Abstract
Arthrodesis of the first metatarsophalangeal joint is indicated for hallux valgus associated with degenerative changes, severe deformity, or rheumatoid arthritis and those for whom primary hallux valgus surgery has failed. Open approach requires extensive soft tissue dissection. The purpose of this Technical Note was to report the details of arthroscopic arthrodesis of the first metatarsophalangeal joint in severe and rigid hallux valgus deformity. This is a combination of endoscopic lateral release of the first metatarsophalangeal joint and arthroscopic arthrodesis of the joint. Endoscopic lateral release will convert the deformity into a flexible one and facilitate a subsequent arthrodesis procedure.
Arthrodesis of the first metatarsophalangeal joint is a reliable operation in the treatment of selected cases of hallux valgus associated with degenerative changes or severe deformity and those for whom primary hallux valgus surgery has failed.1 However, it involves extensive soft tissue dissection for exposure and debridement of the joint. Arthroscopic arthrodesis of the first metatarsophalangeal joint have been developed.2, 3 However, this is for in situ fusion. Recently, technique of arthroscopic first metatarsophalangeal arthrodesis has been reported for repair of fixed hallux varus deformity.4 First metatarsophalangeal arthroscopy in flexible hallux valgus5, 6 and technique of endoscopic lateral release of the first metatarsophalangeal joint7, 8, 9, 10, 11 has been reported. Endoscopic lateral release of the first metatarsophalangeal joint can convert the fixed hallux valgus deformity into a flexible one and arthroscopic first metatarsophalangeal arthrodesis can be performed afterward. The purpose of this Technical Note was to report the technique of arthroscopic first metatarsophalangeal arthrodesis in hallux valgus deformity. It is indicated for severe hallux valgus, hallux valgus associated with degeneration of the first metatarsophalangeal joint, and rheumatoid arthritis.12 The first metatarsal bone can be shortened at the joint level by means of arthroscopic burr if indicated, for example, in rheumatoid forefoot deformity or in severe hallux valgus with contracted skin over the lateral side. This technique is contraindicated in case of failed hallux valgus surgery with shortened first ray and transfer metatarsalgia requiring lengthening arthrodesis.13 It is also contraindicated if the bone quality is too poor for stable screw fixation (Table 1).
Table 1.
Indications and Contraindications of Arthroscopic Arthrodesis of the First Metatarsophalangeal Joint in Hallux Valgus Deformity
| Indications | Contraindications |
|---|---|
| 1. Severe hallux valgus | 1. Failed hallux valgus surgery with shortened first ray and transfer metatarsalgia requiring lengthening arthrodesis |
| 2. Hallux valgus associated with degeneration of the first metatarsophalangeal joint | 2. The bone quality is too poor for stable screw fixation |
| 3. Hallux valgus in rheumatoid arthritis |
Technique
Preoperative Planning and Patient Positioning
Preoperative clinical assessment and radiographs should confirm the surgical indication including severe hallux valgus deformity, rigid deformity, and painful degeneration of the first metatarsophalangeal joint (Fig 1).
Fig 1.
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. Standing radiograph of the feet of the illustrated case shows severe right hallux valgus deformity associated with degeneration of the first metatarsophalangeal joint (arrow). The lateral sesamoid bone (LS) is dislocated into the intermetatarsal space.
The patient is in supine position with the legs spread. A thigh tourniquet is applied to provide a bloodless operative field. A 2.7-mm 30° arthroscope (Henke Sass Wolf, Tuttlingen, Germany) and a 1.9-mm 30° arthroscope (Henke Sass Wolf) are used for this procedure. Fluid inflow is by gravity, and no arthro-pump is used. No continuous traction of the first metatarsophalangeal joint is applied.
