Abstract
Rationale:
SAPHO (synovitis, acne, pustulosis, hyperostosis, and osteitis) syndrome is an autoinflammatory disease with no standardized treatment. Tripterygium wilfordii hook f (TwHF) is a Chinese herb with immunosuppressive effects and has been used to treat some chronic inflammatory diseases. However, it has not been reported as a therapeutic option in SAPHO syndrome. Here we present the first report in which a remarkable remission of SAPHO syndrome was achieved in response to TwHF.
Patient concerns:
A 57-year-old female patient noted swelling and pain at the anterior chest wall and scattered rashes like psoriasis vulgaris. Bone scintigraphy demonstrated the classic “bull's head” sign and magnetic resonance images indicated bone marrow edema on T5.
Diagnoses:
The diagnosis was made by dermatological and osteoarticular manifestations and classical “bull's head” sign in bone scintigraphy.
Interventions:
TwHF with a priming dose of 20 mg 3 times per day and a gradual dose reduction of 20 mg per day in every 3 months. Four months later, methotrexate was added with 10 mg per week.
Outcomes:
Osteoarticular symptoms and radiological abnormalities were improved dramatically.
Lessons:
This case illustrates a promising strategy to treat SAPHO syndrome.
Keywords: remarkable remission, SAPHO syndrome, Tripterygium wilfordii hook f treatment
1. Introduction
SAPHO (synovitis, acne, pustulosis, hyperostosis, and osteitis) syndrome is a rare autoinflammatory disease with no standardized treatment.[1]Tripterygium wilfordii hook f (TwHF) is a Chinese herb with immunosuppressive effects and has been used to treat some chronic inflammatory diseases.[2] We present the first report in which a remarkable remission of SAPHO syndrome was achieved in response to TwHF.
2. Case report
A written informed consent was obtained from the patient for publication of this case report, and the study was approved by the Ethics Committee of Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences.
A 57-year-old female patient noted swelling and pain at the anterior chest wall (ACW) in June 2016. These symptoms were partially relieved after empirical administration of NSAIDs. One month later, she reported limited physical activity of axial joints and scattered erythematous maculopapular rashes covered with silvery-white scales around the whole body, in accordance with the typical characteristics of psoriasis vulgaris. No family history of similar symptoms was reported.
On admission, blood analysis revealed augmented hypersensitivity C-reactive protein (hsCRP) 119.54 mg/dL and erythrocyte sedimentation rate (ESR) 115 mm/h. Complete blood count, liver, and renal function were all within the normal range. Rheumatoid factor (RF), antinuclear antibody (ANA), and human leukocyte antigen B27 (HLA-B27) were all negative. Whole body bone scintigraphy using 99Tc-MDP showed multiple lesions with increased tracer accumulation in sternum, left first anterior rib, right sixth posterior rib, vertebrae, left ilium, and left foot, demonstrating the classic “bull's head” sign in the anterior chest wall (Fig. 1A). Magnetic resonance images (MRI) obtained with various sequences of the spine indicated abnormal signal intensity on T5, which was suggestive of bone marrow edema (Fig. 1B). 18F-fluorodoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) was also performed, indicating multifocal hypermetabolism on bilateral sternoclavicular joints, left ilium, pubis, and T5, L1, L5 vertebrae. Based on dermatological and osteoarticular manifestations and the classic “bull's head” sign, the diagnosis of SAPHO syndrome was made, in accordance with the diagnostic criteria proposed in 1988.[3] Differential diagnosis included metastatic bone malignancy and bacterial osteomyelitis, which were excluded by FDG PET scans.
Figure 1.
