Key Points
Question
Can coronary artery calcium score serve as an alternative marker for age as a predictor of atherosclerotic cardiovascular disease events in older adults?
Findings
In this analysis of pooled US population-based studies, coronary artery calcium score was more likely than age to provide discrimination between lower and higher coronary heart disease risk in older adults. Findings were similar in 2 European cohorts.
Meaning
In older adults without known cardiovascular disease, individual coronary artery calcium score provided better discrimination than chronological age for incident atherosclerotic cardiovascular disease (coronary heart disease in particular) during an 11-year follow-up.
Abstract
Importance
Besides age, other discriminators of atherosclerotic cardiovascular disease (ASCVD) risk are needed in older adults.
Objectives
To examine the predictive ability of coronary artery calcium (CAC) score vs age for incident ASCVD and how risk prediction changes by adding CAC score and removing only age from prediction models.
Design, Setting, and Participants
We conducted an analysis of pooled US population-based studies, including the Framingham Heart Study, the Multi-Ethnic Study of Atherosclerosis, and the Cardiovascular Health Study. Results were compared with 2 European cohorts, the Rotterdam Study and the Heinz Nixdorf Recall Study. Participants underwent CAC scoring between 1998 and 2006 using cardiac computed tomography. The participants included adults older than 60 years without known ASCVD at baseline.
Exposures
Coronary artery calcium scores.
Main Outcomes and Measures
Incident ASCVD events including coronary heart disease (CHD) and stroke.
Results
The study included 4778 participants from 3 US cohorts, with a mean age of 70.1 years; 2582 (54.0%) were women, and 2431 (50.9%) were nonwhite. Over 11 years of follow-up (44 152 person-years), 405 CHD and 228 stroke events occurred. Coronary artery calcium score (vs age) had a greater association with incident CHD (C statistic, 0.733 vs 0.690; C statistics difference, 0.043; 95% CI of difference, 0.009-0.075) and modestly improved prediction of incident stroke (C statistic, 0.695 vs 0.670; C statistics difference, 0.025; 95% CI of difference, −0.015 to 0.064). Adding CAC score to models including traditional cardiovascular risk factors, with only age being removed, provided improved discrimination for incident CHD (C statistic, 0.735 vs 0.703; C statistics difference, 0.032; 95% CI of difference, 0.002-0.062) but not for stroke. Coronary artery calcium score was more likely than age to provide higher category-free net reclassification improvement among participants who experienced an ASCVD event (0.390; 95% CI, 0.312-0.467 vs 0.08; 95% CI −0.001 to 0.181) and to result in more accurate reclassification of risk for ASCVD events among these individuals. The findings were similar in the 2 European cohorts (n = 4990).
Conclusions and Relevance
Coronary artery calcium may be an alternative marker besides age to better discriminate between lower and higher CHD risk in older adults. Whether CAC score can assist in guiding the decision to initiate statin treatment for primary prevention in older adults requires further investigation.
This study examines the predictive ability of coronary artery calcium score vs age for incident atherosclerotic cardiovascular disease and how risk prediction changes by adding coronary artery calcium score and removing only age from prediction models.
Introduction
Using the 2013 American College of Cardiology/American Heart Association cardiovascular disease lipid treatment guidelines and the Pooled Cohort Equation, nearly all individuals aged 60 years and older would potentially qualify for statin treatment on the basis of a 10-year atherosclerotic cardiovascular disease (ASCVD) risk of greater than 7.5% simply by virtue of their age. However, ASCVD events are unlikely to occur even in older adults if they have few cardiovascular risk factors. In addition, even a small increase in geriatric-specific adverse effects associated with statins (eg, rhabdomyolysis) could offset the cardiovascular benefit. Therefore, other discriminators of ASCVD risk besides age are needed in older adults. The 2013 American College of Cardiology/American Heart Association guideline proposed using additional tests to assist with treatment decisions in the presence of uncertainty or hesitation to use statins, and 1 marker that was suggested in the guideline for this purpose was coronary artery calcium (CAC).
Coronary artery calcium, a marker of atherosclerotic burden, has a potential role as an alternative marker for age for predicting ASCVD events. Coronary artery calcium score, when added to models including traditional cardiovascular risk factors (eg, age and blood pressure [BP]), was associated with improved ASCVD risk prediction in older adults. However, CAC score and age were considered jointly in risk prediction models in these studies, and therefore, whether CAC score can be an alternative marker for age as a predictor of ASCVD events in older adults remained to be determined.
Using a pooled individual participant data analysis (≥60 years of age, without known cardiovascular diseases at baseline) from 3 US cohorts (the Framingham Heart Study [FHS], the Multi-Ethnic Study of Atherosclerosis [MESA], and the Cardiovascular Health Study [CHS]), we sought to examine the predictive ability of CAC score vs age for ASCVD, including coronary heart disease (CHD) and stroke. Our results were confirmed by European cohorts, the Rotterdam Study (RS) and the Heinz Nixdorf Recall (HNR) Study.
Methods
Study Participants
Original Cohorts: 3 US Cohorts
Adults older than 60 years without known cardiovascular diseases (including CHD, stroke, and heart failure) at baseline were recruited from the FHS, MESA, and the CHS. The rationale for selecting age 60 years as the cutoff value of older adults in this study is that most individuals 60 years or older may be eligible for statins by US guidelines. Details of the study design and methods of each cohort have been described previously (eMethods in the Supplement).
Briefly, the original FHS cohort began in 1948 and enrolled 5209 participants. Five thousand one hundred twenty-four children of the original FHS cohort and the children’s spouses were enrolled in 1971 (the offspring cohort), and 4095 children of the offspring cohort participants were also enrolled in 2002 (the third-generation cohort). Between 2002 and 2005, 3529 participants (1422 from the offspring cohort and 2093 from the third-generation cohort) underwent CAC scoring using multidetector computed tomography (CT).
The MESA is a prospective, population-based cohort comprising 4 races/ethnicities (white, African American, Hispanic, and Chinese) and 6 US communities. The study recruited 6809 participants aged 45 years to 84 years who did not have cardiovascular diseases between 2000 and 2002. Coronary artery calcium scoring was conducted at baseline using either a cardiac-gated electron-beam CT scanner or multidetector CT.
The CHS is a population-based, prospective cohort study aimed at determining cardiovascular disease risk factors in older adults. Community-dwelling adults 65 years and older were recruited from 4 US field centers. Between 1998 and 2000, 614 participants in Pittsburgh underwent CAC scoring using an electron-beam CT scanner.
