Abstract
Delirium, a prevalent organ dysfunctions in critically ill patients, is independently associated with increased morbidity. This last decade has witnessed an exponential growth in delirium research in hospitalized patients, including those critically ill, and this research has highlighted that delirium needs to be better understood mechanistically, to help foster research that will ultimately lead to its prevention and treatment.
In this invited, evidence-based paper, a multinational and interprofessional group of clinicians and researchers from within the fields of critical care medicine, psychiatry, pediatrics, anesthesiology, geriatrics, surgery, neurology, nursing, pharmacy and the neurosciences, sought to address five questions:
What is the current standard of care in managing ICU delirium?
What have been the major recent advances in delirium research and care?
What are the common delirium beliefs that have been challenged by recent trials?
What are the remaining areas of uncertainty in delirium research?
What are some of the top study areas/trials to be done in the next 10 years?
Herein, we briefly review the epidemiology of delirium, the current best practices for management of critically ill patients at risk for delirium or experiencing delirium; identify recent advances in our understanding of delirium as well as gaps in knowledge, and discuss research opportunities and barriers to implementation, with the goal of promoting an integrated research agenda.
Brief Introduction: Epidemiology of Delirium
Definition
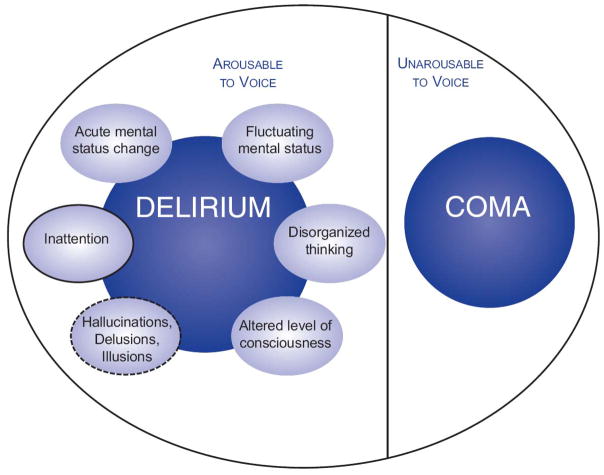
Delirium is a manifestation of acute brain dysfunction defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)[1] as a disturbance in attention and awareness that develops over a short period of time, fluctuates, and is accompanied by a change in cognition. These disturbances are not explained completely by an established or evolving neurocognitive disorder/injury (though it can exist superimposed on a primary cognitive disorder/brain injury), and there is evidence that the disturbance is caused by a direct physiologic consequence of a medical condition, an intoxicating substance, medication use, or from multiple etiologies (Figure 1).
Figure 1.
Acute Brain Dysfunction (Delirium and Coma)
Prevalence
Rates of delirium range from 20–40% among critically ill patients, with the higher rates of 60–80% observed in mechanically ventilated (MV) medical or surgical patients.[2–4] A substantial proportion of ICU patients have hypoactive delirium, [5] and hypoactive delirium may portend worse outcomes than hyperactive delirium.[6]
Delirium and Outcomes
Delirium is a strong independent predictor of longer time on MV and in ICU, cost, and mortality, with every day with delirium being independently associated with an increased hazard of death of 10%.[2] The attributable mortality to delirium (whether delirium causes higher mortality) is difficult to ascertain and still under investigation. Moreover, delirium is a strong predictor of cognitive decline that persists for months to years after ICU, and is associated with patients not returning to their prior quality of life or employment.[7–9]
There is much heterogeneity in delirium etiologies and thus different possible phenotypes (sepsis associated delirium, sedation associated delirium etc.), yet very little evidence exists to support differences in outcomes based on etiological phenotypes. Lumping all delirium together, irrespective of etiology, has helped understand the prevalence, risk factors and outcomes associated with delirium, and to raise awareness of delirium and simplify implementation of monitoring and management programs. The field will advance further when data allow us to characterize delirium etiology, based on pathophysiology and prognosis, to better tailor therapeutic options.
Delirium risk factors
Delirium risk factors can be divided into vulnerability factors (e.g., age, comorbidities) and hospital-related precipitating factors (e.g., acute illness and management related).[10] Patients with increased vulnerability may be predisposed to delirium with the smallest of precipitating factors, and vice-versa. Of many known delirium risk factors, psychoactive medication (particularly benzodiazepines) use, [11] drug-induced coma, sleep alterations, [12] metabolic disturbances and sepsis are common, potentially modifiable factors that clinicians should address when formulating delirium prevention and treatment strategies.
What is the current standard of care for managing delirium?
The lack of feasible biomarkers or radiological findings hampers the promulgation of delirium as a major organ dysfunction when such markers exist for cardiac, renal, and respiratory dysfunction, yet delirium cannot be ignored given its associated outcomes.
Assessment tools
Delirium will frequently go unrecognized if clinicians do not screen patients with validated delirium monitoring instruments. Based on their psychometric properties, the Society of Critical Care Medicine (SCCM) Pain Agitation and Delirium (PAD)[13] guideline recommends the use of sedation scales to assess arousal level followed by the validated Confusion Assessment Method-ICU (CAM-ICU)[14] or the Intensive Care Delirium Screening Checklist (ICDSC)[15] to assess for delirium. All four domains of the CAM-ICU, anchored on the presence of inattention, are evaluated in a focused patient assessment usually taking less than 2 minutes to complete. The 8-domain ICDSC, in contrast, assesses 4 symptoms of delirium in a focused patient assessment (including inattention) and 4 domains over the current and prior nursing shift, with 4 or more positive symptoms consistent with delirium. The importance of monitoring for delirium using one of these validated tools far outweighs their nuanced differences; choice of instrument should be based on clinician preference.
Prevention and management of delirium
Multicomponent, evidence-based bundles aimed at reducing ICU-acquired delirium have been proposed in the literature. For example, use of the ABCDEF Bundle (Table 1) has been associated with a reduction in delirium and ventilation time, with a recent large implementation study showing additional survival benefits.[16, 17] These are before/after and observational studies and thus their benefits need to be interpreted with caution. The Early implementation of Comfort and Analgesia using minimal Sedation and Humane care (eCASH)[18] bundle is a relatively new concept that is yet to be evaluated in clinical practice (Figure 2).
Table 1.
The ABCDEF Bundle Targeting Patient Symptoms
| ABCDEF Bundle Elements | Symptoms Being Addressed | Examples Of Monitoring Tools To Use |
|---|---|---|
| Assessment, prevention, and management of pain | Pain | Numeric Pain Rating Scale (NRS) Behavioral Pain Scale (BPS) Critical Care Pain Observation Tool (CPOT) |
|
Both spontaneous awakening and breathing trials Choice of sedatives and analgesia, |
Agitation or Sedation | Richmond Agitation-Sedation Scale (RASS) Sedation-Agitation Scale (SAS) |
| Delirium assessment, prevention and management | Delirium | Confusion Assessment Method for the ICU (CAM-ICU) Intensive Care Delirium Screening Checklist (ICDSC) Pediatric or Preschool Confusion Assessment Method for the ICU (pCAM-ICU; psCAM-ICU) Cornell Assessment for Pediatric Delirium (CAPD) |
| Early mobility/exercise | ||
| Family engagement and empowerment |
Figure 2.
