Abstract
Background
Major depressive disorder and generalized anxiety disorder are among the most commonly diagnosed mental illnesses in Canada; both are associated with a high societal and economic burden. Treatment for major depressive disorder and generalized anxiety disorder consists of pharmacological and psychological interventions. Three commonly used psychological interventions are cognitive behavioural therapy (CBT), interpersonal therapy, and supportive therapy. The objectives of this report were to assess the effectiveness and safety of these types of therapy for the treatment of adults with major depressive disorder and/or generalized anxiety disorder, to assess the cost-effectiveness of structured psychotherapy (CBT or interpersonal therapy), to calculate the budget impact of publicly funding structured psychotherapy, and to gain a greater understanding of the experiences of people with major depressive disorder and/or generalized anxiety disorder.
Methods
We performed a literature search on October 27, 2016, for systematic reviews that compared CBT, interpersonal therapy, or supportive therapy with usual care, waitlist control, or pharmacotherapy in adult outpatients with major depressive disorder and/or generalized anxiety disorder. We developed an individual-level state-transition probabilistic model for a cohort of adult outpatients aged 18 to 75 years with a primary diagnosis of major depressive disorder to determine the cost-effectiveness of individual or group CBT (as a representative form of structured psychotherapy) versus usual care. We also estimated the 5-year budget impact of publicly funding structured psychotherapy in Ontario. Finally, we interviewed people with major depressive disorder and/or generalized anxiety disorder to better understand the impact of their condition on their daily lives and their experience with different treatment options, including psychotherapy.
Results
Interpersonal therapy compared with usual care reduced posttreatment major depressive disorder scores (standardized mean difference [SMD]: 0.24, 95% confidence interval [CI]: −0.47 to −0.02) and reduced relapse/recurrence in patients with major depressive disorder (relative risk [RR]: 0.41, 95% CI: 0.27–0.63). Supportive therapy compared with usual care improved major depressive disorder scores (SMD: 0.58, 95% CI: 0.45–0.72) and increased posttreatment recovery (odds ratio [OR]: 2.71, 95% CI: 1.19–6.16) in patients with major depressive disorder. CBT compared with usual care increased response (OR: 1.58, 95% CI: 1.11–2.26) and recovery (OR: 3.42, 95% CI: 1.98–5.93) in patients with major depressive disorder and decreased relapse/recurrence (RR: 0.68, 95% CI: 0.65–0.87]). For patients with generalized anxiety disorder, CBT improved symptoms posttreatment (SMD: 0.80, 95% CI: 0.67–0.93), improved clinical response posttreatment (RR: 0.64, 95% CI: 0.55–0.74), and improved quality-of-life scores (SMD: 0.44, 95% CI: 0.06–0.82). There was a significant difference in posttreatment recovery (OR: 1.98, 95% CI: 1.11–3.54) and mean major depressive disorder symptom scores (weighted mean difference: −3.07, 95% CI: −4.69 to −1.45) for patients who received individual versus group CBT. Details about the providers of psychotherapy were rarely reported in the systematic reviews we examined.
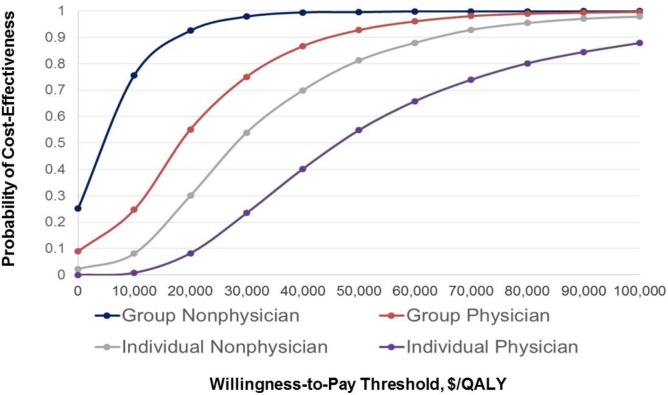
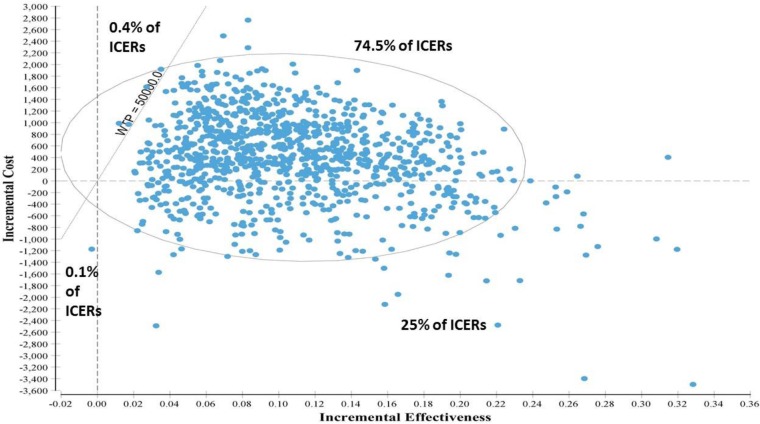
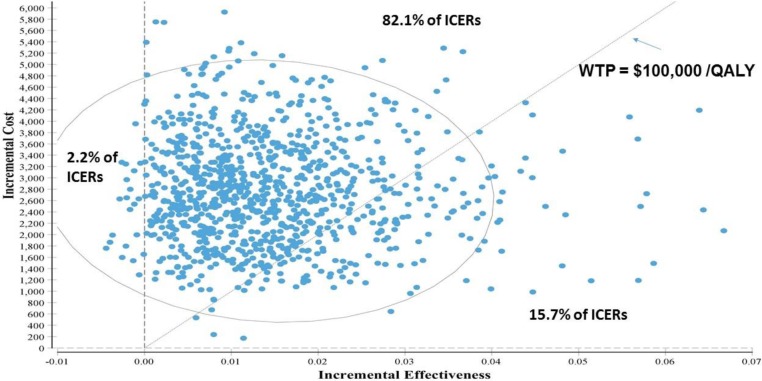
In the base case probabilistic cost–utility analysis, compared with usual care, both group and individual CBT were associated with increased survival: 0.11 quality-adjusted life-years (QALYs) (95% credible interval [CrI]: 0.03–0.22) and 0.12 QALYs (95% CrI: 0.03–0.25), respectively.
Group CBT provided by nonphysicians was associated with the smallest increase in discounted costs: $401 (95% CrI: $1,177 to 1,665). Group CBT provided by physicians, individual CBT provided by nonphysicians, and individual CBT provided by physicians were associated with the incremental costs of $1,805 (95% CrI: 65–3,516), $3,168 (95% CrI: 889–5,624), and $5,311 (95% CrI: 2,539–8,938), respectively. The corresponding incremental cost-effectiveness ratio (ICER) was lowest for group CBT provided by nonphysicians ($3,715/QALY gained) and highest for individual CBT provided by physicians ($43,443/QALY gained). In the analysis that ranked best strategies, individual CBT versus group CBT provided by nonphysicians yielded an ICER of $192,618 per QALY. The probability of group CBT provided by nonphysicians being cost-effective versus usual care was greater than 95% for all willingness-to-pay thresholds over $20,000 per QALY and was around 88% for individual CBT provided by physicians at a threshold of $100,000 per QALY.
We estimated that adding structured psychotherapy to usual care over the next 5 years would result in a net budget impact of $68 million to $529 million, depending on a range of factors. We also estimated that to provide structured psychotherapy to all adults with major depressive disorder (alone or combined with generalized anxiety disorder) in Ontario by 2021, an estimated 500 therapists would be needed to provide group therapy, and 2,934 therapists would be needed to provide individual therapy.
People with major depressive disorder and/or generalized anxiety disorder with whom we spoke reported finding psychotherapy effective, but they also reported experiencing a large number of barriers that prevented them from finding effective psychotherapy in a timely manner. Participants reported wanting more freedom to choose the type of psychotherapy they received.
Conclusions
Compared with usual care, treatment with CBT, interpersonal therapy, or supportive therapy significantly reduces depression symptoms posttreatment. CBT significantly reduces anxiety symptoms posttreatment in patients with generalized anxiety disorder.
Compared with usual care, treatment with structured psychotherapy (CBT or interpersonal therapy) represents good value for money for adults with major depressive disorder and/or generalized anxiety disorder. The most affordable option is group structured psychotherapy provided by nonphysicians, with the selective use of individual structured psychotherapy provided by nonphysicians or physicians for those who would benefit most from it (i.e., patients who are not engaging well with or adhering to group therapy).
OBJECTIVE
This health technology assessment looked at the effectiveness, safety, cost-effectiveness, budget impact, and patient experiences of cognitive behavioural therapy (CBT), interpersonal therapy, and supportive therapy for the treatment of major depressive disorder and generalized anxiety disorder to determine whether these therapies should be publicly funded.
BACKGROUND
Health Condition
Major depressive disorder is the second largest health care problem worldwide in terms of illness-induced disability.1 The essential feature of major depressive disorder is the occurrence of one or more major depressive episodes. Major depressive episodes are defined as periods lasting at least 2 weeks characterized by depressed mood, most of the day, nearly every day, and/or markedly diminished interest or pleasure in all, or almost all, activities.2 To receive a diagnosis of major depressive disorder, within the same 2-week period a person must experience 5 or more symptoms from the criteria for a major depressive episode as described in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).3
Generalized anxiety disorder is a chronic (constantly recurring) anxiety disorder characterized by persistent, excessive, and difficult-to-control worry that may be accompanied by several psychic (mental) symptoms and somatic (bodily) symptoms.4 It is associated with high rates of comorbidity (having more than one condition at a time), and 68% of people with generalized anxiety disorder report having at least one other psychiatric illness (usually depression, another anxiety disorder, or a substance use disorder).4
The current classification of depressive and anxiety disorders is based on the DSM-5 or the tenth revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) Classification of Mental and Behavioural Disorders.5
Clinical Need and Target Population
The lifetime prevalence of major depressive disorder in Canada is 10.8%; annual and 1-month prevalence estimates are 4.0% and 1.3%, respectively.2 Depression affects occupational functioning both through absenteeism and through loss of productivity while attending work when unwell.2 While occupational impairment receives much attention, depression also negatively affect people's ability to perform personal activities, such as parenting and housekeeping. A study in the United States found that people with major depressive disorder were able to perform better at work than in their personal activities.6
Treatment for acute major depressive disorder (during the first 3 months after diagnosis) often consists of pharmacological interventions (medications including selective serotonin reuptake inhibitors, serotonin–norepinephrine reuptake inhibitors, and tricyclic antidepressants) and psychological interventions (talk therapies). The prescribing of antidepressant medications has increased over the last 20 years, mainly owing to the development of a new type of antidepressant medication called selective serotonin reuptake inhibitors, as well as other newer agents.7 While antidepressants continue to be the mainstay of treatment for major depressive disorder, adherence rates remain low in part because of patients' concerns about side effects and possible dependency. In addition, surveys have demonstrated patients' preference for psychological interventions over treatment with antidepressants.7 Therefore, psychological therapies can provide an alternative or additional intervention for major depressive disorder.7
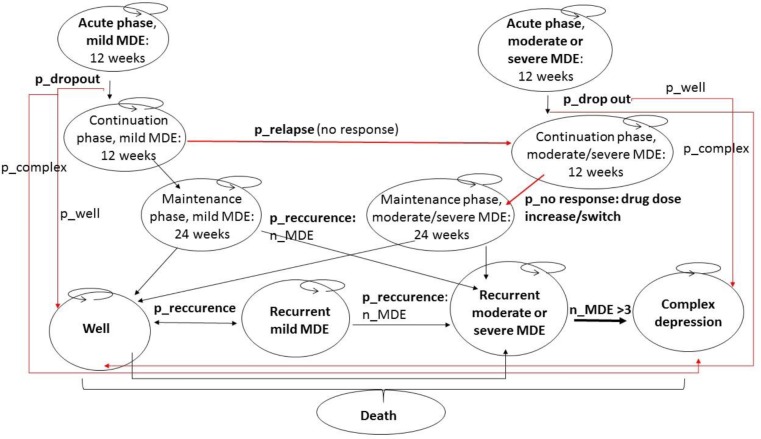
Major depressive disorder is both chronic (lasting 3 months or more) and episodic (consisting of separate episodes) in nature. It consists of initial phases (i.e., the acute and continuation phases, each lasting approximately 3 months) and a maintenance phase (lasting approximately 6 to 24 months, with an average 9 to 12 months).2,8–10 The aim of treatment in the acute and continuation phases is the remission (reduction or elimination) of symptoms and the restoration of psychosocial functioning (a return to the level of psychological and social functioning experienced before the onset of major depressive disorder).2 The aim of treatment in the maintenance phase is to prevent symptoms from recurring.2
In Canada, the 1-year prevalence of generalized anxiety disorder in the general population is about 1% to 3%, and the lifetime prevalence is about 6%.4 Patients with generalized anxiety disorder may experience multiple episodes of the disease over their lifetime, and these episodes may be associated with a multitude of disabilities affecting work, education, and social interactions.4
The primary treatment for generalized anxiety disorder consists of medications (e.g., selective serotonin reuptake inhibitors, serotonin–norepinephrine reuptake inhibitors, tricyclic antidepressants, anxiolytics, and other agents).4 Antidepressants are the first-line treatment (the first type of treatment tried) and have the additional benefit of treating ruminative worry (persistent negative thoughts) and any coexisting depressive symptoms.4 Benzodiazepines, which have a sedative and anti-anxiety effect, were used extensively in the past; however, owing to the potential for developing tolerance and dependence with prolonged use, most guidelines now recommend that for generalized anxiety disorder, benzodiazepines be prescribed for no longer than 2 to 4 weeks.4
As a result of patients' concerns about side effects, psychotherapy is a treatment option that may be considered either as an alternative or additional intervention for generalized anxiety disorder.11
Health Intervention Under Review
Three common types of psychotherapy for the treatment of major depressive disorder and generalized anxiety disorder are cognitive behavioural therapy (CBT), interpersonal therapy, and supportive therapy.12
The Royal Australian and New Zealand College of Psychiatrists defines structured psychotherapy as “the treatment of mental or emotional illness by using defined (often manualized) psychological techniques, pre-planned with clear goals and employed within a specific timeframe.”13 According to the College, patients must be seen by their treatment provider, either individually or in a small group, on at least a monthly basis.13 CBT and interpersonal therapy are considered structured psychotherapies, but supportive therapy is not.13
Cognitive behavioural therapy focuses on helping patients become aware of how certain negative automatic thoughts, attitudes, expectations, and beliefs contribute to feelings of sadness and anxiety.12 Patients learn how these thinking patterns, which may have developed in the past to deal with difficult or painful experiences, can be identified and changed to reduce unhappiness.12
Interpersonal therapy focuses on identifying and resolving problems in establishing and maintaining satisfying relationships.12 Such problems may include dealing with loss, life changes, conflicts, and increasing ease in social situations.12
Supportive therapy (also called nondirective supportive therapy) is typically an unstructured therapy that relies on the basic interpersonal skills of the therapist, such as reflection, empathic listening, and encouragement. It has been defined as a psychological treatment in which therapists do not engage in any therapeutic strategy other than active listening and offering support, focusing on patients' problems and concerns.14 It focuses more on current problems rather than long-term difficulties.12 The overall goal is to reduce patients' discomfort level and help them cope with their current circumstances.12,14
Ontario Context
In Ontario, the delivery of psychotherapy from a psychiatrist or other physician trained in psychotherapy is publicly funded. Services provided by other regulated (i.e., registered), trained health care professionals (e.g., nurses, occupational therapists, psychologists, psychotherapists, and social workers) may be free to patients if the services are offered in government-funded hospitals, clinics, or agencies.12 However, many free services have long wait lists. Other free services include employee assistance programs, community clinics, support groups, distress lines, and drop-in centres.
Therapy provided by registered psychologists or psychotherapists in private practice is not publicly funded. However, the fees may be covered by private insurance or workplace coverage, although such private or workplace plans may not cover the full amount or may provide coverage for only certain types of therapist.12
Status in the United States
In the United States, the Medicare program covers outpatient mental health services and visits with the following professionals15:
Psychiatrist or other physician
Clinical psychologist
Clinical social worker
Clinical nurse specialist
Nurse practitioner
Physician assistant
Medicare covers counselling or therapy only when delivered by a health care professional who accepts assignment, which is an agreement by a health care professional to (a) be paid directly by Medicare; (b) accept the payment amount that Medicare approves for the service; and (c) not bill the patient for more than the fee of the Medicare deductible and coinsurance.15
There are caveats around the specific amount a patient is required to pay for treatment depending on several factors, such as the following15:
Other insurance the patient may have
How much the health care professional charges
Whether the provider accepts assignment
The type of facility in which treatment is provided
The location where the patient receives treatment
Health care professionals may recommend a patient receive treatment more often than what Medicare will cover.15 Or, they may recommend services that Medicare does not cover. In such cases, the patient may have to pay some or all of the treatment costs.15
CLINICAL EVIDENCE
Research Questions
What are the effectiveness and safety of cognitive behavioural therapy (CBT), interpersonal therapy, and supportive therapy in improving outcomes for adult patients with major depressive disorder and adult patients with generalized anxiety disorder?
What are the effectiveness and safety of individual versus group therapy?
What are the effectiveness and safety of psychotherapy versus no treatment or waitlist control?
What are the effectiveness and safety of psychotherapy with and without pharmacotherapy versus pharmacotherapy only?
What are the effectiveness and safety of psychotherapy provided by physician versus nonphysician providers?
Methods
Research questions are developed by Health Quality Ontario in consultation with experts, end users, and/or applicants in the topic area. Our methodological approaches align with Health Quality Ontario's Health Technology Assessments Methods and Process Guide.16
Literature Search
We performed a literature search on October 27, 2016, to retrieve studies published from January 1, 2000, until the search date. We used the Ovid interface to search the following databases: Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects (DARE), Embase, Health Technology Assessment, MEDLINE, National Health Service Economic Evaluation Database (NHSEED), and PsycINFO. We used the EBSCOhost interface to search the Cumulative Index to Nursing & Allied Health Literature (CINAHL).
Search strategies were developed by medical librarians using controlled vocabulary (e.g., Medical Subject Headings) and relevant keywords. Methodological filters were used to limit retrieval to systematic reviews, meta-analyses, and health technology assessments. The final search strategy was peer-reviewed using the Peer Review of Electronic Search Strategies (PRESS) checklist.17 Database auto-alerts were created in CINAHL, Embase, MEDLINE, and PsycINFO and monitored for the duration of the health technology assessment review.
We performed targeted grey literature searching of health technology assessment agency websites and PROSPERO systematic review registry. See Appendix 1 for the literature search strategies, including all search terms.
Literature Screening
A single reviewer reviewed the abstracts, and, for those studies meeting the eligibility criteria, we obtained full-text articles. We also examined reference lists for any additional relevant studies not identified through the search.
Inclusion Criteria
English-language full-text publications
Studies published between January 1, 2000, and October 27, 2016
Systematic reviews of randomized controlled trials only
Studies on adult outpatients with major depressive disorder or generalized anxiety disorder who received CBT, interpersonal therapy, or supportive therapy
Studies that report a definition or diagnostic criteria for major depressive disorder and/or generalized anxiety disorder (i.e., DSM-3, DSM-4, DSM-5, or ICD-10 criteria or based on other validated diagnostic instruments)
Comparators of usual care, waitlist control, or pharmacotherapy
Exclusion Criteria
Animal and in vitro studies
Studies that are not systematic reviews
Studies on children or adolescents (≤ 18 years of age) or older people (≥ 65 years of age)
Studies that focus on postpartum depression, bipolar disorder, dysthymia, seasonal affective disorder, psychotic disorders, or drug or alcohol dependence-related depression
Studies that examine nontraditional CBT (e.g., mindfulness CBT), telephone-based CBT, computer-based CBT, or Internet-based CBT
Studies where relevant data are unable to be extracted (e.g., results for “psychotherapy” are reported without describing the specific type of psychotherapy, or results for “depressive disorders” or “anxiety disorders” are reported without specific breakdowns for major depressive disorder or generalized anxiety disorder, respectively)
Outcomes of Interest
Remission of depression or anxiety symptoms
Prevention of relapse following successful acute treatment
Response to therapy (e.g., ≥ 50% reduction in symptoms from baseline)
Adverse events
Quality of life
Data Extraction
We extracted relevant data on study characteristics; risk-of-bias items; and population, intervention, comparison, outcome, and time (PICOT) criteria using a standardized data form. The form collected information about the following:
Source (i.e., citation information, contact details, and study type)
Methods (i.e., study design)
Outcomes (i.e., outcomes measured, number of participants for each outcome, outcome definition and source of information, unit of measurement, upper and lower limits [for scales], and time points at which outcomes were assessed)
Statistical Analysis
This review reports results only from systematic reviews. We did not perform an analysis of primary studies.
Quality of Evidence
We used A Measurement Tool to Assess Systematic Reviews (AMSTAR) to assess the methodological quality of systematic reviews.18 See Appendix 2 for details of the AMSTAR analysis.
Expert Consultation
In December 2016, we sought expert consultation on the use of CBT, interpersonal therapy, and supportive therapy for the treatment of major depressive disorder and generalized anxiety disorder. Members of the consultation included health care professionals in the specialty areas of psychology, psychiatry, and family medicine. The role of the expert advisors was to help contextualize the evidence and provide advice on the use of CBT, interpersonal therapy, and supportive therapy for the treatment of major depressive disorder and generalized anxiety disorder. However, the statements, conclusions, and views expressed in this report do not necessarily represent the views of the consulted experts.
Results
Literature Search
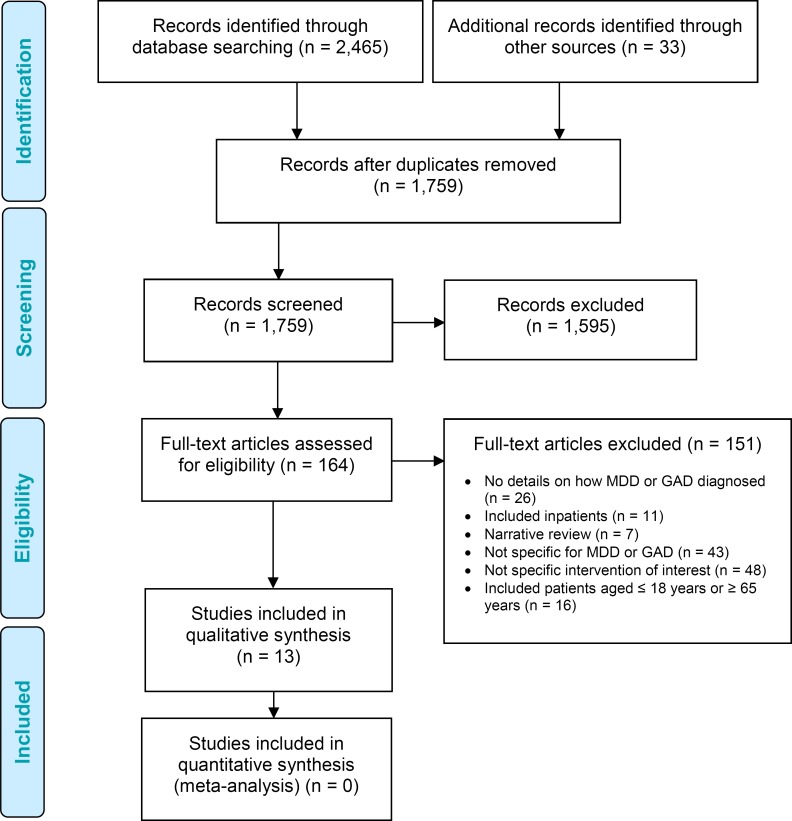
The database and grey literature searches yielded 1,759 citations published between January 1, 2000, and October 27, 2016 (after duplicates removed). We reviewed titles and abstracts to identify potentially relevant articles and obtained the full texts of these articles for further assessment. Thirteen systematic reviews met the inclusion criteria. We hand-searched the reference lists of the included studies, and other sources, to identify any additional relevant studies.
Figure 1 presents the flow diagram for the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) for the clinical evidence review.
Figure 1: PRISMA Flow Diagram—Clinical Evidence Review.
Source: Adapted from Moher et al.19
Abbreviations: GAD, generalized anxiety disorder; MDD, major depressive disorder; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analyses.
Cognitive Behavioural Therapy Compared With Usual Care for Major Depressive Disorder
Depressive Symptoms, Treatment Response, and Remission
Three systematic reviews reported results for symptoms of major depressive disorder after patients received CBT compared with usual care.20–22
In 2016, Cuijpers et al systematically reviewed the effectiveness of CBT for the acute treatment of major depressive disorder compared with control (wait list, usual care, or pill placebo) (63 randomized controlled trials, number of patients not reported).20 Overall, CBT significantly reduced mean major depressive disorder symptom scores for patients who had undergone CBT compared with control (SMD: 0.75, 95% CI: 0.64–0.87]).20
Cuijpers et al reported that 11 of the 63 studies were rated high quality, based on the Cochrane risk-of-bias tool.20 Of note, the authors analyzed for publication bias and estimated that approximately 14% of major depressive disorder studies were missing from publication; thus, the pooled effect size dropped from an SMD of 0.75 to an SMD of 0.65 (95% CI: 0.53–0.78).20
No studies reviewed by Cuijpers et al reported on the providers of CBT.20
Linde et al conducted a meta-analysis to determine the effectiveness of psychotherapy compared with usual care or placebo in primary care patients with major depressive disorder.21 The authors conducted an analysis of 7 randomized controlled trials (N = 518) for face-to-face CBT. The meta-analysis included 5 studies23–27 that were also included in the systematic review by Cuijpers et al.20 The standardized mean difference for posttreatment major depressive disorder symptom scores compared with control was statistically significant, favouring CBT: −0.30 (95% CI: −0.48 to −0.13).
Linde et al also reported a statistically significant pooled estimate for response (defined as a ≥ 50% score reduction on a depression scale) favouring CBT and a statistically nonsignificant pooled estimate for remission (defined as a symptom score below a fixed threshold) for CBT compared with usual care (OR: 1.58, 95% CI: 1.11–2.26, and OR: 1.49, 95% CI: 0.90–2.46, respectively).21
The authors rated the overall quality of the trials in the systematic review as low, based on the Cochrane risk-of-bias criteria.21 The reporting of intervention details for usual care and for co-interventions (e.g., pharmacotherapy) in the groups receiving psychotherapy was often insufficient.21
The providers of treatment in the included studies varied and included counsellors, nurses, psychiatrists, psychologists, psychotherapists, and therapists.21
Churchill et al22 systematically reviewed psychotherapies for the treatment of major depressive disorder and performed an analysis for CBT compared with usual care. Of the 20 studies included in the analysis, 424,25,27,28 were also included in the more recent systematic review by Cuijpers et al.20 Overall, there was a significant difference in posttreatment recovery (12 studies, N = 654; OR: 3.42, 95% CI: 1.98–5.93).22 Posttreatment recovery was defined as patients no longer being deemed to have a clinically meaningful level of depression, as indicated by a score of less than 10 on the Beck Depression Inventory or less than 6 on the Hamilton Depression Rating Scale. The authors also found a significant difference in mean major depressive disorder symptom scores for patients who received CBT versus usual care (20 studies, N = 748; SMD: −1.0, 95% CI: −1.35 to −0.64).22
Churchill et al also reported results for individual versus group CBT.22 Overall, there was a significant difference in posttreatment recovery (6 studies, N = 234; OR: 1.98, 95% CI: 1.11–3.54) and mean major depressive disorder symptom scores (8 studies, N = 283; weighted mean difference [WMD]: −3.07, 95% CI: −4.69 to −1.45]) for patients who received individual versus group CBT.22
The authors rated the overall quality of evidence as low, based on the Cochrane risk-of-bias tool, owing to low scores on internal validity and inadequate reporting of methodology.22
No studies reviewed by Churchill et al reported on the providers of CBT.22
Relapse
Three systematic reviews reported results for relapse of major depressive disorder after patients had received treatment with CBT versus usual care.29–31
Biescheuvel-Leliefeld et al systematically reviewed the effectiveness of psychological interventions compared with usual care or antidepressant drugs in reducing relapse or recurrence rates of patients in remission.29 Usual care was defined as routine clinical management, assessment only, no treatment, or wait list. Relapse and recurrence were defined by the primary study investigators; examples include surpassing a threshold score on a depression scale and demonstrating a change in diagnostic depression status based on clinical assessment. The authors also conducted a subset analysis of 16 randomized controlled trials (N = 529) for CBT.29
CBT significantly reduced the risk of relapse or recurrence compared with usual care (RR: 0.68, 95% CI: 0.65–0.87) but not compared with antidepressant drugs (RR: 0.79, 95% CI: 0.61–1.02).29
The authors rated the overall quality of evidence as low, according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) criteria, owing to varying definitions of remission, recovery, relapse, and recurrence in the primary studies.29
No studies reviewed by Biescheuvel-Leliefeld et al reported on the providers of CBT.29
Clarke et al conducted a meta-analysis to determine the effectiveness of nonpharmacological interventions compared with control (defined as usual care, clinical management, or antidepressant drugs) in people who had recovered from major depressive disorder (defined as being in full or partial remission).30 The authors also conducted a subset analysis of nine randomized controlled trials (N = 853) for CBT. The systematic review included three randomized controlled trials32–34 also included in the meta-analysis by Biescheuvel-Leliefeld et al.29
At 12 and 24 months, the risk of developing a new episode of major depressive disorder was significantly reduced in patients who had received CBT compared with control (RR: 0.75, 95% CI: 0.64–0.89, and RR: 0.72, 95% CI: 0.57–0.91, respectively.30
The authors rated the overall quality of evidence as low, based on the GRADE criteria.30
No studies reviewed by Clarke et al reported on the providers of CBT.30
Guidi et al31 systematically reviewed the effectiveness of CBT compared with usual care or clinical management in the treatment of people with major depressive disorder who had successfully responded to a previous course of treatment with antidepressant drugs. (The difference between usual care and clinical management was not described.) Effectiveness was assessed in terms of relapse or recurrence rates of major depressive disorder. All 13 studies (N = 1,410) reviewed by Guidi et al31 were also included in the reviews by Biescheuvel-Leliefeld et al29 and/or Clarke et al.30 The overall pooled risk ratio for relapse or recurrence for CBT compared with usual care or clinical management was statistically significant, favouring CBT (0.78; 95% CI: 0.67–0.91).
The authors reported that the methodological quality of the studies included in their meta-analysis was high; however, they did not report their method of rating study quality.31
No studies reviewed by Guidi et al reported on the providers of CBT.31
Adverse Events
This outcome was not reported in the systematic reviews.
Quality of Life
This outcome was not reported in the systematic reviews.
Cognitive Behavioural Therapy With and Without Pharmacotherapy Compared With Pharmacotherapy Only for Major Depressive Disorder
Depressive Symptoms, Treatment Response, and Remission
Three systematic reviews reported results for treatment response after patients received CBT and pharmacotherapy compared with pharmacotherapy only for the treatment of major depressive disorder.35–37
Karyotaki et al systematically reviewed the effectiveness (as measured by response rate) of combined pharmacotherapy and psychotherapy compared with psychotherapy only or pharmacotherapy only in both the acute and maintenance treatment of patients with major depressive disorder. The authors also conducted a subset analysis for CBT.35
For acute-phase treatment, there was no significant difference in response rate for combined CBT and pharmacotherapy compared with CBT only at up to 6 months postrandomization (5 comparisons, number of patients not reported; OR: 1.51, 95% CI: 0.79–2.86) and up to 1 year postrandomization (4 comparisons, number of patients not reported; OR: 1.48, 95% CI: 0.59–3.71).35 However, there was a significant difference in response rate when the combination of CBT and pharmacotherapy was compared with pharmacotherapy only at up to 6 months (6 comparisons, number of patients not reported; OR: 3.02, 95% CI: 1.74–5.25) and up to 1 year postrandomization (4 comparisons, number of patients not reported; OR: 3.37, 95% CI: 1.38–8.21).35
For maintenance-phase treatment, no data were available for combined CBT and pharmacotherapy versus CBT only.35 There was a significant difference in response rate when the combination of CBT and pharmacotherapy was compared with pharmacotherapy only at up to 6 months postrandomization (4 comparisons, number of patients not reported; OR: 1.79, 95% CI: 1.19–2.70).35 No data were available for response rates at more than 1 year postrandomization.35
The authors rated the overall quality of evidence as low, based on the Cochrane risk-of-bias tool.35
No studies reviewed by Karyotaki et al reported on the providers of CBT.35
Amick et al meta-analyzed studies to determine the effectiveness (as measured by the rate of response and remission) of second-generation antidepressants (the most commonly prescribed class of antidepressants, including selective serotonin reuptake inhibitors and serotonin– norepinephrine reuptake inhibitors) only versus CBT only and second-generation antidepressants only versus a combination of second-generation antidepressants and CBT for the treatment of major depressive disorder.36 Response was defined as a decrease in depressive severity of equal to or greater than 50%, and remission was defined by the authors of the individual trials.36
For second-generation antidepressants only compared with CBT only, there were no significant differences in remission (3 trials; risk ratio: 0.98, 95% CI: 0.73–1.32), response (5 trials; risk ratio: 0.91, 95% CI: 0.77–1.07), or overall treatment discontinuation (4 trials; risk ratio: 1.00, 95% CI: 0.55–1.81).36
For second-generation antidepressants only compared with a combination of second-generation antidepressants and CBT, the authors found no significant differences for remission (1 trial; risk ratio: 1.06, 95% CI: 0.82–1.38); response (1 trial; risk ratio: 1.03, 95% CI: 0.85–1.26); or overall treatment discontinuation (1 trial; risk ratio: 0.77, 95% CI: 0.37–1.60).36
The authors rated the overall strength of evidence as low, based on methods guidance from the Evidence-Based Practice Centers Program of the Agency for Healthcare Research and Quality.36
The treatment providers in the studies reviewed by Amick et al varied in terms of provider type, training, and experience.36
Cuijpers et al systematically reviewed the effectiveness of acute-phase CBT without any subsequent continuation treatment compared with pharmacotherapy (that was either continued or discontinued) in patients with major depressive disorder.37 The primary outcome was the number of patients who responded to treatment and remained well (defined as treatment response maintained across 6 to 18 months of follow-up).37 Overall, the authors identified 9 studies (N = 506; for CBT, n = 271; for pharmacotherapy, n = 235).37
For acute-phase CBT (without continuation treatment) compared with acute-phase pharmacotherapy with continued pharmacotherapy during follow-up, there was no significant difference in 1-year outcomes (5 studies; OR: 1.62, 95% CI: 0.97–2.72).37
For acute-phase CBT (without continuation treatment) compared with acute-phase pharmacotherapy that was discontinued during follow-up, there was a significant difference in 1-year outcomes, favouring CBT (8 studies; OR: 2.61, 95% CI: 1.58–4.31).37
The authors rated the overall quality of evidence as high, according to the Cochrane risk-of-bias tool.37
No studies reviewed by Cuijpers et al reported on the providers of CBT.37
Relapse
This outcome was not reported in the systematic reviews.
Adverse Events
This outcome was not reported in the systematic reviews.
Quality of Life
This outcome was not reported in the systematic reviews.
Cognitive Behavioural Therapy Compared With Usual Care for Generalized Anxiety Disorder
Anxiety Symptoms, Treatment Response, and Remission
Three systematic reviews reported results for treatment response after patients received CBT compared with usual care for the treatment of generalized anxiety disorder.11,20,38
In 2016, Cuijpers et al systematically reviewed the effectiveness of CBT (as measured by reduction in anxiety symptoms) compared with control (wait list, usual care, or pill placebo) for the acute treatment of patients with anxiety disorders.20 A subset analysis was conducted for generalized anxiety disorder (31 studies, number of patients not reported). Overall, mean generalized anxiety disorder symptom scores were significantly reduced by CBT compared with control (SMD: 0.80, 95% CI: 0.67–0.93).20
The authors rated 9 of the 31 studies as high quality, based on the Cochrane risk-of-bias tool.20 Of note, the authors analyzed for publication bias, and they estimated that about one-quarter of generalized anxiety disorder studies were missing. After adjusting for these missing studies, the effect size dropped from an SMD of 0.80 to an SMD of 0.59 (95% CI: 0.44–0.75). However, this result did not change the statistical significance of the finding.20
No studies reviewed by Cuijpers et al reported on the providers of CBT.20
In 2014, Cuijpers et al meta-analyzed studies to determine the effectiveness of psychotherapies versus control (wait list, usual care, or pill placebo) for people with generalized anxiety disorder.38 The authors also conducted a subset analysis for CBT (28 comparisons, number of patients not reported). We determined that there was overlap between the studies included in this 2014 analysis and those included in the systematic review by Cuijpers et al in 2016 (described above)20; however, the studies within the CBT subset comparison reported in the 2016 systematic review were unique to that publication.38 Overall, there was no significant difference in mean generalized anxiety disorder symptom scores posttreatment for people treated with CBT compared with control (SMD: 0.90, 95% CI: 0.75–1.05).38
The authors rated the overall quality of the studies included in the 2014 systematic review as low, based on the Cochrane risk-of-bias tool.38 The authors commented that the overall quality of the interventions also varied across studies (e.g., not all psychotherapy providers reported using a standard manual, and limited information was provided on treatment components, including those of CBT, and adherence to treatment manuals).38
The authors further stated that the literature on psychotherapy studies for generalized anxiety disorder differs markedly from that for major depressive disorder, in which the same standard treatment manual is used across many studies.38
The authors did not report publication bias for the subset analysis.
No studies reviewed by Cuijpers et al reported on the providers of CBT.38
In 2007, Hunot et al systematically reviewed the effectiveness of CBT compared with usual care or wait list for the treatment of patients with generalized anxiety disorder.11 Primary outcomes included clinical response (8 studies, N = 334) and reduction in generalized anxiety disorder symptoms (12 studies, N = 350) posttreatment.11 There was a significant difference in clinical response and reduction in generalized anxiety disorder symptoms, favouring CBT versus usual care or wait list (RR: 0.64, 95% CI: 0.55–0.74, and SMD: −1.00, 95% CI: −1.24 to −0.77], respectively).11 Seven39–45 of the 12 studies included in the outcome of reduction in generalized anxiety disorder symptom response were also included in the meta-analysis by Cuijpers et al.20
The authors also conducted subset analyses for individual CBT (9 studies) and for group CBT (4 studies) compared with usual care or wait list.11 Patients in individual or group CBT achieved clinical response significantly more than patients in usual care or on wait list (RR: 0.63, 95% CI: 0.51–0.76, and RR: 0.66, 95% CI: 0.54–0.82, respectively).11 Similarly, there was a significant difference in generalized anxiety disorder symptoms, favouring CBT (individual CBT: SMD: −0.98, 95% CI: −1.32 to −0.65; group CBT: SMD: −1.02, 95% CI: −1.35 to −0.69]).11
Hunot et al reported an overall moderate risk of bias for the included studies, according to criteria set out in the Cochrane Handbook.11
The authors reported that the providers of treatment in the studies varied and were described as clinical psychologists; doctoral-, senior-, or advanced-level CBT therapists; “experienced therapists”; or “therapists.”11
Relapse
This outcome was not reported in the systematic reviews.
Adverse Events
This outcome was not reported in the systematic reviews.
Quality of Life
Hunot et al reported on posttreatment improvement in quality of life (3 studies, N = 112).11 The difference in quality-of-life mean scores between people who received CBT and those in the treatment-as-usual/waitlist group was significant, in favour of CBT (SMD: 0.44, 95% CI: 0.06–0.82).11
Interpersonal Therapy Compared With Usual Care for Major Depressive Disorder
Depressive Symptoms, Treatment Response, and Remission
Two systematic reviews reported results for a reduction in depressive symptoms after treatment with interpersonal therapy versus usual care.21,46
Jakobsen et al46 conducted a meta-analysis of 4 randomized controlled trials (N = 553) and reported a significant reduction in depression symptoms for patients with acute major depressive disorder treated with interpersonal therapy compared with usual care. This reduction was based on scores on the Hamilton Depression Rating Scale and the Beck Depression Inventory (mean differences: −3.53 [95% CI: −4.91 to −2.16, P < .0001] and −3.09 [95% CI: −5.35 to −0.83, P = .007]). The authors also reported a significant reduction in the number of patients who did not experience remission (defined as a Hamilton Depression Rating Scale score < 8) in the interpersonal therapy versus treatment-as-usual group (OR: 0.36, 95% CI: 0.24–0.55).46
The authors reported that all trials in the systematic review had a high risk of bias, based on the Cochrane risk-of-bias criteria.46
No studies reviewed by Jakobsen et al reported on the providers of interpersonal therapy, and the definition of usual care varied across the studies (e.g., standard care, clinical management).46
Linde et al conducted a meta-analysis to determine the effectiveness of psychotherapy versus usual care or placebo in primary care patients with major depressive disorder.21 The authors also conducted a meta-analysis of 2 randomized controlled trials (N = 305) for interpersonal therapy. One randomized controlled trial47 was also included in the meta-analysis by Jakobsen et al.46
The standardized mean difference for the posttreatment major depressive disorder scores of patients who had undergone interpersonal therapy compared with control was −0.24 (95% CI: −0.47 to −0.02),21 which indicates that interpersonal therapy significantly improved depression symptoms compared with control.
The authors also reported pooled estimates for response (defined as a depression scale score reduction of ≥ 50%) and remission (defined as a symptom score below a fixed threshold) (OR: 1.28 [95% CI: 0.80–2.05] and OR: 1.37 [95% CI: 0.81–2.34], respectively).21 These results indicate that there was no significant difference between interpersonal therapy and usual care in terms of response or remission.
The authors rated the overall quality of evidence as low, based on the Cochrane risk-of-bias criteria.21
The providers of treatment in the studies reviewed by Linde et al varied and included counsellors, nurses, psychiatrists, psychologists, psychotherapists, and therapists.21 (No distinction between “psychotherapist” and “therapist” was made.) The reporting of intervention details for usual care and co-interventions (e.g., pharmacotherapy) in the groups receiving psychological treatment was often insufficient.21
In 2001, Churchill et al22 conducted a systematic review of psychological treatments compared with usual care for the treatment of major depressive disorder. The authors also conducted a subset analysis of 1 randomized controlled trial47 (N = 185) for interpersonal therapy. Since this single trial was also included in the meta-analyses of Linde et al,21 Biesheuvel-Leliefeld et al,29 and Jakobsen et al,46 details of this study are not discussed here.
Relapse
Two systematic reviews reported results for relapse of major depressive disorder after patients received treatment with interpersonal therapy versus usual care.29,30
Biescheuvel-Leliefeld et al systematically reviewed the effectiveness of psychological interventions compared with usual care or antidepressant drugs in reducing relapse or recurrence rates of patients in remission.29 Usual care was defined as routine clinical management, assessment only, no treatment, or wait list. Relapse and recurrence were defined by the primary study investigators; examples include surpassing a threshold score on a depression scale and demonstrating a change in diagnostic depression status based on clinical assessment. The authors also conducted a subset analysis of 3 randomized controlled trials (N = 142) for interpersonal therapy. The systematic review included 1 randomized controlled trial47 also included in the meta-analyses by Jakobsen et al46 and Linde et al.21
Interpersonal therapy significantly reduced the risk of relapse or recurrence compared with usual care (RR: 0.41, 95% CI: 0.27–0.63) but not compared with antidepressant drugs (RR: 0.83, 95% CI: 0.50–1.38).29
The authors rated the overall quality of evidence for relapse as low, according to the GRADE criteria, owing to varying definitions of remission, recovery, relapse, and recurrence in the primary studies.29
No studies reviewed by Biescheuvel-Leliefeld et al reported on the providers of interpersonal therapy.29
Clarke et al conducted a meta-analysis of 3 randomized controlled trials (N = 342) for interpersonal therapy to determine its effectiveness compared with control (defined as usual care, clinical management, or antidepressant drugs) in patients who had recovered from major depressive disorder (defined as being in full or partial remission).30 One randomized controlled trial48 was included in the meta-analysis by Biescheuvel-Leliefeld et al.29
At 12 months, the risk of developing a new episode of major depressive disorder was significantly reduced in patients who had received interpersonal therapy compared with control (RR: 0.78, 95% CI: 0.65–0.95).30 At 24 months, there was no significant difference between patients who had received interpersonal therapy compared with control in terms of the risk of developing a new episode (RR: 0.92, 95% CI: 0.81–1.05).30
The authors rated the overall quality of evidence for relapse as low, according to the GRADE criteria.30
No studies reviewed by Clarke et al reported on the providers of interpersonal therapy.30
Adverse Events
This outcome was rarely reported in the systematic reviews.