Confirmation Cohorts: 2 European Cohorts
Details of the study design and methods of the RS and the HNR Study have been described previously (eMethods in the Supplement). The RS is a prospective population-based cohort study that recruited participants 55 years and older from 1990 (RS-I). Starting in 2000, the original cohort was extended with a second cohort of participants who reached 55 years of age and those who had moved to the research area (RS-II). Assessment of CAC score was performed with an electron-beam CT C-150 Imatron scanner (GE-Imatron Inc) in the third examination of RS-I (n = 2063) or with 16-slice or 64-slice multidetector CT scanners (SOMATON Sensation 16 or 64; Siemens) in the second examination of RS-II (n = 2524).
The HNR Study is a population-based cohort study that recruited 4814 participants aged 45 years to 75 years from the metropolitan Ruhr area in Germany in 2000 to 2003. Electron-beam CT scans were performed with a C-100 or C-150 scanner (GE Imatron) at 2 sites in Bochum and Mülheim.
The institutional review boards of all 5 studies provided approval, and all participants gave written informed consent before enrollment in each study. The protocol for this study was approved by the institutional review board at Northwestern University.
Risk Factor and CAC Score Measurements
The assessments of traditional cardiovascular risk factors and CAC score in each cohort are described in the eMethods in the Supplement. eTable 1 in the Supplement provides information pertaining to when CT scans were performed and whether the results were reported to participants and physicians. A calcified lesion was defined as an area of at least 2 connected pixels with CT attenuation of more than 130 Hounsfield units. Agatston score was calculated, multiplying the area of each lesion with a weighted attenuation score dependent on the maximal attenuation within the lesion.
Ascertainment of Outcomes
Protocols and criteria for the ascertainment and diagnosis of events have been reported previously (eMethods in the Supplement); they were relatively similar across cohorts. Incident ASCVD during follow-up, including CHD (nonfatal myocardial infarctions and CHD deaths) and stroke (fatal or nonfatal) events, were assessed as outcomes. Physician members of the end points committee within each cohort independently reviewed medical records to adjudicate each possible cardiovascular outcomes, using specific definitions and a detailed manual of operations (http://www.mesa-nhlbi.org/; https://www.framinghamheartstudy.org/; https://chs-nhlbi.org/; and http://www.epib.nl/research/ergo.htm). Participants who did not have events and who did not drop out of the study after the initial examination were censored.
Statistical Analyses
All statistical analyses were performed with Stata version 12.1 (StataCorp). Descriptive statistics are presented as mean (SD), percentages of participants, and medians and quartiles.
Cox proportional hazards models were used to examine the predictive ability of CAC score for cardiovascular outcomes. Incident ASCVD, CHD, and stroke were evaluated as outcomes separately. The proportionality assumption for the Cox regression analysis was confirmed graphically and with the inclusion of a time by CAC score interaction. First, discordance in predictive ability between age and CAC score was assessed based on individual 10-year ASCVD risk. We defined 3 groups: age greater than CAC score discordance, concordance, and age less than CAC score discordance. Second, for assessing model fit, the likelihood ratio χ2 test was used. Comparison of the discriminative ability of each prediction model was conducted with C statistics (Harrell C statistic). Coronary artery calcium score was tested as a stratified variable (the similar cutoff points used in earlier MESA report: 0, 1 to 100, 101 to 300, and >300) and as a continuous variable (log [Agatston score +1] transformation). Covariates included age, sex, race/ethnicity (white, African American, Hispanic, and Asian), study site (FHS, MESA, and CHS), and traditional cardiovascular risk factors (ie, smoking, systolic BP, diabetes, total cholesterol, high-density lipoprotein cholesterol, and lipid-lowering and antihypertensive medication use). These covariates were selected a priori because they are included in the American College of Cardiology/American Heart Association 2013 cardiovascular risk equation. We examined (1) the predictive ability of CAC score vs age for specific cardiovascular outcomes; (2) how risk prediction changes by adding CAC score and removing only age from prediction models including covariates; and (3) how risk prediction changes by replacing CAC score for cardiovascular risk factors (ie, smoking, systolic BP, diabetes, total cholesterol level, high-density lipoprotein cholesterol, and lipid-lowering and antihypertensive medication use) but retaining age in prediction models. We evaluated category-based/category-free net reclassification improvement (NRI) for events and nonevents separately. We used cutoff values for 10-year ASCVD risk of less than 7.5% and at least 7.5%, the statin therapy threshold recommended in the 2013 American College of Cardiology/American Heart Association cholesterol guideline. We then calculated the proportion of participants who were reclassified by the comparison model compared with the base model.
In sensitivity analyses, we examined analyses of the interaction between CAC score and sex, race/ethnicity, or baseline age (<75 years and ≥75 years) in association with specific cardiovascular outcomes and sex-specific, race/ethnicity-specific, and age-specific (<75 years and ≥75 years) C statistic analyses. Statistical significance was defined as a P value < .05 using 2-sided t tests.
We first conducted a pooled individual participant analysis using data from 3 US cohorts. The analyses were independently repeated in 2 confirmation cohorts. Results from original cohorts were compared with those cohorts respectively.
Results
Original Cohorts: 3 US Cohorts
In all cohorts, we excluded participants younger than 60 years; those without CAC information; those with known CHD, stroke, and heart failure at baseline; those who had any missing covariates required in the analysis; and those lost to follow-up. As a result, 515 FHS participants, 3881 MESA participants, 387 CHS participants, 3089 RS participants, and 1901 HNR participants were included (total sample size in original cohorts, n = 4778). Of the 4778 participants, 2582 (54.0%) were women and 2347 (49.0%) were white, and the mean age was 70.1 years. Table 1 shows overall and cohort-specific demographic and clinical characteristics of the included participants. Coronary artery calcium score was higher in men compared with women (men: median, 97.8; interquartile range [IQR], 5.5-439.3; women: median, 14.8; IQR, 0-142.8; P < .001 by Mann-Whitney U test) and white individuals compared with African American, Hispanic, and Asian individuals (white: median, 94.2; IQR, 2.1-395.8; African American: median, 15.7; IQR, 0-146.7; Hispanic: median, 17.2; IQR, 0-128.0; Asian: median, 22.0; IQR, 0-132.3; P < .001 by Kruskal-Wallis test). Thirty-one percent of the study population had a CAC score of 0 at baseline (36.5% of white individuals, 31.4% of African American individuals, 20.7% Hispanic individuals, and 11.2% Asian individuals; eTable 2 in the Supplement). The proportion of participants with a CAC score of 0 was smallest in white individuals compared with other races/ethnicities (23% vs 35%-40%).
