Abstract
Traumatic glenohumeral dislocations often result in significant injury to the anterior-inferior labrum, most commonly leading to recurrent anterior instability. While in skeletally immature patients, shoulder trauma more commonly results in fracture versus a true dislocation, shoulder instability does occur and can be difficult to manage in the setting of open physes. In any event, the goal of treatment is to reduce the risk of recurrence and allow full participation in activities, including sports. Arthroscopic stabilization has been shown to be an effective treatment option for young patients, with good return to sport rates; however, the vast majority of literature on shoulder instability in the youth patient population focuses on anterior instability. Concomitant lesions of the anterior, posterior, and superior labrum have been rarely described in youth athletes and present a formidable clinical challenge, particularly in skeletally immature patients. In this Technical Note, we describe the authors' preferred technique for arthroscopic repair of a traumatic triple labral tear, including anterior, posterior, and type IV SLAP components, in adolescent patients.
Acute shoulder dislocations occur at a rate of approximately 35 per 100,000 person-years in male patients.1 Traumatic dislocations often result in significant injury to the anterior-inferior labrum, most commonly leading to recurrent anterior instability.2, 3 When evaluating the adolescent patient with shoulder instability, it is critical to understand the mechanism of action, chronicity of injury (first time event vs recurrent instability), and prior treatment history, as this information will allow for appropriate clinical decision-making. Although skeletally immature patients inherently have greater elasticity of the capsular structures that may respond well to nonoperative measures, including physical therapy,3 multiple studies have reported unacceptably high rates of recurrence in adolescents treated without surgery.4, 5 Favorable outcomes have been reported following arthroscopic stabilization in skeletally immature patients.6
The vast majority of clinical studies on shoulder instability in the youth patient population have evaluated patients with anterior labral tears or multidirectional labral laxity without an isolated labral tear. Concomitant lesions of the anterior, posterior, and superior labrum have been rarely described in youth athletes and present a formidable clinical challenge, particularly in skeletally immature patients.7 In this Technical Note, we describe the authors' preferred technique for arthroscopic repair of a traumatic triple labral tear, including anterior, posterior, and type IV SLAP components, in adolescent patients.
Technique
Patient Positioning and Anesthesia
Following the induction of regional and general anesthesia, the patient was placed in the lateral decubitus position with all bony prominences well padded. An examination under anesthesia was performed, which revealed a 3+ translation on anterior superior, anterior middle, anterior inferior, and posterior load and shift testing. The patient's right shoulder was prepped and draped in the usual sterile fashion. A time-out was called to confirm the correct patient, procedure, operative site and side, and administration of antibiotics.
Diagnostic Arthroscopy
The arthroscope was inserted into a standard posterior portal 2 cm inferior and 1 cm medial to the posterolateral corner of the acromion, and a standard midglenoid anterior portal was established using an outside-in technique through the rotator interval just lateral to the coracoid process. Diagnostic arthroscopy revealed the labrum torn off the glenoid superiorly and subluxated down in a bucket-handle fashion, with the majority of labral tissue still present and with a viable appearance (Fig 1, Video 1). In addition, a type IV SLAP lesion was present, extending along and into the long head of the biceps tendon. The detachment of the labrum extended near-circumferentially around the glenoid, with the exception of a preserved glenoid-labrum attachment between 6 and 7 o'clock. There was no evidence of a humeral avulsion glenohumeral ligament (HAGL) lesion or reverse-HAGL lesion. The rotator cuff was completely intact.
