Abstract
The number of elderly patients with an aneurysmal subarachnoid hemorrhage (aSAH) has been increasing in aging- or aged societies in many countries. A treatment strategy for the elderly with aSAH has not been established, although many studies have been published emphasizing poor outcome for aSAH. The aim of this study was to analyze the factors and treatments affecting outcome in aSAH in the elderly in a systematic review of the literature by investigating patients over age 75. A literature search was done for “elderly aSAH” in PubMed and Embase. Literature with a clear description of treatment measures for aneurysmal occlusion and outcome was selected. Twelve studies, consisted of 816 cases, met the eligibility criteria. Patient characteristics included 83.2% female, 33.8% poor clinical grade on admission, 57.1% Fischer group 3, and 41% internal carotid artery aneurysm. As complications, symptomatic vasospasm was seen in 25.5% of patients, hydrocephalus in 31.1%, and medical complication in 38.4%. Favorable outcome was 35.0% in total, 45.3% for clipping, 36.3% for coiling, and 9.0% for conservative treatment. Several studies by multivariate analysis indicated that poor clinical grade on admission could be a risk factor for neurological outcome and mortality. Advanced age and selection of conservative treatment without aneurysmal occlusion could be a risk factor for mortality. Patients under age 85 with good clinical grade on admission can be candidates for treatment of aneurysm repair. However, treatment for patients over age 85 or with poor clinical grade should be carefully determined.
Keywords: subarachnoid hemorrhage, cerebral aneurysm, elderly
Introduction
An aging- or aged society is and has been a reality in many developed countries. This is expected to change the epidemiological aspect of many diseases, including their incidences. The incidence of aneurysmal subarachnoid hemorrhage (aSAH) is known to rise with age, especially in women.1) Both the number of elderly patients with aSAH and the total incidence have therefore been estimated to be increasing.2,3) In addition to the characteristics of elderly aSAH, such as a high rate of poor clinical grade on admission, severe aSAH on initial computed tomography (CT) scan, and general complications, the most serious problem is a high rate of poor outcome.4–7) In particular, several studies indicat that poor outcome significantly increases in the patients over age 75.8–10)
In order to improve outcome in elderly aSAH, the risk factors for poor outcome, the indication for aneurysm repair, and the selection of clipping or coiling should be discussed and determined. However, most of the studies performed until now have been retrospective analyses based on cases treated at a single institution, and a definite conclusion could not be reached. The aim of this study was to analyze the factors and treatments affecting outcome in elderly aSAH by a systematic review of the literature, investigating patients over age 75.
Methods
A search was designed to identify relevant articles on aSAH in the elderly. A comprehensive review of the literature was done in a search of PubMed and Embase by using the keywords “subarachnoid hemorrhage,” “cerebral aneurysm,” “elderly,” “aged,” and “old” in both “AND” and “OR” combinations. Inclusion criteria were the following: studies in English with more than 10 patients, studies published up to December 2016, with clear descriptions of treatment measures for aneurysmal occlusion and outcome. If data for cases aged 75 years or older could not be evaluated, the article was excluded from the analysis. The other exclusion criteria were the following: studies including non-aneurysmal SAH, case reports, conference abstracts, review articles, and guidelines.
Two investigators (MN and NS) independently selected potentially acceptable literature according to the above inclusion criteria. The initial selection was based on an examination of the title and a review of the abstract, and in a next selection the investigators reviewed the full text. After a discussion among the investigators, including the senior investigator (HO), a consensus was reached on which studies to include. For multiple publications from the same institution and/or the same authors, the most relevant article was elected in order to avoid inclusion of overlapping patients.
For each study, the following clinical information was extracted: age, gender, clinical grade on admission, degree of aSAH on initial CT scan, location of ruptured cerebral aneurysms, symptomatic cerebral vasospasm, hydrocephalus, medical complication, aneurysmal occlusion, and clinical outcome. Clinical grade on admission was divided into poor grade, which was grade 4 or 5 on the Hunt & Hess classification, the Hunt & Kosnik classification, and/or the WFNS classification, and good grade, which was grades 1, 2, or 3 in the same classifications. Clinical outcome was divided into favorable outcome, which was 0–2 on the modified Rankin Scale (mRS) or good recovery (GR) or moderate disability (MD) on the Glasgow Outcome Scale score (GOS), and poor outcome, which was 3–6 on mRS or severe disability (SD), vegetative state (VS), or death (D) on GOS. The degree of aSAH on the initial CT scan was expressed using Fisher’s original classification. The location of a ruptured cerebral aneurysm was divided into the internal carotid artery (ICA), anterior cerebral artery (ACA), middle cerebral artery (MCA), and vertebrobasilar artery (VBA), and the ACA including the anterior communicating artery.
