Abstract
Purpose
To evaluate the effectiveness of Mom Power, a multifamily parenting intervention to improve mental health and parenting among high-risk mothers with young children in a community-based randomized controlled trial (CB-RCT).
Methods
Participants (N = 122) were high-risk mothers (e.g., interpersonal trauma histories, mental health problems, poverty) and their young children (age < 6 years), randomized either to Mom Power, a parenting intervention (treatment condition) or weekly mailings of parenting information (control condition). In this study, the 13-session intervention was delivered by community clinicians trained to fidelity. Pre- and post-trial assessments included mothers’ mental health symptoms, parenting stress and helplessness, and connection to care.
Results
Mom Power was delivered in the community with fidelity and had good uptake (>65%) despite the risk nature of the sample. Overall, we found improvements in mental health and parenting stress for Mom Power participants but not for controls; in contrast, control mothers increased in parent-child role-reversal across the trial period. The benefits of Mom Power treatment (vs. control) were accentuated for mothers with interpersonal trauma histories.
Conclusions
Results of this CB-RCT confirm the effectiveness of Mom Power for improving mental health and parenting outcomes for high-risk, trauma exposed women with young children.
Keywords: community-based randomized controlled trial, parenting intervention, maternal mental health, parenting stress, interpersonal trauma history
Background
Recent attention to the prevalence and consequence of adverse childhood experiences (ACEs), which include experiences of abuse, neglect, and/or exposure to parents with mental illness or substance abuse while growing up, has heightened attention to the potentially devastating consequences of such childhood exposures for both the physical and mental health of the affected adult (Chapman et al. 2011; Dube et al. 2001; Felitti et al. 1998). Such experiences are not rare; indeed, the ACE study showed that 65% of women (and 62% of men) reported having at least one experience of childhood adversity; for those women, physical abuse (27%), sexual abuse (25%), and having a parent with substance disorder (29%) or with mental illness (25%) were among the most prevalent (Centers for Disease Control and Prevention). In addition, a substantial number of women experience interpersonal trauma as adults; nearly 10% of women have been raped by an intimate partner in their lifetime, nearly 15% have experienced sexual violence other than rape by an intimate partner, and up to 33% have experienced physical violence by an intimate partner (Breiding et al. 2014).
In addition to heightening risk for a variety of physical and emotional symptoms, the interpersonal nature of child maltreatment and adult violence, which is often manifest in the context of close primary relationships (e.g., abuse perpetrated by a parent or intimate partner violence), may also impact the adult’s capacity to form loving and trusting relationships, to be empathic to others’ distress, and in the case of being a parent, to be sensitive and empathically attuned during interactions with the adult’s own child (Grasso et al. 2015; Muzik et al. 2013b). Parents who have experienced interpersonal trauma as children or adults are probabilistically more likely to be re-exposed to additional interpersonal violence across their lifespan (Whitfield et al. 2003) and they are at greater risk for disrupted parenting sensitivity with subsequent cascading negative effects on their children’s development (Gustafsson et al. 2015; Lyons-Ruth and Block 1996).
These patterns of intergenerational transmission of risk underscore the need for effective prevention and intervention models for high-risk parents who have experienced childhood and/or adult trauma. In order to interrupt this vicious cycle of intergenerational risk, there is both a critical need to establish actual physical safety for the child and/or adult, as well as an additional critical goal to promote parents’ own sense of safety and mental health. Once safety is established, then the goal can be to enhance the quality of caregiving through strengthening the capacity for empathy, reflection, and sensitive responsiveness to children’s own social and emotional needs, and thereby to scaffold more positive child outcomes. Yet both clinical experience and extant data converge to suggest that there are often a number of barriers that prevent high-risk mothers from engaging with effective treatments. These barriers are both internal such as feelings of distrust, helplessness or shame, as well as external such as lack of transportation or childcare (Muzik et al. 2013a; Muzik et al. 2015a). Thus, although there are many effective home visitation programs (e.g., Early Head Start, Healthy Families America, Maternal Infant Health Program, Nurse Family Partnership), engagement in these programs is often limited, and drop-out rates early in treatment are often high (Azzi-Lessing 2013; McCurdy et al. 2006). Several studies have shown that families at the highest risk, for example younger parents and those exposed to community violence, engage and participate in these programs at the lowest levels (McGuigan et al. 2003; Nicholson et al. 1999). Reasons for this engagement gap are multifactorial; factors such as overwhelming stress, chaos in day-to-day life, lack of knowledge about available services, and prior negative experiences with service providers and the healthcare and welfare system are often cited as contributory (Muzik et al., 2013; Muzik, Kirk, Alfafara, Jonika, & Waddell, 2015). In particular, women with trauma histories do not easily engage in treatments as trauma exposure can change an individuals’ appraisal of what constitutes safe and trustworthy relationships altering health-seeking behaviors (Herman 1992; Liang et al. 2005), which ultimately sabotages treatment engagement.
Despite these challenges, results of qualitative studies with high-risk, trauma exposed mothers of young children also suggest that many women desire a system of care that creates a safe and non-judgmental environment, offers a wide-range of family-focused services (both mental and physical health), is easily accessible and flexible, has respectful providers and communication, and makes accommodations for family-centered practical support (i.e. child care or transportation; Muzik et al. 2013a; Muzik et al. 2015a). This is critical as available evidence does suggest that high-risk, trauma exposed parents who engage in early treatment with their young children (e.g., Nurse Family Partnership, Nurturing Parenting Program) benefit from these interventions (Eckenrode et al. 2010; Maher et al. 2011), and ultimately these interventions are also cost-effective offsetting potential costs to society due to adverse child outcomes (Reynolds and Temple 2008).
Given the risks identified for mothers who have experienced trauma and adversity, coupled with the need for effective programs that enhance treatment engagement, we have developed a brief “soft-safe entry” multi-family intervention, called Mom Power, designed to strengthen protective factors for the individual and within the family system, and geared towards overcoming barriers to engagement. We use the term “soft-safe entry” as a term to describe a treatment engagement stance characterized by emotional safety, acceptance, and a non-judgmental environment for participants. Mom Power is an experiential curriculum, one in which the facilitators create a warm and welcoming environment for participants to experience the concepts that are taught. It is this experience of “felt security and nurturance” during the group process, that enables the mothers to provide “safe haven and secure base” ((Bowlby 1969) for their children thereafter. The fundamental aim of the intervention is to enhance mothers’ wellbeing and positive parenting and to ignite motivation for further connection with care, ultimately improving children’s outcomes.
Mom Power Conceptual Framework: Strengthening Protective Factors to Mitigate Risk
Frameworks for intervention that emphasize the strengthening of protective factors may be particularly appropriate for low-income, trauma-exposed families, where exposures to risk and adversity are frequent. Strengthening Families™: A Protective Factors Framework (Center for the Study of Social Policy 2016) provides a relevant framework with an emphasis on protective factors that promote the resiliency, health, and success of young children and families. Within this approach protective factors are considered to be the conditions or attributes of individuals, families, and communities that reduce the impact of risk and increase positive outcomes for families. These include: (1) Knowledge of Parenting and Child Development, (2) Parental Resilience, (3) Social-emotional Competence of Children, (4) Social Connections, and (5) Concrete Support in Times of Need (Strengthening Families, 2015). Focus on strengthening protective factors, in addition to reduction of risk factors, has been identified to reduce risk for child abuse and neglect (Browne 2014), and programs and services for families are understood to best enhance positive family outcomes through promotion of these protective factors. Mom Power is grounded in the protective factors framework, and program goal is to mitigate the potentially harmful consequences of stress, adversity, and trauma in high-risk families by strengthening and promoting protective factors to enhance parent and child wellbeing. Mom Power is a time-limited program based on attachment-theory (Bowlby 1969), social learning theory (Grusec 1992), and trauma-informed perspective (Cloitre et al. 2009; Herman 1992), and serves families with young children ages 0–5 who have been exposed to high levels of trauma. Mom Power has established feasibility, acceptability, and preliminary efficacy (Muzik et al. 2015b; Muzik et al., 2016).
