Key Points
Question
Is geographic information systems mapping a useful technique for visualizing access barriers to eye care for patients with diabetes?
Findings
In this cross-sectional study, maps illustrated density of patients with diabetes and their distribution around 5 clinics by zip code, density of ophthalmologists and primary care clinicians by zip code relative to US Census Urban Areas, and a travel time map showing areas reached by car in a user-specified amount of time. Patient access to primary care clinicians and ophthalmologists was influenced by the geography and road networks that connect them.
Meaning
Geographic information systems mapping may be useful for visualizing access barriers to eye care for patients with diabetes.
Abstract
Importance
Minimal information exists on the use of geographic information systems mapping for visualizing access barriers to eye care for patients with diabetes.
Objective
To use geographic information systems mapping techniques to visualize (1) the locations of patients participating in the North Carolina Diabetic Retinopathy Telemedicine Network, (2) the locations of primary care clinicians and ophthalmologists across the state, and (3) the travel times associated with traveling to the 5 primary care clinics in our study.
Design, Setting, and Participants
Cross-sectional study conducted from January 6, 2014, to November 1, 2015, at 5 Area Health Education Center primary care clinics that serve rural and underserved populations in North Carolina. In total, 1787 patients with diabetes received retinal screening photographs with remote expert interpretation to determine the presence and severity of diabetic retinopathy. Participants included patients 18 years or older with type 1 or type 2 diabetes who presented to these 5 clinics for their routine diabetes care.
Main Outcomes and Measures
Development of qualitative maps illustrating the density of patients with diabetes and their distribution around the 5 North Carolina Diabetic Retinopathy Telemedicine Network sites by zip code and the density of ophthalmologists and primary care clinicians by zip code relative to US Census Urban Areas. A travel time map was also created using road network analysis to determine all areas that can be reached by car in a user-specified amount of time.
Results
Mean (SD) age of patients was 55.4 (12.7) years. Women made up 62.7% of the study population. The study included more African American patients (55.4%) compared with white (35.5%) and Hispanic (5.8%) patients. The mean (SD) hemoglobin A1c level was 7.8% (2.4%) (to convert to proportion of total hemoglobin, multiply by 0.01), and the mean (SD) duration of diabetes was 9.2 (8.2) years. Whereas the clinics located in Greensboro, Asheville, and Fayetteville screened patients from more immediate surrounding areas, the Greenville site had the widest distribution of zip codes, suggesting that patients travel from greater distances to reach this facility. Primary care clinicians were spread somewhat uniformly across the state, whereas ophthalmologists were concentrated around urban centers. Also, the number and type of surface roads surrounding the clinics determined the distance and time patients must travel to receive care.
Conclusions and Relevance
Geographic information systems mapping is a useful technique for visualizing geographic access barriers to eye care for patients with diabetes and may help to identify underserved areas that would benefit from the expansion of retinal screening programs via telemedicine.
This study uses geographic information systems mapping techniques to visualize the locations of patients participating in the North Carolina Diabetic Retinopathy Telemedicine Network, the locations of primary care clinicians and ophthalmologists across the state, and the travel times associated with traveling to the 5 primary care clinics in our study.
Introduction
Diabetic retinopathy (DR) is the most common microvascular complication of diabetes and is the leading cause of new cases of blindness among working-age American individuals. By 2050, the prevalence of DR in patients with type 1 and type 2 diabetes 40 and older is projected to increase to 16.0 million (from 5.5 million in 2005), and the prevalence of vision-threatening DR is projected to increase to 3.4 million (from 1.2 million in 2005).
North Carolina has been identified as one of the nation's top 10 “diabetes hot spots,” where the burden of diabetes will be greatest in the next 10 years. By 2025, the number of people with diabetes in North Carolina is projected to increase to almost 1.9 million, at a cost to the state of $17.9 billion. In 2012, the prevalence of diabetes among North Carolinian individuals was 10.4%, which was higher than the national mean of 9.3%.
