Summary
Although bariatric surgery is the most effective treatment for severe and complex obesity, less is known about its psychosocial impact. This systematic review synthesizes qualitative studies investigating the patient perspective of living with the outcomes of surgery. A total of 2,604 records were screened, and 33 studies were included. Data extraction and thematic synthesis yielded three overarching themes: control, normality and ambivalence. These were evident across eight organizing sub‐themes describing areas of life impacted by surgery: weight, activities of daily living, physical health, psychological health, social relations, sexual life, body image and eating behaviour and relationship with food. Throughout all these areas, patients were striving for control and normality. Many of the changes experienced were positive and led to feeling more in control and ‘normal’. Negative changes were also experienced, as well as changes that were neither positive nor negative but were nonetheless challenging and required adaptation. Thus, participants continued to strive for control and normality in some aspects of their lives for a considerable time, contributing to a sense of ambivalence in accounts of life after surgery. These findings demonstrate the importance of long‐term support, particularly psychological and dietary, to help people negotiate these challenges and maintain positive changes achieved after bariatric surgery.
Keywords: bariatric surgery, patient experience, qualitative, synthesis
Introduction
The World Health Organization reported that in 2014 over 600 million people worldwide, or roughly 13% of adults, were obese (body mass index [BMI] of ≥30). This represents a doubling of figures since 1980 1. The health risks of obesity have been well documented, including an increased risk of type 2 diabetes, cardiovascular disease, certain types of cancer, depression, reduced health‐related quality of life (HRQL) and premature death 2, 3, 4, 5, 6, 7, 8, 9, 10. Systematic reviews of quantitative evidence have shown that obesity (bariatric) surgery is the most effective treatment for severe and complex obesity, defined as a BMI ≥40, or between 35 and 40 with another significant disease that could be improved by weight loss, such as diabetes 11, 12, 13, leading to greater weight loss and improvement in some obesity‐related comorbidities (such as diabetes) in the short‐term (up to 2 years post‐surgery), compared with other interventions (lifestyle or drug therapy). Far less data are available with regard to the long‐term outcomes 12, 14, although there is evidence that some patients experience weight re‐gain, which can negatively impact physical and psychological health and HRQL 15, 16, 17, 18, 19, 20. While previous quantitative research mainly focuses on the clinical outcomes of bariatric surgery, previous qualitative research with bariatric surgery patients has provided detailed accounts of the psychosocial impacts of the surgery 21, 22, 23, 24.
Qualitative research can provide valuable insight into patients' experiences of living with the outcomes of a health treatment, in particular the complexity and depth of the lived experience 25. In particular, the qualitative literature highlights the variability and complexity of psychosocial changes associated with surgery and weight change (both gain and loss) 20, 26. However, the current published qualitative literature tends to report on small, single‐centre samples, with individual studies focusing on one or two specific areas impacted by bariatric surgery, such as body image or relationship with food (e.g.27, 28), rather than the full spectrum of outcomes experienced.
It is increasingly being recognized that there should be some attempt to synthesize the understandings gained from these isolated studies to inform the evidence base, as is commonly performed for quantitative research 29, 30, 31. Qualitative synthesis offers a way of bringing together disparate studies and overcoming issues of sample size and focus, generating clinically useful knowledge. Qualitative synthesis has been defined as ‘the bringing together of findings on a chosen theme, the results of which should, in conceptual terms, be greater than the sum of parts’ 29. The aim is not solely to aggregate findings as in quantitative meta‐analyses but to generate new insights that can be used to influence policy and practice, and generate new research questions 29, 32, 33, 34. Qualitative research studies have not been included in previous systematic reviews of bariatric surgery and are often not included in systematic reviews of quantitative evidence more generally, because of the difficulty in synthesizing the findings with quantitative evidence 12, 14, 35.
There are now a number of published qualitative studies that have examined patients' perspectives of living with bariatric surgery, which when synthesized could provide useful knowledge to inform the evidence base and clinical practice. In this study, a systematic review of qualitative research was undertaken to synthesize what is currently known about the patient perspective of living with the outcomes of bariatric surgery. This was undertaken as part of a larger study that aimed to develop a core outcome set for bariatric surgery 36 and to generate new insights on the outcomes of bariatric surgery, which could be used to influence clinical practice and future research.
Methods
A synthesis of relevant qualitative studies was undertaken. The study had three main steps (i) systematic identification of studies; (ii) study appraisal and data extraction; and (iii) inductive thematic synthesis of study findings.
Systematic identification of relevant studies – search strategy and selection criteria
The first author (K. C.) conducted a series of electronic searches in May 2014 in the Ovid versions of MEDLINE, EMBASE, PsycINFO, the Cochrane Library, CINAHL and Web of Science (including Science Citation Index Expanded, Social Sciences Citation Index and Arts & Humanities Citation Index). The search strategies combined search terms for bariatric surgery, with terms for qualitative research ( Supporting Information ). There were no limits for study design or language. Search results were downloaded and managed within Endnote software 37. K. C. screened all abstracts, and full‐text articles were obtained for those that were potentially relevant. Exclusion criteria included (i) participants had not yet undergone bariatric surgery; (ii) experiences of surgery‐specific issues were not investigated; (iii) qualitative methods were not used. Review articles, conference abstracts and theses with no full‐text article published were excluded. Non‐English language articles were translated.
All included articles were double‐checked by the fourth author (A. O. S.) to ensure they met the inclusion criteria. To identify additional relevant studies, the reference lists of included studies were examined, and the journal Qualitative Health Research was hand searched. Additionally, relevant experts in the field (Dr Lindsey Bocchieri‐Ricciardi, Prof Jane Odgen and Dr Karen Throsby) were contacted to identify any additional studies not found through the other search methods.
Appraisal and data extraction
Study appraisal and data extraction were carried out concurrently using a modified version of the Critical Appraisal Skills Program criteria for quality appraisal of qualitative research, which was modified for use in this study (available upon request from the authors) 29. Currently, there is considerable debate as to whether quality appraisal of qualitative research should be undertaken in order to exclude certain studies from reviews 38, 39. Some researchers have found that excluding poor quality studies from qualitative systematic reviews had no meaningful impact on their synthesis findings, as these studies contributed relatively little to the synthesis 30, 38. In this review, quality appraisal was used to facilitate thorough understanding of the studies and was not used to discard any studies. Initially, appraisal and data extraction were carried out independently by K. C. and A. O. S. on five of the studies. Their results were compared and discussed in order to resolve any differences in interpretation of the questions on the data extraction form. Minor changes were then made to the data extraction form. K. C. then carried out appraisal and data extraction on the remainder of the studies, and any queries that arose were discussed with A. O. S.
Inductive thematic synthesis
An inductive thematic synthesis was undertaken, broadly on the basis of the thematic analysis for synthesizing qualitative studies described by Thomas and Harden 30. This includes a process of translating concepts or themes from one study to another, similar to the reciprocal translation technique used in meta‐ethnography, first described by Noblit and Hare and applied to health research by Campbell et al. and Malpass et al. 29, 40, 41. A process of thematic networking was used to map and link themes into basic, organizing and global themes (Fig. 1) 34, 42. Themes reported by the authors of each study were extracted and listed (using authors' original wording) as a separate row in a spreadsheet. Findings from individual studies were then used to populate the columns of the spreadsheet, and a process of reciprocal translation was undertaken, whereby each study was scrutinized for evidence of all themes arising. Throughout this process, the description and wording of the themes were continually revised, and notes made as to how themes related and how some could be merged. Initial thematic networks were drawn to facilitate understanding of the themes, and broad organizing themes were identified 42. Each organizing theme was written up descriptively, and three global themes were identified.