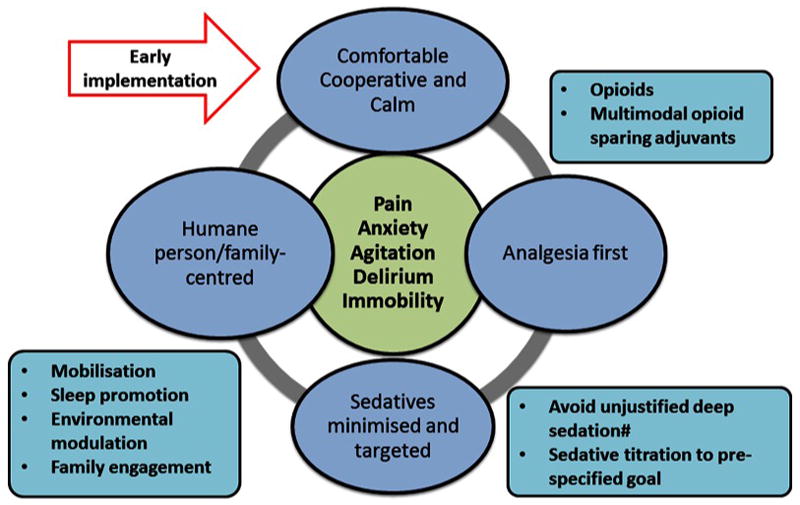
The Early implementation of Comfort and Analgesia using minimal Sedation and Humane care (eCASH) approach
With regards to pharmacological approaches, the SCCM guidelines[13] suggest the use of short-acting agents (e.g., propofol and dexmedetomidine) over benzodiazepines in MV patients, and that dexmedetomidine may be associated with improved delirium outcomes.[19–23] Access to early mobility and physical rehabilitation may shorten the duration of mechanical ventilation and reduce the risk and/or accelerate the resolution of delirium.[24, 25]
While prevention remains the best strategy to combat delirium, effective treatment of delirium is critical to accelerate its resolution. The search for, and management of, delirium risk factors, such as sepsis, pain, hypoperfusion, high fever, deliriogenic medications, and electrolyte imbalance is imperative and is the cornerstone for management in patients with hypoactive delirium. Furthermore, it is important to rule out fearful hallucinations/delusions in any patient with hypoactive delirium. Very limited data support any role for conventional antipsychotic therapy such as haloperidol, or atypical antipsychotics such as olanzapine, quetiapine and ziprasidone, for either delirium prevention or treatment in critically ill adults.[26–28] In MV and non-intubated patients, dexmedetomidine improved hyperactive delirium resolution.[20, 29]
What are the major recent advances in delirium research and care?
The development of animal models to study acute brain dysfunction, the increasing ability to screen for delirium, and the creation of delirium networks have played an important role in advancing delirium research and advocacy.
Experimental models in acute brain dysfunction
The induction of peritonitis by caecal ligation and puncture in rodents is the most used animal model to study acute and long-term brain dysfunctions that are close to those observed in septic patients. This induced brain dysfunction includes behavioral changes such as suppressed spontaneous activity and altered escape reflex that can be scored.[30] However any true cognitive dysfunction, is embedded within, and perhaps masked by, severe sickness behavior (an adapted physiological response elicited by the limbic, neuroendocrine and autonomic systems); most cognitive studies in sepsis therefore refer to dysfunction after peak illness has passed. There are now several validated tests for assessing psychological and cognitive functions that may remain impaired after sepsis in animal models, enabling objective assessment of functioning of particular brain structures or networks. There is also evidence of long-term affective and cognitive changes in studied animal models.[31, 32]
Measures such as glucose metabolism (fluorodeoxyglucose by positron emission tomography), electroencephalography and brain magnetic resonance imaging or spectroscopy are perhaps more informative during peak illness and it is necessary to establish criteria for these in animal models of acute brain dysfunction.[33, 34] An alternative approach has been to examine milder inflammation, induced by lipopolysaccharide, on a background of existing brain vulnerability in models of neurodegeneration and aging. These studies have produced acute onset, fluctuating and transient cognitive dysfunction in domains relevant to delirium.[35]
Monitoring delirium in vulnerable populations
Delirium is grossly underdiagnosed and is surrounded by myths, such as: delirium cannot be assessed in children or in the very old with concomitant cognitive impairment/dementia, or in patients with neurological injury. These myths have recently been challenged.
Children
Approximately 40% of children and 50% of infants and toddlers experience delirium in the ICU.[36, 37] The Pediatric CAM-ICU (pCAM-ICU) with 99% specificity and 83% sensitivity,[36] and the preschool CAM-ICU (psCAM-ICU) with 91% specificity and 75% sensitivity,[37] are validated for use in children from 18 years down to 6 months, accounting for developmental milestones. Similarly, the Cornell Assessment for Pediatric Delirium (CAPD),[38] with specificity of 79% and sensitivity of 94%, is a validated tool for delirium utilizing observed behaviors in infants and children.
Neurologically injured patients
There are emerging data surrounding delirium monitoring and its prognostic value in critically ill patients with primary neurological injury, with both the CAM-ICU and ICDSC utilized.[39–41] The general construct one needs to consider is that delirium— a “micro-diffuse” injury occurring due to cellular and neurotransmitter abnormalities—can occur on top of the a “macro-focal” primary neurological injury, such as stroke or a traumatic brain injury. New baseline neurological function needs to be assessed and documented and any change or fluctuation of neurological function needs to be considered in the context of the primary brain injury or evolvement of the same. Delirium should be considered in the differential diagnosis, given data that delirium superimposed on a primary neurological injury may portend worse outcomes.[39–41]
Cognitively impaired patients
Critically ill patients with mild cognitive impairment are at risk for delirium and similarly delirium can occur in patients with dementia—delirium superimposed on dementia (DSD).[42, 43] In the ICU, delirium evaluation in the context of dementia requires an accurate evaluation of the level of arousal. Acknowledging the current limitations of tools to assess DSD, it is still imperative to screen for DSD, using standard tools such as the CAM-ICU and ICDSC.[43]
Creation of delirium networks and advocacy initiatives
Specialty societies such as the American Geriatric Society and SCCM have provided guidelines to assist their representative constituents to address delirium.[13, 44] Three major international interdisciplinary delirium societies: the Europe Delirium Association, the American Delirium Society and Australasian Delirium Association provide a platform for research collaboration and knowledge translation and have recently formed a global representative group called ‘iDelirium’ to provide a unified voice for advancing care and to increase public health efforts to address delirium worldwide.
The ICU Liberation Collaborative is an initiative that has hospitals working with teams of leading national experts to implement evidence-based bundles of care (e.g. the ABCDEF bundle), enhance teamwork and create partnerships with other institutions across the U.S.
Finally, the Network for Investigation of Delirium across the U.S. (NIDUS) has recently been funded by the National Institute of Aging to foster collaboration and accelerate scientific discovery in delirium.
What are the common beliefs that have been challenged by recent trials?
ICU delirium research has increased substantially in the last 15 years from about 10 articles per year in the early 2000s to an estimated 300 articles per year in 2013–2016.
Is delirium an epiphenomenon or is it causally linked to important outcomes such as mortality and long-term cognitive impairment?