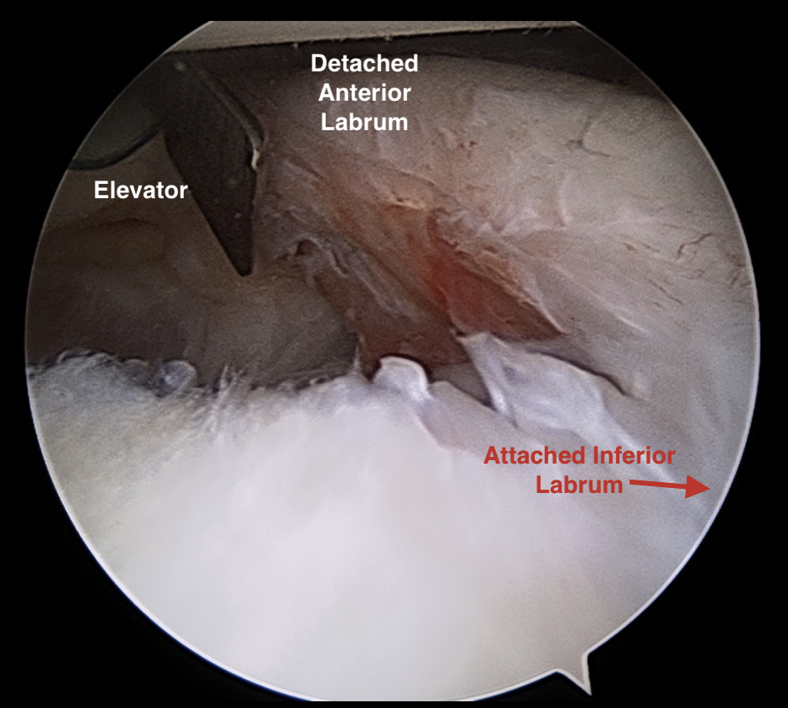
Fig 1.
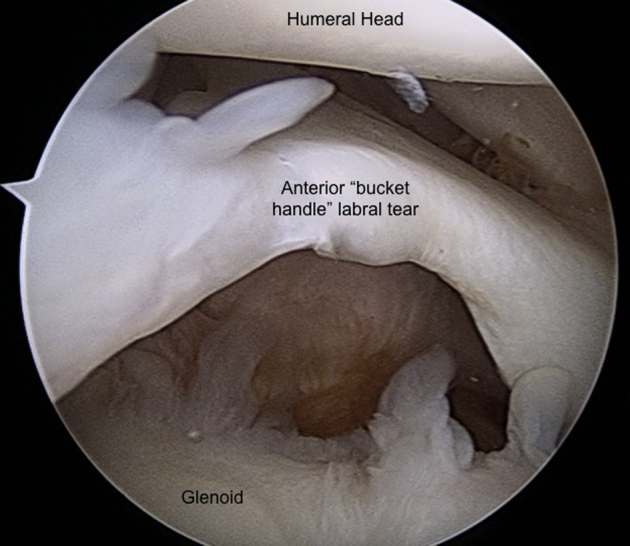
Arthroscopic photograph of the right shoulder demonstrating the bucket-handle-like appearance of the near-circumferential labral tear (viewing from the posterior).