Jakobsen et al stated that 149 of the 4 studies included in their meta-analysis reported adverse events. This was a greater tendency for participants in the treatment-as-usual group to be hospitalized after the end of treatment, but this finding was not statistically significant.46
Quality of Life
This outcome was not reported in the systematic reviews.
Supportive Therapy Compared With Usual Care for Major Depressive Disorder
Depressive Symptoms, Treatment Response, and Remission
We identified 2 systematic reviews that reported results for changes in depressive symptoms after patients had received supportive therapy versus usual care for the treatment of major depressive disorder.14,22
Cuijpers et al conducted a meta-analysis to determine the effectiveness of supportive therapy compared with control (usual care or wait list) (18 studies, N = 899) or pharmacotherapy (4 studies, N = 408) in patients with major depressive disorder.14
Compared with usual care or waitlist control, supportive therapy significantly improved symptoms of depression (SMD: 0.58, 95% CI: 0.45–0.72). However, the authors found no significant difference between supportive therapy and pharmacotherapy (SMD: −0.18, 95% CI: −0.59 to 0.23).14
The authors rated the overall quality of the evidence as low, according to the Cochrane risk-of-bias tool.14
The providers of supportive therapy reported in the studies reviewed by Cuijpers et al were diverse and included nurses, psychiatrists, psychologists, social workers, specialists in counselling, and trained nonspecialists.14
Churchill et al systematically reviewed psychotherapies for the treatment of major depressive disorder and performed an analysis for supportive therapy compared with usual care.22 Of the 4 studies included in this analysis,24,50–52 3 studies24,50,51 were also included in the 2016 systematic review by Cuijpers et al.14 Overall, there was a significant difference in posttreatment recovery (4 studies, N = 118; OR: 2.71, 95% CI: 1.19–6.16]).22 Posttreatment recovery was defined as patients no longer being deemed to have a clinically meaningful level of depression, as indicated by a score of less than 10 on the Beck Depression Inventory or less than 6 on the Hamilton Depression Rating Scale. The authors also found a significant reduction in symptoms for patients who had received supportive therapy versus usual care (4 studies, N = 123; SMD: −0.42, 95% CI: −0.78 to −0.06]).22
The authors reported that the overall quality of evidence was low, based on the Cochrane risk-of-bias tool, owing to low scores on internal validity and inadequate reporting of methodology.22
No studies reviewed by Churchill et al reported on the providers of supportive therapy.22
Adverse Events
This outcome was not reported in the systematic reviews.
Quality of Life
This outcome was not reported in the systematic reviews.
A full summary of the study characteristics and results of all systematic reviews included in this health technology assessment can be found in Appendix 2, Table A2. A summary of the main results is presented in Tables 1a, 1b, and 1c.
Table 1a:
Summary of Results: Cognitive Behavioural Therapy
| Indication | Results |
|---|---|
| Major Depressive Disorder | |
| Symptoms, Treatment Response, Remission |
CBT vs. control (usual care, clinical management, or wait list) Cuijpers et al20
Linde et al21(primary care patients)
Churchill et al22
|
|
ADM + CBT vs. CBT only (acute treatment) Karyotaki et al35
|
|
|
ADM + CBT vs. ADM only (acute treatment) Karyotaki et al35
|
|
|
ADM + CBT vs. ADM only (maintenance treatment) Karyotaki et al35
|
|
|
SGA vs. CBT Amick et al36
|
|
|
SGA only vs. SGA + CBT Amick et al36
Acute CBT (without continuation CBT) vs. acute ADM (with continued ADM) Cuijpers et al37
|
|
|
Acute CBT (without continuation CBT) vs. acute ADM (discontinued at follow-up) Cuijpers et al37
|
|
| Relapse/Recurrence |
CBT vs control (usual care, clinical management, or wait list) Biescheuvel-Leliefeld et al29
Clarke et al30
Guidi et al31
|
| Adverse Events | Not reported |
| Quality of Life | Not reported |
| Generalized Anxiety Disorder | |
| Symptoms, Treatment Response, Remission |
Compared with control (usual care, clinical management, or wait list) Cuijpers et al20
Cuijpers et al53
Hunot et al11
|
| Relapse/Recurrence | Not reported |
| Adverse Events | Not reported |
| Quality of Life | Compared with control (usual care, clinical management, or wait list) |
| Hunot et al11 | |
| Improvement in quality-of-life score: SMD = 0.44 (95% CI: 0.06–0.82) | |
Abbreviations: ADM, antidepressant medication; BDI, Beck Depression Inventory; CBT, cognitive behavioural therapy; CI, confidence interval; GAD, generalized anxiety disorder; HDRS, Hamilton Depression Rating Scale; MDD, major depressive disorder; OR, odds ratio; SGA, second-generation antidepressant; SMD, standardized mean difference; WMD, weighted mean difference.
Defined by Churchill et al as no longer having a clinically meaningful level of depression (as measured by a BDI score < 10 or an HDRS score < 6).22
Table 1b:
Summary of Results: Interpersonal Therapy
| Indication | Results |
|---|---|
| Major Depressive Disorder | |
| Symptoms, Treatment Response, Remission |
Compared with control (usual care, clinical management, or wait list) Jakobsen et al46
Linde et al21(primary care patients)
|
| Relapse/Recurrence |
Biescheuvel-Leliefeld et al29
Clarke et al30
|
| Adverse Events | Not reported |
| Quality of Life | Not reported |
| Generalized Anxiety Disorder | |
| Symptoms, Treatment Response, Remission | Not reported |
| Relapse/Recurrence | Not reported |
| Adverse Events | Not reported |
| Quality of Life | Not reported |
Abbreviations: ADM, antidepressant medication; BDI, Beck Depression Inventory; CI, confidence interval; HDRS, Hamilton Depression Rating Scale; IPT, interpersonal therapy; MDD, major depressive disorder; OR, odds ratio; SMD, standardized mean difference.
Table 1c:
Summary of Results: Supportive Therapy
| Indication | Results |
|---|---|
| Major Depressive Disorder | |
| Symptoms, Treatment Response, Remission |
Cuijpers et al14
Churchill et al22
|
| Relapse/Recurrence | Not reported |
| Adverse Events | Not reported |
| Quality of Life | Not reported |
| Generalized Anxiety Disorder | |
| Symptoms, Treatment Response, Remission | Not reported |
| Relapse/Recurrence | Not reported |
| Adverse Events | Not reported |
| Quality of Life | Not reported |
Abbreviations: BDI, Beck Depression Inventory; CI, confidence interval; HDRS, Hamilton Depression Rating Scale; MDD, major depressive disorder; OR, odds ratio; SMD, standardized mean difference.
Defined by Churchill et al as no longer having a clinically meaningful level of depression (as measured by a BDI score < 10 or an HDRS score < 6).22
Discussion
Cognitive Behavioural Therapy
Cognitive Behavioural Therapy Compared With Usual Care
Three meta-analyses of CBT for the treatment of major depressive disorder indicated that CBT significantly reduced depression symptoms posttreatment compared with usual care.20–22
Three meta-analyses reported results for posttreatment relapse of major depressive disorder following treatment with CBT versus usual care.29–31 Overall, the 3 reviews concluded that CBT significantly reduced the risk of relapse or recurrence compared with usual care.29–31
Two meta-analyses of CBT for the treatment of generalized anxiety disorder indicated that CBT significantly reduced anxiety symptoms posttreatment compared with usual care.11,20
None of the systematic reviews reported on adverse events.
One systematic review of CBT for the treatment of generalized anxiety disorder assessed quality of life.11 The difference in mean quality-of-life scores between patients who had received CBT and those who had received usual care was significant, in favour of CBT.11
The overall quality of the evidence within the systematic reviews was generally reported as low. Reasons for this include antidepressants used in control groups being variously described as “treatment as usual” and “clinical management”; varying definitions provided for recovery, recurrence, relapse, and remission; lack of blinding of patients and treatment providers; and several studies excluding from their analyses randomized patients who did not commence treatment or later dropped out.
Cuijpers et al performed a meta-analysis of CBT versus usual care with regard to symptom reduction.20 They evaluated the evidence for publication bias and estimated that approximately 14% of major depressive disorder studies and 25% of generalized anxiety disorder studies were missing from their meta-analysis; however, they reported that this did not change the statistical significance of their pooled summary estimates.20 Driessen et al investigated publication bias in the literature on psychological interventions for depression and concluded that the efficacy of psychological interventions in general has been overestimated in the published literature, as it has been for pharmacotherapy.54 The authors stated that both treatments are effective but not to the extent that the published literature would suggest.54 As a result, Driessen et al suggest that funding agencies and journals should archive both original protocols and raw data from studies to allow for the detection and correction of outcome-reporting bias.54
Cuijpers et al commented on the quality of CBT in generalized anxiety disorder studies, finding that not all psychotherapy providers reported using a standard manual and that limited information was provided on treatment components, including those of CBT, and adherence to treatment manuals.38 The authors further stated that the literature on psychotherapy studies for generalized anxiety disorder differs markedly from that for major depressive disorder, in which the same standard treatment manual is used across many studies.38
The systematic reviews rarely reported details about the providers of CBT; in those that did, there was variation in provider type.
Cognitive Behavioural Therapy With and Without Pharmacotherapy Compared With Pharmacotherapy Only
For the acute treatment of major depressive disorder, Karyotaki et al reported no significant difference in response rates for combined CBT and antidepressants compared with CBT only at up to 6 months and up to 1 year postrandomization.35
Amick et al systematically reviewed second-generation antidepressants compared with CBT for the treatment of major depressive disorder and found no significant difference in response or remission rates.36
Cuijpers et al compared acute-phase CBT (without continuation treatment) with acute-phase pharmacotherapy (with pharmacotherapy continued during follow-up) in patients with major depressive disorder and found no significant difference in outcome (as measured by the number of patients who responded to treatment and remained well) at a 1-year follow-up.37 However, when acute-phase CBT (without continuation treatment) was compared with acute-phase pharmacotherapy that was discontinued during follow-up, there was a significant difference in 1-year outcomes, favouring CBT.37
The systematic reviews did not report on adverse events or quality of life.
The overall quality of the evidence within 2 systematic reviews was generally reported as low.35,36 However, Cuijpers et al considered the overall quality of the evidence they reviewed to be “relatively high” compared with the quality of studies on psychotherapy for adult depression in general.37
Details about treatment providers were rarely reported in these systematic reviews.
Interpersonal Therapy
Two meta-analyses of interpersonal therapy for the treatment of major depressive disorder indicated that interpersonal therapy significantly reduced depression symptoms posttreatment compared with usual care.21,46
The overall quality of the evidence within the systematic reviews was consistently reported as low. Of note, the feasibility of providing high-quality evidence in psychological studies is difficult, and the issues affecting quality are not easily addressed within the context of randomized controlled trials.22 For example, individual therapist characteristics cannot be controlled for, nor can the nature of the therapeutic encounter be measured with absolute precision.22
The systematic reviews rarely reported on treatment providers.
We identified no systematic reviews of interpersonal therapy for the treatment of generalized anxiety disorder that matched our inclusion criteria.
Supportive Therapy
Two meta-analyses of supportive therapy for the treatment of major depressive disorder concluded that supportive therapy significantly reduced symptoms of major depressive disorder posttreatment compared with usual care. Cuijpers et al found no significant difference between supportive therapy and pharmacotherapy in reducing symptoms of depression in patients with major depressive disorder.14 Churchill et al found a significant difference in posttreatment recovery favouring supportive therapy versus usual care.22
Adverse events and quality of life were not reported in the systematic reviews.
As with interpersonal therapy, the overall quality of the evidence within the systematic reviews was consistently reported as low, based on similar reasons to those discussed for interpersonal therapy, as well as low scores on internal validity and inadequate reporting of methodology.22
The systematic reviews rarely reported on treatment providers.
We identified no systematic reviews of supportive therapy for the treatment of generalized anxiety disorder that matched our inclusion criteria.
Limitations to This Systematic Review
The following limitations apply to our systematic review:
Primary studies were not included in this analysis; we included only systematic reviews.
Interventions were compared with usual care or pharmacotherapy. Psychological interventions were not directly compared with each other
We did not include systematic reviews on long-distance or computer/Internet-based psychotherapy
The patient population was restricted to adults; we excluded pediatric and geriatric populations
We considered only major depressive disorder and generalized anxiety disorder; we did not examine other types of depression or anxiety
Conclusions
Cognitive Behavioural Therapy, Interpersonal Therapy, or Supportive Therapy Compared With Usual Care for Major Depressive Disorder and Generalized Anxiety Disorder
Treatment with CBT, interpersonal therapy, or supportive therapy reduces symptoms of major depressive disorder and increases response/recovery posttreatment
CBT and interpersonal therapy significantly reduce the risk of relapse/recurrence of major depressive disorder
Individual CBT significantly improves posttreatment recovery from major depressive disorder compared with group CBT
CBT significantly reduces symptoms of generalized anxiety disorder and increases response posttreatment
CBT significantly improves quality-of-life scores in people with generalized anxiety disorder
Cognitive Behavioural Therapy With and Without Pharmacotherapy Compared With Pharmacotherapy Only for Major Depressive Disorder
Combined therapy (CBT with pharmacotherapy) significantly improves treatment response compared with pharmacotherapy only
CBT significantly improves treatment response compared with pharmacotherapy only following termination of both acute interventions
Details About Psychotherapy Providers
Of the systematic reviews we examined, 3 reported on provider type; in these reviews, a diverse range of providers was described
ECONOMIC EVIDENCE
Research Questions
What is the cost-effectiveness of a psychological treatment (i.e., CBT, interpersonal therapy, or supportive therapy) provided as the only therapy or combined with pharmacotherapy for the management of adults with major depressive disorder and/or generalized anxiety disorder?
What is the cost-effectiveness of different outpatient models of care for providing in-person psychological treatments in the management of adults with major depressive disorder and/or generalized anxiety disorder?
Methods
Literature Search
We performed an economic literature search on October 28, 2016, for studies published from January 1, 2000, until the search date. To retrieve relevant studies, we used the clinical search strategy with an economic filter.
Database auto-alerts were created in CINAHL, Embase, MEDLINE, and PsycINFO and monitored for the duration of the health technology assessment review. We performed targeted grey literature searching of health technology assessment agency websites and clinical trial registries. See Clinical Evidence, Literature Search (p. 11), for further details on methods used.
Finally, we reviewed the reference lists of the included economic literature for any additional relevant studies not identified through the systematic search.
The literature search strategies, including all search terms, are described in Appendix 1.
Literature Screening
A single reviewer screened titles and abstracts, and, for those studies meeting the inclusion criteria, we obtained full-text articles. For the full-text citations that did not meet the inclusion criteria, we recorded reasons for exclusion.
Inclusion Criteria
English-language, individual-level economic evaluations conducted alongside randomized controlled trials (i.e., trial-based) or economic analyses based on decision analytic models (i.e., model-based)
Studies in adults with major depressive disorder and/or generalized anxiety disorder indicated for psychotherapy
Studies comparing CBT, interpersonal therapy, or supportive therapy with other nonpharmacologic therapies or no treatment (e.g., waitlist control)
Studies comparing different models of providing in-person CBT, interpersonal therapy, or supportive therapy (e.g., group vs. individual therapy, physician vs. nonphysician provider)
Exclusion Criteria
Reviews (systematic and narrative), study protocols, guidelines, conference abstracts, commentaries, letters, and editorials
Economic evaluations of psychotherapy for the treatment of postnatal depression or comorbid depression (i.e., depression coexisting with chronic diseases such as cardiovascular disease, dementia, diabetes mellitus, or inflammatory bowel disease) or studies conducted in adolescent populations
Economic evaluations of psychotherapies provided via computer-based technologies such as computer programs or Internet-based applications
Economic evaluations comparing collaborative team or stepped-care models with usual care for the treatment of major depressive disorder or generalized anxiety disorder
Economic studies in inpatient adults with treatment-resistant depression (secondary psychiatric care)
Feasibility studies exploring different models of care for the treatment of major depressive disorder or generalized anxiety disorder that do not report economic outcomes
Noncomparative studies reporting the costs of psychotherapies
Cost-of-illness studies
Types of Participants
The population of interest was adults (aged 18 years and older) with a new diagnosis or recurrent episode of major depressive disorder and/or generalized anxiety disorder.
Types of Interventions
We compared the following interventions:
In-person (face-to-face) psychotherapy (CBT, interpersonal therapy, or supportive therapy) versus usual care, pharmacotherapy only, or combined pharmacological and psychological therapy
Individual in-person (face-to-face) psychotherapy (CBT, interpersonal therapy, or supportive therapy) versus group psychotherapy (CBT, interpersonal therapy, or supportive therapy)
Types of Outcomes Measures
We examined the following outcomes:
Incremental costs
Incremental effectiveness outcomes (e.g., incremental quality-adjusted life-years, disability-adjusted life-years)
Incremental cost-effectiveness ratios
Incremental net benefit
Data Extraction
We extracted the following data from the included literature:
Source (i.e., name, location, year)
Population and comparator
Interventions
Outcomes (i.e., health outcomes, costs, cost-effectiveness)
Study Applicability and Methodological Quality
We determined the usefulness of each identified study for decision-making by applying a modified applicability checklist for economic evaluations that was originally developed by the National Institute for Health and Care Excellence (NICE) in the United Kingdom. The original checklist is used to inform development of clinical guidelines by NICE. We retained questions from the NICE checklist related to study applicability and modified the wording of the questions to remove references to guidelines and to make it Ontario specific. The results of the applicability checklist and our assessment of the methodological quality of the studies included in the economic literature review are presented in Appendices 4 and 5, respectively.
Results
Literature Search
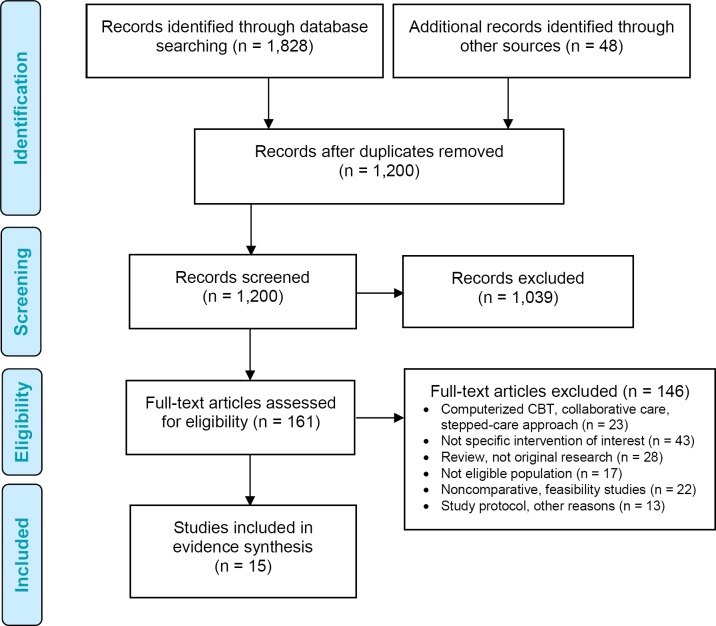
The database and grey literature searches yielded 1,200 citations published between January 1, 2000, and October 28, 2016 (with duplicates removed). We excluded a total of 1,039 articles based on information in the title and abstract. We then obtained the full texts of 161 potentially relevant articles for further assessment. A total of 15 studies met the inclusion criteria and were synthesized to establish the applicability of their findings to the Ontario context. Figure 2 presents the flow diagram for the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) for the economic evidence review.
Figure 2: PRISMA Flow Diagram—Economic Evidence Review.
Source: Adapted from Moher et al.19
Abbreviations: CBT, cognitive behavioural therapy; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analyses.
Review of Included Economic Studies
Of the 15 eligible studies,55–69 14 examined the cost-effectiveness of CBT, 1 examined the cost-effectiveness of interpersonal therapy,58 and none examined the cost-effectiveness of supportive therapy. Nine studies were individual-level cost-effectiveness analyses conducted alongside randomized controlled trials; their sample sizes ranged from 93 to 469 participants.57–60,62,64,66–68 Six economic evaluations were model-based cost-effectiveness analyses.55,56,61,63,65,69 Only 1 model-based cost-effectiveness analysis examined the cost-effectiveness of CBT in patients with generalized anxiety disorder alone55; the rest included populations with major depressive disorder alone or both major depressive disorder and symptoms of anxiety. No studies stated whether patients were diagnosed with generalized anxiety disorder, but some patients were reported to have anxiety. This was not recorded in a systematic way across the studies.
Overall, CBT, provided as individual or group therapy, provided as the only therapy or in combination with pharmacotherapy, represents good value for money at different country-specific willingness-to-pay thresholds. The cost-effectiveness of interpersonal therapy, based on 1 study from the Netherlands,58 is uncertain.
In line with our two research questions, we next summarize, compare, and contrast study designs with respect to the type, perspective, and time horizon of analysis; study populations; comparative strategies; and study outcomes (i.e., effects or benefits and costs). We also describe the main cost-effectiveness findings. Tables 2a, 2b, and 2c summarize the characteristics and results of the included studies.
Table 2a:
Results of Economic Literature Review—Summary: Cost-Effectiveness of CBT for the Treatment of Major Depressive Disorder and/or Generalized Anxiety Disorder
| Name, Year, Location | Economic Analysis, Study Design, and Perspective | Population and Comparator | Interventions | Results | ||
|---|---|---|---|---|---|---|
| Health Outcomes | Costs | Cost-Effectiveness | ||||
| Wiles et al, 2016, United Kingdom68 |
|
|
|
|
|
|
| Koeser et al, 2015, United Kingdom69 |
|
|
|
|
|
|
| Hollinghurst et al, 2014, United Kingdom67; Wiles, 2014, United Kingdom (HTA report, duplicate publication)70 |
|
|
|
|
|
|
| Kafali et al, 2014, Puerto Rico/United States66 |
|
|
|
|
|
|
| Prukkanone et al, 2012, Thailand65 |
|
|
|
|
|
|
| Holman et al, 2011, United Kingdom64 |
|
|
|
|
|
|
| Sava et al, 2009, Romania62 |
|
|
|
|
|
|
| Sado et al, 2009, Japan63 |
|
|
|
|
|
|
| Simon et al, 2006, United Kingdom61 |
|
|
|
|
|
|
| Revicki et al, 2005, United States60 |
|
|
|
|
|
|
| Scott et al, 2003, United Kingdom59 |
|
|
|
|
|
|
Abbreviations: BDI-II, Beck Depression Inventory, second edition; CBT, cognitive behavioural therapy; CER, cost-effectiveness ratio; CoBalT, Cognitive Behavioural Therapy as an adjunct to pharmacotherapy for treatment-resistant depression in Primary Care; CrI, credible interval; DALY, disability-adjusted life-year; ED, emergency department; GP, general practitioner; HDRS-17, Hamilton Depression Rating Scale, 17 items; HR, hazard ratio; HTA, health technology assessment; ICER, incremental cost-effectiveness ratio; MDD, major depressive disorder; MDE, major depressive episode; NA, not applicable; NHS, National Health Service; NR, not reported; PHQ-9, Patient Health Questionnaire-9; PPS, Personal Public Service; REBT, rational emotive behaviour therapy; QALY, quality-adjusted life year; RCT, randomized controlled trial; SD, standard deviation; WTP, willingness-to-pay threshold.
This is the range reported; however, we believe there may have been a typographical error and that the correct range may be 160–300.
Table 2b:
Results of Economic Literature Review—Summary: Cost-Effectiveness of Interpersonal Therapy for the Treatment of Major Depressive Disorder
| Name, Year, Location | Study Design and Perspective | Population and Comparator | Interventions | Results | ||
|---|---|---|---|---|---|---|
| Health Outcomes | Costs | Cost-Effectiveness | ||||
| Bosmans et al, 2007, Netherlands58 |
|
|
|
|
|
|
Abbreviations: CBT, cognitive behavioural therapy; GP, general practitioner; ICER, incremental cost-effectiveness ratio; IPT, interpersonal therapy; MADRS, Montgomery–Åsberg Depression Rating Scale; MDD, major depressive disorder; NR, not reported; PRIME-MD, Primary Care Evaluation of Mental Disorders; QALY, quality-adjusted life-year; RCT, randomized controlled trial; SD, standard deviation.
Table 2c:
Results of Economic Literature Review—Summary: Cost-Effectiveness of Outpatient Models of Care for Providing In-Person CBT for the Treatment of Major Depressive Disorder and/or Generalized Anxiety Disorder
| Name, Year, Location | Study Design and Perspective | Population and Comparator | Interventions | Results | ||
|---|---|---|---|---|---|---|
| Health Outcomes | Costs | Cost-Effectiveness | ||||
| Brown et al, 2011, United Kingdom57 |
|
|
|
|
|
|
| Vos et al, 2005, Australia56 |
|
|
|
|
|
|
| Heuzenroeder et al, 2004, Australia55 |
|
|
|
Total DALYs compared with current practice:
|
|
|
Abbreviations: CBT, cognitive behavioural therapy; DALY, disability-adjusted life-year; GAD, general anxiety disorder; ICER, incremental cost-effectiveness ratio; MDD, major depressive disorder; MDE, major depressive episode; NA, not applicable; NHS, National Health Service; NR, not reported; QALY, quality-adjusted life-year; SD, standard deviation; SNRI, serotonin–norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant.
The Cost-Effectiveness of Cognitive Behavioural Therapy for the Management of Adults with Major Depressive Disorder and/or Generalized Anxiety Disorder
Study Design
Seven trial-based cost-effectiveness analyses (4 from the United Kingdom, 2 from the United States, and 1 from Romania)59,60,62,64,66–68 and 4 model-based cost-effectiveness analyses (2 from the United Kingdom, 1 from Thailand, and 1 from Japan)61,63,65,69 examined the cost-effectiveness of CBT (see Table 2a).
Perspective
Study perspective depended on the features of each country's health care system; thus, the U.S. studies were conducted from a health care payer's perspective, whereas the majority of the other studies were conducted from a societal perspective or included a societal perspective in a sensitivity analysis.
Time Horizon
The duration of follow-up (in trial-based cost-effectiveness analyses) or time horizon (in model-based cost-effectiveness analyses) was short in most studies, ranging from 4 to 24 months, thus not allowing enough time to account for the recurrent and chronic nature of the disorders.
Population
Studies included mixed populations consisting of people with newly diagnosed major depressive disorder and those experiencing recurrent episodes. Therefore, in the majority of the cost-effectiveness analyses we reviewed, the disorder was considered moderate or severe.
Comparators
Most studies compared CBT combined with pharmacotherapy to pharmacotherapy only (i.e., usual care). CBT was provided in the first 4 months of treatment (i.e., in the acute and continuation phases). The total number of in-person CBT sessions in the trial-based cost-effectiveness analyses ranged from 566 to 18,67 and sessions typically lasted 50 to 90 minutes. In the model-based studies, CBT was provided in 10 to 16 weekly sessions, each lasting between 50 and 60 minutes.
Outcomes: Effects and Costs
In all model-based61,63,65,69 and 3 trial-based economic analyses,64,67,68 the effectiveness of CBT versus usual care was expressed in adjusted life-year outcomes (i.e., quality-adjusted life-years [QALYs] or disability-adjusted life-years [DALYs]). The other trial-based cost-effectiveness analyses examined the benefit of CBT in terms of clinically relevant health outcomes such as mean changes in depression scale scores from baseline (i.e., symptom improvement),64,66 the number of relapses or recurrent episodes at the end of follow-up,59 and the number of depression-free days.60,62
All studies found improvements in clinical outcomes and incremental gains in QALYs for CBT compared with usual care (see Table 2a). For example, Revicki et al found that the total number of days with depression decreased by 26 with CBT versus usual care (P = .05),60 and Scott et al found a statistically significant 50% reduction in the rate of recurrence at 62 weeks in patients treated with 16 sessions of CBT versus usual care (mean hazard ratio: 0.51, 95% CI: 0.32–0.92).59
In trial-based cost-utility analyses, CBT was associated with an increase in QALYs of between 0.05 and 0.06. In the model-based cost-utility analyses, this increase was between 0.03 and 0.04 QALYs for moderate major depressive disorder and between 0.08 and 0.11 QALYs for severe major depressive disorder.61,63,69
In all studies, the unit costs were adequately assessed, with the majority of cost-effectiveness analyses using a bottom-up approach for calculating costs incurred during the study. Direct medical costs were calculated from the following estimates:
Cost of treatment (e.g., CBT, pharmacotherapy)
Professionals' time spent on CBT delivery, follow-up, and consultation
Health care employee salaries (including benefits)
Health care service use (e.g., number of hospitalizations; number visits to emergency departments, general practitioners, and psychiatrists)
If a societal perspective was applied, costs included the costs of social care services (e.g., costs of social work or social self-help services, home help, employment services) and indirect costs (e.g., costs of travel time to attend therapy, over-the-counter drugs, private or alternative therapies, loss of earnings owing to time off work, disability payments, productivity loss). Incurred costs in the trial-based cost-effectiveness analyses were collected per participant using validated questionnaires for the assessment of resource use and time.
All studies provided overall treatment costs, including those for CBT, which incurred greater costs than usual care. In addition, a few studies estimated costs solely applicable to the use of CBT, including the number of sessions and the salary of the CBT provider. For example, Scott et al estimated the mean cost of delivering a 16-session course of CBT to be £1,664 (in 1999 £),59 and Revicki et al estimated the mean cost of delivering an 8-session course of CBT to be US$1,844 (in 2005 USD).60
Cost-Effectiveness
All but one modelling study69 found that, compared with usual care, CBT only or CBT in combination with pharmacotherapy represented good value for money at different country-specific willingness-to-pay thresholds. In modelling studies that favoured CBT over usual care, the probability of cost-effectiveness ranged from 76% to 88% for moderate major depressive disorder and was over 96% for severe major depressive disorder (at a country-specific willingness-to-pay threshold of £30,000 per QALY (United Kingdom)61 or ¥6.75 million per QALY (Japan).63
A model-based cost-effectiveness analysis by Koeser et al produced slightly different results than the other cost-effectiveness analyses we reviewed.69 Koeser et al found lower probabilities of CBT being cost-effective in a cost-effectiveness analysis of CBT versus pharmacotherapy only (20% at a willingness-to-pay threshold of £25,000/QALY) and in a cost-effectiveness analysis of the combination of CBT and pharmacotherapy versus pharmacotherapy only (43%).69 These less favourable estimates may be explained in the following ways. First, the base case population was more severely ill than in the other studies; consequently, the model did not consider no treatment as usual care. Second, the efficacy of CBT only or CBT combined with pharmacotherapy was estimated in a Bayesian meta-analysis that included few randomized controlled trials; consequently, the point estimate was associated with a large degree of uncertainty. This uncertainty regarding the intervention effect propagated throughout the model, resulting in a large degree of uncertainty around the estimate of the incremental cost-effectiveness ratio.
The Cost-Effectiveness of Interpersonal Therapy for the Management of Adults With Major Depressive Disorder
Among the studies that met our inclusion criteria, only one compared the cost-effectiveness of interpersonal therapy versus usual care (i.e., no treatment, psychoeducation, or psychoeducation combined with pharmacotherapy). Bosmans et al conducted a 12-month trial-based cost-effectiveness analysis of 143 Dutch adults with major depressive disorder in which 10 sessions of interpersonal therapy were provided over 5 months (see Table 2b).58 Compared with usual care (i.e., no treatment), interpersonal therapy was associated with a statistically significant increase in incremental costs of ζ769 (95% CI: −ζ2,459 to ζ3,433 [in 2003 ζ]) and statistically nonsignificant increments in effects (mean difference: 0.01, 95%CI: −0.08 to 0.10). These results led to a considerable estimate of the incremental cost-effectiveness ratio of ζ76,900 per QALY gained, a large degree of uncertainty regarding this estimate, and the conclusion that interpersonal therapy is not cost-effective at acceptable willingness-to-pay thresholds in the Netherlands.
The Cost-Effectiveness of Outpatient Models of Care for In-Person Cognitive Behavioural Therapy
Study Design
One individual-level economic analysis from the United Kingdom57 and 2 model-based cost-effectiveness analyses from Australia55,56 examined the cost-effectiveness of having in-person CBT provided by different types of provider (Table 2c). The UK study was a cost-minimization analysis that used data from 93 cohort participants of a national psychotherapy service trust.57
Perspective
All studies used a health care payer's perspective.
Time Horizon
The time horizon was 3 months in the individual-level cost-minimization analysis57 and 5 years in the model-based cost-effectiveness analyses.55,56
Population
The study population of the individual-level cost-minimization economic analysis was adults with major depressive disorder.57 The base case populations for the model-based analyses had either major depressive disorder56,57 or generalized anxiety disorder.55
Comparators
The UK study directly compared the costs of providing CBT as 6 to 18 weekly individual sessions with the costs of providing CBT in 10 to 12 weekly group sessions including 8 to 12 participants.57 The 2 Australian model-based cost-effectiveness analyses compared 5 to 7 interventions55,56:
CBT provided by publicly and privately funded providers (psychiatrists or psychologists)
Individual versus group CBT
Different phases of CBT treatment (acute vs. maintenance phase)
Pharmacotherapy (tricyclic antidepressants vs. selective serotonin reuptake inhibitors) with different treatment durations (6 months vs. 5 years)
Bibliotherapy (acute phase)
Outcomes: Benefits and Costs
The largest benefits, expressed in terms of years of life lost and DALYs, were associated with the following55,56:
CBT provided for 9 months only
CBT provided in the acute phase together with CBT booster sessions provided over a period of 5 years
Pharmacotherapy taken for 5 years
The smallest increment in costs was found for CBT provided as group therapy by publicly funded therapists.55,56 A 3-month analysis from the United Kingdom found no statistically significant difference in total costs between group and individual CBT.57
Cost-Effectiveness
In the cost-effectiveness analysis, both group CBT and individual CBT for the treatment of major depressive disorder or generalized anxiety disorder were associated with a favourable estimate of the incremental cost-effectiveness ratio (ICER) of AU$10,000 per DALY when provided by a publicly funded psychologist.55,56
Applicability and Methodological Quality of the Included Studies
We deemed 11 studies partially applicable to our research question, as they had some similarities to our base case population and comparators. The major differences were a short duration of follow-up and a lack or inclusion of patients with mild disease. However, none of the studies was done in Canada or Ontario; thus, the results of the cost-effectiveness analyses cannot be directly translated to the Ontario context owing to differences in health care systems. Appendix 4 describes the applicability of the included studies to the context of Ontario's health care system and to our study objectives.
We found that the majority of studies had important limitations, particularly in terms of the assessment of all important health outcomes, the inclusion of all relevant comparators, the relatively short duration of the time horizons used, and the lack of exploration of uncertainty and its influence on the studies' cost-effectiveness estimates. Appendix 5 outlines the methodological limitations of the examined studies.
Discussion
Our evidence synthesis found that CBT is the most researched psychological therapy for the management of major depressive disorder and generalized anxiety disorder. In the majority of the cost-effectiveness evaluations we reviewed (9 trial-based and 5 model-based), and as compared with usual care, we found that CBT only or in combination with pharmacotherapy represents good value for money for adults with major depressive disorder and/or generalized anxiety disorder at various country-specific willingness-to-pay thresholds. At these thresholds, CBT was found to have a greater than 90% likelihood of being cost-effective for people with severe or recurrent major depressive disorder. However, the cost-effectiveness of structured in-person CBT in populations with mild major depressive disorder or generalized anxiety disorder is largely unknown owing to a lack of economic studies in these populations or our restrictive inclusion criteria regarding the use of computerized CBT.
Evidence is scarce regarding the cost-effectiveness of interpersonal therapy, another regularly used structured psychological therapy for people with major depressive disorder. We identified only 1 trial-based study58; this was conducted in the Netherlands with a small sample of 143 patients with major depressive disorder. It suggested that interpersonal therapy may not be more efficient than usual care (defined as no treatment, psychoeducation, or psychoeducation combined with pharmacotherapy). In addition, no economic evaluation examined the cost-effectiveness of supportive therapy.
Lastly, limited and mixed evidence exists regarding the cost-effectiveness of CBT provided by different types of health care professionals, either as individual or as group therapy. While a 3-month trial-based cost-minimization analysis in 93 adults with major depressive disorder suggested no differences in the mean costs between individual and group CBT,57 2 Australian economic studies suggested that group CBT, provided either short term or long term, by publicly funded psychologists represented good value for money.55,56
Conclusions
Major depressive disorder and generalized anxiety disorder are among the most commonly diagnosed mental illnesses in Canada and are associated with a high societal and economic burden.71–75 Access to cost-effective psychological treatments in Ontario is needed to optimize care.76–78 We evaluated a relatively large number of economic analyses in this review. However, none of the economic analyses was done from the perspective of Ontario or Canada, and many studies had methodological limitations.
PRIMARY ECONOMIC EVALUATION
The published economic evaluations identified in the literature review addressed the cost-effectiveness of structured psychological therapies (CBT or interpersonal therapy), as the only therapy or in combination with pharmacotherapy, for the management of major depressive disorder and/or generalized anxiety disorder in adults, but none took a Canadian or Ontario perspective. Owing to this limitation, we conducted a primary economic evaluation to determine whether in-person structured psychological treatment provided by publicly funded, regulated health care professionals for the management of major depressive disorder and/or generalized anxiety disorder in adult outpatients represents good value for money from the perspective of the Ontario Ministry of Health and Long-Term Care.
Research Question
What is the cost-effectiveness of individual or group CBT versus usual care, where CBT is provided as the only treatment or in combination with pharmacotherapy and is delivered by publicly funded, regulated therapists (physicians or nonphysicians) to adults with major depressive disorder and/or generalized anxiety disorder?
Methods
The information presented in this report follows the reporting standards set out by the Consolidated Health Economic Evaluation Reporting Standards Statement.79 Our methodological approaches follow the recent recommendations set out by the fourth edition of the Canadian Agency for Drugs and Technologies in Health (CADTH) Guidelines for the Economic Evaluation of Health Technologies: Canada80 and align with Health Quality Ontario's Health Technology Assessments Methods and Process Guide.16
Type of Analysis
We conducted cost-effectiveness and cost-utility analyses. Our cost-effectiveness analyses assessed the cost per recurrent episode or per hospitalization avoided and the cost per life-year saved. Our cost-utility analysis assessed the cost per QALY gained.
Target Population
The study population was newly diagnosed adult outpatients aged 18 to 75 years with a primary diagnosis of major depressive disorder alone or in combination with generalized anxiety disorder.
Major depressive disorder has an episodic nature.81,82 In clinical practice, people with mild major depressive disorder follow a different clinical pathway than those with moderate to severe major depressive disorder. As suggested by the clinical experts we consulted, we defined the baseline severity of a major depressive episode by the score on the 9-item Patient Health Questionnaire (PHQ-9),83 which corresponds to the 9 diagnostic criteria of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).71,84–87 Mild major depressive disorder corresponds to a PHQ-9 score of between 10 and 14, and moderate to severe major depressive disorder corresponds to a PHQ-9 score of more than 14. In addition to the DSM-5 criteria, the diagnosis of generalized anxiety disorder corresponds to a score equal to or greater than 10 on a 7-item generalized anxiety disorder scale called the GAD-7.88 It is worth noting that although anxiety disorders can exist in isolation, at least half the time, generalized anxiety disorder coexists with major depressive disorder.89–91 Therefore, in our base case analysis, our target population consisted of people with both major depressive disorder and generalized anxiety disorder; in our scenario analysis, we examined people with generalized anxiety disorder only.
We excluded some populations with depression from our analysis owing to important differences in treatment pathways92,93:
People initially at high risk of suicide, indicated for hospitalization and secondary psychiatric care (in such cases, the depression is considered treatment-resistant disease)
People with comorbid depression (i.e., depression owing to another health condition, such as cardiovascular disease, chronic pain, or diabetes)
Geriatric populations with dementia or cognitive impairment
Adolescents
People who are pregnant or postpartum
Perspective
We conducted this economic analysis from the perspective of the Ontario Ministry of Health and Long-Term Care.
Interventions
Cognitive Behavioural Therapy
The base case analysis examined the cost-effectiveness of CBT as the most commonly used and researched psychological treatment for major depressive disorder. CBT is often provided through 8 to 20 initial sessions over the first 4 months following diagnosis with several follow-up sessions provided during the maintenance phase.89,90,94,95 CBT with continuous and interactive clinician engagement can be delivered as a structured, face-to-face therapy, as a remote, interactive therapy (via phone, teleconference, or Internet-based technologies such as Skype), or as a computer-delivered self-help therapy.71,84–87
Our analysis focused on the structured face-to-face approach to CBT, delivered as either individual or group therapy by a publicly funded, regulated (registered and professionally trained) health care professional (physician or nonphysician). Based on expert consultation, in the base case analysis, we assumed that CBT is provided in 14 weekly sessions, lasting an hour if provided by an individual therapist or 2 hours if provided as group therapy. The training of nonphysician therapists is regulated by professional organizations in Ontario.
Based on expert consultation, we also assumed that CBT provided by regulated nonphysician therapists (e.g., nurses, occupational therapists, psychologists, psychotherapists, social workers) is administered with no difference in terms of resource time or labour costs (i.e., salaries).
Interpersonal Therapy
Interpersonal therapy is often provided on an individual basis and delivered over 6 to 20 sessions.96 Therefore, we conducted a scenario analysis to examine the cost-effectiveness of interpersonal therapy in the initial treatment phase, assuming the same delivery options and number of sessions as for CBT.71,84–87
Pharmacotherapy
In addition to psychological treatments, and depending on disease severity, another common treatment option for noncomplex major depressive disorder (i.e., major depressive disorder that is not treatment-resistant) is pharmacotherapy (i.e., antidepressants, including selective serotonin reuptake inhibitors [SSRIs], such as sertraline, and serotonin–norepinephrine reuptake inhibitors [SNRIs], such as venlafaxine).2,8–10 Generalized anxiety disorder is treated with similar medications to those used for noncomplex major depressive disorder. In the case of treatment-resistant major depressive disorder (a complex form of major depressive disorder), pharmacotherapy is often combined with brain intervention therapies. Examples of such therapies include electroconvulsive therapy, transcranial magnetic stimulation, and magnetic seizure therapy.71,84–87
Given the similarity of treatment pathways for major depressive disorder and generalized anxiety disorder, and the fact that many people experience both major depressive disorder and generalized anxiety disorder, our modelling approach focused on representing the natural and clinical course of major depressive disorder. In addition, and based on current clinical practice (as established through expert consultation), first and recurrent episodes of major depressive disorder are handled in the same way: CBT only or with pharmacotherapy, depending on the episode severity.
Table 3 summarizes the interventions we evaluated in the economic model. The intervention and usual-care strategies depended on the severity of the major depressive disorder episode. Newly diagnosed adults followed different clinical treatment pathways depending on the severity of the episode; that is, whether it was mild or moderate to severe. Mild episodes were considered to be treated with CBT only, whereas mild to moderate episodes were considered to be treated with a combination of CBT and pharmacotherapy, based on recommendations set forth by the 2016 Canadian Network for Mood and Anxiety Treatments (CANMAT) guidelines.2,8–10 For adults with mild major depressive disorder, usual care was no psychological therapy, and for those with moderate to severe major depressive disorder, usual care was pharmacotherapy. Pharmacotherapy was initiated with the lowest daily dose of sertraline, in accordance with the 2016 CANMAT guidelines71,84–87 and clinical practice (as established through expert consultation).
Table 3:
Interventions and Comparators Evaluated in the Primary Economic Model
| Intervention | Comparator | Patient Population |
|---|---|---|
|
Usual care
|
|
|
Usual care
|
|
|
Usual care
|
|
|
Usual care
|
|
Abbreviations: CBT, cognitive behavioural therapy; MDD, major depressive disorder.