Delirium is associated with a 2–3 fold increased risk of death. [2] A more recent study, adjusting for disease severity until delirium onset, determined that delirium was not “causally” related with mortality.[45] These findings do not undermine the deleterious effects associated with delirium but rather raise awareness of the difference between “associations” versus “causality”. Criteria for causality require: strength of association, consistency, temporality, biological gradient, plausibility and an experiment that shows an intervention reducing delirium would result in a decrease in the outcome. Present research does not support all the causality criteria for mortality or for cognitive impairment associated with delirium. Delirium, for example, is independently and consistently associated with cognitive impairment, there is a biological gradient,[7] and it is plausible since transient systemic inflammation (manifesting as delirium) may lead to long-lasting neuro-inflammation.[46] By contrast, delirium does not always precede cognitive impairment and there is no randomized clinical trial (RCT) that shows that treatment of delirium improves long-term cognitive dysfunction.
What is rapidly-reversible sedation-associated delirium?
The level of consciousness, an important component of delirium assessment, is affected by sedation and may confound delirium assessment.[47] Delirium rates may be 10–15% higher when assessed while patients are receiving sedation.[47] This raises the issue of whether sedation-associated delirium has different prognostic effects? A recent evaluation of 102 MV patients receiving continuous sedation showed that of patients who were delirious while on sedation, only 12% rapidly reversed their delirium status within 2 hours of sedation interruption.[48] This small subset of patients who had rapidly-reversible sedation-associated delirium had outcomes similar to patients who never had delirium, while patients in whom delirium persisted > 2 hours after stopping sedation had worse clinical outcomes.[48] This study suggests that clinicians should focus delirium screening efforts, whenever possible, when patients are least sedated, but should not ignore positive delirium assessments when patients are arousable on sedation because in majority of patients delirium persists even after discontinuation of sedation.[48]
What is the role of antipsychotic medications in delirium?
Antipsychotics are given to >10% of ICU patients, often to reduce agitation. Small randomized studies have evaluated the role of antipsychotics to reduce delirium in MV adults.[26–28] Of these, only one study of 36 patients, comparing quetiapine to placebo, showed a reduction in delirium.[26] Important limitations exist for each study.
In the absence of dangerous agitation, there is little reason to administer antipsychotics, given these medications have side effects. Other potential causes of delirium such as pain or substance withdrawal should be considered. Antipsychotic medication should not be used for hypoactive delirium and rarely beyond ICU discharge.[49] While antipsychotic medications have been proposed for distressing symptoms such as hallucinations and delusions,[50] no data supporting their use in ICU patients is available.
Is there a role for dexmedetomidine in hyperactive delirium?
Dexmedetomidine has been shown to reduce post-operative delirium,[19] and when compared to a benzodiazepine infusion reduce delirium prevalence[22] and days without coma or delirium.[23] It should be noted though that in some studies, delirium was not the primary outcome.[22]. Dexmedetomidine has also been shown to help in agitated delirium in non-intubated patients.[29]
Recently the DahLIA trial[20] specifically assessed the role of dexmedetomidine in patients whose critical illness had resolved, but agitation precluded weaning from mechanical ventilation. Seventy-four patients were randomized to dexmedetomidine or placebo; patients treated with dexmedetomidine had increased ventilator-free hours at 7 days (median, 144.8 hours vs 127.5 hours) and faster resolution of their delirium symptoms (median, 23.3 hours vs 40.0 hours).
Do corticosteroids or statin medications have a role in delirium?
Two large studies[51],[10] have suggested that systemic corticosteroids increase the probability of delirium in the ICU. A subsequent single-center observational study of medical-surgical ICU patients,[52] contradicted these finding. A recent single-center sub-study[53] within the Dexamethasone for Cardiac Surgery (DECS) trial[54] showed no difference in delirium outcomes in the ICU randomized to dexamethasone or placebo. One very recent controlled study found that hydrocortisone use in patients with sepsis reduced the incidence of delirium by half.[55] Taken together these studies[52, 53, 55] suggest that corticosteroids with primarily glucocorticoid effects are neither a major risk factor for delirium nor do they reduce its incidence or duration but that corticosteroids with primarily mineralocorticoid activity may in fact reduce delirium incidence.
In critically ill patients, ICU statin use has been associated with reduced delirium,[56, 57] especially early during sepsis;[56] discontinuation of a previously used statin was associated with increased delirium in that study.[56] While we await the results of RCTs of statin therapy with delirium as a primary outcome, the recent Statin AKI Cardiac Surgery RCT of high-dose perioperative atorvastatin treatment showed no difference in delirium outcomes in patients randomized to a statin. Moreover, an ancillary study in ARDS patients also demonstrated no difference in delirium in patients randomized to statins vs. placebo.[58]
Should patients be treated with cholinesterase inhibitors to decrease the duration of delirium?
Impaired cholinergic neurotransmission is proposed as a pathophysiologic mechanism for delirium, making cholinesterase inhibitors an attractive treatment choice to increase acetylcholine levels. A recent RCT[59] randomized critically ill patients with delirium to either rivastigmine or placebo as an adjunct to haloperidol, but the trial had to be halted prematurely because mortality in the rivastigmine group (22%) was higher than in the placebo group (8%) and median duration of delirium was longer in the rivastigmine group (5 vs. 3 days). Given these safety concerns, the SCCM PAD guidelines strongly recommends against the use of cholinesterase inhibitors to either treat or prevent delirium.[13]
Should benzodiazepines always be prescribed in patient at risk for or with symptoms of alcohol withdrawal?
Alcohol use disorder (AUD) is the most serious substance abuse problem in the United States and worldwide, with reported rates of 20% to 50% in hospitalized patients. Many alcohol dependent patients will develop uncomplicated alcohol withdrawal symptoms (AWS), but only 20% will require pharmacological intervention; benzodiazepines have frequently been the mainstay of therapy.[60] The use of objective tools now allows targeting only those patients at risk for complicated-AWS with prophylactic management strategies.[61] Benzodiazepine-sparing protocols consisting of alpha2 agonists (i.e., dexmedetomidine, guanfacine, clonidine) that address the adrenergic storm associated with AWS and/or various anticonvulsant agents (e.g., gabapentin, carbamazepine, valproic acid) acting primarily as glutamate modulators to safely and effectively manage AWS have been recently proposed, and will need to be evaluated in larger studies.
What are remaining areas of uncertainties/work to be done?
Harmonization of outcomes/development of core outcomes
For studies to be maximally informative, and to allow cross comparisons between studies evaluating similar interventions in similar populations, outcomes should be selected, defined, and measured consistently. For these reasons, core outcome sets (COS) have been proposed and these outcome sets include those outcomes perceived, through a rigorous consensus process involving key stakeholders, including patients, as fundamental to measure in all trials related to a specific and defined area of interest (may be based on a disease, condition, or intervention).[62] The COS should be small enough to minimize participant burden, limit research costs, and encourage researcher adoption, but large enough to capture outcomes deemed important to future decisions makers.
Improved statistical methods in delirium research
Evaluating the efficacy of interventions for reducing delirium in the ICU is challenging given that (1) delirium status changes over time, (2) delirium cannot be assessed when patients are comatose (3) delirium assessment often does not continue after ICU discharge, preventing assessment of its full duration, and (4) mortality is a competing event for delirium assessment. Sometimes a composite outcome of delirium status and mortality is used— delirium-free days. However, use of delirium-free days does not fully address the competing risk of coma, leading to use of delirium/coma-free days in some studies.[23] More recently, joint models[63] have been proposed to address these challenges via linking two survival models: one for the recurrent daily delirium status and one for a terminating event (e.g., ICU discharge or death). This approach (as used in recent critical care delirium research[58]) yields a hazard ratio (HR) for delirium in the intervention versus control group, with a HR <1 interpreted as a lower daily hazard of delirium—implying a shorter mean duration of delirium among days at risk for delirium (i.e., days in which a patient is alive, in the ICU, and in a non-comatose state).
