Abstract
Unilateral oculomotor nerve palsy can result from various neurological disorders. We herein report the case of a 68-year-old man with complete unilateral oculomotor nerve palsy following campylobacter infection. Based on the antecedent infection and the patient's decreased tendon reflexes, incomplete Miller Fisher syndrome (MFS) without ataxia was suspected. His serum tested positive for anti-GQ1b antibodies. He recovered over a period of 87 days without immunotherapy. We conclude that incomplete MFS following campylobacter infection can cause unilateral oculomotor nerve palsy without ataxia. Mild MFS should be considered in patients presenting with unilateral isolated ophthalmoplegia and decreased tendon reflexes.
Keywords: oculomotor nerve, oculomotor nerve palsy, ophthalmoplegia, GQ1b, anti-GQ1b antibody syndrome, campylobacter
Introduction
Miller Fisher syndrome (MFS) is characterized clinically by external ophthalmoplegia, ataxia, and loss of the deep tendon reflexes (DTRs). Laboratory tests reveal the presence of immunoglobulin G (IgG) antibodies to GQ1b gangliosides, which exist in the paranodal regions of the extramedullary portion of human oculomotor, trochlear, and abducens nerves, and muscle spindles (1-3). Anti-GQ1b antibodies are also found in Bickerstaff brainstem encephalitis, and acute ophthalmoplegia without ataxia (AO), which are collectively referred to as “anti-GQ1b antibody syndrome” (3-5). Although AO usually causes bilateral external ophthalmoplegia (3, 6), complete unilateral oculomotor nerve palsy due to anti-GQ1b antibody syndrome is an extremely rare and noteworthy symptom (4, 7). Upper respiratory infection has been identified as a preceding infection (4, 7); however, no cases of complete unilateral oculomotor nerve palsy due to MFS following campylobacter infection have been reported (4, 7). We herein report a case of a mild form of MFS with complete unilateral oculomotor nerve palsy without ataxia following gastroenteritis due to campylobacter infection. The patient tested positive for anti-GQ1b antibodies and recovered without immunotherapy. The patient provided his written informed consent for the publication of this report.
Case Report
A 68-year-old man visited our hospital after having woken with diplopia three days previously. There had been no change in the diplopia over that time. Eight days prior to his visit, he experienced symptoms that were consistent with gastroenteritis (fever, diarrhea, and abdominal pain). His medical history included tongue cancer and cervical cord injury. He had no significant past ocular disease history. His medications included oral mecobalamin.
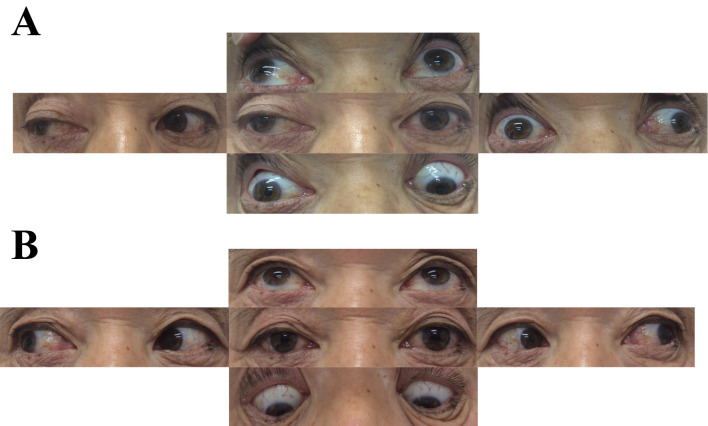
His vital signs were unremarkable. He had no disturbance of consciousness. A neurological examination revealed ptosis on the right side, and exotropia of the right eye (Figure A). The patient's right eye movement showed restricted adduction and vertical gaze, suggesting oculomotor nerve palsy (Figure A). Convergence was impossible. His bilateral pupil sizes were consistent, and his bilateral pupillary light reflex was prompt. He had no other cranial nerve disturbance. The DTRs of his bilateral biceps, triceps, and brachioradial muscles were slightly decreased. His bilateral plantar responses were flexor. His superficial sense, joint position sense, and vibration sense were normal. His tandem stance and gait were also normal. Weakness of the limbs, oropharynx, or face was not observed. Finger-to-nose and heel-to-knee tests showed no dysmetria or decomposition. As he had right oculomotor nerve palsy, and slightly decreased DTRs without ataxia after gastroenteritis, we initially considered his illness to be a mild form of MFS without ataxia, cerebrovascular disease, diabetes mellitus, or myasthenia gravis. Based on the onset of symptoms on waking and the pupil-sparing oculomotor nerve palsy, we considered the possibility of cerebrovascular disease or diabetes mellitus. To exclude these diagnoses, we performed brain magnetic resonance imaging and a blood analysis to determine his blood glucose and hemoglobin A1c levels, but found no abnormalities. No