The Mom Power curriculum rests on five core pillars paralleling the Protective Factors Framework (Muzik et al. 2015b; Strengthening Families™: A Protective Factors Framework 2015). These core pillars are: attachment-based parenting education, self-care, practice, social support, and connection to resources. In the list that follows we briefly describe each of these Mom Power pillars and how they aim to promote specific protective factors.
(1) The Attachment-Based Parenting Education Pillar (Knowledge of Parenting and Child Development)
Psychoeducation is based on attachment-theory (Bowlby, 1969) which highlights the importance of primary relationships and utilizes a Tree metaphor to discuss Bowlby’s attachment concepts of safe haven/secure base (see Figure 1). Within this metaphor mothers gain understanding of children’s capacity to learn and grow at times when they feel safe to explore, to “branch out.” At times when children are distressed or have active attachment needs, mothers are asked to provide a safe haven and meet the need for “connection”, and by doing so the dyad builds and strengthens relational “roots”. The sun in the metaphor represents the warmth, joy and delight that children need from their parents whether they are in moments of exploration (“branching out”) or connection (“building roots”). Throughout the course of Mom Power groups, mothers learn to apply the Tree concepts to caregiving situations. Additionally, we utilize social learning principles (learning takes place in social context of group via observation and modeling) infused with skills-driven practice and exercises from cognitive behavioral therapy (CBT; Beck 2011). Following the weekly curriculum sessions mothers engage in activities (e.g., observing videos, conducting role plays, group discussions) that are designed to practice skills and strengthen insight and sensitive responsiveness to children’s emotional needs. Examples of the Mom Power teaching content and activities have been described in more detail elsewhere (Muzik et al. 2015b).
Figure 1.
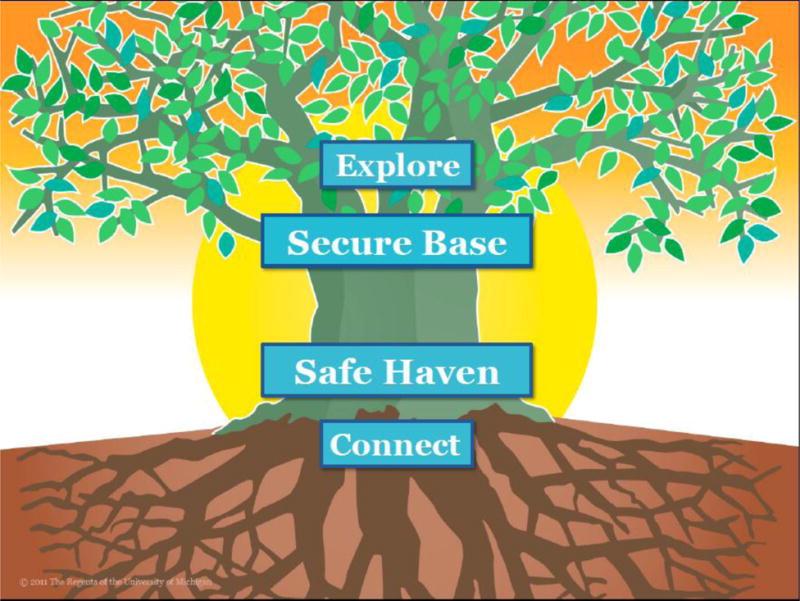
The Mom Power “Tree” Metaphor.
(2) The Self-Care Pillar (Parental Resilience)
Mothers are taught stress reduction, mind-body exercises, and emotion regulation strategies through in class and out of class practice. By the end, they have a self-care “tool kit” including skills such as guided breathing, positive coping thoughts, relaxation, and mindfulness. The curriculum helps mothers build coping skills to help reduce stress, particularly in the context of parenting. Parenting can be a stressful task under any circumstances and parenting stress is exacerbated by other risk factors common to the mothers in Mom Power (e.g., interpersonal violence (IPV) histories, mental health problems, poverty). When a mother feels stressed and overwhelmed or is experiencing symptoms of depression and/or posttraumatic stress disorder, both common to individuals with IPV histories, her own distress can impede her ability to respond calmly and sensitively to her child’s needs. As such, Mom Power helps mothers learn to reduce stress and emotional reactivity in order to build capacity for sensitive caregiving behaviors.
(3) The Practice Pillar (Social-emotional Competence of Children)
The curriculum emphasizes creating safe and predictable routines for mother and child. Real-time support is offered to mothers and children to scaffold skills taught in group regarding sensitive and supportive caregiving. For example, separation (mother leaves to go to group) and reunions (mother returns from group) are intentionally used as “in-vivo” practice opportunities in which mothers are encouraged to notice their child’s behavior, think about their child’s needs, and respond sensitively considering what the child may be thinking or feeling. Within group, leaders help mothers reflect on separations and reunions to identify what went well and what they might like to change/do differently in the future. These discussions map onto the attachment-based curriculum. Mothers also learn developmentally appropriate games, songs, and play activities to use with their child through guided mother-child circle time. Ultimately, this pillar aims to promote social-emotional competence in children by increasing a mother’s awareness of and emotional attunement to her children’s attachment needs. As mothers grow in their emotional attunement, this creates a safe environment for children to express their emotions and have their needs met.
(4) The Social Support Pillar (Social Connections)
Enhancing social support is a key pillar of Mom Power as many of the mothers in Mom Power feel socially isolated and report that they have few people whom they can turn to for support—in parenting and beyond. The group setting offers mothers a chance to connect with other mothers in a safe and supportive environment. The curriculum also has a day when mothers are encouraged to bring someone who supports them (e.g., partner, friend, parent) to help promote “buy in” from critical supports in the mother’s life. “Guest day” is an intentional way for mothers to have the opportunity to share what they have learned, reinforce the importance of parenting support, and communicate to their guest how that person has supported the mother in the past and how they can continue to offer support moving forward. In addition to the “in-group” strategies for building social connections, Mom Power leaders and group attendees brain storm other ways for mothers to build their support networks through strategies such as reaching out to other parents or attending other play groups/parenting groups in the community.
(5) The Connection to Resources Pillar (Concrete Support in Times of Need)
Offering mothers concrete connections to meet their physical and emotional needs beyond the time-limited intervention is an essential component of the Mom Power mission. Connection to care can happen anytime across the 13-week intervention as facilitators monitor each family’s needs and offer “warm handoffs” to other services or providers as needed. In addition to the ongoing connections, individual sessions (held pre, midway, and post group) offer an individualized and private check in with mothers about emotional and physical needs. It is often during these sessions, that mothers feel comfortable reaching out to referral agencies, with the support of the group leader. Referrals range based on family needs but could include things such as individual therapy for the mother, early intervention services, home visitation services, connection to high quality early childhood education programs, legal advocacy and/or safe housing for women in active IPV situations, and/or connection to agencies that provide for basic needs (e.g., food, diapers, car seats). The Mom Power model intentionally fosters a nurturing environment that often creates a safe and trusting relationship between mothers and group leaders. As such, mothers often grow in their willingness to consider other services and follow-up with warm handoffs once that trust is established. Thus, Mom Power actively serves as a treatment engagement program for families by informing families of services, connecting families to services in a personalized and supportive way, and helping families feel safe about accessing services needed to support their physical and emotional needs.