Figure 1.
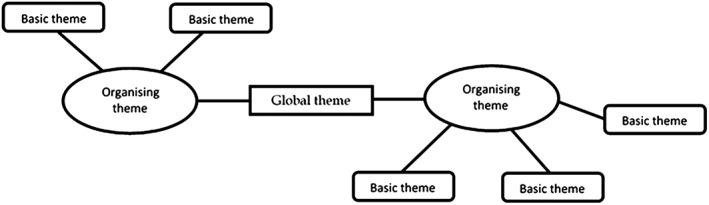
Example of a thematic network.
Results
Study characteristics
Of 2,604 records screened, 41 papers relating to 33 studies met the inclusion criteria to be included in the review (Fig. 2). Detailed characteristics of included studies are presented in Table 1. Included studies were published between 2002 and 2014. Twelve studies (36.4%) were from the USA and Canada, eight (24.2%) from Scandinavia, six (18.2%) from Brazil, five (15.2%) from the UK, one (3.0%) from the Netherlands and one (3.0%) from New Zealand. Four studies were translated from Portuguese.
Figure 2.
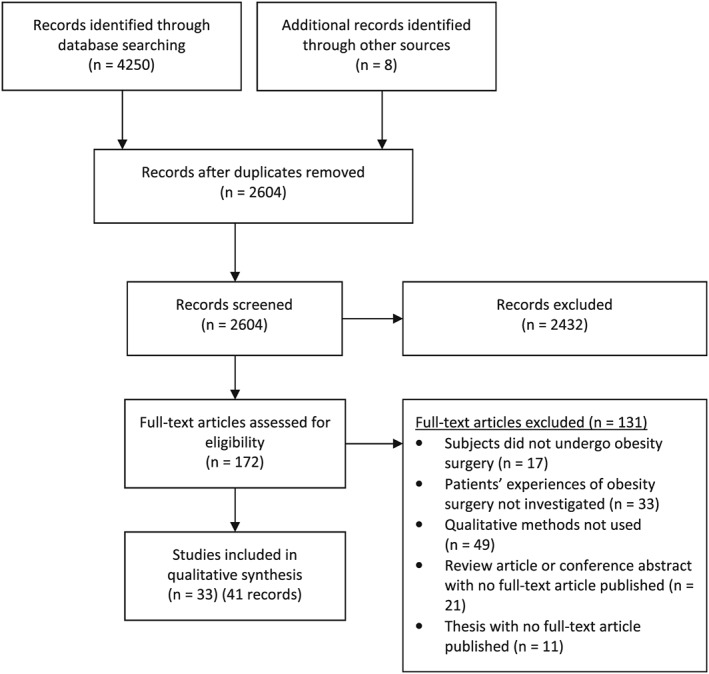
PRISMA systematic review diagram for qualitative synthesis. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta‐Analyses.
Table 1.
Characteristics of included studies in qualitative synthesis
| Study | Focus of investigation | Setting | Sample size and gender | Type of surgery and time since surgery | Data collection method |
|---|---|---|---|---|---|
| Bocchieri et al., 2002 21; Meana and Ricciardi, 2008 22 | Psychosocial experiences following gastric bypass | Hospital | 33 (24 women) | RYGB, 6 months–10 years | Interviews (n = 22), focus groups (n = 11) |
| Ogden et al., 2005, 2006 23, 43 | Post‐surgery HRQL and eating behaviour | Hospital | 15 (14 women) | Variety: gastric banding, gastric bypass and vertical gastroplasty, 4–33 months | Interviews |
| Wysoker, 2005 44 | Individual experiences of bariatric surgery | Not reported | 8 (5 women) | Type not reported, ≥1 year (unclear length of time), | Interviews |
| Earvolino‐Ramirez, 200845 | Case study of gastric bypass surgery | Not reported | 1 woman | Gastric bypass, 8 months | Case study – interview |
| Pastoriza and Guimarães, 200846 | Behavioural change following bariatric surgery | Not reported | 8 (7 women) | Capella method restrictive malabsorptive surgery, 1–5 years | Interviews |
| Throsby, 2008, 2009 47, 48, 49, 50 | Discourse of re‐birth in the context of bariatric surgery | Community | 35 (29 women) | Not reported | One focus group, then interviews |
| Agra and Henriques, 2009 51 | Post‐surgery HRQL | Private gastroenterology practice | 16 women | Gastroplasty, ‘medium‐term post‐op period’ (time not specified) | Interviews |
| Norris, 2009 52 | Outcomes of bariatric surgery | Hospital | 1 woman | Gastroplasty or bypass – unclear, interviewed at 2,6,12 and 18 months post‐op | Case study – longitudinal interviews |
| Sutton et al., 2009 53 | Individual experiences of bariatric surgery | Not reported | 14 women | RYGB, >12 months | Interviews |
| Zijlstra et al., 2009 19 | Outcomes of bariatric surgery | Hospital | 11 (10 women) | AGB, 2–5 years | Interviews |
| Groven et al., 2010, 2012 26, 54 | Side effects of bariatric surgery and bodily change | Health clinic and community | 22 women | Gastric bypass, 5–6 years | Interviews‐two participants interviewed 1 year later |
| LePage, 2010 55 | Individual experiences of bariatric surgery | Bariatric healthcare practices | 12 (8 women) | RYGB, 2–9 years | Interviews |
| Magdaleno et al., 2010, 2011 56, 57, 58 | Discourse of transformation in the context of bariatric surgery | Hospital | 7 women | Type not reported, 18 months–3 years | Interviews |
| Wilson, 2010 59 | Outcomes of bariatric surgery | Personal reflection of author who underwent surgery | 1 woman (author) | Type not reported, 12 months | Kept notes of her own experiences |
| Engström and Forsberg, 2011 60 | Expectations and outcomes of bariatric surgery | Hospital | 16 (12 women) | RYGB and BPD‐DS, interviewed pre‐op, 1, 2 years post‐op | Longitudinal interviews |
| Marcelino and Patrício, 2011 61 | Outcomes of bariatric surgery | Not reported | 6 (5 women) | Gastroplasty, time not reported | Interviews |
| Ogden et al., 2011 20 | Lack of success and revision procedures | Obesity clinic and a patient support group | 10 (8 women) | Variety: band then bypass (n = 4), band then sleeve (n = 2), band awaiting bypass (n = 1), bypass followed by pouch revision (n = 2), bypass only (n = 1), 1–10 years since initial operation | Interviews |
| Throsby, 2012 62 | Bodily discourses in the context of bariatric surgery | Hospital | 153 patient consultations observed (103 women), plus 8 seminars, 15 interviews (11 women) | Gastric banding, except 3 gastric bypass, time not reported | Observations of clinics and seminars, interviews |
| Ivezaj et al., 2012 63 | Substance abuse and bariatric surgery | Substance abuse treatment programme | 24 (18 women) | RYGB, mean time since surgery 5.5 (± 3.1 years) | Interviews |
| Zunker et al., 2012 64 | Eating behaviours post‐surgery | Community and via a research institute | 29 (27 women) | Mostly RYGB, others not specified, 1–14 years, mean 8 years, median 2 years | Structured focus groups – nominal group technique |
| Benson‐Davies et al., 2013 28 | Outcomes of bariatric surgery | Community | 18 women | RYGB, mean 75.0 ± 32.4 months (6.25 years) | Focus groups |
| Castro et al., 2013 65 | Body image following bariatric surgery | Diabetes and hypertension service | 20 women | Gastroplasty, mean 2.85 years (± 0.988) | Interviews |
| Gilmartin, 2013 27 | Body image following bariatric surgery | Hospital | 20 (18 women) | Type not reported, 2–5 years | Interviews |
| Gronning et al., 2013 66 | Decision‐making around bariatric surgery | Hospital | 12 (10 women) | RYGB (n = 10), AGB (n = 1), both RYGB and AGB (n = 1), time not reported | Interviews |
| Knutsen et al., 2013 67 | Empowerment discourses in the context of bariatric surgery | Hospital | 9 (8 women) | RYGB, interviewed twice pre‐op, and at 2 weeks, 2–3 months, 9 months post‐op | Longitudinal interviews |
| Mariano et al., 2013 68 | Outcomes of bariatric surgery | Hospital | 30 (24 women) | RYGB, mean 5.7 years (± 1.3) | Interviews |
| Natvik et al., 2013 69 | Outcomes of bariatric surgery | Hospital | 8 (4 women) | Duodenal switch, 5–7 years | Interviews |
| Stolzenberger et al., 2013 24 | Post‐surgery HRQL | Hospital | 61 (48 women) | RYGB (72%), AGB, 2–9 years | Focus groups |
| Forsberg et al. 2014 70 | Expectations and outcomes of bariatric surgery | Hospital | 10 (8 women) | RYGB, 1–2 months | Interviews |
| Geraci et al., 2014 71 | Outcomes of bariatric surgery | Community | 9 women | SG (n = 7) and RYGB (n = 2), 2.5–7.5 years | Interviews |
