Abstract
This article presents the authors' technique for evaluation of possible abductor tears with magnetic resonance imaging (MRI). By using T2 fat-saturated coronal and axial slices of the hip and T1 coronal images of the pelvis, the authors show how to visualize all tears of the abductor tendons and signs of chronic abductor deficiency. After diagnosis has been made, signs that may help the surgeon determine if open or arthroscopic surgery would be best used are reviewed. Finally, the author reviews indications for a gluteus medius repair with concomitant gluteus maximus reconstruction.
Greater trochanteric bursitis is a self-limiting pathology that is best treated with nonsurgical means in the form of physical therapy, anti-inflammatories, activity modification, and corticosteroid injection.1 This has been the mainstay of treatment for many years. When recalcitrant to nonoperative measures, or if the patient reveals objective abductor weakness or Trendelenburg gait, then magnetic resonance imaging (MRI) of the hip should be performed. Most recalcitrant greater trochanteric bursitis is usually secondary to a neglected abductor tear, which leads to failure of the conservative management.
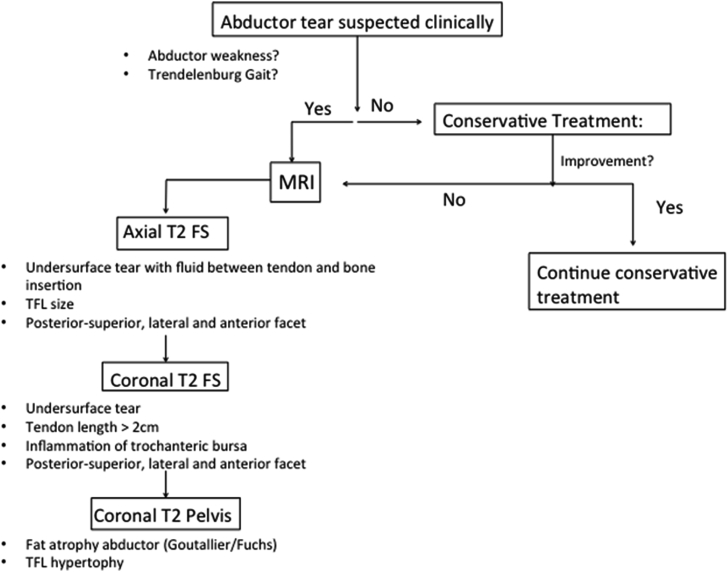
The only plain radiographic sign that has been noted for abductor tears is surface irregularities of the greater trochanter at the insertion site of the abductor tendons that are greater than 2 mm.2 MRI is the gold standard for visualizing abductor tears and characterizing them to determine proper management. Currently there is no algorithmic approach in the literature showing how best to evaluate the abductor tendon with the use of MRI (Fig 1). The purpose of this article was to propose an algorithmic approach to evaluation of the abductor tendon with MRI scan to ensure that all tears are diagnosed properly and to provide likely indications for arthroscopic versus open approach to repair and gluteus maximus transfer.
Fig 1.
Senior author's current algorithm for evaluating the abductors in a patient that presents with greater trochanteric pain syndrome showing when to order an MRI and when to treat the patient conservatively. (FS, fat-saturated; MRI, magnetic resonance imaging; TFL, tensor fascia lata.)
Technique
This technique will describe an algorithmic approach in which to evaluate hip MRI scans for abductor tears as well as a helpful way to assess if the tears can be successfully treated arthroscopically or are more likely to require an open approach (Video 1). The authors will also state their indication for gluteus maximus transfer.