Patients with early stages of DR are often asymptomatic at the time laser treatment or intravitreal antivascular endothelial growth factor injections should be given, making early detection and timely referral to an ophthalmologist imperative to preventing vision loss. However, in our current eye care paradigm, less than 50% of patients with diabetes meet screening guidelines recommending annual retinal examinations by an ophthalmologist. Health care access barriers resulting from socioeconomic, geographic, transportation, education, language, and cultural challenges compromise the quality and effectiveness of DR treatment, thus placing patients with diabetes at unnecessary risk for this blinding disease.
The North Carolina Diabetic Retinopathy Telemedicine Network (NCDRTN) is an innovative screening program developed to address the growing burden of DR in the state. This program aims to reduce eye care access barriers and improve DR evaluation by using the emerging strategy of telemedicine to bring retinal examinations to the point of care of the primary care professional (PCP). The screening network allows PCPs to remotely capture, send, and receive retinal images between the University of North Carolina, Chapel Hill Department of Ophthalmology and 5 Area Health Education Center primary care clinics across North Carolina: Mountain Area Health Education Center in Asheville, Moses Cone Hospital Internal Medicine and Family Medicine clinics in Greensboro, East Carolina University Department of Family Medicine in Greenville, and Southern Regional Area Health Education Center in Fayetteville. From January 6, 2014, to November 1, 2015, our program provided 2006 eye screenings to a total of 1787 patients with diabetes across North Carolina. Results of the larger NCDRTN program evaluation are reported separately.
Studies have demonstrated the effectiveness of telemedicine in reaching underserved populations in remote and rural areas as well as urban settings across the United States. Although geographic and transportation challenges have been cited as reasons for access barriers to eye care, visual data analyses of such barriers are scant. The purpose of this study is to use geographic information systems (GIS) mapping techniques to visualize the location of patients participating in the NCDRTN relative to our program sites and to ophthalmologists and PCPs across the state. Understanding and visualizing patient and physician location data may allow for better identification of areas of need, where access barriers may be preventing patients with diabetes from receiving proper eye care. To improve access to retinal screening for these patients, GIS maps provide the information needed to support building telemedicine programs in the primary care setting. Such mapping may also help to inform future expansion of retinal telescreening programs.
Methods
This project was approved by the University of North Carolina institutional review board. Patients provided oral informed consent at the time of recruitment.
Data Collection
Patient zip code data were collected along with medical and socioeconomic data at the time of retinal imaging in the PCP’s office. A total of 1787 patients with either type 1 or type 2 diabetes were included in the data set, with 361 (20.2%) having any level of DR and 1426 (79.8%) having no DR in either eye. For the purposes of this study, only patients with DR were mapped because they may require further ophthalmologic care or more frequent follow-up within the NCDRTN.
Medical practice zip code data for licensed, active ophthalmologists and PCPs were obtained directly from the North Carolina Medical Board (Raleigh, North Carolina). Of a total of 36 189 active physicians registered with the North Carolina Medical Board as of December 2015, 571 ophthalmologists and 7168 PCPs were included in this study. For purposes of this analysis, PCPs were defined as physicians with an active North Carolina medical license who self-classified in the following primary areas: internal medicine, family medicine, endocrinology, geriatric medicine, adolescent medicine, pediatrics, pediatric endocrinology, general practice, general preventive medicine, and public health and general. Similarly, ophthalmologists were defined as physicians with an active North Carolina medical license who self-classified their primary area of practice within ophthalmology.
Data Aggregation
All maps were generated in ArcGIS software, version 10.2.1 (Esri). To protect patient privacy, precise locations were obscured and discrete points for patients and physicians (ie, ophthalmologists and PCPs) were aggregated to a coarser unit of geography via the use of associated zip code data. This also allowed for easier interpretation of the maps.
Patients and physicians were separately aggregated to their corresponding zip codes to derive counts. To facilitate a wider variety of visualization options, both patients and physicians were aggregated to zip code centroids.
Tabular patient and physician data sets were summarized to derive a count of the number of occurrences of each 5-digit zip code where a patient lives or a physician works. Frequencies of the 5-digit zip codes for each table were calculated using Pivot Tables in Excel. Patients who had some level of DR diagnosed in either eye were used to calculate zip code frequency because these patients would require the most stringent follow-up or referral to an ophthalmologist. The inverse of this selection was also made (ie, patients with no DR diagnosis), and zip code frequency was calculated. Zip code frequencies were also calculated for the appropriate physicians.