Table 1. Participant Characteristics From Original Cohorts (N = 4778) and Confirmation Cohorts (N = 4990)a.
| Descriptive Variable | No. (%) | |||||
|---|---|---|---|---|---|---|
| Original Cohorts (n = 4778) | Confirmation Cohorts (n = 4990) | |||||
| Total (n = 4778) | MESA (n = 3876) | FHS (n = 515) | CHS (n = 387) | Rotterdam Study (n = 3089) | HNR Study (n = 1901) | |
| Age, y | ||||||
| Mean (SD) | 70.1 (6.5) | 69.6 (6.2) | 67.4 (5.0) | 78.8 (3.9) | 68.7 (6.0) | 65.8 (4.4) |
| Median (range) | 69.1 (60.0-96.0) | 69.0 (60.0-84.0) | 66.9 (60.0-83.5) | 78.0 (71.0-96.0) | 67.2 (60.0-98.0) | 65.0 (60.0-76.0) |
| Men | 2196 (46.0) | 1835 (47.3) | 221 (42.9) | 140 (36.2) | 1317 (42.6) | 868 (45.7) |
| Race/ethnicity | ||||||
| Non-Hispanic white | 2347 (49.1) | 1532 (39.6) | 515 (100) | 300 (77.5) | 3089 (100) | 1901 (100) |
| African American | 1158 (24.2) | 1072 (27.7) | 0 | 86 (22.2) | 0 | 0 |
| Hispanic | 463 (17.0) | 463 (11.9) | 0 | 0 | 0 | 0 |
| Asian | 810 (9.7) | 809 (20.9) | 0 | 1 (0.3) | 0 | 0 |
| Current smoking | 412 (8.6) | 356 (9.2) | 25 (4.9) | 31 (8.0) | 501 (16.2) | 274 (14.4) |
| Systolic BP, mean (SD), mm Hg | 132.3 (21.5) | 132.4 (22.0) | 131.7 (18.6) | 132.6 (20.1) | 143.8 (20.0) | 137.4 (20.8) |
| Total cholesterol, mean (SD), mg/dL | 195.2 (35.8) | 193.6 (35.4) | 201.2 (34.7) | 203.3 (39.4) | 225.7 (36.2) | 235.8 (38.7) |
| HDL cholesterol, mean (SD), mg/dL | 52.4 (15.2) | 52.0 (15.1) | 53.8 (16.2) | 54.7 (14.7) | 55.7 (15.5) | 59.5 (16.9) |
| Diabetes | 682 (14.3) | 585 (15.1) | 52 (10.1) | 45 (11.6) | 351 (11.4) | 269 (14.2) |
| Antihypertensive medication use | 1990 (41.7) | 1615 (41.7) | 186 (36.1) | 189 (48.8) | 994 (32.2) | 760 (40.0) |
| Lipid-lowering medication use | 911 (19.1) | 750 (19.4) | 103 (20.0) | 58 (15.0) | 447 (14.5) | 237 (12.5) |
| CAC score | ||||||
| Agatston score, mean (SD) | 265.7 (560.0) | 224.9 (513.5) | 380.7 (703.3) | 521.0 (689.3) | 296.7 (663.3) | 243.2 (584.1) |
| Agatston score, median (IQR) | 42.3 (0-255.1) | 27.3 (0-197.2) | 102.2 (7.6-414.1) | 249.1 (45.0-716.4) | 61.37 (4.00-289.8) | 38.9 (1.5-200.9) |
| Agatston score = 0 | 1478 (30.9) | 1359 (35.1) | 92 (17.9) | 27 (7.0) | 461 (14.9) | 417 (21.9) |
| Agatston score = 1-100 | 1439 (30.1) | 1171 (30.2) | 164 (31.8) | 104 (26.9) | 1333 (43.2) | 780 (41.0) |
| Agatston score = 101-300 | 781 (16.4) | 602 (15.5) | 106 (20.6) | 73 (18.9) | 535 (17.3) | 346 (18.2) |
| Agatston score >300 | 1080 (22.6) | 744 (19.2) | 153 (29.7) | 183 (47.3) | 760 (24.6) | 358 (18.8) |
Abbreviations: CAC, coronary artery calcium; BP, blood pressure; FHS, Framingham Heart Study; CHS, Cardiovascular Health Study; HDL, high-density lipoprotein; HNR, Heinz Nixdorf Recall; IQR, interquartile range; MESA, Multi-Ethnic Study of Atherosclerosis.
SI conversion factor: To convert HDL cholesterol to millimoles per liter, multiply by 0.0259; to convert total cholesterol to millimoles per liter, multiply by 0.0259.
Original cohorts include MESA, FHS, and CHS, and individual participant data meta-analysis was conducted. Confirmation cohorts include the Rotterdam Study and the HNR Study, and the analyses were independently conducted within each study.
Baseline CAC Categories and Outcomes
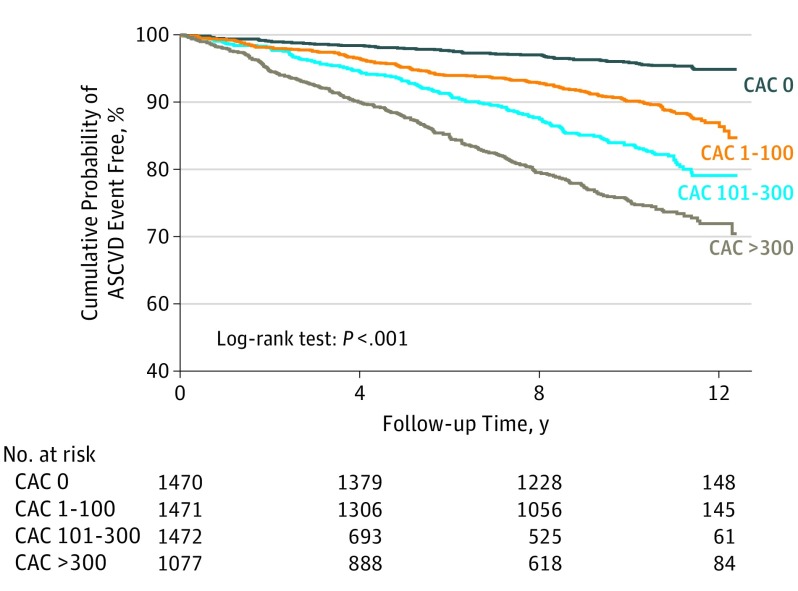
During a median follow-up period of 10.7 years (IQR, 7.4-11.4 years; 44 152.4 person-years), 598 ASCVD events occurred (14.9 per 1000 person-years), including 405 CHD events (9.0 per 1000 person-years) and 228 stroke events (5.0 per 1000 person-years). eTable 3 in the Supplement shows the frequency of cardiovascular outcomes and corresponding event rates (per 1000 person-years) by CAC categories, and those within each cohort are shown in eTable 4 in the Supplement. The event rates for total ASCVD and for each outcome increased across CAC strata. Eleven percent of all ASCVD events (8% of CHD and 16% of stroke) occurred in those with a CAC score of 0, whereas 42% of all ASCVD events (45% of CHD and 38% of stroke) occurred in participants with a CAC score of at least 300 (eTable 3 in the Supplement). Figure 1 shows the Kaplan-Meier cumulative probability of remaining free of an ASCVD event during 12-year follow-up, stratified by CAC categories; the probability progressively reduced with increasing CAC categories. The probability remains high (>90%) in those with a CAC score of 0 during the follow-up.
