Abstract
Objective
To estimate trends in the prevalence and socio-economic distribution of chronic conditions among women hospitalized for obstetric delivery in the United States.
Methods
A retrospective, serial cross-sectional analysis was conducted using 2005 to 2014 data from the National Inpatient Sample. We estimated the prevalence of eight common, chronic conditions, each associated with obstetric morbidity and mortality, among all childbearing women and then across socio-economic predictors of obstetric outcomes. Differences over time were measured and compared across rural vs. urban residence, income, and payer subgroups for each condition.
Results
We identified 8,193,707 delivery hospitalizations, representing 39,273,417 delivery hospitalizations occurring nationally between 2005 and 2014. Identification of at least one chronic condition increased significantly between 2005–2006 and 2013–2014 (66.9 per 1,000 delivery hospitalizations in 2005–2006 vs. 91.8 per 1,000 delivery hospitalizations in 2014–2015). The prevalence of multiple chronic conditions also increased during the study period, from 4.7 (95% CI 4.2–5.2) to 8.1 (95% CI 7.8–8.4) per 1,000 delivery hospitalizations between 2005–2006 and 2013–2014. Chronic respiratory disease, chronic hypertension, substance use disorders, and pre-existing diabetes were the disorders with the greatest increases in prevalence over time Increasing disparities over time were identified across all socio-economic subgroups analyzed including rural vs. urban residence, income, and payer. Key areas of concern include the rate at which substance use disorders rose among rural women and the disproportionate burden of each condition among women from the lowest income communities and among women with Medicaid as their primary payer.
Conclusion
From 2005–2006 through 2013–2014, the prevalence of chronic conditions increased across all segments of the childbearing population. Widening disparities were identified over time, with key areas of concern including disproportionate, progressive increases in the burden of chronic conditions among women from rural and low income communities and those with deliveries funded by Medicaid.
INTRODUCTION
Increasing rates of maternal morbidity and mortality in the United States are well-documented.1 Complications from pre-existing, chronic conditions are the fastest rising cause of maternal mortality in the United States, now accounting for half of all maternal deaths.2 Population-level analyses have identified an increased risk for delivery-related morbidity and mortality among women with certain chronic conditions, including those with chronic respiratory disease, chronic hypertension, substance use disorders, pre-existing diabetes, chronic heart disease, chronic renal disease, human immunodeficiency virus (HIV), and chronic liver disease.3,4
The prevalence of chronic hypertension, substance use disorders, pre-existing diabetes, chronic heart disease, and chronic liver disease increased among the childbearing population through 2006–09, while rates of HIV appeared to have stabilized among the childbearing women by 2011.5–10 Whether the prevalence of these conditions has stabilized, decreased, or worsened since these reports is largely unknown. There is also a paucity of information on how the prevalence of chronic conditions varies by key socio-economic predictors of obstetric morbidity and mortality, including rural vs. urban residence,11 income,4,12 and insurance coverage status.4 These estimates are necessary for providers and policymakers to identify populations that would most benefit from evidence-based interventions to reduce maternal morbidity and mortality and improve maternal health. To address these gaps in knowledge, our objective was to estimate trends in the prevalence and socio-economic distribution of chronic conditions among the childbearing population in the United States between 2005 and 2014.
MATERIALS AND METHODS
We conducted a retrospective, serial cross-sectional analysis on a 20% sample of all delivery hospitalization discharges in the United States between 2005 and 2014 using the Healthcare Cost and Utilization Project’s National Inpatient Sample, compiled by the Agency for Healthcare Research and Quality. The National Inpatient Sample is the largest nationally-representative sample of hospital discharges in the United States.13 The dataset contains clinical and non-clinical data for each hospitalization, including diagnostic and procedure codes, patient demographic characteristics, and expected payment source. Deliveries were identified by ICD-9 codes using previously described methods.14 Because the analysis was of de-identified national data, our study was deemed exempt from review by the Institutional Review Board at the University of Michigan Medical School.
We examined the prevalence of eight common, chronic conditions known to impact obstetric morbidity and mortality: chronic respiratory disease, chronic hypertension, substance use disorders, pre-existing diabetes, chronic heart disease, chronic renal disease, chronic liver disease, and HIV. We focused our analyses on pre-existing conditions rather than pregnancy-related conditions. Chronic conditions were defined using the ICD-9 codes listed in Table 1, which were chosen for inclusion based on review of literature13,14 and author consensus. Sub-group analysis of ICD-9-CM codes included in the variable for chronic respiratory disease revealed that this variable was comprised almost entirely of observations with diagnosis codes for asthma (493.x) and will be referred to as asthma for the remainder of this report.
Table 1.
