Abstract
In China, acute stigma accompanying an HIV diagnosis can lead to self-isolation. In a cultural setting where family relationships are highly valued and contribute critically to well-being, such self-isolation can thwart HIV self-management and engagement in medical care, and so heighten risk for health disparities. To understand this phenomenon, we conducted individual in-depth interviews with 34 persons living with HIV/AIDS (PLWHA) in Shanghai and Beijing. Inductive content analysis revealed a range of forms of self-isolation motivation, beliefs, and behaviors influenced by: 1) internalized stigma and desire to avoid discrimination; 2) HIV-related factors such as HIV-knowledge and disease progression: and 3) familial factors such as a sense of responsibility and family members’ reactions. Based on a proposed framework centering on dialectical family influences (whereby PLWHA are pushed away from, yet pulled toward the family fold), implications for provision of multidisciplinary care in medical settings are considered, including culturally appropriate strategies to decrease health disparities.
Keywords: HIV/AIDS, self-isolation, stigma, social support, China
INTRODUCTION
Approximately 501,000 people are living with HIV/AIDS (PLWHA) in China, of which 205,000 are living with AIDS (UNAIDS, 2015). Given the acute HIV stigma in China, among healthcare providers as well as the general population (Yang, Leu, Simoni, Chen, Shiu, & Zhao, 2015), Chinese PLWHA are at risk for diminished physical and mental health outcomes and poorer overall quality of life (Niu, Luo, Liu, Silenzio, & Xiao, 2016; Yang, Xie, Simoni, Shiu, Chen, Zhao, et al., 2016). Persons of lower socio-economic status, rural origin, and ethnic or sexual minority status, face additional and intersecting challenges to optimal health (Tao, Kipp, Liu, Zhang, Ruan, Yin et al., 2015).
The U.S. Department of Health and Human Services’ Healthy People 2020 Initiative recognizes that a disparity exists when a difference in health outcomes is seen “to a greater or lesser extent between populations,” and that “disability, race or ethnicity, sex, sexual identity, age, disability, socioeconomic status, and geographic location all contribute to an individual’s ability to achieve good health” (U.S. Department of Health and Human Services, 2010). A “health disparity” according to Healthy People 2020 is “a particular type of health difference that is closely linked to social, economic, and/or environmental disadvantage. Health disparities adversely affect groups of people who have systematically experienced greater obstacles to health based on their racial or ethnic group; religion; socioeconomic status; gender; age; mental health; cognitive, sensory, or physical disability; sexual orientation or gender identity; geographic location; or other characteristics historically linked to discrimination or exclusion.” The Initiative underscores the need to recognize the impact of such social determinants on health and well-being among specific populations in order to achieve health equity for all. Although the U.S. government-sponsored initiative focuses selectively on health disparities domestically, the concept of health disparities and their origins in social determinants has universal application. For example, PLWHA in China today are a population at risk for disparate health outcomes due to social determinants, including the stigma attached to their HIV illness and to any other marginalized socio-demographic statuses that apply to them. At risk for health disparities, Chinese PLWHA merit research attention and enhanced outreach and care.
Caregiving for PLWHA in a collectivistic setting such as China, where the family is the fundamental unit, involves family members providing a wide range of support, including medication assistance, financial help, assistance with daily activities, and psychological support (Li, Wu, Wu, Sun, Ciu, & Jia, 2006; Yoshioka & Schustack, 2001). Yet many PLWHA in China engage in self-isolating behaviors, including distancing from family and thereby losing a valuable source of social support (Zhou, 2007; Ogden & Nyblade, 2005; Salter, Go, Le Minh, Gregowski, Ha, Rudolph, et al. 2010). Self-isolating behaviors among PLWHA range from making fewer visits and phone calls, to more extreme measures of sending children away, divorcing spouses, moving far distances from home, living alone, isolating, and engaging in suicidal behaviors (Zhou, 2007; Ogden & Nyblade, 2005; Salter et al. 2010).
Many PLWHA engage in self-isolation because they are wary of being contagious and vigilant about keeping a “safe” distance between their “contagious bodies” and others’ “healthy bodies” during interpersonal interactions (Zhou, 2007). They develop strict self-discipline and continuously self-monitor when interacting with family members, withholding physical affection or thoroughly cleaning everything they touch. Feelings of inferiority are also common reasons for self-isolation. Zhou (2007) suggested that PLWHA often blame themselves for acquiring HIV and internalize societal stigma against HIV and those affected by it. As a result, they accept and even condone the discrimination and mistreatment they receive, and tend to avoid most social connections.
As a form of psychological isolation, many Chinese PLWHA withhold their HIV diagnosis from others due to fear that disclosure may cause distress in the family and add psychological burden, especially for children and the elderly (Salter, et al., 2010; Zhou, 2007). Concerns are heightened as well about potential secondary stigma that may be inflicted on family members, due to their association with someone who is HIV-positive (Salter et al. 2010). Wary of inciting secondary stigma that may affect their family’s social, economic, and psychological well-being, some PLWHA may withdraw from family and community in order to keep their HIV status a secret and protect members of their family (Ogden & Nyblade 2005).
The consequences of self-isolation can be devastating, depriving PLWHA of major sources of support and social connection, and potentially compromising their mental health. Indeed, acute loneliness, even among the general population, has been associated with a high risk for decreased mental health, including depression (Cacioppo & Hawkley, 2003). Moreover, among those with chronic illnesses in general (including HIV, diabetes, and chronic obstructive pulmonary disease), social isolation has been associated not only with increased stress levels, but also with physiological measures of poorer immune system functioning (Cacioppo & Hawkley, 2003; Cole et al., 2007). Social isolation among PLWHA specifically, was found to be associated with exacerbated HIV-related problems such as poorer medication adherence (Mosack, Stevens, Brouwer, & Wendorf, 2015).