Outcomes of Interest
-
Effectiveness outcomes
∘ Number of recurrent events
∘ Number of deaths as a result of suicide
∘ Number of hospitalizations
∘ Life-years (overall survival)
∘ QALYs
Direct medical costs
-
Incremental cost-effectiveness and incremental cost-utility ratios; the ICER is given by the difference in mean expected costs (i.e., the incremental cost) between 2 compared strategies divided by the difference in mean expected outcomes (i.e., the incremental effect) between these strategies
∘ Cost per life-year saved
∘ Cost per QALY gained
Discounting and Time Horizon
Following the 2017 CADTH guidelines, we applied an annual discount rate of 1.5% to both costs and QALYs in the base case analysis.80 We used a 5% discount rate in the sensitivity analysis. All costs are expressed in 2017 Canadian dollars.97 The time horizon for the base case analysis was 5 years. Due to the episodic nature of major depressive disorder, we deemed a 5-year time horizon was long enough to capture both the initial and downstream costs associated with the management of newly diagnosed and recurrent noncomplex major depressive disorder.
Model Structure
We developed a state-transition (Markov) probabilistic microsimulation (individual-level) model to evaluate CBT treatment options for a hypothetical cohort of women and men aged 18 years and older diagnosed with a first episode of major depressive disorder. Our mathematical model simulated the clinical course of major depressive disorder by severity of the initial episodes in each of the 1,000 hypothetical adult patients (Figure 3). The initial age of the hypothetical patients ranged between 18 and 75 years (mean = 33 years) and was separately drawn for each individual from a truncated normal distribution. We tracked overall survival, quality-adjusted survival, number of recurrent episodes, number of hospitalizations, number of deaths as a result of suicide, and costs over the first 5 years following a person's diagnosis of major depressive disorder in the base case, and over longer time frames in scenario analyses (i.e., 10 years, 20 years, and lifetime or until age 100 years).
Figure 3: Model Structure.
Abbreviation: MDE, major depressive episode.
This figure depicts an individual-level (microsimulation) Markov model that includes 11 health states, each represented by an oval, reflecting the course of mild or moderate to severe major depressive disorder. The simulation starts with a hypothetical patient aged between 18 and 75 years (age is drawn from a distribution) with a first mild or moderate to severe major depressive episode. In each 1-week cycle, a patient has a chance to move among health states. Death is an absorbing Markov health state. The model accounts for the age of major depressive disorder onset, counts the number of recurrent events, and modifies the risk of future major depressive episodes and changes in treatment accordingly. It takes into account the probability of death as a result of suicide according to the severity of disease and the probability of hospitalization in the complex depression health state. Transfer to the complex depression health state depends on the number of prior major depressive episodes (n ≥ 3). “p_dropout” denotes the probability of dropping out in the acute-phase states for patients with either a mild or moderate to severe major depressive episode; “p_well” and “p_complex” denote the probabilities of transferring to the well or complex depression health states, respectively, after dropping out in the acute phase; “p_relapse” denotes the probability of relapse and is related to a change in health state (e.g., from mild to moderate major depressive disorder) and change in treatment; “p_no response” in the maintenance phase for a patient with moderate or severe major depressive disorder triggers an increase in dose of antidepressant or a switch from sertraline to venlafaxine; “p_recurrence” denotes the probability of recurrence modelled in different health states, with “n_MDE” denoting a tracker variable that counts a number of recurrent major depressive episodes.
According to clinical guidelines, the course of major depressive disorder consists of the initial phases (i.e., the acute and continuation phases, each lasting approximately 3 months), during which response and relapse are monitored and the goal is to achieve remission, and the maintenance phase (lasting approximately 6 to 24 months, with an average 9 to 12 months), during which full recovery can be established or recurrence of a full major depressive episode can occur.2,8–10 According to the DSM-5, relapse is a new episode of major depressive disorder that occurs once a person has achieved remission during the continuation phase. In contrast, recurrence is a new episode of major depressive disorder that occurs in the maintenance phase after a person has achieved a period of remission including at least 2 months with no significant symptoms.2,8–10 Since relapse and recurrence affect the risk of experiencing another major depressive episode and the potential need for changes to treatment,84,86 a distinction between the initial and maintenance phases is required for modelling purposes.
Therefore, we used a short weekly cycle to monitor changes in the progression of disease and adequately reflect what is being done in current clinical practice:
Dropout (and its consequences) during the first months of treatment
Changes in disease progression or distinguishing relapse from recurrence
Changes in initial disease severity from mild to moderate or severe and the consequent addition of pharmacotherapy
Response to CBT or pharmacotherapy over the first months following a diagnosis of a major depressive episode or later, as well as subsequent changes in pharmacotherapy (i.e., an increase in dosage or a medication switch) when there is no improvement in symptoms or if relapse occurs
As presented in Figure 3, the model simulates the course of major depressive disorder through a series of transitions among 11 different Markov health states:
Health state 1: Major depressive episode, acute phase, mild disease
Health state 2: Major depressive episode, acute phase, moderate to severe disease
Health state 3: Major depressive episode, continuation phase, mild disease
Health state 4: Major depressive episode, continuation phase, moderate to severe disease
Health state 5: Major depressive episode, maintenance phase, mild disease
Health state 6: Major depressive episode, maintenance phase, moderate to severe disease
Health state 7: Recurrent major depressive episode, mild disease
Health state 8: Recurrent major depressive episode, moderate to severe disease
Health state 9: Well, no disease
Health state 10: Complex, treatment-resistant depression
Health state 11: Absorbing health state, death
During each 1-week cycle, patients may stay within a single health state or move among health states. Note, however, that once in health state 11, death, a patient can no longer transition to another state.
The initial depression-phase health states are the acute phase (12 weeks), the continuation phase (12 weeks), and the maintenance phase (up to 24 weeks), during which treatment may be applied, and response, remission, relapse, and recurrence are monitored. These initial health states are categorized by the initial severity of the major depressive episode as mild or moderate to severe, which allows for the possibility of changes in the severity of the initial episode during the acute and continuation phases. It also allows for the consequent addition of pharmacotherapy to CBT for patients initially diagnosed with mild major depressive disorder who progress to moderate or severe and for the dose of sertraline to be increased from 50 mg/day to 100 mg/day in patients whose symptoms are not improving (no response). Patients who do not respond well to an increased dose of sertraline are switched to venlafaxine (75 mg/day), as per expert consultation and the 2016 CANMAT guidelines.84
The frequency of disease progression monitoring (by a general practitioner or psychiatrist) depends on the initial disease severity; in general, monitoring occurs every 2 weeks in the first 4 months and monthly thereafter for the remainder of the first year after a diagnosis of major depressive disorder.
In the first 3 months (i.e., during the acute phase), a hypothetical patient has a chance of dropping out, after which they have a chance of either recovering (transferring to the well health state) or deteriorating (either committing suicide or transferring to the complex depression health state).
If a patient achieves full remission and remains stable during the maintenance phase, they enter the well health state, in which patients are considered to remain stable (without depression and receiving no treatment but having 2 follow-ups a year with a general practitioner).
A patient has a chance of experiencing a recurrent episode from any of the following health states:
The maintenance phase
The well health state (i.e., stable, without depression, and receiving no treatment but having regular check-ups with a general practitioner)
-
One of 2 recurrent health states (mild or moderate to severe):
∘ If recurrence occurs during a maintenance-phase health state, the patient directly enters the recurrent, moderate to severe health state and begins a new course of CBT combined with pharmacotherapy
∘ If recurrence occurs while in the well health state, the patient enters either the recurrent, mild health state or the recurrent, moderate to severe health state (with a different probability of entering each) and undergoes the same treatment pathway as a newly diagnosed patient (i.e., CBT only in the mild health state or CBT combined with pharmacotherapy in the moderate to severe health state)
In line with the literature findings, we modelled the effects of prior major depressive episodes and the age at disease onset on the risk of episode recurrence. We also assumed that a patient could have a maximum of 2 recurrent major depressive episodes before being considered to have complex or treatment-resistant depression, at which point they would be transferred into the complex depression state, which accounts for hospitalization and secondary psychiatric inpatient care.
Finally, each week, based on the lifetime probabilities of Ontario's population, a patient has a chance of dying from all causes from any of the 10 modelled health states.
Main Assumptions
The major structural model assumptions were as follows:
Dropout occurred in the first 3 months of treatment only; this assumption was supported by expert consultation and also extensively tested in the sensitivity analysis
Patients could experience a maximum of 2 major depressive episode recurrences, after which they would enter the complex depression health state and be considered for other type of treatment and secondary psychiatric care. This assumption was supported by clinical guidelines,71,84,86,87 the literature,98 and Health Quality Ontario's Major Depression: Care for Adults and Adolescents quality standard.95 This modelling assumption also aligned with our research objective to determine if the use of structured CBT represents good value for the management of non-treatment resistant major depressive disorder
CBT was provided in the same way for both incident (first) and recurrent major depressive episodes, according to current clinical practice (as established through expert opinion)
The efficacy of individual and group CBT was equal among different types of provider
Individuals who attempted suicide ended their lives
If patients were diagnosed with both major depressive disorder and generalized anxiety disorder, the primary diagnosis was major depressive disorder, and patients were treated accordingly with CBT (14 sessions)
For patients with generalized anxiety disorder alone, the scenario analysis examined the cost-effectiveness of treatment consisting of the same medications used for major depressive disorder but with 10 (rather than 14) sessions of CBT (number of sessions determined based on expert consultation)
Monitoring of the disease progression over time was modelled conservatively in the base case analysis (assuming full treatment adherence and no loss at follow-up visits with a psychiatrist or general practitioner); we checked this assumption in a scenario analysis
Clinical Outcome and Utility Parameters
We used a number of different input parameters to populate the model. These parameters were used to describe the natural history and clinical course of a newly diagnosed or recurrent major depressive episode, including factors affecting the risk of recurrence (e.g., age at disease onset, number of prior episodes), changes in the severity of initial disease (mild to severe major depressive disorder) and consequent changes in treatment options following a transition from mild to moderate or severe disease. To estimate the cost-effectiveness of CBT versus usual care, we populated the model with parameters related to the efficacy of CBT, health state utilities, and costs.
Natural History
To model the natural history of major depressive disorder, we used the literature sources and data from current clinical practice provided through expert consultation (Table 4). The distributions of mild versus moderate to severe cases of major depressive disorder were based on 2 studies.74,99 For newly diagnosed major depressive disorder, we used data from a modelling study by Ferrari at al, which examined the burden of major depressive disorder globally and meta-analyzed the proportions of national U.S., UK, and Australian epidemiologic studies conducted in general populations.74 For recurrent disease, we used data from a large cohort study (the Netherlands Mental Health Survey and Incidence Study [NEMESIS]) that examined the recurrence of major depressive disorder over 20 years and provided a distribution of major depressive disorder by disease severity in people with recurrent disease.99
Table 4:
Input Parameters Associated With the Natural History of Major Depressive Disorder: Probabilities and Risks
| Model Parameter | Mean | Distribution | Source |
|---|---|---|---|
| Probabilities/Rates | |||
| Probability of MDD, by disease severity, no prior episode: | NA | Ferrari et al, 201374 | |
| Mild MDD | 0.68 | ||
| Moderate to severe MDD | 0.32 | ||
| Probability of MDD, by disease severity, with prior episode: | NA | Hardeveld et al, 201399 | |
| Mild MDD | 0.24 | ||
| Moderate to severe MDD | 0.76 | ||
| Probability of dropout, acute phase: | NA | Koeser et al, 201569 | |
| CBT only | 0.18 | ||
| CBT plus pharmacotherapy | 0.23 | ||
| Pharmacotherapy only | 0.30 | ||
| No treatment | 0.29 | ||
| Probability of being not well after dropout | 0.33 | Assumption, expert consultation | |
| Probability of no response, acute phase | NA | Koeser et al, 201569 | |
| CBT only | 0.23 | ||
| CBT plus pharmacotherapy | 0.18 | ||
| Pharmacotherapy only | 0.70 | ||
| Probability of response (no relapse), continuation phase | NA | Koeser et al, 201569 | |
| CBT only | 0.69 | ||
| CBT plus pharmacotherapy | 0.75 | ||
| Pharmacotherapy only | 0.70 | ||
| No treatment | 0.43 | ||
| Annual rate of recurrence, year 1, maintenance phase | 0.15 | NA | Eaton et al, 2008100 |
| Annual rate or recurrence, long-term | NA | Eaton et al, 2008100 | |
| Year 2 | 0.20 | ||
| Year 4 | 0.75 | ||
| Year 5 | 0.70 | ||
| Year 10 | 0.50 | ||
| Annual rate or recurrence, long term, after 6 months of remissiona | NA | Hardeveld et al, 201399 | |
| Year 1 | 0.025 | ||
| Year 2 | 0.045 | ||
| Year 5 | 0.13 | ||
| Year 10 | 0.23 | ||
| Year 15 | 0.23 | ||
| Year 20 | 0.42 | ||
| Rate of hospitalization | 0.10 | NA | Health Quality Ontario 201695 |
| Background rate of death | Ontario life tables | NA | Statistics Canada 2011104 |
| Rate of death by suicide | NA | Khan et al, 2003103; Khan and Schwartz 2007102 | |
| General population | 0.000166 | ||
| Patients with depression | 0.001 | ||
| Patients with chronic/complex depression | 0.0024 | ||
| Risks | Risk Ratio (95% CI) | Distribution | Source |
| Relative risk of recurrent MDD, by age of disease onset, for each additional year | 0.96 (0.93–0.97) |
Normalb (log-odds ratio) |
Eaton et al, 2008100 |
| Relative risk of recurrent MDE, for each additional episode | 1.18 (1.06–1.31) |
Normalb (log-odds ratio) |
Mueller et al, 1999101 |
Abbreviations: CBT, cognitive behavioural disorder; CI, confidence interval; MDD, major depressive disorder; MDE, major depressive episode; NA, not applicable.
Used in sensitivity scenario analysis only.
Distributions assigned in probabilistic sensitivity analysis.
The probabilities of dropout and response to CBT only or in combination with pharmacotherapy were based on meta-analyses conducted within the most recent UK modelling analysis in people with moderate to severe major depressive disorder.69 After dropout, major depressive disorder could resolve on its own or become more severe; complex depression could end with suicide.
In the base case analysis, rates of recurrence were based on 10-year survival curves using data from a large U.S. prospective population-based cohort study with 23 years of follow-up, which included 1,831 participants with first or recurrent episodes.100 In the sensitivity scenario analysis, we used the rate of recurrence over 20 years reported in the NEMESIS study.99 Based on literature findings and expert opinion, we modelled recurrence risks as decreasing with each additional year of age at onset (RR: 0.96, 95% CI: 0.93–0.99)100 and as increasing with each prior major depressive episode (RR: 1.18, 95% CI: 1.06–1.31).101 After a third recurrence, a patient would enter the complex depression state. In this state, the hospitalization rate was modelled using recently published Ontario data.95
Lastly, our model accounted for age-dependent background mortality in Ontario and also for differences in suicide rate based on the severity of major depressive disorder (Table 4). Suicide rates were based on 2 U.S. Food and Drug Administration analyses of clinical trial data.102,103
Intervention Effects
The clinical review determined the efficacy of CBT. Here, we briefly describe the studies that provided the input parameters for our base case and scenario analyses (Table 5).
Table 5:
Summary Efficacy Estimates Used in the Economic Model
| Model Parameter | Relative Risk (95% CI) | Distribution | Source |
|---|---|---|---|
| Risk of recurrence, MDD: CBT only vs. no treatment |
0.68 (0.53–0.76) |
Normal (log-odds ratio) |
Biesheuvel-Leliefeld et al, 201529 |
| Risk of recurrence, MDD: CBT plus pharmacotherapy vs. pharmacotherapy only |
0.94a (0.72–1.21) |
Normal (log-odds ratio) |
Amick et al, 201536 |
| Risk of recurrence, MDD: Individual CBT vs. group CBT |
0.78b (0.69–0.93) |
Normal (log-odds ratio) |
Churchill et al, 200122 |
| Risk of recurrence, GAD: CBT only vs. no treatment |
0.67c (0.65–0.68) |
Normal (log-odds ratio) |
Cuijpers et al, 201620 |
| Risk of recurrence, MDD: Interpersonal therapy only vs. no treatment |
0.41 (0.27–0.63) |
Normal (log-odds ratio) |
Biesheuvel-Leliefeld et al, 201529 |
| Risk of recurrence, second-generation antidepressant, sertraline | 0.80 (0.69–0.93) |
Normal (log-odds ratio) |
Cipriani et al, 2009106 |
Abbreviations: CBT, cognitive behavioural therapy; CI, confidence interval; GAD, generalized anxiety disorder; MDD, major depressive disorder.
Recalculated from the reported relative risk of 1.06 (95% CI: 0.82–1.38).
Relative risk estimated from the odds ratio after accounting for a mean baseline probability of major depressive episode in the placebo arm of 0.57.107
Relative risk calculated from Hedge's g statistic, using established methods after adjusting for baseline rate of event.107
The efficacy of CBT or interpersonal therapy versus that of usual care was derived from a systematic review of 16 randomized controlled trials conducted by Biescheuvel-Leliefeld et al.29 Usual care was defined as routine clinical management, assessment only, no treatment, or wait list and corresponds to our model's “usual care” arm in patients with mild major depressive disorder. This was a recent systematic review, appraised as being of very good methodological quality (see clinical review); moreover, it examined major depressive disorder recurrence among important clinical outcomes.
We established the efficacy of CBT combined with pharmacotherapy (i.e., sertraline as first-line therapy) based on a recent systematic review by Amick et al, which we determined to be of very good methodological quality.36,105 The authors combined data from 3 randomized controlled trials to determine the efficacy of second-generation antidepressants versus a combination of second-generation antidepressants and CBT on achieving full remission in adults with major depressive disorder. We established the efficacy of second-generation antidepressants from a systematic review and network meta-analysis by Cipriani et al, which included 117 randomized controlled trials that compared the efficacies of 12 second-generation antidepressants on major depressive disorder.106
We derived the difference in the effects of individual versus group CBT from a 2001 systematic review by Churchill et al that evaluated major depressive episode recurrence in 6 randomized controlled trials.22 To estimate a risk ratio, we adjusted the reported odds ratio (1.98, 95% CI: 1.11–3.54) using the mean probability of major depressive episode that was calculated from the control arm data reported in a systematic review of randomized controlled trials by Williams et al.107
We based the efficacy of CBT versus usual care for generalized anxiety disorder on a systematic review published in 2016, which meta-analyzed reductions in mean generalized anxiety disorder symptom scores from 31 studies and reported a Hedge's g statistic of 0.80 (95% CI: 0.67–0.93).20 As this was the only clinical outcome reported in the study, we assumed that it represented remission in patients with generalized anxiety disorder, and we recalculated the risk ratio using the recommended method.108
Finally, we accounted for a possible reduction in the effect of CBT owing to publication bias, as suggested by a methodological study that analyzed the results of 61 grants funded by the National Institutes of Health examining the effects of psychological treatments on major depressive disorder published between 1972 and 2008 (see Table 8, Analysis).54
Table 8:
Cost Calculations Used in Scenario Analysis: CBT Provided by GP as Individual or Group Therapy
| CBT Provided by GP | OHIP Codea: Number of Visits | Unit Cost ($) | Unit Time (min.) | Length of CBT Session (min.) | Total Cost of CBT Sessions ($) |
|---|---|---|---|---|---|
| Individual therapy, first 3 sessions | K013: 3 | 62.75 | 30 | 60 | 376.50 |
| Individual therapy, sessions 4–14 | K033: 11 | 38.15 | 30 | 60 | 839.30 |
| Group therapy, for 6–12 people, applying a ratio of 2.77 | K040: 3 | 22.58 | 30 | 120 | 271.00 |
| Group therapy, for 6–12 people, applying a ratio of 2.77 | K041: 11 | 13.96 | 30 | 120 | 614.42 |
Abbreviations: CBT, cognitive behavioural therapy; GP, general practitioner; OHIP, Ontario Health Insurance Plan Schedule of Benefits and Fees.
All OHIP codes derived from Ministry of Health and Long-Term Care 2015.117
Health State Utilities
We specified a quality-of-life utility (weight) for each health state to calculate quality-adjusted life-years (QALYs). A QALY is a measure that jointly accounts for changes in both quantity and quality of life (morbidity).109 A utility is a measure of health-related quality of life and reflects the strength of preference for specified health states. By convention, utilities are anchored on death and best possible health (death is assigned a utility weight of 0, and perfect health is assigned a utility weight of 1).109 The value of a QALY for a certain health state is calculated by multiplying time spent in that health state with the utility assigned to that health state (e.g., 1 year of untreated major depressive disorder with a utility weight of 0.7 equals a QALY of 0.7).
The utilities used in our analysis are presented in Table 6. We derived the majority of these using the standard gamble method.110–113 A 2014 systematic review by Mohiuddin and Payne examined 35 studies and meta-analyzed the utility values elicited in adults with major depressive disorder.110 We based our utility values for untreated depression (categorized by severity) on the values presented in this study. For the “continuation” and “maintenance” Markov health states, we used the treatment-related utility values elicited from a UK study of 457 adults with major depressive disorder and generalized anxiety disorder receiving a psychological therapy114 or from a study of 70 North American adults undergoing pharmacotherapy with imipramine.111
Table 6:
Health State and Intervention Utilities Used in the Economic Model
| Model Parameter | Mean (SD) | Distribution | Source |
|---|---|---|---|
| Utilities | |||
| Acute phase, untreated new MDD | Beta | Mohiuddin and Payne, 2014110 | |
| Mild MDE | 0.69 (0.14) | ||
| Moderate to severe MDE | 0.52 (0.28) | ||
| Past MDD | Beta | Schaffer et al, 2002112 | |
| Mild MDE | 0.79 (0.28) | ||
| Moderate to severe MDE | 0.67 (0.36) | ||
| CBT-treated MDD | Fixed | King et al, 2000114 | |
| 4 months | 0.85 (NR) | ||
| 12 months | 0.85 (NR) | ||
| Pharmacotherapy only–treated MDD | 0.63 (0.19) | Beta | Revicki and Wood, 1998111 |
| Normal health, well health state | 0.94 (0.03) | Beta | Lenert et al, 2000113 |
| Complex depression state, with treatment, nonhospitalized | 0.52 (0.29) | Beta | Mann et al, 2009115; Vallejo-Torres et al, 2015116 |
| Complex depression state, severe phase, hospitalized | 0.34 (0.02) | Beta | Mann et al, 2009115; Vallejo-Torres et al, 2015116 |
Abbreviations: CBT, cognitive behavioural therapy; MDD, major depressive disorder; MDE, major depressive episode; NR, not reported; SD, standard deviation.
We accounted for decreases in health-related quality of life owing to prior major depressive episodes. Thus, in the 2 recurrent major depressive episode Markov states (mild and moderate to severe), we used utility weights determined for Canadian patients with past mild or moderate to severe major depressive episodes.112 The utility value during the acute phase of a recurrent, mild or recurrent, moderate to severe major depressive episode (< 6 months) was a product of the weights assigned for the corresponding severity levels of the past and new episodes (e.g., annual utility for the recurrent, moderate to severe health state: 0.52 × 0.67).
In the Markov well health state, patients were assumed to be stable and not receiving treatment. Lenert et al conducted a mapping study using a sample of 295 patients with major depressive disorder to provide the standard gamble utility weights for those who are “near normal health.”113
In the complex depression health state, we assigned the weights elicited in 114 patients in the United Kingdom with severe major depressive disorder in the acute phase of treatment.115,116 During the event of hospitalization, we assigned a one-time disutility elicited from patients with severe, treatment-resistant major depressive disorder at high risk of suicide and hospitalization.115,116
Cost Parameters
We estimated the direct medical costs associated with the model strategies using the cost estimates presented in Table 7.
Table 7:
Costs Used in the Economic Modela: Interventions, Usual Care, Follow-Ups, Complex Depression, and Hospitalization
| Model Parameter | Mean, $ (SE) | Distribution | Source |
|---|---|---|---|
| Costs of providing CBT, per week | |||
| Initial assessment, one-time costs, total: | 223.35 (55.84) |
Gamma | |
| GP referral | 62.75 | OHIP code K005117 | |
| Assessment by psychiatrist or psychologist | 80.30 | OHIP code K197117 | |
| CBT provided by psychiatrist, weekly | Gamma | ||
| Individual session (1 hour/week) | 160.60 (40.15) |
OHIP code K197117 | |
| Group session (2 hours/week) | 57.80 (14.45) |
OHIP code K205117 | |
| CBT provided by GP, weeklyb | Gamma | ||
| Individual session (1 hour/week) | 86.84 (21.71) |
OHIP codes K013 (first 3 sessions) and K033 (sessions 4–14)117 | |
| Group session (2 hours/week) | 63.24 (15.81) |
OHIP codes K040 (first 3 group sessions) and K041 (sessions 4–14)117 | |
| CBT provided by nonphysician, weeklyc | Gamma | Expert consultation, literature118–121: annual salary of $130,000 plus 30% benefits123,c | |
| Individual session (1 hour/week) | 101.93 (25.48) |
||
| Group session (2 hours/week) | 20.93 (5.10) |
||
| Costs of providing CBT, per week | |||
| CBT provided by nonphysician, weeklyb | Gamma | Expert consultation, literature118–121: annual salary of $130,000 plus 17% benefits122,c | |
| Individual session (1 hour/week) | 86.24 (21.56) |
||
| Group session (2 hours/week) | 17.24 (4.31) |
||
| CBT provided by nonphysician, weeklyb | Gamma | Expert consultation, literature: annual salary of $110,000 plus 30% benefits122,c | |
| Individual session (1 hour/week) | 91.73 (22.93) |
||
| Group session (2 hours/week) | 18.35 (4.59) |
||
| CBT provided by nonphysician, weeklyb | Gamma | Expert consultation, literature: annual salary of $110,000 plus 17% benefits122,c | |
| Individual session (1 hour/week) | 77.62 (19.40) |
||
| Group session (2 hours/week) | 15.52 (3.88) |
||
| Costs of pharmacotherapy,d per week | |||
| Sertraline, 50 mg/day | 6.85 | Fixed | ODB125; Kolber 2014130 |
| Sertraline, 100 mg/day | 7.44 | Fixed | ODB125; Kolber 2014130 |
| Venlafaxine, 75 mg/day | 5.93 | Fixed | ODB125; Kolber 2014130 |
| Costs of follow-up, per week | |||
| CBT only (mild MDD) | 20.85 (5.21) |
Gamma | Calculated based on OHIP codes K005 and K198117; details provided in text |
| CBT plus pharmacotherapy (moderate to severe MDD) | 33.20 (8.30) |
Gamma | Calculated based on OHIP codes K005 and K198117; details provided in text |
| Pharmacotherapy, usual care (moderate to severe MDD) | 33.20 (8.30) |
Gamma | Calculated based on OHIP codes K005 and K198117; details provided in text |
| No treatment, usual care (mild MDD) | 7.24 (1.71) |
Gamma | Calculated based on OHIP codes K005 and K198117; details provided in text |
| Costs: Complex depression | |||
| Responders, weekly | 163.78 (40.92) |
Gamma | Health Quality Ontario 2016127 |
| Nonresponders, weeklyb | 222.47 (55.61) |
Gamma | Health Quality Ontario 2016127 |
| One-time costs of hospitalization (per 10 days) | 5,422.88 (1,355.72) |
Gamma | Bereza et al,129 2012 |
| Costs: Well health state, per week | |||
| Follow-up by GP (2 visits per year) | 2.41 (0.60) |
Gamma | Calculated based on OHIP code K005117 |
Abbreviations: CBT, cognitive behavioural therapy; GP, general practitioner; ODB, Ontario Drug Benefit Program; OHIP, Ontario Health Insurance Plan Schedule of Benefits and Fees; MDD, major depressive disorder; SE, standard error.
Original nondiscounted costs in 2017 Canadian dollars, estimated per weekly cycle; standard error based on an assumption that the mean costs vary by ± 25%.
Used in probabilistic sensitivity scenario analyses.
Labour costs after applied salary adjustment for a full-time professional of 1,658 hours per year.
Costs of drugs include a dispensing fee of $10.22 and a mark-up of $1.71 for 30-day use.130
The costs of CBT treatment consisted of the following:
Costs of the initial assessment: the cost of the visit to a general practitioner to obtain a referral plus the cost of the visit during which a psychiatric assessment is conducted by a psychiatrist or psychologist (see unit costs in Table 7)
Costs of providing CBT by a publicly funded, regulated health care provider
Costs of follow-up during treatment
In the base case analysis, we took a conservative approach and used the unit costs associated with the highest applied hourly rates estimated for publicly funded nonphysician professionals on salary and the fee-for-service physician costs claimed by a psychiatrist. In addition, we chose a psychiatrist to represent the physician force trained for psychotherapy and able to provide structured CBT. However, in the scenario analysis, we tested an assumption that a trained general practitioner could provide structured CBT, including it within the fee-for-service Ontario Health Insurance Plan (OHIP) codes assigned for counselling services (OHIP codes K013, K040).117
The structured face-to-face approach to CBT consists of 14 sessions delivered as individual therapy (1 hour a week to 1 person) or as group therapy (2 hours a week to a group of 12 people). Therefore, we calculated the cost of 1 course of CBT provided by a nonphysician or physician as the product of the number of sessions (14) and the applied hourly salary (for nonphysicians) or fee-for-service costs (for physicians) adjusted for the time spent on a session (1 hour for individual versus 2 hours for group).
Next, we explain the calculations of the labour costs for nonphysicians after adjustment for clinical work.
We based the salary ranges of publicly funded, regulated therapists (i.e., nurses, occupational therapists, psychologists, psychotherapists, and social workers) on data from literature118–121 and information provided through expert consultation. The average annual salary for publicly funded psychotherapists ranges between $110,000 and $130,000, with benefits ranging between 17%122 and 30%.123 To estimate the labour costs associated with clinical activities, we calculated an applied hourly salary. Applied cost recognizes that salaried clinicians spend time on nonpatient activities, so less than 100% of a clinician's time accounts for clinical work.124 It is recognized that the applied rate (i.e., the ratio of applied time to total time) is 85% for medical staff. Using this applied rate, we calculated applied hourly salaries for publicly funded therapists for the base case and scenario analyses. A similar number of hours per year (i.e., 1,657 hours per year for a full-time nurse) has been previously used in labour cost estimations.124 The following provides an example of our calculations:
A full-time equivalent (FTE) works 1,950 hours per year (assuming 7.5 hours per day, 5 days per week, and 52 weeks per year)
Using the applied rate of 85%, the applied time is thus 1,950 × 0.85 = 1,658 hours annually
Given an annual salary of $130,000 with 30% benefits (for a total of $169,000 per year), the applied hourly salary is thus $169,000 ÷ 1,658 = $101.93
We based the costs of follow-up by physicians on the fee-for-service schedule and number of visits. As per the 2016 CANMAT guidelines84 and expert consultation, the number of follow-up visits depended on the severity of a patient's major depressive disorder:
Patients diagnosed with mild major depressive disorder and receiving CBT only were assumed to have follow-up visits with a general practitioner every 2 weeks for the first 4 months and then monthly until the end of 1 year (for a total of 16 visits). We assumed that the consultation with a psychiatrist to update the initial treatment plan occurred once, at the completion of CBT therapy (at 4 months)
Patients initially diagnosed with moderate to severe major depressive disorder treated with both CBT and pharmacotherapy or pharmacotherapy only were assumed to experience the same frequency of visits with a general practitioner, but to have more frequent consultations with a psychiatrist (once a month starting at month 4, for a total of 9 visits)
Patients diagnosed with mild major depressive disorder who initially received no treatment (usual care) were assumed to have monthly follow-up visits with a general practitioner for 6 months
We based drug costs on the costs assigned in the Ontario Drug Benefit program,125 after accounting for dispensing fees and markup costs, as suggested in the literature.126
We estimated the costs of complex depression from data reported in a Health Quality Ontario health technology assessment on the use of electroconvulsive therapy for the management of treatment-resistant depression.127 These estimates are within the range of published cost estimates for a high-cost mental health patient and were generated from Ontario health administrative data.128 We based the costs of hospitalization (estimating a 10-day period for this population) on data from a Canadian cost-effectiveness analysis by Bereza et al conducted in adults with generalized anxiety disorder.129
For the cost of follow-up in patients who are stable (i.e., those in the well health state), we assumed 2 check-ups a year with a general practitioner.
Finally, we tested how changing the frequency of follow-up (with psychiatrists and general practitioners) affected the cost-effectiveness results in a scenario analysis.
In the separate scenario analysis, we assumed that a general practitioner could provide CBT and estimated the costs of individual or group CBT using available OHIP codes (Table 8). However, there is no OHIP fee code for group therapy for 12 people when provided by a general practitioner. For the scenario of CBT delivered by a general practitioner as individual or group therapy, we thus calculated a ratio of 2.77 from differences in the fee-for-service costs between group psychotherapy for 2 people (OHIP code 208: $40.15117) and group psychotherapy for 6 to 12 people (OHIP code 205: $14.45117). We applied this ratio to the individual therapy costs to estimate the cost of group therapy, as shown in Table 8. In summary, we estimated the total cost of 14 individual CBT sessions conducted by a general practitioner to be $1,215.80, with a weekly cost of $86.84, and we estimated the total cost of 14 group CBT sessions conducted by a general practitioner to be $885.40, with a weekly cost of $63.24.
Analysis
We estimated all outcomes using probabilistic sensitivity analysis, as recommended by the 2017 CADTH economic evaluation guidelines80 and decision-modelling guidelines.131–134 Probabilistic sensitivity analysis is an advanced method that handles parameter (second-order) uncertainty and nonlinear relationships among model parameters (which are often present in Markov models).
Parameter uncertainty is handled by setting distributions for input model parameters (see Tables 4 to 7). We assigned distributions for input parameters and repeatedly sampled from those distributions (see Tables 4 to 7). For example, we specified the beta distribution for utilities, the normal distribution for the effect measure of treatment efficacy (i.e., the log-odds ratio), and the gamma distribution for costs. The probabilities of recurrence or death were modelled as time or age dependent. We simulated 1,000 trials, each of which included 1,000 patients, to obtain the mean expected costs and effects of the compared strategies. As it accounts for parameter and decision uncertainty, probabilistic sensitivity analysis generates more accurate estimates of the mean expected effects and mean expected costs than deterministic analysis, and these estimates are used to calculate the ICER.
The results of the probabilistic sensitivity analysis were presented in the cost-effectiveness plane by plotting simulated ICER values. The meaning of the ICER depends on the quadrant(s) of the cost-effectiveness plane in which the ICER resides.131,135 A strategy is considered cost-effective if it is associated with greater expected effects and greater expected costs and if the ICER is below the maximum price that a decision-maker or society is willing to pay for an extra unit of effect.135,136 Although the value of the willingness-to-pay threshold remains controversial,137,138 we used a threshold of $50,000 per QALY gained139 and also examined a threshold of $100,000 per QALY gained. A strategy is considered cost-saving (i.e., below a given willingness-to-pay threshold) if it is associated with greater expected effects and lower expected costs. A strategy is considered dominated by another one if it is associated with lower or equal expected effects for higher or equal expected costs.136
We also used cost-effectiveness acceptability curves to graphically present uncertainty in the ICER.140 These curves show the probability of one alternative being cost-effectiveness over another across a range of willingness-to-pay thresholds ($0 to $100,000/QALY gained). We conducted 2 types of base case cost–utility analysis using the probabilistic sensitivity analysis method:
-
1
First, we compared each strategy with usual care, for three reasons:
There is no gold standard regarding the ideal CBT provider type in Ontario
There is limited access to psychotherapy in Ontario
It is possible that some patients may not be able to undergo group therapy and will be deprived from needed individual therapy (i.e., owing to health equity issues)
-
2
Second, we ranked strategies by costs and benefits, removed inefficient strategies (i.e., dominated strategies associated with equal benefits but greater costs), and determined the ICERs and the best, most cost-effective option in Ontario
Our sensitivity analysis consisted of 19 scenarios that were calculated using probabilistic sensitivity analysis. A description of all scenarios is presented in Table 9. For example, we examined the cost-effectiveness of interpersonal therapy (scenario 3), the change in cost-effectiveness estimates if the efficacy of CBT were reduced by 25% (scenario 4), and the change in cost-effectiveness estimates if the number of CBT sessions were only 6 (scenario 11). We used both ICER and incremental net benefit estimates to indicate the cost-effectiveness of the compared strategies. A positive incremental net benefit indicates that a strategy is cost-effective. For all scenarios, we assumed a willingness-to-pay threshold of $50,000 per QALY gained.
Table 9:
Sensitivity Analysis: Description of Structural and Parameter Assumptions in Probabilistic Sensitivity Analysis Scenarios
| Parameter/Assumption | Base Case Analysis | Scenario Analysis: Major Changes in Parameter Values or Assumptions |
|---|---|---|
| 1. Population | MDD and GAD | GAD only: efficacy of CBT and number of CBT sessions (n = 10) |
| 2. Initial disease severity | Patients with both mild and moderate to severe MDD | Patients with mild MDD only; patients with moderate to severe MDD only |
| 3. Efficacy of interpersonal therapy | RR for CBT: 0.68 (0.53–0.76) | RR for interpersonal therapy: 0.41 (0.27–0.63) |
| 4. Efficacy of CBT | See Table 5 | Reduction of efficacy by 25% |
| 5. Dropout | See Table 4, different among treatment options | 2 × base case probability; 0.5 × base case probability |
| 6. Probability of not being well after dropout | 0.33 | 2 × base case probability; 0.5 × base case probability |
| 7. Rate of recurrence | Table 5, Eaton 2008,100 10-year survival curves | Table 5, NEMESIS,99 20-year survival curves |
| 8. Rate of hospitalization | 0.10 | 2 × base case rate; 0.5 × base case rate |
| 9. Additional disutility owing to past MDD | Yes | No |
| 10. Utility of CBT treatment 10% lower | 0.85 | 0.77 |
| 11. Number of CBT sessions | 14 | Analysis 1: 6 Analysis 2: 20 |
| 12. Costs of physician-provided CBT | Conservative assumption: psychiatrist (data shown in Table 7) | GP (data shown in Table 7) |
| 13. Costs of nonphysician-provided CBT, salary-based FTE: 1,658 hours/year | Conservative assumption: salary of $130,000/year + 30% benefits (see Table 7) | 1: $130,000/year + 17% benefits 2: $110,000/year + 30% benefits 3: $110,000/year + 17% benefits |
| 14. Costs of CBT, 2 providers | Psychiatrist or highest applied salary for nonphysicians ($130,000/year + 30% benefits) | GP or lowest applied salary for nonphysicians ($110,000/year + 17% benefits) |
| 15. Direct medical costs | All costs | CBT-associated costs: assessment, CBT treatment, 1-year follow-up |
| 16. Costs of complex depression | Responders | Nonresponders |
| 17. Follow-up costs | Costs associated with biweekly visits for first 4 months, then monthly visits | Decrease in frequency of follow-up (owing to lack of compliance) by 25%, 50%, and 75% |
| 18. Discount rate | 1.5% | 5% |
| 19. Time horizon | 5 years | 1: 1 year 2: 2 years 3: 10 years 4: 20 years 5: Lifetime |
Abbreviations: CBT, cognitive behavioural therapy; FTE, full-time equivalent; GAD, generalized anxiety disorder; GP, general practitioner; MDD, major depressive disorder; RR, relative risk.
We conduced all analyses using TreeAge Pro 2017 (TreeAge Software, Williamstown, MA) and Excel 2013 (Microsoft, Redmond, WA).
Generalizability
The findings of this economic analysis are generalizable to outpatient adults with mild to severe major depressive disorder and/or generalized anxiety disorder, but they may not be generalized to adults with resistant and complex depression who are at high risk of suicide or are being treated with multiple and complex interventions. These findings may, however, be used to guide decision-making about the specific patient populations in Ontario addressed in the studies evaluated by Health Quality Ontario.
Expert Consultation
Throughout the development of this model, we sought expert consultation. The role of the expert advisors was to review the model structure and inputs to confirm that the information we used reasonably reflects the clinical context for major depressive disorder and generalized anxiety disorder in Ontario. However, the statements, conclusions, and views expressed in this report do not necessarily represent the views of the consulted experts.
Results
In sections below, we present the results of our primary economic evaluation: the base case and sensitivity analyses.
Base Case Analysis
Table 10 describes the differences in clinical outcomes among compared strategies assessed through the base case analysis. Tables 11 and 12 present the results of the cost–utility analysis.
Table 10:
Life Expectancy, Major Depressive Episode Recurrence, Death as a Result of Suicide, and Hospitalization Over 5 Years: Usual Care Versus CBT Strategies
| Strategy | Outcomes | |||
|---|---|---|---|---|
| Mean Life Expectancy (undiscounted survival), years (95% CrI) | Mean Number of Recurrent MDEs (95% CrI) | Mean Number of Deaths as a Result of Suicide, %a (95% CrI) | Mean Number of Hospitalizations, % (95% CrI) | |
| Usual care | 4.94467 (4.91; 4.97) |
2.46 (2.30; 2.63) |
1.81 (1.10; 2.80) |
14.57 (12.30; 16.80) |
| Group CBT by nonphysician | 4.94618 (4.91; 4.97) |
2.42 (2.27; 2.57) |
1.81 (1.10; 2.70) |
13.16 (11.10; 15.30) |
| Group CBT by physician | 4.94618 (4.92; 4.97) |
2.42 (2.27; 2.57) |
1.81 (1.10; 2.70) |
13.16 (11.10; 15.30) |
| Individual CBT by nonphysician | 4.94745 (4.92; 4.97) |
2.37 (2.23; 2.52) |
1.79 (1.10; 2.70) |
12.95 (10.90; 15.10) |
| Individual CBT by physician | 4.94745 (4.91; 4.97) |
2.37 (2.23; 2.52) |
1.79 (1.10; 2.70) |
12.95 (10.90; 15.10) |
Abbreviations: CBT, cognitive behavioural therapy; CrI, credible interval; MDE, major depressive episode.
Death as a result of suicide from all health states.
Table 11:
Cost–Utility Analysis of Individual or Group CBT Delivered by Different Providers Versus Usual Carea
| Strategy | Mean Costs, $ (95% CrI) | Mean QALYs (95% CrI) | Incremental Costsb, $ (95% CrI) | Incremental QALYsc (95% CrI) | ICER: Strategy vs. Usual Care, $/QALY gained |
|---|---|---|---|---|---|
| Usual care | 16,157.79 (9,936; 24,254) |
3.460 (2.56; 4.29) |
– | – | – |
| Group CBT by nonphysician | 16,558.54 (10,789; 24,079) |
3.568 (2.74; 4.33) |
400.75 (−1,177; 1,665) |
0.1079 (0.03;0.22) |
3,715 |
| Group CBT by physician | 17,962.64 (12,112; 25,316) |
3.568 (2.74; 4.33) |
1,804.85 (65; 3,516) |
0.1079 (0.03;0.22) |
16,729 |
| Individual CBT by nonphysician | 19,325.80 (13,669; 26,697) |
3.582 (2.76; 4.34) |
3,168.00 (889; 5,624) |
0.1222 (0.03; 0.25) |
25,914 |
| Individual CBT by physician | 21,468.77 (15,223; 29,621) |
3.582 (2.76; 4.34) |
5,310.98 (2,539;8,938) |
0.1222 (0.03; 0.25) |
43,443 |
Abbreviations: CBT, cognitive behavioural therapy; CrI, credible interval; ICER, incremental cost-effectiveness ratio; QALY, quality-adjusted life-year.
All costs in 2017 Canadian dollars. All costs and effects were discounted at 1.5%.
Incremental cost = average cost (strategy CBT) – average cost (strategy usual care).
Incremental effect = average effect (strategy CBT) – average effect (strategy usual care). Note: Results may appear incorrect because of rounding.
Table 12:
Cost–Utility Analysis: Individual or Group CBT After the Exclusion of Dominated Strategiesa
| Strategy | Mean Costs, $ (95% CrI) | Mean QALYs (95% CrI) | Incremental Costs, $b (95% CrI) | Incremental QALYsc (95% CrI) | ICER: $/QALY gained |
|---|---|---|---|---|---|
| Usual care | 16,157.79 (9,936; 24,254) |
3.460 (2.56; 4.29) |
|||
| Group CBT by nonphysician | 16,558.54 (10,789; 24,079) |
3.568 (2.74; 4.33) |
400.75 (−1,177; 1,665) |
0.1079 (0.03;0.22) |
3,715 |
| Individual CBT by nonphysician | 19,325.80 (13,669; 26,697) |
3.582 (2.76; 4.34) |
2,767.26 (1,179; 4,822) |
0.0144 (0.0001;0.04) |
192,618 |
Abbreviations: CBT, cognitive behavioural therapy; CrI, credible interval; ICER, incremental cost-effectiveness interval; QALY, quality-adjusted life-year.