Standardization of terminology-delirium vs encephalopathy, role of consciousness in delirium diagnosis, arousal level and delirium (untestable patients?)
While the DSM-5 definition[1] of delirium is used widely in clinical and research settings, it does not represent a consensus definition in all fields of medicine. In classic neurologic texts, delirium falls under the broader rubric of acute confusional states, and while including primarily hyperactive delirium subtypes, it excludes hypoactive delirium. The term “encephalopathy” is often employed to describe a range of mental states, including hypoactive delirium when a primary etiology is identified. Given that delirium is often multifactorial, this convention may be reductionist, resulting in overlooking reversible causes. The lack of consensus definition exists even within psychiatry as evidenced by the evolving DSM delirium criteria. For example, the DSM-IV-TR criteria required that a disturbance in consciousness must be present, while in the most recent DSM-5,[1] this criteria was changed to a disturbance in attention and awareness. A particular example is the debate whether delirium can be diagnosed in states with severely reduced arousal, which the DSM-5 specifically excludes.[1] Level of arousal exists along a continuum and there is no clear evidence that patients with severely disturbed arousal are different from patients with milder disturbance. Thus if non-comatose, but non-communicative patients unable to demonstrate inattention, are excluded from delirium evaluations, these cases of delirium may be missed and this will have negative implications on patient safety and outcomes in clinical and research endeavors.
Sleep and delirium
A disturbed sleep-wake rhythm occurs commonly during delirium, but it is unclear whether this is a cause of delirium, an early sign of delirium, or both.[64] A before-after study of a multi-faceted sleep-promoting intervention found 50% lower odds of delirium and coma, though self-reported sleep ratings did not improve. [12] It is therefore unclear whether the reduced delirium resulted from improved sleep.[12]
Melatonin plays an important role in the sleep-wake cycle. In 67 patients, hospitalized due to serious medical problems, a RCT comparing the oral melatonin receptor agonist ramelteon, to placebo, reported a lower incidence of delirium in the ramelteon group.[65]
Alpha-2 agonists, such as dexmedetomidine, may promote sleep,[66] and recent studies point to beneficial effects in ICU patients.[67] The bidirectional relationship between sleep and delirium still need to be better understood.
Electroencephalography in delirium
It is assumed, but not studied extensively, that different etiological subtypes of delirium (e.g. toxic-metabolic, infectious, postoperative) share the same electroencephalographic (EEG) features. The EEG during delirium shows diffuse slowing of background activity and increased spectral variability with often periodic discharges such as triphasic waves and polymorphic delta activity.[68] In some delirious patients, the EEG may show electrographic seizures and periodic epileptiform discharges. Non-convulsive status epilepticus (NCSE) is a form of status epilepticus where there may be minimal seizure activity clinically, but there is evidence of its presence on EEG. Many patients with NCSE present with delirium, and it should be considered in the differential diagnosis in high risk patients. [68] Various approaches are being explored to develop more sensitive delirium monitoring with objective tools. A promising approach seems to be a brief EEG registration with a limited number of electrodes and automated processing.[69]
Family-centered perspective in delirium and humanizing intensive care
Non-pharmacological interventions, including early mobilization, are examples of highly humanistic approaches that involve communication and reassurance, and are effective in preventing delirium.[70],[24] Despite qualitative descriptions of patients’ ICU experiences being significantly enhanced by the presence of family members,[71] no randomized controlled trials have evaluated the potential role of families in altering the course of ICU delirium or post-critical illness trajectories. Similarly the impact of delirium on patient, caregivers,[72] family experiences need to be better studied.
The role of implementation science in rapidly translating delirium research into practice
The current translational cycle of evidence based medical research discoveries into widely implemented clinical therapeutics and healthcare services are inefficient and expensive.[73, 74] Implementation science is an action oriented science that aims to develop tools, processes, and strategies to rapidly implement evidence-based, sustainable, and scalable healthcare solutions into the local healthcare environment.[73] Implementation scientists view the health care system as a complex adaptive network that includes a large number of semi-autonomous agents interacting in dynamic and non-linear ways. This complex interaction leads into constant emerging behaviors with limited centralized control.[75] Principles and the tools of implementation science should be used to create a local coalition of brain research centers, advocacy groups, and clinical services. Brain-care service line should be created across the hospital and ambulatory services, with standardized data collection (preferably leveraging information technology), to serve the clinical operation, quality, and safety mission first, then research, and should lead to delirium specific decision support tools. Finally, delirium scientists need to start innovating in a limited resource environment by including future payments of their solutions into their development requirement; thinking about the value of their solutions within a population health management payment model.
What are some of the top study areas/trials to be done in the next 10 years?
Development and validation of objective tools for delirium screening/diagnosis in critically ill patients e.g. electroencephalogram, computer based apps
Understanding the pathophysiology of delirium and its relationship mechanistically to long-term cognitive decline.
Development of new models to improve delirium phenotyping
Understanding the attributable risk of delirium on outcomes; going beyond associations to causal inferences.
Elucidating the biomarkers of delirium and incorporation into predictive models
-
Large randomized controlled trials that are needed in ICU patients
Safety and efficacy of antipsychotics medications on delirium and long-term outcomes
Safety and efficacy of sleep optimization (nonpharmacological or pharmacological) on delirium and long-term outcomes
Safety and efficacy of cognitive and physical training on delirium and long-term outcomes?
Safety and efficacy of alternate sedation paradigms (dexmedetomidine, clonidine, propofol, general anesthetics) on delirium and long-term outcomes.
The role of humanization of ICU care, specifically family engagement and other non-pharmacological interventions (e.g. restraints), on delirium and patient and family long-term outcomes
Acknowledgments
Funding:
Dr. Pandharipande (R01HL111111 and R01AG 035117) and Dr. Needham (R24HL111895 and R24AG054259) are supported by the National Institutes of Health. Dr. Ely is supported by the National Institutes of Health (R01AG 035117 and R01HL111111) and the VA GRECC. Prof. A.J.C. Slooter is supported by the European Society of Intensive Care Medicine, Technology Foundation STW ((14066) and the European Union (H2020-PHC-12-2014-672974). Dr. Devlin is supported by the National Institutes of Health (1R21G04567212). Dr. Shehabi is funded by the National Health and Medical Research Council of Australia.
Footnotes
Disclosures:
Dr. Pandharipande has a research grant from Hospira Inc.
Dr. Ely has received research grants and/or honoraria from Hospira, Orion, Pfizer and Abbott.
Dr. Arora has an unrestricted education grant from Pfizer Canada and received honoraria from Mallinckrodt Pharmaceutical.
Dr. Devlin has received a research grant from AstraZeneca Pharmaceuticals
Prof. A.J.C. Slooter works on the development of an EEG-based delirium monitor, any (future) profits of this technology will be used for future scientific research only.
Dr. Shehabi has received related unrestricted research and educational from Hospira Inc, Pfizer and Orion Pharma. Speaker honorarium and travel expenses reimbursed to employing institution.
Contributor Information
Pratik Pandharipande, Professor of Anesthesiology and Surgery, Department of Anesthesiology, Division of Anesthesiology Critical Care Medicine, Vanderbilt University Medical Center, Nashville, TN, USA.
E. Wesley Ely, Professor of Medicine, Division of Pulmonary and Critical Care and Health Services Research, Vanderbilt University and VA-GRECC, Nashville, TN, USA.
