Key Points
Question
Has the Medicare Shared Savings Program been associated with changes in medication use or adherence for patients with cardiovascular disease or diabetes in participating accountable care organizations?
Findings
In this population-based study of Medicare beneficiaries from before the start of accountable care organization contracts to 2014, ranging from approximately 4.5 million to 10.8 million person-years, depending on drug class, differential changes in the use of and adherence to common antihypertensive, lipid-lowering, and hypoglycemic medications were minimal for accountable care organization patients vs patients of non–accountable care organization providers.
Meaning
Through its third year of operation, the Medicare Shared Savings Program has not meaningfully increased the use of or adherence to medications that improve outcomes for patients with cardiovascular disease or diabetes.
Abstract
Importance
Many of the quality measures used to assess accountable care organization (ACO) performance in the Medicare Shared Savings Program (MSSP) focus on disease control and medication use among patients with cardiovascular disease and diabetes. To date, the association between participation in the MSSP by provider organizations and medication use or adherence among their patients with cardiovascular disease or diabetes has not been described.
Objective
To assess the association between exposure to the MSSP and changes in the use of and adherence to common antihypertensive, lipid-lowering, and hypoglycemic medications.
Design, Setting, and Participants
Fee-for-service Medicare claims from January 1, 2009, to December 31, 2014, were used to conduct difference-in-differences comparisons of changes for ACO-attributed beneficiaries from before the start of ACO contracts to 2014 with concurrent changes for beneficiaries attributed to local non-ACO providers (control group). A random 20% sample of Medicare beneficiaries contributing 4 482 168 to 10 849 224 beneficiary-years for analysis from 2009 to 2014, depending on the drug class, was examined. Differential changes were estimated separately for cohorts of ACOs entering the MSSP in 2012, 2013, and 2014. Data analysis was conducted from November 1, 2016, to April 5, 2017.
Exposures
Patient attribution to an ACO after entry into the MSSP.
Main Outcomes and Measures
Any use (at least 1 prescription fill) and proportion of days covered (PDC), a standard claims-based measure of adherence, assessed for each of 6 drug classes: statins, angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers, β-blockers, thiazide diuretics, calcium channel blockers, and metformin.
Results
Differences in patient characteristics between the MSSP and control group were generally small after geographic adjustment and changed minimally from the precontract period to 2014. There were no significant differential changes in medication use from the precontract period to 2014 for any cohort of MSSP ACOs in any drug class, except for a slight differential increase in the use of thiazides among beneficiaries with hypertension in the 2013 entry cohort (adjusted differential change, 0.5 percentage point; 95% CI, 0.1-0.8 percentage points; or 1.5% of the overall percentage using thiazides [33.4%], P = .01). Similarly, there were no significant differential changes in PDC among beneficiaries with at least 1 prescription fill, except for slight differential increases in the PDC for β-blockers in the 2012 entry cohort (adjusted differential change, 0.3 percentage point; 95% CI, 0.1-0.5 percentage points; or 0.4% of the mean PDC [82.3%], P = .003) and for metformin in the 2012 and 2013 cohorts (adjusted differential change, 0.5 percentage point; 95% CI, 0.1-0.9 percentage points; or 0.6% of the mean PDC [78.2%], P = .01 for both).
Conclusions and Relevance
Exposure to the MSSP has not been associated with meaningful changes in medication use or adherence among patients with cardiovascular disease and diabetes.
This population-based study examines the use of and adherence to drugs from classes commonly used for therapy in patients with cardiovascular disease and diabetes.
Introduction
Accountable care organizations (ACOs) in the Medicare Shared Savings Program (MSSP) are eligible for shared-savings bonuses if spending for their patient population falls below a financial benchmark. Performance on a set of 33 quality measures determines the proportion of savings that they receive. Through 2014, 14 of the quality measures focused on cardiovascular disease and diabetes, including 11 measures of disease control or medication use. Improving medication use and adherence may be additionally attractive to ACOs as a strategy to achieve savings because the MSSP does not include Part D prescription drug spending in an ACO’s spending or benchmark. Thus, increasing patients’ use of prescription drugs to improve performance on quality measures or to lessen the need for nondrug services may support greater shared-savings bonuses than other quality improvement efforts or substitutions that require increases in certain nondrug services. To our knowledge, the association between participation in the MSSP and medication use or adherence for patients with cardiovascular disease and diabetes has not been described.