The sequences that are used for evaluation of the abductor tendons and muscles are an axial T2 fat-saturated coronal and axial image as well as a T1 coronal image of the pelvis (Table 1). The first images that are examined are the axial T2 fat saturated image. The proximal aspect of the of the abductor muscle belly is visualized. The examiner will slowly scroll distally. As you come just proximal to the musculotendinous junction, the tendons of the gluteus minimus and gluteus medius are easily identifiable (Fig 2). As you continue distally, you can see the insertion of the gluteus medius onto the superior-posterior facet of the greater trochanter, which is the largest portion of the gluteus medius footprint.3 The footprint of the gluteus medius moves from the superior-posterior facet anterodistally onto the lateral facet. As it moves distally, it begins to merge with the proximal aspect of the vastus lateralis at the vastus ridge. The gluteus minimus has a much smaller footprint on the anterior facet of the greater trochanter (Fig 3). It is important to scrutinize the superficial (bursal) side of the tendon for greater trochanteric bursitis and bursal sided tears, as well as the undersurface of both tendons for undersurface tear of the abductor tendons (Fig 4). Tears often progress from the undersurface of the anterior aspect of the gluteus medius and move superficial and posterior.4 The authors find this view the most helpful for finding undersurface tears of the abductor tendons. The other structure that should be evaluated on this view is the size of the tensor fascia lata (TFL) (Fig 5). If the TFL appears to be enlarged from what is normally seen, this can be secondary to an increase in the need for that muscle as an abductor indicating chronic abductor insufficiency. If an enlarged TFL is noted, then heavy scrutiny should be given to the abductor tendons for likely chronic tear of the abductor.5
Table 1.
List of Items the Authors Look For in Each Imaging Sequence to Diagnose Abductor Tears
| Image | Items to Locate |
|---|---|
| Coronal T2 fat-saturated hip | -Superior-posterior facet just posterior to a slice of the lesser trochanter -Footprint of the gluteus medius, which moves anterodistal from the superior to the posterior facet -Length of the tendon from insertion to musculotendinous junction (>2 cm = partial tear) |
| Axial T2 fat-saturated hip | -Locate the normal gluteus medius and minimus tendons proximal to the musculotendinous junction -Scroll down to insertion of medius on the superior-posterior facet and lateral facet—pay close attention to fluid between the footprint and greater trochanter (best sequence to find undersurface tears) -Also note the size of the TFL—if enlarged, often a sign of chronic abductor insufficiency |
| Coronal T1 pelvis | -On the image slice that best visualizes the greater and lesser trochanter, note the percentage of fat atrophy of the gluteus medius. -Also note the sizes of the bilateral TFLs and if one side is larger than the other. |
TFL, tensor fascia lata.
Fig 2.

Axial T2 fat-saturated cuts of the left hip with the patient laying supine with their bilateral legs internally rotated 15°. The abductor tendons are located proximal to the level of the greater trochanter and denoted with red circles (anterior tendon is gluteus minimus; posterior tendon is gluteus medius). It is easy to find the tendons more proximally prior to their insertion on the greater trochanter and then follow them down to their insertions on the anterior, lateral, and superior-posterior facets of the greater trochanter.
Fig 3.

Axial T2 fat-saturated cuts of the left hip with the patient laying supine with their bilateral legs internally rotated 15°. This axial cut reveals the normal insertion of the abductor tendons. The broad footprint of the gluteus medius can be seen as a black strip of tendon that begins at the superior-posterior facet (red circle) of the greater trochanter and moves anterodistally along the lateral facet (circled in yellow). Between the lateral facet insertion of the gluteus medius and anterior facet insertion of the gluteus minimus is the bald spot. The gluteus minimus tendon is a smaller tendon that inserts onto the anterior facet of the greater trochanter (blue circle).