Rakesh C. Arora, Professor - Surgery, Anesthesiology & Perioperative Medicine and Physiology & Pathophysiology, Department of Surgery, University of Manitoba, St. Boniface Hospital, Winnipeg, MB, Canada.
Michele C. Balas, Associate Professor, The Ohio State University, College of Nursing, Center of Excellence in Critical and Complex Care, Columbus, OH, USA.
Malaz Boustani, Indiana University Center for Health Innovation and Implementation Science, Indianapolis, IN, USA.
Gabriel Heras La Calle, International Research Project Humanizing Intensive Care (Proyecto HU-CI), Intensive Care Unit. Hospital Universitario de Torrejón, Madrid. Spain.
Colm Cunningham, Assistant Professor in Neuroscience, School of Biochemistry and Immunology & Trinity College Institute of Neuroscience, Lloyd Institute, Trinity College Dublin, Ireland
John W. Devlin, School of Pharmacy, Northeastern University AND, Division of Pulmonary, Critical Care and Sleep Medicine, Tufts Medical Center;, Boston, MA, USA.
Julius Elefante, Department of Psychiatry, Faculty of Medicine, University of British Columbia, Canada.
Jin H. Han, Associate Professor of Emergency Medicine, Department of Emergency Medicine, Vanderbilt University Medical Center, Nashville, TN, USA.
Alasdair MacLullich, Professor of Geriatric Medicine, Edinburgh Delirium Research Group, Geriatric Medicine Unit, University of Edinburgh, Scotland.
José R. Maldonado, Professor of Psychiatry, Internal Medicine, Emergency Medicine, Surgery & Law, Medical Director, Psychosomatic Medicine Service & Clinic, Medical Director, Emergency Psychiatry Service, Stanford University School of Medicine, Stanford, CA, USA.
Alessandro Morandi, Ancelle Hospital, Department of Rehabilitation,, Cremona, Italy.
Dale M. Needham, Professor of Medicine and of Physical Medicine & Rehabilitation, Division of Pulmonary & Critical Care Medicine, Johns Hopkins University, Baltimore, MD, USA.
Valerie J Page, Consultant in Critical Care, Watford General Hospital, United Kingdom.
Louise Rose, TD Nursing Professor in Critical Care Research, Sunnybrook Health Sciences Centre, Associate Professor, Lawrence S. Bloomberg Faculty of Nursing, University of Toronto, Canada.
Jorge I.F. Salluh, Senior Researcher, Department of Critical Care, rD’ OR Institute for Research and Education and Post-Graduate Program Federal University of Rio de Janeiro, Rio de Janeiro, Brazil.
Tarek Sharshar, Senior Consultant, Department of Intensive Care Medicine, Raymond Poincaré Hospital, Paris, France, Laboratory of Human Histology and animal Models, Institut Pasteur, Paris France.
Yahya Shehabi, Professor of Intensive Care Medicine, School of Clinical Sciences, Faculty of Medicine, Monash University & Medical Center, Melbourne, Australia, University New South Wales, Clinical School of Medicine, NSW 2031.
Yoanna Skrobik, Department of Medicine, McGill University, Montreal, Canada.
Arjen Slooter, Professor of Intensive Care Neuropsychiatry and Consultant Neurologist – Intensivist, Department of Intensive Care Medicine, Brain Center Rudolf Magnus, Utrecht University, University Medical Center Utrecht, The Netherlands.
Heidi AB Smith, Assistant Professor, Department of Anesthesiology & Pediatrics, Division of Pediatric Cardiac Anesthesia, Monroe Carell Jr. Children’s Hospital at Vanderbilt, Nashville, TN, USA.
References
- 1.Association. AP. Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association; Washington DC: 2013. [Google Scholar]
- 2.Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE, Jr, Inouye SK, Bernard GR, Dittus RS. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 3.Pandharipande P, Cotton BA, Shintani A, Thompson J, Pun BT, Morris JA, Jr, Dittus R, Ely EW. Prevalence and risk factors for development of delirium in surgical and trauma intensive care unit patients. J Trauma. 2008;65:34–41. doi: 10.1097/TA.0b013e31814b2c4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McPherson JA, Wagner CE, Boehm LM, Hall JD, Johnson DC, Miller LR, Burns KM, Thompson JL, Shintani AK, Ely EW, Pandharipande PP. Delirium in the cardiovascular ICU: exploring modifiable risk factors. Crit Care Med. 2013;41:405–413. doi: 10.1097/CCM.0b013e31826ab49b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peterson JF, Pun BT, Dittus RS, Thomason JW, Jackson JC, Shintani AK, Ely EW. Delirium and its motoric subtypes: a study of 614 critically ill patients. J Am Geriatr Soc. 2006;54:479–484. doi: 10.1111/j.1532-5415.2005.00621.x. [DOI] [PubMed] [Google Scholar]
- 6.Meagher DJ, Leonard M, Donnelly S, Conroy M, Adamis D, Trzepacz PT. A longitudinal study of motor subtypes in delirium: relationship with other phenomenology, etiology, medication exposure and prognosis. J Psychosom Res. 2011;71:395–403. doi: 10.1016/j.jpsychores.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, Brummel NE, Hughes CG, Vasilevskis EE, Shintani AK, Moons KG, Geevarghese SK, Canonico A, Hopkins RO, Bernard GR, Dittus RS, Ely EW. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369:1306–1316. doi: 10.1056/NEJMoa1301372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Norman BC, Jackson JC, Graves JA, Girard TD, Pandharipande PP, Brummel NE, Wang L, Thompson JL, Chandrasekhar R, Ely EW. Employment Outcomes After Critical Illness: An Analysis of the Bringing to Light the Risk Factors and Incidence of Neuropsychological Dysfunction in ICU Survivors Cohort. Crit Care Med. 2016;44:2003–2009. doi: 10.1097/CCM.0000000000001849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson JC, Pandharipande PP, Girard TD, Brummel NE, Thompson JL, Hughes CG, Pun BT, Vasilevskis EE, Morandi A, Shintani AK, Hopkins RO, Bernard GR, Dittus RS, Ely EW Bringing to light the Risk F, Incidence of Neuropsychological dysfunction in ICUssi. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. The lancet Respiratory medicine. 2014;2:369–379. doi: 10.1016/S2213-2600(14)70051-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wassenaar A, van den Boogaard M, van Achterberg T, Slooter AJ, Kuiper MA, Hoogendoorn ME, Simons KS, Maseda E, Pinto N, Jones C, Luetz A, Schandl A, Verbrugghe W, Aitken LM, van Haren FM, Donders AR, Schoonhoven L, Pickkers P. Multinational development and validation of an early prediction model for delirium in ICU patients. Intensive Care Med. 2015;41:1048–1056. doi: 10.1007/s00134-015-3777-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pandharipande P, Shintani A, Peterson J, Pun BT, Wilkinson GR, Dittus RS, Bernard GR, Ely EW. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology. 2006;104:21–26. doi: 10.1097/00000542-200601000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Kamdar BB, King LM, Collop NA, Sakamuri S, Colantuoni E, Neufeld KJ, Bienvenu OJ, Rowden AM, Touradji P, Brower RG, Needham DM. The effect of a quality improvement intervention on perceived sleep quality and cognition in a medical ICU. Crit Care Med. 2013;41:800–809. doi: 10.1097/CCM.0b013e3182746442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barr J, Fraser GL, Puntillo K, Ely EW, Gelinas C, Dasta JF, Davidson JE, Devlin JW, Kress JP, Joffe AM, Coursin DB, Herr DL, Tung A, Robinson BR, Fontaine DK, Ramsay MA, Riker RR, Sessler CN, Pun B, Skrobik Y, Jaeschke R American College of Critical Care M. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41:263–306. doi: 10.1097/CCM.0b013e3182783b72. [DOI] [PubMed] [Google Scholar]
