Abstract
Objective
To determine if improved geographical accessibility led to increased uptake of maternity care in the south of the United Republic of Tanzania.
Methods
In a household census in 2007 and another large household survey in 2013, we investigated 22 243 and 13 820 women who had had a recent live birth, respectively. The proportions calculated from the 2013 data were weighted to account for the sampling strategy. We examined the association between the straight-line distances to the nearest primary health facility or hospital and uptake of maternity care.
Findings
The percentages of live births occurring in primary facilities and hospitals rose from 12% (2571/22 243) and 29% (6477/22 243), respectively, in 2007 to weighted values of 39% and 40%, respectively, in 2013. Between the two surveys, women living far from hospitals showed a marked gain in their use of primary facilities, but the proportion giving birth in hospitals remained low (20%). Use of four or more antenatal visits appeared largely unaffected by survey year or the distance to the nearest antenatal clinic. Although the overall percentage of live births delivered by caesarean section increased from 4.1% (913/22 145) in the first survey to a weighted value of 6.5% in the second, the corresponding percentages for women living far from hospital were very low in 2007 (2.8%; 35/1254) and 2013 (3.3%).
Conclusion
For women living in our study districts who sought maternity care, access to primary facilities appeared to improve between 2007 and 2013, however access to hospital care and caesarean sections remained low.
Résumé
Objectif
Déterminer si l'amélioration de l'accessibilité géographique a permis d'augmenter le recours aux soins de maternité dans le sud de la République-Unie de Tanzanie.
Méthodes
À l'occasion d'un recensement des ménages réalisé en 2007 et d'une autre grande enquête menée auprès des ménages en 2013, nous nous sommes intéressés respectivement à 22 243 et 13 820 femmes dont la grossesse avait récemment abouti à une naissance vivante. Les proportions calculées à partir des données de 2013 ont été pondérées afin de tenir compte de la stratégie d'échantillonnage. Nous avons examiné l'association entre la distance directe jusqu'à l'établissement de soins primaires ou l'hôpital le plus proche et le recours aux soins de maternité.
Résultats
Le pourcentage de naissances vivantes survenues dans des établissements de soins primaires et des hôpitaux est passé respectivement de 12% (2571/22 243) et 29% (6477/22 243) en 2007 à des valeurs pondérées de 39% et 40% en 2013. Entre les deux enquêtes, nous avons observé une nette augmentation du recours aux établissements de soins primaires par les femmes qui vivaient loin des hôpitaux, mais la proportion de femmes à accoucher à l'hôpital est restée faible (20%). L'année de l'enquête ou la distance jusqu'au centre de soins prénataux le plus proche n'a guère changé les chiffres concernant la venue à quatre consultations prénatales ou plus. Même si le pourcentage global de naissances vivantes survenues par césarienne est passé de 4,1% (913/22 145) lors de la première enquête à une valeur pondérée de 6,5% lors de la seconde, les pourcentages correspondants pour les femmes résidant loin des hôpitaux étaient très faibles en 2007 (2,8%; 35/1254) et en 2013 (3,3%).
Conclusion
Pour les femmes qui vivaient dans les districts observés et qui ont eu besoin de soins de maternité, l'accès aux établissements de soins primaires s'est amélioré entre 2007 et 2013; cependant, l'accès aux hôpitaux et aux césariennes est resté faible.
Resumen
Objetivo
Determinar si una mejora de la accesibilidad geográfica conduce a una mayor aceptación de la atención materna en el sur de la República Unida de Tanzanía.
Métodos
En un censo doméstico de 2007 y otra encuesta doméstica de 2013, se investigaron a 22.243 y 13.820 mujeres que recientemente habían dado a luz a un nacido vivo, respectivamente. Las proporciones calculadas a partir de los datos de 2013 se ponderaron para tener en cuenta la estrategia de muestreo. Se examinó la asociación entre las distancias en línea recta hasta el centro de salud primaria o el hospital más cercano y la aceptación de la atención materna.
Resultados
Los porcentajes de nacidos vivos que se producen en centros de atención primaria y hospitales aumentaron del 12% (2571/22.243) y el 29% (6477/22.243), respectivamente, en 2007 a valores ponderados del 39% y 40%, respectivamente, en 2013. Entre las dos encuestas, las mujeres que vivían lejos de los hospitales mostraron un aumento notable en el uso de centros de atención primaria, pero la proporción que dio a luz en hospitales se mantuvo baja (20%). El uso de cuatro o más visitas prenatales no se vio afectado en gran medida por el año de la encuesta o la distancia a la clínica prenatal más cercana. Aunque el porcentaje general de nacidos vivos por cesárea aumentó del 4,1% (913/22.145) en la primera encuesta a un valor ponderado del 6,5% en la segunda, los porcentajes correspondientes para las mujeres que viven lejos de un hospital fueron muy bajos en 2007 (2,8%; 35/1254) y 2013 (3,3%).
Conclusión
Para las mujeres que viven en nuestros distritos de estudio que buscaron atención materna, el acceso a los centros de atención primaria pareció mejorar entre 2007 y 2013. Sin embargo, el acceso a la atención hospitalaria y a las cesáreas se mantuvo bajo.
ملخص
الغرض
تحديد إذا ما كان تيسير الحصول على الخدمات الصحية في المناطق الجغرافية المختلفة قد أثمر عن زيادة الاستفادة من خدمات رعاية الأمومة في جنوب جمهورية تنزانيا المتحدة.
الطريقة
استعنا بتعداد للأسر تم إجراؤه في عام 2007 وكذلك دراسة استقصائية واسعة النطاق للأسر تم إجراؤها في عام 2013 للبحث في 22243 حالة و13820 حالة أخرى على التوالي من حالات النساء اللاتي رُزقن بمولود حي مؤخرًا. وتم ترجيح النسب المحتسبة اعتمادًا على بيانات عام 2013 لتناسب استراتيجية انتقاء العينات. ونظرنا في الارتباط بين مسافات المسارات المستقيمة المؤدية لأقرب مستشفى أو منشأة صحية رئيسية والاستفادة من خدمات رعاية الأمومة.
النتائج
ارتفعت النسب المئوية للمواليد الأحياء في المستشفيات والمنشآت الصحية الرئيسية من 12% (2571/22243) و29% (6477/22243)، على التوالي، في عام 2007 لتصل إلى القيم المرجحة البالغة 39% و40%، على التوالي، في عام 2013. وتبين أن النساء اللاتي تعشن في مناطق بعيدة عن المستشفيات قد استفدن، في الفترة بين الدراستين الاستقصائيتين، استفادةً ملحوظة فيما يتعلق بحصولهن على خدمات المنشآت الصحية الرئيسية، بينما ظلت نسبة الولادة داخل المستشفيات منخفضة (20%). ولم يؤثر العام الذي تم فيه إجراء الدراسة الاستقصائية، أو المسافة التي تقطعها النساء للوصول إلى أقرب عيادة تقدم خدمات ما قبل الولادة، تأثيرًا كبيرًا على الاستفادة من الزيارات الصحية فيما قبل الولادة والبالغ عددها أربع زيارات أو أكثر. وعلى الرغم من أن النسبة المئوية الإجمالية للمواليد الأحياء الذين تمت ولادتهم بالجراحة القيصرية قد ارتفعت من 4.1% (913/22145) في الدراسة الاستقصائية الأولى لتبلغ القيمة المرجحة لها 6.5% في الدراسة الثانية، فإن النسب المئوية المناظرة للنساء اللاتي تعشن بعيدًا عن المستشفى كانت منخفضة للغاية في عام 2007 (2.8%؛ 35/1254) وعام 2013 (3.3%).