Surgical Technique
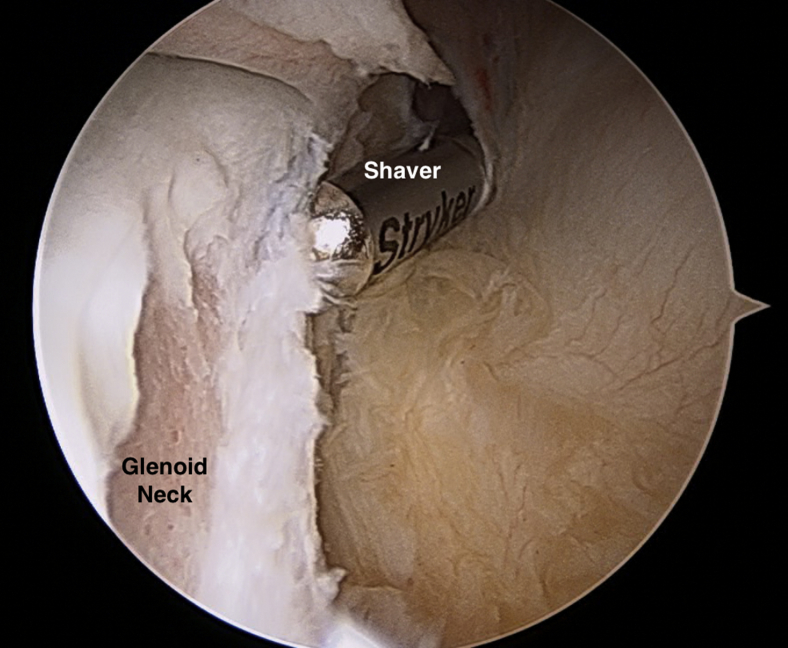
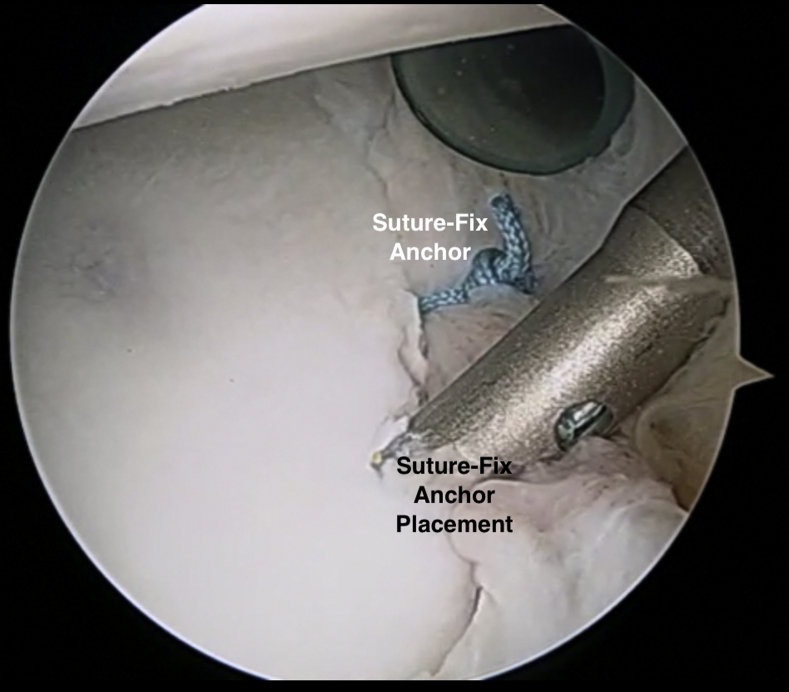
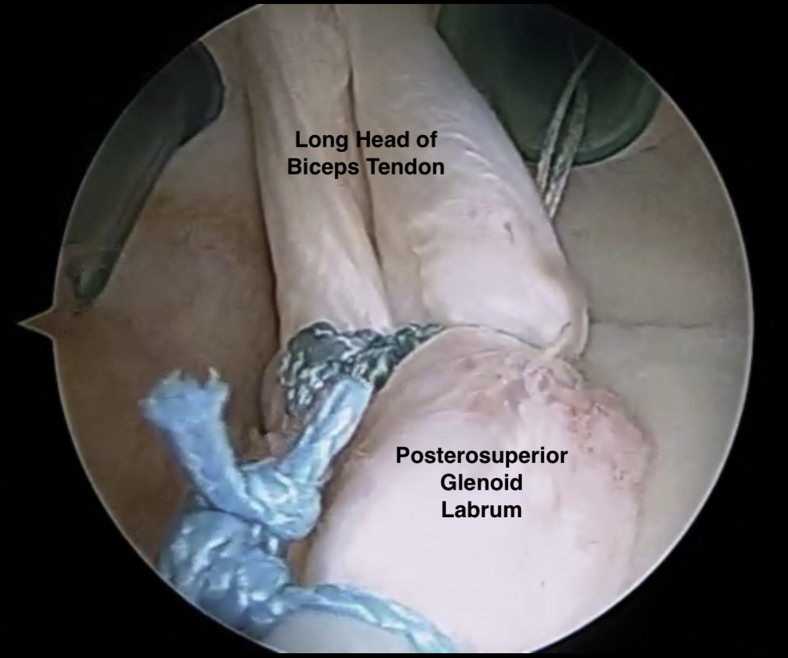
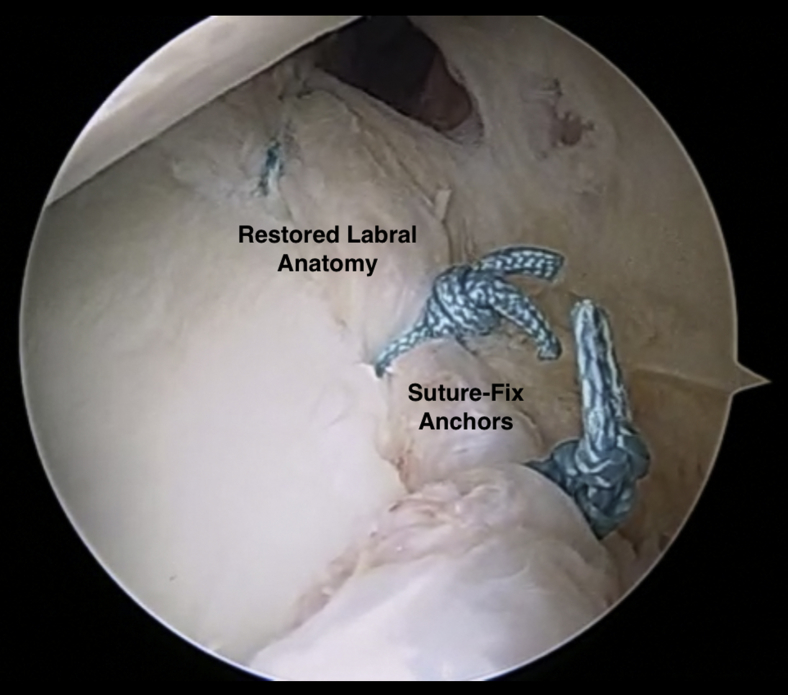
At this point, the decision was made to proceed with the all-arthroscopic repair of this triple labral lesion. First, the neck of the glenoid was abraded to a light bleeding surface anteriorly, superiorly, and posteriorly, using a labral elevator, shaver, and rasp (Figs 2 and 3). Prior to anchor placement, the displaced bucket-handle-like labrum was reduced from the inferior portion of the joint back to the superior portions of the glenoid. The labrum was provisionally held in place with spinal needles placed percutaneously to hold the reduction (Fig 4). Next, suture-fix anchors (Smith and Nephew, Andover, MA) were placed along the glenoid sequentially, beginning anterior-inferiorly and moving from inferior to superior along the anterior aspect of the glenoid (Fig 5). Additional suture anchors were then placed posteriorly along the glenoid, again moving from inferior to superior. For each suture anchor, a spectrum was used for suture passing around the labral tissue, and a standard arthroscopic knot tying technique was used to reduce the labrum back to the glenoid. At this point, the near-circumferential labral lesion was adequately reduced and repaired with the exception of the most superior aspect of the labrum near the biceps anchor insertion, with the lesion now functionally a type II SLAP tear with an associated split in the long head of the biceps tendon. Due to the patient's young age and degree of instability, the decision to fix the superior labrum was made, and 2 additional suture anchors were placed superiorly along the glenoid to repair the SLAP component of the labral tear (Fig 6). At this point, the labrum was completely reduced back to the glenoid and was noted to be essentially anatomic. The stability of the glenohumeral joint was gently assessed, and excellent stability was achieved in the anterior, posterior, and inferior directions.
Fig 2.
Arthroscopic photograph of the right shoulder demonstrating anterior labral preparation with an arthroscopic elevator.
Fig 3.