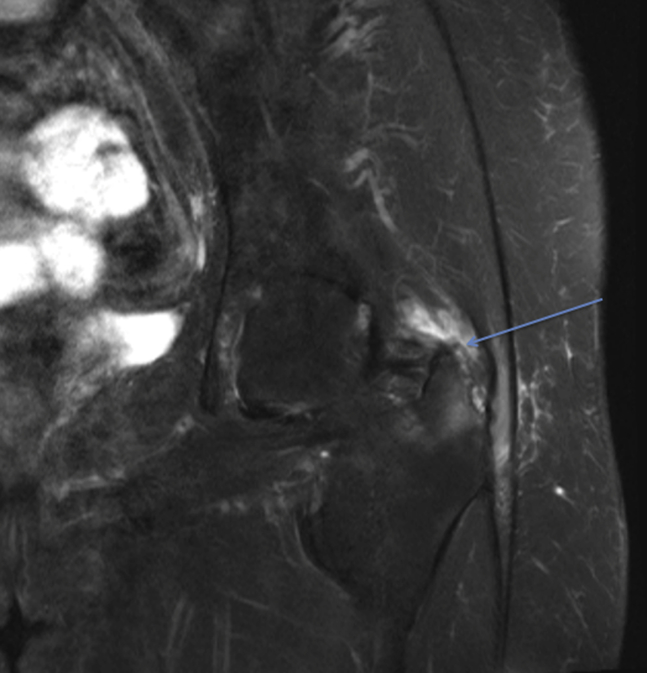
Fig 4.
A T2 fat-saturated coronal MRI cut of the patient's left hip with the patient supine with bilateral legs internally rotated 15°. This shows the undersurface of the gluteus medius torn and retracted from the level of the lateral facet of the greater trochanter (blue arrow). (MRI, magnetic resonance imaging.)
Fig 5.

An axial fat-saturated image of the right hip with the patient lying supine with bilateral legs internally rotated 15° that reveals significant hypertrophy (red circle) of the tensor fascia lata, which when present may indicate chronic abductor insufficiency, which leads to hypertrophy of the secondary abductor.
Next the coronal T2 fat-saturated images are evaluated. Starting from just posterior to the coronal slice that reveals the lesser trochanter, you can visualize the large circular insertion of the gluteus medius onto the superior-posterior facet (Fig 6). As you move anterior with coronal slices, follow the footprint of the gluteus medius distally on the lateral facet where it confluences with the vastus lateralis as previously mentioned. When a larger abductor tear is present, you can oftentimes see a disruption of the proximal tendon of the vastus lateralis insertion as well. In our experience, when the vastus is also disrupted, the size of the tear tends to be substantial. On each section of coronal view that shows the abductor tendons, the length of the tendon from insertion to the musculotendinous junction should be measured. If the length of the tendon is greater than 2 cm, then a high suspicion of a partial-thickness tear should be present (Fig 7).6 This can result from disruption of the insertion of some of the tendon fibers, which may cause retraction of the musculotendinous junction slightly proximally, which in turn can increase the distance from insertion to the junction.
Fig 6.

A coronal T2 fat-saturated image of the right hip with the patient lying supine with bilateral legs internally rotated 15°. The figure notes the normal broad circular superior-posterior facet insertion of the gluteus medius of the greater trochanter (red circle).
Fig 7.

Coronal fat-saturated image of the left hip with the patient lying supine with bilateral legs internally rotated 15°. A high-grade partial-thickness tear of the gluteus medius tendon is suspected on this image. It is annotated that the length from the insertion of the tendon to the musculotendinous junction is greater than 2 cm (green line), indicating a partial-thickness tear. The proximal insertion of the vastus (red arrow) also appears to be injured with inflammation, and a partial tear with fluid surrounding its insertion. Inflammation is also noted in the peritrochanteric region, indicating a component of greater trochanteric bursitis (blue arrow).
The next sequence that is recommended is the coronal T1 view of the pelvis. The purpose of evaluating this set of images is to evaluate the size of the TFL again compared with the contralateral side, and to look for fat atrophy (Fig 8). Goutallier/Fuchs as applied in the shoulder can be applied to the abductor tendons as well.7 A recent study noted that patients with increasing fatty infiltration have worse clinical scores after repair. The image used to measure the amount of fat atrophy is the image that visualizes the lesser and greater troch best in one slice.
Fig 8.