الاستنتاج
ظهور تحسن في مستوى الاستفادة من المنشآت الصحية الرئيسية في الفترة بين عامي 2007 و2013 بالنسبة للنساء ممن يعشن في الأقاليم التي شملتها الدراسة التي أجريناها واللاتي كن بحاجةٍ إلى خدمات رعاية الأمومة، وبالرغم من ذلك فإن درجة الاستفادة من خدمات الرعاية المقدمة داخل المستشفيات والخدمات التي تقدمها أقسام الجراحة القيصرية ظلت منخفضة.
摘要
目的
旨在确定提高地域性普及率是否能在坦桑尼亚联合共和国南部地区增加孕产妇的护理接受率。
方法
在 2007 年的家庭普查和 2013 年的另一次大型家庭调查中,我们分别调查了 22 243 名和 13 820 名最近有活产的妇女。考虑到抽样策略,对 2013 年数据计算的比例进行了加权。我们研究了距离最近的基层医疗机构或医院的直线距离与孕产妇护理接受率之间的联系。
结果
2007 年,基层医疗机构和医院的活产百分比分别从 2007 年的 12% (2571/22 243) 和 29% (6477/22 243) 上升至 2013 年的 39% 和 40%。两次调查之间,远离医院的妇女在使用基层医疗机构方面显著增加,但医院的生育比例仍然很低 (20%)。按调查年份或最近的产前诊所距离评估,四次或更多的产前检查基本上不受影响。虽然通过剖腹产的活产婴儿整体百分比从第一次调查的 4.1% (913/22 145) 增加到第二次调查的加权值 6.5%,但 2007 年和 2013 年离医院较远妇女的相应百分比非常低,分别为 2.8% (35/1254) 和 3.3%。
结论
对于生活在我们的研究区域范围内且要求生育的妇女,在 2007 年至 2013 年期间,使用基层医疗机构的机会似乎有所改善,但是接受医院护理和剖腹产的人员仍然很少。
Резюме
Цель
Определить, приведет ли улучшение географической доступности к более высокой обращаемости в службы охраны материнства на юге Объединенной Республики Танзании.
Методы
В ходе переписи населения в 2007 году и еще одного крупного обследования домашних хозяйств в 2013 году мы исследовали соответственно 22 243 и 13 820 женщин, которые недавно родили живых младенцев. Пропорции, рассчитанные по данным 2013 года, были взвешены для учета стратегии выборки. Мы исследовали связь между расстояниями по прямой до ближайшего медицинского учреждения по оказанию первичной медицинской помощи или больницы и обращаемостью в службы охраны материнства.
Результаты
Процент случаев рождения живых младенцев в медицинских учреждениях по оказанию первичной медицинской помощи и больницах увеличился с 12% (2571/22 243) и 29% (6477/22 243) соответственно в 2007 году до взвешенных значений 39 и 40% соответственно в 2013 году. Между этими двумя обследованиями для женщин, живущих далеко от больниц, был продемонстрирован заметный рост в обращаемости в медицинские учреждения по оказанию первичной медицинской помощи, но доля родов в больницах оставалась низкой (20%). Использование четырех или более дородовых посещений в значительной степени не зависело от года обследования или расстояния до ближайшей антенатальной клиники. Несмотря на то что общий процент случаев рождения живых младенцев путем кесарева сечения увеличился с 4,1% (913/22 145) при первом обследовании до взвешенной величины 6,5% во втором, соответствующие процентные показатели для женщин, живущих далеко от больницы, были очень низкими в 2007 году (2,8%, 35/1254) и 2013 году (3,3%).
Вывод
Для женщин, живущих в районах проведения наших исследований, которые обращались в службы охраны материнства, доступ к медицинским учреждениям по оказанию первичной медицинской помощи улучшился в период с 2007 по 2013 год, однако доступ к стационарной медицинской помощи и кесаревым сечениям оставался низким.
Introduction
Given that there were an estimated 303 000 maternal deaths and 2.6 million neonatal deaths in 2015,1,2 we clearly need better ways to reach mothers and their babies with effective interventions.3 Distance to care is known to influence uptake of health services.4 As the technology for geospatial measurement becomes more widely available, there has been an increasing number of studies, in low- and middle income countries, in which the association between distance to care and either uptake of care or mortality has been investigated.5 In general, pregnant women who live far from a health facility are those least likely to have a facility delivery.6–10 This appears to be the situation in the United Republic of Tanzania,11,12 where distance to the nearest hospital has also been found to be positively correlated with direct obstetric mortality.13 Relatively little is known about the association between antenatal care or caesarean section and distance to the nearest facility.14–16
The United Republic of Tanzania has made substantial progress in reducing child mortality, but much more limited improvements in maternal health.17,18 Much of the success in child health has been due to strong preventive actions that have been mediated by a dense network of primary health facilities17,19 and supported by policies that, since the 1980s, have focused on rural public health.20,21 One explicit aim of the country’s recent policy on primary care is to increase access to delivery care in primary facilities – mainly by establishing one dispensary, that can provide basic antenatal, delivery, outpatient and postnatal care, for every village. Health centres, which already provide basic laboratory diagnostics and inpatient care, are progressively being upgraded so that they can also provide comprehensive emergency obstetric care.22 The focused antenatal care programme, which was introduced in 2002, encourages pregnant women without known risk factors to give birth in primary facilities.23 However, while studies have shown that uptake of intrapartum care is increasing in most parts of the United Republic of Tanzania,18 it is not known whether the Tanzanian women who live in remote rural areas have benefited from the policy change. We therefore examined whether – and, if so, how – over a six-year period, the relationship between uptake of maternity care and distance to a health facility had changed in five rural districts in the south of the United Republic of Tanzania. In surveys in 2007 and 2013, we quantified the effect of both the distance to the nearest primary facility – i.e. dispensary or health centre – and the distance to the nearest hospital on four key indicators of maternity care: (i) four or more visits for antenatal care; (ii) birth in a primary facility; (iii) birth in a hospital; and (iv) birth by caesarean section. By examining the interaction between distance to facility and survey year, we then examined whether changes over time in uptake of care varied by distance to a facility.
Methods
We used information from two geo-referenced household surveys covering the same five districts in the south of the United Republic of Tanzania: (i) a census of all 243 612 households in 2007 – primarily designed to evaluate the impact of intermittent preventive treatment with antimalarials on infant survival;24 and (ii) a sample survey in 2013 that assessed the impact of a home-based counselling strategy on neonatal care and survival.25 In both surveys, the study population comprised women who had had a live birth in the 12 months before the survey and reported on uptake of pregnancy and intrapartum care.
The study area covers three districts of the Lindi region and two districts of the Mtwara region.26 Most of the residents of these districts are poor and live in mud-walled houses in rural villages. Between 2009 and 2013, two dispensaries in the study area were upgraded to become health centres and 14 new dispensaries were inaugurated. By 2013, the study population was served by 156 dispensaries, 15 health centres and six hospitals within the study area and by another two hospitals just outside the district boundaries. All except four of the 179 health facilities serving the study area in 2013 – i.e. two mission hospitals, one mission dispensary and one private health centre – were public facilities that provided maternal health services free of charge.27
In both 2007 and 2013, all eight hospitals serving the study area provided caesarean sections on a daily 24-hour basis, three of the hospitals had maternity waiting homes and all of the hospitals and seven of the health centres were equipped with ambulances. Ambulance use – e.g. for hospital referral – was, however, severely constrained by shortages of fuel, human resources and funds for repair. Although all except one of the 179 facilities offered delivery care, basic emergency obstetric care was not consistently available in the study area.27–29
Data collection
The survey methods are described in detail elsewhere.24,25 In brief, we used a modular questionnaire, administered in Swahili, to assess coverage of essential interventions during pregnancy and childbirth. Use of personal digital assistants to collect data facilitated the checking of standard ranges, consistency and completeness at the time of data entry.30 Household wealth was assessed by asking each household head about household assets and housing type. We mapped the study households using a global positioning system. The positions of the relevant health facilities had been recorded in previous surveys.