| Jensen et al., 2014 72 | Body image following bariatric surgery | Hospital and community | 5 women | RYGB, 1–12 months | Interviews |
| Lyons et al., 2014 73 | Body image following bariatric surgery | Hospital | 15 (12 women) | Type not reported, mean 26.1 months | Focus groups |
| Warholm et al., 2014 74 | Outcomes of bariatric surgery | Hospital | 2 women | BPD‐DS, interviewed at 3, 6, 9 and 12 months post‐op | Longitudinal interviews |
AGB, adjustable gastric band; BPD‐DS, biliopancreatic diversion with duodenal switch; HRQL, health‐related quality of life; RYGB, Roux‐en‐Y gastric bypass; SG, sleeve gastrectomy.
The majority of studies used one‐off individual interviews to collect data (n = 25, 75.8%), only five undertook longitudinal (repeated) interviews over periods of up to 2 years. Four studies (12.1%) used focus group discussion, and two (6.1%) used both interviews and focus groups. One study involved observation of clinic consultations and observation of seminars in addition to conducting interviews 62, and one documented her own experience in a personal notebook 59. Sample sizes ranged from 1 (three studies – one personal reflection and two case studies) to 61 for interview and focus group studies. Across all 33 studies, there were 656 participants recruited, the majority of which were women (529, 80.6%). Twenty‐three of the studies reported both the type of operation that participants underwent and the number of participants who underwent each type of operation. Among these, the majority of participants were reported to have undergone a Roux‐en‐Y gastric bypass (n = 248), followed by the adjustable gastric band (n = 45), gastroplasty (n = 43), duodenal switch (n = 10), sleeve gastrectomy (n = 9) and ‘capella method restrictive malabsorptive surgery’ (n = 8).
Inductive thematic synthesis
Three global themes about the experience of living with the outcomes of bariatric surgery were identified (i) control; (ii) normality; and (iii) ambivalence. These reflected eight organizing themes encompassing a number of basic themes: ‘Weight’, ‘activities of daily living’, ‘physical health’, ‘psychological health’, ‘social relations’, ‘sexual life’, ‘body image’ and ‘eating behaviour and relationship with food’. The organizing themes and the basic themes they encompassed are presented in Table S1. A thematic network showing the organizing and global themes is provided in Fig. 3. Results are now presented under the three global themes with reference to the lower‐level organizing themes where appropriate. Direct participant quotes from the studies have been used to illustrate themes; when these have not been available, the words of the authors from the original studies are quoted to illustrate particular aspects.
Figure 3.
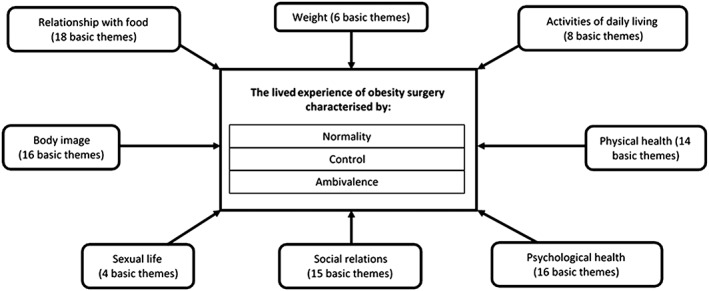
Thematic network describing the lived experience of obesity surgery.
Control
Participants underwent bariatric surgery in the hopes of achieving better control of their eating, weight, health and lives. Central to this was being in control of eating and weight. The synthesis identified a global theme of control, which was reflected across all eight organizing themes. Initially after surgery, many participants reported not being able to tolerate much food and experiencing unpredictable gastrointestinal side effects or a temporary ‘loss of body control’ when eating 19, 22, 23, 24, 51, 69, 70, 71, 72, 74. Some participants also noticed that their taste for certain foods changed 23, 53. It was a challenge to learn how their body now tolerated food, and it took time to figure this out:
‘You just have to find out how much you actually can eat and what you can tolerate….It has been some challenge navigating, such a labyrinth…’. [Female, Denmark] 72
The majority of participants in the studies lost a large amount of weight rapidly in the first 6 to 12 months after surgery. This time period was likened to a ‘honeymoon period’22 (p.197), with participants reporting they felt ‘excited’22 (p.160) and ‘invincible’53 during this time. However, a few participants worried that the weight loss was too quick or ‘progressive’ and were concerned that they could not ‘influence it’ 70. Surgery was described as providing ‘structure’ 44, or a physical control over eating, also described as ‘stomach control’ 67. This included reduced hunger, improved satiety and physical side effects (such as dumping syndrome) if they ate too much. They appreciated this ‘external control’ 23, as prior to surgery they had been unable to control food themselves:
‘Now I feel that the control is taken out of my hands. I didn't have that control over my body because my stomach controlled everything. If I eat too much I'm sick so I don't have the control anymore . . . that's a good thing because I couldn't control on my own’. [Female, UK] 23
This seemed to allow participants to feel more in control of other areas of their lives, which contributed to their overall happiness:
‘My self‐image is so different I project who I really am because I'm in control of my food and my exercise, control of my own schedule. […] I'm physically, emotionally and mentally in a better place’. [Participant, USA] 24
However, many participants reported that after the first post‐operative year, the ‘stomach control’ imposed by the surgery started to wear off, and they were gradually able to eat more as time went on, although not as much as pre‐operatively. This meant they had to rely more on their own ‘head control’67 to manage their eating, and sticking to a healthy diet became increasingly difficult. For some, this led to weight re‐gain, or the fear of re‐gaining weight and subsequently feeling less confident that they could control other areas of their lives:
‘I must admit that I'm quite scared, and often think, ‘What if my weight increases again?’ […] It's the worst case, like a nightmare. […] I've spoken to others who've told me that they've put on weight after two years. I get really anxious when they tell me this’. [Participant, Norway] 67
Nine studies described patients who had experienced some weight re‐gain after the initial good weight loss 19, 20, 22, 26, 28, 60, 68, 69, 71. This led to feelings of ‘shame’ and ‘failure’ 26, 60.