Portal Placement
Toe web and plantar portals are used for the endoscopic lateral release of the first metatarsophalangeal joint. The toe web portal is made at the dorsal surface of the first toe web. It is placed slightly toward the hallux to facilitate subsequent screw insertion via this portal. The plantar portal is at the sole and established by an inside-out method. The arthroscope-trocar is inserted via the toe web portal and advanced proximally along the deep surface of the intermetatarsal ligament till the trocar tip touches the plantar aponeurosis at the level of the tarsometatarsal joint. The passage of the trocar should be performed gently, and there should not be any resistance before the plantar aponeurosis is reached. The plantar aponeurosis is perforated by the trocar tip and the plantar portal is made at this point.
Medial and dorsolateral portals are used for arthroscopic first metatarsophalangeal arthrodesis. Both portals are at the level of the first metatarsophalangeal joint line. The medial portal is at the midpoint of the medial joint line of the first metatarsophalangeal joint, and the dorsolateral portal is at the lateral side of the extensor hallucis longus tendon.
Endoscopic Release of the Intermetatarsal Ligament
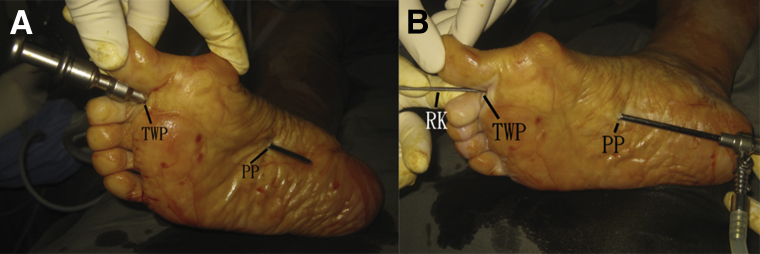
Three- to 4-mm longitudinal skin incisions are made at the toe web and plantar portal. The plantar portal is the viewing portal and the toe web portal is the working portal throughout the endoscopic lateral release of the first tarsometatarsal joint (Fig 2).
Fig 2.
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. (A) The arthroscope-trocar is inserted via the toe web portal (TWP) and advanced proximally along the deep surface of the intermetatarsal ligament till the trocar tip touches the plantar aponeurosis at the level of the tarsometatarsal joint. The plantar aponeurosis is perforated by the trocar tip and the plantar portal (PP) is made at this point. (B) The plantar portal (PP) is the viewing portal and the toe web portal (TWP) is the working portal throughout the endoscopic lateral release of the first tarsometatarsal joint. (RK, retrograde knife.)
The retrograde knife (Smith & Nephew, Andover, MA) is introduced via the toe web portal. It passes under the intermetatarsal ligament until the proximal edge of the ligament is reached. The proximal edge of the ligament is hooked by the knife, and the ligament is cut by retrieval of the knife (Fig 3).
Fig 3.
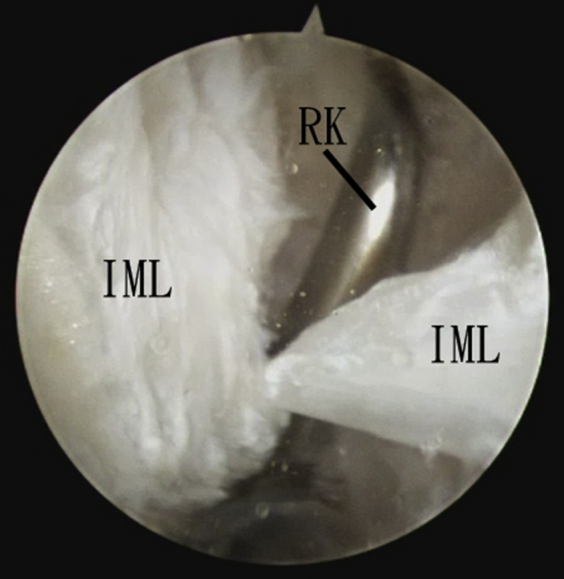
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. The plantar portal is the viewing portal, and the toe web portal is the working portal. The intermetatarsal ligament (IML) is cut by the retrograde knife (RK).