In the present study, we sought to more fully examine the phenomenon of social isolation among Chinese PLWHA by considering systems of individual, familial, and societal influences. We aimed to describe, within a cultural context that values family above all else, how individual interpretations, family interactions, and external factors interact with each other and influence Chinese PLWHA’s self-isolating behaviors.
METHODS
Rationale for Qualitative Approach
We chose a qualitative approach for this study in order to examine the complexity and dynamic process of intrapersonal and intra-familial interactions contributing to self-isolating behaviors. We sought to investigate the range and variation of lived experience through our individual participants’ stories, and to obtain textual descriptions from and give voice to a marginalized population that is experiencing health disparities. These aims were best suited for qualitative methodology (Denzin & Lincoln, 1994), as it is particularly effective in eliciting culturally relevant information about motivations, values, behaviors, and the social context of a particular population.
Setting
Study sites were the HIV/AIDS outpatient clinic at the Shanghai Public Health Clinical Center (SPHCC) and the AIDS ward at Beijing Ditan Hospital, Capital Medical University in China. Both hospitals provide premier treatment for HIV for local residents as well as those traveling from far away to receive specialty care. From 2009–2011, we conducted 19 in-depth individual interviews at SPHCC, and another 15 individual interviews at Beijing Ditan Hospital.
Sample Selection and Characteristics
Participants (N=34) were HIV-positive outpatient adults from the two study sites, that were recruited by clinic staff. We employed purposive sampling with the aim of assembling a diverse group of participants who might be able to convey the full breadth of experiences relevant to the investigation. In terms of generalizability, qualitative research emphasizes gaining a rich and complex understanding of a specific social context or phenomenon rather than collecting data that can be generally informative of other populations or geographic areas (Denzin & Lincoln, 1994). Therefore, in qualitative inquiry, the selection of a sample from the sampling frame does not require a random process so as to ensure representative coverage as in quantitative research. Clinic staff assisted in the recruitment process by inviting individuals to participate who varied in demographic factors of age, gender, and parental status as well as illness-related indicators of time since diagnosis and disease progression.
This sampling method allowed recruitment of a diverse group of participants able to provide a broad spectrum of experiences related to the main themes of interest. Note that “saturation,” as applied in qualitative methodology, indicates the point at which new categories cease to appear in the interviews (Denzin & Lincoln, 1994). After completing in-depth interviews with 19 individuals in Shanghai and 15 in Beijing, the interviewers as a team concluded they had achieved general saturation, that is, a final set of categories sufficient to code the important elements of the central themes.
The final sample of 34 participants ranged in age from 23 to 66 years, with an average age of 41.6 (SD=10.37); 15 were male and 19 were female. Close to half (47%) of the male participants reported acquiring HIV through having sex with men, and over one third (37%) of the female participants reported the same. Other transmission routes reported were blood donating, medical procedures, and intravenous drug use. The majority of the non-local participants were migrants from small villages in the countryside who came to the major cities in search of employment.
Data Collection
We chose the standard qualitative method of in-depth interviews, which are optimal for collecting data on personal perspectives and experiences, especially those involving highly sensitive or stigmatized topics. In-depth interviews utilize an interview schedule comprising open-ended questions posed in a semi-structured approach in order to allow participants to respond in their own words rather than being forced to choose from among a pre-determined response set (Cicourel, 1982). Extensive probing after initial responses is used to elicit richer data that are personally meaningful and culturally salient. This approach allows for the possibility of obtaining information unanticipated by the researcher.
In our study, the 1–2 hour-long interviews were conducted in private offices in the clinics and consisted of a series of open-ended questions about participants’ personal experiences with HIV/AIDS, focusing on mental health, medication management, social support, stigma, and HIV-related coping that were based on the aims of a larger investigation. Table 1 presents the compete interview guide. Participants were asked to describe the experience of how they found out they were HIV-positive, how the diagnosis impacted them emotionally and psychologically, what they had done to respond to their diagnosis and manage their illness, and what resources were helpful in their process. Note that there was no a priori initial inclusion of questions specifically targeting self-isolation. However, with successive interviews, the interview schedule was progressively refined to further probe specific examples of strategies that participants employed to confront the acute HIV stigma they experienced.
Table 1.
Semi-Structured Qualitative Interview Guide
| 1. Experience of the diagnosis |
In this part, I will ask you about your experience when you first heard you were HIV+.
|
Additional prompts if necessary. Please make sure participant addresses the following:
|
| 2. Impact of the diagnosis |
In this part, I will ask you about the impact HIV has had on your life.
|
Additional prompts if necessary. Please make sure participant addresses the following:
|
| 3. Process of coping |
In this part, I will ask you about what you have done to cope with your diagnosis.
|
Additional prompts if necessary. Please make sure participant addresses the following:
|
| 4. Helpful resources |
In this part, I will ask you about what you might want to tell someone else in your situation in order for them to learn from your experience.
|
Additional prompts if necessary. Please make sure participant addresses the following:
|
The interviews were digitally audiotaped with permission, and conducted in Mandarin by Chinese-American bicultural research staff fluent in Mandarin and English, which included the second author. Participants received an incentive for their time (100 RMB, i.e., approximately 15 U.S. dollars), which is commensurate with standard rates for research participation in these settings.
Analytic Strategy
All interviews were transcribed verbatim in Chinese, with each transcript reviewed for accuracy and cross-checked by at least two research team members. One was an interviewer with extensive experience in HIV behavioral research, and the other was one of several research assistants fluent in English and Mandarin. Research assistants were doctoral and undergraduate level psychology students of excellent academic standing, who received qualitative research training and supervision from faculty members of the team, the third, fourth, and fifth authors of this article. Data were entered into and analyzed with Atlas.ti (Version 6), a software program designed specifically for the analysis of qualitative data.