aneurysms were detected by brain magnetic resonance angiography. We then performed other laboratory and electrophysiological studies to differentially diagnose unilateral oculomotor nerve palsy, which was indicated by the antecedent infection and his decreased DTRs. These studies showed that his vitamin B1 and angiotensin-converting enzyme levels, and thyroid function were all normal. The patient was negative for anti-acetylcholine receptor antibodies, myeloperoxidase antineutrophil cytoplasmic antibodies, anti-proteinase 3 antineutrophil cytoplasmic antibodies, and anti-SS-A/Ro and anti-SS-B/La antibodies. A stool culture revealed campylobacter infection. A cerebrospinal fluid analysis revealed no albuminocytologic dissociation (2 cells/μL; total protein of 32 mg/100 mL) and a normal IgG index (0.4). Motor and sensory nerve conduction studies showed no abnormalities. Enzyme-linked immunosorbent assays (ELISAs) showed no IgG or IgM antibodies to the gangliosides GM1, GM2, GM3, GD1a, GD1b, GD3, GT1b, or galactocerebroside, but intense positivity for anti-GQ1b and anti-GT1a antibodies (mean optical density: 0.796 and 0.766, respectively). Based on his clinical presentation, and the results of the neurological examination and laboratory findings, we diagnosed the patient with unilateral oculomotor nerve palsy due to a mild form of MFS without ataxia.
Figure.
The eye movement in the present case. At three days after the onset of symptoms, a neurological examination revealed mild right ptosis and the restriction of adduction and vertical gaze of the right eye, indicating right oculomotor nerve palsy (A). The right oculomotor nerve palsy disappeared on day 87 after the onset of symptoms (B).
We selected conservative treatment because his illness was mild and because a good natural recovery was expected even without immunotherapy (3, 8). On day 33 after the onset of symptoms (during the follow-up period), the DTRs of the upper extremities improved. The patient's right eye movement symptoms began to improve on day 37, and disappeared on day 44; however, slight ptosis persisted. The patient's right oculomotor nerve palsy completely recovered by day 87 (Figure B). It seemed that there was no restriction of left eye movement at the initial assessment. However, based on the findings after the patient's recovery, there might have been limited abduction of the left eye at the time of the initial assessment (Figure B).
Discussion
We presented a case of unilateral oculomotor nerve palsy due to a mild form of MFS without ataxia following campylobacter infection. This case demonstrates three important points: (1) a mild form of MFS without ataxia following campylobacter infection can cause unilateral oculomotor nerve palsy without ataxia; (2) the detection of decreased DTRs is useful for the differential diagnosis of ophthalmoplegia, even if it is unilateral at the onset of symptoms; and (3) unilateral oculomotor nerve palsy due to mild MFS without ataxia may have a good prognosis even without immunotherapy.
Previous reports have described that anti-GQ1b antibodies cause unilateral external ophthalmoplegia (Table) (4, 6, 7, 9-12). Complete isolated oculomotor nerve palsy can develop after an upper respiratory infection (Table) (4, 7). In our case, unilateral isolated oculomotor nerve palsy associated with anti-GQ1b antibodies developed after gastroenteritis, which had been caused by campylobacter infection. Campylobacter jejuni is the most important predisposing factor (13). Strains of C. jejuni produce GD1c- or GT1a-like lipo-oligosaccharides. Campylobacter infection generates IgG anti-GQ1b antibodies in patients with certain immunogenetic backgrounds (3). Anti-GQ1b antibodies bind the paranodal regions of the extramedullary portion of the human oculomotor, trochlear, and abducens nerves, and muscle spindles (1-3). As a result, anti-GQ1b antibodies cause external ophthalmoplegia and hyporeflexia/areflexia (1, 3, 5). However, the reason for unilateral oculomotor nerve involvement is unknown (4, 7). In the present case, the patient might have had a mild form of MFS without ataxia, as his symptoms improved without immunotherapy.