Endoscopic Release of the Adductor Hallucis Insertion
After release of the intermetatarsal ligament, the arthroscope can move dorsally through the cut edges of the intermetatarsal ligament. The arthroscope is turned medially, and the adductor hallucis insertion to the fibular sesamoid can be seen. The adductor hallucis insertion is released by the retrograde knife (Fig 4). Sometimes, several cuts are needed for complete release of the insertion.
Fig 4.
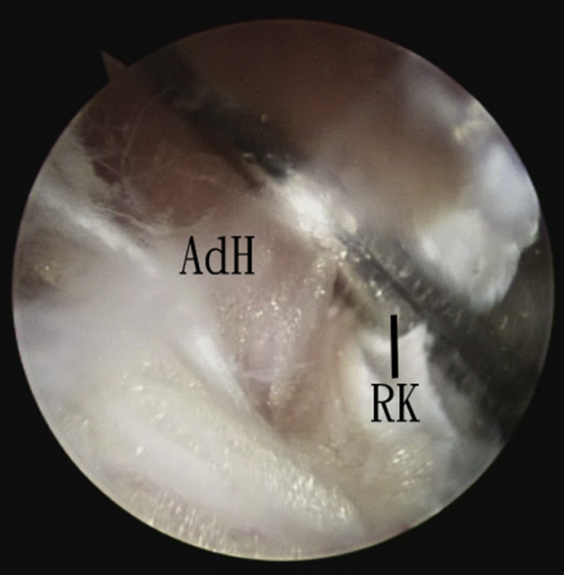
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. The plantar portal is the viewing portal and the toe web portal is the working portal. The adductor hallucis insertion (AdH) is cut by the retrograde knife (RK).
Endoscopic Release of Lateral Capsule-Ligamentous Complex of the First Metatarsophalangeal Joint
After release of the adductor hallucis insertion, the fibular sesamoid bone can be seen. The lateral capsule-ligamentous complex of the first metatarsophalangeal joint can be released just above the fibular sesamoid bone by the retrograde knife (Fig 5). The most proximal part of the release should be started more dorsally to avoid damage to the hallucal digital nerve.8 The release should be proceeded distal enough to cut the suspensory sesamoid ligament.8 This can ensure complete lateral release, and the fibular sesamoid bone can be reduced under the metatarsal head (Fig 6).
Fig 5.
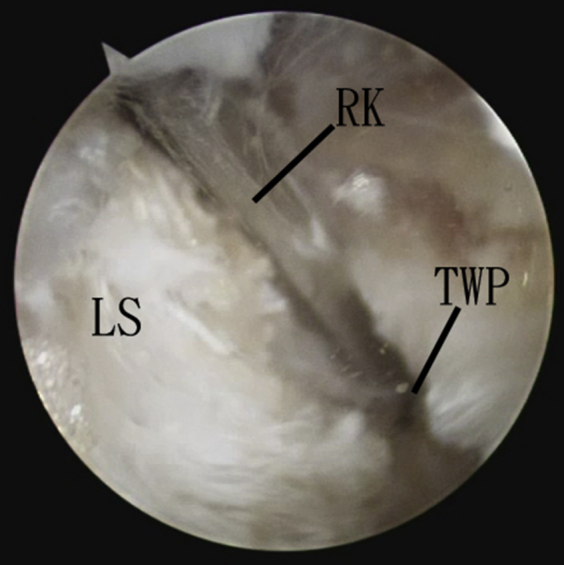
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. The plantar portal is the viewing portal and the toe web portal is the working portal. The lateral capsule-ligamentous complex of the first metatarsophalangeal joint is released just above the lateral sesamoid bone (LS) by the retrograde knife (RK). (TWP, toe web portal.)
Fig 6.