The analysis employed an inductive content analytic approach, where themes are developed through analysis of text, to identify factors associated with reported self-isolation (Hsieh & Shannon, 2005). Research team members first conducted open coding to identify salient descriptive categories for the construction of a codebook or dictionary. Data were coded using a constant comparison analysis framework (Miles & Huberman, 1994), with disagreements resolved by discussion and mutual agreement between raters and research team members. All coding was conducted in Mandarin to retain fidelity of participants’ voices, and only translated for publication purposes. The collection of codes was modified in an iterative fashion after analysis of an initial subset of interviews. Codes relevant to this analysis described data on participants’ motivations, beliefs, and behaviors related to self-isolation. These were then applied to all interviews. Finally, broader themes were extracted by linking, comparing, and framing coded text.
RESULTS
Participants provided rich narratives of their struggles to accept their HIV diagnosis as well as extraordinary resilience in coping and living with HIV in a setting that highly stigmatizes the disease. The two major themes extracted were: 1) forms of self-isolation behaviors such as geographical or psychological separation, and 2) dialectical influences on self-isolation such as stigma, HIV-related factors, and familial influences,
Forms of Self-Isolation
In response to questions regarding experiences of HIV stigma and how participants coped, the theme of self-isolation was frequently observed. As described in previous literature (e.g., Zhou, 2007; Ogden & Nyblade, 2005), geographic separation was the most common form of self-isolation, involving participants physically removing themselves from contact with their families. This took the form of literally moving their place of residence away from their family’s community (e.g., “I made my children move back to the countryside to live with their grandparents”), decreasing time spent in the presence of the family (e.g., “I don’t go to their [brother with a nephew] house any more”); or, when complete self-isolation was not possible, avoiding any possibility of physical contact (e.g., “separating chopsticks and dishes”). Other self-isolation behaviors took the form of social or psychological separation, which has not been well documented in existing literature. For example, some participants in our study described withholding their diagnosis from others as a form of self-isolation (with one participant saying he would take the diagnosis “to [his] grave,” and another saying he would disclose his diagnosis only with his last breath “on [his] dying bed”). Other participants achieved psychological separation by disguising their distress from others (e.g., “being strong in front of parents,” or “hiding weakness”). Others separated themselves by adopting a passive stance toward being rejected by others (“It is his right to leave me”), or by anticipating and even instigating social separation (“I suggested that we divorce”). The ultimate self-isolation was sought in fantasies of escaping this life (“I think about dying often”), and in suicidal thoughts and behaviors (“I thought about driving off the highway so it would look like an accident”).
Influences on Self-Isolation
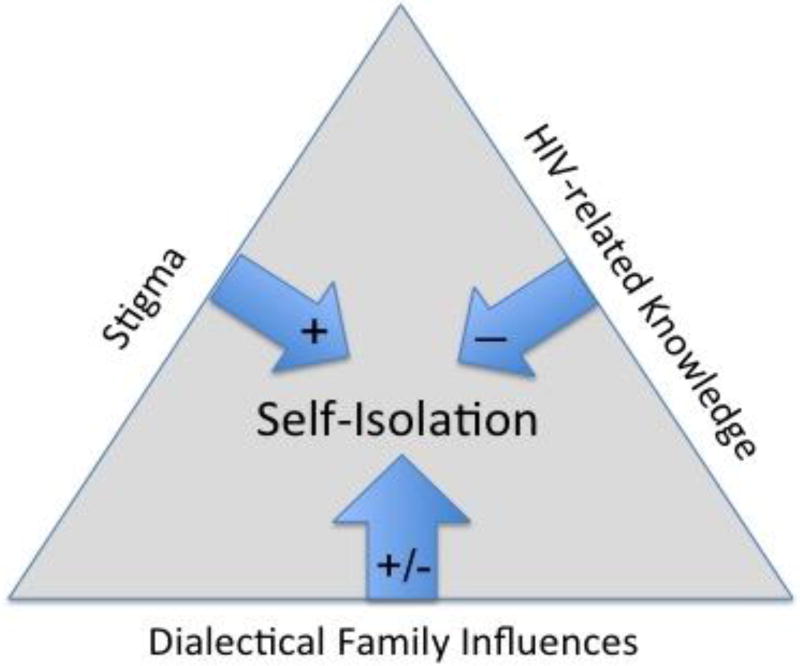
In describing their self-isolation strategies, participants touched upon a myriad of factors that affected their decision-making. As summarized in Figure 1, three major themes of influences emerged
Figure 1.
Influences on Self-Isolation
I. Stigma Motivating Self-Isolation: (“We are beneath other people”)
In China, HIV is acutely stigmatized (Hesketh, Duo, Li & Tomkins, 2005; Liu et al. 2006; Li et al., 2010), with the media replete with socially stigmatizing messages (Yu, 2012). Participants’ narratives revealed the impact of stigma in motivating self-isolation, especially when the stigma was internalized, leading to self-blame and negativity. Negative self-attribution was a commonly reported consequence of experiencing HIV-related stigma that led to participants’ desire to isolate themselves. As one participant remarked:
Like us who have this disease, [we] feel like we are beneath other people, feel like we are unable to be a human being in front of other people. (Female, 58, with siblings and grandchild)
These sentiments are consistent with the established linkage between low self-worth and a desire to isolate socially, a connection frequently noted among depressed individuals (Diaz, Ayala, Bein, Henne, & Marin, 2001; Leary, Schreindorfer, & Haupt, 1995; Colwell & Kato, 2003). Consistent with results in previous research (Salter et al., 2010; Ogden & Nyblade, 2005; Zhou, 2007), our participants reported feelings of shame and inferiority as a reason to self-isolate:
I feel like a murderer at large; I need to hide it from everyone. (Male, 32, with parents)
Many participants blamed themselves for acquiring HIV, thereby heightening their sense of shame:
When you make mistakes, you should be the one to take the responsibility, not others. It is your own fault that you end up on this road [having HIV]; you cannot blame it on anyone else. So, you should take the responsibility when you make mistakes, and you should not burden anyone else with it, that’s how I think about it. (Male, 39, with wife and children)
This was true even among participants who acquired HIV while engaging in behaviors not deemed to be risky, such as sex with only one long-term partner whose HIV-positive status was unknown, as was frequently seen among women who acquired HIV from their husbands.