In 2007, we surveyed all 243 612 households in the five study districts. In 2013, however, we sampled 169 324 households, which were selected by following a two-stage sampling survey.25 Using the results of the national 2012 census, in which 247 350 households were recorded in the study area, we first sampled so-called subvillages. This sampling was proportional to the number of households in each subvillage – typically about 80–100. We included all households in the subvillages with fewer than 130 households, but used segmentation for subvillages with more than 131 households.
Outcomes and explanatory variables
Our main outcomes of interest were uptake of at least four visits for antenatal care, delivery in a health facility and delivery by caesarean section. Using a combination of coordinates and the nearstat command in Stata version 13 (StataCorp. LP, College Station, United States of America), we calculated straight-line distances between each surveyed household and: (i) the nearest antenatal clinic, which could have been in a primary facility or a hospital; (ii) the nearest primary facility offering delivery care; and (iii) the nearest hospital. We did this separately for 2007 and 2013. In the 2007 survey, we attempted to impute the coordinates of households for which no such coordinates were recorded, from the coordinates for neighbouring households. Household wealth quintiles were constructed separately for 2007 and 2013, using principal component analysis.31
Statistical analysis
All analyses were conducted in Stata version 13. For the 2013 data, we accounted for the different sampling structures of the 2007 and 2013 surveys by weighting subvillages by the inverse chance of being included. The percentages reported for 2013 – but not those reported for 2007 – are therefore weighted values. For both 2007 and 2013, we assessed the effect of: (i) distance to nearest antenatal clinic on uptake of at least four visits for antenatal care; (ii) distance to nearest primary facility on delivery in a primary facility; (iii) distance to nearest hospital on hospital delivery; and (iv) distance to nearest hospital on birth by caesarean section. For the analysis of the effect of distance on delivery in a primary facility, we excluded births where a hospital was the nearest facility.
We first used generalized linear models to calculate crude prevalence ratios (cPR) with 95% confidence intervals (CI). We compared the prevalence of each indicator by increasing distance to a primary health facility or hospital and then compared the prevalence of each indicator between 2007 and 2013 within each distance group.32 We adjusted the crude prevalence ratios for potential confounding by the mother’s age, parity, district of residence, education, ethnic group and occupation and her household’s wealth quintile. Using multilevel logistic regression without weighting, we fitted an interaction term between distance to facility and survey year and used the likelihood ratio test to calculate a corresponding P-value. We also used ArcGIS version 9.2 (ESRI, Redlands, USA) to map the absolute increases in facility delivery and caesarean section by administrative ward – as percentages of the live births – between 2007 and 2013.
Ethics
Ethical clearance was obtained from the institutional review boards of Ifakara Health Institute, and the Tanzanian National Institute of Medical Research and the ethics committees of the London School of Hygiene and Tropical Medicine and the Swiss cantons of Basel-Stadt and Basel-Land.
The study population was informed about the surveys by the local government authorities and again, one day prior interview, by a sensitizer who used information sheets in the local language. Written consent to participate was obtained from household heads and the women who answered questions about pregnancy and childbirth.
Results
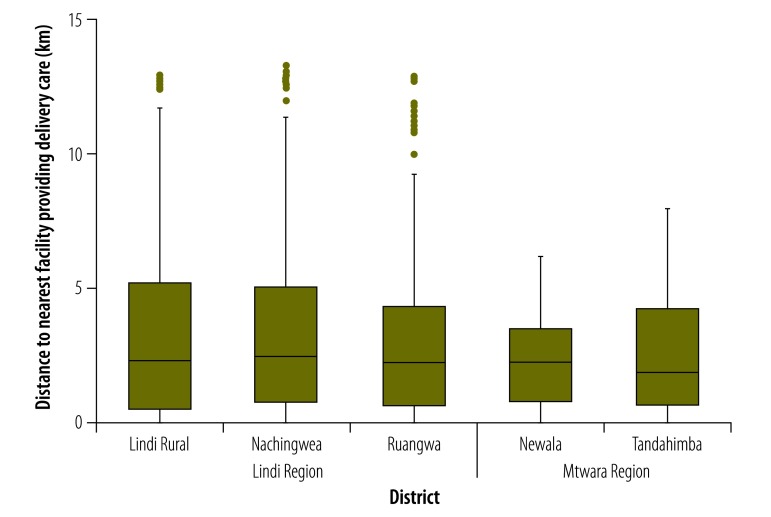
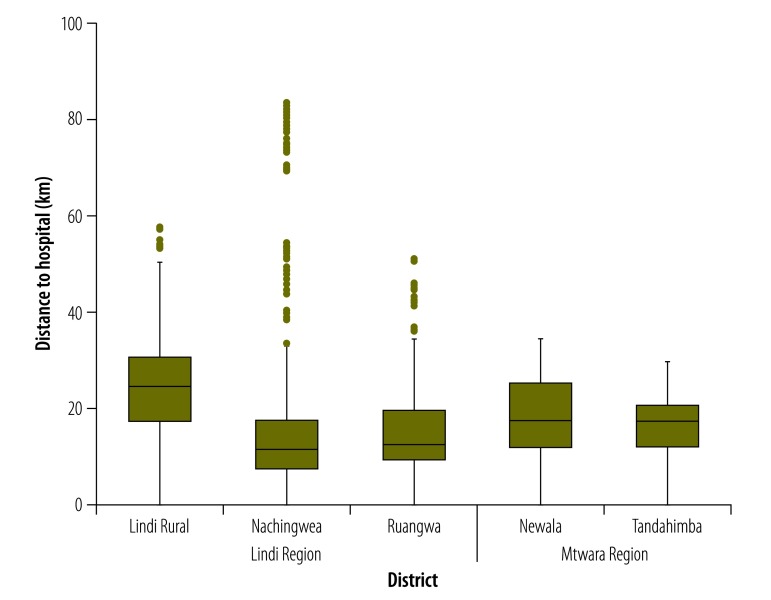
We conducted interviews with 321 093 consenting females who were aged 13–49 years and considered to be women of reproductive age: 193 867 in 2007 and 127 226 in 2013. Overall, 22 243 of these women had a live birth in the 12 months before the 2007 survey and 13 820 in the 12 months before the 2013 survey. Of these interviewees, 21 959 and 13 762 reported on antenatal care, 22 242 and 13 817 on place of birth and 22 145 and 13 810 on caesarean section in the 2007 and 2013 surveys, respectively. The proportions of births represented by the Mtwara region and the Makonde ethnic group were higher in the 2013 survey than in the 2007 survey (Table 1). In general, compared with those interviewed in the 2013 survey, the women interviewed in the 2007 survey were living in poorer households, less educated and of higher parity and lived further from any health facility providing delivery care in the study area (median: 2.7 km in 2007 vs 2.2 km in 2013; Fig. 1). The median distance to a hospital was 18.0 km in both surveys (Fig. 2).