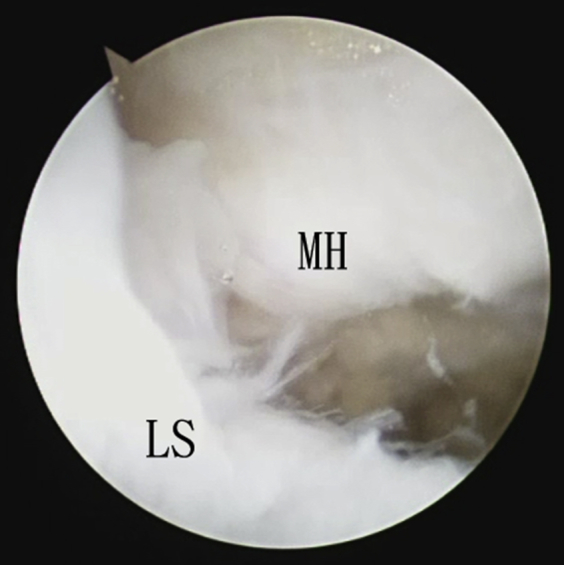
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. After the lateral release, the lateral sesamoid (LS) can be reduced under the metatarsal head (MH).
Arthroscopic Removal of the Articular Cartilage of the First Metatarsophalangeal Joint
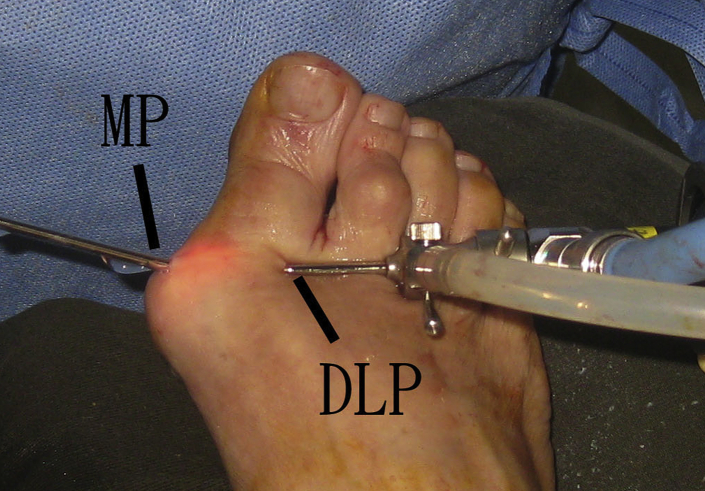
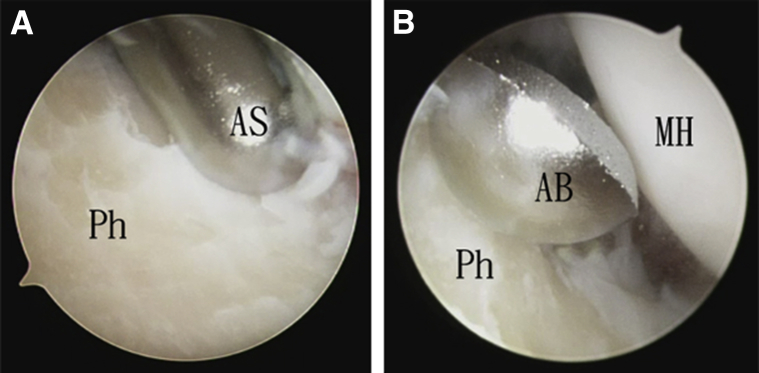
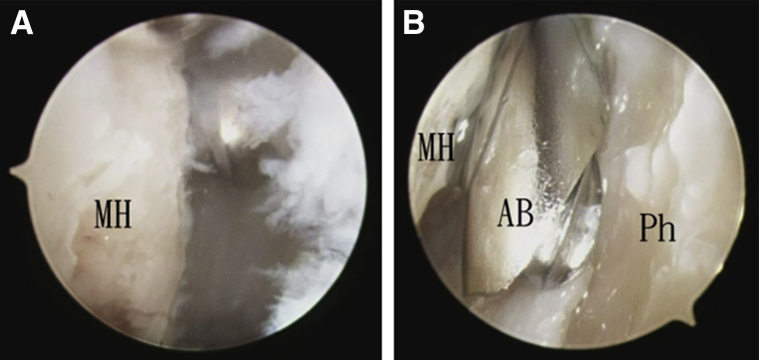
After the lateral release, the hallux valgus deformity can be corrected and the dorsolateral and medial portals can be placed at usual locations (Fig 7). The dorsolateral and medial portals are interchangeable as the viewing and working portals. Different parts of the first metatarsophalangeal joint can be visualized by placing the arthroscope via the medial or dorsolateral portal. The joint can be debrided by an arthroscopic shaver (Dyonics; Smith & Nephew) and an arthroscopic burr (Dyonics; Smith & Nephew) via the opposite portal. The remaining articular cartilage is removed. The subchondral bone and the contour of the articular surfaces are preserved as much as possible (Figs 8 and 9).