Participants who re‐gained weight described relapsing into emotional eating or using food to cope with stress:
‘[…] there was a lot of problems with my husband and my daughter who didn't get on and I was depressed over it […] and we had money problems and what have you and my way of coping was eating’. [Female, UK] 20
Many studies reported that participants started to come to the realization that the surgery was a ‘life change, not just a crutch’45 and that they had to focus on eating healthier lifelong:
‘Right after the surgery, there is this part of you that thinks, “I'm cured. I'm automatically going to lose weight.” But the surgery alone only works by itself for the first several months, maybe a year. But then you have to take over. You have to establish your new habits and your new patterns, and that can be rough because you are confronting a lot of issues that you never confronted before’. [Female, USA] 22 (p.207)
Normality
Throughout all aspects of their lives, normality was something that participants were striving for after having bariatric surgery. Participants described wanting lives that were less burdened by physical and psychological problems, a more normal or socially acceptable appearance, to be able to engage in normal everyday activities and have the same social and work opportunities and expectations for their lives that they felt others did. In some aspects of life, participants in the studies did indeed describe feeling more ‘normal’ after the surgery. For example, many reported experiencing less physical health problems and required less medications:
‘I have arthritis and used to take four different pills. Now I don't have to take any pills. I used to have high blood pressure as well and took an additional two pills for that. I had a tray filled with pills’. [Female, Norway] 66
A dramatic improvement in undertaking usual activities of daily living was reported for most participants in the studies. This included an improved ability to undertake domestic chores and carry out personal hygiene, and the ability to fit into seats in public settings:
‘You had to walk into a restaurant and ask for a chair rather than a booth. My most exciting thing is just sitting in a booth’. [Participant, USA] 24
The participants also reported improved work opportunities including an improved ability to carry out work tasks and better recognition and interactions with colleagues:
‘Suddenly where I work, at meetings and suchlike: […] What do you think about this …….. So they listen to me more. People ask me questions. They consult me. And I don't need to shout loud any more because I can talk and they hear me anyway. So…it's an…almost measurable difference…because the expectations to overweight people are rather low…. a bit hurtful. That's how I felt’. [Female, Norway] 54
Participants were pleased that they were now a more ‘average’ weight or looked more ‘normal’ 23, 65, 67, 73, 74. They appreciated the freedom to shop at a wider range of stores and increased clothing choices that they could use to draw attention to their new bodies:
‘I wear the clothes I like, for example, red, because it draws attention, why not? We lose that fear of going into a shop and receiving comments’. [Female, Brazil] 65
Some enjoyed the fact that they now blended in like ‘a normal person’ or were just ‘another face in the crowd’, as if they had never been obese ‘abnormal’ members of society 23, 24, 65, 69, 74.
However, in other aspects of their lives, participants' sense of normality was challenged. Many participants reported that initially their view of their body was not in sync with the reality of how much weight they had lost or with other people's views of their body:
‘It's how you look at yourself, you still think that you're big, and even if you hear many comments like oh, you are looking so good and so on, and of course it helps a great deal, but the image of myself when looking in the mirror is that my belly is still big and so, ah, I still think it's hard’. [Participant, Sweden] 60
Other changes after surgery that challenged their sense of normality included the development of unpleasant gastrointestinal symptoms (e.g. vomiting and diarrhoea), not being able to eat like others and the development of loose‐hanging excess skin:
‘Eating in public often now attracts attention. […] Now people comment on how little I am eating, and the time it takes me to eat’. [Female, New Zealand] 59
‘[…] I have to kind of get myself put back to what I consider to be normal. Normal is not too skinny and it's certainly not fat, but it's not the hanging skin either’. [Male, Canada] 73
Excess skin caused psychological problems for some who felt ‘depressed’ as a result of their ‘severe body hatred’ 27, 54, 56, 61, 65, 69, 73. Some felt that the excess skin was worse than being fat and sought plastic surgery to remove it as this was the only way they could finally look ‘normal’ 22, 24, 52, 54, 56, 61, 62, 65, 67, 69, 73, 74.
Ambivalence
A global theme of ambivalence was identified around the lived experience of bariatric surgery, which was evident throughout all the studies and organizing themes. This is reflected in the participants' co‐existing accounts of how some things in their lives changed for the better, and other changes were difficult to cope with or adapt to. Many of the studies reported that patients experienced an improvement in several aspects of their physical health, which included improved mobility, reduction in pain, improvement in bariatric‐related comorbidities such as diabetes, a reduction in medications needed and improved fertility 22, 23, 24, 44, 45, 46, 51, 52, 55, 59, 60, 61, 62, 66, 67, 68, 69, 70, 71, 72, 74. Conversely, surgery also led to some negative changes to physical health such as the development of nutritional deficiencies and unpleasant gastrointestinal symptoms:
‘…the women emphasized how their blood values and vitamin levels had changed dramatically after the surgery. […] they constantly struggled with iron deficiency, low haemoglobin percentage, and B12‐deficiency. While these levels were previously regarded as “normal” in terms of medical standards, they were far below the accepted level after the surgery’. [Authors' words] 26
Although most studies reported that, overall, participants' were ‘far healthier’ following surgery and could ‘deal’ with the new problems 24, some felt that their physical health was worse:
‘It feels like I have a rock in the machinery which makes me disabled in my daily life […] I am struggling with low blood pressure […] occasionally I see stars and nearly faint when I work’. [Female, Norway] 26
Similarly, psychological changes were reported as both positive and negative. Participants often reported improved depression, confidence, self‐esteem and a sense of control over their life 67. In contrast, some participants found problems with low self‐esteem and confidence continued to ‘drag on’ and recognized that these long‐standing problems were not ‘going to be cured in a day’22 (p.151). The psychological need to eat remained for some despite being physically unable to eat as much as before:
‘You're actually not hungry when you eat. Your brain keeps telling you that you are hungry. The stomach on the contrary is about to burst… This need, it's not just removed in surgery…There's such a psychological need all the time’. [Female, Denmark] 72
This meant they had to learn to deal differently with difficult emotions that previously they had used food to cope with:
‘I now have to deal with problems that I always fed with my addiction to food. Sometimes I don't really want to have to deal with these problems. It was much easier to just shove them to the side, pat them down, and cover them with food and move onto something else’. [Female, USA] 22 (p.162)
Some participants said that losing weight forced them to re‐discover who they were as a person, which could be a difficult process:
‘You have to be psychologically ready for this surgery because it forces you to look inside yourself, and that can be very hard’. [Female, USA] 22 (p.177)
For some, the weight had served as some ‘protection’ against the outside world22 (p.170), and they felt vulnerable and defenceless as they lost weight 27, 54, 56, 69, 74.