All costs in 2017 Canadian dollars. All costs and effects were discounted at 1.5%.
Incremental cost = average cost (strategy individual CBT) – average cost (strategy group CBT).
Incremental effect = average effect (strategy individual CBT) – average effect (strategy group CBT).
Note: Results may appear incorrect because of rounding.
In terms of clinical outcomes, over a 5-year time horizon, individual CBT increased undiscounted survival (i.e., overall survival or life expectancy) by 0.00278 years (1.015 days) versus usual care, and group CBT increased undiscounted survival by 0.00151 years (0.55 days) versus usual care (see Table 10). Individual and group CBT decreased the number of recurrent major depressive episodes by 0.09 and 0.04, respectively, and reduced the probability of hospitalization by 1.62% and 1.41%, respectively.
In the cost-effectiveness analysis applying the incremental changes in these clinical outcomes and the incremental costs from Table 11, we found the following:
Group CBT provided by nonphysician therapists (vs. usual care) would be associated with the following costs: $10,019 to avoid 1 recurrent major depressive episode, $284 to avoid 1 hospitalization, and $729 to save 1 additional day of life
Individual CBT provided by nonphysician therapists (vs. usual care) would be associated with the following costs: $35,200 to avoid one recurrent major depressive episode, $1,956 to avoid one hospitalization, and $3,121 to save 1 additional day of life
1. Cost–Utility Analysis: All Cognitive Behavioural Therapy Strategies Versus Usual Care
As shown in Table 11, compared with usual care, all CBT strategies were associated with ICERs less than $50,000 per QALY gained. CBT provided as group therapy by a nonphysician was associated with the lowest ICER.
Compared with usual care, CBT provided as group therapy by a nonphysician was associated with an increased discounted survival of 0.11 QALYs (95% credible interval [CrI]: 0.03; 0.22) and increased discounted mean costs of $401 (95% Crl: −$1,177; $1,665), yielding an ICER of $3,715 per QALY gained. In contrast, CBT provided as individual therapy by a physician was associated with the increments in discounted effects of 0.12 QALYs (95% Crl: 0.03; 0.25) and discounted mean costs of $5,310 (95% Crl: $2,539; $8,938), yielding an ICER of $43,443 per QALY gained.
Compared with usual care, CBT provided either as group or individual therapy had high probabilities of cost-effectiveness for the majority of providers. At a $50,000/QALY threshold, these probabilities were 54.8% (individual CBT provided by a physician), 81.2% (individual CBT provided by nonphysicians), 92.7% (group CBT provided by physicians), and 99.5% (group CBT provided by nonphysicians). Individual CBT provided by physicians had an 87.8% likelihood of being cost-effective at the very high willingness-to-pay threshold of $100,000 per QALY. Figure 4 shows cost-effectiveness acceptability curves that graphically represent the probabilities of the examined CBT strategies being cost-effective (compared with usual care) over a wide range of willingness-to-pay thresholds.
Figure 4: Cost-Effectiveness Acceptability Curves: Examined CBT Strategies Versus Usual Care.
Cost-effectiveness acceptability curves graphically present the probability of the 4 examined CBT strategies being cost-effectiveness versus usual care (i.e., no CBT) across various willingness-to-pay thresholds on the x–y coordinate system. The x-axis shows the probability of cost-effectiveness (range: 0–1), and the y-axis shows various willingness-to-pay thresholds (range: $0–$100,000 per QALY gained).
2. Cost–Utility Analysis: Best-Ranked Cognitive Behavioural Therapy Strategies
In this analysis, we excluded the 2 dominated strategies from Table 11 (i.e., group and individual CBT provided by physicians), as these were associated with equal benefits but higher costs than the nonphysician-administered strategies. Table 12 ranks the 3 remaining strategies by increasing costs and shows that, of all 3 options, group CBT provided by nonphysicians is optimal, as this strategy provides good value for money at a very low willingness-to-pay threshold (e.g., $20,000/QALY).
As shown in Figure 5, there was little uncertainty regarding the cost-effectiveness of the group CBT strategy. Thus, in 745 of 1,000 simulations, group CBT provided by nonphysicians was associated with better clinical outcomes and greater costs than usual care, but at a willingness-to-pay threshold below $50,000 per QALY. Group CBT provided by nonphysicians was associated with greater QALYs and lower costs than usual care in 250 simulations (i.e., it was found to be dominant or cost-saving). This strategy was also associated with greater health benefits and costs, but at a threshold above $50,000 per QALY (i.e., it was found not to be cost-effective) in 4 of 1,000 simulations.
Figure 5: Scatter Plots of 1,000 Simulated Pairs of Incremental Costs and Effectiveness (QALYs) in the Cost-Effectiveness Plane: Group CBT Provided by Nonphysicians Versus Usual Care.
Abbreviations: CBT, cognitive behavioural therapy; ICER, incremental cost-effectiveness ratio; WTP, willingness-to-pay threshold ($).
All costs are in 2017 Canadian dollars and discounted at 1.5%. Effectiveness is expressed in quality-adjusted life years (QALYs). Negative QALYs indicate that the CBT strategy was associated with worse quality-adjusted survival, and negative costs indicate that the CBT strategy saved money relative to usual care. The diagonal grey line indicates a willingness-to-pay threshold of $50,000 per QALY. The incremental cost-effectiveness ratio ($3,715/QALY gained) is the slope of a straight line from the origin that passes through the (0.11 QALY, $400) coordinate. A 95% confidence ellipse covers 95% of the estimated joint density and was used to represent uncertainty around the incremental cost-effectiveness ratio estimated in the probabilistic sensitivity analysis.
In addition, compared with group CBT provided by nonphysicians, individual CBT provided by nonphysicians was associated with a small increase in discounted mean survival of 0.01 QALYs (95% CrI: 0.0001; 0.24) and a significant increase in discounted mean costs of $2,767 (95% Crl: $1,179; $4,822), consequently yielding a large ICER value of $192,618 per QALY gained. Uncertainty regarding the ICER was high at a willingness-to-pay threshold of $100,000 per QALY, as shown in Appendix 6 (Figure A1).
Sensitivity Analysis
We conducted 19 scenario analyses to examine parameter and structural model uncertainty and their effects on the robustness of our initial results. The ICER and incremental net benefit estimates for the scenarios are presented in Table 13, which presents cost–utility analysis results comparing each CBT strategy with usual care, and Table 14, which presents cost–utility analysis results comparing best-ranked strategies.
Table 13:
Sensitivity Scenario Analysis Results: CBT Strategies Versus Usual Carea
| Parameter/Assumption: a. Base Case Analysis b. Scenario Analysis |
Group CBT by Nonphysician vs. Usual Care ICER ($/QALY)/INBb > 0 or INB < 0 ($) | Group CBT by Physician vs. Usual Care ICER ($/QALY)/INB > 0 or INB < 0 ($) | Individual CBT by Nonphysician vs. Usual Care ICER ($/QALY)/INB > 0 or INB < 0 ($) | Individual CBT by Physician vs. Usual Care ICER ($/QALY)/INB > 0 or INB < 0 ($) |
|---|---|---|---|---|
| 1. Population | ||||
| a. Base case: MDD and GAD | a. 3,175/4,994 | a. 16,729/3,590 | a. 25,914/2,942 | a. 43,443/800 |
| b. Scenario: GAD only | b. 1,783/INB > 0 | b. 11,599/INB > 0 | b. 18,396/INB > 0 | b. 31,712/INB > 0 |
| 2. Initial disease severity | ||||
| a. Base case: Mild and moderate to severe MDD | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenarios: | b. | b. | b. | b. |
| (i) Mild MDD | (i) 1,973/INB > 0 | (i) 14,258/INB > 0 | (i) 23,371/INB > 0 | (i) 40,079/INB > 0 |
| (ii) Moderate to severe MDD | (ii) 8,839/INB > 0 | (ii) 23,828/INB > 0 | (ii) 32,952/INB > 0 | (ii) 52,615/INB < 0 |
| 3. Efficacy of interpersonal therapy | ||||
| a. Base case: CBT | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenario: Interpersonal therapy | b. Cost-saving/INB > 0 | b. 9,950/INB > 0 | b. 19,209/INB > 0 | b. 33, 671/INB > 0 |
| 4. Efficacy of CBT | ||||
| a. Base case: RR_CBT | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenario: 0.25 × RR_CBT | b. 7,404/INB > 0 | b. 23, 019/INB > 0 | b. 31, 455/INB > 0 | b. 51,409/INB < 0 |
| 5. Dropout | ||||
| a. Base case: see Table 4 | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenarios: | b. | b. | b. | b. |
| (i) 2 × base case probability | (i) 12,839/INB > 0 | (i) 28,636/INB > 0 | (i) 36,689/INB > 0 | (i) 56,912/INB < 0 |
| (ii) 0.5 × base case probability | (ii) Cost-saving/INB > 0 | (ii) 6,674/INB > 0 | (ii) 15,100/INB > 0 | (ii) 28,622/INB > 0 |
| 6. Probability of not being well after dropout | ||||
| a. Base case: 0.33 | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenarios: | b. | b. | b. | b. |
| (i) 2 × base case probability | (i) Cost-saving/INB > 0 | (i) Cost-saving/INB > 0 | (i) 7,582/INB > 0 | (i) 19,488/INB > 0 |
| (ii) 0.5 × base case probability | (ii) 9,391/INB > 0 | (ii) 24,444/INB > 0 | (ii) 33,610/INB > 0 | (ii) 53,400/INB < 0 |
| 7. Rate of recurrence | ||||
| a. Base case: Eaton 2008100 | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenario: NEMESIS99 | b. 7,035/INB > 0 | b. 22,863/INB > 0 | b. 34,575/INB > 0 | b. 56,344/INB < 0 |
| 8. Rate of hospitalization | ||||
| a. Base case: 0.10 | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenarios: | b. | b. | b. | b. |
| (i) 2 × base case rate | (i) 2,904/INB > 0 | (i) 15,931/INB > 0 | (i) 25,119/INB > 0 | (i) 42,665/INB > 0 |
| (ii) 0.5 × base case rate | (ii) 4,137/INB > 0 | (ii) 17,143/INB > 0 | (ii) 26,324/INB > 0 | (ii) 43,842/INB > 0 |
| 9. Additional disutility owing to past MDD | ||||
| a. Base case: Yes | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenario: No | b. 3,751/INB > 0 | b. 16,892/INB > 0 | b. 26,399/INB > 0 | b. 44,256/INB > 0 |
| 10. Utility associated with CBT treatment | ||||
| a. Base case: 0.85 | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenario: 0.765 | b. 6,489/INB > 0 | b. 29,211/INB > 0 | b. 41,226/INB > 0 | b. 69,113/INB < 0 |
| 11. Number of CBT sessions (N) | ||||
| a. Base case: N = 14 | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenarios: | b. | b. | b. | b. |
| (i) N = 6 | (i) 781/INB > 0 | (i) 8,360/INB > 0 | (i) 13,167/INB > 0 | (i) 23,392/INB > 0 |
| (ii) N = 20 | (ii) 7,539/INB > 0 | (ii) 27,659/INB > 0 | (ii) 42,648/INB > 0 | (ii) 69,761/INB < 0 |
| 12. Costs of physician-provided CBT | ||||
| a. Base case: Psychiatrist | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 25,914/INB > 0 |
| b. Scenario: GP | b. 3,175/INB > 0 | b. 18,690/INB > 0 | b. 25,914/INB > 0 | b. 21,806/INB > 0 |
| 13. Costs of nonphysician-provided CBT, salary-based | ||||
| a. Base case: $130,000/year, 30% benefits, FTE: 1,658 hours/year | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenarios: | b. | b. | b. | b. |
| (i) $130,000/year, 17% benefits | (i) 2,675/INB > 0 | (i) No change | (i) 21,296/INB > 0 | (i) No change |
| (ii) $110,000/year, 30% benefits | (ii) 3,129/INB > 0 | (ii) No change | (ii) 23,083/INB > 0 | (ii) No change |
| (iii) $110,000/year, 17% benefits | (iii) 2,139/INB > 0 | (iii) No change | (iii) 18,812/INB > 0 | (iii) No change |
| 14. Costs of CBT, 2 providers | ||||
| a. Base case: Psychiatrist or highest paid nonphysician | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 25,914/INB > 0 |
| b. Scenario: GP or lowest paid nonphysician | b. 2,133/INB > 0 | b. 18,690/INB > 0 | b. 18,812/INB > 0 | b. 21,806/INB > 0 |
| 15. Direct medical costs | ||||
| a. Base case: All treatment costs | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenario: CBT treatment costs | b. 16,763/INB > 0 | b. 29,778/INB > 0 | b. 39,095/INB > 0 | b. 56,624/INB < 0 |
| 16. Costs of complex depression | ||||
| a. Base case: Responders | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenario: Nonresponders | b. Cost-saving/INB > 0 | b. 12,485/INB > 0 | b. 21,629/INB > 0 | b. 39,158/INB > 0 |
| 17. Costs of follow-up | ||||
| a. Base case: 100%, regular visits | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenarios: Reduction of follow-up visits and costs by | b. | b. | b. | b. |
| (i) 25% | (i) 1,825/INB > 0 | (i) 14,840/INB > 0 | (i) 24,282/INB > 0 | (i) 41,812/INB > 0 |
| (ii) 50% | (ii) Cost-saving/INB > 0 | (ii) 12,950/INB > 0 | (ii) 22,651/INB > 0 | (ii) 40,180/INB > 0 |
| (iii) 75% | (iii) Cost-saving/INB > 0 | (iii) 11,060/INB > 0 | (iii) 21,019/INB > 0 | (iii) 38,547/INB > 0 |
| 18. Discount rate | ||||
| a. Base case: 1.5% | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenario: 5% | b. 4,058/INB > 0 | b. 17,154/INB > 0 | b. 26,323/INB > 0 | b. 43,910/INB > 0 |
| 19. Time horizon | ||||
| a. Base case: 5 years | a. 3,175/INB > 0 | a. 16,729/INB > 0 | a. 25,914/INB > 0 | a. 43,443/INB > 0 |
| b. Scenarios: | b. | b. | b. | b. |
| (i) 1 yearc | (i) 16,278/INB > 0 | (i) 30,555/INB > 0 | (i) 34,069/INB > 0 | (i) 50,129/INB < 0 |
| (ii) 2 years | (ii) 9,979/INB > 0 | (ii) 23,885/INB > 0 | (ii) 31,872/INB > 0 | (ii) 49,431/INB > 0 |
| (iii) 10 years | (iii) Cost-saving/INB > 0 | (iii) 6,177/INB > 0 | (iii) 11,789/INB > 0 | (iii) 24,896/INB > 0 |
| (iv) 20 years | (iv) Cost-saving/INB > 0 | (iv) Cost-saving/INB > 0 | (iv) Cost-saving/INB > 0 | (iv) 7,673/INB > 0 |
| (v) Lifetime | (v) Cost-saving/INB > 0 | (v) Cost-saving/INB > 0 | (v) Cost-saving/INB > 0 | (v) Cost-saving/INB > 0 |
Abbreviations: CBT, cognitive behavioural therapy; FTE, full-time equivalent; GAD, generalized anxiety disorder; GP, general practitioner; ICER, incremental cost-effectiveness ratio; INB, incremental net benefit; MDD, major depressive disorder; NEMESIS, Netherlands Mental Health Survey and Incidence Study; QALY, quality-adjusted life-year; RR, relative risk.
All costs in 2017 Canadian dollars.
INB = incremental effects × $50,000/QALY – incremental costs; if INB > 0, then the strategy is cost-effective.
All costs and effects were discounted at 1.5% in the base case analysis and all scenarios, except for scenario 19 using a 1-year time horizon (in this case, discounting was deemed inappropriate).
Table 14:
Sensitivity Scenario Analysis Results: Best-Ranked Strategiesa
| Parameter/Assumption: a. Base case analysis b. Scenario analysis |
Group CBT by Nonphysician vs. Usual Care ICER ($/QALY)/INBb > 0 or INB < 0 ($) | Individual CBT by Nonphysician vs. Group CBT by Nonphysician ICER ($/QALY)/INB > 0 or INB < 0 ($) |
|---|---|---|
| 1. Population | ||
| a. Base case: MDD and GAD | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenario: GAD only | b. 1,783/INB > 0 | b. 147, 657/INB < 0 |
| 2. Initial disease severity | ||
| a. Base case: Mild and moderate to severe MDD | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenarios: | b. | b. |
| (i) Mild MDD | (i) 1,973/INB > 0 | (i) 197,507/INB < 0 |
| (ii) Moderate to severe MDD | (ii) 8,840/INB > 0 | (ii) 183,074/INB < 0 |
| 3. Efficacy of interpersonal therapy | ||
| a. Base case: CBT | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenario: Interpersonal therapy | b. Cost-saving/INB > 0 | b. 312,234/INB < 0 |
| 4. Efficacy of CBT | ||
| a. Base case: RR_CBT | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenario: 0.25 × RR_CBT | b. 7,404/INB > 0 | b. 155,814/INB < 0 |
| 5. Dropout | ||
| a. Base case: see Table 4 | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenarios: | b. | b. |
| (i) 2 × base case probability | (i) 12,839/INB > 0 | (i) 164,239/INB < 0 |
| (ii) 0.5 × base case probability | (ii) Cost-saving/INB > 0 | (ii) 249,960/INB < 0 |
| 6. Probability of not being well after dropout | ||
| a. Base case: 0.33 | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenarios: | b. | b. |
| (i) 2 × base case probability | (i) Cost-saving/INB > 0 | (i) 223,638/INB < 0 |
| (ii) 0.5 × base case probability | (ii) 9,391/INB > 0 | (ii) 185,319/INB < 0 |
| 7. Rate of recurrence | ||
| a. Base case: Eaton 2008100 | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenario: NEMESIS99 | b. 7, 035/INB > 0 | b. 259,382/INB < 0 |
| 8. Rate of hospitalization | ||
| a. Base case: 0.10 | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenarios: | b. | b. |
| (i) 2 × base case rate | (i) 2,904/INB > 0 | (i) 191,998/INB < 0 |
| (ii) 0.5 × base case rate | (ii) 4,137/INB > 0 | (ii) 192,941/INB < 0 |
| 9. Additional disutility owing to past MDD | ||
| a. Base case: Yes | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenario: No | b. 3,751/INB > 0 | b. 210,287/INB < 0 |
| 10. Utility associated with CBT treatment | ||
| a. Base case: 0.85 | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenario: 0.765 | b. 6,486/INB > 0 | b. 183,772/INB < 0 |
| 11. Number of CBT sessions (N) | ||
| a. Base case: N = 14 | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenarios: | b. | b. |
| (i) N = 6 | (i) 781/INB > 0 | (i) 106,181/INB < 0 |
| (i) N = 20 | (ii) 7,539/INB > 0 | (ii) 306, 297/INB < 0 |
| 12. Costs of physician-provided CBTc | ||
| a. Base case: Psychiatrist | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenario: GPc | b. 3,175/INB > 0 | b. 131,431/INB < 0c |
| 13. Costs of nonphysician-provided CBT, salary-based | ||
| a. Base case: $130,000/year, 30% benefits, FTE: 1,658 hours/year | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenarios: | b. | b. |
| (i) $130,000/year, 17% benefits | (i) 2,675/INB > 0 | (i) 161,132/INB < 0 |
| (ii) $110,000/year, 30% benefits | (ii) 3,129/INB > 0 | (ii) 172,929/INB < 0 |
| (iii) $110,000/year, 17% benefits | (iii) 2,139/INB > 0 | (iii) 144,009/INB < 0 |
| 14. Costs of CBT, 2 providers | ||
| a. Base case: Psychiatrist or highest paid nonphysician | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenario: GP or lowest paid nonphysician | b. 2,133/INB > 0 | b. 144,057/INB < 0 |
| 15. Direct medical costs | ||
| a. Base case: All treatment costs | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenario: CBT treatment costs | b. 16,763/INB > 0 | b. 206, 792/INB < 0 |
| 16. Costs of complex depression | ||
| a. Base case: Responders | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenario: Nonresponders | b. Cost-saving/INB > 0 | b. 188,031/INB < 0 |
| 17. Costs of follow-up | ||
| a. Base case:100%, regular visits | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenarios: Reduction of follow-up visits and costs by | b. | b. |
| (i) 25% | (i) 1,825/INB > 0 | (i) 192,925/INB < 0 |
| (ii) 50% | (ii) Cost-saving/INB > 0 | (ii) 193,232/INB < 0 |
| (iii) 75% | (iii) Cost-saving/INB > 0 | (iii) 193,593/INB < 0 |
| 18. Discount rate | ||
| a. Base case: 1.5% | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenario: 5% | b. 4,058/INB > 0 | b. 191,704/INB < 0 |
| 19. Time horizon | ||
| a. Base case: 5 years | a. 3,175/INB > 0 | a. 192,618/INB < 0 |
| b. Scenarios: | b. | b. |
| (i) 1 yeard | (i) 16,278/INB > 0 | (i) 103,891/INB < 0 |
| (ii) 2 years | (ii) 9,979/INB > 0 | (ii) 163,071/INB < 0 |
| (iii) 10 years | (iii) Cost-saving/INB > 0 | (iii) 96,319/INB < 0 |
| (iv) 20 years | (iv) Cost-saving/INB > 0 | (iv) 33,935/INB > 0 |
| (v) Lifetime | (v) Cost-saving/INB > 0 | (v) 5,126/INB > 0 |
Abbreviations: CBT, cognitive behavioural therapy; FTE, full-time equivalent; GAD, generalized anxiety disorder; GP, general practitioner; ICER, incremental cost-effectiveness ratio; INB, incremental net benefit; MDD, major depressive disorder; NEMESIS, Netherlands Mental Health Survey and Incidence Study; QALY, quality-adjusted life-year; RR, relative risk.
All costs in 2017 Canadian dollars.
INB = incremental effects × $50,000/QALY – incremental costs; if INB < 0, then the strategy is not cost-effective.
Individual CBT provided by a nonphysician was more costly than individual CBT provided by a physician (see Table 13) and was eliminated from ranking; the ICER is still over $100,000/QALY.
All costs and effects were discounted at 1.5% in the base case analysis and all scenarios, except for scenario 19 using a 1-year time horizon (in this case, discounting was deemed inappropriate).
The results remained robust in all 19 scenarios comparing group or individual CBT provided by nonphysicians or group CBT provided by physicians with usual care (Table 13). We found that interpersonal therapy represents good value for money when compared with no treatment.
In all analyses, psychological treatment was associated with more benefits. It was also often associated with increments in costs, unless the strategy was shown to be cost saving, in which case the cost of usual care was greater than the cost of psychotherapy. Therefore, the values of the ICERs kept the same rankings in all scenarios, with group CBT provided by nonphysicians being associated with the lowest estimates (ranging from cost-saving values to $16,763/QALY when only the costs of CBT treatment were analyzed).
However, in 9 of 19 scenarios comparing individual CBT provided by physicians with usual care, the ICER was above $50,000 per QALY, suggesting that this strategy may not be optimal (in economic terms) for populations such as patients initially diagnosed with severe major depressive disorder (scenario 2; see Table 13) or patients likely to drop out of treatment (scenario 5; see Table 13), or if the utility associated with CBT were 10% lower (scenario 10; see Table 13).
Further, the ICER was over $69,000 per QALY if the number of CBT sessions were high (e.g., 20) (scenario 11; see Table 13). Interestingly, if the efficacy of CBT were 25% lower than that reported in the literature, the ICER was greater than $52,000 per QALY (scenario 4; see Table 13). Finally, when the downstream costs of major depressive disorder treatment were not taken into account (i.e., those associated with the course of CBT therapy, the initial assessment by a psychiatrist or psychologist, and follow-ups by a general practitioner), and only the costs of CBT treatment were analyzed, the ICER for individual CBT provided by physicians versus usual care was over $56,000 per QALY (scenario 15; see Table 13).
Our second set of probabilistic sensitivity analysis scenarios, shown in Table 14, compared the best-ranked strategies with each other. This analysis demonstrated robust cost-effectiveness findings in all but 2 scenarios. The first of these was the only scenario associated with an ICER less than $50,000 per QALY was one testing the duration of the model's time horizon. After a very long follow-up time of at least 20 years, individual CBT provided by a physician was found to be a better option than group therapy provided by a nonphysician (scenario 19; see Table 14). The second was the scenario that examined CBT provided by a general practitioner (instead of a psychiatrist). We found that the estimated costs of individual CBT provided by general practitioners were somewhat lower than those for individual therapy provided by nonphysicians but that the benefits of the two were equal. Thus, we found that individual CBT provided by general practitioners was comparable to group therapy provided by nonphysicians but that the ICER was still much higher than $100,000 per QALY ($131,431/QALY, scenario 12; see Table 14).
In all other scenarios, we found that a decision-maker would always need to pay more than $100,000 per QALY gained if they were to choose individual CBT over group CBT. In these analyses, the ICERs ranged from $106,000 per QALY to more than $306,000 per QALY (scenario 11; see Table 14).
Discussion
Our model-based cost-effectiveness analysis showed that both individual and group CBT provided by any regulated health care professional (i.e., physician or nonphysician) for the management of major depressive disorder and/or generalized anxiety disorder represent good value for money compared with usual care. All CBT strategies were associated with ICERs less than $50,000 per QALY gained. CBT provided as group therapy by nonphysicians was associated with the lowest ICER of $3,715 per QALY gained, whereas CBT provided as group therapy by psychiatrists was associated with the highest ICER of $43,443 per QALY gained. The probability of group CBT strategies being cost-effective is over 92% at a willingness-to-pay threshold of $50,000 per QALY, and is over 80% for any CBT strategy at a willingness-to-pay threshold of $100,000 per QALY. Our findings remained robust in all scenario analyses, with group CBT provided by nonphysicians being associated with the lowest ICER estimates (ranging from cost-saving values to $16,763 per QALY when we analyzed only the costs of CBT treatment). Our results, which are applicable to the context of Ontario's health system, align with the findings of various cost-effectiveness analyses, described within our systematic review of the economic literature. An additional strength of our economic modeling study is that we examined the incremental cost-effectiveness of structured in-person psychotherapy versus usual care in the management of adults with first and recurrent episodes of mild or moderate to severe depression and/or anxiety.
With respect to changes in the probabilities of important health outcomes over a 5-year follow-up, we found that individual and group CBT increased life expectancy (0.5–1 day), significantly decreased the number of recurrent major depressive episodes, and significantly reduced the probability of hospitalization (1.4%–1.6%). Consequently, there is substantial potential for CBT to reduce the long-term negative effects of recurrent and treatment-resistant (complex) depression.
Interestingly, we found that compared with group CBT provided by nonphysicians, individual CBT provided by nonphysicians was found not to be cost-effective at a willingness-to-pay threshold of $100,000 per QALY. This CBT strategy was associated with extremely high ICERs in both the base case and scenario analyses. However, this finding should be applied to clinical practice with caution for at least three reasons:
-
1
From a health equity perspective, it would be unfair to deprive patients of needed individual therapy if they do not engage well with group therapy
-
2
The large ICER value comes from a tiny difference in QALYs between individual and group CBT
-
3
The evidence that supports differences in effectiveness between individual and group CBT is limited.22
Future research and guidelines should address patient preferences regarding CBT strategy. Given the differences in the costs of various strategies, future guidelines should suggest situations when a particular CBT option may be preferred over another to enable the rational use and better allocation of scarce health care resources.
Although our comprehensive economic analysis used the individual-level Markov modelling approach to accurately represent the clinical course of major depressive disorder, it is associated with several limitations. First, we assumed a limited number of recurrent major depressive episodes before a patient would enter the complex depression health state, and we simplified the patient journey through several clinical pathways. Thus, we did not fully address the complexity of secondary psychiatric care, nor did we model the use of CBT in complex depression or the effectiveness of various additional types of treatment for treatment-resistant depression. Our results remained robust in all scenarios, including those that addressed patient dropout or less frequent follow-up visits, but the benefits of psychotherapies still might be underestimated. Second, we focused on addressing whether psychotherapy represents good value for money and thus did not examine the cost-effectiveness of collaborative team care or stepped care; this decision problem relates to implementation issues, which ought to be carefully tailored to patient needs. Next, based on the limitations of the existing literature, we assumed that the efficacy of CBT is the same for every new episode and that there is no difference in the effectiveness of CBT delivery among the various types of regulated providers of psychotherapy services.
We also demonstrated the cost-effectiveness of CBT for the management of generalized anxiety disorder and interpersonal therapy for the management of major depressive disorder. These result agree with clinical practice, as CBT is recognized as an effective therapy for generalized anxiety disorder, whereas both CBT and interpersonal therapy are used in the management of major depressive disorder. Therefore, our study is generalizable to the population of patients with major depressive disorder and those with generalized anxiety disorder, with either new or manageable recurrent disease. However, our evaluation focused only on populations with major depressive disorder and generalized anxiety disorder. Future research to evaluate psychological treatments for complex forms of depression or other disabling mental health disorders (including all types of anxiety disorders) is needed.
Conclusions
Our economic evaluation suggests that, compared with usual care, structured forms of individual or group psychotherapy (i.e., CBT or interpersonal therapy) delivered by both physicians and nonphysicians represent good value for money.
BUDGET IMPACT ANALYSIS
We conducted a budget impact analysis from the perspective of the Ontario Ministry of Health and Long-Term Care to estimate the cost burden over the next 5 years of providing access to individual or group psychological therapies by regulated therapists to adults diagnosed with major depressive disorder or generalized anxiety disorder. All costs are reported in 2017 Canadian dollars.97 Reporting and analysis were done and are in accordance with the 2012 International Society for Pharmacoeconomics and Outcomes Research good-practice guidelines for budget impact analysis.141
Research Questions
What would the net budget impact be in the first year after the adoption of CBT (2017) and over the following 4 years (2018–2021) under the assumption of a gradual uptake of individual or group CBT in newly diagnosed adult Ontarians with major depressive disorder and/or generalized anxiety disorder?
How many health care professionals would be needed to support timely access to individual or group CBT for a population of adults with major depressive disorder alone or in combination with generalized anxiety disorder?
Methods
We used outputs from our cost-effectiveness analysis model to estimate budget impact. Therefore, our budget impact analysis accounted for heterogeneity in the patient populations with respect to age and disease severity, differences in clinical pathways, disease prognosis, and consequent differences in resource use and costs.
Target Population
Our study population included newly diagnosed adult outpatients aged 18 years or older with a primary diagnosis of mild or moderate to severe major depressive disorder and/or generalized anxiety disorder as defined by the DSM-5 criteria.71,84–87
We based overall estimates of the incidence of primary major depressive disorder on data from the 2012 Canadian Community Health Survey and the 2010 National Population Health Survey.85,142,143 Approximately 30% of patients with major depressive disorder have treatment-resistant depression127 and were thus excluded from our target population. Canadian estimates of the incidence of major depressive disorder were 2.9% in 2 years and 5.7% in 4 years.85,143 Therefore, we used an annual incidence rate of 1.8%144,145 to estimate the target population of adults with major depressive disorder. According to the newest census estimates, there are 11,763,400 adults in Ontario; of these, 148,219 are assumed to be newly diagnosed with major depressive disorder as of 2016 (Table 15).146 In a separate scenario analysis, we examined the generalized anxiety disorder population only.
Table 15:
Expected Number of Newly Diagnosed Patients With Major Depressive Disorder Eligible for CBT in Ontario, 2017 to 2021
| Year | Target Population, N | Uptake, % | Number of Eligible Patients, N |
|---|---|---|---|
| 2017 | 148,219 | 20 | 29,644 |
| 2018 | 148,219 | 40 | 59,288 |
| 2019 | 148,219 | 60 | 88,931 |
| 2020 | 148,219 | 80 | 118,575 |
| 2021 | 148,219 | 100 | 148,219 |
Uptake
In the base case, we assumed that access to psychotherapy would increase gradually over 5 years from 0% to 100% (an increase of 20% each year). We based the assumption of no access to psychotherapy at baseline on expert consultation and literature indicating that a very small percentage of family health teams currently provide structured CBT.118,147
Thus, in Table 15, we present the expected number of patients that would gradually access CBT services in the next 5 years, from 2017 to 2021.
For our budgetary impact calculations, it was important to estimate the cohort of patients at risk. Based on our model outputs, we estimated the percentage of patients who survived at the beginning of each year (Table 16).
Table 16:
Probability of Patients Surviving at the Beginning of Each Year Year
| Year Post-Diagnosis Probability of Major Depressive Disorder | |||||
|---|---|---|---|---|---|
| Strategy, Base Case Analysis | Year 1 | Year 2 | Year 3 | Year 4 | Year 5 |
| Usual care | 1.0000 | 0.99563 | 0.99055 | 0.98555 | 0.98021 |
| Group CBT by nonphysicians or physicians | 1.0000 | 0.99609 | 0.99146 | 0.98652 | 0.98101 |
| Individual CBT by nonphysicians or physicians | 1.0000 | 0.9965 | 0.99182 | 0.98672 | 0.9812 |
Abbreviation: CBT, cognitive behavioural therapy.
Based on data presented in Tables 15 and 16, we estimated the cohort of patients who will be at risk in the next 5 years. In Table 17, we provide an example of these calculations for the scenario comparing CBT provided as a group therapy by nonphysicians with usual care.
Table 17:
Expected Number of Patients at Risk: Group CBT Provided by Nonphysicians Versus Usual Care
| Year Post-Diagnosis of Incident Major Depressive Disorder, N | |||||||
|---|---|---|---|---|---|---|---|
| Year | Strategy | Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Total N at Risk |
| 2017 | Group CBT by nonphysicians | 29,644 | 29,644 | ||||
| Usual care | 29,644 | 29,644 | |||||
| 2018 | Group CBT by nonphysicians | 59,288 | 29,528 | 88,816 | |||
| Usual care | 59,288 | 29,514 | 88,802 | ||||
| 2019 | Group CBT by nonphysicians | 88,931 | 59,056 | 29,391 | 177,378 | ||
| Usual care | 88,931 | 59,028 | 29,364 | 177,323 | |||
| 2020 | Group CBT by nonphysicians | 118,575 | 88,584 | 58,781 | 29,244 | 295,184 | |
| Usual care | 118,575 | 88,543 | 58,727 | 29,215 | 295,060 | ||
| 2021 | Group CBT by nonphysicians | 148, 219 | 118,111 | 88,172 | 58,488 | 29,081 | 442,071 |
| Usual care | 148, 219 | 118,057 | 88,091 | 58,431 | 29,057 | 441,855 | |
Abbreviation: CBT, cognitive behavioural therapy.
For each scenario (Table 18 and Appendices 7–9), we estimated the total number of patients at risk over the next 5 years; these numbers were then used to estimate the net budget impact of publicly funding CBT over the next 5 years.
Table 18:
Expected Number of Patients at Risk in Ontario, 2017 to 2021
| Year Post-Diagnosis of Incident Major Depressive Disorder, N | |||||
|---|---|---|---|---|---|
| Strategy, Base Case Analysis | Year 1 | Year 2 | Year 3 | Year 4 | Year 5 |
| Usual care | 29,644 | 88,802 | 177,323 | 295,060 | 441,855 |
| Group CBT by nonphysicians or physicians | 29,644 | 88,816 | 177,378 | 295,184 | 442,071 |
| Individual CBT by nonphysicians or physicians | 29,644 | 88,827 | 177,412 | 295,248 | 442,169 |
Canadian Costs
Based on the model estimates of direct medical costs (derived from deterministic cost–utility analyses without discounting), we calculated the average annual costs per patient from year 1 to year 5 (Table 19).
Table 19:
Average Costs per Patient Each Year Post-Diagnosis of Major Depressive Disordera
| Year Post-Diagnosis of Major Depressive Disorder, $ | |||||
|---|---|---|---|---|---|
| Strategy, Base Case Analysis | Year 1 | Year 2 | Year 3 | Year 4 | Year 5 |
| Usual care | 3,008 | 3,212 | 3,332 | 3,457 | 3,617 |
| Group CBT by nonphysicians | 3,377 | 3,300 | 3,384 | 3,455 | 3,565 |
| Group CBT by physicians | 3,692 | 3,588 | 3,670 | 3,739 | 3,837 |
| Individual CBT by nonphysicians | 3,966 | 3,903 | 3,973 | 4,031 | 4,094 |
| Individual CBT by physicians | 4,417 | 4,353 | 4,425 | 4,479 | 4,530 |
Abbreviation: CBT, cognitive behavioural therapy.
Average costs per patient were calculated using undiscounted cost outputs generated from our model simulations running for year 1 to year 5. For example, the coverage cost in year 4 was obtained by subtracting a 5-year cumulative cost estimate from a 4-year cumulative cost estimate, for usual care: Average cost for year 5 only = $16,627 – $13,009 = $3,617.
We further adjusted the estimates of average costs per patient for those remaining in the analysis (i.e., survivors) over the next 5 years, using the data presented in Tables 16 and 19, which are the final average cost estimates for patients at risk. We used these data to calculate the net budgetary impact for each scenario (in 2017 Canadian dollars).
Analysis 1: Base Case Budget Impact Analysis and Sensitivity Budget Impact Analyses
To address all possible scenarios in Ontario, we conducted the following budgetary impact analyses:
Base case budget impact analysis: included 4 scenarios to estimate the net budget impact of each of 4 CBT strategies compared with usual care
Sensitivity budget impact analysis—scenario 1: estimated the net budget impact of each CBT strategy in patients with generalized anxiety disorder only
Sensitivity budget impact analysis—scenario 2: addressed the heterogeneity of the major depressive disorder population and determined the net budget impact for the population with moderate to severe major depressive disorder
Sensitivity budget impact analysis—scenario 3: estimated the net budget impact for all CBT strategies using the costs associated with CBT treatment only
Analysis 2: Number of Therapists Needed
Our second objective was to determine the number of health care professionals needed to support timely access to CBT in Ontario. Table 21 presents our estimation of expected numbers of patients who could be treated with either group or individual CBT in one calendar year per full-time therapist.
Table 21:
Expected Number of Patients per Year for Group or Individual CBT per FTE
| Type of CBT | Number of Hours/Session | Number of Patients/Session | FTE: Applied Hours/Yeara | Time Available for CBT | Number of Sessions in One Course of CBT | Number of CBT Courses/Year | Expected Number of Patients/Year |
|---|---|---|---|---|---|---|---|
| Group | 2 | 12 | 1,658 | 829 | 14 | 59 | 708 |
| Individual | 1 | 1 | 1,658 | 1,658 | 14 | 118 | 118 |
Abbreviations: CBT, cognitive behavioural therapy; FTE, full-time equivalent.
The calculation of the applied hourly rate for a full-time employee (FTE) is described in the cost parameters section of the primary economic evaluation.
Based on the outputs of our model, we estimated an average number of major depressive episodes per patient for those remaining in the analysis (i.e., survivors) (Table 22).
Table 22:
Average Number of Major Depressive Episodes per Patient Each Year Post-Diagnosis of Major Depressive Disorder, Patients at Risk
| Year Post-Diagnosis of Major Depressive Disorder | |||||
|---|---|---|---|---|---|
| Strategy, Base Case Analysis | Year 1a | Year 2 | Year 3 | Year 4 | Year 5 |
| Group CBT | 1.33 | 0.55 | 0.52 | 0.52 | 0.51 |
| Individual CBT | 1.27 | 0.54 | 0.53 | 0.52 | 0.51 |
Abbreviation: CBT, cognitive behavioural therapy.
New (n = 1) plus recurrent major depressive episodes.
Table 23 shows estimates of the number of CBT courses needed for patients with newly diagnosed or recurrent disease (years 1 to 5), after adjusting for the number of major depressive episodes (see Table 22) and given a gradual uptake of CBT in the province.
Table 23:
Expected Number of CBT Courses Needed (New and Recurrent Major Depressive Episodes), Ontario, 2017 to 2021
| Year | Strategy | Year Post-Diagnosis of Major Depressive Disorder | Total Number of CBT Courses | ||||
|---|---|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | |||
| 2017 | Group CBT | 39,458 | 39,458 | ||||
| Individual CBT | 37,737 | 37,737 | |||||
| 2018 | Group CBT | 78,915 | 16,232 | 95,147 | |||
| Individual CBT | 75,475 | 16,370 | 91,845 | ||||
| 2019 | Group CBT | 118,373 | 32,464 | 15,404 | 166,241 | ||
| Individual CBT | 113,212 | 32,741 | 15,399 | 161,352 | |||
| 2020 | Group CBT | 157,831 | 48,696 | 30,808 | 15,306 | 252,641 | |
| Individual CBT | 150,950 | 49,111 | 30,799 | 15,394 | 246,254 | ||
| 2021 | Group CBT | 197,288 | 64,928 | 46,212 | 30,612 | 14,717 | 353,758 |
| Individual CBT | 188,687 | 65,482 | 46,198 | 30,788 | 14,960 | 346,115 | |
Abbreviation: CBT, cognitive behavioural therapy.
Results
Analysis 1: Base Case Budget Impact Analysis
Table 24 presents calculations of the net budget impact in detail, using the data presented in Tables 17 and 20 for the scenario comparing group CBT provided by nonphysicians with usual care. This strategy was associated with the lowest ICER in our cost–utility analysis, representing an optimal option for providing access to CBT in Ontario for patients with a primary diagnosis of major depressive disorder (alone or combined with generalized anxiety disorder). Adopting this CBT strategy at a 20% uptake rate would lead to an increase in costs of about $11 million in 2017 and about $68 million in 2021, when full access is achieved.
Table 24:
Net Budget Impact of Adopting Group CBT Provided by Nonphysicians in Ontario: 2017 to 2021
| Year Post-Diagnosis of New Major Depressive Disorder, $ | |||||||
|---|---|---|---|---|---|---|---|
| Year | Strategy | Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Total Budget Impact, $ |
| 2017 | Group CBT by nonphysicians | 100,118,135 | 100,118,135 | ||||
| Usual care | 89,179,996 | 89,179,996 | |||||
| Net Budget Impacta | 10,938,139 | 10,938,139 | |||||
| 2018 | Group CBT by nonphysicians | 200,236,271 | 97,821,368 | 298,057,639 | |||
| Usual care | 178,359,992 | 95,223,671 | 273,583,663 | ||||
| Net Budget Impact | 21,876,278 | 2,597,697 | 24,473,975 | ||||
| 2019 | Group CBT by nonphysicians | 300,354,406 | 195,642,736 | 100,303,320 | 596,300,462 | ||
| Usual care | 267,539,988 | 195,642,736 | 98,777,307 | 556,764,637 | |||
| Net Budget Impact | 32,814,417 | 5,195,394 | 1,526,014 | 39,535,825 | |||
| 2020 | Group CBT by nonphysicians | 400,472,541 | 293,464,104 | 200,603,228 | 102,432,336 | 996,972,209 | |
| Usual care | 356,719,985 | 285,674,240 | 197,551,249 | 102,469,900 | 942,415,374 | ||
| Net Budget Impact | 43,752,557 | 7,789,864 | 3,051,979 | −37,564 | 54,556,835 | ||
| 2021 | Group CBT by nonphysicians | 500,590,676 | 391,282,159 | 300,906,549 | 204,864,671 | 105,686,977 | 1,503,331,033 |
| Usual care | 445,899,981 | 380,897,911 | 296,328,556 | 204,943,308 | 107,226,626 | 1,435,296,382 | |
| Net Budget Impact | 54,690,696 | 10,384,248 | 4,577,993 | −78,636 | −1,539,649 | 68,034,651 | |
Abbreviation: CBT, cognitive behavioural therapy.
Net budget impact = budget impact of a CBT strategy − budget impact for usual care.