Table 1. Characteristics of the female subjects of a two-survey study of access to maternity care, United Republic of Tanzania, 2007 and 2013.
| Characteristic | No. (%) of subjectsa |
Pb | |
|---|---|---|---|
| 2007 survey (n = 22 243) | 2013 survey (n = 13 820) | ||
| Region | < 0.001 | ||
| Lindi | 13 107 (59) | 7131 (49) | |
| Mtwara | 9136 (41) | 6689 (51) | |
| Ethnic group | < 0.001 | ||
| Makonde | 11 989 (54) | 8010 (60) | |
| Other | 10 254 (46) | 5804 (40) | |
| Household wealth quintilec | < 0.001 | ||
| Most poor | 3331 (15) | 1804 (13) | |
| Very poor | 3963 (18) | 2556 (18) | |
| Poor | 4631 (21) | 2810 (20) | |
| Less poor | 4710 (21) | 3025 (22) | |
| Least poor | 4722 (21) | 3426 (25) | |
| Data missing | 886 (4) | 199 (2) | |
| Education | < 0.001 | ||
| None | 6434 (29) | 2744 (20) | |
| Some primary | 3298 (15) | 1579 (11) | |
| Completed primary | 12 367 (56) | 9362 (68) | |
| Secondary or higher | 45 (0.2) | 78 (1) | |
| Data missing | 99 (1) | 57 (0.4) | |
| Occupation | < 0.001 | ||
| Subsistence farmer | 20 959 (94) | 12 829 (93) | |
| Other | 895 (4) | 792 (6) | |
| Data missing | 389 (2) | 199 (2) | |
| Parity | < 0.001 | ||
| 1 | 5206 (23) | 4252 (31) | |
| 2–3 | 9835 (44) | 5398 (39) | |
| 4–6 | 4693 (21) | 3068 (22) | |
| > 6 | 2506 (11) | 1100 (8) | |
| Age, years | < 0.001 | ||
| < 20 | 3193 (14) | 2431 (18) | |
| 20–29 | 10 747 (48) | 6066 (44) | |
| 30–39 | 6684 (30) | 4189 (30) | |
| 40–49 | 1619 (7) | 1134 (8) | |
| Distance to nearest primary facility, kmd | < 0.001 | ||
| < 1.0 | 5472 (27) | 4366 (34) | |
| 1.0– < 2.5 | 2989 (15) | 2415 (19) | |
| 2.5– < 5.0 | 5663 (28) | 3915 (30) | |
| 5.0– < 7.5 | 2868 (14) | 1681 (13) | |
| ≥ 7.5 | 1056 (5) | 447 (3) | |
| Missing data | 2223 (11) | 189 (2) | |
| Distance to nearest hospital, km | < 0.001 | ||
| < 5.0 | 1838 (8) | 949 (7) | |
| 5.0– < 10.0 | 2420 (11) | 1767 (13) | |
| 10.0– < 15.0 | 3646 (16) | 2684 (19) | |
| 15.0– < 25.0 | 7174 (32) | 5099 (39) | |
| 25.0– < 35.0 | 3681 (17) | 2268 (17) | |
| ≥ 35.0 | 1261 (6) | 864 (5) | |
| Missing data | 2223 (10) | 189 (1) | |
a All the subjects were women of reproductive age who reported giving birth in the 12 months before the survey. All of the percentages for 2013 were computed taking sampling weights into consideration.
b For each characteristic, the significance of the between-survey difference was investigated in a χ2 test.
c There are not equal numbers of subjects from each quintile because, in our study population, the mean number of women of reproductive age per household tended to increase with increasing household wealth.
d Excluding the mothers whose nearest facility was a hospital.
Fig. 1.
Distances to the nearest health facility providing delivery care for women in the five study districts, United Republic of Tanzania, 2013
Notes: Distances from home to the nearest facility providing delivery care were evaluated for 3114, 1564, 2437, 2907, and 3609 households in Lindi Rural, Ruangwa, Nachingwea, Newala, and Tandahimba districts, respectively. In these box-and-whisker plots, the horizontal bars, boxes, whiskers and dots indicate medians, interquartile ranges, minimum and maximum values – excluding outliers – and outliers, respectively.
Fig. 2.
Distances to the nearest hospital providing delivery care for women in the five study districts, United Republic of Tanzania, 2013
Notes: Distances from home to the nearest facility providing delivery care were evaluated for 3114, 1564, 2437, 2907, and 3609 households in Lindi Rural, Ruangwa, Nachingwea, Newala, and Tandahimba districts, respectively In these box-and-whisker plots, the horizontal bars, boxes, whiskers and dots indicate medians, interquartile ranges, minimum and maximum values – excluding outliers – and outliers, respectively.
Coverage with four or more antenatal visits increased only marginally, from 41% (9082/21 959) in 2007 to a weighted value of 45% in 2013 (cPR: 1.1; 95% CI: 1.1–1.1), and there was no association between distance to an antenatal clinic and uptake of such antenatal care in 2007 or 2013 (Table 2). Although the interaction between study year and distance to an antenatal clinic was statistically significant (P = 0.011), the between-survey changes seen in uptake of antenatal care in each distance category were very small.
Table 2. Variation in the uptake of antenatal and maternity care according to the distance to nearest primary facility or hospital at which such care was available, United Republic of Tanzania, 2007 and 2013.