Social issues
After losing weight with surgery, many participants commented that they received more positive social feedback; people no longer ‘avoided’ them, and they felt more confident to engage in social activities22, 24, 66, 73:
‘I use to go to a party and find a chair and that's where I would stay the entire party. Now I go to a party and I go around visit with everybody and have a good old time. I was too embarrassed to even move around because I didn't want anyone to notice me’. [Participant, USA] 24
However, some felt resentment or ‘conflict’ about this improved attention as it made them realize just how badly they had been treated when they were obese:
‘You flip between thinking, “Well, I wasn't good enough for you before, so I don't want you around now,” to wanting to embrace the supposedly new you and the new reactions to you’. [Female, USA] 22 (p.87)
Some participants also received negative attention from others who thought they had taken the ‘easy way out’ by having surgery:
‘As the daughter of one of the participants commented, “It's not really an achievement the same as if it had been done normally. You've just had your insides cut up and it doesn't let you eat. Anyone could do it [lose weight].” ’ 49
The impact of the surgery on participants' romantic and sexual lives also demonstrated the ambivalence with which many participants regarded their experience of bariatric surgery. Some participants reported more romantic or sexual attention and had more opportunities for romantic relationships:
‘Men are starting to look at me differently which is kind of fun and I'm going out with a nice guy from school who really treats me like a lady’. [Female, USA] 52
Some found the new romantic attention ‘scary’ and described how they did not have the experience or knowledge to deal with this kind of attention 22, 24, 46, 52. These new social possibilities required the development of new social skills that they had not previously had to use:
‘I was 225 pounds in the eighth grade when girls are experimenting with boys. I was never involved in conversations about boys because I was not having those experiences. So basically, as an adult after the weight loss, when relationships were a possibility, I thought about them the way a thirteen year old would. Physically and professionally, I was in my thirties, but emotionally I was a teenager when it came to relational issues’. [Female, USA] 22 (p.75)
Discussion
Bariatric surgery is the most clinically effective treatment for severe and complex obesity, in terms of both weight loss and the improvement of weight‐related comorbidities. However, it leads to impacts on several other areas of patients' lives, which are important to consider. This systematic review of qualitative research studies synthesized what is currently known about the patient perspective of living with the outcomes of bariatric surgery. The synthesis demonstrated that bariatric surgery led to a number of changes to the lives of participants, including their weight, activities of daily living, physical health, psychological health, social relations, sexual life, body image and eating behaviour and relationship with food. Three global themes (control, normality and ambivalence) were identified, which describe the lived experience of bariatric surgery throughout all these areas of participants' lives. Participants were striving for control of their food, weight and health, as well as developing a new identity as a ‘normal’ or socially acceptable person. Although many of the changes after surgery were reported as being positive and led to participants feeling more normal and in control of their lives, some problems were also experienced. Other changes were seen as neither positive nor negative but were challenging and required adaptation, which contributed to the overall ambivalent nature of many accounts of life after bariatric surgery. These data are important because patients deciding to undergo surgery need to be aware of both the positive and challenging nature of changes reported and need to be supported appropriately in the long term.
Many of the findings from this qualitative synthesis relate to the psychosocial issues faced by patients after undergoing bariatric surgery and have not been identified in the quantitative literature describing outcomes of bariatric surgery. Thus, this synthesis provides important new insights around patients' experiences of bariatric surgery as a whole. In particular, it demonstrates that the effect of bariatric surgery on psychosocial outcomes is far from straightforward. Living with the changes caused by bariatric surgery is complicated, unstable and requires ongoing negotiation. Participants in the included studies initially felt more in control of weight and eating, but this sense of control diminished as time progressed. It is well known that some patients will re‐gain a certain amount of weight between 1 and 10 years post‐surgery 15. The findings of this qualitative synthesis highlight that weight re‐gain can be associated with a feeling of loss of control and a negative psychological experience for patients.
The findings from our synthesis help to provide explanatory background to previous studies evaluating the impact of bariatric surgery on HRQL, which is often reported poorly 12, 75. Where impact on HRQL has been reported, there is significant variation in results, with improvements in some (e.g. physical functioning) but not all (e.g. social and emotional functioning) areas 12, 76, 77, 78. This synthesis has highlighted that although patients in the included studies reported some positive psychological changes such as reduced depression and improved self‐confidence, they also experienced difficulties creating a new identity and developing new coping strategies that did not involve food. Meana and Ricciardi termed these ‘tension‐generating changes’; changes that were neither clearly positive nor negative but required a process of adaptation 21, 22 (p.209). A recent study by Wood and Ogden interviewed people who underwent bariatric surgery more than 8 years ago 79. Those who had maintained good weight loss had been more able to ‘functionalize’ food (e.g. ‘eat to live’ rather than ‘live to eat’ 23, 24) and develop new coping strategies and a more positive self‐image 79.
This synthesis also highlighted that patients who underwent bariatric surgery alternated between feeling they were a more ‘normal’, socially acceptable person and less ‘normal’ because of the development of loose‐hanging excess skin, which impacted on their body image and relationships with others. Some participants said they desired plastic surgery as a way to finally achieve normality. Ogden et al. recently published a study on patients' experiences of plastic surgery to remove excess skin following bariatric surgery 80. They reported that after undergoing both bariatric and plastic surgery, participants' came to the realization that their psychological issues remained untreated and that their physical shape may not have been the key factor contributing to their negative self‐image 80. In this review, it was shown that people who had undergone bariatric surgery may also be presented with a new range of social opportunities, some of which can be frightening (e.g. romantic prospects) as they may be outside the scope of their previous experience. These findings highlight the importance of concurrent psychological support alongside surgery.
Clinical implications and future research
This synthesis emphasizes the need for health professionals to help patients manage the changes and challenges resulting from bariatric surgery. Patients need ongoing support in relation to their sense of control and normality and to help them navigate tensions inherent within the outcomes experienced. The widespread and complex nature of the changes experienced by the participants in the included studies, even several years after bariatric surgery, reinforces the view that obesity is a chronic disease that can be treated but never totally ‘cured’ 81. Therefore, patients require access to life‐long support to manage their obesity and maximize the benefit of their treatments. In particular, it is important for bariatric surgery services to ensure access to long‐term dietary and psychological support to help patients navigate the challenging aspects of life post‐surgery, for example, coping with a return of hunger feelings and control of eating, weight re‐gain and changes to personal identity and body image. Health professionals need to help patients to recognize when a small amount of weight re‐gain is normal, vs. when it is more problematic, and provide additional support in these instances.
Most health professionals working with patients who have undergone bariatric surgery recognize that good follow‐up care is essential in achieving a successful outcome 82, 83, 84. Despite this, follow‐up care after bariatric surgery varies greatly 85, 86, 87. Guidance relating to the long‐term follow‐up care of bariatric surgery patients mainly focuses on the monitoring and treatment of physical symptoms, comorbidities and nutritional deficiencies, with little guidance on how to help patients cope with weight re‐gain, continued control of eating and other psychological issues following surgery 13, 84, 88. There is a need for further research to develop and assess interventions to support patients with long‐term weight maintenance and to cope with the profound changes to their lives after this surgery, particularly to their eating habits and psychological health. The findings of this synthesis are useful for health professionals and policy makers working in bariatric surgery services to inform the future development of these services to be more in line with patient needs. Improved follow‐up care services may lead to better outcomes of bariatric surgery, which would mean cost savings to health care in managing obesity‐related health problems.