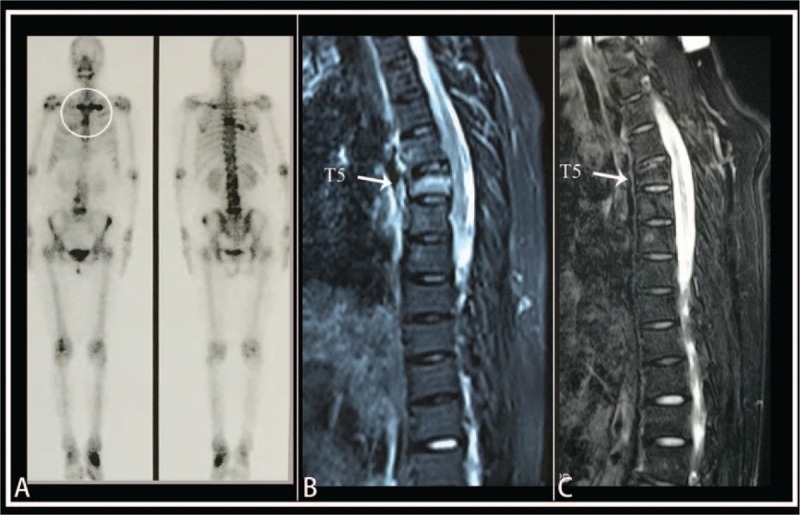
Imaging examination results. (A) 99mTc bone scintigraphy demonstrated the classic “bull's head” sign in the anterior chest wall (while circle). (B) MR image (Fat-suppression T2WI sequence) obtained before TwHF treatment revealed high signal intensity in T5 (white arrow), corresponding to bone marrow edema. (C) Bone marrow edema disappeared (white arrow) 4 months after the administration of TwHF.
Considering the autoinflammatory nature of SAPHO syndrome, which was suggested by recent evidence,[1] TwHF was administered tentatively to exert its anti-inflammatory function with a priming dose of 20 mg 3 times per day and a gradual dose reduction of 20 mg per day in every 3 months. One month later, patient's symptoms were improved remarkably, especially the rashes. Four months later, a remarkable remission of symptoms was achieved and surprisingly the bone marrow edema of T5 disappeared as well (Fig. 1C). The patient reported that she strictly adhered to the medication and no adverse effects were noted. As the ESR and CRP were still above the normal range, methotrexate was added with 10 mg per week. Inflammatory condition parameters and disease activity indexes decreased progressively during the whole period (Fig. 2).
Figure 2.
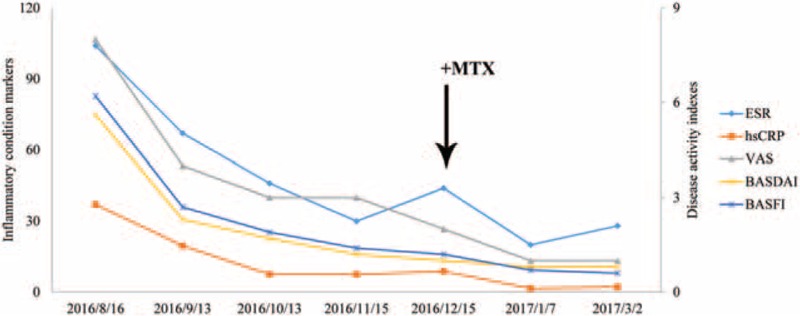
Decrease of inflammatory condition parameters and disease activity indexes after administration of TwHF. Methotrexate (MTX) was added after 4-month treatment of TwHF (black arrow).
3. Discussion
TwHF is a traditional Chinese herb with profound immunosuppressive effects and has been used to treat immunological disorders for years.[2] Numerous studies have illustrated that the nuclear factor NF-κB pathway is the primary target of the bioactive compounds of TwHF.[4] NF-κB plays an important role in the expression of some proinflammatory genes, including cytokines, chemokines, and adhesion molecules, after being activated by proinflammatory cytokines such as IL-1 and TNF-α.[5] In agreement with the concept that SAPHO is an autoinflammatory disorder, proinflammatory cytokines, including IL-1β, TNF-α, and IL-8, are deemed to be important in the pathogenesis of SAPHO syndrome.[6] Moreover, mutation in NOD2 gene, which may lead to an abnormal immune response to bacterial peptidoglycans via activation of NF-κB seems to play a role in SAPHO syndrome as well.[7] Therefore, it was suspected that NF-κB may participate in the pathogenesis of SAPHO syndrome. Further studies are needed to verify this hypothesis.