List of International Classification of Conditions, Ninth Revision, Clinical Modification codes
| Conditions | ICD-9-CM* Codes |
|---|---|
| Chronic respiratory disease | 491.x–496.x |
| Chronic hypertension | 401.x–405.x, 642.0x, 642.1x, 642.2x, 642.7x |
| Substance use disorders | 303.01, 303.02, 303.03, 304.x, 305.0x, 305.2x–305.9x, 648.3x |
| Pre-existing diabetes | 249.x, 250.x, 648.0x |
| Chronic heart disease | 412.x–414.x, 394.x–397.x, 424.x, 428.22, 428.23, 428.32, 428.33, 428.42, 428.43, 428.42, 428.43, 745.0x–747.4x, 648.5x |
| Chronic renal disease | 581.x–583.x, 585.x, 587.x, 588.x, 646.2x |
| Chronic liver disease | 571.x, 572.x |
| HIV | 042.x, V08.x |
ICD-9-CM, International Classification of Conditions, Ninth Revision, Clinical Modification
We controlled for several covariates in our analyses, including age, rural vs. urban residence, median household income quartile for the patient’s ZIP Code, and primary payer. Given that a number of hospitals and HCUP partners do not report data on race or ethnicity, we were unable to include these co-variates.13 Location of residence was defined as rural or urban using the National Center for Health Statistics Classification and Urban Influence Codes.15 Payment sources were grouped into public insurance (Medicaid and Medicare), private insurance, and uninsured or self-pay. Given that fewer than 0.6% of the delivery hospitalizations were funded by Medicare, public sources are referred to as Medicaid throughout the study. The number of observations with missing values was approximately 2% of all delivery hospitalizations, which was considered sufficient for analysis.
We used multivariable logistic regression models with predictive margins to obtain estimates of disease-specific prevalence and to estimate the rates at which any one and multiple chronic conditions were identified per 1,000 delivery hospitalizations. Data was pooled into two-year periods to increase the precision of our estimates. We estimated disease-specific prevalence by key socio-economic predictors for the four most prevalent conditions by interacting rural vs. urban residence, income, and payer with time in adjusted multivariable logistic regression models. Predictive margins were used in all sub-group analyses to generate adjusted prevalence estimates. We examined differences in prevalence for each condition over time by subgroup. We compared changes in prevalence over time across subgroups using a difference-in-differences framework.
We utilized National Inpatient Sample trend weights to allow for comparisons across years. Results are weighted to allow for nationally-representative inferences unless otherwise noted. Full details about sampling and weighting procedures are available at the Healthcare Cost and Utilization Project website.13 Two-sided P values <.05 were considered statistically significant. All analyses were conducted using STATA version 14.2 (StataCorp, College Station, TX).
RESULTS
The sample consisted of 8,193,707 delivery hospitalizations, representing 39,273,417 delivery hospitalizations occurring in the United States from 2005 through 2014. We identified 637,276 delivery hospitalizations in which at least one of eight common, chronic conditions was identified, representing 3,054,540 delivery hospitalizations over the 10-year period. Mean aged increased over the study period from 27.4 (95% CI 27.3–27.6) years in 2005–06 to 28.2 (95% CI 28.2–28.3) years in 2013–14. In comparing delivery hospitalizations among patients identified as having chronic conditions to those without, higher proportions of women with chronic conditions had deliveries funded by Medicaid (51.1% (95% CI 49.9–52.2 ) vs. 42.9% (95% CI 41.9–44.0)) and lived in ZIP Codes with median incomes in the bottom quartile nationally (32.6% (95% CI 31.3–33.8) vs. 26.9% (95% CI 25.8–28.0 )) (Table 2).
Table 2.
Characteristics of Women with Chronic Conditions vs. All Other Women with Hospital Deliveries, United States 2005–2014 (Survey Weighted %, 95% CI)
| Characteristic | All patients (N=8,193,707) | Patients with chronic conditions (n=637,276) | Patients without chronic conditions (n=7,556,431) |
|---|---|---|---|
| Age (years) | |||
| <18 | 2.9 (2.8–3.0) | 2.3 (2.2–2.4) | 2.9 (2.9–3.0) |
| 18–34 | 82.3 (82.1–82.6) | 78.9 (78.6–79.2) | 82.6 (82.3–82.9) |
| ≥35 | 14.8 (14.4–15.1) | 18.8 (18.5–19.2) | 14.4 (14.1–14.8) |
| Residence | |||
| Rural | 14.6 (13.9–15.3) | 14.2 (13.5–15.0) | 14.6 (13.9–15.4) |
| Income | |||
| Bottom quartile* | 27.3 (26.2–28.4) | 32.6 (31.3–33.8) | 26.9 (25.8–28.0) |
| Payer | |||
| Medicaid | 43.6 (42.5–44.7) | 51.1 (49.9–52.2) | 42.9 (41.9–44.0) |
| Private | 50.3 (49.1–51.6) | 43.7 (42.4–44.9) | 50.9 (49.7–52.1) |
| Uninsured or Self-pay | 6.1 (5.7–6.5) | 5.3 (5.0–5.6) | 6.2 (5.8–6.6) |
Represents patients living in a ZIP Code with median income in the bottom income quartile nationally
Overall, identification of any chronic condition at the time of delivery hospitalization increased nearly 40% in relative terms from 2005–06 through 2013–14, from 66.9 (95% CI 63.0–70.8) to 91.8 (95% CI 90.0–93.6) per 1,000 delivery hospitalizations. The prevalence of multiple chronic conditions also increased during the study period, from 4.7 (95% CI 4.2–5.2) to 8.1 (95% CI 7.8–8.4) per 1,000 delivery hospitalizations between 2005–06 and 2013–14.. From 2005–06 through 2013–14, we observed significant increases in the prevalence of all conditions studied except for HIV and chronic heart disease (P for trend <.001 for each condition that increased in prevalence), while rates of HIV remained statistically unchanged over the study period (P=0.48) and the prevalence of chronic heart disease decreased (P<.001) (Table 3).