Results
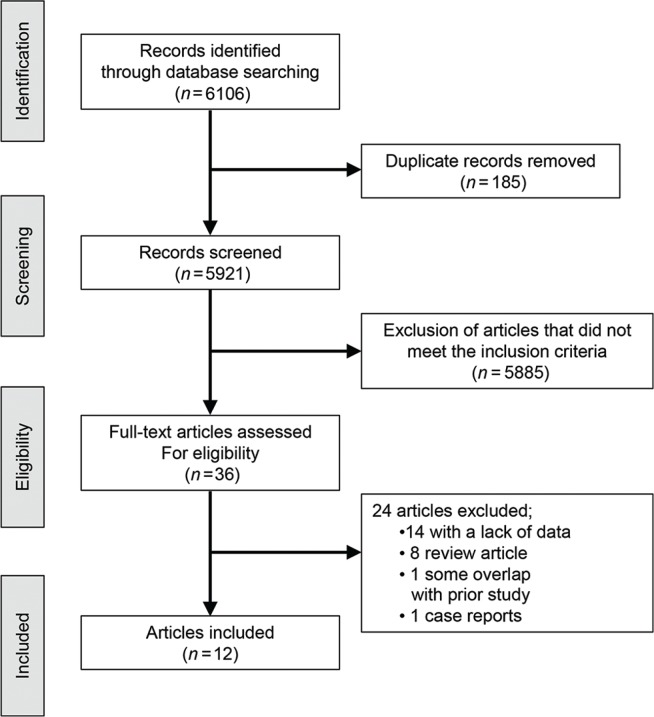
PubMed yielded 5,903 studies, Embase 203. After excluding duplicate studies by reviewing the title and removing studies that failed to meet the inclusion criteria after screening the abstracts, the full text of 36 articles was assessed. One article was excluded because of double publications from the same institution and the same authors. Of two articles by Horiuchi et al., the latest one with more cases was excluded, because it investigated cases 80 years of age or older, while the older one investigated cases 75 years of age or older.11,12) Two articles by Hamada et al. had no overlap of cases, and both articles were included.13,14) Two articles by Asano et al. were from different institutions and had no overlap of cases; both were therefore included.15,16) A flowchart of the literature search for eligible articles is shown in Fig. 1, and 12 studies were finally eligible for the present study.4,5,11,13–21)
Fig. 1.
Flowchart of the literature search procedure.
Consequently, a systematic review was performed using 12 studies, of which four investigated patients over age 75, and eight studies investigated patients over 80 years of age (Table 1). A comparative investigation with other time-spans under age 75 was performed in three studies,5,17,18) and a comparative investigation between several time-spans of 75 or 80 years of age or older was performed in three studies.4,11,17) One article investigated mainly a comparison among different time spans, while the data for the patients over 75 years of age included outcome only.17) Of 12 articles, eight studies were performed in Japan, and the other four studies were performed in several developed countries. Seven studies were published within the last six years. All of the studies were retrospective in design.
Table 1.