Participants not only considered self-isolation as a way to cope with their existing internalized stigma; they also projected into the future and hoped to escape anticipated stigma and discrimination by isolating themselves. Many described avoiding interactions with family members due to concern about being rejected, or being feared by them.
I was afraid that they [family members] would be fearful of me; they would be fearful that I would infect them… When I was home, I did not dare to touch them physically. (Female, age unknown, with parents and siblings)
Self-isolation was seen as a way to allow participants to avoid shame and save face, which is a ubiquitous Chinese value of retaining respect and avoiding humiliation (Ho, 1976). The amount of anticipated stigma varied based on the mode of transmission, or presumed mode by which the participant had contracted HIV, particularly if the participant had not disclosed this information to family members. For example, fear was more strongly endorsed by men who acquired HIV from having sex with other men, rather than commercial sex with female sex workers.
II. HIV-related Factors Discouraging Self-Isolation: (“Though it cannot be cured, it can be managed”)
A second thematic category of influences on HIV-related self-isolation emerged, which generally worked against the tendency to self-isolate. The most commonly mentioned factor was accessibility to accurate HIV-related knowledge. Our participants received HIV-related information from a variety of external sources, including doctors, volunteers, other PLWHA, the media, and hearsay. Participants reported that positive and accurate HIV knowledge from authoritative sources not only decreased their negative self-attributions but also increased positive family responses toward them and their diagnosis. Both of these factors alleviated their motivation to self-isolate.
Reassuring HIV knowledge derived from authoritative sources eased concerns about the lethality of HIV, and so lessened stigma.
[The doctor said] don’t be too scared, it is a chronic disease. Now the medication that the government provides can manage the disease. Though it cannot be cured, it can be managed. (Male, 39, with wife and children)
Knowledge about the routes of HIV transmission eased fears of contagion and hence mitigated the need for self-isolation as a form of protection.
He [the doctor] told me that the common HIV transmission routes were blood transmission and needle sharing; eating with family members generally was not contagious, only blood was contagious. (Female, 32, with parents)
Other information made the prospect of remaining together as a family seem more feasible. This included sources of possible financial aid for HIV-related care.
It is him [the doctor] who introduced me to a volunteer from the fund. That fund helped my son and paid for our children’s tuition. (Female, 40, with siblings and children)
Psychological consultation and stress-reduction techniques were also welcome.
I received volunteer training from Red Ribbon [Society], where I had psychological counseling. There were doctors, nurses and psychologists giving lectures about how to decrease stress. (Male, 39, with wife and children)
Guidance for the newly diagnosed on sources of peer support also diminished the desire to self-impose separation from the family.
I found an HIV-positive QQ group [Internet chat group]. I joined the group and the people there told me to calm down, and told me that I could ask for someone at Beijing Ditan Hospital for help so here I am (Male, 48, partner, child, spouse).
Our participants stressed that information from authoritative sources was particularly reassuring. These reliable sources of HIV knowledge were doctors, volunteers from official AIDS-related organizations, and non-governmental organizations such as the Red Ribbon Society, and other more experienced PLWHA.
If you are a general patient or staff, I would think that you said what you said just to comfort me. Doctors are different; what they say is like gold (shengzhi), at least they have seen a lot, they have seen every kind of patient. They say some HIV patients were initially in the ICU, but now they are quite healthy and being discharged. (Male, 50, with parents, siblings, and children)
While positive and accurate information has become more accessible due to increasing Internet access, wrong, misleading, or conflicting information about the routes of HIV transmission continue to proliferate, which threatens familial support. One participant distanced herself from her daughter because she was confused by the conflicting information.
I’m scared, really scared. I asked a lot of people, some of them told me that saliva is not contagious; some of them told me that saliva is contagious. I’m confused. I don’t know if it is really contagious or not. (Female, 33, with siblings, spouse, and child)
Many participants reported that the knowledge of life experiences of other PLWHA was very encouraging, and this tended to alleviate their need to plan for isolation. Participants realized that, instead of completely cutting off social connections, they still had the option to participate in family life. Some participants considered other people who had been living with HIV for decades as role models.
One thing is that you may find that you are luckier than others, and you will feel grateful. Another thing is that having seen their health conditions, their attitudes for life… You will feel that there is hope. It’s an encouragement. (Male, 48, with wife, child, and same-sex partner)
However, learning about others’ negative experiences could also be very frustrating. Some participants reported internalizing the negative stereotypes depicted by HIV-related media and other PLWHA. One participant recalled watching a video clip about HIV:
A person, African, recorded her change in bed every day for ninety days; it was horrifying, and at last she died. This [video] makes me really conflicted. (Male, age unknown, with parents).
Another participant had witnessed the deaths of four fellow HIV-positive patients and became pessimistic about her future.
Our condition is not like what others say, that we could still live for twenty years. Even for ten years, I feel that is not true. I feel that I could not live that long. (Female, 53, siblings)
Finally, HIV-related disease progression also affected self-isolation tendencies. Improvements in health (e.g., decreased viral load or increased CD4 count) was associated with reduced self-isolation.