Table 3.
Weighted Adjusted National Estimates of Prevalence of Chronic Conditions per 1,000 Delivery Hospitalizations (95% CI)*
| Condition | 2005–2006 | 2007–2008 | 2009–2010 | 2011–2012 | 2013–2014 | P for Trend |
|---|---|---|---|---|---|---|
| Any one condition | 66.9 (63.0–70.8) | 72.5 (69.0–76.0) | 77.3 (73.3–81.3) | 82.8 (79.9–85.6) | 91.8 (90.0–93.6) | <.001 |
| Multiple conditions | 4.7 (4.2–5.2) | 5.3 (4.8–5.8) | 6.3 (5.8–6.9) | 7.0 (6.6–7.4) | 8.1 (7.8–8.4) | <.001 |
|
| ||||||
| Asthma | 24.2 (22.1–26.3) | 29.4 (27.4–31.4) | 32.7 (30.4–35.1) | 36.0 (34.3–37.8) | 40.0 (38.9–41.2) | <.001 |
| Chronic hypertension | 15.8 (15.0–16.7) | 17.6 (16.6–18.6) | 20.5 (19.4–21.6) | 22.2 (21.4–23.0) | 23.6 (23.1–24.2) | <.001 |
| Substance use disorders | 12.9 (11.5–14.3) | 12.8 (11.8–13.9) | 13.4 (12.2–14.6) | 15.2 (14.3–16.0) | 19.6 (18.8–20.4) | <.001 |
| Pre-existing diabetes | 8.6 (8.0–9.2) | 8.8 (8.3–9.4) | 9.6 (9.0–10.2) | 9.9 (9.5–10.3) | 10.3 (10.0–10.6) | <.001 |
| Chronic heart disease | 7.2 (6.6–7.8) | 5.9 (5.4–6.3) | 4.1 (3.8–4.4) | 3.3 (3.1–3.5) | 3.1 (3.0–3.2) | <.001 |
| Chronic renal disease | 2.0 (1.9–2.1) | 2.3 (2.2–2.5) | 2.6 (2.4–2.7) | 2.7 (2.5–2.8) | 2.9 (2.8–3.0) | <.001 |
| HIV | 0.98 (0.81–1.2) | 1.0 (0.74–1.3) | 1.0 (0.82–1.3) | 0.84 (0.70–0.97) | 0.87 (0.78–0.95) | 0.48 |