Methods
Study Population
For each year from 2009 to 2014, we analyzed data from Medicare claims and enrollment files for a random 20% sample of fee-for-service beneficiaries continuously enrolled in Parts A, B, and D in that year (while alive for decedents) and in the previous year to assess established conditions and prior drug use. For each of 6 classes of antihypertensive, lipid-lowering, and hypoglycemic medications, we limited the sample to patients with relevant conditions (Table 1). The presence of each condition at the start of each study year was assessed using data in Medicare Beneficiary Summary Files from the Chronic Conditions Data Warehouse, which draws from claims since 1999 to describe the accumulated burden of chronic disease. The study was approved by the Harvard Medical School Committee on Human Studies, which granted a waiver of informed consent because the study analyzed deidentified secondary data.
Table 1. Study Samples by Medication Class.
| Medication Class | Included Conditionsa | No. (Person-years From 2009-2014) |
|---|---|---|
| Statins | Diabetes, ischemic heart disease, history of AMI, history of stroke or TIA, hyperlipidemia | 9 900 988 |
| ACE inhibitors and ARBs | Diabetes, ischemic heart disease, history of AMI, CHF, history of stroke or TIA, hyperlipidemia, hypertension, chronic kidney disease | 10 849 224 |
| β-Blockers | Ischemic heart disease, history of AMI, congestive heart failure, hypertension | 10 208 164 |
| Thiazide diuretics | Hypertension | 9 332 717 |
| Calcium channel blockers | Hypertension | 9 332 717 |
| Metformin | Diabetes | 4 482 168 |
Abbreviations: ACE, angiotensin-converting enzyme; AMI, acute myocardial infarction; ARB, angiotensin II receptor blocker; TIA, transient ischemic attack.
Presence of each condition at the start of each study year was assessed using data in Medicare Beneficiary Summary Files from the Chronic Condition Data Warehouse, which draws from claims since 1999 to describe the accumulated burden of chronic disease.
Using previously described methods and the Centers for Medicare & Medicaid Services ACO Provider-Level Research Identifiable File, which defines each ACO as a collection of provider taxpayer identification numbers and Centers for Medicare & Medicaid Services Certification Numbers (for safety-net providers), we attributed each beneficiary in each study year to the ACO or non-ACO taxpayer identification numbers, accounting for the most allowed charges for office visits with a primary care physician during that year. Beneficiaries attributed to Pioneer ACOs were excluded because of significant exit from that smaller ACO program before 2014.
Study Variables
For each drug class in each year, we assessed whether beneficiaries had at least 1 prescription filled and, among users, we assessed the proportion of days covered (PDC) by filled prescriptions—a standard claims-based measure of adherence. The denominator of the PDC for a given drug class was 365 days for established users (ie, those with ≥1 prescription for that drug class filled in the 12 months before their first prescription fill of the year). The denominator for new users, defined as those without a prescription filled in the prior 12 months, was the number of days remaining in the year after the first prescription was filled. The numerator was the total days of drugs in the class supplied in the year. The denominator was truncated to the date of death for decedents, and the numerator was truncated to the denominator if it exceeded the denominator (eg, in the case of a 3-month supply received at the end of the year). We assessed these measures for each of the 6 drug classes: statins, angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers, β-blockers, thiazide diuretics, calcium channel blockers, and metformin. We assessed beneficiaries’ sociodemographic and clinical characteristics from Master Beneficiary Summary Files, claims, and US Census data.