| Type of care, distance to that care,km | Interviewees in 2007/2013a | Uptake of care in 2007/2013, %b | cPR (95% CI) |
aPR(95% CI)c |
Pd | ||||
|---|---|---|---|---|---|---|---|---|---|
| 2007 | 2013 | 2007 | 2013 | Change between 2007 and 2013 | |||||
| Antenatal caree | 0.011 | ||||||||
| < 1.0 | 5971/4560 | 44/46 | Reference | Reference | Reference | Reference | 1.0 (1.0–1.1) | ||
| 1.0– < 2.5 | 3638/2709 | 43/47 | 1.0 (0.9–1.0) | 1.0 (1.0–1.1) | 1.0 (0.9–1.0) | 1.0 (1.0–1.1) | 1.1 (1.0–1.2) | ||
| 2.5– < 5.0 | 6067/4133 | 41/45 | 0.9 (0.9–1.0) | 1.0 (0.9–1.1) | 0.9 (0.9–1.0) | 1.0 (1.0–1.1) | 1.1 (1.1–1.2) | ||
| 5.0– < 7.5 | 3001/1702 | 40/44 | 0.9 (0.9–1.0) | 1.0 (0.9–1.0) | 0.9 (0.9–1.0) | 1.0 (0.9–1.1) | 1.1 (1.0–1.2) | ||
| ≥ 7.5 | 1086/471 | 36/41 | 0.8 (0.8–0.9) | 0.9 (0.8–1.0) | 0.8 (0.7–0.9) | 0.9 (0.8–1.0) | 1.1 (1.0–1.3) | ||
| Missing data | 2196/187 | 40/38 | 0.9 (0.8–1.0) | 0.8 (0.7–1.0) | 0.9 (0.8–1.0) | 0.9 (0.7–1.1) | N/A | ||
| Total | 21 959/13 762 | 41/45 | N/A | N/A | N/A | N/A | 1.1(1.1–1.1) | ||
| Delivery in primary facility | < 0.001 | ||||||||
| < 1.0 | 5472/4364 | 22/50 | Reference | Reference | Reference | Reference | 2.3 (2.1–2.5) | ||
| 1.0– < 2.5 | 2989/2415 | 13/42 | 0.6 (0.5–0.7) | 0.8 (0.8–0.9) | 0.6 (0.5–0.7) | 0.8 (0.8–0.9) | 3.4 (3.0–3.9) | ||
| 2.5– < 5.0 | 5663/3914 | 8/35 | 0.3 (0.3–0.4) | 0.7 (0.7–0.8) | 0.3 (0.3–0.4) | 0.7 (0.6–0.8) | 4.8 (4.2–5.6) | ||
| 5.0– < 7.5 | 2867/1681 | 7/35 | 0.3 (0.2–0.4) | 0.7 (0.6–0.8) | 0.3 (0.2–0.4) | 0.7 (0.6–0.8) | 5.3 (4.2–6.6) | ||
| ≥ 7.5 | 1056/447 | 6/28 | 0.3 (0.2–0.4) | 0.6 (0.4–0.7) | 0.3 (0.2–0.4) | 0.6 (0.5–0.7) | 4.1 (2.7–6.2) | ||
| Missing data | 2223/189 | 12/30 | 0.6 (0.4–0.7) | 0.6 (0.4–0.9) | 0.6 (0.4–0.7) | 0.6 (0.4–0.9) | N/A | ||
| Total | 20 270/13 010 | 13/41 | N/A | N/A | N/A | N/A | 3.3 (3.1–3.6) | ||
| Delivery in hospital | < 0.001 | ||||||||
| < 5.0 | 1828/949 | 72/88 | Reference | Reference | Reference | Reference | 1.2 (1.1–1.3) | ||
| 5.0– < 10.0 | 2420/1767 | 34/57 | 0.5 (0.4–0.5) | 0.7 (0.6–0.7) | 0.6 (0.5–0.6) | 0.7 (0.7–0.8) | 1.6 (1.5–1.8) | ||
| 10.0– < 15.0 | 3646/2683 | 26/41 | 0.4 (0.3–0.4) | 0.5 (0.4–0.5) | 0.5 (0.4–0.5) | 0.5 (0.5–0.6) | 1.5 (1.4–1.7) | ||
| 15.0– < 25.0 | 7173/5099 | 22/33 | 0.3 (0.3–0.3) | 0.4 (0.4–0.4) | 0.4 (0.4–0.4) | 0.4 (0.4–0.5) | 1.4 (1.3–1.5) | ||
| 25.0– < 35.0 | 3681/2267 | 23/27 | 0.3 (0.3–0.4) | 0.3 (0.3–0.3) | 0.4 (0.4–0.4) | 0.3 (0.3–0.4) | 1.1 (1.0–1.3) | ||
| ≥ 35.0 | 1261/863 | 21/22 | 0.3 (0.3–0.3) | 0.3 (0.2–0.3) | 0.3 (0.3–0.4) | 0.3 (0.2–0.3) | 0.9 (0.7–1.1) | ||
| Missing data | 2223/189 | 30/47 | 0.4 (0.4–0.5) | 0.5 (0.4–0.7) | 0.5 (0.4–0.6) | 0.6 (0.5–0.8) | N/A | ||
| Total | 22 242/13 817 | 29/40 | N/A | N/A | N/A | N/A | 1.3 (1.2–1.4) | ||
| Birth by caesarean section | 0.208 | ||||||||
| < 5.0 | 1833/949 | 8.0/12.6 | Reference | Reference | Reference | Reference | 1.5 (1.2–1.9) | ||
| 5.0– < 10.0 | 2415/1764 | 5.1/8.0 | 0.6 (0.5–0.8) | 0.6 (0.5–0.8) | 0.9 (0.7–1.1) | 0.7 (0.6–0.9) | 1.5 (1.2–1.9) | ||
| 10.0– < 15.0 | 3636/2683 | 3.9/6.3 | 0.5 (0.4–0.6) | 0.5 (0.4–0.6) | 0.7 (0.5–0.8) | 0.6 (0.5–0.7) | 1.5 (1.2–1.9) | ||
| 15.0– < 25.0 | 7136/5097 | 3.8/6.1 | 0.5 (0.4–0.6) | 0.5 (0.4–0.6) | 0.7 (0.5–0.8) | 0.6 (0.5–0.7) | 1.5 (1.2–1.7) | ||
| 25.0– < 35.0 | 3658/2264 | 2.9/5.3 | 0.4 (0.3–0.5) | 0.4 (0.3–0.5) | 0.5 (0.4–0.6) | 0.5 (0.4–0.6) | 1.8 (1.4–2.3) | ||
| ≥ 35.0 | 1254/864 | 2.8/3.3 | 0.4 (0.2–0.5) | 0.3 (0.2–0.4) | 0.5 (0.3–0.8) | 0.3 (0.2–0.4) | 1.0 (0.6–1.7) | ||
| Missing data | 2213/189 | 4.0/8.9 | 0.5 (0.4–0.7) | 0.7 (0.4–1.2) | 0.7 (0.5–0.9) | 0.8 (0.5–1.4) | N/A | ||
| Total | 22 145/13 810 | 4.1/6.5 | N/A | N/A | N/A | N/A | 1.5 (1.3–1.6) | ||
aPR: adjusted prevalence ratio; CI: confidence interval; cPR: crude prevalence ratio; N/A: not applicable.
a Women of reproductive age who reported giving birth in the previous 12 months.
b All of the percentages for 2013 were computed taking sampling weights into consideration.
c Adjusted for the mother’s age, parity, district of residence, education, ethnic group and occupation and her household’s wealth quintile.
d For the interaction between distance to facility and survey year, as assessed in likelihood ratio tests.
e At least four visits.
Table 2 summarizes the cPRs and adjusted PRs (aPR). After excluding the data for areas where a hospital is the nearest facility, the proportion of births occurring in primary facilities increased from 13% (2546/20 270) in 2007 to a weighted value of 41% in 2013 (aPR: 3.3). The proportion of births occurring in hospitals also increased, from 29% (6475/22 242) in 2007 to a weighted value of 40% in 2013 (aPR: 1.3). In both surveys, the distance to a primary facility was strongly associated with delivery in a primary facility. The between-survey increases in the proportion of births occurring in primary facilities were most pronounced among the women who lived relatively far away from a primary facility (P < 0.001; Table 2). For example, for those living less than 1.0 km from a primary facility, the proportion of births that occurred in such a facility increased from 22% (1219/5472) in 2007 to a weighted value of 50% in 2013 (aPR: 2.3). The corresponding values for those living at least 7.5 km from a primary facility were 6% (63/1056) and 28%, respectively (aPR: 4.1). In contrast, the between-survey increases in the proportion of births occurring in hospitals were greatest for those living at least 5.0 km, but less than 10.0 km from a hospital – 34% (824/2420) versus a weighted value of 57% (aPR: 1.6) – or at least 10.0 km but no more than 15.0 km from a hospital – 26% (960/3646) versus a weighted value of 41% (aPR: 1.5) (Table 2).