Just this year, they [the doctors] did not find any virus in my blood. So I let him [my grandson] kiss me. In the summer, we slept together and I sweated, if he touched me, I would clean (him). Now there is no detectable virus, I let him hug me, kiss me. (Female, 58, with siblings and grandchild)
Conversely, several PLWHA planned to cut all ties with family and or even commit suicide if their condition deteriorated, such as if and when they developed AIDS.
When I develop AIDS. … I will drive off a cliff, making it look like an accident. (Male, 48, with wife, child, and same-sex partner)
III. Dialectical Familial Influences on Self-Isolation: (“I must. For my family”)
In Chinese culture, an individual’s value is embedded within the family (Triandis, Bontempo, & Villareal, 1988). Unsurprisingly, participants’ stories resonated with the strong cultural emphasis placed on the importance of family relationships and family welfare. Interestingly, family appeared to have dialectical influences on self-isolation. As seen in the data presented below, strict adherence to cultural values emphasizing the importance of family could have opposing influences, either pulling the participant back into the family fold or pushing him or her away.
A common theme in references to family was the participants’ concerns for their family’s physical health and psychological well-being, which were consistently linked to increases in self-isolating behaviors. The majority of the participants expressed their intentions to protect family members’ physical health by implementing strict hygiene rituals if they could not completely isolate their physical selves. These hygiene behaviors included: “using different wash basins,” “separating soaps,” “separating laundry,” and “sterilizing dishes” (Female, 59, with parents, siblings, husband, and child). Many female participants in particular were terrified by the idea of infecting family and had more extreme behaviors such as: “after using the washing machine, I use a sterilizing agent on my clothes” (Female, 58, with siblings and grandchild); “always wearing gloves while in my daughter’s house,” “sterilizing my daughter’s toilet seat after sitting on it,” and “using paper towels to hold the door handle to prevent leaving sweat on it” (Female, 46, with siblings, children, and grandchild).
Importantly, our participants demonstrated that such concerns were not always caused by misleading information about transmission routes and contagiousness of HIV; instead, they did not want to take any chances, even though they knew the possibility of infection was very slim. One participant explained:
Every parent worries. If you can separate [dishes], you should separate instead of mixing them together, right? Though it is not [contagious], and I know it is not, I have to separate them. (Female, 52, with children)
Other than family’s physical health, participants also mentioned that they wanted to protect their family’s psychological well-being. Our participants tried to protect their family from experiencing distress by keeping their health condition a secret and consequently distancing themselves from their family in the process:
If I told them [my parents], there is nothing they can do, they cannot help me. I would only be making them worry. (Male, 40, with parents)
Similarly, if participants saw themselves as a burden to the family, they would attempt to remove the burden by cutting off connections and family ties. One participant stated:
When [my husband’s] diagnosis came out negative, I said to him that we should file for divorce. He asked me why. I asked him, “Aren’t I a burden to you?” (Female, 33, with siblings, spouse, child)
Concern for the family’s well-being also manifested in consideration for the potential secondary stigma and discrimination family members might experience. One participant tried to divorce her husband because she feared the potential discrimination her husband would face in the workplace.
He is a businessman. If people in his business circles or his friends learn about that [my positive HIV status], they will not only push me out, they will push him out as well. And it will destroy his career and everything. (Female, 33, with siblings, husband, and child)
In addition, participants mentioned their worries about family members’ possible negative self-attribution due to association with an HIV-positive individual:
Now I have the disease, I’m causing my wife and child shame, you know… they will think that they are less than other people, less than an average person. (Male, 48, with partner, child, and wife)
Concerns for their family’s physical health and psychological well-being often pushed participants away from their families and towards increased self-isolation, but a strong sense of filial piety (respect for one’s family, elders, and ancestors) and family responsibility had an opposing effect. As Chinese cultural values dictate that adults (especially married ones) carry important duties and are primarily responsible for contributing to the family for both older and younger generations (Ho, 1976), participants commonly reported that an unfulfilled family responsibility was a major reason for continuing to engage in family life. Indeed, middle-aged participants often described their responsibilities to financially provide for their children, be available to assist their children, let their parents have peaceful twilight years, and take care of the burial procedures when their parents die:
I have to live; I still have a couple of things that are unfinished… My parents are old, I have to take care of their funerals (houshi), I have to let them live happily until the end. My child is studying abroad. I have to take care of his education, and try to be there for him as long as possible when he grows up. (Male, 48, with wife, child, and same-sex partner)
Evident from these descriptions of their family relationships, was the participants’ positioning of themselves as self-directed actors with agency in their familial affairs; they could protect their family by self-isolating or assume responsibility for their family’s welfare by eschewing self-isolation behaviors. However, the family also had the potential of having agency with respect to the PLWHA. Indeed, the family’s immediate responses to a participant’s HIV-positive diagnosis could either alleviate or aggravate feelings of shame and inferiority, fear of rejection, and self-blame. Positive family responses were seen as welcoming and were generally associated with less intense self-isolation; however, negative family responses tended to precede increased self-isolating behaviors.
Many participants reported that their family members were helpful in many ways after learning about the participant having HIV, such as providing more emotional support as well as tangible and financial assistance. For example: “[My parents] care about me more now” (Female, 32, with parents); “My mother told me to treat myself; if I [want] special foods, to just buy and eat them” (Female, age unknown, with parents and siblings); and “[My sister] said if you need money, I’ll lend you money” (Female, age unknown, with parents, and siblings).
The family’s demonstration of acceptance of the diagnosis and absence of stigmatization had particularly positive influences on participants.