Creation of Density Maps
Frequency tables were joined to zip code Shapefiles, a common format for spatial data within GIS, to allow for displaying density of patients or physicians at the zip code level. To join the data, tabular joins were done in ArcMap: patient zip code frequency tables were joined to a Shapefile of zip code polygons and a Shapefile of zip code points, using the zip code field as a common ID. This same process was carried out for PCPs and ophthalmologists.
Once joined, new files for the joins listed previously were created, resulting in zip code point and polygon files showing the number of patients and physicians within each zip code. These count data were used to display the zip codes in 3 different density maps:
A graduated color (choropleth) map showing the number of patients per zip code, where light colors indicate low values and dark colors indicate high values.
Two dot density maps showing a stylized distribution of physicians within each zip code polygon. In these maps, points were randomly scattered within the boundaries of each zip code polygon, with each point corresponding to a user-defined number of individuals.
Creation of Travel Time Map
The travel time map was created in ArcMap using tools in the Network Analysis toolbox, which bases calculations on density and type of surface roads (ie, number of lanes and speed limit) and travel rules (ie, 1-way restrictions and limited access roads). “Service areas,” or polygons representing all of the areas that can be reached by car in a user-specified amount of time by traversing the real-world road network, were created around each of the 5 NCDRTN primary care clinics. Three different service areas were created: 20 minutes, 40 minutes, and 60 minutes.
Results
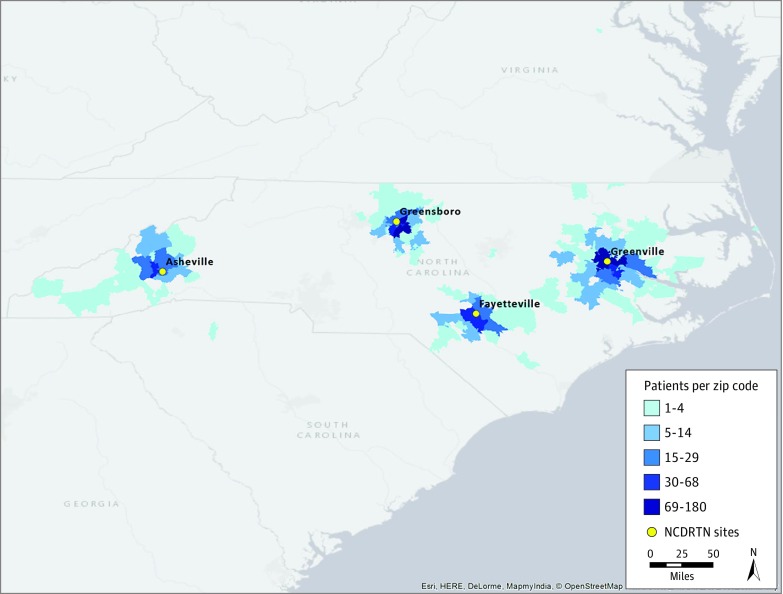
Figure 1 illustrates the density of patients with diabetes and their distribution around the 5 NCDRTN sites by zip code. The Greenville clinic site had the widest distribution of darkly shaded zip codes, suggesting that more patients traveled from outlying areas in the eastern part of the state to seek medical care at this facility. Twelve percent of patient zip codes around the Greenville site (5 patient zip codes within an urban area of 43 total zip codes) overlapped with the urban boundaries of the city; these zip codes accounted for 67% of patients visiting this site (285 patients within an urban area of 427 patients enrolled at Greenville site), and patients traveled a mean of 21 miles from rural areas to this clinic. The Greensboro, Asheville, and Fayetteville sites had a more concentrated distribution of zip codes, with most patients deriving from areas closer to the clinic sites and a comparatively smaller number of patients traveling from farther away. Sixty-six percent of patient zip codes around the Asheville site (23 patient zip codes within an urban area of 35 total zip codes), 50% around Fayetteville (13 patient zip codes within an urban area of 26 total zip codes), and 69% around Greensboro overlapped with the urban boundaries of these cities (25 patient zip codes within an urban area of 36 total zip codes); these zip codes accounted for 92% of patients visiting the Asheville site (284 patients within an urban area of 308 total patients), 92% visiting Fayetteville (336 patients within an urban area of 365 total patients), and 96% visiting Greensboro (594 patients within an urban area of 619 total patients). Patients going to Asheville, Fayetteville, or Greensboro traveled mean shorter distances of 15.7 miles, 10.8 miles, or 9.74 miles, respectively.