Conventional nonbiological disease-modifying antirheumatic drugs (DMARDs) are not recommended in the treatment of axial spondyloarthritis (ax-SpA) for its limited benefit on axial involvement indicated by available evidence.[8] However, TwHF, which belongs to DMARDs, was remarkably effective for bone marrow edema in spine in this case. This intriguing phenomenon may be attributed to the heterogeneity of pathogenesis between SAPHO syndrome and ax-SpA or the predilection of TwHF on axial skeletal involvement in autoinflammatory diseases.
One of the main biases may be the spontaneous disappearance of systematic inflammation and bone inflammatory foci after a sufficient time interval. The clinical course of SAPHO syndrome is marked by relapses and remissions.[9] Therefore, the improvement of symptoms and change on MRI might be linked to the fluctuation of the disease over time, instead of the TwHF treatment. Another bias comes from the drug combination with MTX. However, remarkable remission had been achieved before the administration of MTX, indicating that it was not caused by MTX.
4. Conclusions
To the best of our knowledge, this is the first report of using TwHF to treat SAPHO syndrome. To our excitement, patient's condition was progressively improved and finally a remarkable remission of both symptoms and abnormal signal intensity on MRI were achieved. This dramatic change illustrates the potential therapeutic role of TwHF in SAPHO syndrome, which needs to be clarified by further clinical trials.
Footnotes
Abbreviations: ACW = anterior chest wall, MRI = magnetic resonance imaging, SAPHO = synovitis, acne, pustulosis, hyperostosis, and osteitis, TwHF = Tripterygium wilfordii hook f.
CL, XS, and YC equally contributed to this study.
CL is currently receiving a grant 2016-4-40112 from Capital Medical Research and Development Fund and a grant 2016YFC0901501 from the National Key Research and Development Program of China. For the remaining authors none were declared.
The authors have no conflicts of interest to disclose.
References
- [1].Firinu D, Garcia-Larsen V, Manconi PE, et al. SAPHO syndrome: current developments and approaches to clinical treatment. Curr Rheumatol Rep 2016;18:35. [DOI] [PubMed] [Google Scholar]
- [2].Kao PN, Qiu D. Immunosuppressive and anti-inflammatory mechanisms of triptolide, the principal active diterpenoid from the Chinese medicinal herb Tripterygium wilfordii Hook. f. Drugs R D 2003;4:1–8. [DOI] [PubMed] [Google Scholar]
- [3].Benhamou CL, Chamot AM, Kahn MF, et al. Synovitis-acne-pustulosis hyperostosis-osteomyelitis syndrome (SAPHO). A new syndrome among the spondyloarthropathies? Clin Exp Rheumatol 1988;6:109–12. [PubMed] [Google Scholar]
- [4].Wong KF, Yuan Y, Luk JM. Tripterygium wilfordii bioactive compounds as anticancer and anti-inflammatory agents. Clin Exp Pharmacol Physiol 2012;39:311–20. [DOI] [PubMed] [Google Scholar]
- [5].Lawrence T. The nuclear factor NF-kappaB pathway in inflammation. Cold Spring Harb Perspect Biol 2009;1:a001651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Marzano AV, Borghi A, Meroni PL, et al. Pyoderma gangrenosum and its syndromic forms: evidence for a link with autoinflammation. Br J Dermatol 2016;175:882–91. [DOI] [PubMed] [Google Scholar]
- [7].Burgemeister LT, Baeton DLP, Tas SW. Biologics for rare inflammatory diseases: TNF blockage in the SAPHO syndrome. Neth J Med 2012;70:444–9. [PubMed] [Google Scholar]
- [8].Simone D, Nowik M, Gremese E, et al. Disease-modifying antirheumatic drugs (DMARD) and combination therapy of conventional DMARD in patients with spondyloarthwritis and psoriatic arthritis with axial involvement. J Rheumatol Suppl 2015;93:65–9. [DOI] [PubMed] [Google Scholar]
- [9].Magrey M, Khan MA. New insights into synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome. Curr Rheumatol Rep 2009;11:329–33. [DOI] [PubMed] [Google Scholar]