Figure 1. Kaplan-Meier Curves of the Cumulative Probability of Atherosclerotic Cardiovascular Disease (ASCVD) Event–Free by Coronary Artery Calcium (CAC) Categories in Original Cohorts.
The cumulative probability of free of ASCVD events by CAC categories is shown; ASCVD included coronary heart disease and stroke. The log-rank was used to calculate P values. CHD indicates coronary heart disease.
Predictive Ability of CAC Score vs Age for Outcomes
Discordance in predictive ability of ASCVD events between age and CAC score is shown in original cohorts in eTable 5 in the Supplement. The proportion of participants in each group was as follows: age greater than CAC score discordance group, 23.0%; concordance group, 62.9%; and age less than CAC score discordance group, 14.1%.
Results from Cox models suggest that both CAC score and age were positively associated with risk for ASCVD, CHD, and stroke (eTable 6 in the Supplement, models 1-3). When CAC score and age were analyzed jointly, their risks were attenuated but retained statistical significance (models 4-5). Differences in C statistics for outcomes between CAC score vs age are shown in eFigure 1 in the Supplement. Coronary artery calcium score (vs age) had a greater association with incident CHD (C statistic, 0.733 vs 0.690; C statistics difference, +0.043; 95% CI of difference, 0.009-0.075) and modestly improved prediction for stroke (C statistic, 0.695 vs 0.670; C statistics difference, +0.025; 95% CI of difference, −0.015 to 0.064). When we compared the C statistics between CAC score alone and age alone, results were generally similar (eTable 7 in the Supplement).
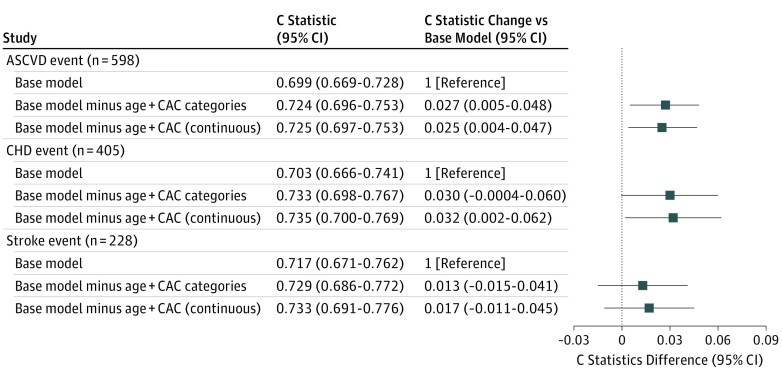
Adding CAC Score and Removing Only Age From Prediction Models
In CHD prediction models, model fit assessed by likelihood ratio χ2 change was improved when we added CAC score to models including cardiovascular risk factors, with only age being removed (eTable 8 in the Supplement). C statistics also significantly increased after adding log CAC (Agatston score +1) to the CHD prediction model including cardiovascular risk factors with only age being removed (C statistic, 0.735 vs 0.703; C statistics difference, +0.032; 95% CI of difference, 0.002-0.062) but modestly in stroke prediction models (C statistic, 0.733 vs 0.717; C statistics difference, +0.017; 95% CI of difference, −0.011 to 0.045) (Figure 2).
Figure 2. Predictive Ability of Risk Factor Covariates With Coronary Artery Calcium (CAC) and Without Age for Cardiovascular Outcomes in Original Cohorts.
Figure shows differences in C statistics and 95% CIs for individual cardiovascular outcome after CAC score was added to base models, with only age being removed. The base model includes age and the following covariates: sex, race/ethnicity, study site, current smoking, systolic blood pressure, total cholesterol, high-density lipoprotein cholesterol, diabetes, and use of antihypertensive drugs and lipid-lowering drugs. Coronary artery calcium score was tested as a categorical variable (0, 1 to 100, 101 to 300, and >300) and as a continuous variable (log [Agatston score +1] transformation). ASCVD indicates atherosclerotic cardiovascular disease; CHD, coronary heart disease.
Replacing CAC Score for Cardiovascular Risk Factors but Retaining Age in Prediction Models
Replacing CAC score for risk factors but retaining age improved model fit and discrimination for CHD (C statistic, 0.740 vs 0.703; C statistics difference, +0.037; 95% CI of difference, 0.012-0.062), whereas it reduced the discrimination of incident stroke (eTable 9 in the Supplement).
Repeated Cox analysis including CAC score and all risk factors including age, with the inclusion of an interaction term, suggested that there were no significant interactions between CAC score and sex, race/ethnicity, or age in association with all cardiovascular outcomes. Sex-specific, race/ethnicity–specific, and age-specific (<75 years and ≥75 years) C statistics analyses showed similar results (eFigures 2-17 in the Supplement).
Coronary artery calcium score was more likely than age to provide higher category-free NRI among participants who experienced an ASCVD event and to result in more accurate reclassification of risk for ASCVD events among these individuals (Table 2). In participants who did not experience an ASCVD event, adjusting the model of category-based NRI by adding CAC score to the other cardiovascular risk factors resulted in a greater improvement in risk reclassification compared with the model adjusted by adding age.