Arthroscopic photograph of the right shoulder demonstrating anterior labral preparation with an arthroscopic burr.
Fig 4.
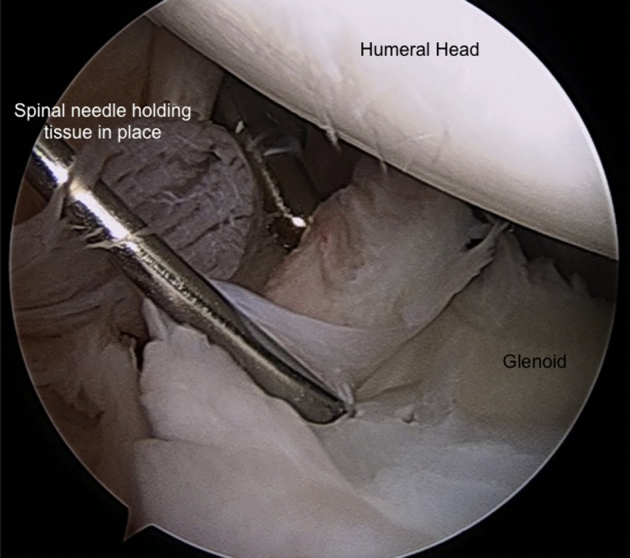
Arthroscopic photograph of the right shoulder demonstrating provisional labral stabilization to the glenoid rim with an 18-g spinal needle.
Fig 5.
Arthroscopic photograph of the right shoulder demonstrating the final appearance of the repaired anterior and posterior labrum following near-circumferential suture-anchor fixation.
Fig 6.
Arthroscopic photograph of the right shoulder demonstrating the split biceps tendon in the setting of the SLAP tear repair.
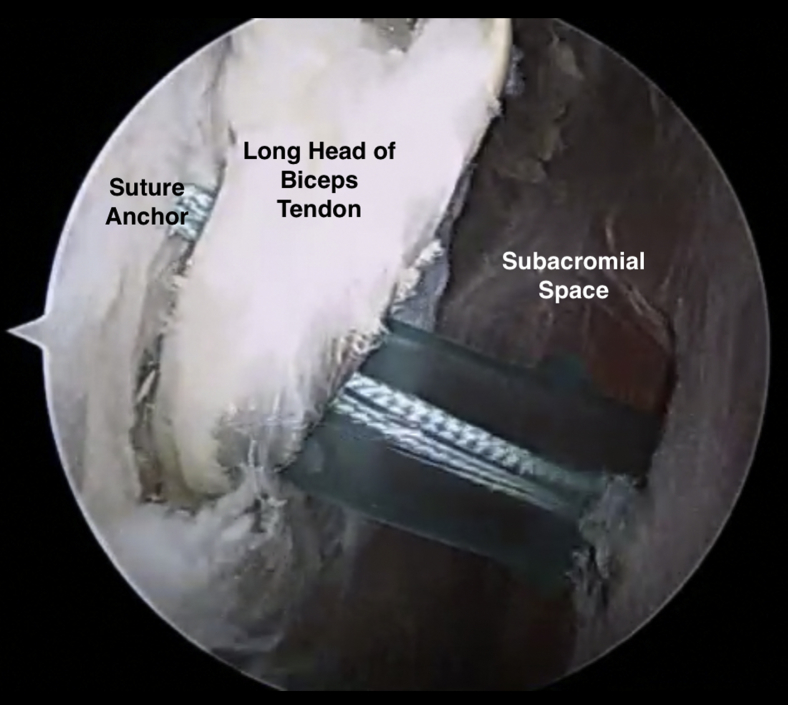
At this point, the long head of the biceps tendon was tagged with a no.1 PDS suture, and attention was turned to the subacromial space. A subacromial bursectomy was performed, allowing for visualization of the biceps tendon. The biceps tendon was carefully unroofed and was tenodesed essentially in situ in the suprapectoral location with 2 1.7 suture fix suture anchors (Smith and Nephew); the sutures from the suture anchors were passed both around and through the biceps tendon and tied with via standard arthroscopic knot-tying techniques (Fig 7). The arthroscope was then inserted back into the glenohumeral joint, and the injured, split portion of the long head of the biceps tendon was cut from its attachment onto the superior labrum (Fig 8). This technique allowed for an anatomic fixation of the long head of the biceps tendon without excessive tension, while at the same time allowing for the removal and debridement of the torn/split intra-articular portion of the biceps tendon.