Summary of the literatures
| Study | Country | Setting | Years of study | Eligible age | Range of analyzed age (Mean years) | Number of cases |
|---|---|---|---|---|---|---|
| Hamada et al., 199913) | Japan | Single center | 1992–1997 | 80 ≤ | 80–83 (81) | 10 |
| Hamada et al., 200114) | Japan | Single center | 1995–1998 | 80 ≤ | 80–89 (84) | 29 |
| Mont’alverne et al., 200517) | France | Single center | 1993–2003 | 75 ≤ | – | 14 |
| Nieuwkamp et al., 20064) | Netherlands | Single center | 1990–2004 | 75 ≤ | – | 170 |
| Asano et al., 200715) | Japan | Single center | 2000–2005 | 80 ≤ | 80–92 (84) | 24 |
| Horiuchi et al., 201111) | Japan | Multi center | 1988–2009 | 75 ≤ | 75–93 (79.5) | 333 |
| Asano et al., 201116) | Japan | Single center | 1998–2009 | 80 ≤ | 80–90 (84) | 28 |
| Scholler et al., 20135) | Germany | Single center | 1996–2007 | 80 ≤ | 80–97 | 25 |
| Hishikawa et al., 201418) | Japan | Single center | 2003–2012 | 80 ≤ | 82–84 (83) | 12 |
| Sadamasa et al., 201419) | Japan | Single center | 2005–2011 | 80 ≤ | 80–98 | 69 |
| Wilson et al., 201420) | USA | Single center | 2005–2012 | 80 ≤ | – | 16 |
| Shimamura et al., 201621) | Japan | Single center | 2005–2013 | 75 ≤ | 75–90 (79) | 86 |
| Total | 816 |
For patient characteristics, females dominated at 83.2% (Table 2). For clinical grade on admission, patients with a good grade consisting of 1–3 on the WFNS classification, the Hunt & Hess classification, or the Hunt & Kosnik classification amounted to 520 cases (66.2%), and 266 patients (33.8%) had a poor condition consisting of 4 or 5 on the same classifications. However, one of the studies by Hamada et al. investigated cases with grade 1 or 2 on the Hunt & Hess classification,13) and the other study by Hamada et al. investigated cases with grade 3 on the Hunt & Hess classification,14) which suggested these two studies contained case selection bias. Excluding these studies therefore rendered the number of cases with a good grade at 481 (64.4%), and cases with a poor grade were 266 (35.6%). Group 3 of Fisher’s classification amounted to 281 (57.1%), and group 4 was 109 (22.2%). The ICA was dominant (41.0%) as the site of ruptured aneurysm compared to other sites.
Table 2.
Characteristics
| Study | Gender | Clinical grade on admission | Fisher group | Site of aneurysm | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Good-grade | Poor-grade | 1 | 2 | 3 | 4 | ICA | ACA | MCA | VBA | |
| Hamada et al., 199913) | 0 | 10 | 10 | 0 | 0 | 5 | 5 | 0 | 4 | 3 | 3 | 0 |
| Hamada et al., 200114) | 4 | 25 | 29 | 0 | 0 | 1 | 21 | 7 | 10 | 6 | 13 | 0 |
| Mont’alverne et al., 200517) | – | – | – | – | – | – | – | – | – | – | – | – |
| Nieuwkamp et al., 20064) | 31 | 139 | 110 | 60 | – | – | – | 36 | 42 | 16 | 14 | |
| Asano et al., 200715) | 4 | 20 | 10 | 14 | – | – | – | 3 | 5 | 3 | 4 | |
| Horiuchi et al., 201111) | 59 | 274 | 217 | 116 | 14 | 56 | 182 | 81 | 130 | 93 | 89 | 21 |
| Asano et al., 201116) | 7 | 21 | 19 | 9 | – | – | – | – | 10 | 9 | 4 | 4 |
| Scholler et al., 20135) | 4 | 21 | 12 | 13 | 2 | 1 | 13 | 6 | 6 | 12 | 2 | 4 |
| Hishikawa et al., 201418) | 6 | 6 | 8 | 4 | 0 | 3 | 9 | 0 | – | – | – | 1 |
| Sadamasa et al., 201419) | 9 | 60 | 37 | 32 | – | – | – | – | 56 | 0 | 11 | 8 |
| Wilson et al., 201420) | 3 | 13 | – | – | – | – | – | – | – | – | – | – |
| Shimamura et al., 201621) | 8 | 78 | 68 | 18 | 3 | 17 | 51 | 15 | – | – | – | – |
| Total | 135 (16.8%) | 667 (83.2%) | 520 (66.2%) | 266 (33.8%) | 19 (3.9%) | 83 (16.9%) | 281 (57.1%) | 109 (22.2%) | 255 (41.0%) | 170 (27.3%) | 141 (22.7%) | 56 (9.0%) |
As the treatment selection, clipping was performed in 479 cases, coiling in 115 cases, and conservative treatment without aneurysmal occlusion was chosen for 218 cases (Table 3). Two studies investigated only cases that underwent clipping,11,13) and three studies investigated only cases that underwent coiling.17,18,20)
Table 3.