Statistical Analysis
Using a difference-in-differences approach and linear regression, we compared changes in medication use and adherence for ACO-attributed beneficiaries from before to after the start of ACO contracts with concurrent changes for beneficiaries attributed to non-ACO providers (the control group). The precontract period was 2009-2011 for ACOs entering the MSSP in 2012 (n = 114), 2009-2012 for ACOs entering in 2013 (n = 106), and 2009-2013 for ACOs entering in 2014 (n = 115). Because reductions in health care utilization have grown larger with longer MSSP participation, we focused on differential changes from the precontract period to 2014. Model covariates included patients’ sociodemographic and clinical characteristics, fixed effects for each hospital referral region by year combination to adjust for local spending changes, and fixed effects for each ACO to adjust for any shifts in the distribution of patients across ACOs.
In sensitivity analyses, we modeled a dichotomous indicator of adherence (≥80%), added Part D plan fixed effects to adjust for benefit design, and conducted a subgroup analysis of new users, since medication initiation may present opportunities for establishing adherence. Statistical significance was defined as P < .05 for 2-sided tests. Statistical analysis was conducted using SAS, version 9.4 (SAS Institute Inc). Data analysis was conducted from November 1, 2016, to April 5, 2017.
Results
Sample sizes ranged from 4 482 168 to 10 849 224 beneficiary-years, depending on the drug class (Table 1). A mean of 24.8% of the beneficiaries were attributed to MSSP ACOs annually. Among beneficiaries attributed to an ACO in 2012 or 2013, 82.0% of those remaining enrolled in fee-for-service Medicare were attributed to the same ACO in the subsequent year. Differences in patient characteristics between the MSSP and control group were generally small after geographic adjustment and changed minimally from the precontract to postcontract period (Table 2, eTable in the Supplement).
Table 2. Differential Changes in Patient Characteristics From Precontract Period to 2014 for ACO-Attributed Patients vs Control Groupa.
| Patient Characteristic | Unadjusted Precontract, Meanb | Adjusted Precontract Difference, ACOs vs Control Group, % | Differential Change From Precontract Period to 2014 for ACOs vs Control Group, % | ||||
|---|---|---|---|---|---|---|---|
| 2012 Entry Cohort | 2013 Entry Cohort | 2014 Entry Cohort | 2012 Entry Cohort | 2013 Entry Cohort | 2014 Entry Cohort | ||
| Age, mean (SD), y | 73.2 (12.1) | 0.4c | 0.3 | −0.4 | −0.1 | 0.0 | 0.1 |
| Women, % | 63.0 | 1.0d | 0.4 | −0.1 | −0.5e | −0.3 | 0.0 |
| Race or ethnic group, %f | |||||||
| Non-Hispanic white | 82.8 | −1.6 | −0.1 | −0.2 | −0.5 | −0.7e | −0.6e |
| Non-Hispanic black | 10.1 | −0.5 | −0.4 | 0.5 | 0.2 | 0.2 | 0.3 |
| Hispanic | 2.7 | 0.1 | −0.6c | 0.0 | 0.2 | 0.2c | 0.1 |
| Other | 4.4 | 2.0 | 1.1 | −0.2 | 0.0 | 0.2 | 0.2c |
| Medicaid recipient, % | 36.1 | −0.5 | −2.5 | −1.0 | 0.4 | 0.7c | 0.6 |
| Disabled, %g | 26.4 | −2.0e | −2.1e | 0.5 | 0.2 | 0.1 | −0.1 |
| End-stage renal disease, % | 1.5 | 0.1 | −0.1 | 0.1 | 0.0 | 0.1 | −0.1e |
| Long-term nursing home resident, % | 2.4 | 0.7 | −0.5d | −0.4d | −0.3 | 0.1 | 0.0 |
| No. of CCW conditions, (SD)h | 4.7 (2.38) | 0.0 | −0.1 | −0.1 | 0.0 | 0.0 | 0.0 |
| HCC risk score, mean (SD)i | 1.54 (1.30) | −0.01 | −0.03d | −0.02 | 0.00 | 0.00 | 0.00 |
| ZCTA-level characteristic, % | |||||||
| Below FPL | 10.0 | −0.4c | −0.5e | −0.5c | 0.1e | 0.1d | 0.1e |
| High school degree | 73.6 | 0.9 | 1.2c | 0.9c | −0.4e | −0.3c | −0.1c |
| College degree | 18.5 | 0.7 | 0.9c | 1.2e | −0.4d | −0.1 | −0.1 |
Abbreviations: ACOs, accountable care organizations; CCW, Chronic Conditions Data Warehouse; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease; FPL, federal poverty level; HCC, Hierarchical Condition Category; ZCTA, zip code tabulation area.