Table 2. Change in ASCVD Risk Stratification by CAC Score and Age in Original Cohorts (N = 4778)a.
| Base Model (Predicted Risk) | Base Model + Log CAC (Predicted Risk) | Category-Based NRI (SE), % | Category-Free NRI (95% CI), % | |||
|---|---|---|---|---|---|---|
| <7.5% | ≥7.5% | Total | ||||
| Model 1: ASCVD risk stratification by CAC score | ||||||
| Participants who experienced ASCVD events, % | ||||||
| <7.5 | 27 | 41 | 68 | -0.024 (-0.054 to 0.013) | 0.390 (0.312 to 0.469) | |
| ≥7.5 | 53 | 477 | 530 | |||
| Total | 80 | 518 | 598 | |||
| Participants who did not experience ASCVD events, % | ||||||
| <7.5 | 971 | 347 | 1318 | 0.122 (0.107 to 0.141) | 0.105 (0.08 to 0.137) | |
| ≥7.5 | 862 | 2000 | 2862 | |||
| Total | 1833 | 2347 | 4180 | |||
| Model 2: ASCVD risk stratification by age | ||||||
| Participants who experienced ASCVD events, % | ||||||
| <7.5 | 32 | 36 | 68 | -0.025 (-0.050 to 0.011) | 0.098 (-0.001 to 0.181) | |
| ≥7.5 | 48 | 482 | 530 | |||
| Total | 80 | 518 | 598 | |||
| Participants who did not experience ASCVD events, % | ||||||
| <7.5 | 975 | 343 | 1318 | 0.067 (0.051 to 0.081) | 0.199 (0.171 to 0.225) | |
| ≥7.5 | 627 | 2235 | 2862 | |||
| Total | 1602 | 2578 | 4180 | |||
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; CAC, coronary artery calcium; NRI, net reclassification improvement.
Reclassification tables are separated for cases and noncases, with rows indicating the risk categories based on the base model and columns indicating the new risk stratification after the addition of Log CAC (Agatston score +1) (model 1) or age (model 2) to the base model. The base model included sex, race/ethnicity, study site, current smoking, systolic blood pressure, total cholesterol, high-density lipoprotein cholesterol, diabetes, and use of antihypertensive drugs and lipid-lowering drugs. The cells note the number of participants reclassified by predicted risk.
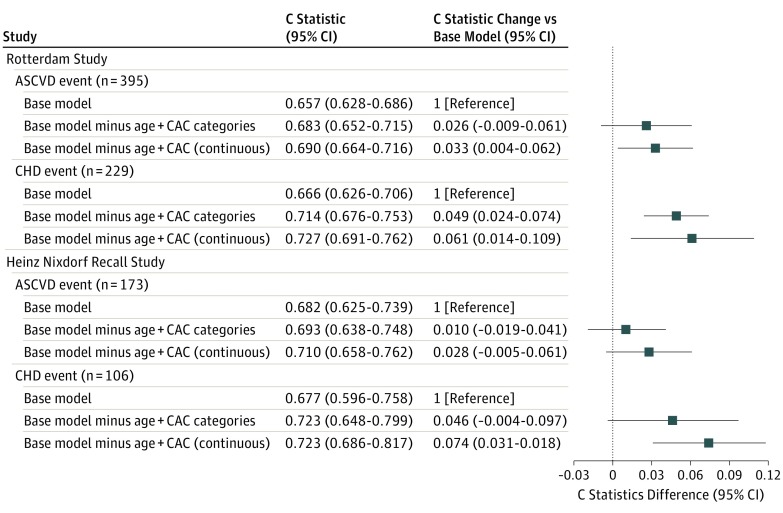
Confirmation Cohorts: 2 European Cohorts
Demographic and clinical characteristics of the included participants are shown in Table 1. eTable 4 in the Supplement shows the frequency of cardiovascular outcomes and corresponding event rates (per 1000 person-years). Discordance in predictive ability of ASCVD events between age and CAC score is shown in eTable 10 and eTable 11 in the Supplement. The proportion of participants in each group was as follows: age greater than CAC score discordance group, 15% to 18%; concordance group, 64% to 79%; and age less than CAC score discordance group, 2% to 20%. Coronary artery calcium score had a greater association with incident CHD compared with age, whereas age performed better than CAC score for predicting stroke (Figure 3 and eFigures 18-21 in the Supplement). Cardiovascular risk factor covariates with CAC score and without age provided improved discrimination for incident CHD but not for stroke (eFigures 20-21 in the Supplement). Replacing CAC score for risk factors but retaining age improved model fit and discrimination for CHD, whereas it reduced the discrimination of incident stroke (eTable 12 in the Supplement). In the RS, CAC score was more likely than age to provide higher category-free NRI and total number of correctly reclassified participants for ASCVD events (eTable 13 in the Supplement). In contrast, a difference in the categorical NRI between age and CAC score was modest in the HNR Study (eTable 14 in the Supplement).
Figure 3. Predictive Ability of Risk Factor Covariates With Coronary Artery Calcium (CAC) and Without Age for Cardiovascular Outcomes in Confirmation Cohorts.
Figure shows differences in C statistics and 95% CIs for individual cardiovascular outcome after CAC score was added to base models, with only age being removed. The base model includes age and the following covariates: sex, current smoking, systolic blood pressure, total cholesterol, high-density lipoprotein cholesterol, diabetes, and use of antihypertensive drugs and lipid-lowering drugs. Coronary artery calcium score was tested as a categorical variable (0, 1 to 100, 101 to 300, and >300) and as a continuous variable (log [Agatston score +1] transformation). ASCVD indicates atherosclerotic cardiovascular disease; CHD, coronary heart disease.
Discussion
Our study, based on results from a pooled individual participant data analysis from 3 US cohorts comprising older adults (≥60 years) without known cardiovascular diseases at baseline (n = 4778; mean age, 70.1 years; and 51% nonwhite), demonstrated that (1) 1478 participants (30.9%) had a CAC score of 0 and their probability of remaining ASCVD event–free over 12-year follow-up remains high (>90%); (2) CAC score instead of age had a greater association with incident CHD and a modest association with stroke; (3) traditional cardiovascular risk factor with CAC score and without age provided improved discrimination for incident CHD and modest discrimination for stroke; (4) age plus CAC score without cardiovascular risk factors provided improved discrimination for incident CHD but not for stroke; and (5) CAC score improved risk reclassification for incident ASCVD better than age. The superior ability of CAC score vs age for predicting CHD events was confirmed in 2 well-described European cohorts showing similar results.