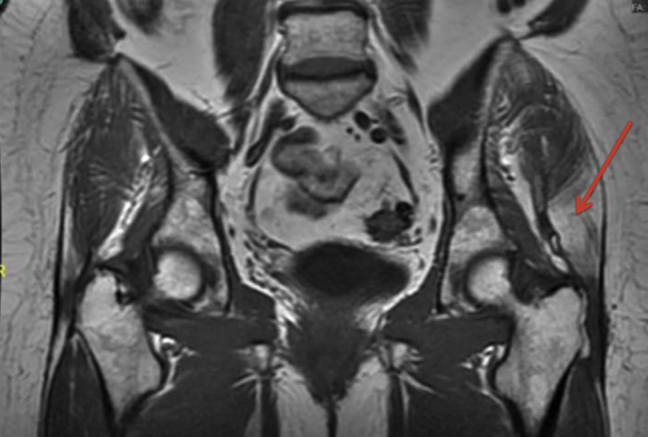
A T1-weighted coronal image of the pelvis with the patient lying supine with bilateral legs internally rotated 15°. The figure highlights a significant amount of fat atrophy on the left side of the patient's pelvis (red arrow) compared with the normal muscle tissue of the right hip. This would be classified as a Goutallier/Fuchs grade II (25%-50% fat atrophy).
Arthroscopic treatment is suited well for partial-thickness tears of either the gluteus medius and/or the gluteus minimus. The senior author advocates for an endoscopic approach in most situations with the exception of a full-thickness tear with greater than 2 cm of retraction, Goutallier/Fuchs grade III or IV fat atrophy, or revision abductor repair. The senior author will perform a gluteus maximus transfer concomitantly with repair if the abductor tendon is irreparable or if the muscle is dysfunctional due to fatty atrophy (>50%) by MRI and by gross examination.8
Discussion
The technique described above is an algorithmic approach to evaluating the abductor tendons with MRI that will allow providers to accurately diagnose and determine the best method for surgical treatment of a patient with an abductor tear. The advantages of this technique are that by systematically using this method the chance of a missed abductor injury are very slight (Tables 2 and 3). As stated previously, abductor tears usually start from the undersurface of the anterior aspect of the gluteus medius and propagate posteriorly and superficial. Treating surgeons whether open or arthroscopic can be deceived when looking at the insertion of the abductor tendons, because the undersurface cannot be visualized. With careful MRI review along with blunt palpation, searching for areas of delamination will allow accurate selection for the sight of an incision in the tendon for transtendinous repair technique.9 The authors also describe the MRI signs that may preclude an arthroscopic approach. This should be taken within the context that the senior author is an experienced hip arthroscopist, and all treating surgeons may need to develop their own criteria for what deserves an open approach in their practice. If treating surgeons are able to decisively know whether an open or an arthroscopic approach is best suited for an abductor tear, this saves them from having to change from an arthroscopic to open approach mid-case, which can be time intensive.
Table 2.
Advantages of Algorithmic Approach to Abductor Tendon Evaluation
| Advantages of Algorithmic Approach |
|---|
| -Simple method for abductor evaluation on MRI -Decreases the frequency of missed abductor injury -Assists surgeon for undersurface tears as in where to make the transtendinous split -Gives parameters to assist in making the determination of whether to proceed with open or endoscopic repair -Assist surgeon in making the decision if patient might require a gluteus maximus transfer in addition to repair |
MRI, magnetic resonance imaging.
Table 3.
Pearls and Pitfalls of the Technique
| Pearls | Pitfalls |
|---|---|
| -Systematically go through the axial and coronal images of every patient -Axial images: Follow the tendons from the musculotendinous junction to the various insertion sites, and look for fluid deep into the tendons for undersurface tears; look for TFL hypertrophy -Coronal imaging: Measure the length of the gluteus medius, look for superficial or deep fluid, which may indicate a tear; look for fat atrophy of the TFL |
-MRI imaging is not perfect and can have false negatives and false positives, which can confuse treatment |
The limitations of this method are that the quality of the MRI depends on the MRI machine used, the ability of the patient to remain still within the scanner, and the skill of the interpreting physician. This will not ensure that all abductor tears will be diagnosed, only that missing tears will be minimized.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: B.G.D reports personal fees and other from Arthrex; other from Breg; other from ATI; personal fees and other from Pacira and Stryker; personal fees from Orthomerica, DJO Global, Amplitude, and Medacta, outside the submitted work; and he is a board member for the American Hip Institute, which funds research and is the institute where our studies are performed; he is also a board member at the AANA (Arthroscopy Association of North America) Learning Center Committee and Arthroscopy journal. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
This study was performed at the American Hip Institute.