Fig 7.
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. First metatarsophalangeal arthroscopy is performed through the dorsolateral (DLP) and medial (MP) portals.
Fig 8.
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. The medial portal is the viewing portal and the dorsolateral portal is the working portal. (A) The articular cartilage of the base of the proximal phalanx (Ph) is removed by the arthroscopic shaver (AS). (B) The articular cartilage of the metatarsal head (MH) is resected by the arthroscopic burr (AB).
Fig 9.
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. The dorsolateral portal is the viewing portal and the medial portal is the working portal. (A) The articular cartilage of the metatarsal head (MH) is resected. (B) The articular cartilage of the base of the proximal phalanx (Ph) is removed by the arthroscopic burr (AB).
Microfracture of the Fusion Surfaces
The subchondral bone is microfractured by an arthroscopic awl (Acufex; Smith & Nephew) via the dorsolateral and medial portals with the arthroscope in the opposite portal (Fig 10).
Fig 10.
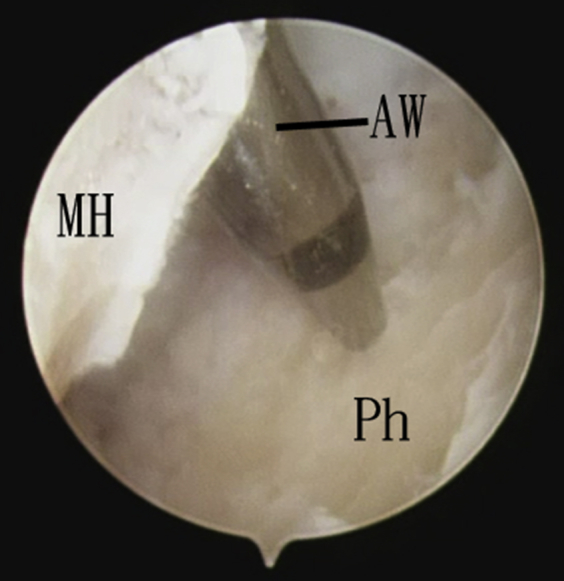
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. The dorsolateral portal is the viewing portal and the medial portal is the working portal. The subchondral bone is microfractured by an arthroscopic awl (AW). (MH, metatarsal head; Ph, base of proximal phalanx.)