| Chronic liver disease | 0.18 (0.15–0.21) | 0.21 (0.18–0.24) | 0.28 (0.24–0.31) | 0.35 (0.30–0.39) | 0.37 (0.34–0.41) | <.001 |
Adjusted for age, payer, rural vs. urban residence, and national income quartile for ZIP Code of residence
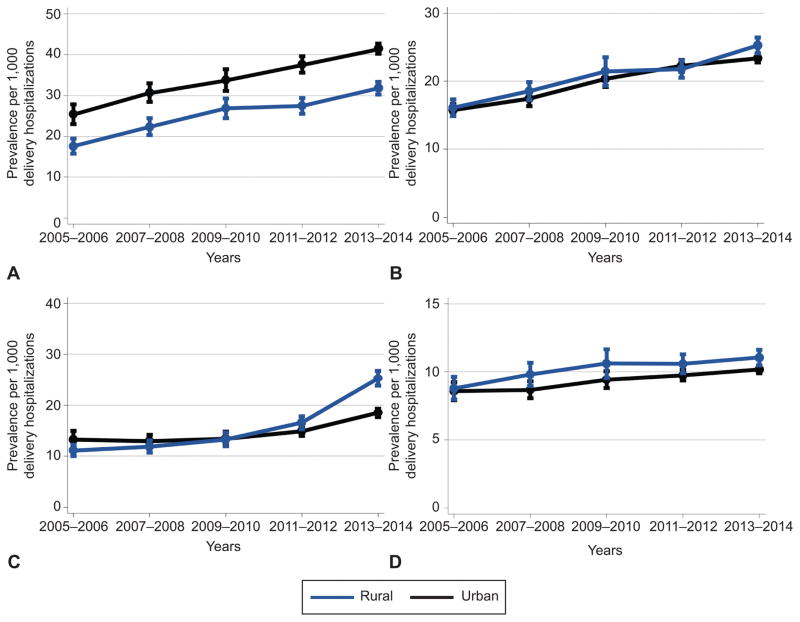
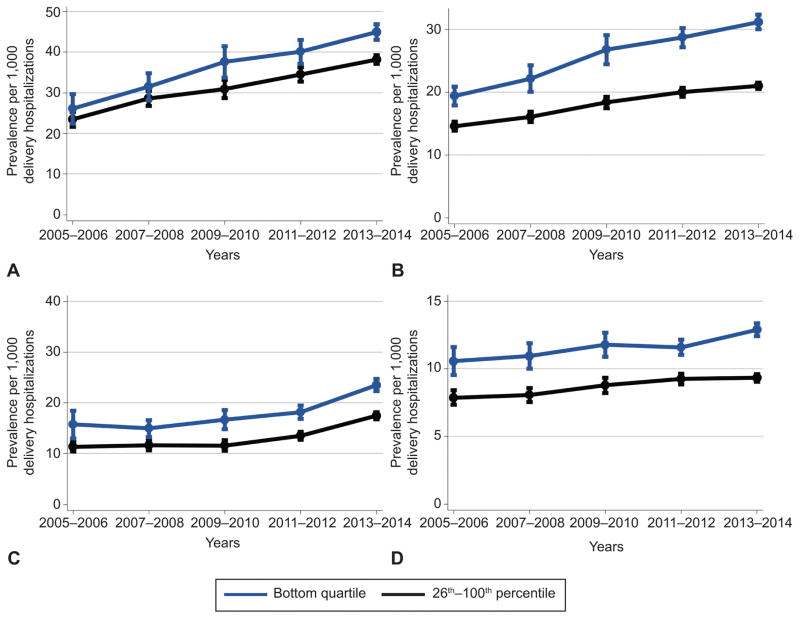
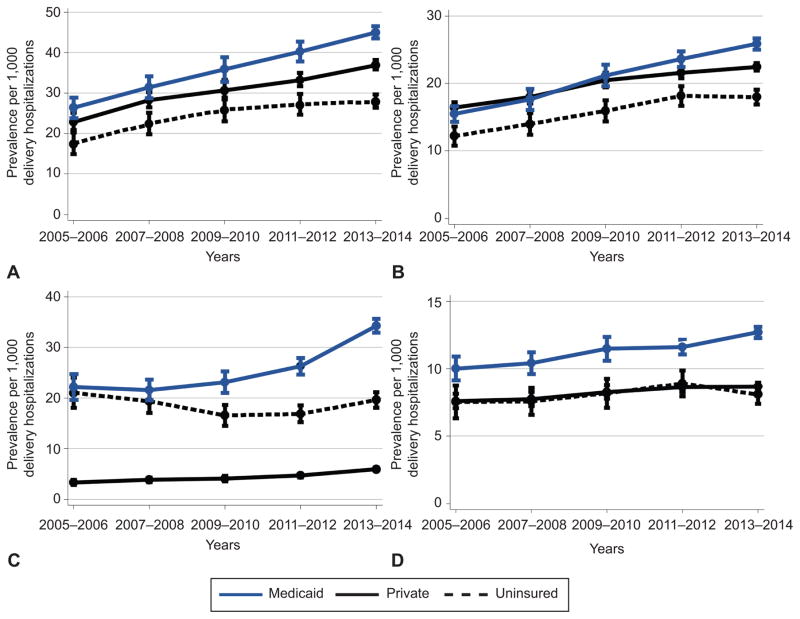
In stratifying the four most prevalent conditions by rural vs. urban residence, increases in prevalence were identified for each condition across both groups between 2005–06 and 2013–14 (Figure 1). Similarly, the prevalence of each condition increased over the study period across both income subgroups (Figure 2) and both the publicly and privately insured populations (Figure 3).
Figure 1.
Adjusted trends in asthma (A), chronic hypertension (B), substance use disorders (C), and preexisting diabetes mellitus (D) per 1,000 delivery hospitalizations by rural compared with urban residence. Error bars indicate 95% confidence interval. Adjusted for age, payer, and income.
Figure 2.
Adjusted trends in asthma (A), chronic hypertension (B), substance use disorders (C), and preexisting diabetes mellitus (D) per 1,000 delivery hospitalizations by national income percentile for zip code of residence. Error bars indicate 95% confidence interval. Adjusted for age, payer, and rural compared with urban residence.
Figure 3.