Fig 7.
Arthroscopic photograph of the right shoulder from the subacromial space demonstrating right shoulder in situ biceps tenodesis prior to biceps tenotomy.
Fig 8.
Arthroscopic photograph of the right shoulder demonstrating the biceps tenotomy following in situ arthroscopic biceps tenodesis.
Rehabilitation
The patient is maintained in an abduction sling for the first 4 to 6 weeks following surgery. Gentle pendulum exercises are permitted on the first post-operative day. Gentle passive shoulder range of motion (ROM) is permitted during the first 4 weeks under the care of a physical therapist. At week 4, active-assist ROM is permitted, progressing to active ROM by week 6, with full ROM expected by week 10. Periscapular strengthening is allowed to gently progress beginning at week 6, and return to contact/collision sports is not permitted until 6 months.
Discussion
In this Technical Note, we describe an arthroscopic technique of a combined anterior, posterior, and superior labral repair with concomitant biceps tenodesis for a near complete traumatic labral separation in a skeletally immature adolescent. In skeletally immature patients, shoulder trauma more commonly results in fracture than a dislocation and labral tear due in part to open physes.3 In the event of a labral tear, the goal of treatment is to reduce the risk of recurrence and allow full participation in activities including sports.8 Arthroscopic stabilization has been shown to be an effective treatment option for young patients with good return-to-sport rates; however, the vast majority of literature regards anterior labral tears.6, 9
Very little literature describing triple labral tears is available, with the largest series to date consisting of 7 patients reported by Lo and Burkhart in 2005.7 In their series, triple labral lesions account for 2.4% of lesions of the glenoid labrum over a 3-year span, with the mean age of patients with this diagnosis being 25 years. All patients had experienced a traumatic onset of symptoms, with only 2 patients having had prior instability surgery. In their series, the authors reported that all patients had a type II SLAP lesion, whereas our patient had a type IV SLAP lesion. Lo and Burkhart treated each patient with suture anchor fixation, with 6 of 7 patients satisfied with their surgical outcome.7
Other authors have published smaller case series of arthroscopic management of labral tears 270° or greater.10 Alpert et al. reported on a cohort of 13 patients with multidirectional instability who were treated using bioabsorbable single-loaded suture anchors (Arthrex, Naples, FL), with 85% either completely or mostly satisfied at mean 56-month follow-up. Twelve of the 13 patients had had discrete trauma prior to onset of symptoms, and 4 patients (31%) experienced more than 2 recurrent instability events.
Pearls and pitfalls of this technique can be found in Table 1, while advantages and disadvantages of the technique can be found in Table 2. Given the severity of his injury, nonoperative measures were highly unlikely to offer any substantial long-term benefit. Ultimately, early surgical intervention with anatomic repair using the technique described can result in a successful outcome.
Table 1.
Pearls and Pitfalls of the Surgical Technique
| Pearls | Pitfalls |
|---|---|
| • Use spinal needles to temporarily reduce the labrum in order to facilitate capsular shift. • Begin the repair inferiorly and work superiorly. • Be prepared to work anteriorly and posteriorly in a back-and = forth fashion to ensure equal capsular tension. |
• It can be difficult to manage this type of global labral tear with malreduction of the labrum. • Suture passage around the bony Bankart portion anteriorly. • Multiple steps are required with portal switching from anterior to posterior in order to check the labrum-capsular tension with repair. |
Table 2.