Predictive Ability of CAC Score vs Chronological Age for Outcomes
Aging is the most consistent and robust contributor to incident ASCVD. However, arterial aging is a complex and heterogeneous process across individuals. Even at old age, 31% of our study population had a CAC score of 0; however, the results require careful interpretation because the proportion differed by race/ethnicity (23% in white individuals vs 35%-40% in other races/ethnicities). Atherosclerotic cardiovascular disease risk was low in participants with a CAC score of 0 (4.5 per 1000 person-years). This suggests that age per se does not necessarily pose an invariant risk for ASCVD events among older adults. The US Preventive Services Task Force recommended statin use in primary prevention of ASCVD events in adults in 2016. Doubts remain as to using statins for primary prevention in older adults, especially individuals older than 75 years. Our data illustrate that older adults with a CAC score of zero may consider avoiding long-term statin use.
Coronary artery calcium score provided superior prediction for incident CHD compared with chronological age in both US and European cohorts. Conversely, we observed a nonsignificant trend for improved stroke prediction with CAC score compared with age in US cohorts, whereas age performed better than CAC score in European cohorts. Potential mechanisms behind the discrepancy include (1) intraindividual heterogeneity of disease severity across distinct vascular beds (ie, CAC represents the disease substrate of the coronary artery); (2) various causes of stroke in older adults (eg, embolisms from cardiac arrhythmia and small vessel diseases); and the proportion may vary by race/ethnicity. In US cohorts, although there was no significant interaction between CAC score and race/ethnicity in association with stroke risk, the predictive ability of CAC score for incident stroke appear to vary across race/ethnicity; and (3) stroke is an age-associated disease, ie, the incidence rate of stroke doubles for each successive decade after age 55 years.
Age Plus CAC Score Without Measuring Cardiovascular Risk Factors in Predicting Outcomes
Replacing CAC score for cardiovascular risk factors but retaining age provided improved prediction of incident CHD in both US and European cohorts. The CHD prediction with risk factors (cholesterol in particular) decreases with age, partly because of selective survival and the influence of comorbidities on risk factor levels. In addition, one-time measurement of risk factors in late life is unlikely to reflect individual cumulative exposure to risk factor during a lifetime. Coronary artery calcium reflects exposure not only to measured (eg, cholesterol and BP) but also unmeasured (eg, environmental and sociopsychological factors) risk factors over a lifetime. Therefore, measuring CAC score (ie, disease-based prediction) instead of assessing cardiovascular risk factors (ie, risk-based prediction) may lead to an optimization of CHD prediction in older adults. In contrast, replacing CAC score for cardiovascular risk factors reduced the discrimination for incident stroke in both US and European cohorts. This suggests that a certain risk factor (eg, BP) is associated with and predictive of incident stroke at older age. Stroke is common in older adults, and therefore, CAC scoring may be limited as a sole risk estimator for ASCVD (ie, CHD and stroke) in older adults. Given smaller effect of statins on stroke prevention compared with CHD prevention in older adults, CAC scoring may be beneficial to guide statin therapy for preventing incident CHD in older adults.
Limitations and Strengths
Strengths of this study include the large, community-based multiethnic cohorts and external confirmation in 2 well-described European cohorts. However, there are limitations. First, participants receiving statins were included from all cohorts, and CAC score was reported to participants and their physicians in the FHS, MESA, CHS, and RS. This might lead to risk factor modification for participants, which potentially leads to an underestimation of the true association between CAC score and ASCVD risk. Second, assessments of CAC score, cardiovascular risk factors, and outcomes were relatively similar but not identical across cohorts. In aggregate, these factors would tend to underestimate the true associations between CAC score or cardiovascular risk factors and outcomes. Third, CAC score was more likely than age to improve risk reclassification for incident ASCVD. However, the difference might be partly owing to limited age distribution in the study populations. Fourth, we cannot address all the complex interplay balancing issues of CAC scoring, including cost-effectiveness, access, utility (including potential adverse events), and integration in shared decision-making approaches from stakeholder perspective (ie, patients). These issues need to be examined in future studies.
Conclusions
In older adults without known cardiovascular diseases, individual CAC score instead of chronological age provided better discrimination for incident ASCVD (CHD in particular) over an 11-year follow-up. Besides age, CAC may be an alternative marker to better discriminate between lower and higher CHD risk in older adults. Given the absence of clear agreement on risk thresholds to initiate stains for primary prevention of ASCVD in older adults, clinical judgment and patient input are critical components during the decision-making process. Coronary artery calcium score may assist in such a shared decision-making approach. Clinical trials are needed to assess whether CAC score can help refine treatment decisions and subsequently reduce unnecessary medical expenditure and adverse effects of statins and increase treatment efficiency in older adults.
eMethods. Information on cohorts.
eTable 1. CT scan dates in each cohort.
eTable 2. The frequency of ASCVD events and the corresponding incident rates (per 1,000 person-years) by race and CAC score in original cohorts.
eTable 3. The frequency of cardiovascular outcomes and corresponding incidence rates (per 1,000 person-years) according to CAC categories in original cohorts (n=4778).
eTable 4. The frequency of cardiovascular outcomes and corresponding incident rates (per 1000 person-years) according to included cohorts.
eTable 5. Discordance in predictive ability between age and CAC score in original cohort (n=4778).
eTable 6. Model fit and HRs for incident cardiovascular outcomes in original cohorts (n=4778).
eTable 7. Predictive ability of CAC score alone versus age alone for cardiovascular outcomes in original cohorts (n=4778).
eTable 8. Adding CAC score and removing age only from prediction models: model fit and HRs in original cohorts (n=4778).
eTable 9. Replacing CAC score for all risk factors but retaining age in prediction models: model fit, HRs, and C statistics in original cohorts (n=4778).
eTable 10. Discordance in predictive ability between age and CAC score in the Rotterdam Study (n=3089).
eTable 11. Discordance in predictive ability between age and CAC score in the Heinz Nixdorf Recall (n=1901).
eTable 12. Replacing CAC score for all risk factors but retaining age in prediction models: C statistics in confirmation cohorts (n=4990).
eTable 13. Change in ASCVD risk stratification by CAC score and age in the Rotterdam Study (n=3,089).
eTable 14. Change in ASCVD risk stratification by CAC score and age in the Heinz Nixdorf Recall (n=1,901).
eFigure 1. Predictive ability of CAC score versus age for cardiovascular outcomes.
eFigures 2-5. Race-specific predictive ability of CAC score versus age for cardiovascular outcomes.
eFigures 6-7. Sex-specific predictive ability of CAC score versus age for cardiovascular outcomes.
eFigures 8-9. Age-specific (<75 years and >75 years) predictive ability of CAC score versus age for cardiovascular outcomes.
eFigures 10-13. Race-specific predictive ability of risk factor covariates with CAC score and without age for cardiovascular outcomes.
eFigures 14-15. Sex-specific predictive ability of risk factor covariates with CAC score and without age for cardiovascular outcomes.
eFigures 16-17. Age-specific (<75 years and >75 years) predictive ability of risk factor covariates with CAC score and without age for cardiovascular outcomes.
eFigures 18-19. Predictive ability of CAC score versus age for cardiovascular outcomes; external confirmation by the Rotterdam Study and the Heinz Nixdorf Recall Study.
eFigures 20-21. Predictive ability of risk factor covariates with CAC score and without age for cardiovascular outcomes; external confirmation by the Rotterdam Study and the Heinz Nixdorf Recall Study.