Adjusted trends in asthma (A), chronic hypertension (B), substance use disorders (C), and pre-existing diabetes mellitus (D) per 1,000 delivery hospitalizations by primary payer. Error bars indicate 95% confidence interval. Adjusted for age, income, and rural compared with urban residence.
By 2013–14, substance use disorders were identified at a higher rate among rural women, and all four conditions were identified at higher rates among women in the lowest income communities and those with deliveries funded by Medicaid. In many cases, this was driven by larger increases in prevalence among rural, low income, and Medicaid populations than among peers in comparison groups. For instance, the prevalence of substance use disorders in 2005–06 was comparable across rural and urban populations, but the increase in substance use disorders over the study period was larger among rural women (difference-in-differences (DID): 9.0 (95% CI 6.7–11.3) per 1,000 delivery hospitalizations)—resulting in a higher prevalence among rural women by 2013–14 (Table 4). Larger increases in asthma (DID: 4.2, 95% CI 0.86–7.5) and chronic hypertension (5.4, 95% CI 3.7–7.1; both per 1,000 delivery hospitalizations) were identified among women from communities with median incomes in the bottom national income quartile compared to those from wealthier communities (Table 5). Larger increases in the prevalence of all four conditions were identified among the Medicaid populations compared to their privately insured counterparts: asthma (DID: 4.6, 95% CI 2.3–6.9), chronic hypertension (4.4, 95% CI 3.1–5.7), substance use disorders (9.4, 95% CI 6.7–12.2) and pre-existing diabetes (1.6, 95% CI 0.80–2.4; all per 1,000 delivery hospitalizations) (Table 6).
Table 4.
Adjusted Trends in Asthma, Chronic Hypertension, Substance Use Disorders, and Pre-existing Diabetes Mellitus per 1,000 Delivery Hospitalizations by Rural Compared with Urban Residence (95% CI)*
| Condition | 2005–2006 | 2013–2014 | Difference | 2005–2006 | 2013–2014 | Difference | Difference-in-differences |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Rural Residence | Urban Residence | ||||||
|
|
|
||||||
| Asthma | 17.5 (15.7–19.4) | 31.8 (30.2–33.3) | 14.2 (11.9–16.6) | 25.4 (23.0–27.8) | 41.5 (40.2–42.7) | 16.1 (13.4–18.8) | −1.8 (−5.1–1.5) |
| Chronic hypertension | 16.1 (14.9–17.4) | 25.3 (24.1–26.4) | 9.2 (7.5–10.9) | 15.8 (14.9–16.6) | 23.4 (22.8–23.9) | 7.6 (6.5–8.6) | 1.6 (−0.070–3.3) |
| Substance use disorders | 11.1 (10.0–12.2) | 25.3 (23.9–26.7) | 14.2 (12.4–15.9) | 13.3 (11.6–15.0) | 18.5 (17.7–19.3) | 5.2 (3.3–7.0) | 9.0 (6.7–11.3) |
| Pre-existing diabetes | 8.8 (8.0–9.6) | 11.0 (10.5–11.6) | 2.3 (1.2–3.3) | 8.6 (7.9–9.2) | 10.2 (9.9–10.5) | 1.6 (0.89–2.3) | 0.65 (−0.39–1.7) |
Adjusted for age, payer, and income.
Table 5.
Adjusted Trends in Asthma, Chronic Hypertension, Substance Use Disorders, and Pre-existing Diabetes Mellitus per 1,000 Delivery Hospitalizations by National Income Percentile for Zip Code of Residence (95% CI)*
| Condition | 2005–2006 | 2013–2014 | Difference | 2005–2006 | 2013–2014 | Difference | Difference-in-differences |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Income: Bottom quartile† | Income: 26th–100th Percentile* | ||||||
|
|
|
||||||
| Asthma | 26.1 (22.4–29.7) | 45.0 (43.0–46.9) | 18.9 (14.9–22.9) | 23.2 (21.6–25.3) | 38.2 (37.1–39.2) | 14.7 (12.6–16.9) | 4.2 (0.86–7.5) |
| Chronic hypertension | 19.4 (17.9–20.9) | 31.2 (30.0–32.4) | 11.8 (9.9–13.7) | 14.6 13.9–15.4) | 21.0 (20.5–21.5) | 6.4 (5.5–7.3) | 5.4 (3.7–7.1) |
| Substance use disorders | 15.7 (13.0–18.5) | 23.5 (22.3–24.7) | 7.8 (4.8–10.8) | 11.4 (10.4–12.3) | 17.4 (16.7–18.2) | 6.1 (4.9–7.2) | 1.7 (−0.81–4.2) |
| Pre-existing diabetes | 10.6 (9.5–11.6) | 12.9 (12.4–13.4) | 2.3 (1.2–3.5) | 7.9 (7.3–8.4) | 9.3 (9.1–9.6) | 1.5 (0.85–2.1) | 0.86 (−0.065–1.8) |
Adjusted for age, payer, and rural compared with urban residence.