- 14.Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, Truman B, Speroff T, Gautam S, Margolin R, Hart RP, Dittus R. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286:2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 15.Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med. 2001;27:859–864. doi: 10.1007/s001340100909. [DOI] [PubMed] [Google Scholar]
- 16.Balas MC, Vasilevskis EE, Olsen KM, Schmid KK, Shostrom V, Cohen MZ, Peitz G, Gannon DE, Sisson J, Sullivan J, Stothert JC, Lazure J, Nuss SL, Jawa RS, Freihaut F, Ely EW, Burke WJ. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med. 2014;42:1024–1036. doi: 10.1097/CCM.0000000000000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barnes-Daly MA, Phillips G, Ely EW. Improving Hospital Survival and Reducing Brain Dysfunction at Seven California Community Hospitals: Implementing PAD Guidelines Via the ABCDEF Bundle in 6,064 Patients. Crit Care Med. 2016 doi: 10.1097/CCM.0000000000002149. [DOI] [PubMed] [Google Scholar]
- 18.Vincent JL, Shehabi Y, Walsh TS, Pandharipande PP, Ball JA, Spronk P, Longrois D, Strom T, Conti G, Funk GC, Badenes R, Mantz J, Spies C, Takala J. Comfort and patient-centred care without excessive sedation: the eCASH concept. Intensive Care Med. 2016;42:962–971. doi: 10.1007/s00134-016-4297-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Su X, Meng ZT, Wu XH, Cui F, Li HL, Wang DX, Zhu X, Zhu SN, Maze M, Ma D. Dexmedetomidine for prevention of delirium in elderly patients after non-cardiac surgery: a randomised, double-blind, placebo-controlled trial. Lancet. 2016 doi: 10.1016/S0140-6736(16)30580-3. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 20.Reade MC, Eastwood GM, Bellomo R, Bailey M, Bersten A, Cheung B, Davies A, Delaney A, Ghosh A, van Haren F, Harley N, Knight D, McGuiness S, Mulder J, O’Donoghue S, Simpson N, Young P, Dah LIAI Australian, New Zealand Intensive Care Society Clinical Trials G. Effect of Dexmedetomidine Added to Standard Care on Ventilator-Free Time in Patients With Agitated Delirium: A Randomized Clinical Trial. JAMA. 2016;315:1460–1468. doi: 10.1001/jama.2016.2707. [DOI] [PubMed] [Google Scholar]
- 21.Jakob SM, Ruokonen E, Grounds RM, Sarapohja T, Garratt C, Pocock SJ, Bratty JR, Takala J Dexmedetomidine for Long-Term Sedation I. Dexmedetomidine vs midazolam or propofol for sedation during prolonged mechanical ventilation: two randomized controlled trials. JAMA. 2012;307:1151–1160. doi: 10.1001/jama.2012.304. [DOI] [PubMed] [Google Scholar]
- 22.Riker RR, Shehabi Y, Bokesch PM, Ceraso D, Wisemandle W, Koura F, Whitten P, Margolis BD, Byrne DW, Ely EW, Rocha MG, Group SS. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA. 2009;301:489–499. doi: 10.1001/jama.2009.56. [DOI] [PubMed] [Google Scholar]
- 23.Pandharipande PP, Pun BT, Herr DL, Maze M, Girard TD, Miller RR, Shintani AK, Thompson JL, Jackson JC, Deppen SA, Stiles RA, Dittus RS, Bernard GR, Ely EW. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA. 2007;298:2644–2653. doi: 10.1001/jama.298.22.2644. [DOI] [PubMed] [Google Scholar]
- 24.Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, Spears L, Miller M, Franczyk M, Deprizio D, Schmidt GA, Bowman A, Barr R, McCallister KE, Hall JB, Kress JP. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373:1874–1882. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schaller SJ, Anstey M, Blobner M, Edrich T, Grabitz SD, Gradwohl-Matis I, Heim M, Houle T, Kurth T, Latronico N, Lee J, Meyer MJ, Peponis T, Talmor D, Velmahos GC, Waak K, Walz JM, Zafonte R, Eikermann M. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet. 2016;388:1377–1388. doi: 10.1016/S0140-6736(16)31637-3. [DOI] [PubMed] [Google Scholar]
- 26.Devlin JW, Roberts RJ, Fong JJ, Skrobik Y, Riker RR, Hill NS, Robbins T, Garpestad E. Efficacy and safety of quetiapine in critically ill patients with delirium: a prospective, multicenter, randomized, double-blind, placebo-controlled pilot study. Crit Care Med. 2010;38:419–427. doi: 10.1097/CCM.0b013e3181b9e302. [DOI] [PubMed] [Google Scholar]
- 27.Girard TD, Pandharipande PP, Carson SS, Schmidt GA, Wright PE, Canonico AE, Pun BT, Thompson JL, Shintani AK, Meltzer HY, Bernard GR, Dittus RS, Ely EW Investigators MT. Feasibility, efficacy, and safety of antipsychotics for intensive care unit delirium: the MIND randomized, placebo-controlled trial. Crit Care Med. 2010;38:428–437. doi: 10.1097/ccm.0b013e3181c58715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Page VJ, Ely EW, Gates S, Zhao XB, Alce T, Shintani A, Jackson J, Perkins GD, McAuley DF. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomised, double-blind, placebo-controlled trial. The lancet Respiratory medicine. 2013;1:515–523. doi: 10.1016/S2213-2600(13)70166-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carrasco G, Baeza N, Cabre L, Portillo E, Gimeno G, Manzanedo D, Calizaya M. Dexmedetomidine for the Treatment of Hyperactive Delirium Refractory to Haloperidol in Nonintubated ICU Patients: A Nonrandomized Controlled Trial. Crit Care Med. 2016;44:1295–1306. doi: 10.1097/CCM.0000000000001622. [DOI] [PubMed] [Google Scholar]