Table 20:
Average Costs per Patient Each Year Post-Diagnosis of Major Depressive Disorder, Patients at Risk
| Year Post-Diagnosis of Major Depressive Disorder, $ | |||||
|---|---|---|---|---|---|
| Strategy, Base Case Analysis | Year 1 | Year 2 | Year 3 | Year 4 | Year 5 |
| Usual care | 3,008 | 3,226 | 3,364 | 3,507 | 3,690 |
| Group CBT by nonphysicians | 3,377 | 3,313 | 3,413 | 3,503 | 3,634 |
| Group CBT by physicians | 3,692 | 3,602 | 3,702 | 3,790 | 3,912 |
| Individual CBT by nonphysicians | 3,966 | 3,917 | 4,005 | 4,085 | 4,172 |
| Individual CBT by physicians | 4,417 | 4,368 | 4,461 | 4,539 | 4,616 |
Abbreviations: CBT, cognitive behavioural therapy.
The net budget impact of the other 3 CBT strategies ranges from $20 million (group CBT provided by physicians) to $42 million (individual CBT provided by physicians) in 2017, and from $199 million (group CBT provided by physicians) to $529 million in 2021 (individual CBT provided by physicians) (Table 25).
Table 25:
Results of Budget Impact Analysis: Other CBT Strategies Versus Usual Care
| Total Budget Impact, $ | |||||
|---|---|---|---|---|---|
| Strategy, Base Case Analysis | 2017a | 2018 | 2019 | 2020 | 2021a |
| Group CBT by physicians | 109,433,424 | 325,237,147 | 649,846,395 | 1,085,291,631 | 1,634,490,392 |
| Usual care | 89,179,996 | 273,583,663 | 556,764,637 | 942,415,374 | 1,435,296,382 |
| Net Budget Impact,b $ | 20,253,428 | 51,653,484 | 93,081,758 | 142,876,257 | 199,194,010 |
| Individual CBT by nonphysicians | 117,579,310 | 350,862,865 | 701,909,623 | 1,172,443,595 | 1,764,326,970 |
| Usual care | 89,179,996 | 273,583,663 | 556,764,637 | 942,415,374 | 1,435,296,382 |
| Net Budget Impact, $ | 28,399,314 | 77,279,202 | 145,144,985 | 230,028,221 | 329,030,588 |
| Individual CBT by physicians | 130,938,018 | 390,903,806 | 782,042,830 | 1,305,968,464 | 1,964,160,363 |
| Usual care | 89,179,996 | 273,583,663 | 556,764,637 | 942,415,374 | 1,435,296,382 |
| Net Budget Impact, $ | 41,758,022 | 117,320,143 | 225,278,193 | 363,553,090 | 528,863,981 |
Abbreviation: CBT, cognitive behavioural therapy.
In 2017, uptake is assumed to be 20%; in 2021, it is assumed to be 100%.
Net budget impact = budget impact for a CBT strategy − budget impact for usual care.
Analysis 1: Sensitivity Budget Impact Analyses
Scenario 1: Generalized Anxiety Disorder Population
We conducted the first scenario analysis for the population with generalized anxiety disorder only, treated with 10 sessions of CBT. The evidence for the incidence of generalized anxiety disorder in Canada and worldwide is scarce148,149; approximately 2.5% of Ontarians are reported to have generalized anxiety disorder.72 After accounting for adults who have both major depressive disorder and generalized anxiety disorder (50%), we arrived at a target population estimate of 147,042 people with generalized anxiety disorder. The annual average costs per patient for the population at risk are presented in Appendix 7. Table 26 presents final budget impact estimates.
Table 26:
Results of Budget Impact Analysis: CBT Strategies Versus Usual Care for Generalized Anxiety Disorder
| Total Budget Impact, $ | |||||
|---|---|---|---|---|---|
| Strategy | 2017a | 2018 | 2019 | 2020 | 2021a |
| Group CBT by nonphysicians | 98,693,036 | 293,247,501 | 586,076,288 | 979,319,853 | 1,476,239,531 |
| Usual care | 88,472,218 | 271,413,133 | 552,347,567 | 934,938,319 | 1,423,906,803 |
| Net Budget Impact,b $ | 10,220,817 | 21,834,369 | 33,728,721 | 44,381,535 | 52,332,728 |
| Group CBT by physicians | 106,777,231 | 315,722,756 | 629,124,740 | 1,049,059,000 | 1,578,533,746 |
| Usual care | 88,472,218 | 271,413,133 | 552,347,567 | 934,938,319 | 1,423,906,803 |
| Net Budget Impact, $ | 18,305,012 | 44,309,623 | 76,777,173 | 114,120,681 | 154,626,943 |
| Individual CBT by nonphysicians | 113,993,482 | 358,648,017 | 692,277,529 | 1,138,335,268 | 1,698,839,970 |
| Usual care | 88,472,218 | 271,413,133 | 552,347,567 | 934,938,319 | 1,423,906,803 |
| Net Budget Impact, $ | 25,521,263 | 87,234,884 | 139,929,962 | 203,396,950 | 274,933,167 |
| Individual CBT by physicians | 125,801,644 | 370,456,006 | 735,521,418 | 1,222,690,294 | 1,833,701,289 |
| Usual care | 88,472,218 | 271,413,133 | 552,347,567 | 934,938,319 | 1,423,906,803 |
| Net Budget Impact, $ | 37,329,426 | 99,042,873 | 183,173,851 | 287,751,976 | 409,794,486 |
Abbreviation: CBT, cognitive behavioural therapy.
In 2017, the uptake is assumed to be 20%; in 2021, it is assumed to be 100%.
Net budget impact = budget impact for a CBT strategy − budget impact for usual care.
The net budget impact associated with CBT strategies for the generalized anxiety disorder population is also large. It ranges from $10 million (group CBT provided by nonphysicians) to $37 million (individual CBT provided by physicians) in 2017, and from $52 million (group CBT provided by nonphysicians) to $410 million in 2021 (individual CBT provided by physicians) (see Table 26).
Scenario 2: Heterogeneity of the Major Depressive Disorder Population: Moderate to Severe Major Depressive Disorder
The second scenario addressed the heterogeneity of the major depressive disorder population by assessing the budget impact for patients with a more severe form of major depressive disorder. This population is prone to a higher rate of episode recurrence and worse health outcomes. Based on the literature, approximately 32% of patients with major depressive disorder are initially diagnosed with moderate to severe major depressive disorder (n = 47,430). Appendix 8 provides calculations of annual average costs per patient for the population at risk. Table 27 presents final budget impact analysis results.
Table 27:
Results of Budget Impact Analysis: CBT Strategies Versus Usual Care for Moderate to Severe Major Depressive Disorder
| Total Budget Impact, $ | |||||
|---|---|---|---|---|---|
| Strategy | 2017a | 2018 | 2019 | 2020 | 2021a |
| Group CBT by nonphysicians | 32,951,097 | 97,987,988 | 195,844,408 | 327,382,099 | 493,522,667 |
| Usual care | 29,119,218 | 88,583,852 | 179,595,194 | 303,269,453 | 461,231,561 |
| Net Budget Impact,b $ | 3,831,879 | 9,404,136 | 16,249,214 | 24,112,646 | 32,291,106 |
| Group CBT by physicians | 35,793,820 | 106,377,266 | 212,468,311 | 354,865,948 | 534,423,245 |
| Usual care | 29,119,218 | 88,583,852 | 179,595,194 | 303,269,453 | 461,231,561 |
| Net Budget Impact, $ | 6,674,602 | 17,793,414 | 32,873,117 | 51,596,495 | 73,191,684 |
| Individual CBT by nonphysicians | 38,178,830 | 114,084,086 | 228,342,388 | 381,638,126 | 574,451,555 |
| Usual care | 29,119,218 | 88,583,852 | 179,595,194 | 303,269,453 | 461,231,561 |
| Net Budget Impact, $ | 9,059,611 | 25,500,234 | 48,747,194 | 78,368,673 | 113,219,994 |
| Individual CBT by physicians | 42,209,146 | 126,363,500 | 253,114,396 | 423,079,255 | 636,627,791 |
| Usual care | 29,119,218 | 88,583,852 | 179,595,194 | 303,269,453 | 461,231,561 |
| Net Budget Impact, $ | 13,089,928 | 37,779,648 | 73,519,202 | 119,809,802 | 175,396,231 |
Abbreviation: CBT, cognitive behavioural therapy.
In 2017, the uptake is assumed to be 20%; in 2021, it is assumed to be 100%.
Net budget impact = budget impact for a CBT strategy − budget impact for usual care.
Owing to a smaller target population, the net budget impact for this scenario is much lower than for others. It ranges from $4 million (group CBT provided by nonphysicians) to $13 million (individual CBT provided by physicians) in 2017. In 2021, adopting any CBT strategy at an uptake rate of 100% would lead to an increase in costs ranging from $32 million (group CBT provided by nonphysicians) to $175 million (individual CBT provided by physicians).
Scenario 3: Costs Associated With CBT Treatment Only
The third scenario estimated the budget impact if only the costs associated with CBT treatment are included (i.e., the costs of the initial assessment, providing 14 sessions of CBT, and follow-ups by a psychiatrist and general practitioner). This analysis included all adults with newly diagnosed major depressive disorder (n = 148,219). Appendix 9 presents calculations of the annual average costs per patient for the population at risk. Table 28 presents final budgetary impact results.
Table 28:
Results of Budget Impact Analysis: Costs of CBT Treatment Only
| Total Budget Impact, $ | |||||
|---|---|---|---|---|---|
| Strategy | 2017a | 2018 | 2019 | 2020 | 2021a |
| Group CBT by nonphysicians | 22,997,928 | 59,904,987 | 110,802,768 | 175,506,678 | 253,482,427 |
| Usual care | 5,680,333 | 15,812,270 | 30,275,788 | 48,956,464 | 71,681,269 |
| Net Budget Impact,b $ | 17,317,595 | 44,092,717 | 80,526,979 | 126,550,214 | 181,801,158 |
| Group CBT by physicians | 32,313,218 | 87,084,496 | 164,348,701 | 263,826,100 | 384,641,787 |
| Usual care | 5,680,333 | 15,812,270 | 30,275,788 | 48,956,464 | 71,681,269 |
| Net Budget Impact, $ | 26,632,884 | 71,272,226 | 134,072,912 | 214,869,636 | 312,960,518 |
| Individual CBT by nonphysicians | 40,550,958 | 113,406,373 | 218,971,729 | 356,949,014 | 526,416,893 |
| Usual care | 5,680,333 | 15,812,270 | 30,275,788 | 48,956,464 | 71,681,269 |
| Net Budget Impact, $ | 34,870,625 | 97,594,104 | 188,695,940 | 307,992,550 | 454,735,624 |
| Individual CBT by physicians | 53,909,666 | 153,447,315 | 299,104,936 | 490,473,883 | 726,250,286 |
| Usual care | 5,680,333 | 15,812,270 | 30,275,788 | 48,956,464 | 71,681,269 |
| Net Budget Impact, $ | 48,229,333 | 137,635,045 | 268,829,148 | 441,517,419 | 654,569,017 |
Abbreviation: CBT, cognitive behavioural therapy.
In 2017, the uptake is assumed to be 20%; in 2021, it is assumed to be 100%.
Net budget impact = budget impact for a CBT strategy − budget impact for usual care.
Overall, the results from the sensitivity analyses indicate the ranges of investment over the next 5 years for the Ontario Ministry of Health and Long-Term Care if the Ministry were to adopt any of the compared CBT strategies. Although all CBT strategies represented good value for money in the primary economic evaluations, they are associated with large net budget impacts, ranging from $17 million to $48 million in the first year of adoption at an uptake rate of 20%. Adopting any CBT strategy at an uptake rate of 100% would cost the province an additional $182 million to $656 million, depending on the type of CBT (group vs. individual) and type of delivery (nonphysician vs. physician).
Analysis 2: Estimating the Number of Therapists Needed in Ontario, 2017 to 2021
Based on the expected number of patients who could be treated per full-time therapist annually with either group CBT (N = 708, Table 21) or individual CBT (N = 118, Table 21), and the expected number of CBT courses per year (Table 23), we calculated that 500 therapists would be needed to provide group CBT therapy for all potential patients with a primary diagnosis of major depressive disorder (alone or combined with general anxiety disorder) in Ontario in 2021 (Table 29). For individual CBT, 2,934 therapists would be needed to provide therapy for all potential patients in Ontario in 2021.
Table 29:
Expected Number of Therapists Needed to Provide Group and Individual CBT in Ontario, 2017 to 2021
| Year | Strategy | Year Post-Diagnosis of Major Depressive Disorder | Total Number of Therapists | ||||
|---|---|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | |||
| 2017 | Group CBT | 56 | 56 | ||||
| Individual CBT | 320 | 320 | |||||
| 2018 | Group CBT | 111 | 23 | 134 | |||
| Individual CBT | 640 | 139 | 779 | ||||
| 2019 | Group CBT | 167 | 46 | 22 | 235 | ||
| Individual CBT | 959 | 277 | 131 | 1,367 | |||
| 2020 | Group CBT | 223 | 69 | 44 | 22 | 358 | |
| Individual CBT | 1,279 | 416 | 261 | 130 | 2,086 | ||
| 2021 | Group CBT | 279 | 92 | 65 | 43 | 21 | 500 |
| Individual CBT | 1,599 | 555 | 392 | 261 | 127 | 2,934 | |
Abbreviation: CBT, cognitive behavioural therapy.
Based on expert consultation, psychotherapy training may take about 8 months for professionals with Master's degrees. This consists of about 1,000 hours of client work, 100 hours of supervised work, and 50 hours of providing in-person psychotherapy, as regulated by the College of Registered Psychotherapists of Ontario. For psychologists with an undergraduate degree, training may take around 4,000 hours of supervised clinical practice (as regulated by the College of Psychologists of Ontario). Further, CBT therapists (of any regulated health profession) should be certified in CBT delivery by a national CBT credentialing body to ensure the quality of therapeutic delivery.
According to estimates from the Ontario Psychological Association (personal communication) and the Ontario Society of Psychotherapists (personal communication), there are currently around 4,100 trained psychologists (50% employed in public practice) and around 270 trained psychotherapists providing psychological therapies in Ontario.
Discussion
We conducted a model-based budget impact analysis to examine the range of investment needed to enable full access to necessary structured psychological treatments for patients with major depressive disorder and/or generalized anxiety disorder. We used CBT as a representative type of structured psychotherapy, as it is the most researched form of psychological therapy and is also widely used in clinical practice.
Our budget impact analysis found that the costs of adopting CBT are high, most likely owing to the large number of people suffering from major depressive disorder and generalized anxiety disorder. Adding CBT to usual care over the next 5 years would cost the province between $68 million and $529 million, depending on the type of treatment (group vs. individual) and type of provider (nonphysician vs. physician). Our analysis indicates that CBT provided as group therapy by any publicly funded, regulated therapist (i.e., a nonphysician) is the most affordable option for the province. However, individual CBT represents good value for money and should be available to those patients who are not engaging well with or adhering to group therapy. If individual CBT provided by nonphysicians were provided to a maximum of 20% of patients with major depressive disorder, the net budget impact would be about $28 million.
Our analysis also shows that restricting CBT to patients with moderate to severe major depressive disorder may be a more affordable option. Assuming that 1 in 5 patients would have access to psychotherapy in 2017, the increase in costs would be $4 million for group CBT provided by nonphysicians or $13 million for individual CBT provided by physicians. At the end of 2021, if all potential patients were to have full access, the corresponding cost increases would range from $32 million to $175 million.
To provide CBT to all potential patients with a primary diagnosis of major depressive disorder by 2021 in Ontario, around 500 therapists would be needed to deliver group therapy, and about 2,930 therapists would be needed to deliver individual therapy.
It is important to recognize that any regulated health professional providing psychotherapy should be certified by a national credentialing body to ensure the quality of therapeutic delivery. Data from professional organizations and our analysis suggest that we may currently have an adequate number of regulated professionals who could potentially provide therapy in the first years of adoption. Therefore, implementation efforts would need to be focused on investments in infrastructure120 and the organization of outpatient psychological treatment care for adults with major depressive disorder and generalized anxiety disorder in Ontario.
Conclusions
The most affordable option for providing publicly funded structured psychotherapy to adults with major depressive disorder and/or generalized anxiety disorder is group psychotherapy delivered by regulated nonphysician therapists. Selective delivery of individual structured psychotherapy by regulated nonphysician therapists or physicians is recommended for those patients who would benefit most from it (i.e., those who are not engaging well with or adhering to group therapy).
PATIENT, CAREGIVER, AND PUBLIC ENGAGEMENT
Objective
The objective of this analysis was to explore the underlying values, needs, impacts, and preferences of those who have lived experience with major depressive disorder and generalized anxiety disorder and psychological treatments for these disorders. The treatment focus was cognitive behavioural therapy (CBT), interpersonal therapy, and supportive therapy.
Background
Public and patient engagement explores the lived experience of a person with a health condition, including the impact that the condition and its treatment has on the patient, as well as the patient's family or other caregivers, and on the patient's personal environment. Public and patient engagement increases awareness and builds appreciation for the needs, priorities, and preferences of the person at the centre of a treatment program. The insights gained through public and patient engagement provide an in-depth picture of lived experience through an intimate look at the values that underpin the experience.
Lived experience is a unique source of evidence about the personal impact of a health condition and how that condition is managed, including what it is like to navigate the health care system with that condition, and how health technologies or interventions may or may not make a difference in people's lives. Information shared from lived experience can also identify gaps or limitations in published research (for example, outcome measures that do not reflect what is important to those with lived experience).150–152 Additionally, lived experience can provide information or perspectives on the ethical and social values implications of technologies and interventions.
Mental health conditions can have a significant impact on the lives of people living with these conditions and their families. To understand the impact of these disorders on the quality of life of those living with them, we spoke with people and families of people with lived experience of these mental health conditions who also had experience with psychotherapy treatment. Understanding and appreciating the day-to-day functioning of people with major depressive disorder and generalized anxiety disorder and their experience with types of treatment, including psychotherapy, helps to contextualize the potential value of psychotherapy.
Methods
Engagement Plan
Engagement as a concept captures a range of efforts used to involve the public and patients in various domains and stages of health technology assessment decision-making.153 Rowe and Frewer outline three types of engagement: communication, consultation, and participation.154 Communication constitutes a one-way transfer of information from the sponsor to the individual, whereas participation involves the sponsor and individual collaborating through real-time dialogue. Consultation refers to the sponsor seeking out and obtaining information (e.g., through experiential input) from the public, patients, and caregivers affected by the technology or intervention in question.155
The engagement plan for this health technology assessment focused on consultation. Within this typology, the engagement design focused on interviews to elicit the lived experience of patients with major depressive disorder or generalized anxiety disorder and their families, as well as their experiences with accessing and using psychotherapy as a treatment option.
The qualitative interview was selected as an appropriate methodology because it allowed us to explore the meaning of central themes in the lived experience of the participants. The main task in interviewing is to understand the meaning of what participants say.156 Interviews are particularly useful for getting the story behind a participant's experiences, which was the objective of this portion of the study. The sensitive nature of exploring quality of life for this topic is another factor supporting the use of interviews for this project.
Recruitment of Participants
Our recruitment strategy for this project used an approach called purposive sampling to actively recruit people with direct lived experience.157–160 Patient, Caregiver, and Public Engagement staff contacted people with experience of psychotherapy and their families through a variety of partner organizations, health clinics, local and provincial mental health support associations, and foundations.
Inclusion Criteria
We sought to speak with people who had experienced treatment with psychotherapy, specifically CBT, interpersonal therapy, or supportive therapy, for the treatment of major depressive disorder and/or generalized anxiety disorder. Participants were not required to currently be receiving psychotherapy treatment, only to have had lived experience with it. We sought a broad geographic, cultural, and socioeconomic representation to elicit possible equity issues in accessing and receiving psychotherapy treatment.
Exclusion Criteria
We set no exclusion criteria.
Participants
We spoke with 20 people with a history of major depressive disorder and/or generalized anxiety disorder who had experienced psychotherapy as a form of treatment. Participants were all over 18 years of age and were recruited from locations across Ontario. Participants reported living in rural and remote locations, as well as urban centres.
Approach
At the beginning of the interview, we explained the purpose of the health technology assessment process (including the role and mandate of Health Quality Ontario and the Ontario Health Technology Advisory Committee), risks of participation, and protection of personal health information. We explained these attributes to participants orally and through a letter of information (Appendix 10) and obtained consent from participants prior to commencing the interview (Appendix 11). Interviews were recorded and transcribed.
Interview questions focused on the impact of the lived condition on the participants' and their families' quality of life, experiences with other health interventions to manage and treat their mental health condition, experiences with psychotherapy, any barriers experienced to receiving treatment, and any perceived benefits or limitations of treatment. The interview guide is presented in Appendix 12.
The interview were semi-structured, consisted of a series of open-ended questions, and lasted for approximately 30 to 90 minutes. Questions for the interview were based on a list developed by the Health Technology Assessment International Interest Group on Patient and Citizen Involvement in HTA to elicit lived experiences specific to the impact of a health technology or intervention.161
Data Extraction and Analysis
We selected a modified version of a grounded theory methodology to analyze transcripts of participant interviews, because this methodology captures themes and allows elements of lived experience to be compared among participants. The inductive nature of grounded theory follows an iterative process of eliciting, documenting, and analyzing responses while simultaneously collecting and analyzing data using a constant comparative approach.162,163 Through this approach, staff coded transcripts and compared themes using the qualitative software program NVivo (QSR International, Doncaster, Victoria, Australia). NVivo allowed us to identify and interpret patterns in the interview data about the meaning and implications of living with major depressive disorder or generalized anxiety disorder from the patients' perspective of what is important in their daily lived experience, both before and after receiving psychotherapy treatment.
Results
Lived Experience of Major Depressive Disorder and Generalized Anxiety Disorder
Symptoms of depression or anxiety manifested in various ways and were associated with a myriad of causes, from childhood trauma, to events experienced as an adult (e.g., divorce, death of a family member, estrangement from family) or other psychological conditions. Many participants emphasized the unique and personal nature of their experiences and outcomes, stating that their views of mental health treatments such as psychotherapy may not apply to others.
Despite these personal differences, participants did express some commonalities in their experiences. Participants consistently reported that their disorder had a significant negative impact on their lives and that this impact extended to all facets of their lives: social, emotional, and physical. Several participants spoke of the reduced quality of life caused by the impact of their mental health condition. Common examples were estrangement from friends and families, a reduced capacity to work, and a withdrawal from social events and connections:
“… because they just don't understand depression. A lot of them thought I was just faking it. Some of them thought all the normal thoughts of people who don't really understand depression. So, we lost, my wife and [I], lost a lot of friends and family members.”
Participants often spoke of their mental health issues beginning in adolescence or earlier, resulting in a negative impact that lasted for decades. Participants said that they associated their mental health condition with stigma and shame, whether manifested as an adult or adolescent:
“I can remember that feeling, just feeling worthless, and there was no chance to have a better life.”
“When I look at it, I say, ‘Look, it took me 40 years before I went and got somebody to help me with this. You know you don't have to wait 40 years.’”
Participants reported wanting to hide the challenges they were facing and hesitating to share their problems with others, even members of their own families. In some cases, participants had experienced physical or emotional trauma in childhood and felt that these experiences had caused their depression or anxiety. These participants said that seeking help for their complex mental health issues was especially challenging. Almost all participants spoke of the challenge of first overcoming the perceived stigma and shame to seek treatment. Often, this took years:
“Because of the way my parents were talking to me, I was really scared of them finding out that I was trying to get help.”
“Growing up with a father who suffered from anxiety and depression, there was always this huge stigma, so of course you naturally carry that along. And also a big part of it is I never wanted to be a bother to people.”
“I think frankly, a lot of people, myself included, with mental illness, they wait until—wait and wait and wait and wait until it become unbearable, and then they seek help.”
Other Types of Treatment for Major Depressive Disorder and Generalized Anxiety Disorder
Participants reported pharmacotherapy as the primary alternative or companion to psychotherapy to treat their mental health conditions. However, they often reported hesitation when first making the decision to receive treatment with medication, worried about potential side effects and the stigma associated with taking medication:
“I was afraid that they'd give me meds, and that was taboo. I thought I don't want to be on antidepressants, but I was feeling unbalanced.”
“I wouldn't take antidepressants. I just wouldn't. Certainly, when I was 25, the formulations of these things were a lot cruder than they are now, and some of them had horrible side effects. These days, some of the side effects are far less emphatic, but they're still there. So I wouldn't take antidepressants.”
“Just a bias. You know the old ‘I don't want to take medication feeling'? I was afraid of it.”
The effectiveness of pharmacotherapy in treating major depressive disorder or generalized anxiety disorder varied for the people we interviewed. While some found medication beneficial, others reported that medications were rarely helpful and expressed frustration at what they perceived as an over-reliance on pharmacotherapy in the health care system. These participants often traced their depression or anxiety to specific traumatic events in their past and felt that medication would not relieve the ultimate source of their mental health issues:
“And medication won't change the way you think. It will change some of the biochemistry, which helps, but it certainly will not change the way you think.”
“I did not have luck with antidepressants, probably because the nature of my depression wasn't chemically based.”
Those participants who did report finding medication helpful and effective often found its effect to be limited in terms of its ability to eliminate their disorder completely. They often mentioned needing to try many different medications before finding one, or a combination of medications, that was effective. In addition, most participants viewed pharmacotherapy as a complement to psychotherapy rather than an alternative, stating that the most effective treatment for their mental health conditions was a careful combination of both psychotherapy and pharmacotherapy. However, this balance was often difficult to establish quickly or reliably:
“Yes, psychotherapy has helped, but sometimes, there was one or two times when what I really needed was an antidepressant, [and] that [was what] I got the biggest result from.”
“And for medication, I think it serves a purpose for folks to be able to get into the cognitive space to be able to benefit from therapy, but medication alone would have never worked for me.”
“I've known people who've tried maybe 60 medications—six-zero—and nothing works. And there [are] not doctors doing some studies of trying to figure out what would work better with your genetic composition; it's still very much a crap shoot of figuring out what's going to work for you or not.”
Owing to the personal and unique nature of mental health disorders, participants often reported accessing multiple therapies in an attempt to find one that was effective. This occurred over a number of years, as participants attempted different treatments provided by different health care professionals. However, because of the cost and access challenges associated with what were perceived as the more effective treatments, participants often continued to use these less effective treatments, which resulted in longer treatment periods and frustration with the health care system:
“Well, I tried a lot of things, because again, you only get certain access to stuff, because of the limitations, right. What are you going to do? So, most people try a psychiatrist, and then the psychiatrist doesn't really do any therapy with you, right, he's only going to do medication. So, then I tried a psychoanalyst, ‘cause he was a psychiatrist, and again that's covered, but that wasn't helpful either. And I actually spent a long time with that person who didn't really help me.”
“So I have made those choices before [relating to cost challenges] where I would go to some online communities that are a little bit more risky; sometimes you['d] meet somebody who's really awesome and really reflective, and sometimes you'd meet somebody who was not in that community for the right reasons.”
Barriers to Accessing Psychotherapy
The experience of constantly searching for effective and accessible treatment was a common one for the people we interviewed. Participants reported searching for treatments that balanced effectiveness with cost. And, owing to the interpersonal nature of psychotherapy treatment, participants reported feeling that its effectiveness was often dependent on the health care professional providing the therapy. Therefore, participants identified three main barriers to finding effective and sustainable psychotherapy care: cost, physical access to the right health care professional (which often necessitated excessive wait times), and lack of information about care options.
Cost
For a large number of people interviewed, the cost of psychotherapy was reported as a barrier to accessing the type and frequency of psychotherapy they felt was needed to effectively treat their condition. Participants were often forced to choose between effectiveness and cost in their treatment decisions, which resulted in a longer duration of their mental health condition and a negative impact on their quality of life:
“The psychoanalysis was not effective, and yet that was the only thing financially that was available at the time for me because I didn't have an income at that point. Now, later, when I was making something of an income, then I could afford to access some of these other groups that were helpful.”
“My biggest frustration is that the proper treatment, at least for people like me, is almost inaccessible because of cost.”
“And then I have to limit how long can I see somebody, or how often, given the amount of money it's costing me.”
Participants who were able to afford the mental health treatment of their choice by paying out of pocket still reported feeling anxious about the cost of treatment and grateful when sliding fee scales were occasionally offered by a mental health care provider. This anxiety can arise from paying for health care services that may not ultimately be effective, whether owing to the interpersonal dynamics between the patient and therapist or the type of therapy offered:
“And I've been with her six years now, and I'm paying out of pocket, about $4,000 to $5,000 a year. And I really wanted to speak about that, too, because I think that that is such a huge issue: that this place is what's actually dealing with the core issues that caused my anxiety, which maybe I can actually finally get some relief from, and it's really frustrating [to always pay].”
“I see [my therapist] every two weeks because that's what we can afford. We rely on their sliding scale [for cost].”
“I know people who've actually gone into quite significant debt to be able to afford therapy, especially because you don't ever know if the therapy that you can have access to right now is going to be the one that works.”
Physical Access to Appropriate Treatment Providers
Participants reported that physically being unable to access a desired type of treatment provider was a common barrier. This physical barrier could be geographical in nature or come in the form of long wait lists. Participants from northern Ontario spoke of the long distance and travel time needed to see their chosen treatment provider. People from urban areas frequently spoke of how fortunate they felt to have a larger number of options for mental health services, which may not be available elsewhere:
“I don't understand generally how people get mental health services when they don't live near University Avenue [in Toronto].”
“To go and see a counsellor in Thunder Bay, I have to drive 3 hours; well, my [partner] has to drive 3 hours.”
“I know that there are services out there, but what there [are] are few and far between, and everything takes so long to get on that it's—even when you're really actively looking for help, it's hard to get.”
Participants from all parts of the province consistently lamented the long wait lists that prevented them from accessing mental health services they felt could be helpful. Long wait lists were a source of extreme frustration and often resulted in participants accessing what they felt was less effective treatment or remaining with a health care professional they did not feel was helping them:
“It is very hard to access if folks aren't in university; you're probably going to be waiting for anywhere from 6 months to 18 months for a free therapist or paying anywhere from $170 to $200 an hour to see somebody.”
“So I thought this cannot go on. This simply cannot go on. So I decided to do something about it, and rather than going the bureaucratic route and going to see my family doctor and have him recommend a psychiatrist who could see me Tuesday afternoons but only in 8 months from now because that really is—you know, that's really how it works—I decided I would just, you know, find someone myself.”
Several patients reported using hospital emergency department services in an attempt to circumvent long wait lists and access mental health services more quickly:
“I think the general knowledge is that you're never going to get psychotherapy in Ontario if you're on the wait list. The only way to get psychotherapy through the OHIP or hospital system is through [the] ER [emergency room].”
“I've talked to other people who say they're really desperate for psychiatric care and they want—if nothing else, they want somebody who can give them meds and help them mitigate the issue a little, and my recommendation is always, I hate to say it, but fake a suicide attempt and go to [the] ER; [that] will get you to the front of the line.”
“He suggested that I take myself into emergency during a really bad time and that emergency would help me to fast-track to get to a psychiatrist. But when I showed up at the hospital and explained that, they actually started yelling at me, and told me off, that this was not the process to follow.”
Lack of Information About Care Options
A number of people interviewed mentioned a lack of information as a barrier to accessing the treatment that would be most effective. Participants reported feeling overwhelmed by the complexities of accessing the health care system and the different types of treatment available for mental health conditions. The feeling of being overwhelmed was reported to be more acute if the person's depression or anxiety had begun as an adolescent:
“There's stuff online that would be helpful for people to help themselves. But again, without somebody to [explain] that, I think it's a little harder for people to access it.”
“A psychiatrist, a psychologist, a therapist, a cognitive behavioural therapist…. Like, unless you're actually in the business, I don't know who does what. And you don't even know how they might even help you.”
Several participants reported frustration at knowing that help and information were available, whether online or elsewhere, but not knowing how or where to access them:
“Compared to other diseases, this is the one area where information can be so much more valuable because it's not like you can take out your own kidney. But you can, to
some degree, help yourself with mental health and the help of a GP [general practitioner].”
“Thunder Bay is kind of like the hub of northwestern Ontario, [but] what they offer in this area is not always super clear or concise…. It's just when you're actively really trying to access services and get help and still not get[ting] a lot of the information, it's very frustrating. So I would say that would probably have to be one of the biggest [frustrations] for sure.”
Psychotherapy for Major Depressive Disorder and Generalized Anxiety Disorder
Participants reported positive results from receiving psychotherapy treatment once they were able to access it, but they differed in terms of which type of psychotherapy they found most effective: CBT, interpersonal therapy, or supportive therapy. Participants also had differences of opinion regarding preferences for group therapy versus individual psychotherapy. Some people found it more effective to speak in a group setting, whereas others found the most benefit from individual therapy sessions with a trusted health care professional.
The differences in preference and perception of effectiveness of the different types of psychotherapy are likely a result of the personal and unique nature of a patient's experience of a mental health condition; methods that are most effective for one person may not be effective for another. The people we interviewed expressed this sentiment, acknowledging that their experiences, values, and perceptions of psychotherapy would not necessarily apply to others:
“My biggest frustration is limited modality. Don't tell me the kind of therapy I need to subscribe to get help. Be open enough to see that I am a unique, complex individual [who] needs to have the right fit, because once I'm better I'm highly productive and I'm an asset, but you keep shoving me into a square [hole]…. Well, I'm round; it doesn't work.”
When speaking of the benefits of psychotherapy, many participants expressed relief at finding someone trusted in whom to confide and with whom share their emotional burden. This was especially true when a person had spent a great deal of time and money before finding a treatment provider with whom they could form this trusting relationship:
“I felt like the weight of the world had been lifted off my shoulders because someone was fighting for me.”
“I think it was the chemistry; I think when you seek professional help, and when you need a family physician or any type of professional like that, the chemistry's either there or it's not, it works or it doesn't, and for me, [it was the] people that it did.”
Other participants saw the benefit of psychotherapy in terms of the tools they learned to help them deal with their depression or anxiety, which allowed them to gain a sense of independence and self-reliance:
“I found that the psychotherapy is the more [help] that I need. It's actually giving me the skills and working on things.”
“I think some of the skills that they would teach through CBT and then later on [in dialectical behaviour therapy] really helped me get through situations where my thoughts were unhealthy and gave me the skills to be able to challenge those unhealthy thoughts.”
“Like, for example, cognitive therapy was really helpful [for] looking at thoughts and refuting them or [assessing] how realistic are they, that kind of thing, as well as mindfulness-based training, learning how to breathe during an anxiety attack, that kind of stuff.”
Finally, some participants who traced their depression or anxiety to traumatic childhood events felt that psychotherapy helped them to discuss and examine those events in a healthy way. Speaking of these events with a trusted treatment provider allowed a degree of relief and unburdening, which patients reported as being extremely beneficial:
“I haven't had a serious depression since starting that therapy, and it's funny, it feels like…it's like finally scratching an itch that I couldn't reach before. Finally being able to talk about some of those things is what's allowing it to get resolved.”
“It's really been the only thing that I have done that I have felt like my family and friends have noticed that it's made a big difference in me. It's not just medicating and keep going, it's actually going back and stripping away and looking at some painful things, but processing them in a way where I don't have to continually have this trauma and nightmares and horrible things for the rest of my life.”
A large number of the people we interviewed reflected on the time they had spent searching for treatment before finding effective psychotherapy. They lamented this as time wasted and expressed great frustration at the years needlessly spent living with depression or anxiety before finding effective psychotherapy:
“Now as an adult, looking back, I have a much better understanding about what I went through and what would have been helpful, but at the time, when you have no reference or base of information to know what I need, what to ask for, it wasn't something that I was able to articulate.”
“I believe it's true that had I gotten, you know, this kind of therapy back in my 20s, I could have dealt with, resolved, and moved on and kept my career. It's the worst thing of my depression these days, the fact that I can't work.”
“In the perfect world where the resources were available, it is 15 years of time when I could have sorted out a lot of the issues I'm dealing with now when I have a psychiatrist. I could have done that earlier.”
Discussion
The people we interviewed consistently reported on the negative impact that major depressive disorder and generalized anxiety disorder had on their quality of life. While the causes of the participants' disorders varied, participants expressed a similar desperate desire to find effective treatment for their conditions. They reported that after overcoming the perceived stigma and shame of their mental health issues, which itself was a lengthy process, they faced a long journey to obtain effective and sustainable treatment, whether psychotherapy, pharmacotherapy, or both. Owing to the personal and unique nature of each person's experience of a mental health issue, the participants' treatment journeys and the perceived benefits of treatment varied. Participants also differed in their views of the effectiveness of different types of psychotherapy (i.e., CBT, interpersonal therapy, and supportive therapy) and their preference for group versus individual therapy. However, all participants agreed that ultimately receiving their preferred type of psychotherapy benefited them in dealing with their depression or anxiety.
Participants commonly experienced obstacles before finding successful treatment. These obstacles were often associated with access to the mental health treatment providers and treatments of their choice. Participants also reported experiencing a number of equity issues when trying to obtain psychotherapy services, including barriers associated with cost, geography, and access to information about different care options.
Conclusions
The people we spoke with who had lived experience of major depressive disorder or generalized anxiety disorder reported positive experiences with psychotherapy. However, they also reported experiencing a large number of barriers that prevented them from finding effective psychotherapy in a timely manner. Participants reported wanting more freedom to choose the type of psychotherapy they received. Too often, they felt they were forced to balance effectiveness and cost in their mental health treatment, which they felt resulted in having to rely on less effective treatment and increased time spent suffering from their condition.
Acknowledgments
The medical editor was Kara Stahl. Others involved in the development and production of this report were Harrison Heft, Claude Soulodre, Ana Laing, Kellee Kaulback, Andrée Mitchell, Anil Thota, Vivian Ng, Nancy Sikich, and Irfan Dhalla.
We are grateful to the following individuals for their expert advice in the preparation of this report: Nick Kates and Randi McCabe (McMaster University and St. Joseph's Healthcare Hamilton); Jan Kasperski (Ontario Psychological Association); Stephanie Carter, Judith Laposa, and Enza Mancuso (Centre for Addiction and Mental Health); Claire Watson (Ontario Society of Psychotherapists); Harindra Wijeysundera (University of Toronto); and David Tannenbaum (Mount Sinai Hospital, Toronto).
The statements, conclusions, and views expressed in this report do not necessarily represent the views of the consulted experts.
ABBREVIATIONS
- ADM
Antidepressant medication
- AMSTAR
A Measurement Tool to Assess Systematic Reviews
- BDI
Beck Depression Inventory
- CADTH
Canadian Agency for Drugs and Technologies in Health
- CBT
Cognitive behavioural therapy
- CER
Cost-effectiveness ratio
- CI
Confidence interval
- CrI
Credible interval
- DALY
Disability-adjusted life-year
- DSM
Diagnostic and Statistical Manual
- ED
Emergency department
- FTE
Full-time equivalent
- GAD
Generalized anxiety disorder
- GP
General practitioner
- GRADE
Grading of Recommendations Assessment, Development, and Evaluation
- HDRS
Hamilton Depression Rating Scale
- HR
Hazard ratio
- ICD-10
International Statistical Classification of Diseases and Related Health Problems, tenth edition
- ICER
Incremental cost-effectiveness ratio
- INB
Incremental net benefit
- IPT
Interpersonal therapy
- MDD
Major depressive disorder
- MDE
Major depressive episode
- ODB
Ontario Drug Benefit Program
- OHIP
Ontario Health Insurance Plan
- OR
Odds ratio
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- QALY
Quality-adjusted life-year
- RCT
Randomized controlled trial
- RR
Relative risk
- SD
Standard deviation
- SE
Standard error
- SGA
Second-generation antidepressant
- SMD
Standardized mean difference
- SNRI
Serotonin–norepinephrine reuptake inhibitor
- SSRI
Selective serotonin reuptake inhibitor
- TCA
Tricyclic antidepressant
- WMD
Weighted mean difference
- WTP
Willingness-to-pay threshold
GLOSSARY
- Base case, cost-effectiveness analysis
A set of recommended methods used for all evaluations that promote uniformity and transparency and that enable the comparison of results for different technologies and different decisions.
- Base case, budget impact analysis
A projected or virtual scenario in which no changes are made to current practice. The base case is used for comparison with an alternative scenario in which the technology under review is used.
- Cognitive behavioural therapy
A method of talk therapy that focusses on solving problems by changing patterns of thought and behavior.
- Cost-effective
Good value for money. The overall benefit of the technique or intervention justifies the cost.
- Cost–utility analysis
A type of analysis that estimates the value for money of an intervention by weighing the cost of the intervention against the improvements in length of life and quality of life. The result is expressed as a dollar amount per “quality-adjusted life-year” or QALY.
- Disability-adjusted life-year (DALY)
An alternative to the quality-adjusted life year. One DALY represents 1 year of healthy life. The calculation determines DALYs lost to an individual's disease burden compared to a theoretical maximum. Lost DALYs are sometimes age-rated so that disability in a young person may have a larger impact on DALY score than the same disability in an older person.
- Discounting
A method that considers that costs and health benefits are worth more today than in the future.
- Generalized anxiety disorder
A chronic condition resulting in a person having much greater than normal levels of worry, usually about normal life issues such as health or money, often without a clear external source. Physical symptoms may include sleeplessness, exhaustion, headaches, or nausea.
- Incremental cost
The extra cost associated with using one test or treatment instead of another.
- Incremental cost-effectiveness ratio
Determines “a unit of benefit” for an intervention by dividing the incremental cost by the effectiveness. The incremental cost is the difference between the cost of the treatment under study and an alternative treatment. The effectiveness is usually measured as additional years of life or as “quality-adjusted life-years.”
- Incremental net benefit
A type of cost-effectiveness analysis that examines the difference in benefits compared to the difference in costs of two interventions. It is expressed as a dollar figure representing the difference between the increased benefit (the “relative benefit”) of the intervention of interest and the “willingness to pay” threshold (the maximum value assigned to a health benefit) minus the cost of the alternative intervention.
- Interpersonal therapy
A form of talk therapy that focuses on the patient's relationships with other people, especially friends and family, and how they see themselves relative to their environment.
- Major depressive disorder
A persistent and often recurring mental condition involving feelings of sadness and lack of desire to engage in pleasurable activities. Work, family, sleep, appetite, interpersonal relations, and general health may be negatively affected.
- Markov model
A type of modelling that measures the health state of a patient over the course of treatment. A patient may stay in one health state or move from one health state to another, depending on the effect of the treatment and the progression of the disease.
- Quality-adjusted life-year (QALY)
A measurement that takes into account both the number of years gained by a patient from a procedure and the quality of those extra years (ability to function, freedom from pain, etc.). The QALY is commonly used as an outcome measure in cost-utility analyses.
- Randomized controlled trial
A type of study in which subjects are assigned randomly into different groups, with one group receiving the treatment under study and the other group(s) receiving a different treatment or a placebo (no treatment) to determine the effectiveness of one approach compared with the other.
- Sensitivity
The ability of a test to accurately identify persons with the condition tested for (that is, how well it returns positive results in persons who have the condition).
- Sensitivity analysis
Every evaluation contains some degree of uncertainty. Study results can vary depending on the values taken by key parameters. Sensitivity analysis is a method that allows estimates for each parameter to be varied to show the impact on study results. There are various types of sensitivity analyses. Examples include deterministic, probabilistic, and scenario.
- Statistical significance
The outcome of an analysis is statistically significant if the assumption that there is no effect (the “null hypothesis”) is sufficiently unlikely to be true. Typically, the outcome is considered statistically significant if there is less than a 5% chance that the outcome would have occurred if the null hypothesis were true.
- Supportive therapy
Treatment designed to improve, or sustain a patient's physiological well-being and self-reliance.
- Systematic review
A process to answer a research question by methodically identifying and assessing all available studies that evaluate the specified research question. The systematic review process is designed to be transparent and objective and is aimed at reducing bias in determining the answers to research questions.
- Time horizon
Costs and outcomes are examined within a chosen time frame. In an economic evaluation, this time frame is referred to as the time horizon.
- Utility
The perceived value placed on a person's health status.
APPENDICES
Appendix 1: Literature Search Strategies
Clinical Evidence Search
Search date: October 27, 2016
Databases searched: Ovid MEDLINE, Embase, PsycINFO, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, CRD Health Technology Assessment Database, and NHS Economic Evaluation Database, and EBSCOhost CINAHL.