Mom Power: Intervention Structure
The Mom Power intervention is manualized and delivered by two trained Master’s level-prepared clinicians across 13-sessions (3 individual and 10 group sessions), with corresponding parent-and child-group curricula. The target participants are mothers with histories of trauma or abuse (in childhood or adulthood) who may also present with depression, anxiety, and/or high levels of distress, all of which may interfere with sensitive, responsive parenting. The three individual sessions (usually home-based) are scheduled: before group starts, then midway through the 10-week group, and as final exit session post-group. The individual sessions are intended to engage, build therapeutic alliance, and tailor therapeutic messaging and referrals. The 10 group sessions each last 3-hours and mothers participate together with their child(ren) in the age range (0 to 5 years). Group sessions are structured as follows: Group starts with a shared meal for mothers, their children, and intervention facilitators to promote a “soft-safe” group atmosphere. Following the meal, separate “mom” and “child” groups are conducted in two adjacent rooms. Group concludes with a reunion of mother and children followed by a group mother-child “play session” designed to promote shared positive affect, connection, and exposure to developmentally appropriate games and songs. During each of the 10 “mom” group sessions, facilitators present evidence-based parenting and self-care skill concepts in a friendly, interactive, non-judgmental, and accessible format. The Mom Power curriculum is structured but personalized, building a framework for understanding children’s behaviors and paired with tailored feedback that addresses the unique experiences of each mother-child dyad. While mothers are in their group sessions, children attend the “child” group sessions where each child is paired with an adult care provider, typically a university student or agency volunteer, who provides individual attention and a safe, validating, developmentally-appropriate and child-led experience for the child.
The Mom Power Pilot Study: Preliminary Efficacy
We previously reported results of a Mom Power Phase 1 open trial aimed to assess feasibility, acceptability, and pilot outcomes of this intervention (Muzik et al. 2015b). In this pilot, 99 high-risk mother-child dyads were recruited from primary care, community mental health clinics, and fliers posted in community locations. Participating mothers had high trauma-load (75% endorsed at least one type of traumatic experience), 50% presented with a mental health diagnosis (PTSD and/or depression), and participating women were predominantly low income. Despite the high-risk nature of the participants, the intervention had high engagement rate with over 70% of participating mothers attending the full program. The pilot showed that completers (i.e., mothers who attended ≥70% of the 10 group sessions) improved on parenting and mental health outcomes, in contrast to non-completers (i.e., women who attended ≤70% of sessions). In addition, positive treatment effects were most pronounced for women with high baseline (pre-intervention) risk (i.e., a mental health diagnosis, and/or trauma exposure).
Current Study
Given promising open-trial results, a community-based randomized control trial (CB-RCT) was the logical next step to evaluating program effectiveness. In the current paper we present results of such a CB-RCT of Mom Power, again utilizing a sample of mothers with young children from high-risk communities. Importantly, the intervention arm in this CB-RCT was delivered by model-trained community clinicians at agencies that partnered with our university-based research team thus enhancing the ecological validity of the implementation trial.
Methods
This study was approved by the University of Michigan Institutional Review Board (ID# HUM00018944); written, informed consent was obtained from all adults, and each mother was given incentives for data collection during study participation. Details of study assessments and the intervention procedure are discussed in the procedure section.
Participants & Recruitment
Mothers were recruited between September, 2011 and May, 2012 either through self-referral by responding to fliers posted in low-income community locations (e.g., child care facilities, WIC offices, women’s shelters), primary care clinics (family medicine, pediatrics, and OB/GYN), and community mental health clinics, or through active invitation and referral by their primary care or mental health providers. In both recruitment modalities mothers were invited to participate in a research project investigating the benefit of a ‘parenting and self-care’ group. Mothers were enrolled to the study when they presented with at least one risk factor known to interfere with effective parenting of young children. These risk factors included: a mother’s history of childhood maltreatment or adult IPV, past or current depression and anxiety, involvement with child protection services, social isolation (self-perceived/provider-rated), and/or limited access to resources such as food, finances, or housing. Besides risk status, additional inclusion criteria were being at least 15-years-old, English-speaking, and pregnant with a first child or having at least one child in the age range 0–5. Maternal enrollment criteria were assessed through demographic questionnaires, which were site- specific but all tapped into risk factors standardly assessed in the geographic region through public health (www.michigan.gov/mihp/ M500 Maternal Risk Identifier Worksheet).
Interested and eligible mothers engaged in an initial phone call with research staff and were told study specifics of the clinical research trial. The potential participants were informed that once they consented to the study and underwent the baseline assessment that they would be randomized either to a weekly multifamily group [Mom Power Intervention] condition or a weekly mailing [Control] condition (see Study Flow Diagram, Figure 2). A total of 129 women were enrolled into the study; of those, 122 provided written consent and baseline data during a home visit (seven women could not be located after enrollment). Sixty-eight women were allocated to the Intervention condition and 54 to the control condition (see Figure 2).
Figure 2.
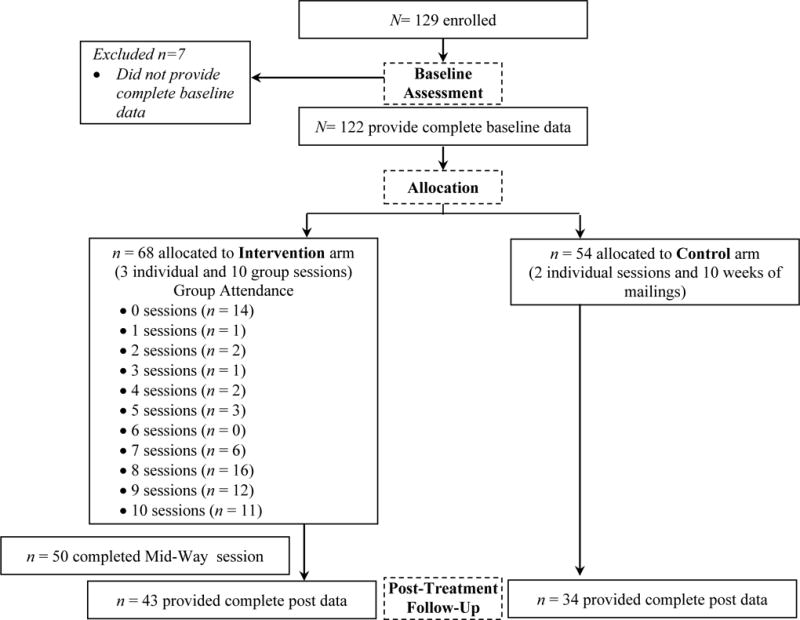
Study Flow Chart
Procedure
Assessments
A pre-trial baseline and a post-trial exit assessment were performed either in the participant’s home or, if preferred, at the primary care/mental health office. At the baseline visit, study staff reviewed study protocol, answered any questions about study participation, and obtained written consent from the mother. Then mothers completed self-report questionnaires on demographics, trauma exposure, mental health, and parenting. Mothers also underwent an interview about parenting attitudes and a standard interaction sequence with their target child that was video-taped for later coding (both interview and interaction data content not in this manuscript). The exit assessment followed the same protocol as the baseline visit; in addition, women provided satisfaction ratings about the multifamily group experience. Women received two $20 payments for completion of survey data during the baseline and the exit visit.
Randomization
Following completion of the baseline assessment, women were randomized using a computer-generated algorithm (urn randomization stratified by baseline trauma exposure and depression to ensure balanced groups (Schulz & Grimes, 2002; Wei & Lachin, 1988) to either the multifamily group [treatment condition] or mailing group [control condition]. This specific type of randomization design is used with small samples to assure that certain key characteristics such as, in our case, maternal trauma-exposure and depression, are equal across both groups. Randomization occurred in blocks of 10–15. Women were informed of their group assignment via phone call within 1 week of the baseline assessment. All women randomized into the control arm were informed that they could participate in the multifamily group free of charge after the study end. All participating women were also informed that during the trial they could continue with any existing services they were already receiving.