Treatment methods
| Study | Clipping | Wrapping or trapping | Coiling | Conservative |
|---|---|---|---|---|
| Hamada et al., 199913) | 10 | 0 | ||
| Hamada et al., 200114) | 15 | 0 | 14 | |
| Mont’alverne et al., 200517) | 14 | |||
| Nieuwkamp et al., 20064) | 34 | 2 | 13 | 121 |
| Asano et al., 200715) | 5 | 0 | 1 | 18 |
| Horiuchi et al., 201111) | 333 | 0 | ||
| Asano et al., 201116) | 10 | 0 | 6 | 12 |
| Scholler et al., 20135) | 4 | 0 | 13 | 8 |
| Hishikawa et al., 201418) | 12 | |||
| Sadamasa et al., 201419) | 23 | 0 | 20 | 26 |
| Wilson et al., 201420) | 16 | |||
| Shimamura et al., 201621) | 45 | 2 | 20 | 19 |
| Total | 479 (58.7%) | 4 (0.5%) | 115 (14.1%) | 218 (26.7%) |
As complications, symptomatic vasospasm was seen in 93 of 364 cases (25.5%), hydrocephalus in 117 of 376 cases (31.1%), and medical complication was seen in 123 of 320 cases (38.4 %) (Table 4).
Table 4.
Complications
| Study | Vasospasm | Hydrocephalus | Medical complication |
|---|---|---|---|
| Hamada et al., 199913) | 2/10 | 2/10 | 1/10 |
| Hamada et al., 200114) | 10/29 | – | 8/29 |
| Mont’alverne et al., 200517) | – | – | – |
| Nieuwkamp et al., 20064) | 37/170 | 70/170 | 79/170 |
| Asano et al., 200715) | – | – | – |
| Horiuchi et al., 201111) | – | – | – |
| Asano et al., 201116) | – | – | – |
| Scholler et al., 20135) | – | 3/25 | 21/25 |
| Hishikawa et al., 201418) | – | – | – |
| Sadamasa et al., 201419) | 14/69 | 17/69 | – |
| Wilson et al., 201420) | – | 12/16 | – |
| Shimamura et al., 201621) | 30/86 | 13/86 | 14/86 |
| Total | 93/364 (25.5%) | 117/376 (31.1%) | 123/320 (38.4%) |
Numerator means applicable cases and denominator means total number of cases in each study.
Overall, favorable outcome was achieved in 285 cases (35.0%), and outcome was poor in 530 cases (65.0%) (Table 5). When clinical outcome was evaluated according to the treatment for aneurysm occlusion, favorable outcome was 45.3% in clipping, 36.3% in coiling, and 9.0% in conservative treatment. Outcome was largely influenced by clinical grade on admission, as described later; therefore, outcome was evaluated according to the treatment and clinical grade on admission (Table 6). In patients with a good grade, favorable outcome was 57.5% in clipping, 35.2% in coiling, and 16.4% in conservative treatment. For patients with a poor grade, favorable outcome was 16.3% in clipping, 11.1% in coiling, and 0% in conservative treatment. The study by Horiuchi et al. had the most power with the most cases, whereby the cases treated by clipping were retrospectively analyzed with the conclusion that clipping was useful.11) Excluding this study to avoid bias in outcome evaluation in favor of clipping renders favorable outcome in clipping at 38.5% in the cases with good grade, and 0% in the cases with poor grade.
Table 5.
Outcome according to treatment
| Study | Evaluating timing | Evaluating score | Clipping | Coiling | Conservative | Total | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Favorable outcome | Poor outcome | Favorable outcome | Poor outcome | Favorable outcome | Poor outcome | Favorable outcome | Poor outcome | |||
| Hamada et al., 199913) | At discharge | GOS | 8 | 2 | 8 | 2 | ||||
| Hamada et al., 200114) | At discharge | GOS | 3 | 12 | 1 | 13 | 4 | 25 | ||
| Mont’alverne et al., 200517) | At discharge | GOS | 10 | 4 | 10 | 4 | ||||
| Nieuwkamp et al., 20064) | At discharge | GOS | 8 | 26 | 2 | 11 | 14 | 107 | 25 | 145 |
| Asano et al., 200715) | 1M | mRS | 2 | 3 | 0 | 1 | 0 | 18 | 2 | 22 |
| Horiuchi et al., 201111) | At discharge | GOS | 170 | 163 | 170 | 163 | ||||
| Asano et al., 201116) | “At last” | mRS | 1 | 9 | 0 | 6 | 0 | 12 | 1 | 27 |
| Scholler et al., 20135) | At discharge | GOS | – | – | – | – | – | – | 13 | 11 |
| Hishikawa et al., 201418) | At discharge | mRS | 0 | 12 | 0 | 12 | ||||
| Sadamasa et al., 201419) | 3M | mRS | 6 | 17 | 11 | 9 | 1 | 25 | 18 | 51 |
| Wilson et al., 201420) | 6M | GOS | 7 | 9 | 7 | 9 | ||||
| Shimamura et al., 201621) | 1M | mRS | 17 | 28 | 7 | 13 | 3 | 16 | 27 | 59 |
| Total | 215 (45.3%) | 260 (54.7%) | 37 (36.3%) | 65 (63.7%) | 19 (9.0%) | 191 (91.0%) | 285 (35.0%) | 530 (65.0%) | ||
Table 6.