Database: EBM Reviews – Cochrane Database of Systematic Reviews <2005 to October 26, 2016>, EBM Reviews – Database of Abstracts of Reviews of Effects <1st Quarter 2015>, EBM Reviews – Health Technology Assessment <3rd Quarter 2016>, EBM Reviews – NHS Economic Evaluation Database <1st Quarter 2015>, Embase <1980 to 2016 Week 43>, Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) <1946 to Present>, PsycINFO <1967 to October Week 3 2016> Search Strategy:
-
1
Depressive Disorder, Major/(37477)
-
2
((depression* or depressive* or melancholia*) adj2 (major or disorder* or chronic or treatment resistant or severe or intractable or persistent or acute or clinical or unipolar*)).ti,ab,kf. (211579)
-
3
Anxiety Disorders/(55295)
-
4
((anxiet* adj3 generali#ed) or GAD).ti,ab,kf. (35372)
-
5
or/1–4 (291922)
-
6
Cognitive Therapy/(75023)
-
7
(((cognitive or behavio*) adj2 (therap* or psychotherap*)) or cognitive behavio* or CBT).ti,ab,kf. (130287)
-
8
Psychotherapy/(179385)
-
9
(((inter-personal or interpersonal) adj2 (therap* or psychotherap*)) or IPT).ti,ab,kf. (8309)
-
10
(supportive adj2 (counsel?ing or therap* or psychotherap*)).ti,ab,kf. (15900)
-
11
or/6–10 (337312)
-
12
5 and 11 (26204)
-
13
Meta Analysis.pt. (75032)
-
14
Meta-Analysis/or Meta-Analysis as Topic/or exp Technology Assessment, Biomedical/(278355)
-
15
(((systematic* or methodologic*) adj3 (review* or overview*)) or pooled analysis or published studies or published literature or hand search* or handsearch* or medline or pubmed or embase or cochrane or cinahl or data synthes* or data extraction* or HTA or HTAs or (technolog* adj (assessment* or overview* or appraisal*))).ti,ab. (569603)
-
16
(meta analy* or metaanaly* or health technolog* assess*).mp. (402075)
-
17
or/13–16 (798205)
-
18
12 and 17 (2433)
-
19
(Comment or Editorial or Letter or Congresses).pt. (3079506)
-
20
18 not 19 (2407)
-
21
(adolescent/or exp child/or exp infant/) not exp adult/(3647446)
-
22
20 not 21 (2210)
-
23
limit 22 to english language [Limit not valid in CDSR,DARE; records were retained] (2014)
-
24
23 use ppez (612)
-
25
12 use coch,dare,clhta,cleed (96)
-
26
24 or 25 (708)
-
27
major depression/(155728)
-
28
((depression* or depressive* or melancholia*) adj2 (major or disorder* or chronic or treatment resistant or severe or intractable or persistent or acute or clinical or unipolar*)).tw,kw. (221397)
-
29
generalized anxiety disorder/(10981)
-
30
((anxiet* adj3 generali#ed) or GAD).tw,kw. (36257)
-
31
or/27–30 (322221)
-
32
cognitive therapy/or cognitive behavioral therapy/(75879)
-
33
(((cognitive or behavio*) adj2 (therap* or psychotherap*)) or cognitive behavio* or CBT).tw,kw. (138989)
-
34
*Psychotherapy/(112510)
-
35
psychotherapy/ and (psychological or psychotherap*).tw,kw. (109012)
-
36
(((inter-personal or interpersonal) adj2 (therap* or psychotherap*)) or IPT).tw,kw. (8947)
-
37
(supportive adj2 (counsel?ing or therap* or psychotherap*)).tw,kw. (16551)
-
38
or/32–37 (308774)
-
39
31 and 38 (26091)
-
40
Meta Analysis/ or “Meta Analysis (Topic)”/ or Biomedical Technology Assessment/ (270975)
-
41
(((systematic* or methodologic*) adj3 (review* or overview*)) or pooled analysis or published studies or published literature or hand search* or handsearch* or medline or pubmed or embase or cochrane or cinahl or data synthes* or data extraction* or HTA or HTAs or (technolog* adj (assessment* or overview* or appraisal*))).ti,ab. (569603)
-
42
(meta analy* or metaanaly* or health technolog* assess*).mp. (402075)
-
43
or/40–42 (797109)
-
44
39 and 43 (2920)
-
45
Comment/ or Editorial/ or Letter/ or conference abstract.pt. (5348466)
-
46
44 not 45 (2826)
-
47
exp juvenile/ not exp adult/ (1996249)
-
48
46 not 47 (2736)
-
49
limit 48 to english language [Limit not valid in CDSR,DARE; records were retained] (2535)
-
50
49 use emez (888)
-
51
major depression/ (155728)
-
52
((depression* or depressive* or melancholia*) adj2 (major or disorder* or chronic or treatment resistant or severe or intractable or persistent or acute or clinical or unipolar*)).ti,ab,id. (217534)
-
53
generalized anxiety disorder/ (10981)
-
54
((anxiet* adj3 generali#ed) or GAD).ti,ab,id. (35417)
-
55
or/51–54 (318654)
-
56
cognitive therapy/ or cognitive behavior therapy/ (90317)
-
57
(((cognitive or behavio*) adj2 (therap* or psychotherap*)) or cognitive behavio* or CBT).ti,ab,id. (133272)
-
58
interpersonal psychotherapy/ (1323)
-
59
(((inter-personal or interpersonal) adj2 (therap* or psychotherap*)) or IPT).ti,ab,id. (8525)
-
60
Supportive Psychotherapy/ (491)
-
61
(supportive adj2 (counsel?ing or therap* or psychotherap*)).ti,ab,id. (15968)
-
62
or/56–61 (183003)
-
63
55 and 62 (19716)
-
64
(((systematic* or methodologic*) adj3 (review* or overview*)) or pooled analysis or published studies or published literature or hand search* or handsearch* or medline or pubmed or embase or cochrane or cinahl or data synthes* or data extraction* or HTA or HTAs or (technolog* adj (assessment* or overview* or appraisal*))).ti,ab. (569603)
-
65
(meta analy* or metaanaly* or health technolog* assess*).mp. (402075)
-
66
(systematic review or meta analysis).md. (28295)
-
67
or/64–66 (783417)
-
68
63 and 67 (1821)
-
69
(editorial or comment reply or letter).dt. (167736)
-
70
68 not 69 (1781)
-
71
limit 70 to english language [Limit not valid in CDSR,DARE; records were retained] (1652)
-
72
70 use psyb (498)
-
73
26 or 50 or 72 (2094)
-
74
limit 73 to yr=“2000 -Current” [Limit not valid in DARE; records were retained] (1998)
-
75
74 use emez (855)
-
76
74 use ppez (580)
-
77
74 use psyb (468)
-
78
74 use coch (21)
-
79
74 use dare (24)
-
80
74 use clhta (16)
-
81
74 use cleed (34)
-
82
remove duplicates from 74 (1443)
EBSCOhost CINAHL
| # | Query | Results |
|---|---|---|
| S1 | (MH “Depression”) | 71,813 |
| S2 | ((depression* OR depressive* OR melancholia*) N2 (major OR disorder* OR chronic OR treatment resistant OR severe OR intractable OR persistent OR acute OR clinical OR unipolar*)) | 16,211 |
| S3 | (MH “Generalized Anxiety Disorder”) | 187 |
| S4 | ((anxiet* N3 generali?ed) OR GAD) | 2,169 |
| S5 | S1 OR S2 OR S3 OR S4 | 78,415 |
| S6 | (MH “Cognitive Therapy”) | 13,350 |
| S7 | (((cognitive or behavio*) N2 (therap* or psychotherap*)) or cognitive behavio* or CBT) | 31,999 |
| S8 | (MH “Psychotherapy”) | 14,828 |
| S9 | (((inter-personal OR interpersonal) N2 (therap* OR psychotherap*)) or IPT) | 633 |
| S10 | ((supportive N2 (counsel#ing OR therap* OR psychotherap*)) | 1,199 |
| S11 | S6 OR S7 OR S8 OR S9 OR S10 | 46,131 |
| S12 | S5 AND S11 | 6,517 |
| S13 | (MH “Meta Analysis”) | 25,396 |
| S14 | (PT “Meta Analysis”) or (PT “Systematic Review”) | 57,035 |
| S15 | ((systematic* or methodologic*) N3 (review* or overview*)) or pooled analysis or published studies or published literature or hand search* or handsearch* or medline or pubmed or embase or cochrane or cinahl or data synthes* or data extraction* or HTA or HTAs or (technolog* N1 (assessment* or overview* or appraisal*)) | 112,308 |
| S16 | S13 OR S14 OR S15 | 122,305 |
| S17 | S12 AND S16 | 511 |
| S18 | ((MH “Child+” or MH “Adolescent+”) NOT (MH “Adult+”)) | 355,103 |
| S19 | S17 NOT S18 | 475 |
| S20 | S17 NOT S18 | 475 |
| S21 | S17 NOT S18 Limiters – Published Date: 20000101-20161231 | 467 |
Grey Literature
Search date: October 31, 2016
Websites searched: HTA Database Canadian Repository, Alberta Health Technologies Decision Process reviews, Canadian Agency for Drugs and Technologies in Health (CADTH), Institut national d'excellence en santé et en services sociaux (INESSS), Institute of Health Economics (IHE), McGill University Health Centre Health Technology Assessment Unit, National Institute for Health and Care Excellence (NICE), Agency for Healthcare Research and Quality (AHRQ) Evidence-based Practice Centers, Australian Government Medical Services Advisory Committee, Blue Cross Blue Shield Center for Clinical Effectiveness, Centers for Medicare & Medicaid Services Technology Assessments, Institute for Clinical and Economic Review, Ireland Health Information and Quality Authority Health Technology Assessments, Washington State Health Care Authority Health Technology Reviews, NHS PROSPERO International prospective register of systematic reviews
Keywords used: cognitive; CBT; behavioural therapy; behavioral therapy; behavioral counselling; behavioral counseling; behavioural counselling; behavioural counseling; Interpersonal; IPT; supportive therapy; supportive counselling; supportive counseling; psychotherapy
Results: 33
Economic Evidence Search
Search date: October 28, 2016
Databases searched: Ovid MEDLINE, Embase, PsycINFO, Cochrane Database of Systematic Reviews, Cochrane CENTRAL, Database of Abstracts of Reviews of Effects, CRD Health Technology Assessment Database, and NHS Economic Evaluation Database, and EBSCOhost CINAHL
Database: EBM Reviews – Cochrane Central Register of Controlled Trials <September 2016>, EBM Reviews – Cochrane Database of Systematic Reviews <2005 to October 26, 2016>, EBM Reviews – Database of Abstracts of Reviews of Effects <1st Quarter 2015>, EBM Reviews -Health Technology Assessment <3rd Quarter 2016>, EBM Reviews – NHS Economic Evaluation Database <1st Quarter 2015>, Embase <1980 to 2016 Week 43>, Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) <1946 to Present>, PsycINFO <1967 to October Week 3 2016>
Search Strategy:
-
1
Depressive Disorder, Major/ (40109)
-
2
((depression* or depressive* or melancholia*) adj2 (major or disorder* or chronic or treatment resistant or severe or intractable or persistent or acute or clinical or unipolar*)).ti,ab,kf. (221938)
-
3
Anxiety Disorders/ (57341)
-
4
((anxiet* adj3 generali#ed) or GAD).ti,ab,kf. (36896)
-
5
or/1–4 (305251)
-
6
Cognitive Therapy/ (80546)
-
7
(((cognitive or behavio*) adj2 (therap* or psychotherap*)) or cognitive behavio* or CBT).ti,ab,kf. (141200)
-
8
Psychotherapy/ (181148)
-
9
(((inter-personal or interpersonal) adj2 (therap* or psychotherap*)) or IPT).ti,ab,kf. (8935)
-
10
(supportive adj2 (counsel?ing or therap* or psychotherap*)).ti,ab,kf. (16864)
-
11
or/6–10 (352063)
-
12
5 and 11 (28550)
-
13
economics/ (269968)
-
14
economics, medical/ or economics, pharmaceutical/ or exp economics, hospital/ or economics, nursing/ or economics, dental/ (769533)
-
15
economics.fs. (388040)
-
16
(econom* or price or prices or pricing or priced or discount* or expenditure* or budget* or pharmacoeconomic* or pharmaco-economic*).tw. (849741)
-
17
exp “costs and cost analysis”/ (550111)
-
18
cost*.ti. (253441)
-
19
cost effective*.tw. (272778)
-
20
(cost* adj2 (util* or efficacy* or benefit* or minimi* or analy* or saving* or estimate* or allocation or control or sharing or instrument* or technolog*)).ab. (176474)
-
21
models, economic/ (157347)
-
22
markov chains/ or monte carlo method/ (67139)
-
23
(decision adj1 (tree* or analy* or model*)).tw. (38698)
-
24
(markov or markow or monte carlo).tw. (111289)
-
25
quality-adjusted life years/ (31631)
-
26
(QOLY or QOLYs or HRQOL or HRQOLs or QALY or QALYs or QALE or QALEs).tw. (58119)
-
27
((adjusted adj (quality or life)) or (willing* adj2 pay) or sensitivity analys*s).tw. (108223)
-
28
or/13–27 (2507433)
-
29
12 and 28 (2059)
-
30
(Comment or Editorial or Letter or Congresses).pt. (3085197)
-
31
29 not 30 (2010)
-
32
(adolescent/ or exp child/ or exp infant/) not exp adult/ (3693427)
-
33
31 not 32 (1887)
-
34
limit 33 to english language [Limit not valid in CDSR,DARE; records were retained] (1758)
-
35
34 use ppez (415)
-
36
29 use coch,cctr,clhta,dare (240)
-
37
12 use cleed (35)
-
38
or/35–37 (690)
-
39
major depression/ (155730)
-
40
((depression* or depressive* or melancholia*) adj2 (major or disorder* or chronic or treatment resistant or severe or intractable or persistent or acute or clinical or unipolar*)).tw,kw. (232451)
-
41
generalized anxiety disorder/ (10981)
-
42
((anxiet* adj3 generali#ed) or GAD).tw,kw. (37814)
-
43
or/39–42 (334608)
-
44
cognitive therapy/ or cognitive behavioral therapy/ (81402)
-
45
(((cognitive or behavio*) adj2 (therap* or psychotherap*)) or cognitive behavio* or CBT).tw,kw. (151198)
-
46
*Psychotherapy/ (112510)
-
47
psychotherapy/ and (psychological or psychotherap*).tw,kw. (109980)
-
48
(((inter-personal or interpersonal) adj2 (therap* or psychotherap*)) or IPT).tw,kw. (9608)
-
49
(supportive adj2 (counsel?ing or therap* or psychotherap*)).tw,kw. (17515)
-
50
or/44–49 (324083)
-
51
43 and 50 (28057)
-
52
Economics/ (269968)
-
53
Health Economics/ or exp Pharmacoeconomics/ (221305)
-
54
Economic Aspect/ or exp Economic Evaluation/ (421523)
-
55
(econom* or price or prices or pricing or priced or discount* or expenditure* or budget* or pharmacoeconomic* or pharmaco-economic*).tw. (849741)
-
56
exp “Cost”/ (527901)
-
57
cost*.ti. (253441)
-
58
cost effective*.tw. (272778)
-
59
(cost* adj2 (util* or efficacy* or benefit* or minimi* or analy* or saving* or estimate* or allocation or control or sharing or instrument* or technolog*)).ab. (176474)
-
60
Monte Carlo Method/ (53965)
-
61
(decision adj1 (tree* or analy* or model*)).tw. (38698)
-
62
(markov or markow or monte carlo).tw. (111289)
-
63
Quality-Adjusted Life Years/ (31631)
-
64
(QOLY or QOLYs or HRQOL or HRQOLs or QALY or QALYs or QALE or QALEs).tw. (58119)
-
65
((adjusted adj (quality or life)) or (willing* adj2 pay) or sensitivity analys*s).tw. (108223)
-
66
or/52–65 (2108872)
-
67
51 and 66 (2224)
-
68
Comment/ or Editorial/ or Letter/ or conference abstract.pt. (5347471)
-
69
67 not 68 (2117)
-
70
exp juvenile/ not exp adult/ (1996249)
-
71
69 not 70 (2068)
-
72
limit 71 to english language [Limit not valid in CDSR,DARE; records were retained] (1964)
-
73
72 use emez (653)
-
74
major depression/ (155730)
-
75
((depression* or depressive* or melancholia*) adj2 (major or disorder* or chronic or treatment resistant or severe or intractable or persistent or acute or clinical or unipolar*)).ti,ab,id. (227896)
-
76
generalized anxiety disorder/ (10981)
-
77
((anxiet* adj3 generali#ed) or GAD).ti,ab,id. (36942)
-
78
or/74–77 (330338)
-
79
cognitive therapy/ or cognitive behavior therapy/ (95840)
-
80
(((cognitive or behavio*) adj2 (therap* or psychotherap*)) or cognitive behavio* or CBT).ti,ab,id. (144188)
-
81
interpersonal psychotherapy/ (1323)
-
82
(((inter-personal or interpersonal) adj2 (therap* or psychotherap*)) or IPT).ti,ab,id. (9151)
-
83
Supportive Psychotherapy/ (491)
-
84
(supportive adj2 (counsel?ing or therap* or psychotherap*)).ti,ab,id. (16932)
-
85
or/79–84 (196531)
-
86
78 and 85 (21425)
-
87
economics/ or economy/ (375609)
-
88
pharmacoeconomics/ or health care economics/ (169786)
-
89
(econom* or price or prices or pricing or priced or discount* or expenditure* or budget* or pharmacoeconomic* or pharmaco-economic*).tw. (849741)
-
90
exp “costs and cost analysis”/ (550111)
-
91
cost*.ti. (253441)
-
92
cost effective*.tw. (272778)
-
93
(cost* adj2 (util* or efficacy* or benefit* or minimi* or analy* or saving* or estimate* or allocation or control or sharing or instrument* or technolog*)).ab. (176474)
-
94
markov chains/ (15616)
-
95
(decision adj1 (tree* or analy* or model*)).tw. (38698)
-
96
(markov or markow or monte carlo).tw. (111289)
-
97
(QOLY or QOLYs or HRQOL or HRQOLs or QALY or QALYs or QALE or QALEs).tw. (58119)
-
98
((adjusted adj (quality or life)) or (willing* adj2 pay) or sensitivity analys*s).tw. (108223)
-
99
or/87–98 (1932041)
-
100
86 and 99 (1246)
-
101
(editorial or comment reply or letter).dt. (167736)
-
102
100 not 101 (1230)
-
103
limit 102 to english language [Limit not valid in CDSR,DARE; records were retained] (1171)
-
104
103 use psyb (287)
-
105
38 or 73 or 104 (1630)
-
106
limit 105 to yr=“2000 -Current” [Limit not valid in DARE; records were retained] (1509)
-
107
106 use ppez (373)
-
108
106 use emez (613)
-
109
106 use psyb (257)
-
110
106 use coch (20)
-
111
106 use cctr (198)
-
112
106 use dare (7)
-
113
106 use clhta (7)
-
114
106 use cleed (34)
-
115
remove duplicates from 106 (1089)
-
116
115 use ppez,emez,psyb (888)
-
117
115 use coch,cctr,dare,clhta,cleed (201)
EBSCOhost CINAHL
| # | Query | Results |
|---|---|---|
| S1 | (MH “Depression”) | 71,813 |
| S2 | ((depression* OR depressive* OR melancholia*) N2 (major OR disorder* OR chronic OR treatment resistant OR severe OR intractable OR persistent OR acute OR clinical OR unipolar*)) | 16,211 |
| S3 | (MH “Generalized Anxiety Disorder”) | 187 |
| S4 | ((anxiet* N3 generali?ed) OR GAD) | 2,169 |
| S5 | S1 OR S2 OR S3 OR S4 | 78,415 |
| S6 | (MH “Cognitive Therapy”) | 13,350 |
| S7 | (((cognitive or behavio*) N2 (therap* or psychotherap*)) or cognitive behavio* or CBT) | 31,999 |
| S8 | (MH “Psychotherapy”) | 14,828 |
| S9 | (((inter-personal OR interpersonal) N2 (therap* OR psychotherap*)) or IPT) | 633 |
| S10 | ((supportive N2 (counsel#ing OR therap* OR psychotherap*)) | 1,199 |
| S11 | S6 OR S7 OR S8 OR S9 OR S10 | 46,131 |
| S12 | S5 AND S11 | 6,517 |
| S13 | (MH “Economics”) | 10,842 |
| S14 | (MH “Economic Aspects of Illness”) | 6,438 |
| S15 | (MH “Economic Value of Life”) | 511 |
| S16 | MH “Economics, Dental” | 104 |
| S17 | MH “Economics, Pharmaceutical” | 1,735 |
| S18 | MW “ec” | 138,769 |
| S19 | (econom* or price or prices or pricing or priced or discount* or expenditure* or budget* or pharmacoeconomic* or pharmaco-economic*) | 205,522 |
| S20 | (MH “Costs and Cost Analysis+”) | 82,690 |
| S21 | TI cost* | 38,428 |
| S22 | (cost effective*) | 25,086 |
| S23 | AB (cost* N2 (util* or efficacy* or benefit* or minimi* or analy* or saving* or estimate* or allocation or control or sharing or instrument* or technolog*)) | 15,992 |
| S24 | (decision N1 (tree* or analy* or model*)) | 4,531 |
| S25 | (markov or markow or monte carlo) | 2,544 |
| S26 | (MH “Quality-Adjusted Life Years”) | 2,477 |
| S27 | (QOLY or QOLYs or HRQOL or HRQOLs or QALY or QALYs or QALE or QALEs) | 4,904 |
| S28 | ((adjusted N1 (quality or life)) or (willing* N2 pay) or sensitivity analys?s) | 9,730 |
| S29 | S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 | 272,052 |
| S30 | S12 AND S29 | 357 |
| S31 | ((MH “Child+” or MH “Adolescent+”) NOT (MH “Adult+”)) | 355,103 |
| S32 | S30 NOT S31 | 343 |
| S33 | S30 NOT S31 Limiters – Published Date: 20000101-20161231; Language: English | 319 |
Grey Literature
Search date: October 31, 2016
Websites searched: HTA Database Canadian Repository, Alberta Health Technologies Decision Process reviews, Canadian Agency for Drugs and Technologies in Health (CADTH), Institut national d'excellence en santé et en services sociaux (INESSS), Institute of Health Economics (IHE), McGill University Health Centre Health Technology Assessment Unit, National Institute for Health and Care Excellence (NICE), Agency for Healthcare Research and Quality (AHRQ) Evidence-based Practice Centers, Australian Government Medical Services Advisory Committee, Blue Cross Blue Shield Center for Clinical Effectiveness, Centers for Medicare & Medicaid Services Technology Assessments, Institute for Clinical and Economic Review, Ireland Health Information and Quality Authority Health Technology Assessments, Washington State Health Care Authority Health Technology Reviews, Tufts Cost-Effectiveness Analysis Registry, ClinicalTrials.gov
Keywords used: cognitive; CBT; behavioural therapy; behavioral therapy; behavioral counselling; behavioral counseling; behavioural counselling; behavioural counseling; Interpersonal; IPT; supportive therapy; supportive counselling; supportive counseling; psychotherapy
Results: 48
Appendix 2: Evidence Quality Assessment
Table A1:
AMSTAR Scores of Included Systematic Reviews
| Author, Year | AMSTAR Scorea | (1) Provided Study Design | (2) Duplicate Study Selection | (3) Broad Literature Search | (4) Considered Status of Publication | (5) Listed Excluded Studies | (6) Provided Characteristics of Studies | (7) Assessed Scientific Quality | (8) Considered Quality in Report | (9) Methods to Combine Appropriate | (10) Assessed Publication Bias | (11) Stated Conflict of Interest |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hunot et al11 | 9 | √ | √ | √ | √ | √ | √ | √ | √ | √ | ✗ | ✗ |
| Cuijpers et al38 | 8 | √ | √ | √ | ✗ | ✗ | √ | √ | √ | √ | √ | ✗ |
| Cuijpers et al20 | 8 | √ | √ | √ | ✗ | ✗ | √ | √ | √ | √ | √ | ✗ |
| Guidi et al31 | 6 | √ | √ | √ | ✗ | ✗ | √ | ✗ | ✗ | √ | √ | ✗ |
| Churchill et al22 | 9 | √ | √ | √ | √ | √ | √ | √ | √ | √ | ✗ | ✗ |
| Cuijpers et al37 | 7 | √ | ✗ | √ | ✗ | ✗ | √ | √ | √ | √ | √ | ✗ |
| Biesheuvel-Leliefeld et al29 | 8 | √ | √ | √ | ✗ | ✗ | √ | √ | √ | √ | √ | ✗ |
| Linde et al21 | 9 | √ | √ | √ | √ | ✗ | √ | √ | √ | √ | √ | ✗ |
| Karyotaki et al35 | 8 | √ | √ | √ | ✗ | ✗ | √ | √ | √ | √ | √ | ✗ |
| Clarke et al30 | 7 | √ | √ | √ | ✗ | ✗ | √ | √ | √ | √ | ✗ | ✗ |
| Amick et al36 | 9 | √ | √ | √ | √ | ✗ | √ | √ | √ | √ | √ | ✗ |
| Cuijpers et al14 | 9 | √ | √ | √ | √ | ✗ | √ | √ | √ | √ | √ | ✗ |
| Jakobsen et al46 | 7 | √ | √ | √ | ✗ | ✗ | √ | √ | √ | √ | ✗ | ✗ |
Abbreviation: AMSTAR, A Measurement Tool to Assess Systematic Reviews.
The maximum possible score is 11. Details of AMSTAR score are provided in Shea et al.18
Appendix 3: Characteristics of Systematic Reviews
Table A2:
Characteristics of Systematic Reviews
| Author, Year | Objective | Study Design and Methods | Results | Limitations/Comments |
|---|---|---|---|---|
| Cognitive Behavioural Therapy Versus Usual Care for Major Depressive Disorder | ||||
| Cuijpers et al, 201620 | To conduct a meta-analysis of RCTs to determine the efficacy of CBT for the acute treatment of MDD compared with control (wait list, usual care, or pill placebo). |
Treatment Provider No details reported Inclusion Criteria RCTs Recruited patients met diagnostic criteria (e.g., DSM) Therapies that used individual, group, or guided self-help formats Exclusion Criteria Self-guided therapies without any professional support To calculate effect sizes, all measures examining depressive symptoms (e.g., BDI, HDRS) were used. |
Pooled Effect Size 63 comparisons g = 0.75 (95% CI: 0.64–0.87) NNT = 3.86 Egger's test found considerable asymmetry of the funnel plot (intercept: 1.54; 95% CI 0.59–2.50, P = .001), which indicated publication bias Waitlist Control g = 0.98 (95% CI: 0.80–1.17) NNT = 2.85 Usual Care g = 0.60 (95% CI: 0.45–0.75) NNT = 4.99 Pill Placebo g = 0.55 (95% CI: 0.28–0.81) NNT = 5.51 |
The authors assessed the methodological quality of most studies as low or unknown, according to the Cochrane risk-of-bias assessment tool. Eleven of the 63 studies were rated as high quality. The duration of treatment and follow-up was not reported. The number of treatment sessions varied from 1 to 25. For publication bias with regard to MDD, 14% of the studies were missing, and the pooled effect size dropped from g = 0.75 to g = 0.65 (95% CI: 0.53–0.78). |
| Guidi et al, 201631 | To determine the efficacy of the sequential use of psychotherapy after pharmacotherapy in the treatment of patients with MDD. |
Treatment Provider No details reported Inclusion Criteria RCTs examining the efficacy of the sequential use of psychotherapy following response to acute-phase pharmacotherapy in adults with MDD Exclusion Criteria Studies that did not report on the face-to-face delivery of psychotherapy Studies of continuation and maintenance treatments for MDD in which psychotherapy was also given during the acute phase ≤18 years of age Patients with bipolar disorder, dysthymia, minor depressive disorder, seasonal affective disorder, psychotic disorders, or active medical illness |
13 studies (N = 1,410) Follow-up ranged from 12 months to 52 months after treatment. Length of maintenance treatment ranged from 8 to 32 weeks. Primary outcome measure = relapse or recurrence rates of MDD as defined by study investigators (reaching cut-off on any depression rating scale and/or the occurrence of a defined MDE after remission/recovery in acute-phase treatment) at the longest available follow-up. All studies used CBT as psychotherapy. Three studies compared a sequential treatment arm with antidepressant medication and clinical management, 6 with usual care, 1 with psychoeducation and usual care, and 3 with clinical management only. Overall, the pooled risk ratio for relapse/recurrence was 0.78 (95% CI: 0.67–0.91); NNT = 8. Sequential Use of Psychotherapy During Continuation of Antidepressant Medication 9 studies Pooled risk ratio for relapse: 0.71 (95% CI: 0.68–0.96) NNT = 10 Sequential Use of Psychotherapy After Discontinuation of Antidepressant Medication 4 studies Pooled risk ratio for relapse: 0.67 (95% CI: 0.48–0.94) NNT = 5 |
The methodological quality of the studies was reported as high by the authors; however, the method of rating quality was not reported. Usual care involved standard care as typically provided by the referring agencies with no restriction on the use of pharmacotherapy. |
| Clarke et al, 201530 | To determine the effectiveness of nonpharmacological interventions compared with control in patients who have recovered from MDD. A subset analysis was conducted for CBT. |
Treatment Provider No details reported Inclusion Criteria Adults in full or partial remission from MDD were randomized to either a nonpharmacological intervention or a control condition (usual care, clinical management, or pharmacotherapy) Followed up for a minimum of 1 year after randomization Remission was any reduction in symptoms to below a diagnostic threshold or other threshold on a validated assessment tool Exclusion Criteria Studies that randomized patients to acute treatment even if they then followed them up after recovery |
Compared with control, the average risk of developing a new MDE by 12 months was reduced by 25% for CBT (RR = 0.75, 95% CI: 0.64–0.89). Data for relapse at 24 months were available for 7 of the 10 CBT studies. The effect for CBT at 24 months was similar to the effect at 12 months (RR = 0.72, 95% CI: 0.57–0.91). There was considerable variation among the trials in terms of the nature and duration of the intervention and the inclusion of patients who had undergone previous psychological or pharmacological treatments. Generally, the authors of the CBT trials had adapted CBT for relapse, produced their own manuals, and used this modified version in their own trials. Sessions were between 30 and 90 minutes and spanned periods of 8 to 35 weeks. Most trials treated patients individually. |
There was considerable overlap in the content of the controls; e.g., antidepressant drugs were used in control groups described as “usual care” and as “clinical management,” as well as those described as “medication” arms. There was a large difference in the control event rate for relapse across trials (for 12-month data, range = 0.2–0.79). Overall, the authors reported that half the studies in the meta-analysis were unclear or were at high risk of bias for attrition because of uncertainty about dropout or because of high levels of attrition. The authors used GRADE for each intervention. The evidence was generally of low quality; reasons for downgrading were inconsistency of results, indirectness of evidence, imprecision, and reporting bias. |
| Biesheuvel-Leliefeld et al, 201529 | To determine the effectiveness of psychological interventions in reducing the relapse or recurrence rates of MDD. A subset analysis was reported for CBT. |
Treatment Provider No details reported Inclusion Criteria RCTs Adults with recurrent MDD who were in remission (according to their own definition in the individual trial paper) at randomization Patients received a psychological intervention to reduce the risk of relapse or recurrence Control condition (usual care [routine clinical management, assessment only, no treatment, or waitlist control with unrestricted access to usual care] or antidepressant drugs) Studies reported relapse or recurrence rates using established screeners with a predefined cut-off point for MDD (HRSD, BDI, or diagnostic interview) All modes of delivery were included (face-to-face, group, follow-up booster sessions, Internet) Exclusion Criteria None reported |
16 trials (17 contrasts) CBT after remission was delivered by various modes: weekly group sessions, individual sessions, over the Internet, and as booster sessions (various numbers of sessions during various duration of periods with a minimum of 3 sessions). Duration of follow-up ranged from 22 to 332 weeks. In total, 529 patients received CBT. CBT vs. Usual Care Risk ratio: 0.68 (95% CI: 0.65–0.87) Risk difference: −0.196 (95% CI: −0.28 to −0.11) NNT = 5 CBT vs. Antidepressant Drugs Risk ratio: 0.79 (95% CI: 0.61–1.02) Risk difference: −0.16 (95% CI: −0.30 to −0.016) NNT = 6 |
The authors classified the overall quality of evidence as low according to the GRADE criteria. There were differences in the methodological design of the trials, including the definitions of remission, recovery, relapse, and recurrence; the type and duration of interventions; and whether there was a preceding acute intervention in the same trial (e.g., usual care was often described inadequately, and information on the exact method of determining recurrence [interview vs. questionnaire] was sometimes not provided. Owing to nature of psychological interventions, and the difficulty of comparing these with placebo interventions, the highest-quality evidence may not be possible in such studies. Factors that lower quality of evidence, such as differences in interventions (e.g., owing to differences in client–therapist relations) and difficulties blinding patients, outcome reporters, and personnel, will likely remain in studies investigating the effects of psychological interventions. |
| Linde et al, 201521 | To determine the effectiveness of psychological treatments compared with usual care or placebo in the treatment of primary care patients with MDD. A subset analysis was conducted for face-to-face CBT. |
Treatment Provider Varied (i.e., counsellors, nurses, psychiatrists, psychologists, psychotherapists, therapists) Inclusion Criteria Adults with unipolar MDD Patients had to be recruited through direct referral from a GP or other primary care physician not specialized in mental health care or through screening of patients in the waiting room or from a list in a primary care physician's practice Exclusion Criteria Studies that recruited patients from community-based centres specializing in mental health care |
Face-to-Face CBT Standardized Mean Differences for Posttreatment Depression Scores Compared With Control 7 studies WMD = −0.30 (95% CI: −0.48 to −0.13) Response (defined as at least a 50% score reduction on a depression rating scale) OR = 1.58 (95% CI: 1.11–2.26) NNT = 10 (95% CI: 5–47) Remission (defined as having a symptom score below a fixed threshold) OR = 1.49 (95% CI: 0.90–2.46) |
The reporting of intervention details in usual care groups and of co-interventions (e.g., pharmacotherapy) in the groups receiving psychological treatment was often insufficient. One-third of trials were considered to have a low risk of bias. The reporting of treatment discontinuation, dropout from the study, and loss to follow-up rarely provided sufficient detail to assess whether attrition was a result of acceptability of the treatment or organizational problems. No study reported adverse events or adverse effects for psychological treatments (not even studies including a pharmacotherapy treatment group). The authors reported that given the limited number, rather low quality, and considerable heterogeneity of the available studies, the findings of their review must be interpreted carefully. |
| Churchill et al, 200122 | To conduct a systematic review of all controlled clinical trials in which brief (completed within a time limited framework of ≤ 20 sessions) psychological treatments were compared with one another or with usual care in the treatment of MDD. Therapies included CBT (and variants), interpersonal therapy, and supportive therapy. |
Treatment Provider No details reported Inclusion Criteria Adults aged 16–65 years of age Primary diagnosis of MDD (according to Research Diagnostic Criteria, DSM-3/4 criteria, ICD criteria, or other validated diagnostic instruments, or based on assessment of levels of depressive symptomatology through self-rated or clinician-rated validated instruments) Compared with each other or usual care Exclusion Criteria Marital/couples therapy |
CBT (and variants) vs. Usual Care/Wait List Control Posttreatment Recovery 12 trials (N = 654) OR = 3.42 (95% CI: 1.98–5.93) Mean Differences (Symptoms): Posttreatment 20 studies (N = 748) SMD = −1.0 (95% CI: −1.35 to −0.64) Mean Change in Symptoms from Baseline: Posttreatment 5 studies (N = 172) WMD = 2.38 (95% CI: 0.05–4.71) No Symptoms at Follow-Up 3 months 4 studies (N = 310) OR = 1.59 (95% CI: 0.65–3.90) Mean Differences (Symptoms): Follow-Up 1 month 4 studies (N = 152) SMD = −1.20 (95% CI: −2.10 to −0.31) 2 months 2 studies (N = 44) SMD = −0.73 (95% CI: −1.80 to 0.33) 3 months 2 studies (N = 155) SMD = −0.36 (95% CI: −0.68 to −0.04) 6 months 3 studies (N = 160) SMD = −0.73 (95% CI: −1.50 to 0.03) Mean Change in Symptom Levels From Baseline: Follow-Up 3 months 2 studies (N = 155) WMD = 7.11 (95% CI: 3.25–10.98) 6 months 2 studies (N = 144) WMD = 6.41 (95% CI: 2.48–10.34) Individual CBT vs. Group CBT Posttreatment Recovery 6 studies (N = 231) OR = 1.98 (95% CI: 1.11–3.54) Mean Difference (Symptoms) 8 studies (N = 283) WMD = −3.07 (95% CI: −4.69 to −1.45) Mean Change (Symptoms) No studies reported data No Symptoms at Follow-Up 6 months 2 studies (N = 113) OR = 1.28 (95% CI: 0.52–3.20) Mean Differences (Symptoms): Follow-Up 1 month 2 studies (N = 74) WMD = 5.20 (95% CI: 0.21–10.19) 2 months 3 studies (N = 84) WMD = 0.21 (95% CI: −3.53 to 3.96) 3 months 2 studies (N = 65) WMD = 0.25 (95% CI: −4.61 to 5.11) 6 months 4 studies (N = 155) WMD = 3.21 (95% CI: −2.18 to 8.60) Mean Change in Symptom Levels From Baseline: Follow-Up No studies reported data |
Low scores on internal-validity items were recorded for all but a small number of trials in the review. This, coupled with the inadequate reporting of methodology, resulted in low overall quality scores. Evaluation of psychotherapy poses methodological challenges that are not easily addressed within the context of RCTs. Blinding of therapists in RCTs of psychological treatments cannot be achieved by the inclusion of an inactive placebo psychotherapy arm. Individual therapist characteristics cannot be controlled, nor can the nature of the therapeutic encounter be predetermined or measured with absolute precision. The nature of psychotherapy requires active participation by patients, and it is possible that at least some would be able to identify prominent theoretical constructs during therapy thereby introducing potential bias on the part of the patient. The use of antidepressants in the studies was variable. More than half the studies included in the entire review excluded randomized patients who did not commence treatment or who later dropped out. The majority of the trials used the BDI to measure outcomes in terms of recovery from depressive symptoms. The BDI is a widely used self-rated instrument; however, it is limited to the measurements of symptomatic clinical outcomes. Patients with MDD are affected in many other aspects, and broader measures of levels of functioning, such as quality-of-life scales, might be more meaningful and sensitive to changes in patients. The use of quality-of-life measures was extremely rare in the included studies. Although many authors reported using manuals to standardize individual psychotherapy interventions, only 16% of all included studies monitored the psychological intervention through weekly supervision discussions with the therapists. Nearly 40% of all studies included in the review failed to monitor adherence to the psychotherapy interventions under evaluation. Funnel plots indicated that small negative trials might have been omitted in the literature. Publication bias and other reporting biases are very likely explanations for possible missing studies. The reporting of adverse effects resulting from psychological treatments was poor. Reasons for patient dropout were infrequently investigated or reported by the authors. More than half the studies used volunteer populations (through local radio and newspaper advertising and sometimes offering small cash payments to people who agreed to participate). Patients who volunteer to participate in intervention studies are a self-selected group who tend to experience generally lower morbidity rates than those who do not take part and whose motivation for treatment and attrition rates may differ from the experimental population and from the general patient population. |
| Cognitive Behavioural Therapy and Pharmacotherapy Versus Pharmacotherapy Only for Major Depressive Disorder | ||||
| Karyotaki et al, 201635 | To determine the effectiveness of combined pharmacotherapy and general psychotherapy vs. general psychotherapy or pharmacotherapy only in the treatment of patients with MDD at 6 months or longer postrandomization. Results for CBT were reported in subanalyses. |
Treatment Provider No details reported Inclusion Criteria RCTs Adults ≥ 18 years of age Acute- and maintenance-phase treatments Outcomes at 6 months or longer postrandomization Exclusion Criteria None reported |
Primary outcome = treatment response and sustained response Combined CBT and Antidepressants vs. CBT, Acute Phase Response ≥ 6 Months Postrandomization 5 comparisons OR = 1.51 (95% CI: 0.79–2.86) Response ≥ 1 Year Postrandomization 4 comparisons OR = 1.48 (95% CI: 0.59–3.71) Combined CBT and Antidepressants vs. Antidepressants, Acute Phase Response ≥ 6 Months Postrandomization 6 comparisons OR = 3.02 (95% CI: 1.74–5.25) Response ≥ 1 Year Postrandomization 4 comparisons OR = 3.37 (95% CI: 1.38–8.21) Maintenance CBT and Antidepressants vs. CBT No data reported Maintenance CBT and Antidepressants vs. Antidepressants Response ≥ 6 Months Postrandomization 4 comparisons OR = 1.79 (95% CI: 1.19–2.70) Response ≥ 1 Year Postrandomization No data reported |
For trials on acute-phase treatment, the duration of follow-up ranged from 6 to 48 months after randomization. For maintenance studies, patients entered into either a maintenance psychotherapy combined with antidepressants or maintenance antidepressants group and were followed for 6 to 24 months. Acute-phase treatment had a duration ranging from 6 to 29 sessions, while maintenance-phase psychotherapeutic interventions consisted of 6 to 20 sessions conducted either weekly, biweekly, or monthly. Both older and newer antidepressants were used, including amitriptyline, fluoxetine, fluvoxamine, imipramine, nortriptyline, and sertraline. Overall, there was a general high risk of bias in the RCTs, according to the Cochrane risk-of-bias tool. |
| Amick et al, 201536 | To compare the benefits and harms of second-generation antidepressants and CBT in the initial treatment of a current episode of MDD in adults. |
Treatment Provider No details reported Inclusion Criteria RCTs Adults ≥ 18 years of age Acute-phase MDD Exclusion Criteria ≤ 18 years of age Patients with perinatal depression, seasonal affective disorder, psychotic depression, or treatment-resistant depression |
Second-Generation Antidepressants vs. CBT Monotherapy Remission: 3 trials (N = 432); risk ratio: 0.98 (95% CI 0.73–1.32) Response: 5 trials (N = 660); risk ratio: 0.91 (95% CI: 0.77–1.07) Overall discontinuation of treatment: 4 trials (N = 646); risk ratio: 1.00 (95% CI: 0.55–1.81) Discontinuation of treatment because of adverse effects: 3 trials (N = 632); risk ratio: 2.54 (95% CI: 0.39–16.47) Second-Generation Antidepressants vs. Combination of Second-Generation Antidepressants and CBT Remission: 2 trials (N = 376); risk ratio: 1.06 (95% CI: 0.82–1.38) Response: 2 trials (N = 376); risk ratio: 1.03 (95% CI: 0.85–1.26) Overall discontinuation of treatment: 2 trials (N = 256); risk ratio: 0.77 (95% CI: 0.37–1.60) Discontinuation of treatment because of adverse effects: 2 trials (N = 256); risk ratio: 2.93 (95% CI: 0.72–11.91) |
According to the authors, the type, training, and experience of the clinicians who provided the interventions were quite diverse. The authors reported that the overall strength of evidence was low, based on methods guidance for the Evidence-Based Practice Centers Program of the Agency for Healthcare Research and Quality. |
| Cognitive Behavioural Therapy Versus Pharmacotherapy Only for Major Depressive Disorder | ||||
| Cuijpers et al, 201337 | To compare the effects of acute-phase CBT without any subsequent continuation treatment with the effects of pharmacotherapy that either were continued or discontinued across 6 to 18 months of follow-up. |
Treatment Provider No details reported Inclusion Criteria RCTs Adults ≥ 18 years of age Acute-phase MDD Follow-up of 6–18 months Exclusion Criteria Studies in which CBT was continued during follow-up (although a maximum of 5 booster sessions during follow-up was allows as long as these were not regularly planned) Depression not diagnosed with a standardized diagnostic interview (e.g., structured clinical interview for DSM disorders) Studies in inpatients Studies in adolescents |
9 studies N = 506 patients (CBT n = 271; pharmacotherapy n = 235) Number of CBT treatment sessions ranged from 18 to 24. During the follow-up phase, 3 studies offered up to 4 CBT booster sessions, whereas the other 6 did not offer any additional treatment. The overall quality of the studies was relatively high, compared with the quality of studies on psychotherapy for adult depression in general. Outcome = number of patients who responded to treatment and remained well. Although at least some of the follow-ups were long enough for patients free from relapse to have met the criteria for recovery, the authors used the term “relapse” to refer to all instances of symptom return. Acute-Phase CBT vs. Continuation Pharmacotherapy 5 studies compared 1-year outcomes OR = 1.62 (95% CI: 0.97–2.72) Heterogeneity was zero (95% CI: 0%–79%) NNT = 10 (95% CI not reported) Acute-Phase CBT vs. Pharmacotherapy Discontinuation 8 studies compared 1-year outcomes OR = 2.61 (95% CI: 1.58–4.31) Heterogeneity was zero (95% CI: 0%–68%) NNT = 5 (95% CI: 4–11) |
Small number of studies. Small number of patients within the studies. Variation in the methods used between the studies in terms of drugs, measures and other characteristics. Variability in when pharmacotherapy was discontinued across the studies. |
| Cognitive Behavioural Therapy Versus Usual Care for Generalized Anxiety Disorder | ||||
| Cuijpers et al, 201620 | To meta-analyze RCTs to determine the efficacy of CBT for the acute treatment of GAD compared with control (wait list, usual care, or pill placebo). A subset analysis was conducted for GAD (the study included GAD, social anxiety disorder, and panic disorder). The purpose of the overall study was to report the current best evidence of the effects of CBT in the treatment of GAD, panic disorder, social anxiety disorder, and MDD. |
Treatment Provider No details reported Inclusion Criteria RCTs Recruited patients met diagnostic criteria (e.g., DSM) Therapies that used individual, group, or guided self-help formats Exclusion Criteria Self-guided therapies without any professional support To calculate effect sizes, all measures examining anxiety symptoms (e.g., Beck Anxiety Inventory, PSWQ) were used |
31 studies on GAD were identified. Pooled Effect Size 31 comparisons SMD = 0.80 (95% CI: 0.67–0.93) NNT = 3.58 The Eggers test for publication bias was significant (intercept: 1.60 [95% CI: 0.38–2.83], P = .006). Waitlist Control SMD = 0.85 (95% CI: 0.72–0.99) NNT = 3.35 Usual Care SMD = 0.45 (95% CI: 0.26–0.64) NNT = 6.93 Pill Placebo SMD = 1.32 (95% CI: 0.83–1.81) NNT = 2.08 |
The methodological quality of most studies was low or unknown, according to the Cochrane risk-of-bias tool. Nine of the 31 studies were rated as high quality. The number of treatment sessions varied from 1 to 25. The deadline for the literature search was August 14, 2015. For publication bias with regard to GAD, it was estimated that about one-quarter of the studies were missing; after adjusting for these missing studies, the effect size dropped from g = 0.80 to g = 0.59 (95% CI: 0.44–0.75). |