Intervention Condition
Women randomized to the intervention arm received the 13-session Mom Power intervention (3 individual sessions and 10 group sessions) led by community clinicians trained in the model (see below training and fidelity). Individual sessions were held at participant’s home or an office (based on preference), and occurred before, midway through, and post 10 weeks of group sessions. All three of the individual sessions were therapeutic in that the manualized content and framework is designed to create a safe and welcoming relationship, to build rapport, to gather information to guide personalization of the intervention, and to help validate mother’s current concerns, thoughts, and feelings. Groups were held at community locations (e.g., churches) or primary care sites, and were co-facilitated by two interventionists, at least one being a Master’s level clinician. On average, group size contained 8–10 mothers, and a total of 8 groups were conducted between October 2011 and August 2012. Mothers received $5 each week as a transportation incentive for group participation. For attending at least 7 of the 10 group sessions mothers were compensated an additional $15 bonus and received a graduation certificate.
Training and fidelity in Mom Power model
Community clinicians of partnering local agencies underwent a 3-day in-person training conducted by the model developers (MM, KR, MS). The intervention is manualized and both individual and group sessions follow a written curriculum. Model fidelity is supported by weekly reflective supervision. In addition, group sessions were video-taped for later coding utilizing a fidelity monitoring scale created by one of the developers (Schuster, 2013). The fidelity scale indexes 12 criteria to evaluate whether facilitators adhered to core components of the Mom Power intervention in regards to content and framework. Each of the 12 criteria are scored on a Likert-scale (ranging from 1–5), with 5 representing the highest and 1 the lowest level of fidelity. The content subscales index fidelity to the manual, such as following the scheduled activities and video discussions, using the content language and presenting the activities as written. The framework subscales index whether facilitators succeeded in setting a therapeutic framework, including creating a welcoming atmosphere, maintaining charge of the group while also responding to concerns, helping to restore emotional balance and working well with co-facilitators. A random sample of 20% of all sessions were scored by the model developer (MS) for fidelity (n= 16 sessions). Summary content and framework subscale scores were computed by averaging item responses on the two subscales. The fidelity criteria were measured on a 1–5 scale, where a 1 generally indicated poor adherence to the model and unacceptable clinical behaviors whereas a 5 generally indicated excellent and advanced clinical skill, and a 3 reflects “good enough” clinical skill with room for improvement. For example, for the framework criteria that “facilitators create a welcoming environment,” a score of 1 reflects, “Facilitators dismiss, ridicule, or are hostile toward participants,” a score of 3 reflects, “Facilitators are warm and inviting some of the time,” and a 5 reflects, “Facilitators are relaxed, smile, validate responses, invite participants to participate most/all of the time.” On average, the groups received a content subscale score of 4.02 (SD = .72) and framework subscale score of 3.85 (SD = .69), both indicating satisfactory fidelity.
Control Condition
Mothers randomized into the control condition also received individual sessions (2 total performed by research staff at baseline and exit) and 10 weekly mailings of the Mom Power curriculum content written in easy to comprehend, 8th –grade level English. The goal of these sessions was the same of the intervention and control conditions; indeed, at baseline the family had not yet been randomized and the goal was to engage the family, build rapport, and to collect assessment data. Weekly control group mailings included a pre-stamped post card for the mother to send back indicating that the week’s material had been read (however. no formal testing on whether the material had been indeed read was done). For each postcard returned the participant was compensated $5. For sending back at least 7 of 10 post cards the participant was compensated an additional $15. Thus, both groups received the same remuneration, and both groups had access to parallel content with regards to the parenting curriculum, albeit delivered in different formats.
Measures
During the baseline and exit assessment mothers self-reported on a range of outcomes via standard rating scales written in easy to comprehend language. All mothers were very respectfully given the option to complete questionnaires verbally with study staff support, yet no participant requested this option suggesting that all mothers were able to read the questionnaires and thus likely had the reading level needed to read the mailed materials in the control condition.
Demographics
Mothers self-reported on age, annual household income, education level, marital status, and race/ethnicity; in addition, they reported on age and gender of all children participating. Participating mothers with more than one child in the age range (0 to 5 years) were asked to indicate one target child (self-selected) and answer all parenting measures specific to the index child.
Trauma exposure
Childhood maltreatment and adult life stress/trauma exposure were assessed using a modified version of the Life Stressor Checklist (Wolfe and Kimerling 1997). Endorsed lifetime stressors were categorized as interpersonal trauma or other trauma. Sums were calculated based on how many events were endorsed for each category (interpersonal trauma vs. other trauma) and to ascertain a total number of traumas experienced across categories. Interpersonal trauma was defined as one person doing something to abusive to another person and included personal childhood exposure to physical, sexual or emotional abuse and neglect, and/or personal adult exposure to harassment, rape and/or physical violence. Other trauma was defined as traumatic events that were not interpersonal (victim/perpetrator) in nature and included being in a serious accident, experiencing an unexpected death of someone close, taking care of someone seriously ill and witnessing or hearing of someone being brutally harmed or murdered.
Mental health
Depression symptoms and diagnosis were assessed using the Postpartum Depression Screening Scale (PPDS; Beck and Gable 2001), a 35 item, five-point Likert scale, self-report questionnaire indicating whether participants strongly agree to strongly disagree on items tapping into symptoms consistent with depression. A cutoff score of ≥ 80 indicates a clinical diagnosis for major post-partum depression. The PPDS has a high sensitivity of 94% and a specificity of 98% for major depression. In our sample, Cronbach’s alpha at baseline is .97.
PTSD symptoms and diagnosis were assessed using The National Women’s Study PTSD Module (NWS-PTSD) (Kilpatrick et al. 1989), a 17 item self-report scale probing for the presence and absence of all 17 symptoms consistent with a PTSD diagnosis in DSM-IV (American Psychiatric Association 1994). A scoring algorithm provides a total symptom count and meeting criteria for DSM-IV PTSD diagnosis (American Psychiatric Association 1994). The NWS-PTSD has high sensitivity of 96% and specificity of 80% for current PTSD (Resnick et al. 1993). In our sample, Cronbach’s alpha at baseline is .89.
Parenting
Parenting stress was measured via the Parenting Stress Index-short form (PSI-SF) (Abidin 1995) and other parenting outcomes (i.e., helplessness, role reversal) were measured via subscales from the Caregiving Helplessness Questionnaire (CHQ; (George & Solomon, 2011). The PSI-SF is a widely used, well -validated 36-item, five-point Likert scale, self-report measure yielding a total score on perceived parenting stress and 3 subscale scores (parental distress, parent-child dysfunctional-interaction, and difficult child). In this study we utilized the total score. In our sample, Cronbach’s alpha for PSI-SF at baseline is .91. Two subscales of the Caregiving Helplessness Questionnaire (CHQ; (Solomon and George 2008) were also used to assess parenting: caregiver helplessness and child caregiving behaviors, which indicates role-reversal for the parent-child relationship. Items are scored on a 5-point scale indicating how characteristic each statement is to the parent and/or child. Both subscales utilized are comprised of a sum of appropriate items. The CHQ has been shown to have sound psychometrics (George and Solomon 2011). In our sample, Cronbach’s alpha for CHQ subscales is .66 for caregiving helplessness and .79 for child caregiving behaviors at baseline.