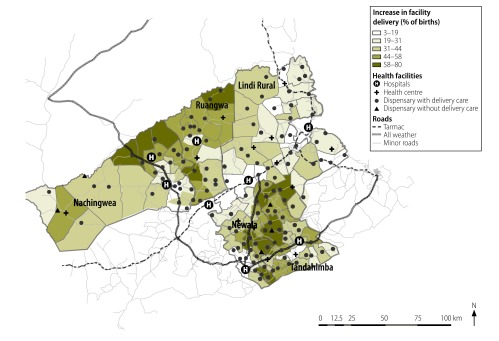
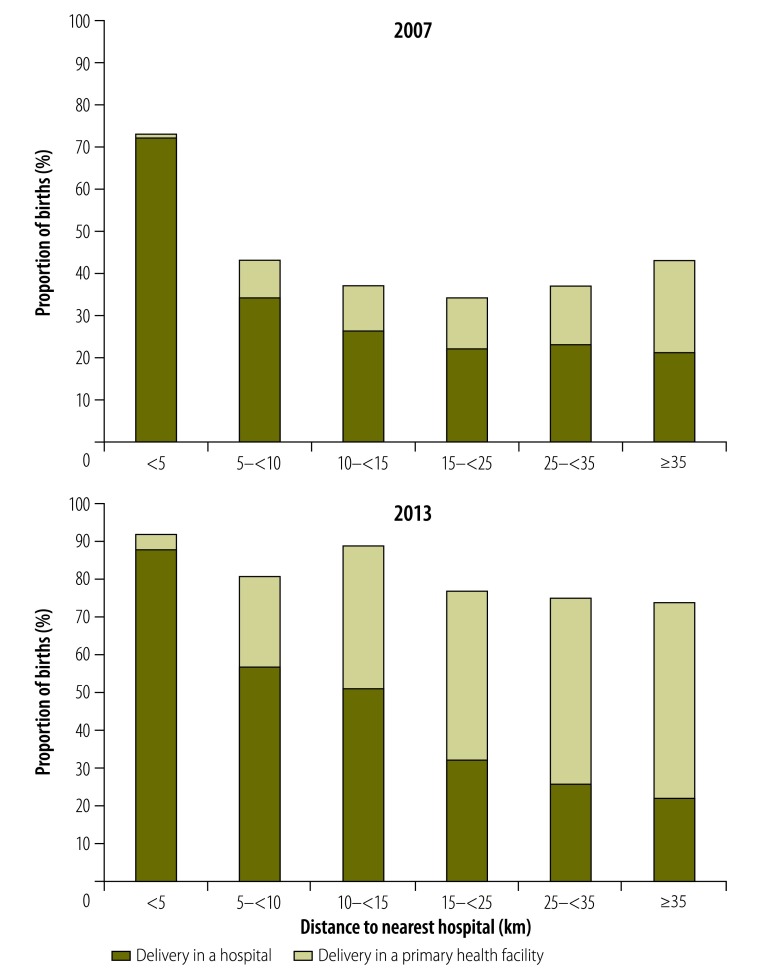
Overall, the proportion of women giving birth in any health facility, whether it was a primary facility or a hospital, increased from 41% (9021/22 242) in 2007 to a weighted value of 79% in 2013. The greatest absolute increase was seen in the rural, remote wards that were at least 10.0 km from a hospital (Fig. 3). The share of births occurring in primary facilities increased with the distance to the nearest hospital. In terms of the weighted proportions for 2013, only 4% of the women living very close to a hospital – i.e. at a distance of less than 5.0 km – gave birth in a primary facility. The corresponding proportions for the women living at least 25.0 km but less than 35.0 km and more than 35.0 km from their nearest hospital were much greater: 49% and 52%, respectively (Fig. 4).
Fig. 3.
Ward map of the five study districts showing the increases in facility deliveries, United Republic of Tanzania, 2007–2013
Notes: The map, which shows the percentage increase in the proportions of births in the previous 12 months that were facility deliveries, is based on data collected in interviews with 22 243 women in 2007 and 13 833 in 2013. All of the percentages for 2013 were computed taking sampling weights into consideration.
Fig. 4.
Changes in the proportions of births occurring in a health facility according to distance to nearest hospital, United Republic of Tanzania, 2007 and 2013
Note: All of the percentages for 2013 were computed taking sampling weights into consideration.
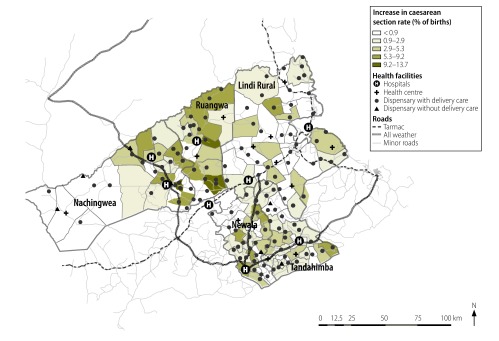
The proportion of births represented by caesarean sections increased from 4.1% (913/22 145) in 2007 to a weighted value of 6.5% in 2013. The level of increase in the frequency of caesarean sections appeared unaffected by the distance to the nearest hospital (P = 0.208; Table 2; Fig. 5) even though, in both surveys, there was a strong negative association between distance to the nearest hospital and delivery by caesarean section. For the women living more than 35.0 km from their nearest hospital, there was no between-survey increase in the proportion of births represented by caesarean sections (aPR: 1.0; Table 2).
Fig. 5.
Ward map of the five study districts showing the increases in caesarean sections, United Republic of Tanzania, 2007–2013
Notes: The map, which shows the percentage increase in the proportions of births in the previous 12 months that involved caesarean sections, is based on data collected in interviews with 22 243 women in 2007 and 13 833 in 2013. All of the percentages for 2013 were computed taking sampling weights into consideration.
Discussion
The data presented here provide evidence of substantial increases, between 2007 and 2013, in the proportion of births in the study area, represented by deliveries in primary facilities and hospitals. The large increase we observed in facility births is consistent with findings from other Tanzanian studies.18,33,34 The increased uptake of delivery in primary facilities for women who live in the more remote areas, often far from a hospital, is particularly noteworthy. The increase probably indicates that the national policy to improve access to maternity care – by promoting delivery care in primary facilities and further increasing the number of such facilities – is being successful.23,35 The United Republic of Tanzania’s substantial socioeconomic development,36 including improvements in the road network, may have helped women to travel moderate distances while seeking maternity care. Also, two projects to support birth preparedness, at community level, may also have had a beneficial impact in the study area.25,37
While we may have seen an important reduction in the inequality of geographical access to primary care for childbirth, there appeared to be little between-survey improvement in access to hospital-based delivery care or caesarean sections. In our study area, the district hospitals are expected to send ambulances to dispensaries, to collect patients who need emergency hospital care. However, such emergency referrals are severely constrained by lack of funds at district level to pay for the fuel, maintenance and repairs needed to keep ambulances on the road.37 In addition, only three of the hospitals serving the study area had maternity waiting homes.
While the optimal caesarean section rate remains a matter of controversy,38–41 rates of about 3% – as seen in the more remote settings in our study area – are far too low to meet the needs of pregnant women and their babies.