Rate of favorable outcome according to treatment and clinical grade on admission
| Study | Clipping | Coiling | Conservative | |||
|---|---|---|---|---|---|---|
| Good-grade | Poor-grade | Good-grade | Poor-grade | Good-grade | Poor-grade | |
| Hamada et al., 199913) | 8/10 | 0 | ||||
| Hamada et al., 200114) | 3/15 | 0 | 1/14 | 0 | ||
| Mont’alverne et al., 200517) | – | – | ||||
| Nieuwkamp et al., 20064) | 8/32 | 0/2 | 2/12 | 1/1 | 14/64 | 0/57 |
| Asano et al., 200715) | 2/4 | 0/1 | 0 | 0/1 | 0/6 | 0/12 |
| Horiuchi et al., 201111) | 147/217 | 23/116 | ||||
| Asano et al., 201116) | 1/7 | 0/3 | 0/4 | 0/2 | 0/8 | 0/4 |
| Scholler et al., 20135) | – | – | – | – | – | – |
| Hishikawa et al., 201418) | 0/8 | 0/4 | ||||
| Sadamasa et al., 201419) | 6/11 | 0/12 | 10/15 | 1/5 | 1/11 | 0/15 |
| Wilson et al., 201420) | – | – | ||||
| Shimamura et al., 201621) | 17/38 | 0/7 | 7/15 | 0/5 | 3/13 | 0/6 |
| Total | 192 / 334 (57.5%) | 23/141 (16.3%) | 19/54 (35.2%) | 2/18 (11.1%) | 19/116 (16.4%) | 0/94 (0%) |
| 45 / 117* (38.5%) | 0/25* (0%) | |||||
Numerator means applicable cases and denominator means total number of cases in each study.
The number was expressed by excluding the report by Horiuchi et al.
Of 12 studies, five investigated risk factors for neurological outcomes by using multivariate analysis (Table 7).4,5,11,16,21) Reported risk factors for neurological outcomes were poor clinical grade on admission in four studies,5,11,16,21) medical complication in two studies,5,21) being male in one study,21) selection of conservative treatment without aneurysm occlusion in one study,5) ACA aneurysm in one study,11) cerebral vasospasm in one study,5) hydrocephalus in one study,5) aging in one study5) and premorbid condition in one study.21) However, none of the studies showed the actual number of cases, and meta-analysis of these risk factors using accumulated cases could not be performed. A comparative investigation among several time-spans at 75 or 80 years of age or older performed in three studies showed there was no cutoff age affecting outcome.4,11,17) Neurological outcome for patients over age 85 was shown in five articles, and 72 of 90 patients (80.0%) had poor outcome.4,11,15–17) Excluding the study by Horiuchi et al., poor outcome was seen in 56 of 60 patients (93.3%) over 85 years old.4,15–17)
Table 7.
Risk factors for neurological outcome and mortality indicated by multivariate analysis
| Risk factor | Number of reported literatures | |
|---|---|---|
| Neurological outcome | Mortality | |
| Poor clinical grade on admission | 4 | 3 |
| Medical complication | 2 | 1 |
| Aging | 1 | 3 |
| Selection of conservative treatment without aneurysm occlusion | 1 | 2 |
| Male | 1 | 1 |
| Cerebral vasospasm | 1 | – |
| ACA aneurysm | 1 | – |
| Hydrocephalus | 1 | – |
| Premorbid condition | 1 | – |
| Rebleeding | – | 1 |
| Intraventricular hemorrhage | – | 1 |
Four studies investigated risk factors for mortality by using multivariate analysis.4,5,15,21) Reported risk factors for mortality were poor clinical grade on admission in three studies4,5,15) and aging in three studies.5,15,21) Mortality of patients over age 85 was documented in four articles, and 37 of 60 patients (61.7%) died.4,15–17) As the other risk factors for mortality, selection of conservative treatment without aneurysm occlusion was pointed out in two studies,5,15) medical complication in one study,21) rebleeding in one study,4) intraventricular hemorrhage in one study,4) being male in one study.21) Meta-analysis of these risk factors using accumulated cases could also not be performed, due to the absence of the actual number of cases in several studies.