Connection to care
Using the Connection to Services Tracking Sheet (Muzik et al. 2009) study staff tracked any referrals given to participants in the course of participation in the Mom Power trial. Referrals were tracked by recipient (mother or child) and type of referral (mental and/or physical health, substance use treatment, individual therapy, child developmental assessment, home-based services or child-care center, case management for tangibles/housing/insurance, educational assistance). The Connection to Services Tracking Sheet was completed anytime across the study duration if/when a family was given a referral. Additionally, a 6-item self-report retrospective questionnaire (Rosenblum 2009) was completed at the follow-up assessment and assessed mothers’ perceptions of their connection to community professionals (doctors, nurses, social workers, counselors, etc.), understanding of their child(ren)’s behaviors, and comfort with seeking assistance or support from existing social supports. Each item was rated on two 6-point Likert scales, first asking mothers to rate what they recalled as their perception before at baseline, and second, reporting on their current perception after program participation.
Participant satisfaction
Participants were given a self-report evaluation of the perceived helpfulness of the intervention and to tap into protective factors that strengthen family functioning at the post-trial assessment only. The protective factors identified for positive family functioning are as follows: 1. Enhancing parental resilience; 2. Providing an array of social connections; 3. Providing parents with concrete support in times of need; 4. Facilitating knowledge of parenting and child development; and 5. Supporting healthy social & emotional development in young children. This 28-item survey (Muzik and Stanton 2009) utilizes a 5-point Likert scale to indicate the level of agreement with a series of statements regarding the program’s content, delivery and the participants’ overall experience and learning.
Analyses and Hypotheses
Statistical analysis was performed using SPSS v.22, and all hypotheses with a priori specified directional effects (i.e., hypothesized reduction in mental health symptoms and improvement in parenting) utilized 1-tailed significance tests. Baseline differences on mental health and parenting ratings between treatment and control groups were assessed using independent samples t-tests and chi-square tests. Outcome analyses are based on intention to treat analyses. Given the relatively small sample size for each condition, primary analyses used paired-sample t-tests run separately by condition in order to assess changes from baseline to post-trial on mental health and parenting variables in the control and treatment groups. Additionally, dosing effects for women in the treatment condition were assessed via correlations between attendance and change scores in outcome variables. Group attendance was defined as the number of weeks attended and change scores were computed for mental health and parenting variables by subtracting the post-group score from the pre-group score. A positive change score indicated that the variable score dropped across the intervention period, whereas a negative change score indicated that the variable score got higher across the trial period.
We hypothesized that women in the treatment condition (Mom Power) would show improvements in mental health, parenting, and connection to care, and that women in the control condition would evidence no changes on these outcomes. In addition, given our pilot data showing that Mom Power was most effective for higher-risk women (Muzik et al. 2015b) in the present study we also predicted that women with greater baseline risk, that is, those endorsing a history of interpersonal trauma, would show greater treatment response than women without interpersonal trauma histories.
Results
Demographics of Sample
Demographic and baseline data are available for mothers who provided baseline data (N = 122). Of these, 68 were randomized into the intervention condition and 54 to the control condition. Women in both conditions were balanced on demographic, mental health and trauma variables (see Table 1).
Table 1.
Participant Characteristics
| Baseline Characteristics between Conditions (N = 122)
| ||||
|---|---|---|---|---|
| Domain | Mom Power (n = 68) |
Control Condition (n = 54) |
||
|
| ||||
| Mean (SD) or n (%) | Mean (SD) or n (%) | t or X2 | p-value | |
| Demographics | ||||
| Age | 23.69 (8.04) | 23.33 (5.97) | 0.27 | .786 |
| Child Age | 14.77 (13.30) | 19.82 (17.17) | −1.70 | .093 |
| Education | ||||
| Less than H.S. | 30 (44.12%) | 18 (33.33%) | 1.47 | .226 |
| More than H.S. | 38 (55.88%) | 36 (66.67%) | ||
| Income | ||||
| Less than 15k/yr | 43 (64.18%) | 31 (58.49%) | 0.41 | .524 |
| More than 15k/yr | 24 (35.82%) | 22 (41.51%) | ||
| Marital Status | ||||
| Single | 44 (64.71%) | 35 (64.81%) | 0.00 | .990 |
| Partnered | 24 (35.29%) | 19 (35.19%) | ||
| Race | ||||
| Minority | 47 (69.12%) | 39 (72.22%) | 0.14 | .709 |
| Caucasian | 21 (30.88%) | 15 (27.78%) | ||
| Trauma Exposure | ||||
| # of Traumas IPV | 5.54 (3.60) | 4.94 (3.53) | 0.92 | .358 |
| IPV in Childhood | 44 (64.71%) | 30 (55.56%) | 1.06 | .304 |
| Environmental Trauma | 30 (44.1%) 61 (89.71%) |
23 (42.6%) 50 (92.59%) |
0.28 0.31 |
.866 .580 |
|
| ||||
| Mental Health | ||||
| Baseline PTSD symptoms | 6.71 (5.54) | 5.63 (4.27) | 1.34 | .184 |
| Baseline MDD symptoms | 82.94 (33.47) | 78.31 (27.24) | 0.82 | .411 |
|
| ||||
| Connection to Care | ||||
| Receiving mental health services at baseline | 20 (29.41%) | 13 (24.07%) | 0.44 | .510 |
Note. H.S. = High School, k = $1000, IPV = Interpersonal violence/trauma, PTSD = Posttraumatic Stress Disorder, MDD = Major Depressive Disorder, MP = Mom Power.
Overall, participants in the total sample (N = 122) were predominantly members of an ethnic/racial minority group (n = 86, 71%), young (Mage= 24 years), single (n = 79, 65%), lower educational attainment (n = 48, 39% < high school), and low-income (n = 74, 62% < $15,000 annual household income) mothers with young children (Mage= 16.5 months). At the baseline assessment 74 (61%) mothers reported exposure to interpersonal trauma, 41 (34%) met criteria for PTSD and 55 (45%) for a depression diagnosis based on self-report measures. Ninety-one percent of all women experienced at least one non-interpersonal (other) trauma in their life time. Only 33 (27%) women were already receiving any mental health services for themselves at the baseline assessment.
Adherence
Of the 68 women allocated to the intervention arm, fourteen mothers (20%) dropped out before the first session; these immediate drop-outs did not differ from those who attended on baseline demographic, trauma or mental health variables (p=ns). Attendees received an average of 6 (SD = 4) group sessions; 45 (66%) participants attended at least 7 out of the 10 possible group sessions. In our pilot study (Muzik et al. 2015b) we identified that attending at least 7 of the 10 group sessions (“completers”) accounted for positive treatment effect. In the control arm, 42 (78%) women mailed back at least 7 out of 10 cards indicating that they had read the material. Post-trial assessments were completed on 43 (63%) of women in the intervention arm, and 34 (63%) of women in the control arm; attrition for exit data collection was equal across conditions (p = ns). Not completing a post-trial assessment was significantly related to non-completion of group (X2 = 29.49, p < .001) for women in the treatment condition, and to lower than high school educational attainment in the control condition (X2 = 4.14, p < .05). Mental health diagnosis, traumatic experiences, and socioeconomic variables were unrelated to completing a post-trial assessment for either condition. The satisfaction rating of treatment arm completers (n = 43) was high: 37 (95%) reported feeling better able to understand their child’s needs, 36 (92%) felt supported from other mothers in the group, 37 (93%) reported receiving useful information about parenting, and 38 (95%) felt welcomed to share their thoughts, feelings and struggles as a parent. Similarly, the control group also received the same satisfaction measure as those in the intervention, but questions specific to group attendance were eliminated (i.e. satisfaction with location, facilitators, meal, etc), and control group satisfaction with the information received was high.