Bunionectomy via the Medial Portal
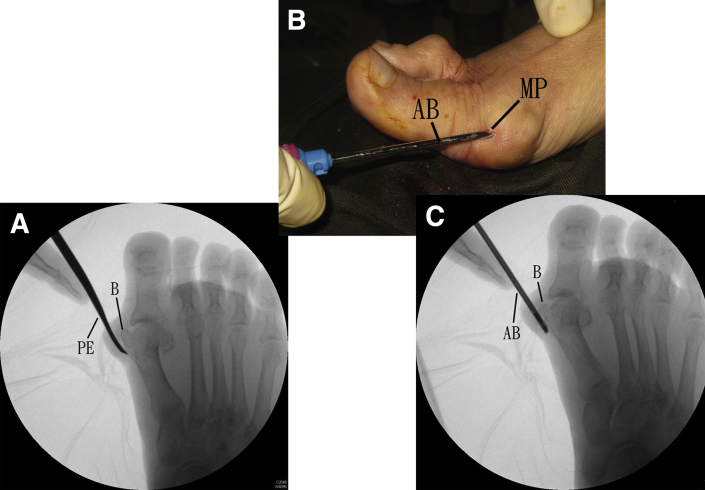
The soft tissue over the bunion is stripped by a small periosteal elevator via the medial portal. Bunionectomy is then performed with the arthroscopic burr via the medial portal and under fluoroscopic guide (Fig 11).
Fig 11.
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. (A) The soft tissue over the bunion (B) is stripped by a small periosteal elevator (PE) via the medial portal. (B) Bunionectomy is then performed with the arthroscopic burr (AB) via the medial portal (MP). (C) This is performed under fluoroscopic guide.
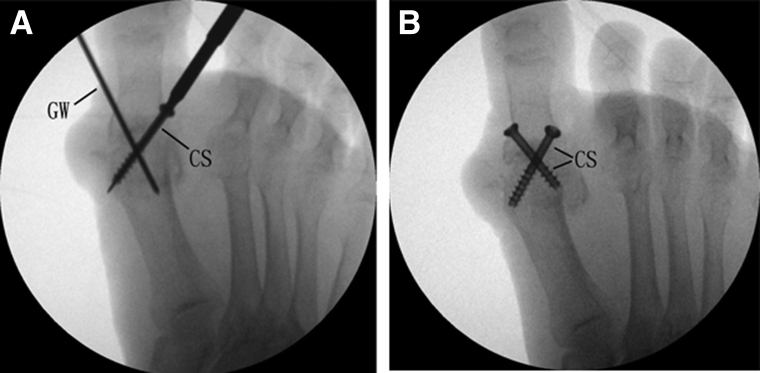
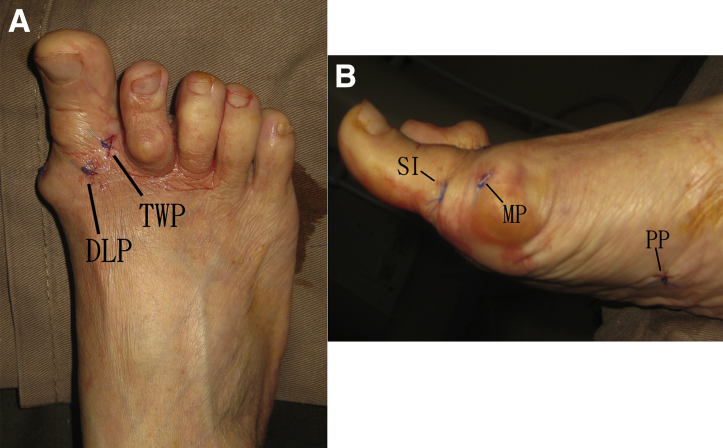
Positioning of the First Metatarsophalangeal Joint and Screw Fixation
The first metatarsophalangeal joint is then placed into the desirable position for arthrodesis. This is transfixed with two 4.0-mm cannulated screws (Synthes, West Chester, PA) (Fig 12, Video 1, Table 2). One of the screws can be inserted via the toe web portal. After the procedure, the portal incisions are closed with simple sutures (Fig 13), and bulky dressing is applied. This is protected by a dorsal slab for 4 to 6 weeks before weight-bearing walking with wooden-based sandal is allowed.
Fig 12.
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. (A) The first metatarsophalangeal joint is then placed into the desirable position for arthrodesis. Guide wires (GWs) are inserted under fluoroscopic guide. (B) The arthrodesis site is transfixed by two 4.0-mm cannulated screws (CSs).