Figure 1. Patients With Diabetes in the North Carolina Diabetic Retinopathy Telemedicine Network (NCDRTN) per Zip Code.
Figure shows density of patients with diabetes and their distribution around the 5 NCDRTN sites by zip code. Greenville clinic site has widest distribution of darkly shaded zip codes, suggesting patients travel from outlying rural areas to seek medical care at this facility. Greensboro, Asheville, and Fayetteville sites have more concentrated distributions of zip codes, suggesting patients travel from areas that are tightly clustered around the urban centers. Maps generated by Esri, HERE, DeLorme, MapmyIndia, USGS, NOAA, NPS, OpenStreetMap contributors, and the GIS user community.
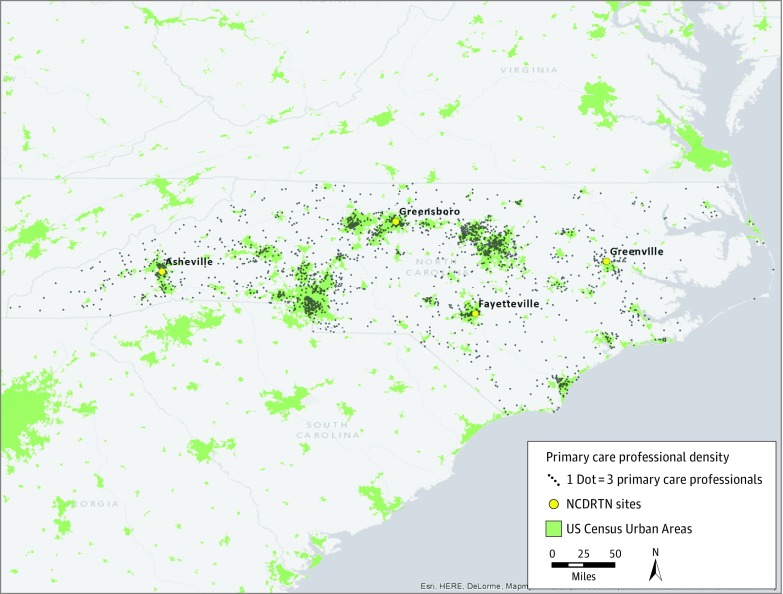
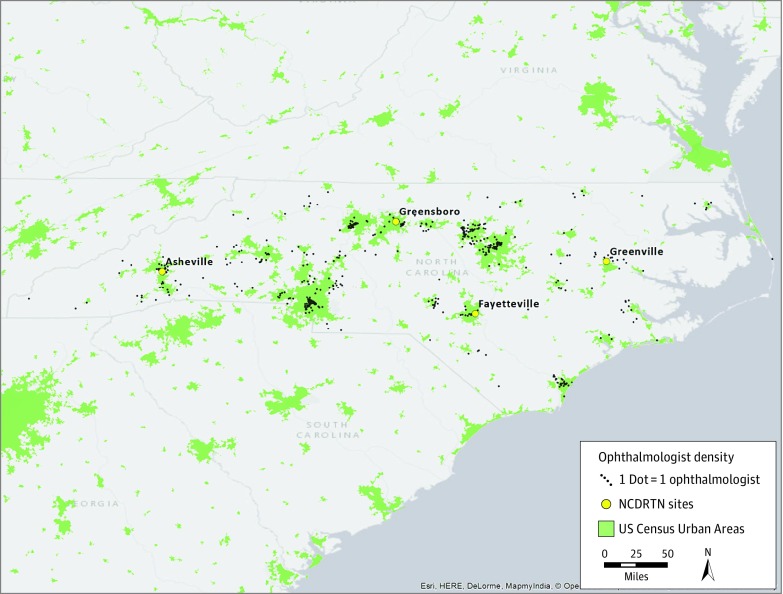
Figures 2 and 3 demonstrate the density of licensed PCPs and ophthalmologists throughout the state, respectively. It is apparent from these maps that PCPs are found in greater numbers and are distributed more widely in both rural and urban areas across the state, whereas ophthalmologists are fewer in number and distributed mainly within urban centers. The state’s 7168 PCPs are found in 63% of all zip codes (468 zip codes with at least 1 PCP of 743 total zip codes). Of these, 80% of PCPs are in urban zip codes (374 urban zip codes with at least one PCP of 468 zip codes with at least one PCP). The state’s 571 ophthalmologists are found in only 17% of zip codes (126 zip codes with at least 1 ophthalmologist of 743 total zip codes), with 98% of ophthalmologists in urban zip codes (123 urban zip codes with at least 1 ophthalmologist of 126 zip codes with at least 1 ophthalmologist).
Figure 2. Density of Primary Care Professionals in North Carolina.