Estimates are reported for a combined sample of beneficiaries with at least 1 of the conditions required for study inclusion. Means and percentages were adjusted for geography to reflect comparisons within hospital referral regions.
Precontract means are presented for 2009-2011 for consistency, but in estimation of differential changes, the precontract period was extended through 2012 for the 2013 cohort and through 2013 for the 2014 cohort.
Statistically different from zero at a P < .05 level.
Statistically different from zero at a P < .001 level.
Statistically different from zero at a P < .01 level.
Race or ethnic group was determined from Medicare master beneficiary summary files.
Disability was the original reason for Medicare eligibility.
A total of 27 conditions were included: acute myocardial infarction, Alzheimer disease, Alzheimer disease and related disorders or senile dementia, anemia, asthma, atrial fibrillation, benign prostatic hyperplasia, chronic kidney disease, chronic obstructive pulmonary disease, depression, diabetes, heart failure, hip or pelvic fracture, hyperlipidemia, hypertension, hypothyroidism, ischemic heart disease, osteoporosis, rheumatoid arthritis/osteoarthritis, stroke/transient ischemic attack, breast cancer, colorectal cancer, endometrial cancer, lung cancer, prostate cancer, cataracts, and glaucoma. Indicators for all 27 conditions were included in analytic models, as well as indicators of having multiple (≥2 through ≥9) conditions. Counts of conditions presented in the table include all conditions except cataracts and glaucoma. The presence of each condition was assessed as of the outset of each year (ie, diagnoses present in the CCW prior to the study year).
Hierarchical Condition Categories risk scores are derived from demographic and diagnostic data in Medicare enrollment and claims files, with higher scores indicating higher predicted spending in the subsequent year.
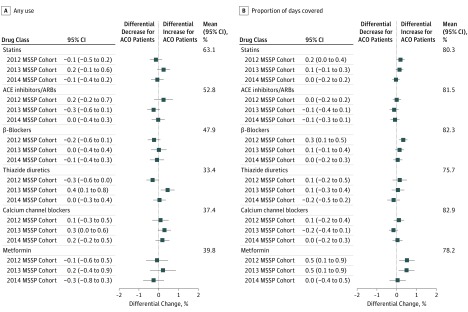
There were no significant differential changes in medication use from the precontract period to 2014 for any cohort of MSSP ACOs in any of the drug classes (Figure, A), except for a slight differential increase in use of thiazides among beneficiaries with hypertension in the 2013 entry cohort (adjusted differential change, 0.5 percentage point; 95% CI, 0.1-0.8 percentage points; or 1.5% of the overall percentage using thiazides [33.4%]; P = .01). Similarly, there were no significant differential changes in PDC among beneficiaries with at least 1 prescription fill (Figure, B), except for slight differential increases in the PDC for β-blockers in the 2012 entry cohort (adjusted differential change, 0.3 percentage point; 95% CI, 0.1-0.5 percentage points; or 0.4% of the mean PDC [82.3%]; P = .003) and for metformin in the 2012 and 2013 cohorts (adjusted differential change, 0.5 percentage point; 95% CI, 0.1-0.9 percentage points; or 0.6% of the mean PDC [78.2%]; P = .01 for both). Results from sensitivity analyses were substantively similar.
Figure. Differential Changes in Medication Use and Adherence by Drug Class for Accountable Care Organization (ACO)–Attributed Beneficiaries vs the Control Group.
For each medication class and Medicare Shared Savings Program (MSSP) entry cohort, adjusted differential changes in any use (A) and proportion of days covered (PDC) (B) are displayed for ACO-attributed beneficiaries vs the control group. Mean proportions for each measure and medication class are provided to support interpretation of absolute differential changes in relative terms (ie, estimates divided by the mean). Robust variance estimators were used to account for clustering within ACOs (for the ACO group) or hospital referral regions (for the control group). Error bars indicate 95% CIs. ACE indicates angiotensin-converting enzyme; ARBs, angiotensin II receptor blockers.