The persistently low uptake of antenatal care by Tanzanian women has been noted previously.42 In our study, distance to a facility had no apparent effect on uptake of such care. This observation is in line with findings from Zambia,15 but conflicts with the results of an earlier study in the United Republic of Tanzania.35 However, this earlier study did not include dispensaries, which are the main providers of antenatal care in the country.35 As the World Health Organization has now increased the recommended number of antenatal visits to at least eight,43 it is, perhaps, even more important to examine the reasons for the suboptimal levels of antenatal care seen in the United Republic of Tanzania.44
Our study had several strengths, including its reliance on two large representative datasets from, effectively, the same study population and the use of the same questionnaire and a short recall period in both surveys. However, there may be limitations. First, the use of straight-line distance to a facility, to evaluate geographical accessibility, is sometimes regarded as inferior to calculating travel time45 – although this depends on the setting.46 The results of a Tanzanian study in which topographic maps were used to estimate travel time47 indicated that, at least in the United Republic of Tanzania, straight-line distances may correlate fairly well with travel times. Second, our analysis is based on a full census of the study area in 2007 but only a sample survey in 2013. Despite adjusting our estimates to take account of this difference between the surveys, we still found unanticipated and unexpected differences between the composition of the study population in 2007 and that of the study population in 2013. These differences, however, can probably be attributed to migration and other demographic changes26 rather than to our sampling procedure. Third, our 2007 data came from women who differed, in terms of three known drivers of the uptake of facility care –i.e. age, education and parity48 – from the women who provided our data in 2013. We did, however, make adjustments in our data analyses for each of these potential confounders. Lastly, we used prevalence ratios to estimate the strength of the effect of distance to the nearest facility on uptake of care. While this improves the ease of interpretation, it also increases confidence intervals.32
The increased uptake of facility births in our study area is encouraging. However, our analysis indicates that this increase did not translate into a substantial concurrent increase in caesarean sections. A plausible explanation is the lack of a functioning link between primary and secondary facilities, especially poor emergency referral from the primary facilities. We believe that our findings – together with existing evidence on deficits in the quality of care in primary facilities and on the high levels of neonatal mortality in our study area and other parts of the United Republic of Tanzania25,27,28,33 – indicate a need to revisit the policy of providing maternity care in primary facilities that are not linked to hospitals through a functioning referral system. Intrapartum care, in East Africa and elsewhere, needs to be strengthened by improvements in the quality of care and referral systems.49
Acknowledgements
CH, JS and CR have dual appointments with The Centre for Maternal, Adolescent, Reproductive, and Child Health, London School of Hygiene and Tropical Medicine, England. CH also has a dual appointment with the Department of Public Health Sciences, Karolinska Institutet, Solna, Sweden.
Funding:
Data collection in 2007 was supported by a grant from the Bill & Melinda Gates Foundation through the intermittent preventive treatment of malaria in infants consortium. The survey in 2013 was funded through another grant from the Bill & Melinda Gates Foundation, awarded to Save the Children.
Competing interest:
None declared.
References
- 1.Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. ; United Nations Maternal Mortality Estimation Inter-Agency Group collaborators and technical advisory group. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. 2016. January 30;387(10017):462–74. 10.1016/S0140-6736(15)00838-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levels and trends in child mortality. Report 2015. Estimates developed by the UN Inter-agency Group for Child Mortality Estimation. New York: United Nations Children’s Fund; 2015. Available from: http://www.childmortality.org/files_v20/download/igme%20report%202015%20child%20mortality%20final.pdf [cited 2017 Oct 10].
- 3.Building a future for women and children. The 2012 report. New York: United Nations Children’s Fund; 2012. Available from: https://www.unicef.org/eapro/Countdown_to_2015.pdf [cited 2017 Oct 10].
- 4.Jolly R, Kamunvi F, King M, Sebuliba P, editors. The economy of a district hospital. Oxford: Oxford University Press; 1966. [Google Scholar]
- 5.Tatem AJ, Campbell J, Guerra-Arias M, de Bernis L, Moran A, Matthews Z. Mapping for maternal and newborn health: the distributions of women of childbearing age, pregnancies and births. Int J Health Geogr. 2014. January 4;13(1):2. 10.1186/1476-072X-13-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gabrysch S, Cousens S, Cox J, Campbell OMR. The influence of distance and level of care on delivery place in rural Zambia: a study of linked national data in a geographic information system. PLoS Med. 2011. January 25;8(1):e1000394. 10.1371/journal.pmed.1000394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Målqvist M, Sohel N, Do TT, Eriksson L, Persson L-A. Distance decay in delivery care utilisation associated with neonatal mortality. A case referent study in northern Vietnam. BMC Public Health. 2010. December 13;10(1):762. 10.1186/1471-2458-10-762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gage AJ. Barriers to the utilization of maternal health care in rural Mali. Soc Sci Med. 2007. October;65(8):1666–82. 10.1016/j.socscimed.2007.06.001 [DOI] [PubMed] [Google Scholar]
- 9.Gage AJ, Guirlène Calixte M. Effects of the physical accessibility of maternal health services on their use in rural Haiti. Popul Stud (Camb). 2006. November;60(3):271–88. 10.1080/00324720600895934 [DOI] [PubMed] [Google Scholar]
- 10.Mwaliko E, Downing R, O’Meara W, Chelagat D, Obala A, Downing T, et al. “Not too far to walk”: the influence of distance on place of delivery in a western Kenya health demographic surveillance system. BMC Health Serv Res. 2014. May 10;14(1):212. 10.1186/1472-6963-14-212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mpembeni RN, Killewo JZ, Leshabari MT, Massawe SN, Jahn A, Mushi D, et al. Use pattern of maternal health services and determinants of skilled care during delivery in southern Tanzania: implications for achievement of MDG-5 targets. BMC Pregnancy Childbirth. 2007. December 6;7(1):29. 10.1186/1471-2393-7-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ruktanonchai CW, Ruktanonchai NW, Nove A, Lopes S, Pezzulo C, Bosco C, et al. Equality in maternal and newborn health: modelling geographic disparities in utilisation of care in five East African countries. PLoS One. 2016. August 25;11(8):e0162006. 10.1371/journal.pone.0162006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hanson C, Cox J, Mbaruku G, Manzi F, Gabrysch S, Schellenberg D, et al. Maternal mortality and distance to facility-based obstetric care in rural southern Tanzania: a secondary analysis of cross-sectional census data in 226 000 households. Lancet Glob Health. 2015. July;3(7):e387–95. 10.1016/S2214-109X(15)00048-0 [DOI] [PubMed] [Google Scholar]
- 14.Simkhada B, Teijlingen ER, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. 2008. February;61(3):244–60. 10.1111/j.1365-2648.2007.04532.x [DOI] [PubMed] [Google Scholar]
- 15.Kyei NNA, Campbell OMR, Gabrysch S. The influence of distance and level of service provision on antenatal care use in rural Zambia. PLoS One. 2012;7(10):e46475. 10.1371/journal.pone.0046475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hounton S, Chapman G, Menten J, De Brouwere V, Ensor T, Sombié I, et al. Accessibility and utilisation of delivery care within a Skilled Care Initiative in rural Burkina Faso. Trop Med Int Health. 2008. July;13 Suppl 1:44–52. 10.1111/j.1365-3156.2008.02086.x [DOI] [PubMed] [Google Scholar]
- 17.Afnan-Holmes H, Magoma M, John T, Levira F, Msemo G, Armstrong CE, et al. ; Tanzanian Countdown Country Case Study Group. Tanzania’s countdown to 2015: an analysis of two decades of progress and gaps for reproductive, maternal, newborn, and child health, to inform priorities for post-2015. Lancet Glob Health. 2015. July;3(7):e396–409. 10.1016/S2214-109X(15)00059-5 [DOI] [PubMed] [Google Scholar]
- 18.Tanzania demographic and health survey and malaria indicator survey (TDHS-MIS) 2015-16. Rockville: ICF International, 2016. Available from: https://dhsprogram.com/pubs/pdf/FR321/FR321.pdf [cited 2017 Oct 10].
