoto T. Role of major spine surgery using Kaneda anterior instrumentation for osteoporotic vertebral collapse. J Spinal Disord Tech 2010;23:53–6. [DOI] [PubMed] [Google Scholar]
- [15].Mochida J, Toh E, Chiba M, et al. Treatment of osteoporotic late collapse of a vertebral body of thoracic and lumbar spine. J Spinal Disord 2001;14:393–8. [DOI] [PubMed] [Google Scholar]
- [16].Bak KH, Cheong JH, Kim JM, et al. Pedicle subtraction wedge osteotomy in kyphosis after osteoporotic compression fracture. Spinal Surg 2007;21:1–9. [Google Scholar]
- [17].Saita K, Hoshino Y, Kikkawa I, et al. Posterior spinal shortening for paraplegia after vertebral collapse caused by osteoporosis. Spine (Phila Pa 1976) 2000;25:2832–5. [DOI] [PubMed] [Google Scholar]
- [18].Suzuki T, Abe E, Miyakoshi N, et al. Posterior-approach vertebral replacement with rectangular parallelepiped cages (PAVREC) for the treatment of osteoporotic vertebral collapse with neurological deficits. J Spinal Disord Tech 2013;26:E170–6. [DOI] [PubMed] [Google Scholar]
- [19].Zhang X, Hu W, Yu J, et al. An effective treatment option for Kummell's disease with neurological deficits: modified transpedicular subtraction and disc osteotomy combined with long-segment fixation. Spine (Phila Pa 1976) 2016;41:E923–30. [DOI] [PubMed] [Google Scholar]
- [20].Yang S D-L, Yang S S-D, Chen S Q, et al. The treatment evaluation for osteoporotic Kummell's disease by modified posterior vertebral column resection: minimum of one-year follow-up. Med Sci 2017;23:606–12. [DOI] [PMC free article] [PubMed] [Google Scholar]