| Cuijpers et al, 201438 | To meta-analyze RCTs of psychological treatments for GAD. A subset analysis was conducted for CBT. |
Treatment Provider No details reported Inclusion Criteria RCTs of psychological treatments compared with control (wait list, usual care, or placebo) Adults ≥ 18 years of age Patients meeting diagnostic criteria for GAD according to a formal diagnostic interview Exclusion Criteria Patients ≤ 18 years of age |
CBT vs. Control Post-Test 28 comparisons SMD = 0.90 (95% CI: 0.75–1.05) NNT = 2.10 |
There is large overlap in the studies included in this meta-analysis and the 2016 analysis by Cuijpers et al.20 The authors stated that the effects of psychotherapies may also have been overestimated because of publication bias. Publication bias was assessed for all psychotherapies together and not broken down specifically for CBT. Many studies did not provide follow-up assessments. According to the authors:
|
| Hunot et al, 200711 | To examine the efficacy of psychological treatments compared with treatments as usual/wait list for patients with GAD. |
Treatment Provider Varied (i.e., clinical psychologists; doctoral-, senior-, or advanced-level CBT therapists; “experienced therapists”; “therapists”) Inclusion Criteria RCTs Adults 18–75 years of age treated in a primary, secondary, or community setting Use a formal standardized interview to diagnose GAD based on ICD or DSM criteria Any comorbidity in patients must be secondary to the diagnosis of GAD (however, studies involving patients with a comorbid psychiatric diagnosis of substance-related disorder, schizophrenia, or psychotic disorder were excluded) Exclusion Criteria Inpatients |
CBT vs. Usual Care/Wait List 13 studies Primary Outcomes Clinical Response Posttreatment 8 studies (N = 334) 3 studies used clinician-rated composite measure of anxiety severity to assess clinical response; 5 used structured diagnostic interviews RR = 0.64 (95% CI: 0.55–0.74) Reduction in Anxiety Symptoms Posttreatment 12 studies (N = 350) Measures to assess anxiety symptoms comprised the SCID (3 studies), ADIS (2 studies), HAM-A (5 studies), and Zung Anxiety Inventory (2 studies) SMD = −1.00 (95% CI: −1.24 to −0.77) Secondary Outcomes: Posttreatment Reduction in Worry/Fear Symptoms 9 studies (N = 256) Measures included the STAI-T (3 studies), PSWQ (5 studies), and Fear Survey Questionnaire (1 study) SMD = −0.90 (95% CI: −1.16 to −0.64) Reduction in Depressive Symptoms 11 studies (N = 317) Measures included the HDRS (1 study), BDI (9 studies), and the depression subscale of the GHQ-28 (1 study) SMD = −0.96 (95% CI: −1.20 to −0.72) Improvement in Social Functioning 3 studies (N = 69) Measures included the social functioning subscale of the SF-36 (2 studies) and the extraversion subscale of the Eysenck Personality Inventory SMD = 1.01 (95% CI: 0.00–2.03) Improvement in Quality of Life 3 studies (N = 112) Measures included the SF-36 (2 studies) and the Quality-of-Life Inventory (1 study) SMD = 0.44 (95% CI: 0.06–0.82) Adverse Effects No studies reported data Individual or Group Therapy (Subgroup Analysis) 9 studies used individual therapy, and 4 studies used group therapy Clinical Response Ind: RR = 0.63 (95% CI: 0.51–0.76) Grp: RR = 0.66 (95% CI: 0.54–0.82) Anxiety Symptoms Ind: SMD = −0.98 (95% CI: −1.32 to −0.65) Grp: SMD = −1.02 (95% CI: −1.35 to −0.69) Worry Symptoms Ind: SMD = −0.92 (95% CI: −1.37 to −0.48) Grp: SMD = −0.66 (95% CI: −1.03 to −0.29) Depression Symptoms Ind: SMD = −1.06 (95% CI: −1.39 to −0.72) Grp: SMD = −0.86 (95% CI: −1.20 to −0.53) ≤ 8 or > 8 Sessions (Subgroup Analysis) 4 studies used ≤ 8 sessions, and 9 studies used > 8 sessions Clinical Response ≤ 8: RR = 0.49 (95% CI: 0.26–0.91) >8: RR = 0.66 (95% CI: 0.57–0.76) Anxiety Symptoms ≤ 8: SMD = −1.00 (95% CI: −1.56 to −0.44) > 8: SMD = −1.00 (95% CI: −1.26 to −0.74) Worry Symptoms ≤ 8: SMD = −0.62 (95% CI: −1.50 to 0.27) > 8: SMD = −0.93 (95% CI: −1.20 to −0.65) Depression Symptoms ≤ 8: SMD = −1.35 (95% CI: −2.03 to −0.66) > 8: SMD = −0.91 (95% CI: −1.16 to −0.65) |
Study quality was assessed according to the criteria set out in the Cochrane Handbook. Overall, there was a moderate risk of bias in the studies based on unclear allocation concealment. All studies were randomized; however, none provided information on the methods used. Allocation concealment in most studies remains unknown. 72% of all studies in the review used blind assessors. No studies reported whether integrity of blinding was assessed. Studies were mostly small, with a mean sample size of 54 patients. One study included a sample size calculation. 76% of studies used manuals or protocols to standardize treatment approaches for CBT together with the employment of therapists who were experienced in the psychological model under examination. Testing therapists’ fidelity to treatment manuals through the systematic or random checking of audiotapes by independent clinicians is an additional key methodological aspect of assessing psychological studies to ensure that any observed treatment effect can be attributed to specific components and characteristics of the model. 52% of the included studies tested therapists’ treatment fidelity; therefore, there is no certainty in many studies that therapists were adhering to the required psychological model. 66% of studies allowed for the concurrent use of benzodiazepines or antidepressants either in ongoing use, as new courses during the trial period, or in follow-up. Adherence to ongoing treatment was reported in 4 studies that presented mean attendance rates at therapy sessions or adherence to homework assignments. Publication bias was assessed for the two primary outcomes. For clinical response, the funnel plot showed possible asymmetry, which might suggest that small trials with negative outcomes were not included in the review. For reduction in anxiety symptoms, the funnel plot showed a more symmetrical spread. |
| Interpersonal Therapy Versus Usual Care for Major Depressive Disorder | ||||
| Jakobsen et al, 201146 | To systematically review RCTs to determine beneficial and harmful effects of interpersonal therapy versus usual care. |
Provider of Treatment No details reported Inclusion Criteria Adults ≥ 17 years of age Primary diagnosis of MDD based on standardized criteria (e.g., DSM or ICD) Exclusion Criteria Comorbid serious somatic illness Late-life depression (≥ 65 years of age) Pregnancy-related depression Drug or alcohol dependence–related depression |
Depressive Symptoms 4 trials (N = 553) HDRS: WMD = −3.53 (95% CI: −4.91 to −2.16), P < .0001 BDI: WMD = −3.09 (95% CI: −5.35 to −0.83), P = .007 Remission (HDRS < 8) (event = patient not remitting) 3 trials (N = 430) OR = 0.36 (95% CI: 0.24–0.55), P = .00001 Adverse Events Adverse events were reported narratively; no statistics provided Quality of Life None of the RCTs reported this outcome |
All trials had a high risk of bias. Adverse events were not thoroughly reported. The duration of treatment ranged from 5 weeks of treatment to 16 weekly sessions followed by 4 monthly sessions. Four studies used individual treatment, and one study used both individual and group therapy. The length of follow-up was not reported. The extent and form of usual care varied greatly across studies. |
| Clarke et al, 201530 | To determine the effectiveness of nonpharmacological interventions compared with control in patients who have recovered from MDD. A subset analysis was conducted for interpersonal therapy. |
Treatment Provider No details reported Inclusion Criteria Adults in full or partial remission from MDD were randomized to either a nonpharmacological intervention or a control condition (usual care, clinical management, or pharmacotherapy) Followed up for a minimum of 1 year after randomization Remission was any reduction in symptoms to below a diagnostic threshold or other threshold on a validated assessment tool Exclusion Criteria Studies that randomized patients to acute treatment even if they then followed them up after recovery |
6 trials Compared with controls, the average risk of developing a new MDE by 12 months was reduced by 22% for interpersonal therapy (RR = 0.78, 95% CI: 0.65–0.95) Data for relapse at 24 months were available for all 6 of the interpersonal therapy trials. The effect of interpersonal therapy was not sustained (RR = 0.92, 95% CI: 0.81–1.05) |
Considerable overlap in the content of the controls; e.g., antidepressant drugs were used in control groups described as “usual care” and as “clinical management,” as well as those described as “medication” arms. There was a large difference in the control event rate for relapse across trials (for 12-month data, range = 0.2–0.79). Overall, the authors reported that half the studies in the meta-analysis were unclear or at high risk of bias for attrition because of uncertainty about dropouts or because of high levels of attrition. The authors used GRADE for each intervention. Evidence was generally of low quality; reasons for downgrading were inconsistency of results, indirectness of evidence, imprecision, and reporting bias. All interpersonal therapy trials were conducted by related research groups from the University of Pittsburgh. All trials provided monthly sessions for the duration of follow-up. |
| Biesheuvel-Leliefeld et al, 201529 | To determine the effectiveness of psychological interventions in reducing relapse or recurrence rates of MDD. A subset analysis was reported for interpersonal therapy. |
Treatment Provider No details reported Inclusion Criteria RCTs Adults with recurrent MDD who were in remission (according to their own definition in the individual trial paper) at randomization Patients received a psychological intervention to reduce the risk of relapse or recurrence Control condition (usual care [routine clinical management, assessment only, no treatment, or waitlist control with unrestricted access to usual care] or antidepressant drugs) Studies reported relapse or recurrence rates using established screeners with a predefined cut-off point for MDD (HDRS, BDI, or diagnostic interview) All modes of delivery were included (face-to-face, group, follow-up booster sessions, Internet) Exclusion Criteria None reported |
3 trials (6 contrasts) Interpersonal therapy was delivered in individual sessions (varying from monthly maintenance sessions over 8 months to weekly maintenance sessions over 4 months) Duration of follow-up ranged from 17 to 156 weeks In total, 142 patients received interpersonal therapy Interpersonal Therapy vs. Usual Care Risk ratio: 0.41 (95% CI: 0.27–0.63) NNT = 6 Interpersonal Therapy vs. Antidepressant Drugs Risk ratio: 0.83 (95% CI: 0.50–1.38) NNT = not reported |
The authors classified the overall quality of evidence as low according to the GRADE criteria. There were differences in the methodological design of the trials, including the definitions of remission, recovery, relapse, and recurrence; the type and duration of interventions; and whether there was a preceding acute intervention in the same trial (e.g., usual care was often described inadequately, and information on the exact method of determining recurrence [interview vs. questionnaire] was sometimes not provided. Owing to nature of psychological interventions, and the difficulty of comparing these with placebo interventions, the highest-quality evidence may not be possible in such studies. Factors that lower quality of evidence, such as differences in interventions (e.g., owing to differences in client–therapist relations) and difficulties blinding patients, outcome reporters, and personnel, will likely remain in studies investigating the effects of psychological interventions. |
| Linde et al, 201521 | To determine the effectiveness of psychological treatments compared with usual care or placebo in the treatment of primary care patients with MDD. A subset analysis was conducted for face-to-face interpersonal therapy. |
Treatment Provider Varied (i.e., counsellors, nurses, psychiatrists, psychologists, psychotherapists, therapists) Inclusion Criteria Adults with unipolar MDD Patients had to be recruited through direct referral from a GP or other primary care physician not specialized in mental health care or through screening of patients in the waiting room or from a list in a primary care physician's practice Exclusion Criteria Studies that recruited patients from community-based centres specializing in mental health care |
Face-to-Face Interpersonal Therapy Standardized Mean Differences for Posttreatment MDD Scores Compared With Control 2 studies WMD = −0.24 (95% CI: −0.47 to −0.02) Response (defined as at least a 50% score reduction on a depression rating scale) OR = 1.28 (0.80–2.05) Remission (defined as having a symptom score below a fixed threshold) OR = 1.37 (0.81–2.34) |
The reporting of intervention details in usual care groups and of co-interventions (e.g., pharmacotherapy) in the groups receiving psychological treatment was often insufficient. One-third of trials were considered to have a low risk of bias. The reporting of treatment discontinuation, dropout from the study, and loss to follow-up rarely provided sufficient detail to assess whether attrition was a result of acceptability of the treatment or organizational problems. No study reported adverse events or adverse effects for psychological treatments (not even studies including a pharmacotherapy treatment group). The authors reported that given the limited number, rather low quality, and considerable heterogeneity of the available studies, the findings of their review must be interpreted carefully. |
| Churchill et al, 200122 | To conduct a systematic review of all controlled clinical trials in which brief (completed within a time-limited framework of ≤ 20 sessions) psychological treatments were compared with one another or with usual care in the treatment of MDD. Therapies included CBT (and variants), interpersonal therapy, and supportive therapy. |
Treatment Provider No details reported Inclusion Criteria Adults aged 16–65 years of age Primary diagnosis of MDD (according to Research Diagnostic Criteria, DSM-3/4 criteria, ICD criteria, or other validated diagnostic instruments, or based on assessment of levels of depressive symptomatology through self-rated or clinician-rated validated instruments) Compared with each other or usual care Exclusion Criteria Marital/couples therapy |
Interpersonal Therapy vs. Usual Care/Waitlist Control Posttreatment Recovery 1 study (N = 185) OR = 3.52 (95% CI: 1.91–6.51) Mean Differences (Symptoms): Posttreatment 1 study (N = 185) WMD = −3.21 (95% CI: −5.18 to −1.24) Mean Change in Symptoms From Baseline: Posttreatment 1 study (N = 185) WMD = 2.09 (95% CI: 0.04–4.14) No Symptoms at Follow-Up 8 months 1 study (N = 185) OR = 3.72 (95% CI: 2.03–6.81) Mean Differences (Symptoms): Follow-Up 8 months 1 study (N = 185) WMD = −3.77 (95% CI: −5.66 to −1.88) Mean Change in Symptom Levels From Baseline: Follow-Up 8 months 1 study (N = 185) WMD = 2.64 (95% CI: 0.56–4.72) |
Low scores on internal-validity items were recorded for all but a small number of trials in the review. This, coupled with the inadequate reporting of methodology, resulted in low overall quality scores. Evaluation of psychotherapy poses methodological challenges that are not easily addressed within the context of RCTs. Blinding of therapists in RCTs of psychological treatments cannot be achieved by the inclusion of an inactive placebo psychotherapy arm. Individual therapist characteristics cannot be controlled, nor can the nature of the therapeutic encounter be predetermined or measured with absolute precision. The nature of psychotherapy requires active participation by patients, and it is possible that at least some would be able to identify prominent theoretical constructs during therapy thereby introducing potential bias on the part of the patient. The use of antidepressants in the studies was variable. More than half the studies included in the entire review excluded randomized patients who did not commence treatment or who later dropped out. The majority of the trials used the BDI to measure outcomes in terms of recovery from depressive symptoms. (The BDI is a widely used self-rated instrument; however, it is limited to the measurements of symptomatic clinical outcomes. Patients with MDD are affected in many other aspects, and broader measures of levels of functioning, such as quality-of-life scales, might be more meaningful and sensitive to changes in patients. The use of quality-of-life measures was extremely rare in the included studies. Although many authors reported using manuals to standardize individual psychotherapy interventions, only 16% of all included studies monitored the psychological intervention through weekly supervision discussions with the therapists. Nearly 40% of all studies included in the review failed to monitor adherence to the psychotherapy interventions under evaluation. Funnel plots indicated that small negative trials might have been omitted in the literature. Publication bias and other reporting biases are very likely explanations for possible missing studies. The reporting of adverse effects resulting from psychological treatments was poor. Reasons for patient dropout were infrequently investigated or reported by the authors. More than half the studies used volunteer populations (through local radio and newspaper advertising and sometimes offering small cash payments to people who agreed to participate). Patients who volunteer to participate in intervention studies are a self-selected group who tend to experience generally lower morbidity rates than those who do not take part and whose motivation for treatment and attrition rates may differ from the experimental population and from the general patient population. |
| Supportive Therapy Versus Usual Care for Major Depressive Disorder | ||||
| Churchill et al, 200122 | To conduct a systematic review of all controlled clinical trials in which brief (completed within a time-limited framework of ≤ 20 sessions) psychological treatments were compared with one another or with usual care in the treatment of MDD. Therapies included CBT (and variants), interpersonal therapy, and supportive therapy. |
Treatment Provider No details reported Inclusion Criteria Adults aged 16–65 years of age Primary diagnosis of MDD (according to Research Diagnostic Criteria, DSM-3/4 criteria, ICD criteria, or other validated diagnostic instruments, or based on assessment of levels of depressive symptomatology through self-rated or clinician-rated validated instruments) Compared with each other or usual care Exclusion Criteria Marital/couples therapy |
Supportive Therapy vs. Usual Care/Waitlist Control Posttreatment Recovery 4 studies (N = 118) OR = 2.71 (95% CI: 1.19–6.16) Mean Differences (Symptoms): Posttreatment 4 studies (N = 123) SMD = −0.42 (95% CI: −0.78 to −0.06) Mean Change in Symptoms From Baseline Posttreatment 2 studies (N = 79) SMD = −0.01 (95% CI: −0.45 to 0.43) No Symptoms at Follow-Up No data available Mean Differences (Symptoms): Follow-Up 2 months 1 study (N = 22) SMD = −0.27 (95% CI: −1.11 to 0.57) 6 months 1 study (N = 17) SMD = −2.01 (95% CI: −3.27 to −0.75) Mean Change in Symptom Levels From Baseline: Follow-Up 2 months 1 study (N = 22) WMD = −4.30 (95% CI: −17.05 to 8.45) |
Low scores on internal-validity items were recorded for all but a small number of trials in the review. This, coupled with the inadequate reporting of methodology, resulted in low overall quality scores. Evaluation of psychotherapy poses methodological challenges that are not easily addressed within the context of RCTs. Blinding of therapists in RCTs of psychological treatments cannot be achieved by the inclusion of an inactive placebo psychotherapy arm. Individual therapist characteristics cannot be controlled, nor can the nature of the therapeutic encounter be predetermined or measured with absolute precision. The nature of psychotherapy requires active participation by patients, and it is possible that at least some would be able to identify prominent theoretical constructs during therapy thereby introducing potential bias on the part of the patient. The use of antidepressants in the studies was variable. More than half the studies included in the entire review excluded randomized patients who did not commence treatment or who later dropped out. The majority of the trials used the BDI to measure outcomes in terms of recovery from depressive symptoms. The BDI is a widely used self-rated instrument; however, it is limited to the measurements of symptomatic clinical outcomes. Patients with MDD are affected in many other aspects, and broader measures of levels of functioning, such as quality-of-life scales, might be more meaningful and sensitive to changes in patients. The use of quality-of-life measures was extremely rare in the included studies. Although many authors reported using manuals to standardize individual psychotherapy interventions, only 16% of all included studies monitored the psychological intervention through weekly supervision discussions with the therapists. Nearly 40% of all studies included in the review failed to monitor adherence to the psychotherapy interventions under evaluation. Funnel plots indicated that small negative trials might have been omitted in the literature. Publication bias and other reporting biases are very likely explanations for possible missing studies. The reporting of adverse effects resulting from psychological treatments was poor. Reasons for patient dropout were infrequently investigated or reported by the authors. More than half the studies used volunteer populations (through local radio and newspaper advertising and sometimes offering small cash payments to people who agreed to participate). Patients who volunteer to participate in intervention studies are a self-selected group who tend to experience generally lower morbidity rates than those who do not take part and whose motivation for treatment and attrition rates may differ from the experimental population and from the general patient population. |
| Cuijpers et al, 201214 | To conduct a meta-analysis of RCTs to determine the efficacy of supportive therapy compared with control (waitlist or usual care) or pharmacotherapy for the treatment of MDD. |
Treatment Provider Varied (i.e., nurses, psychiatrists, psychologists, social workers, specialists in counselling, and trained nonspecialists) Inclusion Criteria RCTs Adults with MDD assessed via diagnostic interview Exclusion Criteria Studies in which nonprofessional therapists were used Patients ≤ 18 years of age Patients who did not have MDD |
Supportive Therapy vs. Control Overall Mean Effect Size 18 comparisons g = 0.58 (95% CI: 0.45–0.72), P < .001 NNT = 3.14 HDRS Only 5 comparisons g = 0.46 (95% CI: 0.19–0.73), P < .001 NNT = 3.91 BDI Only 8 comparisons g = 0.52 (95% CI: 0.32–0.73), P < .001 NNT = 3.50 3–6 Months of Follow-Up 4 comparisons g = 0.22 (95% CI: −0.05 to 0.50) NNT = 8.06 9–12 Months of Follow-Up 4 comparisons g = 0.09 (95% CI: −0.12 to 0.31) NNT = 20.00 Supportive Therapy vs. Pharmacotherapy Overall Effect Size 4 comparisons g = −0.18 (95% CI −0.59 to 0.23) NNT: ns |
The majority of the studies did not examine long-term effects. Most studies focused on mild to moderate MDD The quality of the studies varied. Eight studies met all 4 quality criteria (the Cochrane Collaboration risk-of-bias criteria), while 12 studies met 3 of the 4 criteria. |
Abbreviations: ADIS, Anxiety Disorder Interview Schedule; BDI, Becks Depression Inventory; CBT, cognitive behavioural therapy; CI, confidence interval; DSM, Diagnostic and Statistical Manual; GAD, generalized anxiety disorder; GHQ-28, General Health Questionnaire-28; GP, general practitioner; GRADE, Grading of Recommendations Assessment, Development, and Evaluation; HAM-A, Hamilton Anxiety Rating Scale; HDRS, Hamilton Depression Rating Scale; ICD, International Statistical Classification of Diseases and Related Health Problems; MDD, major depressive disorder; MDE, major depressive episode; NNT, number needed to treat; ns, not significant; OR, odds ratio; PSWQ, Penn State Worry Questionnaire; RCT, randomized controlled trial; RR, relative risk; SCID, Structured Clinical Interview for DSM-4; SF-36; 36-Item Short-Form Health Survey; SMD, standardized mean difference; STAI-T, State–Trait Anxiety Inventory; WMD, weighted mean difference.
Appendix 4: Results of Applicability Checklist for Studies Included in Economic Literature Review
Table A3:
Assessment of the Cost-Effectiveness of CBT or Interpersonal Therapy for Major Depressive Disorder and Generalized Anxiety Disorder
| Objective: To assess the cost-effectiveness of CBT or interpersonal therapy for the treatment of adults with major depressive disorder and/or generalized anxiety disorder in Ontario | |||||
|---|---|---|---|---|---|
| Author, Year | Is the study population similar to the question? | Are the interventions similar to the question? | Is the health care system in which the study was conducted sufficiently similar to the current Ontario context? | Was/were the perspective(s) clearly stated, and what were they? | Are estimates of relative treatment effect from the best available source? |
| Wiles et al, 201668 | Partially, severe and treatment-resistant depression | Yes | No, United Kingdom | Yes | Yes |
| Koeser et al, 201569 | Yes | Partially | No, United Kingdom | Yes | Yes |
| Hollinghurst et al, 201467 | Yes | Yes | No, United Kingdom | Yes | Yes |
| Kafali et al, 201466 | Partially, uninsured Latino women | Yes | No, Puerto Rico/United States | No | Yes |
| Prukkanone et al, 201265 | Partially, Thai adults with MDD | Partially | No, Thailand | Yes | Unclear |
| Brown et al, 201157 | Yes | Partially | No, United Kingdom | Yes | Unclear |
| Holman et al, 201164 | Partially, older adults with MDD | Partially | No, United Kingdom | Yes | Yes |
| Sava et al, 200962 | Yes | Partially | No, Romania | Yes | Yes |
| Sado et al, 200963 | Partially, Japanese population | Yes | No, Japan | Yes | Unclear |
| Bosmans et al, 200758 | Yes | Yes | No, Netherlands | Yes | Yes |
| Simon et al, 200661 | Yes | Partially | No, United Kingdom | Yes | Yes |
| Vos et al, 200556 | Yes | Yes | No, Australia | Yes | Unclear |
| Revicki et al, 200560 | Partially, low-income women | Partially | No, United States | Yes | Yes |
| Heuzenroeder et al, 200455 | Yes | Yes | No, Australia | Yes | Unclear |
| Scott et al, 200359 | Partially, chronic MDD | Partially | No, United Kingdom | Yes | Unclear |
| Author, Year | Are all future costs and outcomes discounted? (If yes, at what rate?) | Is the value of health effects expressed in terms of quality-adjusted life-years? | Are costs and outcomes from other sectors fully and appropriately measured and valued? | Overall judgment (Directly applicable/partially applicable/not applicable) |
|---|---|---|---|---|
| Wiles et al, 201668 | Yes, 3.5% | Yes | Yes | Partially applicable |
| Koeser et al, 201569 | Yes, 3.5% | Yes | Yes | Partially applicable |
| Hollinghurst et al, 201467 | No, 1 year (0%) | Yes | Yes | Partially applicable |
| Kafali et al, 201466 | No, 6 months | No | Unclear | Not applicable |
| Prukkanone et al, 201265 | Yes, 3% | Yes, DALY | Unclear | Partially applicable |
| Brown et al, 201157 | No, 0% | No | Yes | Partially applicable |
| Holman et al, 201164 | No, 0% | No | Yes | Not applicable |
| Sava et al, 200962 | No, 0% | No | Yes | Not applicable |
| Sado et al, 200963 | No, 0% | Yes | Yes | Partially applicable |
| Bosmans et al, 200758 | No, 0% | Yes | Yes | Partially applicable |
| Simon et al, 200661 | No, 0% | Yes | Yes | Partially applicable |
| Vos et al, 200556 | Yes, 3% | Yes, DALY | Yes | Partially applicable |
| Revicki et al, 200560 | No, 0% | No | Unclear | Partially applicable |
| Heuzenroeder et al, 200455 | No, 0% | No | Yes | Partially applicable |
| Scott et al, 200359 | Yes, 6% | No | Yes | Not applicable |
Abbreviations: CBT, cognitive behavioural therapy; DALY, disability-adjusted life-year; MDD, major depressive disorder. Note: Response options for all items were “yes,” “partially,” “no,” “unclear,” and “NA” (not applicable).
Appendix 5: Methodological Quality of Studies Included in Economic Literature Review
Table A4:
Assessment of the Cost-Effectiveness of CBT or Interpersonal Therapy for Major Depressive Disorder and Generalized Anxiety Disorder
| Objective: To assess the cost-effectiveness of CBT and interpersonal therapy for the treatment of adults with major depressive disorder and/or generalized anxiety disorder in Ontario | |||||||
|---|---|---|---|---|---|---|---|
| Author, Year | Does the model structure adequately reflect the nature of the health condition under evaluation? | Is the time horizon sufficiently long to reflect all important differences in costs and outcomes? | Are all important and relevant health outcomes included? | Are the estimates of relative treatment effects obtained from best available sources? | Do the estimates of relative treatment effect match the estimates contained in the clinical report? | Are all important and relevant (direct) costs included in the analysis? | Are the estimates of resource use obtained from best available sources? |
| Wiles et al, 201668 | NA | Yes | Partially | Yes | Partially | Yes | Yes |
| Koeser et al, 201569 | Partially | No | Yes | Yes | Partially | Yes | Yes |
| Hollinghurst et al, 201467 | NA | No | No | Yes | Partially | Yes | Yes |
| Kafali et al, 201466 | NA | No | No | Yes | No | Yes | Yes |
| Prukkanone et al, 201265 | Partially | Yes | No | Unclear | Partially | Yes | Unclear |
| Brown et al, 201157 | NA | No | No | Unclear | No | Yes | Yes |
| Holman et al, 201164 | NA | No | No | Yes | No | Yes | Yes |
| Sava et al, 200962 | NA | No | No | Yes | No | Yes | Yes |
| Sado et al, 200963 | Partially | No | Yes | Unclear | No | Yes | Yes |
| Bosmans et al, 200758 | NA | No | No | Yes | No | Yes | Yes |
| Simon et al, 200661 | Partially | No | Yes | Yes | Partially | Yes | Yes |
| Vos et al, 200556 | Unclear | Yes | Partially | Unclear | No | Yes | Yes |
| Revicki et al, 200560 | NA | No | No | Yes | No | Yes | Yes |
| Heuzenroeder et al, 200455 | Unclear | No | No | Yes | No | Yes | Yes |
| Scott et al, 200359 | NA | No | No | Unclear | No | Yes | Yes |
| Author, Year | Are the unit costs of resources obtained from best available resources? | Is an appropriate incremental analysis presented or can it be calculated from the reported data? | Are all important and uncertain parameters subjected to appropriate sensitivity analysis? | Is there a potential conflict of interest? | Overall assessment including applicability to the project (Minor limitations/potentially serious limitations/very serious limitations) |
|---|---|---|---|---|---|
| Wiles et al, 201668 | Yes | Partially | No | Unclear | Potentially serious limitations |
| Koeser et al, 201569 | Yes | Yes | Unclear | No | Potentially serious limitations |
| Hollinghurst et al, 201467 | No | No | No | Unclear | Potentially serious limitations |
| Kafali et al, 201466 | Yes | No | No | Unclear | Potentially serious limitations |
| Prukkanone et al, 201265 | Unclear | No | No | Unclear | Potentially serious limitations |
| Brown et al, 201157 | Yes | No | No | Unclear | Potentially serious limitations |
| Holman et al, 201164 | Yes | No | No | Unclear | Potentially serious limitations |
| Sava et al, 200962 | Unclear | No | No | Unclear | Very serious limitations |
| Sado et al, 200963 | Unclear | Yes | Yes | Unclear | Potentially serious limitations |
| Bosmans et al, 200758 | Yes | No | Unclear | Unclear | Potentially serious limitations |
| Simon et al, 200661 | Yes | Yes | Unclear | Unclear | Potentially serious limitations |
| Vos et al, 200556 | Yes | No | No | Unclear | Potentially serious limitations |
| Revicki et al, 200560 | Yes | No | No | Unclear | Potentially serious limitations |
| Heuzenroeder et al, 200455 | Yes | No | No | Unclear | Potentially serious limitations |
| Scott et al, 200359 | Yes | No | No | Unclear | Potentially serious limitations |
Abbreviation: CBT, cognitive behavioural therapy.
Note: Response options for all items were “yes,” “partially,” “no,” “unclear,” and “NA” (not applicable).
Appendix 6: Incremental Cost-Effectiveness Scatter Plot: Individual CBT Provided by Nonphysicians Versus Group CBT Provided by Nonphysicians
Figure A1: Scatter Plots of 1,000 Simulated Pairs of Incremental Costs and Effects in the Cost-Effectiveness Plane: Individual CBT Provided by Nonphysicians Versus Group CBT Provided by Nonphysicians.
Abbreviations: CBT, cognitive behavioural therapy; ICER, incremental cost-effectiveness ratio; WTP, willingness-to-pay threshold. All costs are in 2017 Canadian dollars and discounted at 1.5%. Effectiveness is expressed in quality-adjusted life-years (QALYs). Negative QALYs indicate that the individual CBT strategy was associated with worse quality-adjusted survival, and negative costs indicate that the individual CBT strategy saved money relative to the group CBT strategy. The diagonal line indicates a willingness-to-pay threshold of $100,000 per QALY. The incremental cost-effectiveness ratio ($192,618/QALY gained) is the slope of a straight line from the origin that passes through the (0.01 QALY, $2,767) coordinate. A 95% confidence ellipse covers 95% of the estimated joint density and was used to represent uncertainty around the incremental cost-effectiveness ratio estimated in the probabilistic sensitivity analysis.
Appendix 7: Budget Impact Analysis—Scenario 1: Generalized Anxiety Disorder Population Only
Table A5:
Generalized Anxiety Disorder Population Scenario—Expected Number of Patients at Risk after Adopting CBT in Ontario, 2017 to 2021
| Strategy, Base Case Analysis | Year Post-Diagnosis of New Major Depressive Disorder, N | ||||
|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | |
| Usual care | 29,409 | 88,097 | 175,916 | 292,719 | 438,348 |
| Group CBT by nonphysicians or physicians | 29,409 | 88,111 | 175,969 | 292,842 | 438,562 |
| Individual CBT by nonphysicians or physicians | 29,409 | 88,123 | 176,004 | 292,905 | 438,660 |
Abbreviation: CBT, cognitive behavioural therapy.
Table A6:
Generalized Anxiety Disorder Population Scenario—Average Costs per Patient Each Year Post-Diagnosis, Patients at Risk, Ontario, 2017 to 2021
| Strategy, Base Case Analysis | Year Post-Diagnosis of New Generalized Anxiety Disorder, $ | ||||
|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | |
| Usual care | 3,008.39 | 3,226.39 | 3,363.89 | 3,507.44 | 3,690.22 |
| Group CBT by nonphysicians | 3,355.94 | 3,272.39 | 3,370.63 | 3,460.92 | 3,593.86 |
| Group CBT by physicians | 3,630.83 | 3,487.69 | 3,582.67 | 3,671.76 | 3,797.14 |
| Individual CBT by nonphysicians | 3,876.21 | 4,458.51 | 3,050.58 | 3,874.28 | 3,966.30 |
| Individual CBT by physicians | 4,277.73 | 4,055.58 | 4,128.33 | 4,207.71 | 4,291.87 |
Abbreviation: CBT, cognitive behavioural therapy.
Appendix 8: Budget Impact Analysis—Scenario 2: Moderate to Severe Major Depressive Disorder or Generalized Anxiety Disorder
Table A7:
Moderate to Severe Major Depressive Disorder Scenario—Expected Number of Patients at Risk After Adopting CBT in Ontario, 2017 to 2021
| Strategy, Base Case Analysis | Year Post-Diagnosis of New Major Depressive Disorder, N | ||||
|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | |
| Usual care | 9,486 | 28,418 | 56,749 | 94,430 | 141,405 |
| Group CBT by nonphysicians or physicians | 9,486 | 28,421 | 56,761 | 94,459 | 141,463 |
| Individual CBT by nonphysicians or physicians | 9,486 | 28,428 | 56,780 | 94,494 | 141,515 |
Abbreviation: CBT, cognitive behavioural therapy.
Table A8:
Moderate to Severe Major Depressive Disorder Scenario—Average Costs per Patient Each Year Post-Diagnosis, Patients at Risk, Ontario, 2017 to 2021
| Strategy, Base Case Analysis | Year Post-Diagnosis of New Major Depressive Disorder, $ | ||||
|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | |
| Usual care | 3,069.70 | 3,212.51 | 3,356.39 | 3,493.36 | 3,689.22 |
| Group CBT by nonphysicians | 3,473.65 | 3,395.68 | 3,489.58 | 3,599.20 | 3,718.34 |
| Group CBT by physicians | 3,773.33 | 3,680.66 | 3,774.59 | 3,880.14 | 3,993.53 |
| Individual CBT by nonphysicians | 4,024.75 | 3,989.68 | 4,075.77 | 4,169.80 | 4,246.00 |
| Individual CBT by physicians | 4,449.62 | 4,435.83 | 4,526.72 | 4,615.92 | 4,682.88 |
Abbreviation: CBT, cognitive behavioural therapy.
Appendix 9: Budget Impact Analysis—Scenario 3: Costs Associated With CBT
Table A9:
CBT Treatment Costs Scenario—Expected Number of Patients at Risk After Adopting CBT in Ontario, 2017 to 2021
| Strategy, Base Case Analysis | Year Post-Diagnosis of New Major Depressive Disorder, N | ||||
|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | |
| Usual care | 29,644 | 88,802 | 177,323 | 295,060 | 441,855 |
| Group CBT by nonphysicians or physicians | 29,644 | 88,816 | 177,378 | 295,184 | 442,071 |
| Individual CBT by nonphysicians or physicians | 29,644 | 88,827 | 177,412 | 295,248 | 442,169 |
Abbreviation: CBT, cognitive behavioural therapy.
Table A10:
CBT Treatment Costs Scenario—Average Costs per Patient Each Year Post-Diagnosis of Major Depressive Disorder, Patients at Risk, Ontario, 2017 to 2021
| Strategy, Base Case Analysis | Year Post-Diagnosis of New Major Depressive Disorder, $ | ||||
|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | |
| Usual care | 191.62 | 150.83 | 147.51 | 144.35 | 139.17 |
| Group CBT by nonphysicians | 775.81 | 471.05 | 476.02 | 472.12 | 456.37 |
| Group CBT by physicians | 1,090.05 | 760.57 | 765.30 | 759.61 | 733.75 |
| Individual CBT by nonphysicians | 1,367.94 | 1,093.58 | 1,112.55 | 1,108.06 | 1,082.71 |
| Individual CBT by physicians | 1,818.58 | 1,544.62 | 1,568.65 | 1,562.73 | 1,526.82 |
Abbreviation: CBT, cognitive behavioural therapy.
Appendix 10: Letter of Information
LETTER OF INFORMATION
SUMMARY:
Health Quality Ontario (HQO) is conducting a formal assessment of Psychotherapy treatments for adult patients with Major Depressive Disorder and/or Generalized Anxiety Disorder, to better understand how these treatment options should be funded by the healthcare system. An important part of this assessment involves speaking to patients and families of those who suffer (or may have suffered) from these disorders, who may or may not have used psychotherapy for treatment. Our goal is to illuminate the lived-experience of patients and families who have experienced Major Depressive Disorder and/or Generalized Anxiety Disorder, and the context around psychotherapy treatment.
WHAT DO YOU NEED FROM ME?
-
✓
Willingness to share your story
-
✓
20–40 minutes of your time for a phone or in-person interview
-
✓
Permission to audio- (not video-) record the interview
WHY DO YOU NEED THIS INFORMATION?
Health Quality Ontario (HQO) is conducting a Health Technology Assessment of the effectiveness and safety of cognitive behavioural therapy, interpersonal therapy, and supportive therapy for adult patients with major depressive disorder and/or generalized anxiety disorder. As part of HQO's core function to promote health care supported by the best evidence available, established scientific methods are used to analyze the evidence for a wide range of health interventions, including diagnostic tests, medical devices, interventional and surgical procedures, health care programs and models of care. These analyses may be informed and complemented by input from a range of individuals, including patients and clinical experts, and serve as the basis recommendations about whether health care interventions should be publicly funded or not.
The perspective that you share will be useful to help provide context to the day-to-day realities of patients dealing with mental health issues and the decisions they face in terms of therapies. The ultimate goal of the project is to provide recommendations to the Ontario Health Technology Assessment Committee who advises the Ontario Ministry of Health and Long-term Care on the appropriateness of funding.
WHAT YOUR PARTICIPATION INVOLVES
If you agree to enroll, you will be asked to participate in an interview conducted by HQO staff. The interview will likely last 20–40 minutes. The session will be conducted in a private location and will be audio-taped. The interviewer will ask you questions about your lived experience with major depressive disorder and/or generalized anxiety disorder and your perspectives of psychotherapy treatment in Ontario.
Participation is voluntary. You may refuse to participate, refuse to answer any questions or withdraw before your interview. Withdrawal will in no way affect care you receive.
CONFIDENTIALITY
All information collected for the review will be kept confidential and privacy will be protected except as required by law. The results of this review will be published, however no identifying information will be released or published. Any records containing information from your interview will be stored securely.
RISKS TO PARTICIPATION:
There are no known physical risks to participating. Some participants may experience discomfort or anxiety after speaking about their lived experience. If this is the case, please contact any staff.
HEALTH QUALITY ONTARIO STAFF:
Appendix 11: Consent and Release Form
Consent and Release Form
This form is to be read and completed in accordance with the following instructions before it can be signed.
-
1.
I, _____ _____ allow Health Quality Ontario (Ontario Health Quality Council) to use to inform the development of an evidence based review:
Check off all appropriate boxes:
-
a)
___ a recording of my voice
-
b)
___ a quotation or summary of my opinion that I expressed during an interview
-
c)
___ name & contact information
-
a)
-
2.
Please read the following paragraphs before affixing your signature under section 3.
-
a)
Personal information collected pursuant to, and on this form, will be used for purposes described on this form and for no other purpose. Health Quality Ontario (Ontario Health Quality Council) acknowledges that you have provided this personal information freely and voluntarily. If you have any questions about this collection of this personal information, contact:
-
b)
By signing this form as indicated below, you agree to hereby release and forever discharge the Health Quality Ontario (Ontario Health Quality Council), its officers, employees, agents and representatives from any and all claims, demands, expenses, actions, causes of action and for any and all liability howsoever caused, arising out of, or in any way related to the collection, use and disclosure of information, recordings and images authorized to be collected pursuant to, or on this form.
-
c)
By signing this form as indicated below, you agree to forever waive any and all rights that you may have to the use of information and recordings that are authorized to be collected pursuant to, or on this form; and you acknowledge that all information, recordings and images shall hereafter remain the exclusive property of the Health Quality Ontario (Ontario Health Quality Council).
-
a)
-
3.
Signature is to be affixed in the appropriate space provided below.
I have read this form after it was completed, I understand and agree to be bound by its contents, and I am eighteen (18) years of age or over.
Signature _____
Print name _____
Date _____
Appendix 12: Interview Guide
Interview for Psychotherapy HTA
Intro
Explain HQO purpose, HTA process, and purpose of interview History of mental health condition (MDD or GAD) (general only)
Lived- Experience
Day-to-day routine
What is the impact of mental health condition on quality of life?
What is the impact on family?
Therapies
Experience with other therapies and mental health services
Decision-making in choosing therapies? Was it difficult to weigh up potential benefits and risks when deciding on which therapies to go with?
Availability of information surrounding mental health services – enough? Technology in mental health services.
Pharmacotherapy
Barriers to accessing therapies, including psychotherapy?