References
- 1.Stone NJ, Robinson JG, Lichtenstein AH, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25, suppl 2):S1-S45. [DOI] [PubMed] [Google Scholar]
- 2.Pencina MJ, Navar-Boggan AM, D’Agostino RB Sr, et al. Application of new cholesterol guidelines to a population-based sample. N Engl J Med. 2014;370(15):1422-1431. [DOI] [PubMed] [Google Scholar]
- 3.Stamler J, Stamler R, Neaton JD, et al. Low risk-factor profile and long-term cardiovascular and noncardiovascular mortality and life expectancy: findings for 5 large cohorts of young adult and middle-aged men and women. JAMA. 1999;282(21):2012-2018. [DOI] [PubMed] [Google Scholar]
- 4.Lloyd-Jones DM, Dyer AR, Wang R, Daviglus ML, Greenland P. Risk factor burden in middle age and lifetime risks for cardiovascular and non-cardiovascular death (Chicago Heart Association Detection Project in Industry). Am J Cardiol. 2007;99(4):535-540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Odden MC, Pletcher MJ, Coxson PG, et al. Cost-effectiveness and population impact of statins for primary prevention in adults aged 75 years or older in the United States. Ann Intern Med. 2015;162(8):533-541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blaha MJ, Silverman MG, Budoff MJ. Is there a role for coronary artery calcium scoring for management of asymptomatic patients at risk for coronary artery disease? clinical risk scores are not sufficient to define primary prevention treatment strategies among asymptomatic patients. Circ Cardiovasc Imaging. 2014;7(2):398-408. [DOI] [PubMed] [Google Scholar]
- 7.Alexopoulos N, Raggi P. Calcification in atherosclerosis. Nat Rev Cardiol. 2009;6(11):681-688. [DOI] [PubMed] [Google Scholar]
- 8.Vliegenthart R, Oudkerk M, Hofman A, et al. Coronary calcification improves cardiovascular risk prediction in the elderly. Circulation. 2005;112(4):572-577. [DOI] [PubMed] [Google Scholar]
- 9.Newman AB, Naydeck BL, Ives DG, et al. Coronary artery calcium, carotid artery wall thickness, and cardiovascular disease outcomes in adults 70 to 99 years old. Am J Cardiol. 2008;101(2):186-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elias-Smale SE, Proença RV, Koller MT, et al. Coronary calcium score improves classification of coronary heart disease risk in the elderly: the Rotterdam study. J Am Coll Cardiol. 2010;56(17):1407-1414. [DOI] [PubMed] [Google Scholar]
- 11.Tota-Maharaj R, Blaha MJ, Blankstein R, et al. Association of coronary artery calcium and coronary heart disease events in young and elderly participants in the multi-ethnic study of atherosclerosis: a secondary analysis of a prospective, population-based cohort. Mayo Clin Proc. 2014;89(10):1350-1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tota-Maharaj R, Blaha MJ, McEvoy JW, et al. Coronary artery calcium for the prediction of mortality in young adults <45 years old and elderly adults >75 years old. Eur Heart J. 2012;33(23):2955-2962. [DOI] [PubMed] [Google Scholar]
- 13.Leening MJ, Elias-Smale SE, Kavousi M, et al. Coronary calcification and the risk of heart failure in the elderly: the Rotterdam Study. JACC Cardiovasc Imaging. 2012;5(9):874-880. [DOI] [PubMed] [Google Scholar]
- 14.Hofman A, van Duijn CM, Franco OH, et al. The Rotterdam Study: 2012 objectives and design update. Eur J Epidemiol. 2011;26(8):657-686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmermund A, Möhlenkamp S, Stang A, et al. Assessment of clinically silent atherosclerotic disease and established and novel risk factors for predicting myocardial infarction and cardiac death in healthy middle-aged subjects: rationale and design of the Heinz Nixdorf RECALL Study: risk factors, evaluation of coronary calcium and lifestyle. Am Heart J. 2002;144(2):212-218. [DOI] [PubMed] [Google Scholar]
- 16.Dawber TR, Kannel WB, Lyell LP. An approach to longitudinal studies in a community: the Framingham Study. Ann N Y Acad Sci. 1963;107:539-556. [DOI] [PubMed] [Google Scholar]
- 17.Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families: the Framingham offspring study. Am J Epidemiol. 1979;110(3):281-290. [DOI] [PubMed] [Google Scholar]
- 18.Feinleib M, Kannel WB, Garrison RJ, McNamara PM, Castelli WP. The Framingham Offspring Study: design and preliminary data. Prev Med. 1975;4(4):518-525. [DOI] [PubMed] [Google Scholar]
- 19.Splansky GL, Corey D, Yang Q, et al. The Third Generation Cohort of the National Heart, Lung, and Blood Institute’s Framingham Heart Study: design, recruitment, and initial examination. Am J Epidemiol. 2007;165(11):1328-1335. [DOI] [PubMed] [Google Scholar]
- 20.Bild DE, Bluemke DA, Burke GL, et al. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;156(9):871-881. [DOI] [PubMed] [Google Scholar]
- 21.Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1(3):263-276. [DOI] [PubMed] [Google Scholar]
- 22.Tell GS, Fried LP, Hermanson B, Manolio TA, Newman AB, Borhani NO. Recruitment of adults 65 years and older as participants in the Cardiovascular Health Study. Ann Epidemiol. 1993;3(4):358-366. [DOI] [PubMed] [Google Scholar]
- 23.Hoffmann U, Massaro JM, Fox CS, Manders E, O’Donnell CJ. Defining normal distributions of coronary artery calcium in women and men (from the Framingham Heart Study). Am J Cardiol. 2008;102(9):1136-1141, 1141.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carr JJ, Nelson JC, Wong ND, et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234(1):35-43. [DOI] [PubMed] [Google Scholar]
- 25.Schmermund A, Möhlenkamp S, Berenbein S, et al. Population-based assessment of subclinical coronary atherosclerosis using electron-beam computed tomography. Atherosclerosis. 2006;185(1):177-182. [DOI] [PubMed] [Google Scholar]
- 26.D’Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6):743-753. [DOI] [PubMed] [Google Scholar]
- 27.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827-832. [DOI] [PubMed] [Google Scholar]
- 28.Newson RB. Comparing the predictive powers of survival models using Harrell’s C or Somers’. D Stata J. 2010;10:339-358. [Google Scholar]
- 29.Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358(13):1336-1345. [DOI] [PubMed] [Google Scholar]
- 30.Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27(2):157-172. [DOI] [PubMed] [Google Scholar]
- 31.Kennedy KF, Pencina MJ A SAS macro to compute added predictive ability of new markers predicting a dichotomous outcome. http://analytics.ncsu.edu/sesug/2010/SDA07.Kennedy.pdf. Accessed May 30, 2017.