- 30.Reis PA, Comim CM, Hermani F, Silva B, Barichello T, Portella AC, Gomes FC, Sab IM, Frutuoso VS, Oliveira MF, Bozza PT, Bozza FA, Dal-Pizzol F, Zimmerman GA, Quevedo J, Castro-Faria-Neto HC. Cognitive dysfunction is sustained after rescue therapy in experimental cerebral malaria, and is reduced by additive antioxidant therapy. PLoS pathogens. 2010;6:e1000963. doi: 10.1371/journal.ppat.1000963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weberpals M, Hermes M, Hermann S, Kummer MP, Terwel D, Semmler A, Berger M, Schafers M, Heneka MT. NOS2 gene deficiency protects from sepsis-induced long-term cognitive deficits. J Neurosci. 2009;29:14177–14184. doi: 10.1523/JNEUROSCI.3238-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anderson ST, Commins S, Moynagh PN, Coogan AN. Lipopolysaccharide-induced sepsis induces long-lasting affective changes in the mouse. Brain, behavior, and immunity. 2015;43:98–109. doi: 10.1016/j.bbi.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 33.Bozza FA, Garteiser P, Oliveira MF, Doblas S, Cranford R, Saunders D, Jones I, Towner RA, Castro-Faria-Neto HC. Sepsis-associated encephalopathy: a magnetic resonance imaging and spectroscopy study. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2010;30:440–448. doi: 10.1038/jcbfm.2009.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Semmler A, Hermann S, Mormann F, Weberpals M, Paxian SA, Okulla T, Schafers M, Kummer MP, Klockgether T, Heneka MT. Sepsis causes neuroinflammation and concomitant decrease of cerebral metabolism. J Neuroinflammation. 2008;5:38. doi: 10.1186/1742-2094-5-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davis DH, Skelly DT, Murray C, Hennessy E, Bowen J, Norton S, Brayne C, Rahkonen T, Sulkava R, Sanderson DJ, Rawlins JN, Bannerman DM, MacLullich AM, Cunningham C. Worsening cognitive impairment and neurodegenerative pathology progressively increase risk for delirium. Am J Geriatr Psychiatry. 2015;23:403–415. doi: 10.1016/j.jagp.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith HA, Boyd J, Fuchs DC, Melvin K, Berry P, Shintani A, Eden SK, Terrell MK, Boswell T, Wolfram K, Sopfe J, Barr FE, Pandharipande PP, Ely EW. Diagnosing delirium in critically ill children: Validity and reliability of the Pediatric Confusion Assessment Method for the Intensive Care Unit. Crit Care Med. 2011;39:150–157. doi: 10.1097/CCM.0b013e3181feb489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith HA, Gangopadhyay M, Goben CM, Jacobowski NL, Chestnut MH, Savage S, Rutherford MT, Denton D, Thompson JL, Chandrasekhar R, Acton M, Newman J, Noori HP, Terrell MK, Williams SR, Griffith K, Cooper TJ, Ely EW, Fuchs DC, Pandharipande PP. The Preschool Confusion Assessment Method for the ICU: Valid and Reliable Delirium Monitoring for Critically Ill Infants and Children. Crit Care Med. 2016;44:592–600. doi: 10.1097/CCM.0000000000001428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Traube C, Silver G, Kearney J, Patel A, Atkinson TM, Yoon MJ, Halpert S, Augenstein J, Sickles LE, Li C, Greenwald B. Cornell Assessment of Pediatric Delirium: a valid, rapid, observational tool for screening delirium in the PICU*. Crit Care Med. 2014;42:656–663. doi: 10.1097/CCM.0b013e3182a66b76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mitasova A, Kostalova M, Bednarik J, Michalcakova R, Kasparek T, Balabanova P, Dusek L, Vohanka S, Ely EW. Poststroke delirium incidence and outcomes: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Crit Care Med. 2012;40:484–490. doi: 10.1097/CCM.0b013e318232da12. [DOI] [PubMed] [Google Scholar]
- 40.Naidech AM, Beaumont JL, Rosenberg NF, Maas MB, Kosteva AR, Ault ML, Cella D, Ely EW. Intracerebral hemorrhage and delirium symptoms. Length of stay, function, and quality of life in a 114-patient cohort. Am J Respir Crit Care Med. 2013;188:1331–1337. doi: 10.1164/rccm.201307-1256OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Frenette AJ, Bebawi ER, Deslauriers LC, Tessier AA, Perreault MM, Delisle MS, Bertrand JC, Desjardins M, Rico P, Khwaja K, Burry LD, Bernard F, Williamson DR. Validation and comparison of CAM-ICU and ICDSC in mild and moderate traumatic brain injury patients. Intensive Care Med. 2016;42:122–123. doi: 10.1007/s00134-015-3964-1. [DOI] [PubMed] [Google Scholar]
- 42.Fick DM, Agostini JV, Inouye SK. Delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2002;50:1723–1732. doi: 10.1046/j.1532-5415.2002.50468.x. [DOI] [PubMed] [Google Scholar]
- 43.Morandi A, Han JH, Meagher D, Vasilevskis E, Cerejeira J, Hasemann W, MacLullich AM, Annoni G, Trabucchi M, Bellelli G. Detecting Delirium Superimposed on Dementia: Evaluation of the Diagnostic Performance of the Richmond Agitation and Sedation Scale. Journal of the American Medical Directors Association. 2016 doi: 10.1016/j.jamda.2016.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.American Geriatrics Society Expert Panel on Postoperative Delirium in Older Adults. Book Clinical Practice Guideline for Postoperative Delirium in Older Adults. American Geriatrics Society; City: 2014. Clinical Practice Guideline for Postoperative Delirium in Older Adults. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Klein Klouwenberg PMC, Zaal IJ, Spitoni C, Ong DSY, van der Kooi AW, Bonten MJM, Slooter AJC, Cremer OL. The attributable mortality of delirium in critically ill patients: prospective cohort study. BMJ. 2014:349. doi: 10.1136/bmj.g6652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van Gool WA, van de Beek D, Eikelenboom P. Systemic infection and delirium: when cytokines and acetylcholine collide. Lancet. 2010;375:773–775. doi: 10.1016/S0140-6736(09)61158-2. [DOI] [PubMed] [Google Scholar]
- 47.Haenggi M, Blum S, Brechbuehl R, Brunello A, Jakob S, Takala J. Effect of sedation level on the prevalence of delirium when assessed with CAM-ICU and ICDSC. Intensive Care Med. 2013;39:2171–2179. doi: 10.1007/s00134-013-3034-5. [DOI] [PubMed] [Google Scholar]
- 48.Patel SB, Poston JT, Pohlman A, Hall JB, Kress JP. Rapidly reversible, sedation-related delirium versus persistent delirium in the intensive care unit. Am J Respir Crit Care Med. 2014;189:658–665. doi: 10.1164/rccm.201310-1815OC. [DOI] [PubMed] [Google Scholar]
- 49.Morandi A, Vasilevskis E, Pandharipande PP, Girard TD, Solberg LM, Neal EB, Koestner T, Torres RE, Thompson JL, Shintani AK, Han JH, Schnelle JF, Fick DM, Ely EW, Kripalani S. Inappropriate medication prescriptions in elderly adults surviving an intensive care unit hospitalization. J Am Geriatr Soc. 2013;61:1128–1134. doi: 10.1111/jgs.12329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383:911–922. doi: 10.1016/S0140-6736(13)60688-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schreiber MP, Colantuoni E, Bienvenu OJ, Neufeld KJ, Chen KF, Shanholtz C, Mendez-Tellez PA, Needham DM. Corticosteroids and transition to delirium in patients with acute lung injury. Crit Care Med. 2014;42:1480–1486. doi: 10.1097/CCM.0000000000000247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wolters AE, Veldhuijzen DS, Zaal IJ, Peelen LM, van Dijk D, Devlin JW, Slooter AJ. Systemic Corticosteroids and Transition to Delirium in Critically Ill Patients. Crit Care Med. 2015;43:e585–588. doi: 10.1097/CCM.0000000000001302. [DOI] [PubMed] [Google Scholar]