[My sister] said, “It [HIV] is nothing; I have a neighbor who is living with HIV, it has been seven years, he is exactly the same as normal people, just a bit skinny”. (Female, 33, with siblings, husband, and child).
Unfortunately, negative family responses that communicated a message of fear of contracting HIV from the participants were very common and tended to encourage participants’ self-isolation. Many family members were fearful of HIV contagion and tried to reduce their direct or indirect physical contact with the participants: by separating the dishes, “When we eat together, they [my siblings] put food in a separate bowl for me” (Female, 53, with siblings); by separating laundry, “My sister-in-law never washes my clothes with theirs” (Female, 40, with siblings and children); and by rarely visiting, “My sister did not dare to come to my place; she said my place was full of germs” (Female, 50, with siblings and grandchildren).
Family members sometimes did not intend to reject or hurt the participants, but the participants interpreted some of their family’s behaviors as rejections or signs of resentment. Often, even family members who were attempting to be supportive could result in participants increasing self-isolation. One participant reported that her siblings regularly invited her to dinner, but she continuously refused their invitations. She explained: “My sisters said it was nothing, as if they did not mind me coming to eat with them. But I could tell that they were still scared.” (Female, 58, with siblings and grandchild)
As with reactions to the diagnosis, family responses to initial self-isolating behaviors could determine the course of future events – either pushing away the participant or pulling him or her back into the family. Most family responses to the participants’ attempts at self-isolation were helpful in decreasing the isolation.
Initially, I proposed to my mother that if you think it’s not [okay] to eat together or something, we can separate the dishes, but they refused to let me. (Female, 32, with parents)
Some PLWHA expressed feelings of ambivalence, acknowledging that pushing away loved ones would cause them great pain but still feeling that it was the right thing to do. Participants described that their family’s positive responses relieved them of this emotional turmoil. One participant described the ambivalence he experienced when his boyfriend refused to break up with him:
If my boyfriend left me, I would in fact be miserable. In some sense, his being with me is my mental support. If he were not with me anymore, I would be lonely. I told my boyfriend I really wanted him to breakup with me, not living under this dark shadow [of being HIV positive]. But if he actually left me, I would be very upset. Maybe this is a Chinese thinking pattern, you don’t want something to happen, but it should happen. (Male, 48, with wife, child, and same-sex partner)
Similarly, a female participant tried to divorce her husband but he refused. Her husband’s responses made her feel loved and accepted; as a result, they grew closer than ever.
He said, “You just have a disease. Everyone gets sick once a while. It’s not like you made an unforgivable mistake; it’s not your fault you got this disease.” [Now] my family is my biggest support. Without them, I could not live to this day. (Female, 33, with husband, siblings, child)
DISCUSSION
This qualitative investigation examined self-isolating motivations, beliefs, and behaviors among Chinese PLWHA. The prevailing acute HIV stigma in China was internalized by participants in the form of negative self-attribution and the desire to avoid discrimination, which generally led to increased self-isolating behaviors. However, some HIV-related factors appeared to diminish the tendency toward self-isolation; these included knowledge of HIV and how it is transmitted, familiarity with the positive experiences of other PLWHA, and good management of their HIV. Familial factors had dialectical influences on self-isolation, either pushing PLWHA away from their families out of a desire to protect their family, or pulling them back into the family fold out of a sense of responsibility. Family responses to the HIV diagnosis and to PLWHA’ initial attempts to self-isolate could determine the course of future events, either welcoming back PLWHA, or pushing them away.
Several researchers have emphasized the importance of viewing the behaviors of Chinese PLWHA in the context of family relationships and the broader social and cultural environment (Li et al., 2006; Li, Sun, Wu, Wu, Lin, & Yan, 2007a; Lee, Kochman, & Sikkema, 2002; Ogden and Nyblade, 2005; Yang et al., 2016; Simoni, Yang, Shiu, Chen, Udell, Bao, et al., 2015). For example, significant differences have been reported between the support systems of HIV-positive individuals in the United States as compared to China (Yu, Yang, Shiu, Simoni, Xiao, Chen, et al., 2015; Li et al., 2006; Li, Liang, Ding, & Ji, 2011). Broadly speaking, Chinese PLWHA rely more heavily on family to cope with emotional stress. This context helps elucidate how, in our study, the family’s response to HIV was critical in determining how participants came to accept their diagnosis and whether they would respond by self-isolating. Societal influences, including public education campaigns and media depicting HIV/AIDS as a shameful disease, propagate fear-based messages that reinforced the public’s fear about HIV/AIDS and contribute to PLWHA’ self-stigmatization.
Implications for Health Equity
In the U.S., Healthy People 2020 defines health equity as the “attainment of the highest level of health for all people” and emphasizes that achieving health equity requires “valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and the elimination of health and health care disparities” (US Department of Health and Human Services, 2010). In China, for PLWHA, health equity clearly will require broader societal acceptance of the disease, and support for those living with HIV. Chinese government support has been forthcoming, including with the Four Frees and One Care policy, which mandates provisions that increase access to HIV testing and treatment such as free antiretroviral therapy (Sun, Lu, Wu, Poundstone, Zeng, Xu et al., 2010). These forces can be buttressed at the individual provider level, with the provision of respectful care that does not stigmatize those seeking treatment. Medical care should be provided in the context of social and psychological support, though China lacks a cadre of trained mental health professionals. Indeed, similar emphasis for mental health equity has yet to occur (Yang, Simoni, Cheryan, Shiu, Chen, et al., 2017).
In our own efforts to address mental health equity issues for Chinese PLWHA, we have worked to expand the role of nurses as mental health care providers who deliver brief interventions in primary care settings as opportunity arises. To date, however, there has not been backing for a broader systemic plan to provide mental health services on a regular basis (e.g., Simoni et al., 2015).