- 19.Kruk ME, Mbaruku G. Public health successes and frail health systems in Tanzania. Lancet Glob Health. 2015. July;3(7):e348–9. 10.1016/S2214-109X(15)00036-4 [DOI] [PubMed] [Google Scholar]
- 20.Jonsson U. Ideological framework and health development in Tanzania 1961-2000. Soc Sci Med. 1986;22(7):745–53. 10.1016/0277-9536(86)90226-1 [DOI] [PubMed] [Google Scholar]
- 21.Gilson L. Management and health care reform in sub-Saharan Africa. Soc Sci Med. 1995. March;40(5):695–710. 10.1016/0277-9536(95)80013-A [DOI] [PubMed] [Google Scholar]
- 22.United Republic of Tanzania. Primary Health Service Development Programme 2007-2017 (MAMM). Dar es Salaam: Ministry of Health and Social Welfare; 2007. [Google Scholar]
- 23.Reproductive and Child Health Section. Focused antenatal care, malaria and syphilis in pregnancy. Orientation package for service providers. Dar es Salaam: Ministry of Health; 2002. [Google Scholar]
- 24.Schellenberg JR, Maokola W, Shirima K, Manzi F, Mrisho M, Mushi A, et al. Cluster-randomized study of intermittent preventive treatment for malaria in infants (IPTi) in southern Tanzania: evaluation of impact on survival. Malar J. 2011. December 30;10(1):387. 10.1186/1475-2875-10-387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hanson C, Manzi F, Mkumbo E, Shirima K, Penfold S, Hill Z, et al. Effectiveness of a home-based counselling strategy on neonatal care and survival: a cluster-randomised trial in six districts of rural southern Tanzania. PLoS Med. 2015. September 29;12(9):e1001881. 10.1371/journal.pmed.1001881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.2012 population and housing census. Dar es Salaam: National Bureau of Statistics; 2013. [Google Scholar]
- 27.Hanson C, Ronsmans C, Penfold S, Maokola W, Manzi F, Jaribu J, et al. Health system support for childbirth care in southern Tanzania: results from a health facility census. BMC Res Notes. 2013. October 30;6(1):435. 10.1186/1756-0500-6-435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Penfold S, Shamba D, Hanson C, Jaribu J, Manzi F, Marchant T, et al. Staff experiences of providing maternity services in rural southern Tanzania - a focus on equipment, drug and supply issues. BMC Health Serv Res. 2013. February 14;13(1):61. 10.1186/1472-6963-13-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baker U, Hassan F, Hanson C, Manzi F, Marchant T, Swartling Peterson S, et al. Unpredictability dictates quality of maternal and newborn care provision in rural Tanzania-a qualitative study of health workers’ perspectives. BMC Pregnancy Childbirth. 2017. February 6;17(1):55. 10.1186/s12884-017-1230-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shirima K, Mukasa O, Schellenberg JA, Manzi F, John D, Mushi A, et al. The use of personal digital assistants for data entry at the point of collection in a large household survey in southern Tanzania. Emerg Themes Epidemiol. 2007. June 1;4(1):5. 10.1186/1742-7622-4-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography. 2001. February;38(1):115–32. [DOI] [PubMed] [Google Scholar]
- 32.Santos CA, Fiaccone RL, Oliveira NF, Cunha S, Barreto ML, do Carmo MB, et al. Estimating adjusted prevalence ratio in clustered cross-sectional epidemiological data. BMC Med Res Methodol. 2008. December 16;8(1):80. 10.1186/1471-2288-8-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fogliati P, Straneo M, Brogi C, Fantozzi PL, Salim RM, Msengi HM, et al. How can childbirth care for the rural poor be improved? A contribution from spatial modelling in rural Tanzania. PLoS One. 2015. September 30;10(9):e0139460. 10.1371/journal.pone.0139460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kruk ME, Hermosilla S, Larson E, Mbaruku GM. Bypassing primary care clinics for childbirth: a cross-sectional study in the Pwani region, United Republic of Tanzania. Bull World Health Organ. 2014. April 1;92(4):246–53. 10.2471/BLT.13.126417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tanzania service provision assessment survey 2014-2015. Rockville: ICF International; 2016. Available from: https://dhsprogram.com/pubs/pdf/SPA22/SPA22.pdf [cited 2017 Oct 10].
- 36.The World Bank in Tanzania [Internet]. Washington: World Bank; 2016. Available from: http://www.worldbank.org/en/country/tanzania [cited 2017 Feb 10].
- 37.Waiswa P, Manzi F, Mbaruku G, Rowe AK, Marx M, Tomson G, et al. ; EQUIP study team. Effects of the EQUIP quasi-experimental study testing a collaborative quality improvement approach for maternal and newborn health care in Tanzania and Uganda. Implement Sci. 2017. July 18;12(1):89. 10.1186/s13012-017-0604-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Molina G, Weiser TG, Lipsitz SR, Esquivel MM, Uribe-Leitz T, Azad T, et al. Relationship between cesarean delivery rate and maternal and neonatal mortality. JAMA. 2015. December 1;314(21):2263–70. 10.1001/jama.2015.15553 [DOI] [PubMed] [Google Scholar]
- 39.Betran AP, Torloni MR, Zhang J, Ye J, Mikolajczyk R, Deneux-Tharaux C, et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod Health. 2015. June 21;12(1):57. 10.1186/s12978-015-0043-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ye J, Zhang J, Mikolajczyk R, Torloni MR, Gülmezoglu AM, Betran AP. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: a worldwide population-based ecological study with longitudinal data. BJOG. 2016. April;123(5):745–53. 10.1111/1471-0528.13592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ye J, Betrán AP, Guerrero Vela M, Souza JP, Zhang J. Searching for the optimal rate of medically necessary cesarean delivery. Birth. 2014. September;41(3):237–44. 10.1111/birt.12104 [DOI] [PubMed] [Google Scholar]
- 42.Gupta S, Yamada G, Mpembeni R, Frumence G, Callaghan-Koru JA, Stevenson R, et al. Factors associated with four or more antenatal care visits and its decline among pregnant women in Tanzania between 1999 and 2010. PLoS One. 2014. July 18;9(7):e101893. 10.1371/journal.pone.0101893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization; 2016. [PubMed] [Google Scholar]
- 44.Callaghan-Koru JA, McMahon SA, Chebet JJ, Kilewo C, Frumence G, Gupta S, et al. A qualitative exploration of health workers’ and clients’ perceptions of barriers to completing four antenatal care visits in Morogoro region, Tanzania. Health Policy Plan. 2016. October;31(8):1039–49. 10.1093/heapol/czw034 [DOI] [PubMed] [Google Scholar]
- 45.Noor AM, Amin AA, Gething PW, Atkinson PM, Hay SI, Snow RW. Modelling distances travelled to government health services in Kenya. Trop Med Int Health. 2006. February;11(2):188–96. 10.1111/j.1365-3156.2005.01555.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nesbitt RC, Gabrysch S, Laub A, Soremekun S, Manu A, Kirkwood BR, et al. Methods to measure potential spatial access to delivery care in low- and middle-income countries: a case study in rural Ghana. Int J Health Geogr. 2014. June 26;13(1):25. 10.1186/1476-072X-13-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Straneo M, Fogliati P, Azzimonti G, Mangi S, Kisika F. Where do the rural poor deliver when high coverage of health facility delivery is achieved? Findings from a community and hospital survey in Tanzania. PLoS One. 2014. December 2;9(12):e113995. 10.1371/journal.pone.0113995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gabrysch S, Campbell OM. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. 2009. August 11;9(1):34. 10.1186/1471-2393-9-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Campbell OMR, Calvert C, Testa A, Strehlow M, Benova L, Keyes E, et al. The scale, scope, coverage, and capability of childbirth care. Lancet. 2016. October 29;388(10056):2193–208. 10.1016/S0140-6736(16)31528-8 [DOI] [PubMed] [Google Scholar]