Advantages and Disadvantages of the Surgical Technique
| Advantages | Disadvantages |
|---|---|
| • All-suture suture anchors provide least intrusion on growth plates and multiple fixation points. • The lateral decubitus position provides excellent exposure to the posterior and inferior quadrants of the shoulder. • Arthroscopic in situ biceps tenodesis ensures anatomic tenodesis and cosmesis. |
• Technically challenging with numerous steps. • Difficult visualization and suture management given the extent of the tear pattern. • Biceps technique requires second step of returning to the glenohumeral joint to remove biceps remnant. |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.W.T. receives support from the Arthroscopy Association of North America, Exactech, OrthoSpace, Rotation Medical, and Smith and Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
A review of preoperative x-rays and magnetic resonance imaging of a young male athlete after sustaining a traumatic dislocation from a motor vehicle accident reveal a bony Bankart lesion with associated labral tear superiorly, anteriorly, and posteriorly. A 3-dimensional computer tomography scan revealed a small Hill-Sachs deformity. This injury was termed a triple labral lesion that was subsequently taken to the operating room for arthroscopic repair. The patient was placed in the lateral decubitus position and a diagnostic arthroscopy was performed. This confirmed the imaging findings of a triple labral lesion as seen through first the posterior portal and then anterior superior portal. A type IV superior labral anterior posterior tear was also found to be present. The labral tissue was gently elevated off the glenoid with use of a Bankart elevator followed by abrasion of the neck of the glenoid using a shaver and arthroscopic grasp. Prior to suture anchor placement, the bucket handle tear of the labrum is reduced from the inferior portion of the joint. At this time suture anchor placement of Suture-Fix anchors (Smith & Nephew, Andover, MA) was initiated sequentially beginning anterior and moving inferior to superior. For each suture anchor placement a Spectum (Conmed, Utica, NY) suture passer was utilized for suture passing around the labral tissue and standard arthroscopic knot techniques were utilized to secure the labrum back to the neck of the glenoid. These steps were repeated for the posterior labral repair. A total of 4 suture anchors were placed anteriorly and 4 were placed posteriorly for adequate reduction. The superior labral anterior posterior tear was then repaired with the lesion reduced to a type II SLAP tear associated with a split in the long head of the biceps tendon. 2 suture anchors were placed to reduce the tear. At this time the anatomic repair was evaluated for stability and found to be secure circumferentially. Attention was then turned to the subacromial space were a bursectomy was performed using an arthroscopic shaver. The biceps tendon was then tenodesed in the suprapectoral location utilizing two 1.7 mm SutureFix anchors (Smith & Nephew). Following tenodesis the arthroscope was reintroduced into the glenohumeral joint and the biceps attachment to the superior labrum was cut. Rehabilitation protocol is noted for return to full-contact athletics at 6 months if full strength and range of motion is achieved.