Density of licensed primary care professionals throughout the state, shown using 1-to-3 dot density plotting. Figure demonstrates larger numbers of primary care professionals who are distributed more widely across both rural and urban areas of the state when compared against US Census Urban Areas (in green). Maps generated by Esri, HERE, DeLorme, MapmyIndia, USGS, NOAA, NPS, OpenStreetMap contributors, and the GIS user community.
Figure 3. Density of Ophthalmologists in North Carolina.
Density of licensed ophthalmologists throughout the state, shown using 1-to-1 dot density plotting. Figure demonstrates ophthalmologists are fewer in number and concentrated mainly within urban centers when compared against US Census Urban Areas (in green). Maps generated by Esri, HERE, DeLorme, MapmyIndia, USGS, NOAA, NPS, OpenStreetMap contributors, and the GIS user community.
The density of these physicians has been plotted by zip code relative to US Census Urban Areas containing at least 50 000 people (shown in green in Figures 2 and 3). Given that each black dot in Figure 2 represents 3 PCPs, this map demonstrates that PCPs make up one-fifth of all physicians in the state (7168 PCPs of 36 189 total physicians). The Census Urban Areas provide a visual reference point to highlight the differences in distribution of PCPs and ophthalmologists. For example, 83% of urban zip codes vs 32% of rural zip codes have at least 1 PCP (374 zip codes with a PCP in urban areas of 451 total urban zip codes vs 94 zip codes with a PCP in rural areas of 292 total rural zip codes). In contrast, 27% of urban zip codes (123 urban zip codes with an ophthalmologist of 451 total urban zip codes) vs 1% of rural zip codes have at least 1 ophthalmologist (3 rural zip codes with an ophthalmologist of 292 total rural zip codes). Uncertainty around the preceding estimates is difficult to quantify because this GIS-mapping technique assumes patients and physicians are located at the center of their zip codes, when in actuality, they may live or work anywhere within the entire combination of rural and urban areas that their zip codes encompass.