Strengths and limitations of this synthesis
This qualitative synthesis is, to the authors' knowledge, the first attempt to synthesize the wealth of qualitative literature that exists in the field of bariatric surgery. There is an increasing recognition that qualitative research studies need to be synthesized to inform policy and practice as is often performed for quantitative studies 40. As a large number of studies conducted in different countries were identified and synthesized, this synthesis will help future qualitative researchers focus their research questions on areas less well explored and will also help to provide recommendations for future clinical practice. A limitation of this review is that a single reviewer initially screened records, rather than two reviewers, which could have led to the possible exclusion of relevant articles. However, any queries on inclusion or exclusion were discussed with a second reviewer who also cross‐checked that all full‐text articles selected for inclusion met the inclusion criteria. The rigour of the synthesis was enhanced by a second reviewer completing independent dual data extraction on a sample of included studies. Preliminary thematic networks were also discussed between three of the authors to discuss and agree the emergence of themes. A limitation of this synthesis is that we included only published data and did not include unpublished data or ‘grey literature’.
Conclusion
This systematic review and thematic synthesis has highlighted the profound long‐term impact that bariatric surgery has on many different aspects of people's lives and the challenges they experience in coming to terms with these changes. The overarching themes of control, normality and ambivalence characterized the complexity of changes experienced. Participants came to the realization that to achieve and maintain positive outcomes from the surgery, they had to sustain life‐long changes to their eating habits, which were much more difficult than anticipated. Surgery was not the end of their journey with obesity but rather the beginning of a new and sometimes challenging path. These findings contribute to the knowledge base about the long‐term outcomes of obesity surgery and demonstrate the importance of ongoing support to help people negotiate these challenges and maintain the positive changes achieved.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supporting information
Supporting Information: Search strategies for systematic review and synthesis of qualitative studies.
Table S1: Organising themes and their associated basic themes in thematic synthesis.
Acknowledgements
This article summarizes independent research funded by a National Institute for Health Research (NIHR) Doctoral Research Fellowship (K. D. Coulman). This work was also supported by the Medical Research Council (MRC) ConDuCT‐II Hub (Collaboration and innovation for Difficult and Complex randomised controlled Trials In Invasive procedures ‐ MR/K025643/1). The views and opinions expressed in this publication are those of the authors and do not necessarily reflect those of the National Health Service, the NIHR' the Department of Health, or the MRC.
Coulman, K. D. , MacKichan, F. , Blazeby, J. M. , and Owen‐Smith, A. (2017) Patient experiences of outcomes of bariatric surgery: a systematic review and qualitative synthesis. Obesity Reviews, 18: 547–559. doi: 10.1111/obr.12518.
References
- 1. World Health Organisation . Obesity and overweight. 2015. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/.
- 2. Health and Social Care Information Centre . Health Survey for England – 2014, chapter 9: Adult obesity and overweight; 2015. [Google Scholar]
- 3. Lim SS, Vos T, Flaxman AD et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA 1999; 282: 1523–1529. [DOI] [PubMed] [Google Scholar]
- 5. Kopelman P. Health risks associated with overweight and obesity. Obes Rev 2007; 8: 13–17. [DOI] [PubMed] [Google Scholar]
- 6. Sarwer DB, Steffen KJ. Quality of life, body image and sexual functioning in bariatric surgery patients. Eur Eat Disord Rev 2015; 23: 504–508. [DOI] [PubMed] [Google Scholar]
- 7. Warkentin LM, Majumdar SR, Johnson JA et al. Predictors of health‐related quality of life in 500 severely obese patients. Obesity 2014; 22: 1367–1372. [DOI] [PubMed] [Google Scholar]
- 8. Fontaine KR, Barofsky I. Obesity and health‐related quality of life. Obes Rev 2001; 2: 173–182. [DOI] [PubMed] [Google Scholar]
- 9. Kolotkin RL, Meter K, Williams GR. Quality of life and obesity. Obes Rev 2001; 2: 219–229. [DOI] [PubMed] [Google Scholar]
- 10. Luppino FS, de Wit LM, Bouvy PF et al. Overweight, obesity, and depression: a systematic review and meta‐analysis of longitudinal studies. Arch Gen Psychiatry 2010; 67: 220–229. [DOI] [PubMed] [Google Scholar]
- 11. Dietz WH, Baur LA, Hall K et al. Management of obesity: improvement of health‐care training and systems for prevention and care. Lancet 2015; 385: 2521–2533. [DOI] [PubMed] [Google Scholar]
- 12. Colquitt JL, Pickett K, Loveman E, Frampton Geoff K. Surgery for weight loss in adults. Cochrane Database Syst Rev 2014; CD003641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. National Institute for Health and Care Excellence . Obesity: identification, assessment and management of overweight and obesity in children, young people and adults. London, 2014. [PubMed]
- 14. O'Brien PE, MacDonald L, Anderson M, Brennan L, Brown WA. Long‐term outcomes after bariatric surgery: fifteen‐year follow‐up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg 2013; 257: 87–94. [DOI] [PubMed] [Google Scholar]
- 15. Sjostrom L. Review of the key results from the Swedish Obese Subjects (SOS) trial – a prospective controlled intervention study of bariatric surgery. J Intern Med 2013; 273: 219–234. [DOI] [PubMed] [Google Scholar]
- 16. Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ, Colditz GA. The effectiveness and risks of bariatric surgery: an updated systematic review and meta‐analysis, 2003–2012. JAMA Surg 2014; 149: 275–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gloy VL, Briel M, Bhatt DL et al. Bariatric surgery versus non‐surgical treatment for obesity: a systematic review and meta‐analysis of randomised controlled trials. BMJ 2013; 347: f5934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mann J, Jakes A, Hayden J, Barth J. Systematic review of qualitative and quantitative definitions of failure in revisional bariatric surgery. British Obesity and Metabolic Surgery Society 6th Annual Scientific Meeting. Newcastle‐upon‐Tyne, UK; 2015.