References
- 1.Zacchilli M.A., Owens B.D. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am. 2010;92:542–549. doi: 10.2106/JBJS.I.00450. [DOI] [PubMed] [Google Scholar]
- 2.Robinson C.M., Seah M., Akhtar M.A. The epidemiology, risk of recurrence, and functional outcome after an acute traumatic posterior dislocation of the shoulder. J Bone Joint Surg Am. 2011;93:1605–1613. doi: 10.2106/JBJS.J.00973. [DOI] [PubMed] [Google Scholar]
- 3.Li X., Ma R., Nielsen N.M., Gulotta L.V., Dines J.S., Owens B.D. Management of shoulder instability in the skeletally immature patient. J Am Acad Orthopaed Surg. 2013;21:529–537. doi: 10.5435/JAAOS-21-09-529. [DOI] [PubMed] [Google Scholar]
- 4.Longo U.G., van der Linde J.A., Loppini M., Coco V., Poolman R.W., Denaro V. Surgical versus nonoperative treatment in patients up to 18 years old with traumatic shoulder instability: a systematic review and quantitative synthesis of the literature. Arthroscopy. 2016;32:944–952. doi: 10.1016/j.arthro.2015.10.020. [DOI] [PubMed] [Google Scholar]
- 5.Postacchini F., Gumina S., Cinotti G. Anterior shoulder dislocation in adolescents. J Shoulder Elbow Surg. 2000;9:470–474. doi: 10.1067/mse.2000.108385. [DOI] [PubMed] [Google Scholar]
- 6.Jones K.J., Wiesel B., Ganley T.J., Wells L. Functional outcomes of early arthroscopic bankart repair in adolescents aged 11 to 18 years. J Ped Orthoped. 2007;27:209–213. doi: 10.1097/bpo.0b013e31803173d6. [DOI] [PubMed] [Google Scholar]
- 7.Lo I.K., Burkhart S.S. Triple labral lesions: pathology and surgical repair technique-report of seven cases. Arthroscopy. 2005;21:186–193. doi: 10.1016/j.arthro.2004.09.022. [DOI] [PubMed] [Google Scholar]
- 8.Milewski M.D., Nissen C.W. Pediatric and adolescent shoulder instability. Clin Sports Med. 2013;32:761–779. doi: 10.1016/j.csm.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 9.Ozturk B.Y., Maak T.G., Fabricant P. Return to sports after arthroscopic anterior stabilization in patients aged younger than 25 years. Arthroscopy. 2013;29:1922–1931. doi: 10.1016/j.arthro.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 10.Alpert J.M., Verma N., Wysocki R., Yanke A.B., Romeo A.A. Arthroscopic treatment of multidirectional shoulder instability with minimum 270 degrees labral repair: minimum 2-year follow-up. Arthroscopy. 2008;24:704–711. doi: 10.1016/j.arthro.2008.01.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A review of preoperative x-rays and magnetic resonance imaging of a young male athlete after sustaining a traumatic dislocation from a motor vehicle accident reveal a bony Bankart lesion with associated labral tear superiorly, anteriorly, and posteriorly. A 3-dimensional computer tomography scan revealed a small Hill-Sachs deformity. This injury was termed a triple labral lesion that was subsequently taken to the operating room for arthroscopic repair. The patient was placed in the lateral decubitus position and a diagnostic arthroscopy was performed. This confirmed the imaging findings of a triple labral lesion as seen through first the posterior portal and then anterior superior portal. A type IV superior labral anterior posterior tear was also found to be present. The labral tissue was gently elevated off the glenoid with use of a Bankart elevator followed by abrasion of the neck of the glenoid using a shaver and arthroscopic grasp. Prior to suture anchor placement, the bucket handle tear of the labrum is reduced from the inferior portion of the joint. At this time suture anchor placement of Suture-Fix anchors (Smith & Nephew, Andover, MA) was initiated sequentially beginning anterior and moving inferior to superior. For each suture anchor placement a Spectum (Conmed, Utica, NY) suture passer was utilized for suture passing around the labral tissue and standard arthroscopic knot techniques were utilized to secure the labrum back to the neck of the glenoid. These steps were repeated for the posterior labral repair. A total of 4 suture anchors were placed anteriorly and 4 were placed posteriorly for adequate reduction. The superior labral anterior posterior tear was then repaired with the lesion reduced to a type II SLAP tear associated with a split in the long head of the biceps tendon. 2 suture anchors were placed to reduce the tear. At this time the anatomic repair was evaluated for stability and found to be secure circumferentially. Attention was then turned to the subacromial space were a bursectomy was performed using an arthroscopic shaver. The biceps tendon was then tenodesed in the suprapectoral location utilizing two 1.7 mm SutureFix anchors (Smith & Nephew). Following tenodesis the arthroscope was reintroduced into the glenohumeral joint and the biceps attachment to the superior labrum was cut. Rehabilitation protocol is noted for return to full-contact athletics at 6 months if full strength and range of motion is achieved.