Within the cultural context of China, it is important to consider family-based interventions for mental health that can reduce self-isolation by PLWHA. A good example from the literature is Li et al.’s (2011) intervention called Together for Empowerment Activities (TEA), which is delivered in three ways: small groups of PLWHA and their families, home-based family activity with children, and community events that promote social integration. TEA is designed to increase PLWHA’s social support network and decrease symptoms of depression. By helping PLWHA maintain a positive relationship with family members, interventions can increase PLWHA’ experience of positive social interactions and social support, which is particularly helpful for this population (Yang et al., 2015).
Finally, accessibility to HIV information, knowledge of experiences of other HIV-positive individuals, and progress in disease treatment set the stage for participants’ appraisal of their HIV positive status as well as interactions with family. Having accurate information, positive role models, and improved disease status tended to lessen negative self-attribution and decrease the motivation to protect their family through self-isolation. Such factors also encourage family members to respond to the diagnosis and to PLWHA’ isolation behaviors with more acceptance and positivity. Promoting HIV education and establishing positive role models during the diagnostic and treatment process may be helpful in improving PLWHA’ self-perceptions and increase their likelihood of maintaining connections with family.
Limitations
There are several limitations to this study. First, the data were collected at premier HIV treatment centers in the most developed cities in China, and this type of setting may have affected the types of concerns raised by our participants and the range of their experiences. Secondly, although consultation was routinely obtained with two different research groups, coding was primarily conducted by two members of the research team who led this current study. Therefore, the development of our semi-structured interview guide, conducting of the interviews, and coding and analysis of the data may be subject to researcher bias, which is important to acknowledge in qualitative research (Morrow, 2005).
Conclusions
Despite these limitations, this study provides insight into how Chinese people living with HIV/AIDS manage stigma, learn about HIV, and cope with HIV in their family contexts – and how these factors interact to influence self-isolation motivations, beliefs, and behaviors. Thorough understanding of this process allows for increased ability to support Chinese PLWHA in their HIV-related distress and provides an important framework for research on distress reduction interventions to reduce health disparities in similarly marginalized populations.
Future research is needed to assess the impact of isolation behaviors of PLWHA on their psychological and physical health, and use quantitative methodology to predict mental health outcomes. Furthermore, while previous research has documented the negative impact of social isolation among multiple populations (Cacioppo & Hawkley, 2003; Cole, Hawkley, Arevalo, Sun, Rose, & Cacioppo, 2007), no research we could locate examines differences between consequences caused by isolation initiated by other people versus isolation initiated by PLWHA, themselves. Future research may determine whether self-initiated isolation is associated with fewer negative consequences (as a protective factor), or with more negative consequences associated with stronger internalized stigma. Intervention research is needed on the development and evaluation of culturally appropriate interventions to assist PLWHA and their families cope more effectively with HIV/AIDS and minimize health inequities for this population.
Acknowledgments
This study was funded by National Institute of Mental Health under award number F31MH099925. Additional support was provided by the University of Washington Center for AIDS Research (CFAR) under award number AI027757 and the University of Washington Department of Psychology. We gratefully acknowledge the participants and providers at Beijing Ditan Hospital and Shanghai Public Health Clinical Center for their assistance with the project.
Footnotes
Conflict of Interest: Tianyi Xie, Joyce P. Yang, Jane M. Simoni, Cheng-Shi Shiu, Wei-ti Chen, Hongxin Zhao, and Hongzhou Lu declare that they have no conflict of interest.
Compliance with Ethical Standards
Human Rights and Informed Consent. All procedures followed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Research protocol and study materials were approved by the Institutional Review Boards at the University of Washington, Shanghai Public Health Clinical Center, and Beijing Ditan Hospital. Written informed consent was obtained from all individual participants included in the study.
References
- Achat H, Kawachi I, Spiro A, III, DeMolles DA, Sparrow D. Optimism and depression as predictors of physical and mental health functioning: The Normative Aging Study. Annals of Behavioral Medicine. 2000;22:127–130. doi: 10.1007/BF02895776. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Berntson GG. The anatomy of loneliness. Current directions in psychological science. 2003;12(3):71–74. [Google Scholar]
- Cicourel A. Interviews, surveys, and the problem of ecological validity. The American Sociologist. 1982;17(1):11–20. [Google Scholar]
- Cole SW, Hawkley LC, Arevalo JM, Sun CY, Rose RM, Cacioppo JT. Social regulation of gene expression in human leukocytes. Genome Biology. 2007;8:R189. doi: 10.1186/gb-2007-8-9-r189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colwell J, Kato M. Investigation of the relationship between social isolation, self-esteem, aggression and computer game play in Japanese adolescents. Asian Journal of Social Psychology. 2003;6(2):149–158. [Google Scholar]
- Denzin N, Lincoln Y, editors. Handbook of Qualitative Research. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- Díaz RM, Ayala G, Bein E, Henne J, Marin BV. The impact of homophobia, poverty, and racism on the mental health of gay and bisexual Latino men: findings from 3 US cities. American Journal of Public Health. 2001;91(6):927–932. doi: 10.2105/ajph.91.6.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho D. On the concept of face. American Journal of Sociology. 1976;81(4):867–884. [Google Scholar]