Primary Outcomes
1. Maternal Mental Health
Mean level scores for self-reported mental health symptoms before and after the trial by randomization condition are displayed in Table 2. Women in the intervention condition decreased significantly on PTSD symptoms (p < .05), whereas women in the control condition significantly decreased in depression symptoms (p < .05).
Table 2.
Mental Health and Parenting Outcomes
| Mom Power (n = ~44) | Control Condition (n = ~34) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Baseline | Post-Treatment | Baseline | Post-Treatment | ||||||||
|
| |||||||||||
| Domain | Measure | M (SD) | M (SD) | t (n) | p-value | d | M (SD) | M (SD) | t (n) | p-value | d |
| Mental Health | Depression Symptoms | 80.19 (29.93) | 74.63 (25.88) | 1.48 (44) | .147 | .199 | 77.43 (29.00) | 69.96 (34.77) | 1.99 (34) | .055* | .233 |
| PTSD Symptoms | 6.71 (4.53) | 5.21 (4.23) | 2.44 (43) | .019* | .342 | 5.18 (4.31) | 4.29 (4.81) | 1.68 (34) | .103 | .195 | |
| Parenting | Parenting Stress | 76.77 (22.36) | 69.91 (18.49) | 1.87 (40) | .069* | .334 | 79.16 (22.57) | 74.97 (21.41) | 1.63 (31) | .113 | .190 |
| Caregiving Helplessness | 10.19 (4.31) | 9.71 (3.87) | .75 (38) | .459 | .117 | 10.79 (3.98) | 10.33 (4.65) | .65 (30) | .522 | .106 | |
| Child Caregiving Behavior | 21.19 (5.33) | 21.94 (5.80) | −.95 (36) | .350 | −.135 | 20.21 (7.08) | 22.14 (6.19) | −2.11 (29) | .045* | −.290 | |
Note. PTSD = Posttraumatic Stress Disorder.
p < 0.05
Consistent with prior evaluation of MP (Muzik et al. 2015b), we predicted that treatment effects would be most pronounced for women with baseline risk. Therefore, we reanalyzed the data on mental health outcomes separately for the subsample of women who endorsed interpersonal trauma history at baseline. Results of these sub analyses among women with a history of interpersonal trauma (n = 43) show significant decreases in mental health symptoms for the Mom Power treatment condition (Depression: p < .05; and PTSD: p < .05; see Table 3), and no changes in mental health symptoms for the control condition.
Table 3.
Mental Health and Parenting Outcomes for Baseline Sample with History of IPV
| Mom Power (n = ~ 27) | Control Condition (n = ~17) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Baseline | Post-Treatment | Baseline | Post-Treatment | ||||||||
|
| |||||||||||
| Domain | Measure | M (SD) | M (SD) | t (n) | p-value | d | M (SD) | M (SD) | t (n) | p-value | d |
| Mental Health | Depression Symptoms | 94.23 (28.21) | 81.63 (26.28) | 2.54 (27) | .017* | .462 | 82.27 (30.22) | 76.73 (39.97) | 0.90 (17) | .381 | .156 |
| PTSD Symptoms | 8.27 (4.36) | 6.46 (4.66) | 2.11 (26) | .046* | .401 | 7.47 (3.67) | 6.29 (4.91) | 1.33 (16) | .204 | .272 | |
| Parenting | Parenting Stress | 85.52 (21.74) | 72.23 (18.86) | 1.87 (24) | .075T | .653 | 81.78 (21.39) | 77.82 (21.54) | 0.33 (16) | .333 | .184 |
| Caregiving Helplessness | 12.11 (4.40) | 10.56 (4.42) | 1.69 (23) | .106 | .351 | 11.31 (4.13) | 11.19 (5.39) | .10 (16) | .918 | .025 | |
| Child Caregiving Behavior | 20.90 (5.67) | 21.24 (6.05) | −.31 (21) | .761 | −.058 | 20.25 (7.98) | 22.94 (5.54) | −2.17 (16) | .046* | −.391 | |
Note. IPV = Interpersonal violence, PTSD = Posttraumatic Stress Disorder.
p < 0.05;
p < 0.10
2. Parenting Outcomes
Mean level parenting scores before and after the trial by randomization condition are displayed in Table 2. Regarding parenting stress, there was a significant decrease in PSI-SF total score for women in the treatment condition (p < .05) but not for controls. Regarding role-reversal, there was a significant increase in the Child Caregiving Behavior Subscale of the CHQ, suggestive of increased role-reversal, but only for women in the control condition (p < .05). There were no significant changes in either condition for the Caregiving Helplessness subscale of the CHQ.
Consistent with prior analyses, we computed pre-post-tests on parenting variables for subset of women with interpersonal trauma history at baseline (see Table 3). In these analyses, women in the Mom Power treatment condition continued to demonstrate a significant decrease in parenting stress (p < .05), while women in the control condition did not. In addition, women in the control condition continued to show a significant increase in Child Caregiving Behavior (p < .05), suggesting increased role-reversal in these parent-child relationships.
3. Connection to Care
In the Mom Power treatment condition, 35 (51.5%) of families were given referrals by the study team for additional services, whereas in the control condition only 5 (11%) received targeted referrals (X2 = 24.34, p < .001). Referrals were predominantly for further mental health services (primarily home-based) and tangible goods assistance (food, housing, clothing assistance, etc.). Women also rated their perceived change in connection to care from pre-to-post assessment on a 6-item survey as a result of the trial; scores on these subjective ratings improved for both groups (from Mpre = 5.3 (SD = 2.76) to Mpost = 7.5 (SD = 2.38) (t(41) = −2.17, p < .001) for Mom Power and Mpre = 6.00 (SD = 2.07) to Mpost = 7.30 (SD = 2.32) (t(29) = −4.28, p < .001) for controls).
4. Intervention Satisfaction
Participants rated acceptance and helpfulness of the intervention in a 28-item survey (Muzik & Stanton, 2009) that was rated using a 5-point Likert scale (1=strongly disagree to 5=strongly agree). The questionnaire was composed of statements about their experience with the program, group format, facilitators, other group attendees and knowledge gained.
5. Dosing
For the overall group of women in the Mom Power treatment condition, there were no significant correlations between attendance and change scores in mental health or parenting variables. However, in sub analyses for women in the treatment condition with interpersonal trauma (versus those without), we did find significant results for the parenting domain. Specifically, women with at least one interpersonal trauma experience (n=23) showed significant correlation between attendance rate and positive change score on caregiving helplessness, a subscale on the CHQ (r = .47, p < .05), indicating the more groups they attended the greater the positive effect on caregiving helplessness (i.e., greater drop in caregiving helplessness score from pre to post).
Discussion
The present study tested the effectiveness of Mom Power, a multifamily parenting and mental health intervention for high-risk mothers and their young children, using a community-based randomized control trial (CB-RCT). Mom Power is a theory-driven, time limited (13 sessions), and manualized intervention that aims for broad reach, easy access, good acceptance among target population, and to strengthen protective factors both within the individual and the whole family. The ultimate goal is to promote mothers’ mental health and positive parenting, which is assumed to have positive downstream effects on children’s wellbeing. The study was conducted in partnership with community agencies with the intervention delivered by trained community clinicians, strengthening the ecological validity of the findings.