Discussion
In 12 articles adopted in the present study, seven were investigated in Japan and the others were performed in other developed countries. Seven of the studies were published within the last six years. These seem to reflect that many countries are recently becoming aged or are aging societies. The definition of “elderly” in the field of aSAH varied according to the published articles. In the first report investigating aSAH in the elderly, patient age was over 50 years.22) In the first report studying aSAH in Japan, the age was over 60.23) Subsequently, several ages were investigated as “elderly.” In the present study, those studies with ages over 75 were included and investigated. This was due to the fact that several studies have indicated that clinical outcome was significantly different when the cut-off age was set at 75 years.8–10) There have been no studies showing an age lower than 75 year old could be a cut-off point. We believe that 75 years of age should be considered “elderly” for aSAH when proper treatment is discussed in order to improve outcome.
One of the characteristics of elderly aSAH emerging from the present study is that the female gender greatly predominates. Comparative studies between the elderly versus younger age have indicated that female gender is predominant above the age of 65 years,24) 70 years,6) or with increasing age.5,7) This is associated with the epidemiological fact that the incidence of aSAH increases with age in females and that females usually have a longer average lifespan.1) As the site of aneurysm, ICA aneurysm was dominant at about 40%, which might be due to the fact that ICA aneurysm was seen to predominate in the female.25) Poor clinical grade on admission was 35.6% with the exclusion of studies with selection bias, and this was similar to the studies that investigated patients over age 70 in the North American multicenter study or the hospital-based study in Japan, which also indicated that poor clinical grade on admission increased with age.6,7) This might be due to the fragility of the elderly brain and increased numbers of aSAH.6) The degree of aSAH on CT scan has been considered to increase with age, because the subarachnoid space enlarges in association with atrophy of the elderly brain.6,7) The present study showed that Fisher’s group 3 was 57% and group 4 was 22%. A recent prospective observational cohort study showed that severe aSAH with modified Fisher grades 3 or 4 was 40% considering all age categories,26) while the study based on the Japanese Stroke Databank indicated severe aSAH with Fisher grades 3 or 4 was 81.8% considering all age categories.27) Whether severe aSAH is dominant in elderly cases should be determined in the future.
In considering the appropriate treatment for aSAH in the elderly, necessary information includes risk factors in outcome, indication for treatment of ruptured aneurysm, and the proper method for aneurysmal occlusion. The most important risk factor for outcome was clinical grade on admission. This could affect not only neurological outcome but also mortality, as demonstrated by multivariate analysis in four reports and three reports, respectively. In total, of 253 cases with poor clinical grade on admission, only 25 cases (9.9%) showed favorable outcome. If the study by Horiuchi et al., which had the most power with total of 333 cases, was excluded because of possibly favoring clipping, only two of 137 cases (1.5%) with poor clinical grade on admission showed favorable outcome, and these two cases underwent coiling. In total, 141 cases with poor clinical condition underwent clipping, 23 cases (16.3%) were with favorable outcome. However, if the study by Horiuchi et al. was excluded,11) none of 25 cases (0 %) showed favorable outcome. These results point to the fact that the indication for treatment of aneurysmal occlusion for poor clinical grade cases should be careful considered if taking life expectancy into consideration.
Age and medical complication were also indicated as risk factors for neurological outcome and mortality by several studies. The cutoff age could not be established by comparative investigation among several generations over 75 years of age; however, favorable outcome were hardly obtained in patients over age 85. The cutoff age for the indication of progressive treatment should be determined by future studies. The present study revealed that medical complication was seen in 38.4% of cases; therefore, its reduction is very important in improving overall outcome. Shimamura et al. indicated that early ambulation was effective for preventing dementia and medical complication.28)
Clipping versus coiling has been a controversial problem. Subgroup analysis of elderly patients in an international subarachnoid aneurysm trial revealed coiling brought significantly better outcome for IC and posterior communicating artery aneurysms, while clipping brought significantly better outcomes for MCA aneurysms.29) However, only 29 (10.4%) of 278 cases were patients over age 75. In the present study, if the study by Horiuchi et al. is excluded, in the cases with good clinical grade on admission, favorable outcome was achieved in 38.5% of cases by clipping and in 35.2% by coiling, which showed no significant difference. The analysis according to the site of aneurysm could not be performed because of a lack of the data in the present study. The conclusion should be a future problem by accumulating a large number of cases with appropriate patient information.