Supplementary Data
Video showing an algorithmic approach in which to evaluate MRI scans for abductor tendon pathology. The video uses axial and coronal images of the hip and pelvis with Fat Saturated and T1 weighted sequences to adequately evaluate the tendons to determine if pathology is present. For the MRI scan the patient is supine with their bilateral legs internally rotated 15°. The video reveals normal and then abnormal images for viewer comparison to assist in diagnosis of pathology. (MRI, magnetic resonance imaging.)
References
- 1.Lustenberger D.P., Ng V.Y., Best T.M., Ellis T.J. Efficacy of treatment of trochanteric bursitis: A systematic review. Clin J Sport Med. 2011;21:447–453. doi: 10.1097/JSM.0b013e318221299c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steinert L., Zanetti M., Hodler J., Pfirrmann C.W., Dora C., Saupe N. Are radiographic trochanteric surface irregularities associated with abductor tendon abnormalities? Radiology. 2010;257:754–763. doi: 10.1148/radiol.10092183. [DOI] [PubMed] [Google Scholar]
- 3.Robertson W.J., Gardner M.J., Barker J.U., Boraiah S., Lorich D.G., Kelly B.T. Anatomy and dimensions of the gluteus medius tendon insertion. Arthroscopy. 2008;24:130–136. doi: 10.1016/j.arthro.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 4.Kagan A., 2nd Rotator cuff tears of the hip. Clin Orthop Relat Res. 1999;368:135–140. [PubMed] [Google Scholar]
- 5.Sutter R., Kalberer F., Binkert C.A., Graf N., Pfirrmann C.W., Gutzeit A. Abductor tendon tears are associated with hypertrophy of the tensor fasciae latae muscle. Skeletal Radiol. 2013;42:627–633. doi: 10.1007/s00256-012-1514-2. [DOI] [PubMed] [Google Scholar]
- 6.Cvitanic O., Henzie G., Skezas N., Lyons J., Minter J. MRI diagnosis of tears of the hip abductor tendons (gluteus medius and gluteus minimus) AJR Am J Roentgenol. 2004;182:137–143. doi: 10.2214/ajr.182.1.1820137. [DOI] [PubMed] [Google Scholar]
- 7.Bogunovic L., Lee S.X., Haro M.S. Application of the Goutallier/Fuchs rotator cuff classification to the evaluation of hip abductor tendon tears and the clinical correlation with outcome after repair. Arthroscopy. 2015;31:2145–2151. doi: 10.1016/j.arthro.2015.04.101. [DOI] [PubMed] [Google Scholar]
- 8.Whiteside L.A. Surgical technique: Transfer of the anterior portion of the gluteus maximus muscle for abductor deficiency of the hip. Clin Orthop Relat Res. 2012;470:503–510. doi: 10.1007/s11999-011-1975-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Domb B.G., Nasser R.M., Botser I.B. Partial-thickness tears of the gluteus medius: Rationale and technique for trans-tendinous endoscopic repair. Arthroscopy. 2010;26:1697–1705. doi: 10.1016/j.arthro.2010.06.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video showing an algorithmic approach in which to evaluate MRI scans for abductor tendon pathology. The video uses axial and coronal images of the hip and pelvis with Fat Saturated and T1 weighted sequences to adequately evaluate the tendons to determine if pathology is present. For the MRI scan the patient is supine with their bilateral legs internally rotated 15°. The video reveals normal and then abnormal images for viewer comparison to assist in diagnosis of pathology. (MRI, magnetic resonance imaging.)