- 19. Zijlstra H, Boeije HR, Larsen JK, van Ramshorst B, Geenen R. Patients' explanations for unsuccessful weight loss after laparoscopic adjustable gastric banding (LAGB). Patient Educ Couns 2009; 75: 108–113. [DOI] [PubMed] [Google Scholar]
- 20. Ogden J, Avenell S, Ellis G. Negotiating control: patients' experiences of unsuccessful weight‐loss surgery. Psychol Health 2011; 26: 949–964. [DOI] [PubMed] [Google Scholar]
- 21. Bocchieri LE, Meana M, Fisher BL. Perceived psychosocial outcomes of gastric bypass surgery: a qualitative study. Obes Surg 2002; 12: 781–788. [DOI] [PubMed] [Google Scholar]
- 22. Meana M, Ricciardi L. Obesity Surgery: Stories of Altered Lives. University of Nevada Press: Reno, Nevada, 2008. [Google Scholar]
- 23. Ogden J, Clementi C, Aylwin S. The impact of obesity surgery and the paradox of control: a qualitative study. Psychol Health 2006; 21: 273–293. [DOI] [PubMed] [Google Scholar]
- 24. Stolzenberger KM, Meaney CA, Marteka P, Korpak S, Morello K. Long‐term quality of life following bariatric surgery: a descriptive study. Bariatr Surg Pract Patient Care 2013; 8: 29–38. [Google Scholar]
- 25. Pope C, Mays N. Chapter 1 ‐ Qualitative methods in health research In: Pope C, Mays N. (eds). Qualitative Research in Health Care, 3rd edn. Blackwell Publishing Ltd: Malden, Massachusetts, 2006, pp. 1–11. [Google Scholar]
- 26. Groven KS, Raheim M, Engelsrud G. “My quality of life is worse compared to my earlier life”: living with chronic problems after weight loss surgery. Int J Qual Stud Health Well‐being 2010; 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gilmartin J. Body image concerns amongst massive weight loss patients. J Clin Nurs 2013; 22: 1299–1309. [DOI] [PubMed] [Google Scholar]
- 28. Benson‐Davies S, Davies ML, Kattelmann K. Understanding eating and exercise behaviors in post Roux‐en‐Y gastric bypass patients: a quantitative and qualitative study. Bariatr Surg Pract Patient Care 2013; 8: 61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Campbell R, Pound P, Morgan M et al. Health Technol Assess 2011; 15. [DOI] [PubMed] [Google Scholar]
- 30. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008; 8: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sandelowski M, Docherty S, Emden C. Qualitative metasynthesis: issues and techniques. Res Nurs Health 1997; 20: 365–371. [DOI] [PubMed] [Google Scholar]
- 32. Lachal J, Orri M, Speranza M et al. Qualitative studies among obese children and adolescents: a systematic review of the literature. Obes Rev 2013; 14: 351–368. [DOI] [PubMed] [Google Scholar]
- 33. Clarke J, Fletcher B, Lancashire E, Pallan M, Adab P. The views of stakeholders on the role of the primary school in preventing childhood obesity: a qualitative systematic review. Obes Rev 2013; 14: 975–988. [DOI] [PubMed] [Google Scholar]
- 34. Pocock M, Trivedi D, Wills W, Bunn F, Magnusson J. Parental perceptions regarding healthy behaviours for preventing overweight and obesity in young children: a systematic review of qualitative studies. Obes Rev 2010; 11: 338–353. [DOI] [PubMed] [Google Scholar]
- 35. Noyes J, Popay J, Pearson A, Hannes K, Booth A. Chapter 20: Qualitative research and cochrane reviews In: Higgins J, Green S. (eds). Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org [Google Scholar]
- 36. Coulman KD, Howes N, Hopkins J et al. A comparison of health professionals' and patients' views of the importance of outcomes of bariatric surgery. Obes Surg 2016; 26: 2738–2746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Endnote X7. New York, NY: Thomson Reuters; 2015.
- 38. Carroll C, Booth A, Lloyd‐Jones M. Should we exclude inadequately reported studies from qualitative systematic reviews? An evaluation of sensitivity analyses in two case study reviews. Qual Health Res 2012; 22: 1425–1434. [DOI] [PubMed] [Google Scholar]
- 39. Barbour RS. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog? BMJ 2001; 322: 1115–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Noblit GW, Hare RD. Meta‐Ethnography: Synthesizing Qualitative Studies. Sage Publications, Inc.: Newbury Park, 1988. [Google Scholar]
- 41. Malpass A, Shaw A, Sharp D et al. "Medication career" or "moral career"? The two sides of managing antidepressants: a meta‐ethnography of patients' experience of antidepressants. Soc Sci Med 2009; 68: 154–168. [DOI] [PubMed] [Google Scholar]
- 42. Attride‐Stirling J. Thematic networks: an analytic tool for qualitative research. Qual Res 2001; 1: 385–405. [Google Scholar]
- 43. Ogden J, Clementi C, Aylwin S, Patel A. Exploring the impact of obesity surgery on patients' health status: a quantitative and qualitative study. Obes Surg 2005; 15: 266–272. [DOI] [PubMed] [Google Scholar]
- 44. Wysoker A. The lived experience of choosing bariatric surgery to lose weight. J Am Psychiatr Nurses Assoc 2005; 11: 26–34. [Google Scholar]
- 45. Earvolino‐Ramirez M. Living with bariatric surgery: totally different but still evolving. Bariatr Surg Pract Patient Care 2008; 3: 17–24. [Google Scholar]
- 46. Pastoriza CA, Guimarães SM. Positives changes in the quotidian of patients submitted to the stomach reduction surgery (bariatric) [Portuguese]. Enfermagem Atual 2008; 8: 18–24. [Google Scholar]
- 47. Throsby K. ‘There's something in my brain that doesn't work properly’: weight loss surgery and the medicalisation of obesity In: Malson H, Burns M. (eds). Critical Feminist Approaches to Eating Dis/orders. Routledge: London; New York, 2009, pp. 185–195. [Google Scholar]
- 48. Throsby K. The war on obesity as a moral project: weight loss drugs, obesity surgery and negotiating failure. Sci Cult 2009; 18: 201–216. [Google Scholar]
- 49. Throsby K. ‘That's a bit drastic’: risk and blame in accounts of obesity surgery In: Alexander F, Throsby K. (eds). Gender and Interpersonal Violence. Palgrave Macmillan: Basingstoke; New York, 2008, pp. 83–99. [Google Scholar]
- 50. Throsby K. Happy re‐birthday: weight loss surgery and the 'new me'. Body Soc 2008; 14: 117‐+. [Google Scholar]
- 51. Agra G, Henriques MER. The women's existence that they underwent the gastroplasty [Portuguese]. Rev Eletr Enf 2009; 11: 982–992. [Google Scholar]
- 52. Norris J. Case study. Struggling for normalcy. Bariatr Surg Pract Patient Care 2009; 4: 95–101. [Google Scholar]
- 53. Sutton DH, Murphy N, Raines DA. Transformation: the "life‐changing" experience of women who undergo a surgical weight loss intervention. Bariatr Surg Pract Patient Care 2009; 4: 299–306. [Google Scholar]
- 54. Groven KS, Raheim M, Engelsrud G. Dis‐appearance and dys‐appearance anew: living with excess skin and intestinal changes following weight loss surgery. Med Health Care Philos 2012. [DOI] [PubMed] [Google Scholar]
- 55. LePage CT. The lived experience of individuals following Roux‐en‐Y gastric bypass surgery: a phenomenological study. Bariatr Surg Pract Patient Care 2010; 5: 57–64. [Google Scholar]