Table 2.
Pearls and Pitfalls of Arthroscopic Arthrodesis of the First Metatarsophalangeal Joint in Hallux Valgus Deformity
| Pearls | Pitfalls |
|---|---|
| 1. The toe web portal is placed slightly toward the hallux to facilitate subsequent screw insertion via this portal. 2. The suspensory sesamoid ligament should be released before the fibular sesamoid can be reduced. 3. The contour of the articular surfaces should be preserved. 4. The first metatarsal bone can be shortened at the joint level by means of arthroscopic burr if indicated, e.g., in rheumatoid forefoot deformity or in severe hallux valgus with contracted skin over the lateral side. |
1. Release of the proximal part lateral capsule-ligamentous complex may injure the nearby hallucal digital nerve. 2. The dislocated fibular sesamoid bone should be reduced under the first metatarsal head. Subluxed fibular sesamoid bone will block the reduction of the 1-2 intermetatarsal angle after first metatarsophalangeal arthrodesis. |
Fig 13.
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. After the procedure, the portal incisions are closed with simple sutures. (A) Dorsal view shows the correction of hallux valgus deformity and the toe web (TWP) and dorsolateral (DLP). (B) Medial view shows the plantar portal (PP), medial portal (MP), and the screw insertion point (SI).
Discussion
It is difficult to perform first metatarsophalangeal arthroscopy in cases of severe hallux valgus or associated degeneration of the joint because the joint is contracted and joint anatomy is distorted. Endoscopic lateral release can relieve the soft tissue tension around the joint. Correction of the hallux valgus deformity restores the normal arthroscopic anatomy and facilitates the subsequent arthroscopic arthrodesis.
We adopt the 2-screw fixation technique because it has been reported to have a fusion success rate of 91% to 100%.14 The 1-2 intermetatarsal angle is usually acceptably corrected by the first metatarsophalangeal arthrodesis.15 Therefore, additional procedures, for example, a proximal first metatarsal osteotomy to correct the intermetatarsal angle, will not be necessary.
The advantages of this minimally invasive approach include better cosmesis, less soft tissue dissection, and fewer wound complications. The potential risks of this procedure include malunion, nonunion of the arthrodesis site, and injury to the hallucal digital nerve (Table 3).
Table 3.
Advantages and Risks of Arthroscopic Arthrodesis of the First Metatarsophalangeal Joint in Hallux Valgus Deformity
| Advantages | Risks |
|---|---|
| 1. Less wound complication | 1. Malunion of the arthrodesis site |
| 2. Less soft tissue trauma | 2. Nonunion of the arthrodesis site |
| 3. Better cosmesis | 3. Injury to the hallucal digital nerve |
Footnotes
The authors reports that he has no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. The plantar portal is the viewing portal and the toe web portal is the working portal. The intermetatarsal ligament, adductor hallucis insertion, and lateral capsule-ligamentous complex are released with a retrograde knife. After correction of the hallux valgus deformity, the first metatarsophalangeal arthroscopy is performed with the dorsolateral and medial portals. The 2 portals are interchangeable as the working and viewing portals. The articular cartilage is resected and the subchondral bone is microfractured. The joint is placed in desirable position and is transfixed by 2 cannulated screws.