- Hsieh H, Shannon S. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15:1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Leary MR, Schreindorfer LS, Haupt AL. The role of low self-esteem in emotional and behavioral problems: Why is low self-esteem dysfunctional? Journal of Social and Clinical Psychology. 1995;14(3):297–314. [Google Scholar]
- Lee RS, Kochman A, Sikkema KJ. Internalized stigma among people living with HIV-AIDS. AIDS and Behavior. 2002;6(4):309–319. [Google Scholar]
- Li L, Wu S, Wu Z, Sun S, Cui H, Jia M. Understanding family support for people living with HIV/AIDS in Yunnan, China. AIDS and Behavior. 2006;10(5):509–517. doi: 10.1007/s10461-006-9071-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Sun S, Wu Z, Wu S, Lin C, Yan Z. Disclosure of HIV status is a family matter: Field notes from China. Journal of Family Psychology. 2007a;21(2):307–314. doi: 10.1037/0893-3200.21.2.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Lin C, Wu Z, Wu S, Rotheram-Borus MJ, Detels R, et al. Stigmatization and shame: consequences of caring for HIV/AIDS patients in China. AIDS care. 2007b;19(2):258–263. doi: 10.1080/09540120600828473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Liang LJ, Ding YY, Ji G. Facing HIV as a family: predicting depressive symptoms with correlated responses. Journal of Family Psychology. 2011;25(2):202–209. doi: 10.1037/a0022755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. Thousand Oaks: SAGE; 1994. [Google Scholar]
- Morrow SL. Quality and trustworthiness in qualitative research in counseling psychology. Journal of Counseling Psychology. 2005;52(2):250–260. [Google Scholar]
- Mosack KE, Stevens PE, Brouwer AM, Wendorf AR. Shared Illness and Social Support Within Two HIV-Affected African American Communities. Qualitative Health Research. 2015 doi: 10.1177/1049732315612044. 1049732315612044. [DOI] [PubMed] [Google Scholar]
- Niu L, Luo D, Liu Y, Silenzio VMB, Xiao S. The Mental Health of People Living with HIV in China, 1998–2014: A Systematic Review. PLOS ONE. 2016;11(4):e0153489. doi: 10.1371/journal.pone.0153489. http://doi.org/10.1371/journal.pone.0153489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden J, Nyblade L. Common at its core: HIV-related stigma across contexts. Washington, DC: International Centre for Research on Women; 2005. [Google Scholar]
- Qiao S, Li X, Stanton B. Practice and perception of parental HIV disclosure to children in Beijing, China. Qualitative health research. 2014;24(9):1276–1286. doi: 10.1177/1049732314544967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salter ML, Go VF, Le Minh N, Gregowski A, Ha TV, Rudolph A, et al. Influence of perceived secondary stigma and family on the response to HIV infection among injection drug users in Vietnam. AIDS education and prevention: official publication of the International Society for AIDS Education. 2010;22(6):558. doi: 10.1521/aeap.2010.22.6.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Yang JP, Shiu CS, Chen WT, Udell W, Bao MJ, Lu HZ. Nurse-delivered counseling intervention for parental HIV disclosure: Results from a pilot randomized controlled trial in China. AIDS. 2015;29:S99–107. doi: 10.1097/QAD.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun X, Lu F, Wu Z, Poundstone K, Zeng G, Xu P, et al. Evolution of information-driven HIV/AIDS policies in China. International Journal of Epidemiology. 2010;39(suppl_2):ii4–ii13. doi: 10.1093/ije/dyq217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao J, Kipp AM, Liu Y, Zhang C, Ruan Y, Yin L, Vermund SH. HIV-related stigma and depression among recently diagnosed HIV-infected men who have sex with men in China; Presented at the International Aids Society.2015. [Google Scholar]
- Triandis HC, Bontempo R, Villareal MJ, Asai M, Lucca N. Individualism and collectivism: Cross-cultural perspectives on self-ingroup relationships. Journal of personality and Social Psychology. 1988;54(2):323. [Google Scholar]
- UNAIDS. 2015 China AIDS Response Progress Report. 2015 Accessed from http://www.unaids.org/sites/default/files/country/documents/CHN_narrative_report_2015.pdf.
- U.S. Department of Health and Human Services. The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. Phase I report: Recommendations for the framework and format of Healthy People 2020. Section IV: Advisory Committee findings and recommendations. 2010 Available from: http://www.healthypeople.gov/sites/default/files/PhaseI_0.pdf.
- Yang JP, Leu JX, Simoni JM, Chen WT, Shiu CS, Zhao HX. ‘Please don’t make me ask for help’: Implicit social support and mental health in Chinese individuals living with HIV/AIDS. AIDS & Behavior. 2015;19(8):1501–9. doi: 10.1007/s10461-015-1041-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang JP, Simoni JM, Cheryan S, Shiu CS, Chen WT, Zhao HX, Lu HZ. The development of a brief HIV-related distress reduction intervention for newly diagnosed individuals in China. Cognitive & Behavioral Practice, epub ahead of print. 2017 doi: 10.1016/j.cbpra.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang JP, Xie TY, Simoni JM, Shiu CS, Chen WT, Zhao HX, Lu HZ. A mixed-methods study supporting a model of Chinese parental HIV disclosure. AIDS & Behavior. 2016;20(1):165–73. doi: 10.1007/s10461-015-1070-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshioka MR, Schustack A. Disclosure of HIV status: Cultural Issues of Asian patients. AIDS Patient Care and STDs. 2001;15(2):77–82. doi: 10.1089/108729101300003672. [DOI] [PubMed] [Google Scholar]
- Yu Y, Yang JP, Shiu CS, Simoni JM, Xiao SY, Chen WT, Rao D. Psychometric testing of the Chinese version of the Medical Outcomes Study Social Support Survey (MOS-SSS-CM) among people living with HIV/AIDS in Mainland China. Applied Nursing Research. 2015;28(4):328–33. doi: 10.1016/j.apnr.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou YR. “If you get AIDS… You have to endure it alone”: Understanding the social constructions of HIV/AIDS in China. Social Science & Medicine. 2007;65(2):284–295. doi: 10.1016/j.socscimed.2007.03.031. [DOI] [PubMed] [Google Scholar]