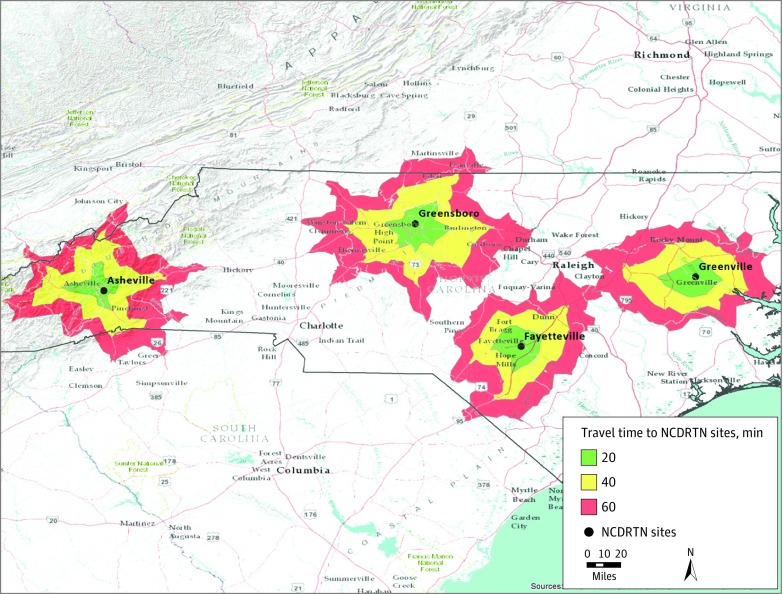
The travel time map allows for visualization of potential access barriers patients may face as a result of the number and type of surface roads available in their geographic area. As shown in Figure 4, the 20-minute service area represents all areas that can be reached within 20 minutes of travel time. The 40-minute service area represents all areas that can be reached within 40 minutes of travel time; this area is displayed as a ring around the 20-minute area, thus representing areas that can be reached in 20 to 40 minutes of driving, and similarly for the 60-minute service area. Of note, we performed an analysis of the city public transit systems in each of these areas and found that they were limited, so we did not graphically include these data in Figure 4. However, the existing city public transit system in North Carolina falls well within the 20-minute travel areas. Therefore, travel times by private automobile vs city transit are likely to be fairly similar. Notably, public transit service only exists around our clinic sites in areas that are characterized by a dense network of surface roads.
Figure 4. Driving Time to North Carolina Diabetic Retinopathy Telemedicine Network Sites.
Travel time map allows for visualization of potential access barriers based on number and type of surface roads surrounding each clinic. Twenty-minute service area represents all areas that can be reached within 20 driving minutes. Forty-minute service area contains all areas that can be reached between 20 and 40 driving minutes. Sixty-minute service area contains all areas that can be reached between 40 and 60 driving minutes. Maps generated by Esri, HERE, DeLorme, MapmyIndia, USGS, NOAA, NPS, OpenStreetMap contributors, and the GIS user community.
The city of Greensboro has an extensive network of interstate roads passing through or around the city, which better connects patients with the more developed and resource-rich metropolitan areas of the North Carolina Piedmont region. The metropolitan areas of the Triad (Greensboro, Winston-Salem, and High Point) and the Triangle (Chapel Hill, Durham, and Raleigh) contain a number of well-known health care facilities and hospital centers that offer patients in the Greensboro area ample opportunities for seeking quality care. In contrast, Greenville and Fayetteville are smaller cities with larger surrounding rural areas. They contain a sparser network of small roads with lower travel speeds that limits patient access to the few health care facilities in these 2 regions. Those living in the greater Asheville area face an additional and unique access barrier because they must contend with mountainous terrain to travel to the urban portions of Asheville. Because patients here must use small mountain roads with low travel speeds to access health care facilities within the city of Asheville, their perceived distance to health clinics may be inflated when compared with patients who can easily access interstate roads for quicker travel. Figure 4 thus illustrates how travel time along road networks may influence uptake of health care services. This map shows that the spread of travel activity is influenced by how easily people can travel along interstate corridors, which effectively extend the distance that a person is able to travel in a given amount of time.
Discussion
In this study, we have demonstrated that GIS mapping is a useful technique for visualizing geographic access barriers to eye care for patients with diabetes. By mapping the statewide distribution of health care professionals serving the primary care needs of patients with diabetes alongside ophthalmologists in North Carolina relative to the zip codes from which patients travel to reach our 5 NCDRTN sites, we have shown that patient accessibility to these physicians is influenced by the geography and road networks that connect them. This knowledge will help inform the future expansion of the NCDRTN program as we are able to identify opportunities for strategic collaborations between PCPs and ophthalmologists across the state.
To date, there has been minimal published literature on the use of GIS mapping for evaluating geographic access barriers, such as distance and travel time, to health care facilities in the United States. A few studies have used spatial analysis to determine how distance to hospitals and specialist care affects timely health care delivery, and at least 2 studies have used spatial analysis to identify areas of high diabetes prevalence so public health programs can be targeted to places where patient uptake of preventive care services is more likely.