Results from this CB-RCT suggest that participation in Mom Power was associated with improvements in mental health and parenting, and that the impact of the Mom Power group was most pronounced for women with an interpersonal violence/trauma (IPV) history. Specifically, among women with a history of IPV, only those assigned to the Mom Power intervention condition demonstrated a significant decrease in PTSD symptoms, depression symptoms, and parenting stress; IPV-exposed women assigned to the control condition showed no change in mental health symptoms and, in contrast to the Mom Power group, demonstrated a worsening pattern for certain parenting indicators. Additionally, women with a history of IPV exhibited dosing effects with their gains in feelings of caregiver efficacy correlating positively to the number of weeks that they attended group.
Importantly, it is clear that a 13-session intervention may not be sufficient for meeting the needs of all participants, and in this regard, it is particularly meaningful that results revealed that participation in the Mom Power intervention led to more treatment referrals and to self-reported increased engagement in additional community-based services; half of the families from the treatment arm connected with follow up services as opposed to only 11% of families in control arm. The referrals utilized were broad and spanned from services that addressed tangible needs to therapeutic offerings, such as mental health services or home-based mother-infant psychotherapy. This outcome is particularly important, as this increased and sustained engagement in services and treatment offerings has potential for even more sustained, long-term improvements for mother and child and the family system. Taken together these findings underscore the value of Mom Power as treatment-engagement intervention, functioning as a safe “soft-entry” to treatment for those who otherwise might not receive relevant referrals and/or might be hesitant to accept and follow through with referrals provided.
Additional evidence of the value of Mom Power as a treatment-engagement preventive intervention comes from the data suggesting that despite high levels of economic and demographic adversity fully two-thirds of the mothers enrolled in the Mom Power treatment arm attended at least 7 group sessions, the number of sessions previously determined to be necessary for therapeutic benefit (Muzik, Rosenblum, et al., 2015). Furthermore, group attendees did not differ from those women who dropped out. In the current study drop out was most common before the mother even attended the first multifamily group session (n = 14, 20%), which is a common occurrence in parenting programs reported also by others (Azzi-Lessing 2013; McCurdy et al. 2006). Previously, in our open pilot study we have found differential predictions to engagement to the Mom Power intervention based on race (Muzik et al. 2014), but this was not the case in this trial.
In addition to evidence for a positive therapeutic benefit of participation in Mom Power, mothers who participated also endorsed high levels of satisfaction rates with the intervention. In general, > 90 % of mothers in the treatment arm reported that they perceived the intervention to have helped them understand their child’s needs and how to respond, and that they felt supported by peers and facilitators throughout the group process. The Mom Power intervention is intentionally delivered as group format in order to counteract stigma and sense of social isolation that many high-risk mothers experience, and because it enhances opportunities to both give and receive peer support, both of which have been identified as beneficial in prior peer-to-peer intervention research (Maton 1988; Pagano et al. 2010; Roberts et al. 1999). The group approach, coupled with a strengths-based emphasis on promoting protective factors, is designed to empower mothers and enhance their sense of connectedness to other women who have faced and addressed similar challenges and circumstances.
There are several limitations of this study. First, as Mom Power is a potential tool for treatment engagement to further services, study results would be strengthened by the addition of objective data on whether women followed through with referrals. Second, attrition for post-Mom Power assessment was high (37%) due to competing clinical demands for community clinicians, who collected the data in the intervention group, interfering with data collection. Third, data on child outcomes would allow for further analysis examining correlations between potential changes in maternal behaviors and how they relate to child outcomes. Lastly, a later follow up assessment, for example 6 or 12 months post-trial termination would be beneficial to test the long-term impact of the intervention.
Conclusion and Clinical Implications
Results of this CB-RCT confirm the effectiveness of Mom Power for improving mental health and parenting outcomes for high-risk, trauma exposed mothers of young children. Given that this RCT was based in the community with community clinicians, the results have several meaningful clinical implications. These results support the notion that implementation of the Mom Power intervention is feasible for community-based clinicians and that they are able to implement Mom Power with fidelity. These findings have significant implications for implementation and dissemination research and provide a framework for how to develop, evaluate, and disseminate interventions that are evidence-based, feasible for community clinicians, and effective in the communities in which they aim to serve. The high retention rates across the intervention also suggest that this multi-family group provides a safe, welcoming place for these high-risk mothers to find support in parenting. From a clinical perspective, Mom Power joins other parenting-enhancing therapies geared towards high-risk mothers and their young children (for review see (Muzik et al. 2015b; Muzik et al. 2014), all of which have the ultimate goal to interrupt intergenerational transmission of risk, and instead, strengthen the family’s protective factors and resilience. Current research supports that through attention to mothers’ needs for social support, parenting education, stress-reduction and self-care, as well as through connecting them to community resources and care, these mothers, despite a traumatic past or adverse current living circumstances, may positively impact their children’s life trajectories.
Acknowledgments
The research presented was supported through funds from the State of Michigan, Department of Community Health, (PI: Muzik, F023865-2009 and F029321-2010); Michigan Institute for Clinical & Health Research (MICHR) (PI: Rosenblum, UL1RR024986-2010), and the Robert Wood Johnson Health & Society Scholars Program (PI: Muzik; N012918-2010). We thank the community agencies (i.e., Starfish Family Services, Inkster, Michigan; The Guidance Center, Southgate, Michigan) and their clinicians serving the families for participating in this trial. We thank the families who participated in this project. We acknowledge the valuable efforts of the Mom Power project staff in program development, implementation and data collection.
Footnotes
Disclosures of Conflicts of Interest: none
ClinicalTrials.gov Identifier: NCT01554215
References
- Abidin RR. Parenting Stress Index: Professional Manual. 3. Psychological Assessment Resources, Inc; Odessa, FL: 1995. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: Diagnostic criteria from DSM-IV. American Psychiatric Association; 1994. [Google Scholar]
- Azzi-Lessing L. Serving Highly Vulnerable Families in Home-Visitation Programs. Infant Mental Health Journal. 2013;34:376–390. doi: 10.1002/imhj.21399. [DOI] [Google Scholar]
- Beck CT, Gable RK. Further validation of the Postpartum Depression Screening Scale. Nursing Research. 2001;50:155–164. doi: 10.1097/00006199-200105000-00005. [DOI] [PubMed] [Google Scholar]
- Beck JS. Cognitive behavior therapy: basics and beyond. xix. Guilford Press; New York: 2011. p. 391. [Google Scholar]
- Bowlby J. Attachment. Basic Books; New York: 1969. [Google Scholar]
- Breiding MJ, Chen J, Black MC. Intimate Partner Violence in the United States — 2010. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; Atlanta, GA: 2014. [Google Scholar]
- Browne CH. National Quality Improvement Center on Early Childhood. Zero to Three. 2014;35:2–9. [Google Scholar]
- Center for the Study of Social Policy. Strengthening Families: A Protective Factors Framework. 2016 http://www.cssp.org/reform/strengtheningfamilies. Accessed January 6, 2016.
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Violence Prevention Prevalence of Individual Adverse Childhood Experiences. 2016 Jan 6; http://www.cdc.gov/violenceprevention/acestudy/prevalence.html.