Represents median national income percentile for patient’s ZIP Code
Table 6.
Adjusted Trends in Asthma, Chronic Hypertension, Substance Use Disorders, and Pre-existing Diabetes Mellitus per 1,000 Delivery Hospitalizations by Primary Payer (95% CI)*
| Condition | 2005–2006 | 2013–2014 | Difference | 2005–2006 | 2013–2014 | Difference | Difference-in-differences |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Medicaid | Private Payer | ||||||
|
|
|
||||||
| Asthma | 26.4 (23.8–28.9) | 44.9 (43.5–46.5) | 18.6 (15.6–21.6) | 23.0 (20.9–25.1) | 37.0 (35.9–38.2) | 14.1 (11.7–16.5) | 4.6 (2.3–6.9) |
| Chronic hypertension | 15.5 (14.3–16.6) | 25.9 (25.0–26.7) | 10.4 (8.9–11.8) | 16.4 (15.6–17.2) | 22.5 (21.9–23.0) | 6.0 (5.1–7.0) | 4.4 (3.1–5.7) |
| Substance use disorders | 22.2 (19.7–24.7) | 34.3 (32.9–35.6) | 12.1 (9.1–15.0) | 3.3 (2.8–3.9) | 6.0 (5.6–6.3) | 2.6 (2.0–3.2) | 9.4 (6.7–12.2) |
| Pre-existing diabetes | 10.0 (9.1–10.9) | 12.7 (12.3–13.1) | 2.7 (1.7–3.7) | 7.6 (7.1–8.2) | 8.7 (8.4–8.9) | 1.1 (0.45–1.7) | 1.6 (0.80–2.4) |
Adjusted for age, income, and rural compared with urban residence.
DISCUSSION
In the United States, identification of at least one chronic condition occurred in nearly 10% of all delivery hospitalizations by 2013–14—a relative increase of 40% since 2005–06. Between 2005–06 and 2013–14, the prevalence of asthma, chronic hypertension, substance use disorders, and pre-existing diabetes mellitus increased across all segments of the childbearing population. Increasing disparities were identified across all socio-economic categories analyzed in this study. These findings provide the most recent national estimates of the prevalence of chronic conditions among childbearing women and add important, new knowledge about the distribution of chronic conditions across key socio-economic predictors of obstetric outcomes.
A particularly striking finding is the substantial increase in substance use disorders among childbearing women, particularly among women from rural communities. These findings are consistent with recent reports of rising neonatal abstinence syndrome incidence,7 including disproportionate increases among neonates residing in the rural United States.16 While substance use screening is recommended for all women during prenatal care,17 effective provision of this service has been complicated by a recent surge in legislation penalizing pregnant women for disclosing substance use. Punitive legislation has disproportionately impacted women in rural states,18 where additional barriers to treatment may already exist, including a scarcity of addiction providers willing to treat pregnant women.19 Our findings support the need for policy- and practice-level interventions to facilitate treatment of substance use disorders among childbearing women, particularly among women residing in rural America.
Increasing economic disparities in health were also identified in this study. Prior work has described higher rates of risk factors for chronic conditions among low-income pregnant women, including lack of health insurance prior to pregnancy, and higher rates of smoking, obesity, and mental health disorders.20 Researchers have also suggested that economic and social factors associated with living in poverty—such as food insecurity, fear of crime, and discrimination—can also adversely affect a woman’s long-term health, including development of chronic conditions and poor birth outcomes.21 The widening economic disparities in health status identified in this study suggest it is increasingly important for providers to understand the socio-economic contexts in which childbearing women are at increasing risk for development of chronic conditions.
Our analyses also reveal higher prevalence and larger increases in the prevalence of chronic conditions among women receiving Medicaid during pregnancy. This is important because childbirth is financed differently from all other healthcare in the United States. Approximately half of all births in the United States are funded by Medicaid.22 High insurance coverage rates at delivery, as found in this study, mask the high rates of the often low-income women who are uninsured before or after their pregnancies, as categorical Medicaid coverage ends 60 days postpartum.23 Futhermore, insurance coverage for pregnancy care and delivery does not necessarily mean that benefits include chronic disease management. For instance, variation exists in insurance coverage of evidence-based medication-assisted-treatment for substance use disorders.24 A key priority for maternal health researchers is to continue to examine the cost-benefit of expanding access to evidence-based care, particularly among women with chronic conditions, which may sway policy decisions for insurance benefits design and eligibility.
There are two other notable findings that deserve further discussion. First, the prevalence of chronic heart conditions appears to have decreased over the study period. Because our study sought to focus on pre-existing rather than pregnancy-related conditions, we kept with similar recent analyses in opting opted to exclude patients with cardiomyopathy from our definition of chronic heart disease.3,4 Peripartum cardiomyopathy became a new ICD-9-CM code in 2003, and uptake of this code likely increased overtime potentially drawing from other categories of heart disease. Second, the uninsured or self-pay population comprised approximately 6% of our sample and may partially reflect hospital births occurring among foreign born women in the United States. Lower levels of previous contact with the healthcare system and the healthy immigrant effect may explain why chronic condition prevalence is lower among the uninsured or self-pay population compared to Medicaid beneficiaries. Further understanding the demographic composition and health needs among this population is an important area for future work.