- 56. Magdaleno R, Chaim EA, Pareja JC, Turato ER. The psychology of bariatric patient: what replaces obesity? A qualitative research with Brazilian women. Obes Surg 2011; 21: 336–339. [DOI] [PubMed] [Google Scholar]
- 57. Magdaleno R, Chaim EA, Turato ER. Surgical treatment of obesity: some considerations on the transformations of the eating impulse. Rev Latinoam Psicopat Fund, São Paulo 2010; 13: 425–440. [Google Scholar]
- 58. Magdaleno R, Chaim EA, Turato ER. Understanding the life experiences of Brazilian women after bariatric surgery: a qualitative study. Obes Surg 2010; 20: 1086–1089. [DOI] [PubMed] [Google Scholar]
- 59. Wilson LH. Occupational consequences of weight loss surgery: a personal reflection. J Occup Sci 2010; 17: 47–54. [Google Scholar]
- 60. Engstrom M, Forsberg A. Wishing for deburdening through a sustainable control after bariatric surgery. Int J Qual Stud Health Well‐being 2011; 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Marcelino LF, Patricio ZM. The complexity of obesity and life after bariatric surgery: a public health issue. [Portuguese]. Cien Saude Colet 2011; 16: 4767–4776. [DOI] [PubMed] [Google Scholar]
- 62. Throsby K. Obesity surgery and the management of excess: exploring the body multiple. Sociol Health Illn 2012; 34: 1–15. [DOI] [PubMed] [Google Scholar]
- 63. Ivezaj V, Saules KK, Wiedemann AA. "I didn't see this coming.": why are postbariatric patients in substance abuse treatment? Patients' perceptions of etiology and future recommendations. Obes Surg 2012; 22: 1308–1314. [DOI] [PubMed] [Google Scholar]
- 64. Zunker C, Karr T, Saunders R, Mitchell JE. Eating behaviors post‐bariatric surgery: a qualitative study of grazing. Obes Surg 2012; 22: 1225–1231. [DOI] [PubMed] [Google Scholar]
- 65. Castro M, Ferreira V, Chinelato R, Ferreira M. Body image in women undergone bariatric surgery: sociocultural interactions. [Portuguese]. Motricidade 2013; 9: 82–95. [Google Scholar]
- 66. Gronning I, Scambler G, Tjora A. From fatness to badness: the modern morality of obesity. Health (London) 2013; 17: 266–283. [DOI] [PubMed] [Google Scholar]
- 67. Knutsen IR, Terragni L, Foss C. Empowerment and bariatric surgery: negotiations of credibility and control. Qual Health Res 2013; 23: 66–77. [DOI] [PubMed] [Google Scholar]
- 68. Mariano ML, Monteiro CS, de Paula MA. Bariatric surgery: its effects for obese in the workplace. [Portuguese]. Rev Gaucha Enferm 2013; 34: 38–45. [DOI] [PubMed] [Google Scholar]
- 69. Natvik E, Gjengedal E, Raheim M. Totally changed, yet still the same: patients' lived experiences 5 years beyond bariatric surgery. Qual Health Res 2013; 23: 1202–1214. [DOI] [PubMed] [Google Scholar]
- 70. Forsberg A, Engström Å, Söderberg S. From reaching the end of the road to a new lighter life – people's experiences of undergoing gastric bypass surgery. Intensive Crit Care Nurs 2014; 30: 93–100. [DOI] [PubMed] [Google Scholar]
- 71. Geraci AA, Brunt A, Marihart C. The work behind weight‐loss surgery: a qualitative analysis of food intake after the first two years post‐op. ISRN Obes 2014; 2014: 427062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Jensen JF, Petersen MH, Larsen TB, Jorgensen DG, Gronbaek HN, Midtgaard J. Young adult women's experiences of body image after bariatric surgery: a descriptive phenomenological study. J Adv Nurs 2014; 70: 1138–1149. [DOI] [PubMed] [Google Scholar]
- 73. Lyons K, Meisner BA, Sockalingam S, Cassin SE. Body image after bariatric surgery: a qualitative study. Bariatr Surg Pract Patient Care 2014; 9: 41–49. [Google Scholar]
- 74. Warholm C, Øien AM, Raheim M. The ambivalence of losing weight after bariatric surgery. Int J Qual Stud Health Well‐being 2014; 9: 22876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Coulman KD, Abdelrahman T, Owen‐Smith A, Andrews RC, Welbourn R, Blazeby JM. Patient‐reported outcomes in bariatric surgery: a systematic review of standards of reporting. Obes Rev 2013; 14: 707–720. [DOI] [PubMed] [Google Scholar]
- 76. Dixon JB, Schachter LM, O'Brien PE et al. Surgical vs conventional therapy for weight loss treatment of obstructive sleep apnea: a randomized controlled trial. JAMA 2012; 308: 1142–1149. [DOI] [PubMed] [Google Scholar]
- 77. O'Brien PE, Dixon JB, Laurie C et al. Treatment of mild to moderate obesity with laparoscopic adjustable gastric banding or an intensive medical program: a randomized trial. Ann Intern Med 2006; 144: 625–633. [DOI] [PubMed] [Google Scholar]
- 78. Lindekilde N, Gladstone BP, Lubeck M et al. The impact of bariatric surgery on quality of life: a systematic review and meta‐analysis. Obes Rev 2015. [DOI] [PubMed] [Google Scholar]
- 79. Wood KV, Ogden J. Patients' long‐term experiences following obesity surgery with a focus on eating behaviour: a qualitative study. J Health Psychol 2016; 21: 2447–2456. [DOI] [PubMed] [Google Scholar]
- 80. Ogden J, Birch A, Wood K. ‘The wrong journey’: patients' experience of plastic surgery post weight loss surgery. Qual Res Sport, Exerc Health 2015; 7: 294–308. [Google Scholar]
- 81. Rippe JM, Crossley S, Ringer R. Obesity as a chronic disease: modern medical and lifestyle management. J Am Diet Assoc 1998; 98: S9–15. [DOI] [PubMed] [Google Scholar]
- 82. Myers VH, Adams CE, Barbera BL, Brantley PJ. Medical and psychosocial outcomes of laparoscopic Roux‐en‐Y gastric bypass: cross‐sectional findings at 4‐year follow‐up. Obes Surg 2012; 22: 230–239. [DOI] [PubMed] [Google Scholar]
- 83. Heber D, Greenway FL, Kaplan LM, Livingston E, Salvador J, Still C. Endocrine and nutritional management of the post‐bariatric surgery patient: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2010; 95: 4823–4843. [DOI] [PubMed] [Google Scholar]
- 84. Mechanick JI, Youdim A, Jones DB et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis 2013; 9: 159–191. [DOI] [PubMed] [Google Scholar]
- 85. National Confidential Enquiry into Patient Outcome and Death . Too lean a service? A review of the care of patients who underwent bariatric surgery. 2012.
- 86. Gesquiere I, Augustijns P, Lannoo M, Matthys C, Van der Schueren B, Foulon V. Barriers in the approach of obese patients undergoing bariatric surgery in Flemish hospitals. Obes Surg 2015; 25: 2153–2158. [DOI] [PubMed] [Google Scholar]
- 87. Reames BN, Birkmeyer NJ, Dimick JB et al. Variation in the Care of Surgical Conditions: Obesity, A Dartmouth Atlas of Health Care Series Lebanon, NH: The Dartmouth Institute for Health Policy & Clinical Practice, 2014. [PubMed] [Google Scholar]
- 88. Parretti HM, Hughes CA, O'Kane M, Woodcock S, Pryke RG. Ten Top Tips for the management of patients post‐bariatric surgery in primary care. Br J Obes 2015; 1: 68–73. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information: Search strategies for systematic review and synthesis of qualitative studies.
Table S1: Organising themes and their associated basic themes in thematic synthesis.