References
- 1.Wood E.V., Walker C.R., Hennessy M.S. First metatarsophalangeal arthrodesis for hallux valgus. Foot Ankle Clin. 2014;19:245–258. doi: 10.1016/j.fcl.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Vaseenon T., Phisitkul P. Arthroscopic debridement for first metatarsophalangeal joint arthrodesis with a 2- versus 3-portal technique: A cadaveric study. Arthroscopy. 2010;26:1363–1367. doi: 10.1016/j.arthro.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 3.Perez Carro L., Busta Vallina B. Arthroscopic-assisted first metatarsophalangeal joint arthrodesis. Arthroscopy. 1999;15:215–217. doi: 10.1053/ar.1999.v15.0150211. [DOI] [PubMed] [Google Scholar]
- 4.Lui T.H. Arthroscopic first metatarsophalangeal arthrodesis for repair of fixed hallux varus deformity. J Foot Ankle Surg. 2015;54:1127–1131. doi: 10.1053/j.jfas.2015.06.027. [DOI] [PubMed] [Google Scholar]
- 5.Lui T.H. First metatarsophalangeal arthroscopy in patients with post-traumatic hallux valgus. Foot. 2015;25:270–276. doi: 10.1016/j.foot.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Lui T.H. First metatarsophalangeal joint arthroscopy in patients with hallux valgus. Arthroscopy. 2008;24:1122–1129. doi: 10.1016/j.arthro.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 7.Lui T.H., Ling S.K., Yuen S.C. Endoscopic-assisted correction of hallux valgus deformity. Sports Med Arthrosc Rev. 2016;24:e8–e13. doi: 10.1097/JSA.0000000000000078. [DOI] [PubMed] [Google Scholar]
- 8.Lui T.H., Chan K.B., Chan L.K. Endoscopic distal soft-tissue release in the treatment of hallux valgus: A cadaveric study. Arthroscopy. 2010;26:1111–1116. doi: 10.1016/j.arthro.2009.12.027. [DOI] [PubMed] [Google Scholar]
- 9.Lui T.H., Chan K.B., Chow H.T., Ma C.M., Chan P.K., Ngai W.K. Arthroscopy-assisted correction of hallux valgus deformity. Arthroscopy. 2008;24:875–880. doi: 10.1016/j.arthro.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Lui T.H. Arthroscopy and endoscopy of the foot and ankle: Indications for new techniques. Arthroscopy. 2007;23:889–902. doi: 10.1016/j.arthro.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Lui T.H., Ng S., Chan K.B. Endoscopic distal soft tissue procedure in hallux valgus surgery. Arthroscopy. 2005;21:1403. doi: 10.1016/j.arthro.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 12.Drampalos E., Vun S.H., Fayyaz I. Intramedullary and intra-osseous arthrodesis of the hallux metatarsophalangeal joint. J Orthop Surg. 2016;24:358–361. doi: 10.1177/1602400317. [DOI] [PubMed] [Google Scholar]
- 13.Chowdhary A., Drittenbass L., Stern R., Assal M. Technique tip: Simultaneous first metatarsal lengthening and metatarsophalangeal joint fusion for failed hallux valgus surgery with transfer metatarsalgia. Foot Ankle Surg. 2017;23:e8–e11. doi: 10.1016/j.fas.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 14.Lucas K.J., Morris R.P., Buford W.L., Jr., Panchbhavi V.K. Biomechanical comparison of first metatarsophalangeal joint arthrodeses using triple-threaded headless screws versus partially threaded lag screws. Foot Ankle Surg. 2014;20:144–148. doi: 10.1016/j.fas.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 15.McKean R.M., Bergin P.F., Watson G., Mehta S.K., Tarquinio T.A. Radiographic evaluation of intermetatarsal angle correction following first MTP joint arthrodesis for severe hallux valgus. Foot Ankle Int. 2016;37:1183–1186. doi: 10.1177/1071100716656442. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity of the right foot. The patient is in supine position with the legs spread. The plantar portal is the viewing portal and the toe web portal is the working portal. The intermetatarsal ligament, adductor hallucis insertion, and lateral capsule-ligamentous complex are released with a retrograde knife. After correction of the hallux valgus deformity, the first metatarsophalangeal arthroscopy is performed with the dorsolateral and medial portals. The 2 portals are interchangeable as the working and viewing portals. The articular cartilage is resected and the subchondral bone is microfractured. The joint is placed in desirable position and is transfixed by 2 cannulated screws.