Conclusion
Based on this analysis of the literature, patients over age 85 with poor clinical condition on admission are hardly candidates for aneurysm repair treatment. Treatment of aneurysmal occlusion should be carefully considered for cases over age 85 or with poor clinical condition on admission. Patients under age 85 with good clinical condition on admission can be candidates for aneurysm repair treatment, and care should be taken to minimize postoperative complication in order to obtain favorable outcome.
Footnotes
Conflicts of Interest Disclosure
The authors declare that they have no conflicts of interest.
References
- 1). Ohkuma H, Fujita S, Suzuki S: Incidence of aneurysmal subarachnoid hemorrhage in Shimokita, Japan, from 1989 to 1998. Stroke 33: 195– 199, 2002. [DOI] [PubMed] [Google Scholar]
- 2). Yamashita K, Kashiwagi S, Kato S, Takasago T, Ito H: Cerebral aneurysms in the elderly in Yamaguchi, Japan. Analysis of the Yamaguchi Data Bank of Cerebral Aneurysm from 1985 to 1995. Stroke 28: 1926– 1931, 1997. [DOI] [PubMed] [Google Scholar]
- 3). Kaminogo M, Yonekura M: Trends in subarachnoid haemorrhage in elderly persons from Nagasaki, Japan: analysis of the Nagasaki SAH Data Bank for cerebral aneurysm, 1989–1998. Acta Neurochir (Wien) 144: 1133– 1138, discussion 1138–1139, 2002. [DOI] [PubMed] [Google Scholar]
- 4). Nieuwkamp DJ, Rinkel GJ, Silva R, Greebe P, Schokking DA, Ferro JM: Subarachnoid haemorrhage in patients > or = 75 years: clinical course, treatment and outcome. J Neurol Neurosurg Psychiatr 77: 933– 937, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5). Schöller K, Massmann M, Markl G, et al. : Aneurysmal subarachnoid hemorrhage in elderly patients: long-term outcome and prognostic factors in an interdisciplinary treatment approach. J Neurol 260: 1052– 1060, 2013. [DOI] [PubMed] [Google Scholar]
- 6). Inagawa T, Yamamoto M, Kamiya K, Ogasawara H: Management of elderly patients with aneurysmal subarachnoid hemorrhage. J Neurosurg 69: 332– 339, 1988. [DOI] [PubMed] [Google Scholar]
- 7). Lanzino G, Kassell NF, Germanson TP, et al. : Age and outcome after aneurysmal subarachnoid hemorrhage: why do older patients fare worse? J Neurosurg 85: 410–418, 1996. [DOI] [PubMed] [Google Scholar]
- 8). Proust F, Gérardin E, Derrey S, et al. : Interdisciplinary treatment of ruptured cerebral aneurysms in elderly patients. J Neurosurg 112: 1200– 1207, 2010. [DOI] [PubMed] [Google Scholar]
- 9). Park J, Woo H, Kang DH, Kim Y: Critical age affecting 1-year functional outcome in elderly patients aged ≥ 70 years with aneurysmal subarachnoid hemorrhage. Acta Neurochir (Wien) 156: 1655– 1661, 2014. [DOI] [PubMed] [Google Scholar]
- 10). Shirao S, Yoneda H, Kunitsugu I, Suehiro E, Koizumi H, Suzuki M: Age limit for surgical treatment of poor-grade patients with subarachnoid hemorrhage: A project of the Chugoku-Shikoku division of the Japan neurosurgical society. Surg Neurol Int 3: 143, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11). Horiuchi T, Hongo K: Clipping surgery for aneurysmal subarachnoid hemorrhage in patients aged 75 years or older. Neurol Res 33: 853– 857, 2011. [DOI] [PubMed] [Google Scholar]
- 12). Horiuchi T, Tsutsumi K, Ito K, Hongo K: Results of clipping surgery for aneurysmal subarachnoid hemorrhage in the ninth and tenth decades of life. J Clin Neurosc 21: 1567– 1569, 2014. [DOI] [PubMed] [Google Scholar]
- 13). Hamada J, Hasegawa S, Kai Y, Morioka M, Fujioka S, Ushio Y: Surgery and long-term outcome for ruptured anterior circulation aneurysms in patients in their ninth decade of life. Surg Neurol 52: 123– 126; discussion 126–127, 1999. [DOI] [PubMed] [Google Scholar]