Our findings should be interpreted in light of the limitations of our data source and study design. First, it is possible that some women underwent more than one delivery in the study period and, as such, each discharge record may not reflect a unique woman. Second, claims that do not generate a specific payment, such as ICD-9-CM codes for chronic conditions, may be associated with low sensitivity. As a result, our point estimates are likely to be conservative. It is also possible increases reflect increasingly aggressive coding practices over time; however, increases in the prevalence of one and multiple chronic conditions among reproductive aged women have also been identified in nationally available survey datasets,25,26 lending support to our findings. Lastly, we were unable to account for race or ethnicity and obesity, two important predictors of obstetric outcomes, because a number of hospitals and HCUP partners do not report race or ethnicity13 and the low sensitivity for detecting obesity in administrative data.27
From 2005–06 through 2013–14, the prevalence of chronic conditions increased among the childbearing population. Increasing disparities were identified over time, with the burden of these conditions in many cases disproportionately and progressively falling on women in rural or low-income communities and those with deliveries funded by Medicaid. These findings should inform evidence-based interventions to reduce maternal morbidity and mortality and improve maternal health.
Acknowledgments
Supported by the National Clinician Scholars Program. Michele Heisler is supported by National Institutes of Health grant P30 DK092926.
Footnotes
Financial Disclosure
Vanessa K. Dalton is an expert-witness for Bayer. The other authors did not report any potential conflicts of interest.
Each author has indicated that he or she has met the journal’s requirements for authorship.
Presented at the Congress on Women’s Health, Washington, DC, April 28–30, 2017; the American College of Obstetricians and Gynecologists Annual Clinical and Scientific Meeting, San Diego, CA, May 6–9, 2017; and the AcademyHealth Annual Research Meeting, New Orleans, LA, June 25–27, 2017.
References
- 1.MacDorman MF, Declercq E, Cabral H, Morton C. Recent Increases in the U.S. Maternal Mortality Rate: Disentangling Trends From Measurement Issues. Obstet Gynecol. 2016;128:447–55. doi: 10.1097/AOG.0000000000001556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pregnancy Mortality Surveillance System: Trends in Pregnancy-Related Deaths. Division of Reproductive Health, Centers for Disease Control; Available at: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html. Retrieved February 7, 2017. [Google Scholar]
- 3.Mhyre JM, Bateman BT, Leffert LR. Influence of patient comorbidities on the risk of near-miss maternal morbidity or mortality. Anesthesiology. 2011;115:963–72. doi: 10.1097/ALN.0b013e318233042d. [DOI] [PubMed] [Google Scholar]
- 4.Creanga AA, Bateman BT, Kuklina EV, Callaghan WM. Racial and ethnic disparities in severe maternal morbidity: a multistate analysis, 2008–2010. Am J Obstet Gynecol. 2014;210:435e1–8. doi: 10.1016/j.ajog.2013.11.039. [DOI] [PubMed] [Google Scholar]
- 5.Kuklina EV, Callaghan WM. Chronic heart disease and severe obstetric morbidity among hospitalisations for pregnancy in the USA: 1995–2006. BJOG. 2011;118:345–52. doi: 10.1111/j.1471-0528.2010.02743.x. [DOI] [PubMed] [Google Scholar]
- 6.Bateman BT, Bansil P, Hernandez-Diaz S, Mhyre JM, Callaghan WM, Kuklina EV. Prevalence, trends, and outcomes of chronic hypertension: a nationwide sample of delivery admissions. Am J Obstet Gynecol. 2012;206:134e1–8. doi: 10.1016/j.ajog.2011.10.878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000–2009. JAMA. 2012;307:1934–40. doi: 10.1001/jama.2012.3951. [DOI] [PubMed] [Google Scholar]
- 8.Correa A, Bardenheier B, Elixhauser A, Geiss LS, Gregg E. Trends in prevalence of diabetes among delivery hospitalizations, United States, 1993–2009. Matern Child Health J. 2015;19:635–42. doi: 10.1007/s10995-014-1553-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ewing AC, Datwani HM, Flowers LM, Ellington SR, Jamieson DJ, Kourtis AP. Trends in hospitalizations of pregnant HIV-infected women in the United States: 2004 through 2011. Am J Obstet Gynecol. 2016;215(4):499e1–8. doi: 10.1016/j.ajog.2016.05.048. [DOI] [PubMed] [Google Scholar]