Psychotherapy
Experience with Psychotherapy – types, group v individual Expectations, barriers, benefits/drawbacks
Mental health services in Ontario – biggest challenge?
Contrast emotion (anxiety, worry) vs logic? As this applies to risk and side-effects?
Author contributions
This report was developed by a multidisciplinary team from Health Quality Ontario. The lead clinical epidemiologist was Kristen McMartin, the lead health economist was Olga Gajic-Veljanoski, the public and patient engagement specialist was David Wells, and the medical librarians were Caroline Higgins and Melissa Walter.
KEY MESSAGES
People with major depressive disorder experience depressed mood and loss of interest or pleasure in activities. People with generalized anxiety disorder experience persistent, excessive, and difficult-to-control worry. Often, people experience both disorders at the same time. Major depressive disorder and generalized anxiety disorder cause many symptoms that negatively affect work, education, and social interactions.
Treatments for these disorders consist of pharmacological interventions (medications) and psychological interventions (talk therapies). Three commonly used psychological interventions for major depressive disorder and generalized anxiety disorder are cognitive behavioural therapy (CBT), interpersonal therapy, and supportive therapy.
The objectives of this report were to assess the effectiveness and safety of CBT, interpersonal therapy, and supportive therapy for the treatment of adults with major depressive disorder and/or generalized anxiety disorder. We also assessed the cost-effectiveness of structured psychotherapy (CBT or interpersonal therapy) and calculated the budget impact of publicly funding structured psychotherapy. We then interviewed people with major depressive disorder and/or generalized anxiety disorder to learn about their experiences of these disorders and with different types of therapy.
Compared with usual care, treatment with CBT, interpersonal therapy, or supportive therapy has been found to reduce depression symptoms and increase response or recovery posttreatment. In people with generalized anxiety disorder, treatment with CBT has been found to reduce symptoms of anxiety, improve outcomes, and improve ratings of quality of life.
Compared with usual care, treatment with structured psychotherapy provided by physicians or nonphysicians, delivered as individual or group in-person therapy, represents good value for money. The most affordable option is structured group psychotherapy provided by nonphysicians, with the selective use of individual psychotherapy provided by nonphysicians or physicians for those who would benefit most from it.
People with major depressive disorder and/or generalized anxiety disorder reported positive experiences with psychotherapy but also a large number of barriers that prevented them from finding effective psychotherapy in a timely manner. People with whom we spoke reported wanting more freedom to choose the type of psychotherapy they received, than they are currently able to access.
Contributor Information
Health Quality Ontario:
Kristen McMartin, Olga Gajic-Veljanoski, David Wells, Caroline Higgins, and Melissa Walter
About Health Quality Ontario
Health Quality Ontario is the provincial advisor on the quality of health care. We are motivated by a single-minded purpose: Better health for all Ontarians.
Who We Are
We are a scientifically rigorous group with diverse areas of expertise. We strive for complete objectivity, and look at things from a vantage point that allows us to see the forest and the trees. We work in partnership with health care providers and organizations across the system, and engage with patients themselves, to help initiate substantial and sustainable change to the province's complex health system.
What We Do
We define the meaning of quality as it pertains to health care, and provide strategic advice so all the parts of the system can improve. We also analyze virtually all aspects of Ontario's health care. This includes looking at the overall health of Ontarians, how well different areas of the system are working together, and most importantly, patient experience. We then produce comprehensive, objective reports based on data, facts and the voice of patients, caregivers and those who work each day in the health system. As well, we make recommendations on how to improve care using the best evidence. Finally, we support large scale quality improvements by working with our partners to facilitate ways for health care providers to learn from each other and share innovative approaches.
Why It Matters
We recognize that, as a system, we have much to be proud of, but also that it often falls short of being the best it can be. Plus certain vulnerable segments of the population are not receiving acceptable levels of attention. Our intent at Health Quality Ontario is to continuously improve the quality of health care in this province regardless of who you are or where you live. We are driven by the desire to make the system better, and by the inarguable fact that better has no limit.
REFERENCES
- (1).Levav I, Rutz W. The WHO World Health Report 2001 new understanding–new hope. Isr J Psychiatry Relat Sci. 2002; 39 (1): 50–6. [PubMed] [Google Scholar]
- (2).Patten SB, Kennedy SH, Lam RW, O'Donovan C, Filteau MJ, Parikh SV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. I. Classification, burden and principles of management. J Affect Disord. 2009; 117 Suppl 1:S5–14. [DOI] [PubMed] [Google Scholar]
- (3).American Psychiatric Assocation. Diagnostic and statistical manual of mental disorders. 5th ed. Washington (DC): The Association; 2013. [Google Scholar]
- (4).Swinson R, Antony MM, Bleau P, Chokta P, Craven MA, Fallu A, et al. Management of anxiety disorders. Can J Psychiatry. 2006; 51 Suppl 2:1–92S. [Google Scholar]
- (5).World Health Organization. ICD-10, the ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. Geneva (Switzerland): The Organization; 2010. [Google Scholar]
- (6).Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS–R). JAMA. 2003; 289 (23): 3095–105. [DOI] [PubMed] [Google Scholar]
- (7).Churchill R, Moore HMT, Furukawa TA, Caldwell DM, Davies P, Jones H, et al. ‘Third wave’ cognitive and behavioural therapies versus treatment as usual for depression. Cochrane Database of Systematic Reviews. 2013(10). [DOI] [PubMed]
- (8).Kennedy SH, Lam RW, Parikh SV, Patten SB, Ravindran AV. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. Introduction. J Affect Disord. 2009; 117 Suppl 1:S1–2. [DOI] [PubMed] [Google Scholar]
- (9).Lam RW, Kennedy SH, Grigoriadis S, McIntyre RS, Milev R, Ramasubbu R, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. III. Pharmacotherapy. J Affect Disord. 2009; 117 Suppl 1:S26–43. [DOI] [PubMed] [Google Scholar]
- (10).Parikh SV, Segal ZV, Grigoriadis S, Ravindran AV, Kennedy SH, Lam RW, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. II. Psychotherapy alone or in combination with antidepressant medication. J Affect Disord. 2009; 117 Suppl 1:S15–25. [DOI] [PubMed] [Google Scholar]
- (11).Hunot V, Churchill R, Silva de Lima M, Teixeira V. Psychological therapies for generalised anxiety disorder. Cochrane Database Syst Rev. 2007(1): Cd001848. [DOI] [PMC free article] [PubMed]
- (12).Centre for Addiction and Mental Health. About therapy. Challenges and choices: finding mental health services in Ontario [Internet]. Toronto (ON);: The Centre; 2012 [cited 2017 Feb]. Available from: http://www.camh.ca/en/hospital/visiting_camh/rights_and_policies/Pages/challenges_choices_abouttherapy.aspx [Google Scholar]
- (13).Royal Australian and New Zealand College of Psychiatrists. Structured psychotherapy requirements [Internet]. Melbourne (Australia): The College; 2017. [cited 2017 Feb]. Available from: https://www.ranzcp.org/Files/PreFellowship/2012-Fellowship-Program/Adult-Certificate/Structured-psychotherapy-requirements.aspx [Google Scholar]
- (14).Cuijpers P, Driessen E, Hollon SD, van Oppen P, Barth J, Andersson G. The efficacy of non-directive supportive therapy for adult depression: a meta-analysis. Clin Psychol Rev. 2012; 32 (4): 280–91. [DOI] [PubMed] [Google Scholar]
- (15).U.S. Centers for Medicare and Medicaid Services. Your Medicare coverage: is my test, item or service covered? Mental health care (outpatient) [Internet]. Baltimore (MD): The Centers; 2017. [cited 2017 Feb]. Available from: https://www.medicare.gov/coverage/outpatient-mental-health-care.html [Google Scholar]
- (16).Health Quality Ontario. Health technology assessments: methods and process guide [Internet]. Toronto (ON): Queen's Printer for Ontario; 2017. Mar [cited 2017 May 7]. Available from: http://www.hqontario.ca/Portals/0/documents/evidence/reports/hta-methods-and-process-guide-en.pdf [Google Scholar]
- (17).McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016; 75: 40–6. [DOI] [PubMed] [Google Scholar]
- (18).Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007; 7: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (19).Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6 (7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).Cuijpers P, Cristea IA, Karyotaki E, Reijnders M, Huibers MJH. How effective are cognitive behavior therapies for major depression and anxiety disorders? A meta-analytic update of the evidence. World Psychiatry. 2016; 15 (3): 245–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (21).Linde K, Sigterman K, Kriston L, Rucker G, Jamil S, Meissner K, et al. Effectiveness of psychological treatments for depressive disorders in primary care: systematic review and meta-analysis. Ann Fam Med. 2015; 13 (1): 56–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al. A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression. Health Technol Assess. 2001; 5 (35): 1–173. [DOI] [PubMed] [Google Scholar]
- (23).Laidlaw K, Davidson K, Toner H, Jackson G, Clark S, Law J, et al. A randomised controlled trial of cognitive behaviour therapy vs treatment as usual in the treatment of mild to moderate late life depression. Int J Geriatr Psychiatry. 2008; 23 (8): 843–50. [DOI] [PubMed] [Google Scholar]
- (24).Scott AI, Freeman CP. Edinburgh primary care depression study: treatment outcome, patient satisfaction, and cost after 16 weeks. BMJ. 1992; 304 (6831): 883–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (25).Scott C, Tacchi MJ, Jones R, Scott J. Acute and one-year outcome of a randomised controlled trial of brief cognitive therapy for major depressive disorder in primary care. Br J Psychiatry. 1997; 171: 131–4. [DOI] [PubMed] [Google Scholar]
- (26).Smit A, Kluiter H, Conradi HJ, van der Meer K, Tiemens BG, Jenner JA, et al. Short-term effects of enhanced treatment for depression in primary care: results from a randomized controlled trial. Psychol Med. 2006; 36 (1): 15–26. [DOI] [PubMed] [Google Scholar]
- (27).Teasdale JD, Fennell MJ, Hibbert GA, Amies PL. Cognitive therapy for major depressive disorder in primary care. Br J Psychiatry. 1984; 144: 400–6. [DOI] [PubMed] [Google Scholar]
- (28).Ross M, Scott M. An evaluation of the effectiveness of individual and group cognitive therapy in the treatment of depressed patients in an inner city health centre. J R Coll Gen Pract. 1985; 35 (274): 239–42. [PMC free article] [PubMed] [Google Scholar]
- (29).Biesheuvel-Leliefeld KE, Kok GD, Bockting CL, Cuijpers P, Hollon SD, van Marwijk HW, et al. Effectiveness of psychological interventions in preventing recurrence of depressive disorder: meta-analysis and meta-regression. J Affect Disord. 2015; 174: 400–10. [DOI] [PubMed] [Google Scholar]
- (30).Clarke K, Mayo-Wilson E, Kenny J, Pilling S. Can non-pharmacological interventions prevent relapse in adults who have recovered from depression? A systematic review and meta-analysis of randomised controlled trials. Clin Psychol Rev. 2015; 39: 58–70. [DOI] [PubMed] [Google Scholar]
- (31).Guidi J, Tomba E, Fava GA. The sequential integration of pharmacotherapy and psychotherapy in the treatment of major depressive disorder: a meta-analysis of the sequential model and a critical review of the literature. Am J Psychiatry. 2016; 173 (2): 128–37. [DOI] [PubMed] [Google Scholar]
- (32).Jarrett RB, Kraft D, Doyle J, Foster BM, Eaves GG, Silver PC. Preventing recurrent depression using cognitive therapy with and without a continuation phase: a randomized clinical trial. Arch Gen Psychiatry. 2001; 58 (4): 381–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (33).Jarrett RB, Kraft D, Schaffer M, Witt-Browder A, Risser R, Atkins DH, et al. Reducing relapse in depressed outpatients with atypical features: a pilot study. Psychother Psychosom. 2000; 69 (5): 232–9. [DOI] [PubMed] [Google Scholar]
- (34).Jarrett RB, Minhajuddin A, Gershenfeld H, Friedman ES, Thase ME. Preventing depressive relapse and recurrence in higher-risk cognitive therapy responders: a randomized trial of continuation phase cognitive therapy, fluoxetine, or matched pill placebo. JAMA Psychiatry. 2013; 70 (11): 1152–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (35).Karyotaki E, Smit Y, Holdt Henningsen K, Huibers MJ, Robays J, de Beurs D, et al. Combining pharmacotherapy and psychotherapy or monotherapy for major depression? A meta-analysis on the long-term effects. J Affect Disord. 2016; 194: 144–52. [DOI] [PubMed] [Google Scholar]
- (36).Amick HR, Gartlehner G, Gaynes BN, Forneris C, Asher G, Morgan LC, et al. Comparative benefits and harms of second generation antidepressants and cognitive behavioral therapies in initial treatment of major depressive disorder: systematic review and meta-analysis. BMJ. 2015; 351: h6019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (37).Cuijpers P, Hollon SD, Van Straten A, Bockting C, Berking M, Andersson G. Does cognitive behaviour therapy have an enduring effect that is superior to keeping patients on continuation pharmacotherapy? A meta-analysis. BMJ Open [Internet]. 2013. [cited 2017 Jul 7]; 3 (4): e002542 Available from: http://bmjopen.bmj.com/content/3/4/e002542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (38).Cuijpers P, Sijbrandij M, Koole S, Huibers M, Berking M, Andersson G. Psychological treatment of generalized anxiety disorder: a meta-analysis. Clin Psychol Rev. 2014; 34 (2): 130–40. [DOI] [PubMed] [Google Scholar]
- (39).Barlow D, Rapee R, Brown T. Behavioral treatment of generalized anxiety disorder. Behav Ther. 1992; 23 (4): 551–70. [Google Scholar]
- (40).Butler G, Fennell M, Robson P, Gelder M. Comparison of behavior therapy and cognitive behavior therapy in the treatment of generalized anxiety disorder. J Consult Clin Psychol. 1991; 59 (1): 167–75. [DOI] [PubMed] [Google Scholar]
- (41).Dugas MJ, Ladouceur R, Leger E, Freeston MH, Langlois F, Provencher MD, et al. Group cognitive-behavioral therapy for generalized anxiety disorder: treatment outcome and long-term follow-up. J Consult Clin Psychol. 2003; 71 (4): 821–5. [DOI] [PubMed] [Google Scholar]
- (42).Ladouceur R, Dugas MJ, Freeston MH, Leger E, Gagnon F, Thibodeau N. Efficacy of a cognitive-behavioral treatment for generalized anxiety disorder: evaluation in a controlled clinical trial. J Consult Clin Psychol. 2000; 68 (6): 957–64. [PubMed] [Google Scholar]
- (43).Mohlman J, Gorenstein EE, Kleber M, de Jesus M, Gorman JM, Papp LA. Standard and enhanced cognitive-behavior therapy for late-life generalized anxiety disorder: two pilot investigations. Am J Geriatr Psychiatry. 2003; 11 (1): 24–32. [PubMed] [Google Scholar]
- (44).Stanley MA, Hopko DR, Diefenbach GJ, Bourland SL, Rodriguez H, Wagener P. Cognitive-behavior therapy for late-life generalized anxiety disorder in primary care: preliminary findings. Am J Geriatr Psychiatry. 2003; 11 (1): 92–6. [PubMed] [Google Scholar]
- (45).Wetherell JL, Gatz M, Craske MG. Treatment of generalized anxiety disorder in older adults. J Consult Clin Psychol. 2003; 71 (1): 31–40. [DOI] [PubMed] [Google Scholar]
- (46).Jakobsen JC, Hansen JL, Simonsen E, Gluud C. The effect of interpersonal psychotherapy and other psychodynamic therapies versus ‘treatment as usual’ in patients with major depressive disorder. PLoS One. 2011; 6 (4): e19044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (47).Schulberg HC, Block MR, Madonia MJ, Scott CP, Rodriguez E, Imber SD, et al. Treating major depression in primary care practice: eight-month clinical outcomes. Arch Gen Psychiatry. 1996; 53 (10): 913–9. [DOI] [PubMed] [Google Scholar]
- (48).Frank E, Prien RF, Jarrett RB, Keller MB, Kupfer DJ, Lavori PW, et al. Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Remission, recovery, relapse, and recurrence. Arch Gen Psychiatry. 1991; 48 (9): 851–5. [DOI] [PubMed] [Google Scholar]
- (49).Schramm E, van Calker D, Dykierek P, Lieb K, Kech S, Zobel I, et al. An intensive treatment program of interpersonal psychotherapy plus pharmacotherapy for depressed inpatients: acute and long-term results. Am J Psychiatry. 2007; 164 (5): 768–77. [DOI] [PubMed] [Google Scholar]
- (50).Fuchs CZ, Rehm LP. A self-control behavior therapy program for depression. J Consult Clin Psychol. 1977; 45 (2): 206–15. [DOI] [PubMed] [Google Scholar]
- (51).Shaw BF. Comparison of cognitive therapy and behavior therapy in the treatment of depression. J Consult Clin Psychol. 1977; 45 (4): 543–51. [DOI] [PubMed] [Google Scholar]
- (52).Nezu AM. Efficacy of a social problem-solving therapy approach for unipolar depression. J Consult Clin Psychol. 1986; 54 (2): 196–202. [DOI] [PubMed] [Google Scholar]
- (53).Cuijpers P, Koole SL, van Dijke A, Roca M, Li J, Reynolds CF., 3rd Psychotherapy for subclinical depression: meta-analysis. Br J Psychiatry. 2014; 205 (4): 268–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (54).Driessen E, Hollon SD, Bockting CL, Cuijpers P, Turner EH. Does publication bias inflate the apparent efficacy of psychological treatment for major depressive disorder? A systematic review and meta-analysis of US National Institutes of Health-funded trials. PLoS One. 2015; 10 (9): e0137864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (55).Heuzenroeder L, Donnelly M, Haby MM, Mihalopoulos C, Rossell R, Carter R, et al. Cost-effectiveness of psychological and pharmacological interventions for generalized anxiety disorder and panic disorder. Aust N Z J Psychiatry. 2004; 38 (8): 602–12. [DOI] [PubMed] [Google Scholar]
- (56).Vos T, Corry J, Haby MM, Carter R, Andrews G. Cost-effectiveness of cognitive-behavioural therapy and drug interventions for major depression. Aust N Z J Psychiatry. 2005; 39 (8): 683–92. [DOI] [PubMed] [Google Scholar]
- (57).Brown JS, Sellwood K, Beecham JK, Slade M, Andiappan M, Landau S, et al. Outcome, costs and patient engagement for group and individual CBT for depression: a naturalistic clinical study. Behav Cogn Psychother. 2011; 39 (3): 355–8. [DOI] [PubMed] [Google Scholar]
- (58).Bosmans JE, van Schaik DJ, Heymans MW, van Marwijk HW, van Hout HP, de Bruijne MC. Cost-effectiveness of interpersonal psychotherapy for elderly primary care patients with major depression. Int J Technol Assess Health Care. 2007; 23 (4): 480–7. [DOI] [PubMed] [Google Scholar]
- (59).Scott J, Palmer S, Paykel E, Teasdale J, Hayhurst H. Use of cognitive therapy for relapse prevention in chronic depression. Cost-effectiveness study. Br J Psychiatry. 2003; 182: 221–7. [DOI] [PubMed] [Google Scholar]
- (60).Revicki DA, Siddique J, Frank L, Chung JY, Green BL, Krupnick J, et al. Cost-effectiveness of evidence-based pharmacotherapy or cognitive behavior therapy compared with community referral for major depression in predominantly low-income minority women. Arch Gen Psychiatry. 2005; 62 (8): 868–75. [DOI] [PubMed] [Google Scholar]
- (61).Simon J, Pilling S, Burbeck R, Goldberg D. Treatment options in moderate and severe depression: decision analysis supporting a clinical guideline. Br J Psychiatry. 2006; 189: 494–501. [DOI] [PubMed] [Google Scholar]
- (62).Sava FA, Yates BT, Lupu V, Szentagotai A, David D. Cost-effectiveness and cost-utility of cognitive therapy, rational emotive behavioral therapy, and fluoxetine (Prozac) in treating depression: a randomized clinical trial. J Clin Psychol. 2009; 65 (1): 36–52. [DOI] [PubMed] [Google Scholar]
- (63).Sado M, Knapp M, Yamauchi K, Fujisawa D, So M, Nakagawa A, et al. Cost-effectiveness of combination therapy versus antidepressant therapy for management of depression in Japan. Aust N Z J Psychiatry. 2009; 43 (6): 539–47. [DOI] [PubMed] [Google Scholar]
- (64).Holman AJ, Serfaty MA, Leurent BE, King MB. Cost-effectiveness of cognitive behaviour therapy versus talking and usual care for depressed older people in primary care. BMC Health Serv Res. 2011; 11: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (65).Prukkanone B, Vos T, Bertram M, Lim S. Cost-effectiveness analysis for antidepressants and cognitive behavioral therapy for major depression in Thailand. Value Health. 2012; 15 (1 Suppl): S3–8. [DOI] [PubMed] [Google Scholar]
- (66).Kafali N, Cook B, Canino G, Alegria M. Cost-effectiveness of a randomized trial to treat depression among Latinos. J Ment Health Policy Econ. 2014; 17 (2): 41–50. [PMC free article] [PubMed] [Google Scholar]
- (67).Hollinghurst S, Carroll FE, Abel A, Campbell J, Garland A, Jerrom B, et al. Cost-effectiveness of cognitive-behavioural therapy as an adjunct to pharmacotherapy for treatment-resistant depression in primary care: economic evaluation of the CoBalT Trial. Br J Psychiatry. 2014; 204 (1): 69–76. [DOI] [PubMed] [Google Scholar]
- (68).Wiles NJ, Thomas L, Turner N, Garfield K, Kounali D, Campbell J, et al. Long-term effectiveness and cost-effectiveness of cognitive behavioural therapy as an adjunct to pharmacotherapy for treatment-resistant depression in primary care: follow-up of the CoBalT randomised controlled trial. Lancet Psychiatry. 2016; 3 (2): 137–44. [DOI] [PubMed] [Google Scholar]
- (69).Koeser L, Donisi V, Goldberg DP, McCrone P. Modelling the cost-effectiveness of pharmacotherapy compared with cognitive-behavioural therapy and combination therapy for the treatment of moderate to severe depression in the UK. Psychol Med. 2015; 45 (14): 3019–31. [DOI] [PubMed] [Google Scholar]
- (70).Wiles N, Thomas L, Abel A, Barnes M, Carroll F, Ridgway N, et al. Clinical effectiveness and cost-effectiveness of cognitive behavioural therapy as an adjunct to pharmacotherapy for treatment-resistant depression in primary care: the CoBalT randomised controlled trial. Health Technol Assess. 2014; 18 (31): 1–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (71).Lam RW, Kennedy SH, Parikh SV, MacQueen GM, Milev RV, Ravindran A, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: introduction and methods. Can J Psychiatry. 2016; 61 (9): 506–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (72).Brien S, Grenier L, Kapral ME, Kurdyak P, Vigod S, for Health Quality Ontario and Institute for Clinical Evaluative Sciences. Taking stock: a report on the quality of mental health and addictions services in Ontario. An HQO/ICES report. Toronto (ON): Queen's Printer for Ontario; 2015. [Google Scholar]
- (73).Jacobs P, Dewa C, Lesage A, Vasiliadis H-M, Escober C, Mulvale G, et al. The cost of mental health and substance abuse services in Canada. Edmonton (AB): Institute of Health Economics; 2010. [Google Scholar]
- (74).Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013; 10 (11): e1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (75).Patten SB, Williams JV, Lavorato DH, Wang JL, McDonald K, Bulloch AG. Descriptive epidemiology of major depressive disorder in Canada in 2012. Can J Psychiatry. 2015; 60 (1): 23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (76).Kurdyak P, Stukel TA, Goldbloom D, Kopp A, Zagorski BM, Mulsant BH. Universal coverage without universal access: a study of psychiatrist supply and practice patterns in Ontario. Open Med. 2014; 8 (3): e87–99. [PMC free article] [PubMed] [Google Scholar]
- (77).Goldner EM, Jones W, Fang ML. Access to and waiting time for psychiatrist services in a Canadian urban area: a study in real time. Can J Psychiatry. 2011; 56 (8): 474–80. [DOI] [PubMed] [Google Scholar]
- (78).Payne KA, Myhr G. Increasing access to cognitive-behavioural therapy (CBT) for the treatment of mental illness in Canada: a research framework and call for action. Healthc Policy. 2010; 5 (3): e173–85. [PMC free article] [PubMed] [Google Scholar]
- (79).Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS)–explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health. 2013; 16 (2): 231–50. [DOI] [PubMed] [Google Scholar]
- (80).Canadian Agency for Drugs and Technologies in Health. Guidelines for the economic evaluation of health technologies: Canada. 4th ed [Internet]. Ottawa (ON): The Agency; 2017. [cited 2017 Apr 4]. Available from: https://www.cadth.ca/guidelines-economic-evaluation-health-technologies-canada-4th-edition [Google Scholar]
- (81).Patten SC. The duration of major depressive episodes in the Canadian general population. Chronic Dis Can. 2001; 22 (1): 6–11. [PubMed] [Google Scholar]
- (82).Patten SB. Recurrence risk in major depression. Depress Anxiety. 2013; 30 (1): 1–4. [DOI] [PubMed] [Google Scholar]
- (83).Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999; 282 (18): 1737–44. [DOI] [PubMed] [Google Scholar]
- (84).Kennedy SH, Lam RW, McIntyre RS, Tourjman SV, Bhat V, Blier P, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 3. Pharmacological treatments. Can J Psychiatry. 2016; 61 (9): 540–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (85).Lam RW, McIntosh D, Wang J, Enns MW, Kolivakis T, Michalak EE, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 1. Disease burden and principles of care. Can J Psychiatry. 2016; 61 (9): 510–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (86).Parikh SV, Quilty LC, Ravitz P, Rosenbluth M, Pavlova B, Grigoriadis S, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 2. Psychological treatments. Can J Psychiatry. 2016; 61 (9): 524–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (87).Patten SB. Updated CANMAT guidelines for treatment of major depressive disorder. Can J Psychiatry. 2016; 61 (9): 504–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (88).Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006; 166 (10): 1092–7. [DOI] [PubMed] [Google Scholar]
- (89).National Institute for Health and Clinical Excellence. Generalised anxiety disorder and panic disorder in adults: management. London (UK): The Institute; 2011. [PubMed] [Google Scholar]
- (90).National Institute for Health and Clinical Excellence. Depression in adults: recognition and management. London (UK): The Institute; 2009. [PubMed] [Google Scholar]
- (91).Canadian Psychiatric Association. Clinical practice guidelines. Management of anxiety disorders. Can J Psychiatry. 2006; 51 (8 Suppl 2): 9–91s. [PubMed] [Google Scholar]
- (92).MacQueen GM, Frey BN, Ismail Z, Jaworska N, Steiner M, Lieshout RJ, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 6. Special populations: youth, women, and the elderly. Can J Psychiatry. 2016; 61 (9): 588–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (93).Milev RV, Giacobbe P, Kennedy SH, Blumberger DM, Daskalakis ZJ, Downar J, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 4. Neurostimulation treatments. Can J Psychiatry. 2016; 61 (9): 561–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (94).Pare M, Gilbert B. Psychological therapy and counseling. Toronto (ON): Ontario Guidelines Advisory Committee; 2002. [Google Scholar]
- (95).Health Quality Ontario. Major depression: care for adults and adolescents [Internet]. Toronto (ON): Queen's Printer for Ontario; 2016. [cited 2017 Apr 18]. Available from: http://www.hqontario.ca/portals/0/documents/evidence/quality-standards/qs-depression-clinical-guide-1609-en.pdf [Google Scholar]
- (96).Interpersonal Psychotherapy Institute. About IPT [Internet]. Coralville (IA): The Institute; 2017. [cited 2017 Jan 18]. Available from: https://iptinstitute.com/about-ipt/ [Google Scholar]
- (97).Statistics Canada. Consumer price index, health and personal care, by province (Canada) [Internet]. Ottawa (ON): Statistics Canada; 2016. [cited 2017 Jan 18]. Available from: http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/econ161a-eng.htm [Google Scholar]
- (98).Nierenberg AA, DeCecco LM. Definitions of antidepressant treatment response, remission, nonresponse, partial response, and other relevant outcomes: a focus on treatment-resistant depression. J Clin Psychiatry. 2001; 62 Suppl 16:5–9. [PubMed] [Google Scholar]
- (99).Hardeveld F, Spijker J, De Graaf R, Nolen WA, Beekman AT. Recurrence of major depressive disorder and its predictors in the general population: results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Psychol Med. 2013; 43 (1): 39–48. [DOI] [PubMed] [Google Scholar]
- (100).Eaton WW, Shao H, Nestadt G, Lee HB, Bienvenu OJ, Zandi P. Population-based study of first onset and chronicity in major depressive disorder. Arch Gen Psychiatry. 2008; 65 (5): 513–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (101).Mueller TI, Leon AC, Keller MB, Solomon DA, Endicott J, Coryell W, et al. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. Am J Psychiatry. 1999; 156 (7): 1000–6. [DOI] [PubMed] [Google Scholar]
- (102).Khan A, Schwartz K. Suicide risk and symptom reduction in patients assigned to placebo in duloxetine and escitalopram clinical trials: analysis of the FDA summary basis of approval reports. Ann Clin Psychiatry. 2007; 19 (1): 31–6. [DOI] [PubMed] [Google Scholar]
- (103).Khan A, Khan S, Kolts R, Brown WA. Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: analysis of FDA reports. Am J Psychiatry. 2003; 160 (4): 790–2. [DOI] [PubMed] [Google Scholar]
- (104).Statistics Canada. Life tables, Canada, provinces and territories (2009 to 2011, no. 5) [Internet]. Ottawa (ON): Statistics Canada; 2011. [cited 2017 Aug 3]. Available from: http://www.statcan.gc.ca/access_acces/alternative_alternatif.action?loc=http://www.statcan.gc.ca/pub/84-537-x/2013005/tbl_2009_2011-eng.xlsx [Google Scholar]
- (105).Gartlehner G, Gaynes BN, Amick HR, Asher GN, Morgan LC, Coker-Schwimmer E, et al. Comparative benefits and harms of antidepressant, psychological, complementary, and exercise treatments for major depression: an evidence report for a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016; 164 (5): 331–41. [DOI] [PubMed] [Google Scholar]
- (106).Cipriani A, Furukawa TA, Salanti G, Geddes JR, Higgins JP, Churchill R, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009; 373 (9665): 746–58. [DOI] [PubMed] [Google Scholar]
- (107).Williams N, Simpson AN, Simpson K, Nahas Z. Relapse rates with long-term antidepressant drug therapy: a meta-analysis. Hum Psychopharmacol. 2009; 24 (5): 401–8. [DOI] [PubMed] [Google Scholar]
- (108).Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Chichester (UK): John Wiley & Sons Ltd.; 2009. [Google Scholar]
- (109).Drummond MF, Sculpher MJ, Torrance GW, O'Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. 3rd ed. New York: Oxford University Press; 2005. [Google Scholar]
- (110).Mohiuddin S, Payne K. Utility values for adults with unipolar depression: systematic review and meta-analysis. Med Decis Making. 2014; 34 (5): 666–85. [DOI] [PubMed] [Google Scholar]
- (111).Revicki DA, Wood M. Patient-assigned health state utilities for depression-related outcomes: differences by depression severity and antidepressant medications. J Affect Disord. 1998; 48 (1): 25–36. [DOI] [PubMed] [Google Scholar]
- (112).Schaffer A, Levitt AJ, Hershkop SK, Oh P, MacDonald C, Lanctot K. Utility scores of symptom profiles in major depression. Psychiatry Res. 2002; 110 (2): 189–97. [DOI] [PubMed] [Google Scholar]
- (113).Lenert LA, Sherbourne CD, Sugar C, Wells KB. Estimation of utilities for the effects of depression from the SF-12. Med Care. 2000; 38 (7): 763–70. [DOI] [PubMed] [Google Scholar]
- (114).King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al. Randomised controlled trial of non-directive counselling, cognitive-behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care. Health Technol Assess. 2000; 4 (19): 1–83. [PubMed] [Google Scholar]
- (115).Mann R, Gilbody S, Richards D. Putting the ‘Q’ in depression QALYs: a comparison of utility measurement using EQ-5D and SF-6D health related quality of life measures. Soc Psychiatry Psychiatr Epidemiol. 2009; 44 (7): 569–78. [DOI] [PubMed] [Google Scholar]
- (116).Vallejo-Torres L, Castilla I, Gonzalez N, Hunter R, Serrano-Perez P, Perestelo-Perez L. Cost-effectiveness of electroconvulsive therapy compared to repetitive transcranial magnetic stimulation for treatment-resistant severe depression: a decision model. Psychol Med. 2015; 45 (7): 1459–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (117).Ministry of Health and Long-Term Care. Schedule of benefits: physician services under the Health Insurance Act [Internet]. Toronto (ON): The Ministry; 2015. [cited 2017 Aug 1]. Available from: http://www.health.gov.on.ca/en/pro/programs/ohip/sob/physserv/sob_master20160401.pdf [Google Scholar]
- (118).Kates N, McPherson-Doe C, George L. Integrating mental health services within primary care settings: the Hamilton Family Health Team. J Ambul Care Manage. 2011; 34 (2): 174–82. [DOI] [PubMed] [Google Scholar]
- (119).Rosser WW, Colwill JM, Kasperski J, Wilson L. Patient-centered medical homes in Ontario. N Engl J Med. 2010; 362 (3): e7. [DOI] [PubMed] [Google Scholar]
- (120).Rosser WW, Colwill JM, Kasperski J, Wilson L. Progress of Ontario's family health team model: a patient-centered medical home. Ann Fam Med. 2011; 9 (2): 165–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (121).Association of Family Health Teams of Ontario. Optimizing value of and access to team-based primary care [Internet]. Toronto (ON): The Association; 2015. Jun 4 [cited 2016 Nov 16]. Available from: http://www.afhto.ca/highlights/evidence/optimizing-value-of-and-access-to-team-based-primary-care/ [Google Scholar]
- (122).Canadian Agency for Drugs and Technologies in Health. Guidance document for the costing of health care resources in the Canadian setting. 2nd ed [Internet]. Ottawa (ON): The Agency; 2016. Jun [cited 2017 Apr 4]. Available from: https://www.cadth.ca/guidance-document-costing-health-care-resources-canadian-setting [Google Scholar]
- (123).Association of Family Health Teams of Ontario. Toward a primary care recruitment and retention strategy for Ontario. Toronto (ON): The Association; 2014. [Google Scholar]
- (124).Gidwani RA. A budget impact analysis of chronic disease screening: the business care of rapid HIV testing in VA emergency departments. Ann Arbor (MI): UMI Dissertation Publishing; 2009. [Google Scholar]
- (125).Ontario Ministry of Health and Long-Term Care. Ontario drug benefit formulary/comparative drug index [Internet]. Toronto (ON): The Ministry; 2015. [cited 2017 Aug 3]. Available from: https://www.formulary.health.gov.on.ca/formulary/ [Google Scholar]
- (126).Alberta College of Family Physicians. Price comparison of commonly prescribed pharmaceuticals in Alberta 2014 [Internet]. Edmonton (AB): The College; 2014. [cited 2017 Apr 4]. Available from: https://www.acfp.ca/wp-content/uploads/2014/06/ACFPPricingDoc2014.pdf [Google Scholar]
- (127).Health Quality Ontario. Repetitive transcranial magnetic stimulation for treatment-resistant depression: an economic analysis. Ont Health Technol Assess Ser. 2016; 16 (6): 1–51. [PMC free article] [PubMed] [Google Scholar]
- (128).de Oliveira C, Cheng J, Vigod S, Rehm J, Kurdyak P. Patients with high mental health costs incur over 30 percent more costs than other high-cost patients. Health Aff (Millwood). 2016; 35 (1): 36–43. [DOI] [PubMed] [Google Scholar]
- (129).Bereza BG, Machado M, Papadimitropoulos M, Sproule B, Ravindran AV, Einarson TR. A Markov model approach assessing the cost of illness of generalized anxiety disorder in Canada. Neurol Ther. 2012; 1 (1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (130).Kolber MC, Lee J, Nickonchuk T. Price comparison of commonly prescribed pharmaceuticals in Alberta 2014 [Internet]. Edmonton (AB): Alberta College of Family Physicians; 2014. [cited 2017 Aug 3]. Available from: https://www.acfp.ca/wp-content/uploads/2014/06/ACFPPricingDoc2014.pdf [Google Scholar]
- (131).O'Brien BJ, Briggs AH. Analysis of uncertainty in health care cost-effectiveness studies: an introduction to statistical issues and methods. Stat Methods Med Res. 2002; 11 (6): 455–68. [DOI] [PubMed] [Google Scholar]
- (132).Caro JJ, Briggs AH, Siebert U, Kuntz KM. Modeling good research practices–overview: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force-1. Med Decis Making. 2012; 32 (5): 667–77. [DOI] [PubMed] [Google Scholar]
- (133).Siebert U, Alagoz O, Bayoumi AM, Jahn B, Owens DK, Cohen DJ, et al. State-transition modeling: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force-3. Med Decis Making. 2012; 32 (5): 690–700. [DOI] [PubMed] [Google Scholar]
- (134).Briggs AH. Handling uncertainty in cost-effectiveness models. Pharmacoeconomics. 2000; 17 (5): 479–500. [DOI] [PubMed] [Google Scholar]
- (135).Stinnett AA, Mullahy J. The negative side of cost-effectiveness analysis. JAMA. 1997; 277 (24): 1931–2; author reply 2–3. [PubMed] [Google Scholar]
- (136).Cantor SB. Cost-effectiveness analysis, extended dominance, and ethics: a quantitative assessment. Med Decis Making. 1994; 14 (3): 259–65. [DOI] [PubMed] [Google Scholar]
- (137).Gafni A, Birch S. Incremental cost-effectiveness ratios (ICERs): the silence of the lambda. Soc Sci Med. 2006; 62 (9): 2091–100. [DOI] [PubMed] [Google Scholar]
- (138).Detsky AS, Laupacis A. Relevance of cost-effectiveness analysis to clinicians and policy makers. JAMA. 2007; 298 (2): 221–4. [DOI] [PubMed] [Google Scholar]
- (139).Winkelmayer WC, Weinstein MC, Mittleman MA, Glynn RJ, Pliskin JS. Health economic evaluations: the special case of end-stage renal disease treatment. Med Decis Making. 2002; 22 (5): 417–30. [DOI] [PubMed] [Google Scholar]
- (140).Fenwick E, O'Brien BJ, Briggs A. Cost-effectiveness acceptability curves–facts, fallacies and frequently asked questions. Health Econ. 2004; 13 (5): 405–15. [DOI] [PubMed] [Google Scholar]
- (141).Sullivan SD, Mauskopf JA, Augustovski F, Jaime Caro J, Lee KM, Minchin M, et al. Budget impact analysis-principles of good practice: report of the ISPOR 2012 Budget Impact Analysis Good Practice II Task Force. Value Health. 2014; 17 (1): 5–14. [DOI] [PubMed] [Google Scholar]
- (142).Patten SB, Williams JV, Lavorato DH, Wang JL, McDonald K, Bulloch AG. Major depression in Canada: what has changed over the past 10 years? Can J Psychiatry. 2016;61 (2): 80–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (143).Wang J, Williams J, Lavorato D, Schmitz N, Dewa C, Patten SB. The incidence of major depression in Canada: the National Population Health Survey. J Affect Disord. 2010; 123 (1–3): 158–63. [DOI] [PubMed] [Google Scholar]
- (144).Patten SB, Lee RC. Refining estimates of major depression incidence and episode duration in Canada using a Monte Carlo Markov model. Med Decis Making. 2004; 24 (4): 351–8. [DOI] [PubMed] [Google Scholar]
- (145).Patten SB, Lee RC. Describing the longitudinal course of major depression using Markov models: data integration across three national surveys. Population health metrics. 2005; 3: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (146).Statistics Canada. Table 051-0001 – Estimates of population, by age group and sex for July 1, Canada, provinces and territories, annual (persons unless otherwise noted), CANSIM (database) [Internet]. Ottawa (ON): Statistics Canada; 2016. [cited 2017 Aug 3]. Available from: http://www5.statcan.gc.ca/cansim/a26?lang=eng&retrLang=eng&id=0510001&&pattern=&stByVal=1&p1=1&p2=37&tabMode=dataTable&csid [Google Scholar]
- (147).Farrar S, Kates N, Crustolo AM, Nikolaou L. Integrated model for mental health care. Are health care providers satisfied with it? Can Fam Physician. 2001;47: 2483–8. [PMC free article] [PubMed] [Google Scholar]
- (148).Somers JM, Goldner EM, Waraich P, Hsu L. Prevalence and incidence studies of anxiety disorders: a systematic review of the literature. Can J Psychiatry. 2006; 51 (2): 100–13. [DOI] [PubMed] [Google Scholar]
- (149).Watterson RA, Williams JV, Lavorato DH, Patten SB. Descriptive epidemiology of generalized anxiety disorder in Canada. Can J Psychiatry. 2016 Jul 10; 62 (1): 24–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (150).Barham L. Public and patient involvement at the UK National Institute for Health and Clinical Excellence. Patient. 2011; 4 (1): 1–10. [DOI] [PubMed] [Google Scholar]
- (151).Messina J, Grainger DL. A pilot study to identify areas for further improvements in patient and public involvement in health technology assessments for medicines. Patient. 2012; 5 (3): 199–211. [DOI] [PubMed] [Google Scholar]
- (152).Ontario Patient Engagement Subcommittee. Public engagement for health technology assessment at Health Quality Ontario—final report from the Ontario Health Technology Advisory Committee Public Engagement Subcommittee. [Internet]. Toronto (ON): Queen's Printer for Ontario; 2015. Apr [cited 2017 Jul 11]. Available from: http://www.hqontario.ca/Portals/0/documents/evidence/special-reports/report-subcommittee-20150407-en.pdf [Google Scholar]
- (153).Tjornhoj-Thomsen T, Hansen HP. Knowledge in health technology assessment: who, what, how? Int J Technol Assess Health Care. 2011;27 (4): 324–9. [DOI] [PubMed] [Google Scholar]
- (154).Rowe G, Frewer LJ. A typology of public engagement mechanisms. Sci Technol Hum Val. 2005; 30 (2): 251–90. [Google Scholar]
- (155).Brundisini F, Giacomini M, DeJean D, Vanstone M, Winsor S, Smith A. Chronic disease patients' experiences with accessing health care in rural and remote areas: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser. 2013; 13 (15): 1–33. [PMC free article] [PubMed] [Google Scholar]
- (156).Kvale S. Interviews: an introduction to qualitative research interviewing. Thousand Oaks (CA): Sage Publications; 1996. [Google Scholar]
- (157).Kuzel AJ. Sampling in qualitative inquiry. In: Miller WL, Crabtree BF, editors. Doing qualitative research. Thousand Oaks (CA): Sage Publications; 1999. p. 33–45. [Google Scholar]
- (158).Morse J. Emerging from the data: cognitive processes of analysis in qualitative research. In: Morse J, editor. Critical issues in qualitative research methods Thousand Oaks (CA): Sage Publications; 1994. p. 23–41. [Google Scholar]
- (159).Patton MQ. Qualitative research and evaluation methods. 3rd ed. Thousand Oaks (CA): Sage Publications; 2002. [Google Scholar]
- (160).Strauss AL, Corbin JM. Basics of qualitative research: techniques and procedures of developing a grounded theory. 2nd ed. Thousand Oaks (CA): Sage Publications; 1998. [Google Scholar]
- (161).Health Technology Assessment International. Introduction to health technology assessment [Internet]. Edmonton (AB): Health Technology Assessment International; 2015. [cited 2017 Feb]. Available from: http://www.htai.org/fileadmin/HTAi_Files/ISG/PatientInvolvement/v2_files/Resource/PCISG-Resource-Intro_to_HTA__KFacey__Jun13.pdf [Google Scholar]
- (162).Strauss AL, Corbin JM. Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol. 1990; 13 (1): 3–21. [Google Scholar]
- (163).Strauss AL, Corbin JM. Grounded theory methodology: an overview. In: Denzin NK, Lincoln YS, editors. Handbook of qualitative research. Thousand Oaks (CA): Sage Publications; 1994. p. 273–85. [Google Scholar]