Discussion
Through its third year of operation, the MSSP has been associated with minimal increases in the use of or adherence to common antihypertensive, lipid-lowering, and hypoglycemic medications that improve cardiovascular outcomes. We could not analyze the effects of the MSSP on blood pressure, cholesterol, or glucose levels directly because performance on disease control measures is reported only for ACOs and only after the start of ACO contracts, but our findings suggest that reported improvements in disease control among ACOs may reflect ongoing trends due to factors other than ACO contract incentives.
Limitations
Three caveats to this conclusion bear noting. First, improvements in disease control could have been achieved by ACOs nonpharmacologically through lifestyle modifications or bariatric surgery. Second, we could not observe dose intensification with prescription drug claims. However, differential changes in dose intensification would have to be uncorrelated with differential changes in prescription medication supply or initiation of additional agents (eg, in efforts to control blood pressure) to go undetected by our analysis. Such a pattern of results is a plausible but improbable outcome of effective efforts to improve disease control through medication use. Third, it is possible that efforts to limit polypharmacy resulted in appropriate reductions in prescriptions for ACO patients that obscured beneficial increases in use and adherence in our estimation of mean net effects. Differential changes in use were minimal, however, even for medications unlikely to be discontinued in such efforts (ie, statins and metformin).
Conclusions
Our findings suggest that incentives in the MSSP to improve disease control and lower hospitalization rates and nondrug spending for patients with cardiovascular disease and diabetes have not been associated with meaningful increases in medication use and adherence.
eTable. Differential Changes in Patient Characteristics From Pre-Contract Period to 2014 for ACO-Attributed Patients vs Control Group, Among Beneficiaries Taking Medications
References
- 1.Centers for Medicare & Medicaid Services 33 ACO Quality Measures. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/ACO-Shared-Savings-Program-Quality-Measures.pdf. Accessed April 1, 2017.
- 2.Chronic Conditions Data Warehouse https://www.ccwdata.org/web/guest/home. Accessed June 1, 2017.
- 3.McWilliams JM, Hatfield LA, Chernew ME, Landon BE, Schwartz AL. Early performance of accountable care organizations in Medicare. N Engl J Med. 2016;374(24):2357-2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ResDac. Research Data Assistance Center Research Data Assistance Center. Shared Savings Program Accountable Care Organizations provider-level RIF. http://www.resdac.org/cms-data/files/ssp-aco-provider-level-rif. Accessed April 1, 2017.
- 5.Choudhry NK, Shrank WH, Levin RL, et al. Measuring concurrent adherence to multiple related medications. Am J Manag Care. 2009;15(7):457-464. [PMC free article] [PubMed] [Google Scholar]
- 6.US Census Bureau 2010. American Community Survey. http://www.census.gov/programs-surveys/acs/data.html. Accessed April 1, 2017.
- 7.McWilliams JM. Changes in Medicare Shared Savings Program savings from 2013 to 2014. JAMA. 2016;316(16):1711-1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McWilliams JM, Gilstrap LG, Stevenson DG, Chernew ME, Huskamp HA, Grabowski DC. Changes in postacute care in the Medicare Shared Savings Program. JAMA Intern Med. 2017;177(4):518-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Egan BM, Li J, Qanungo S, Wolfman TE. Blood pressure and cholesterol control in hypertensive hypercholesterolemic patients: national health and nutrition examination surveys 1988-2010. Circulation. 2013;128(1):29-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Medicare & Medicaid Services Medicare ACOs provide improved care while slowing cost growth in 2014. 2015; https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2015-Fact-sheets-items/2015-08-25.html. Published August 25, 2015. Accessed April 1, 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Differential Changes in Patient Characteristics From Pre-Contract Period to 2014 for ACO-Attributed Patients vs Control Group, Among Beneficiaries Taking Medications