- Chapman DP, et al. Adverse childhood experiences and sleep disturbances in adults. Sleep Med. 2011;12:773–779. doi: 10.1016/j.sleep.2011.03.013. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stolbach BC, Herman JL, van der Kolk B, Pynoos R, Wang J, Petkova E. A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress. 2009;22:399–408. doi: 10.1002/jts.20444. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA. 2001;286:3089–3096. doi: 10.1001/jama.286.24.3089. doi:joc11276 [pii] [DOI] [PubMed] [Google Scholar]
- Eckenrode J, et al. Long-term effects of prenatal and infancy nurse home visitation on the life course of youths: 19-year follow-up of a randomized trial. Archives of pediatrics & adolescent medicine. 2010;164:9–15. doi: 10.1001/archpediatrics.2009.240. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, et al. The relationship of adult health status to childhood abuse and household dysfunction. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- George C, Solomon J. Disorganized attachment and caregiving. First. Guilford Press; New York: 2011. [Google Scholar]
- Grasso DJ, Henry D, Kestler J, Nieto R, Wakschlag LS, Briggs-Gowan MJ. Harsh Parenting As a Potential Mediator of the Association Between Intimate Partner Violence and Child Disruptive Behavior in Families With Young Children. Journal of Interpersonal Violence. 2015 doi: 10.1177/0886260515572472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grusec JE. Social learning theory and developmental psychology: The legacies of Robert Sears and Albert Bandura. Developmental Psychology. 1992;28:776–786. doi: 10.1037/0012-1649.28.5.776. [DOI] [Google Scholar]
- Gustafsson HC, Coffman JL, Cox MJ. Intimate Partner Violence, Maternal Sensitive Parenting Behaviors, and Children's Executive Functioning. Psychology of violence. 2015;5:266–274. doi: 10.1037/a0037971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman J. Trauma and Recovery: The Aftermath of Violence – from Domestic Abuse to Political Terror. Basic Books; New York: 1992. [Google Scholar]
- Kilpatrick DG, Resnick HS, Saunders BE, Best CL. The National Women's Study PTSD Module. Medical University of Souh Carolina; Charleston, SC: 1989. [Google Scholar]
- Liang B, Goodman L, Tummala-Narra P, Weintraub S. A Theoretical Framework for Understanding Help-Seeking Processes Among Survivors of Intimate Partner Violence. Am J Community Psychol. 2005;36:71–84. doi: 10.1007/s10464-005-6233-6. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Block D. The disturbed caregiving system: Relations among childhood trauma, maternal caregiving, and infant affect and attachment. Infant Mental Health Journal. 1996;17:257–275. doi: 10.1002/(sici)1097-0355(199623)17:3<257::aid-imhj5>3.0.co;2-l. [DOI] [Google Scholar]
- Maher EJ, Marcynyszyn LA, Corwin TW, Hodnett R. Dosage matters: The relationship between participation in the Nurturing Parenting Program for infants, toddlers, and preschoolers and subsequent child maltreatment. Children and youth services review. 2011;33:1426–1434. doi:http://dx.doi.org/10.1016/j.childyouth.2011.04.014. [Google Scholar]
- Maton KI. Social support, organizational characteristics, psychological well-being, and group appraisal in three self-help group populations. Am J Community Psychol. 1988;16:53–77. doi: 10.1007/BF00906072. [DOI] [PubMed] [Google Scholar]
- McCurdy K, et al. Understanding maternal intentions to engage in home visiting programs. Children and youth services review. 2006;28:1195–1212. doi: 10.1016/j.childyouth.2005.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuigan WM, Katzev AR, Pratt CC. Multi-level determinants of retention in a home-visiting child abuse prevention program. Child Abuse & Neglect. 2003;27:363–380. doi: 10.1016/s0145-2134(03)00024-3. [DOI] [PubMed] [Google Scholar]
- Muzik M, Ads M, Bonham C, Rosenblum KL, Broderick A, Kirk R. Perspectives on trauma-informed care from mothers with a history of childhood maltreatment: A qualitative study. Child Abuse & Neglect. 2013a;37:1215–1224. doi: 10.1016/j.chiabu.2013.07.014. doi:http://dx.doi.org/10.1016/j.chiabu.2013.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M, Bocknek EL, Broderick A, Richardson P, Rosenblum KL, Thelen K, Seng JS. Mother–infant bonding impairment across the first 6 months postpartum: The primacy of psychopathology in women with childhood abuse and neglect histories. Archives of Women's Mental Health. 2013b;16:29–38. doi: 10.1007/s00737-012-0312-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M, Kirk R, Alfafara E, Jonika J, Waddell R. Teenage mothers of black and minority ethnic origin want access to a range of mental and physical health support: a participatory research approach. Health Expectations:n/a-n/a. 2015a doi: 10.1111/hex.12364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M, Miller N, Alfafara E. Mom Power Connection to Services Tracking Sheet 2009 [Google Scholar]
- Muzik M, Rosenblum KL, Alfafara EA, Schuster MM, Miller NM, Waddell RM, Kohler ES. Mom Power: preliminary outcomes of a group intervention to improve mental health and parenting among high-risk mothers. Archives of Women's Mental Health. 2015b doi: 10.1007/s00737-014-0490-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M, Schmicker M, Alfafara E, Dayton C, Schuster M, Rosenblum KL. Predictors of Treatment Engagement to the Parenting Intervention Mom Power Among Caucasian and African American Mothers. Journal of Social Service Research. 2014:1–19. doi: 10.1080/01488376.2014.917451. [DOI] [Google Scholar]
- Muzik M, Stanton E. Mom Power Group Evaluation. 2009. Unpublished Survey. [Google Scholar]
- Muzik M, Rosenblum K, Schuster M, Kohler E, Alfafara E. A Mental Health and Parenting Intervention for Adolescent and Young Adult Mothers and their Infants. J Depress Anxiety. 2016;5(233):2167–1044.1000233. [Google Scholar]
- Nicholson B, Brenner V, Fox R. A community-based parenting program with low-income mothers of young children. Families in Society: The Journal of Contemporary Social Services. 1999;80:247–253. [Google Scholar]
- Pagano ME, Post SG, Johnson SM. Alcoholics Anonymous-Related Helping and the Helper Therapy. Principle Alcoholism treatment quarterly. 2010;29:23–34. doi: 10.1080/07347324.2011.538320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61:984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Reynolds AJ, Temple JA. Cost-effective early childhood development programs from preschool to third grade. Annual review of clinical psychology. 2008;4:109–139. doi: 10.1146/annurev.clinpsy.3.022806.091411. [DOI] [PubMed] [Google Scholar]
- Roberts LJ, Salem D, Rappaport J, Toro PA, Luke DA, Seidman E. Giving and receiving help: interpersonal transactions in mutual-help meetings and psychosocial adjustment of members. Am J Community Psychol. 1999;27:841–868. doi: 10.1023/a:1022214710054. [DOI] [PubMed] [Google Scholar]
- Rosenblum KL. Mom Power Retrospective Pre-post Questionnaire. 2009. Unpublished Survey. [Google Scholar]
- Schulz KF, Grimes DA. Allocation concealment in randomised trials: defending against deciphering. Lancet. 2002;359(9306):614–618. doi: 10.1016/S0140-6736(02)07750-4. [DOI] [PubMed] [Google Scholar]
- Schuster M. Mom Power Fidelity Scale. 2013. Unpublished Survey. [Google Scholar]
- Solomon J, George C. The measurement of attachment security and related constructs in infancy and early childhood. In: Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research and clinical applications. 2. Guilford Press; New York, NY: 2008. pp. 383–416. [Google Scholar]
- Strengthening Families™: A Protective Factors Framework. 2015 http://www.cssp.org/reform/strengtheningfamilies. Accessed August 16, 2015.
- Wei L, Lachin JM. Properties of the urn randomization in clinical trials. Control Clin Trials. 1988;9(4):345–364. doi: 10.1016/0197-2456(88)90048-7. [DOI] [PubMed] [Google Scholar]
- Whitfield CL, Anda RF, Dube SR, Felitti VJ. Violent childhood experiences and the risk of intimate partner violence in adults assessment in a large health maintenance organization. Journal of Interpersonal Violence. 2003;18:166–185. [Google Scholar]
- Wolfe J, Kimerling R. Gender issues in the assessment of posttraumatic stress disorder. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. Guilford Press; New York, NY US: 1997. pp. 192–238. [Google Scholar]