- 10.Ellington SR, Flowers L, Legardy-Williams JK, Jamieson DJ, Kourtis AP. Recent trends in hepatic diseases during pregnancy in the United States, 2002–2010. Am J Obstet Gynecol. 2015;212:524e1–e7. doi: 10.1016/j.ajog.2014.10.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lisonkova S, Haslam MD, Dahlgren L, Chen I, Synnes AR, Lim KI. Maternal morbidity and perinatal outcomes among women in rural versus urban areas. CMAJ. 2016;188:E456–E65. doi: 10.1503/cmaj.151382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindquist A, Noor N, Sullivan E, Knight M. The impact of socioeconomic position on severe maternal morbidity outcomes among women in Australia: a national case–control study. BJOG. 2015;122:1601–9. doi: 10.1111/1471-0528.13058. [DOI] [PubMed] [Google Scholar]
- 13.Overview of the National (Nationwide) Inpatient Sample (NIS) Healthcare Cost and Utilization Project (HCUP); Available at: https://www.hcup-us.ahrq.gov/nisoverview.jsp. Retrieved February 9, 2017. [Google Scholar]
- 14.Kuklina EV, Whiteman MK, Hillis SD, Jamieson DJ, Meikle SF, Posner SF, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008;12:469–77. doi: 10.1007/s10995-007-0256-6. [DOI] [PubMed] [Google Scholar]
- 15.NCHS Urban-Rural Classification Scheme for Counties. National Center for Health Statistics (NCHS), Centers for Disease Control; Available at: https://www.cdc.gov/nchs/data_access/urban_rural.htm. Retrieved February 9, 2017. [Google Scholar]
- 16.Villapiano NG, Winkelman TA, Kozhimannil KB, Davis MM, Patrick SW. Rural and urban differences in neonatal abstinence syndrome and maternal opioid use, 2004 to 2013. JAMA Pediatr. 2016;171(2):194–196. doi: 10.1001/jamapediatrics.2016.3750. [DOI] [PubMed] [Google Scholar]
- 17.Opioid use and opioid use disorder in pregnancy. Committee Opinion No. 711. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2017;130:e81–94. doi: 10.1097/AOG.0000000000002235. [DOI] [PubMed] [Google Scholar]
- 18.Jarlenski M, Hogan C, Bogen DL, Chang JC, Bodnar LM, Van Nostrand E. Characterization of US State Laws Requiring Health Care Provider Reporting of Perinatal Substance Use. Womens Health Issues. 2017;27(3):264–270. doi: 10.1016/j.whi.2016.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lander LR, Marshalek P, Yitayew M, Ford D, Sullivan CR, Gurka KK. Rural healthcare disparities: challenges and solutions for the pregnant opioid-dependent population. W V Med J. 2013;109:22–8. [PubMed] [Google Scholar]
- 20.Bombard JM, Dietz PM, Galavotti C, England LJ, Tong VT, Hayes DK, et al. Chronic diseases and related risk factors among low-income mothers. Matern Child Health J. 2012;16:60–71. doi: 10.1007/s10995-010-0717-1. [DOI] [PubMed] [Google Scholar]
- 21.Braveman P. What is health equity: and how does a life-course approach take us further toward it? Matern Child Health J. 2014;18:366–72. doi: 10.1007/s10995-013-1226-9. [DOI] [PubMed] [Google Scholar]
- 22.Markus AR, Andres E, West KD, Garro N, Pellegrini C. Medicaid covered births, 2008 through 2010, in the context of the implementation of health reform. Womens Health Issues. 2013;23:e273–e80. doi: 10.1016/j.whi.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 23.Daw JR, Hatfield LA, Swartz K, Sommers BD. Women In The United States Experience High Rates Of Coverage ‘Churn’ In Months Before And After Childbirth. Health Aff (Millwood) 2017;36:598–606. doi: 10.1377/hlthaff.2016.1241. [DOI] [PubMed] [Google Scholar]
- 24.Substance Abuse and Mental Health Services Administration. Medication-Assisted Treatment: Medication and Counseling Treatment, Insurance and Payments. Available at: https://www.samhsa.gov/medication-assisted-treatment/treatment/insurance-payments. Retrieved July 17, 2017.
- 25.Hayes DK, Fan AZ, Smith RA, Bombard JM. Trends in selected chronic conditions and behavioral risk factors among women of reproductive age, behavioral risk factor surveillance system, 2001–2009. Prev Chronic Dis. 2011;8(6):A120. [PMC free article] [PubMed] [Google Scholar]
- 26.Ward BW, Schiller JS. Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Prev Chronic Dis. 2013;25(10):E65. doi: 10.5888/pcd10.120203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martin B-J, Chen G, Graham M, Quan H. Coding of obesity in administrative hospital discharge abstract data: accuracy and impact for future research studies. BMC Health Serv Res. 2014;14:70. doi: 10.1186/1472-6963-14-70. [DOI] [PMC free article] [PubMed] [Google Scholar]