- 32.Kannel WB, Vasan RS. Is age really a non-modifiable cardiovascular risk factor? Am J Cardiol. 2009;104(9):1307-1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grundy SM. Coronary plaque as a replacement for age as a risk factor in global risk assessment. Am J Cardiol. 2001;88(2A):8E-11E. [DOI] [PubMed] [Google Scholar]
- 34.Najjar SS, Scuteri A, Lakatta EG. Arterial aging: is it an immutable cardiovascular risk factor? Hypertension. 2005;46(3):454-462. [DOI] [PubMed] [Google Scholar]
- 35.Chou R, Dana T, Blazina I, Daeges M, Jeanne TL. Statins for prevention of cardiovascular disease in adults: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;316(19):2008-2024. [DOI] [PubMed] [Google Scholar]
- 36.Goldstein LB, Bushnell CD, Adams RJ, et al. ; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Epidemiology and Prevention; Council for High Blood Pressure Research; Council on Peripheral Vascular Disease, and Interdisciplinary Council on Quality of Care and Outcomes Research . Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(2):517-584. [DOI] [PubMed] [Google Scholar]
- 37.Sudlow CL, Warlow CP; International Stroke Incidence Collaboration . Comparable studies of the incidence of stroke and its pathological types: results from an international collaboration. Stroke. 1997;28(3):491-499. [DOI] [PubMed] [Google Scholar]
- 38.Ueshima H, Sekikawa A, Miura K, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008;118(25):2702-2709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim AS, Johnston SC. Global variation in the relative burden of stroke and ischemic heart disease. Circulation. 2011;124(3):314-323. [DOI] [PubMed] [Google Scholar]
- 40.Go AS, Mozaffarian D, Roger VL, et al. ; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics: 2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6-e245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.de Ruijter W, Westendorp RG, Assendelft WJ, et al. Use of Framingham risk score and new biomarkers to predict cardiovascular mortality in older people: population based observational cohort study. BMJ. 2009;338:a3083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Störk S, Feelders RA, van den Beld AW, et al. Prediction of mortality risk in the elderly. Am J Med. 2006;119(6):519-525. [DOI] [PubMed] [Google Scholar]
- 43.Lloyd-Jones DM. Coronary artery calcium scoring: are we there yet? J Am Coll Cardiol. 2015;66(15):1654-1656. [DOI] [PubMed] [Google Scholar]
- 44.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration . Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903-1913. [DOI] [PubMed] [Google Scholar]
- 45.Shepherd J, Blauw GJ, Murphy MB, et al. ; PROSPER study group . Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360(9346):1623-1630. [DOI] [PubMed] [Google Scholar]
- 46.Nasir K. Overhauling cardiovascular risk prediction in primary prevention: difficult journey worth the destination. Circ Cardiovasc Qual Outcomes. 2015;8(5):466-468. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Information on cohorts.
eTable 1. CT scan dates in each cohort.
eTable 2. The frequency of ASCVD events and the corresponding incident rates (per 1,000 person-years) by race and CAC score in original cohorts.
eTable 3. The frequency of cardiovascular outcomes and corresponding incidence rates (per 1,000 person-years) according to CAC categories in original cohorts (n=4778).
eTable 4. The frequency of cardiovascular outcomes and corresponding incident rates (per 1000 person-years) according to included cohorts.
eTable 5. Discordance in predictive ability between age and CAC score in original cohort (n=4778).
eTable 6. Model fit and HRs for incident cardiovascular outcomes in original cohorts (n=4778).
eTable 7. Predictive ability of CAC score alone versus age alone for cardiovascular outcomes in original cohorts (n=4778).
eTable 8. Adding CAC score and removing age only from prediction models: model fit and HRs in original cohorts (n=4778).
eTable 9. Replacing CAC score for all risk factors but retaining age in prediction models: model fit, HRs, and C statistics in original cohorts (n=4778).
eTable 10. Discordance in predictive ability between age and CAC score in the Rotterdam Study (n=3089).
eTable 11. Discordance in predictive ability between age and CAC score in the Heinz Nixdorf Recall (n=1901).
eTable 12. Replacing CAC score for all risk factors but retaining age in prediction models: C statistics in confirmation cohorts (n=4990).
eTable 13. Change in ASCVD risk stratification by CAC score and age in the Rotterdam Study (n=3,089).
eTable 14. Change in ASCVD risk stratification by CAC score and age in the Heinz Nixdorf Recall (n=1,901).
eFigure 1. Predictive ability of CAC score versus age for cardiovascular outcomes.
eFigures 2-5. Race-specific predictive ability of CAC score versus age for cardiovascular outcomes.
eFigures 6-7. Sex-specific predictive ability of CAC score versus age for cardiovascular outcomes.
eFigures 8-9. Age-specific (<75 years and >75 years) predictive ability of CAC score versus age for cardiovascular outcomes.
eFigures 10-13. Race-specific predictive ability of risk factor covariates with CAC score and without age for cardiovascular outcomes.
eFigures 14-15. Sex-specific predictive ability of risk factor covariates with CAC score and without age for cardiovascular outcomes.
eFigures 16-17. Age-specific (<75 years and >75 years) predictive ability of risk factor covariates with CAC score and without age for cardiovascular outcomes.
eFigures 18-19. Predictive ability of CAC score versus age for cardiovascular outcomes; external confirmation by the Rotterdam Study and the Heinz Nixdorf Recall Study.
eFigures 20-21. Predictive ability of risk factor covariates with CAC score and without age for cardiovascular outcomes; external confirmation by the Rotterdam Study and the Heinz Nixdorf Recall Study.