Table.
Clinical Features of Patients with Unilateral External Ophthalmoplegia Due to Anti-GQ1b Antibody Syndrome.
| Reference | Age | Sex | Affected eye side | Ptosis | Gage limitation | Isolated oculomotor nerve involvement | Deep tendon reflex | Antecedent infection | Treatment | Recovery period |
|---|---|---|---|---|---|---|---|---|---|---|
| (4) | 27 | F | Right | No | Vertical | Partial | Normal | Diarrhea | IVIg or Steroid | Follow up loss |
| 30 | M | Right | Right | Adduction, vertical | Complete | Decreased | URI | IVIg or Steroid | 6 months | |
| 53 | M | Left | Left | Vertical, horizontal | None | Decreased | URI | IVIg or Steroid | 3 months | |
| (6) | 18 | F | Right | No | Horizontal, vertical | None | Decreased | Fever, headche | No | NR |
| 26 | F | Left | No | Abduction | None | Normal | Sore throat | No | NR | |
| 26 | F | Left | No | Adduction, abduction | None | Decreased | URI | No | NR | |
| 32 | M | Left | No | Abduction | None | Decreased | No | Steroid | NR | |
| 35 | M | Left | No | Abduction, down | None | Decreased | URI | No | NR | |
| (7) | 47 | M | Left | Left | Adduction, vertical | Complete | Normal | URI | Steroid plus IVIg | 28 day |
| (9) | 35 | M | Left | Left | Horizontal, vertical | None | Absent | URI | No | 3 months |
| (10) | 32 | M | Left | Left | Horizontal, vertical | None | NR | URI | No | 5 weeks |
| (11) | 27 | M | Right | No | Abduction | None | Decreased | URI | IVIg | 52 days |
| (12) | 62 | F | Right | Right | Vertical, horizontal | None | NR | No | Steroid | 3 months |
| Present case | 68 | M | Right | Right | Adduction, vertical | Complete | Decreased | Gastroenteritis (Camplybacter infection) | No | 44 days |
F: female, M: male, URI: upper respiratory infection, IVIg: intravenous immunoglobulin, NR: not reported
Although most patients with unilateral external ophthalmoplegia are <50 years of age, the present patient was 68 years of age (Table) (4, 6, 7, 9-12). The median age at the onset of MFS is 44 years (14). This difference in the age at the onset of the disease may have affected the differential diagnosis. In the present case, we considered cerebrovascular disease and diabetes mellitus due to the unilateral oculomotor nerve palsy occurring at an older age and because the patient first noticed the symptoms on waking. Furthermore, the patient recovered over a period of 87 days without immunotherapy. If we had not examined the anti-GQ1b antibody status due to the older age-of-onset, we might have overlooked the correct diagnosis and misdiagnosed the patient with idiopathic unilateral oculomotor nerve palsy. Decreased DTRs may be a clinical clue that suggesting mild MFS without ataxia. Decreased DTRs are occasionally observed in patients with unilateral ophthalmoplegia resulting from anti-GQ1b antibody syndrome (Table) (4, 6, 7, 9-12). In our case, the DTRs were decreased in the initial neurological examination, and recovered during the follow-up period. Thus, a mild form of MFS without ataxia should be considered in patients presenting with unilateral isolated ophthalmoplegia and decreased DTRs, even in patients of older age.
The treatment for MFS remains controversial because some forms are self-limiting and because patients show spontaneous recovery (3, 15). Intravenous immunoglobulin slightly accelerates the improvement of ophthalmoplegia and ataxia (3, 8), but does not change the recovery period. Furthermore, plasmapheresis does not facilitate the improvement of ophthalmoplegia and ataxia (16). Thus, based on the severity of the patient's disease, we decided to apply conservative therapy. Without treatment, the median period for the recovery of ophthalmoplegia is 88 days (3, 15). In this case, although slight ptosis persisted, the patient's oculomotor nerve palsy disappeared by day 87.
In conclusion, a mild form of MFS without ataxia following campylobacter infection can cause unilateral oculomotor nerve palsy without ataxia. Mild MFS without ataxia must be considered in patients presenting with unilateral isolated ophthalmoplegia and decreased DTRs. Immunotherapy for mild MFS should be considered depending on the severity of the symptoms.
The authors state that they have no Conflict of Interest (COI).