- 53.Sauer AM, Slooter AJ, Veldhuijzen DS, van Eijk MM, Devlin JW, van Dijk D. Intraoperative dexamethasone and delirium after cardiac surgery: a randomized clinical trial. Anesth Analg. 2014;119:1046–1052. doi: 10.1213/ANE.0000000000000248. [DOI] [PubMed] [Google Scholar]
- 54.Dieleman JM, Nierich AP, Rosseel PM, van der Maaten JM, Hofland J, Diephuis JC, Schepp RM, Boer C, Moons KG, van Herwerden LA, Tijssen JG, Numan SC, Kalkman CJ, van Dijk D Dexamethasone for Cardiac Surgery Study G. Intraoperative high-dose dexamethasone for cardiac surgery: a randomized controlled trial. JAMA. 2012;308:1761–1767. doi: 10.1001/jama.2012.14144. [DOI] [PubMed] [Google Scholar]
- 55.Keh D, Trips E, Marx G, et al. Effect of hydrocortisone on development of shock among patients with severe sepsis: The hypress randomized clinical trial. JAMA. 2016 doi: 10.1001/jama.2016.14799. [DOI] [PubMed] [Google Scholar]
- 56.Morandi A, Hughes CG, Thompson JL, Pandharipande PP, Shintani AK, Vasilevskis EE, Han JH, Jackson JC, Laskowitz DT, Bernard GR, Ely EW, Girard TD. Statins and delirium during critical illness: a multicenter, prospective cohort study. Crit Care Med. 2014;42:1899–1909. doi: 10.1097/CCM.0000000000000398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Page VJ, Davis D, Zhao XB, Norton S, Casarin A, Brown T, Ely EW, McAuley DF. Statin use and risk of delirium in the critically ill. Am J Respir Crit Care Med. 2014;189:666–673. doi: 10.1164/rccm.201306-1150OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Needham DM, Colantuoni E, Dinglas VD, Hough CL, Wozniak AW, Jackson JC, Morris PE, Mendez-Tellez PA, Ely EW, Hopkins RO. Rosuvastatin versus placebo for delirium in intensive care and subsequent cognitive impairment in patients with sepsis-associated acute respiratory distress syndrome: an ancillary study to a randomised controlled trial. The lancet Respiratory medicine. 2016 doi: 10.1016/S2213-2600(16)00005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van Eijk MM, Roes KC, Honing ML, Kuiper MA, Karakus A, van der Jagt M, Spronk PE, van Gool WA, van der Mast RC, Kesecioglu J, Slooter AJ. Effect of rivastigmine as an adjunct to usual care with haloperidol on duration of delirium and mortality in critically ill patients: a multicentre, double-blind, placebo-controlled randomised trial. Lancet. 2010;376:1829–1837. doi: 10.1016/S0140-6736(10)61855-7. [DOI] [PubMed] [Google Scholar]
- 60.Moss M, Burnham EL. Alcohol abuse in the critically ill patient. Lancet. 2006;368:2231–2242. doi: 10.1016/S0140-6736(06)69490-7. [DOI] [PubMed] [Google Scholar]
- 61.Maldonado JR, Sher Y, Das S, Hills-Evans K, Frenklach A, Lolak S, Talley R, Neri E. Prospective Validation Study of the Prediction of Alcohol Withdrawal Severity Scale (PAWSS) in Medically Ill Inpatients: A New Scale for the Prediction of Complicated Alcohol Withdrawal Syndrome. 2015 doi: 10.1093/alcalc/agv043. [DOI] [PubMed] [Google Scholar]
- 62.Sanderson T, Morris M, Calnan M, Richards P, Hewlett S. What outcomes from pharmacologic treatments are important to people with rheumatoid arthritis? Creating the basis of a patient core set. Arthritis Care Res (Hoboken) 2010;62:640–646. doi: 10.1002/acr.20034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rondeau V, Mathoulin-Pelissier S, Jacqmin-Gadda H, Brouste V, Soubeyran P. Joint frailty models for recurring events and death using maximum penalized likelihood estimation: application on cancer events. Biostatistics. 2007;8:708–721. doi: 10.1093/biostatistics/kxl043. [DOI] [PubMed] [Google Scholar]
- 64.Trompeo AC, Vidi Y, Locane MD, Braghiroli A, Mascia L, Bosma K, Ranieri VM. Sleep disturbances in the critically ill patients: role of delirium and sedative agents. Minerva Anestesiol. 2011;77:604–612. [PubMed] [Google Scholar]
- 65.Hatta K, Kishi Y, Wada K, Takeuchi T, Odawara T, Usui C, Nakamura H. Preventive effects of ramelteon on delirium: a randomized placebo-controlled trial. JAMA psychiatry. 2014;71:397–403. doi: 10.1001/jamapsychiatry.2013.3320. [DOI] [PubMed] [Google Scholar]
- 66.Nelson LE, Lu J, Guo T, Saper CB, Franks NP, Maze M. The alpha2-adrenoceptor agonist dexmedetomidine converges on an endogenous sleep-promoting pathway to exert its sedative effects. Anesthesiology. 2003;98:428–436. doi: 10.1097/00000542-200302000-00024. [DOI] [PubMed] [Google Scholar]
- 67.Wu XH, Cui F, Zhang C, Meng ZT, Wang DX, Ma J, Wang GF, Zhu SN, Ma D. Low-dose Dexmedetomidine Improves Sleep Quality Pattern in Elderly Patients after Noncardiac Surgery in the Intensive Care Unit: A Pilot Randomized Controlled Trial. Anesthesiology. 2016;125:979–991. doi: 10.1097/ALN.0000000000001325. [DOI] [PubMed] [Google Scholar]
- 68.Kaplan PW. The EEG in metabolic encephalopathy and coma. J Clin Neurophysiol. 2004;21:307–318. [PubMed] [Google Scholar]
- 69.van der Kooi AW, Zaal IJ, Klijn FA, Koek HL, Meijer RC, Leijten FS, Slooter AJ. Delirium detection using EEG: what and how to measure. Chest. 2015;147:94–101. doi: 10.1378/chest.13-3050. [DOI] [PubMed] [Google Scholar]
- 70.Inouye SK, Bogardus ST, Jr, Charpentier PA, Leo-Summers L, Acampora D, Holford TR, Cooney LM., Jr A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340:669–676. doi: 10.1056/NEJM199903043400901. [DOI] [PubMed] [Google Scholar]
- 71.Svenningsen H, Tonnesen E. Delirium incidents in three Danish intensive care units. Nurs Crit Care. 2011;16:186–192. doi: 10.1111/j.1478-5153.2011.00421.x. [DOI] [PubMed] [Google Scholar]
- 72.Belanger L, Ducharme F. Patients’ and nurses’ experiences of delirium: a review of qualitative studies. Nurs Crit Care. 2011;16:303–315. doi: 10.1111/j.1478-5153.2011.00454.x. [DOI] [PubMed] [Google Scholar]
- 73.Azar J, Adams N, Boustani M. The Indiana University Center for Healthcare Innovation and Implementation Science: Bridging healthcare research and delivery to build a learning healthcare system. Z Evid Fortbild Qual Gesundhwes. 2015;109:138–143. doi: 10.1016/j.zefq.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 74.Boustani MA, Frame A, Munger S, Healey P, Westlund J, Farlow M, Hake A, Austrom MG, Shepard P, Bubp C, Azar J, Nazir A, Adams N, Campbell NL, Chehresa A, Dexter P. Connecting research discovery with care delivery in dementia: the development of the Indianapolis Discovery Network for Dementia. Clinical interventions in aging. 2012;7:509–516. doi: 10.2147/CIA.S36078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Boustani M, Baker MS, Campbell N, Munger S, Hui SL, Castelluccio P, Farber M, Guzman O, Ademuyiwa A, Miller D, Callahan C. Impact and recognition of cognitive impairment among hospitalized elders. J HospMed. 2010;5:69–75. doi: 10.1002/jhm.589. [DOI] [PMC free article] [PubMed] [Google Scholar]