Because diabetes prevalence is projected to increase from 25 million to a staggering 125 million Americans by 2050, the number of patients with diabetes requiring annual retinal screening will far exceed the capacity of eye care clinicians who as of 2017 see less than half of patients with diabetes needing DR evaluation. Coupled with an aging population, various access barriers to care, and growing shortages of PCPs nationwide, the paradigm for diabetic eye care will not be able to meet patients’ needs without using innovative strategies for health care delivery. Our study shows that telemedicine holds great potential for reducing travel times and geographic barriers to care by allowing physicians to connect over large distances with patients in some of the most rural and underserved areas. However, large-scale and cost-effective implementation of sustainable telemedicine systems will require strategic allocation of health care resources. Geographic information systems mapping is a helpful tool for informing the scaleup of such systems because areas can easily be identified where investments in telemedicine programs would be most worthwhile. By using publicly available census data, other demographic variables, and socioeconomic determinants of health in conjunction with patient medical records, this type of data visualization can help inform strategic planning for the expansion of broader public health care services.
A major strength of our study is that it includes patient data from an innovative eye screening program spanning 5 different primary care clinics across a geographically diverse state. These clinics provide health care to patients in both rural and urban areas across the mountains, piedmont, and coastal regions of North Carolina. Given the variety of geographic areas included in this study, the number and quality of road networks in these areas also play an important role in the access barriers that patients face to receiving quality health care.
Limitations
The findings of this study should be interpreted in the context of the following limitations. Although our study included a total of 1787 patients with diabetes, only 361 (20.2%) had any level of DR. Given the small sample size of patients with disease, we were not able to visualize whether those facing more geographic barriers to health care also experience higher rates of DR. Additionally, to protect patient privacy, we used coarse, 5-digit zip code–level data to map to zip code centroids. More detailed 9-digit zip code–level data and individual address information may have provided more accurate visualization of the exact distance patients are traveling to reach our primary care clinics. Also, some patients may access health care via public transportation; however, much of North Carolina still lacks a robust public transit infrastructure, so we limited our study to automobile transit only. While optometrists also refer patients to ophthalmologists, we did not include them in the definition of PCPs because medical primary care clinicians (ie, MD and DO physicians, physician’s assistants, and nurse practitioners) are the first line in primary diabetes prevention and play a much larger role in prevention, management, and treatment of diabetes and its complications.
Future research considerations might include studying larger sample sizes of patients with diabetes to assess the strength of the correlation between the quality of road networks, geography, socioeconomic determinants of health, and access barriers to health care. Public transportation data from areas with robust transit infrastructures would also allow for a more complete understanding of access barriers.
Conclusions
Telemedicine is a powerful tool for reducing vision loss from DR on the population level because it can help to increase surveillance rates while reducing socioeconomic disparities and access barriers to care. Expanding telemedicine coverage to areas of greatest need requires strategic planning to ensure the efficient and effective use of this new health care service delivery model. As demonstrated in this study, GIS mapping is a valuable method for understanding where such resources may be best allocated so that they target the patients and communities who need them most.
References
- 1.Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys Ther. 2008;88(11):1254-1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Published 2011. Accessed March 22, 2017.
- 3.Saaddine JB, Honeycutt AA, Narayan KMV, Zhang X, Klein R, Boyle JP. Projection of diabetic retinopathy and other major eye diseases among people with diabetes mellitus: United States, 2005-2050. Arch Ophthalmol. 2008;126(12):1740-1747. [DOI] [PubMed] [Google Scholar]
- 4.Diabetes 2025: US, state, and metropolitan trends. http://www.altfutures.org/diabetes2025/. Accessed March 22, 2017.
- 5.North Carolina State Center for Health Statistics Data for percentage of adults with diabetes North Carolina vs HNC 2020 Target. http://healthstats.publichealth.nc.gov/indicator/view_numbers/Diabetes.HNC2020.html. Published 2012. Accessed March 22, 2017.