Acknowledgement
The authors thank Prof. Susumu Kusunoki for performing the anti-ganglioside antibody analysis.
References
- 1. Chiba A, Kusunoki S, Obata H, Machinami R, Kanazawa I. Serum anti-GQ1b IgG antibody is associated with ophthalmoplegia in Miller Fisher syndrome and Guillain-Barré syndrome: clinical and immunohistochemical studies. Neurology 43: 1911-1917, 1993. [DOI] [PubMed] [Google Scholar]
- 2. Liu JX, Willison HJ, Pedrosa-Domellof F. Immunolocalization of GQ1b and related gangliosides in human extraocular neuromuscular junctions and muscle spindles. Invest Ophthalmol Vis Sci 50: 3226-3232, 2009. [DOI] [PubMed] [Google Scholar]
- 3. Shahrizaila N, Yuki N. Bickerstaff brainstem encephalitis and Fisher syndrome: anti-GQ1b antibody syndrome. J Neurol Neurosurg Psychiatry 84: 576-583, 2013. [DOI] [PubMed] [Google Scholar]
- 4. Lee SH, Lim GH, Kim JS, et al. . Acute ophthalmoplegia (without ataxia) associated with anti-GQ1b antibody. Neurology 71: 426-429, 2008. [DOI] [PubMed] [Google Scholar]
- 5. Fukami Y, Wong AH, Funakoshi K, Safri AY, Shahrizaila N, Yuki N. Anti-GQ1b antibody syndrome: anti-ganglioside complex reactivity determines clinical spectrum. Eur J Neurol 23: 320-326, 2016. [DOI] [PubMed] [Google Scholar]
- 6. Yuki N, Odaka M, Hirata K. Acute ophthalmoparesis (without ataxia) associated with anti-GQ1b IgG antibody: clinical features. Ophthalmology 108: 196-200, 2001. [DOI] [PubMed] [Google Scholar]
- 7. Ichikawa H, Kamiya Y, Susuki K, Suzuki M, Yuki N, Kawamura M. Unilateral oculomotor nerve palsy associated with anti-GQ1b IgG antibody. Neurology 59: 957-958, 2002. [DOI] [PubMed] [Google Scholar]
- 8. Mori M, Kuwabara S, Fukutake T, Hattori T. Intravenous immunoglobulin therapy for Miller Fisher syndrome. Neurology 68: 1144-1146, 2007. [DOI] [PubMed] [Google Scholar]
- 9. Susuki K, Yuki N, Muramatsu M, Hirata K. Unilateral ophthalmoparesis and limb ataxia associated with anti-GQ1b IgG antibody. J Neurol 247: 652-653, 2000. [DOI] [PubMed] [Google Scholar]
- 10. Smith J, Clarke L, Severn P, Boyce R. Unilateral external ophthalmoplegia in Miller Fisher syndrome: case report. BMC Ophthalmol 7: 7, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kinno R, Ichikawa H, Tanigawa H, Itaya K, Kawamura M. Unilateral abducens nerve palsy as an early feature of multiple mononeuropathy associated with anti-GQ1b antibody. Case Rep Neurol 3: 82-85, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Suzuki T, Chiba A, Kusunoki S, Chikuda M, Fujita T, Misu K. Anti-GQ1b ganglioside antibody and ophthalmoplegia of undetermined cause. Br J Ophthalmol 82: 916-918, 1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Koga M, Gilbert M, Li J, et al. . Antecedent infections in Fisher syndrome: a common pathogenesis of molecular mimicry. Neurology 64: 1605-1611, 2005. [DOI] [PubMed] [Google Scholar]
- 14. Ito M, Kuwabara S, Odaka M, et al. . Bickerstaff's brainstem encephalitis and Fisher syndrome form a continuous spectrum: clinical analysis of 581 cases. J Neurol 255: 674-682, 2008. [DOI] [PubMed] [Google Scholar]
- 15. Mori M, Kuwabara S, Fukutake T, Yuki N, Hattori T. Clinical features and prognosis of Miller Fisher syndrome. Neurology 56: 1104-1106, 2001. [DOI] [PubMed] [Google Scholar]
- 16. Mori M, Kuwabara S, Fukutake T, Hattori T. Plasmapheresis and Miller Fisher syndrome: analysis of 50 consecutive cases. J Neurol Neurosurg Psychiatry 72: 680, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]