- 14). Hamada J, Morioka M, Miura M, Fujioka S, Marubayashi T, Ushio Y: Management outcome for ruptured anterior circulation aneurysms with a Hunt and Hess clinical grade of III in patients in the 9th decade of life. Surg Neurol 56: 294– 300, 2001. [DOI] [PubMed] [Google Scholar]
- 15). Asano S, Hara T, Haisa T, et al. : Outcomes of 24 patients with subarachnoid hemorrhage aged 80 years or older in a single center. Clin Neurol Neurosurg 109: 853– 857, 2007. [DOI] [PubMed] [Google Scholar]
- 16). Asano S, Watanabe T, Shinohara T, et al. : Importance of the initial grade of subarachnoid hemorrhage in the patients with the age of 80 years and older from a single center analysis. Acta Neurol Belg 111: 213– 216, 2011. [PubMed] [Google Scholar]
- 17). Mont’alverne F, Musacchio M, Tolentino V, Riquelme C, Tournade A: Endovascular management for intracranial ruptured aneurysms in elderly patients: outcome and technical aspects. Neuroradiology 47: 446– 457, 2005. [DOI] [PubMed] [Google Scholar]
- 18). Hishikawa T, Takasugi Y, Shimizu T, et al. : Cerebral vasospasm in patients over 80 years treated by coil embolization for ruptured cerebral aneurysms. Biomed Res Int 2014: 253867, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19). Sadamasa N, Koyanagi M, Fukuda H, Chin M, Handa A, Yamagata S: Is aneurysm repair justified for the patients aged 80 or older after aneurysmal subarachnoid hemorrhage? J Neurointerv Surg 6: 664–666, 2014. [DOI] [PubMed] [Google Scholar]
- 20). Wilson TJ, Davis MC, Stetler WR, et al. : Endovascular treatment for aneurysmal subarachnoid hemorrhage in the ninth decade of life and beyond. J Neurointerv Surg 6: 175– 177, 2014. [DOI] [PubMed] [Google Scholar]
- 21). Shimamura N, Naraoka M, Katagai T, et al. : Analysis of factors that influence long-term independent living for elderly subarachnoid hemorrhage patients. World Neurosurg 90: 504– 510, 2016. [DOI] [PubMed] [Google Scholar]
- 22). Goebert WH, Jr: Ruptured cerebral aneurysm in the older patient. Geriatrics 23: 113– 114, 1968. [PubMed] [Google Scholar]
- 23). Ohmoto T, Mino S, Nishimoto A, Higashi T, Miyake S, Doi A: Operative results of ruptured intracranial aneurysms in aged patients. Neurol Med Chir (Tokyo) 20: 721– 728, 1980. [DOI] [PubMed] [Google Scholar]
- 24). Rinaldo L, Rabinstein AA, Lanzino G: Elderly age associated with poor functional outcome after rupture of anterior communicating artery aneurysms. J Clin Neurosci 34: 108– 111, 2016. [DOI] [PubMed] [Google Scholar]
- 25). Kongable GL, Lanzino G, Germanson TP, et al. : Gender-related differences in aneurysmal subarachnoid hemorrhage. J Neurosurg 84: 43– 48, 1996. [DOI] [PubMed] [Google Scholar]
- 26). van Donkelaar CE, Bakker NA, Veeger NJ, et al. : Prediction of outcome after subarachnoid hemorrhage: timing of clinical assessment. J Neurosurg 126: 52– 59, 2017. [DOI] [PubMed] [Google Scholar]
- 27). Yamada S, Ishikawa M, Yamamoto K, Ino T, Kimura T, Kobayashi S, Japan Standard Stroke Registry Study Group : Aneurysm location and clipping versus coiling for development of secondary normal-pressure hydrocephalus after aneurysmal subarachnoid hemorrhage: Japanese Stroke DataBank. J Neurosurg 123: 1555– 1561, 2015. [DOI] [PubMed] [Google Scholar]
- 28). Shimamura N, Matsuda N, Satou J, Nakano T, Ohkuma H: Early ambulation produces favorable outcome and nondemential state in aneurysmal subarachnoid hemorrhage patients older than 70 years of age. World Neurosurg 81: 330– 334, 2014. [DOI] [PubMed] [Google Scholar]
- 29). Ryttlefors M, Enblad P, Kerr RS, Molyneux AJ: International subarachnoid aneurysm trial of neurosurgical clipping versus endovascular coiling: subgroup analysis of 278 elderly patients. Stroke 39: 2720– 2726, 2008. [DOI] [PubMed] [Google Scholar]