- 6.Centers for Disease Control and Prevention National diabetes statistics report: estimates of diabetes and its burden in the United States, 2014. http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed March 22, 2017.
- 7.Lee PP, Feldman ZW, Ostermann J, Brown DS, Sloan FA. Longitudinal rates of annual eye examinations of persons with diabetes and chronic eye diseases. Ophthalmology. 2003;110(10):1952-1959. [DOI] [PubMed] [Google Scholar]
- 8.Paz SH, Varma R, Klein R, Wu J, Azen SP; Los Angeles Latino Eye Study Group . Noncompliance with vision care guidelines in Latinos with type 2 diabetes mellitus: the Los Angeles Latino Eye Study. Ophthalmology. 2006;113(8):1372-1377. [DOI] [PubMed] [Google Scholar]
- 9.Ferris FL III, Davis MD, Aiello LM. Treatment of diabetic retinopathy. N Engl J Med. 1999;341(9):667-678. [DOI] [PubMed] [Google Scholar]
- 10.Shi Q, Zhao Y, Fonseca V, Krousel-Wood M, Shi L. Racial disparity of eye examinations among the U.S. working-age population with diabetes: 2002-2009. Diabetes Care. 2014;37(5):1321-1328. doi: 10.2337/dc13-1038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Academy of Ophthalmology Retina/Vitreous Panel Diabetic retinopathy preferred practice pattern guidelines: updated 2016. http://www.aao.org/preferred-practice-pattern/diabetic-retinopathy-ppp-updated-2016. Published 2016. Accessed March 22, 2017.
- 12.Cavallerano J. Optometric clinical practice guideline. care of the patient with diabetes mellitus, reference guide for clinicians. http://www.aoa.org/documents/CPG-3.pdf. Accessed March 22, 2017.
- 13.American Diabetes Association Microvascular complications and foot care. Diabetes Care. 2016;39(suppl 1):S72-S80 [DOI] [PubMed] [Google Scholar]
- 14.Garg S, Jani PD, Kshirsagar AV, King B, Chaum E. Telemedicine and retinal imaging for improving diabetic retinopathy evaluation. Arch Intern Med. 2012;172(21):1677-1678. [DOI] [PubMed] [Google Scholar]
- 15.Mansberger SL, Gleitsmann K, Gardiner S, et al. Comparing the effectiveness of telemedicine and traditional surveillance in providing diabetic retinopathy screening examinations: a randomized controlled trial. Telemed J E Health. 2013;19(12):942-948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mansberger SL, Sheppler C, Barker G, et al. Long-term comparative effectiveness of telemedicine in providing diabetic retinopathy screening examinations: a randomized clinical trial. JAMA Ophthalmol. 2015;133(5):518-525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chin EK, Ventura BV, See K-Y, Seibles J, Park SS. Nonmydriatic fundus photography for teleophthalmology diabetic retinopathy screening in rural and urban clinics. Telemed J E Health. 2014;20(2):102-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Owsley C, McGwin G Jr, Lee DJ, et al. ; Innovative Network for Sight (INSIGHT) Research Group . Diabetes eye screening in urban settings serving minority populations: detection of diabetic retinopathy and other ocular findings using telemedicine. JAMA Ophthalmol. 2015;133(2):174-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Velez R, Tyler M, Chen J, Babcock M, Moran WP. Project I See in NC: initial results of a program to increase access to retinal examinations among diabetic individuals in North Carolina. N C Med J. 2011;72(5):360-364. [PubMed] [Google Scholar]
- 20.Olayiwola JN, Sobieraj DM, Kulowski K, St Hilaire D, Huang JJ. Improving diabetic retinopathy screening through a statewide telemedicine program at a large federally qualified health center. J Health Care Poor Underserved. 2011;22(3):804-816. [DOI] [PubMed] [Google Scholar]
- 21.Lin G, Allan DE, Penning MJ. Examining distance effects on hospitalizations using GIS: a study of three health regions in British Columbia, Canada. Environ Plan A. 2002;34(11):2037-2053. doi: 10.1068/a3528 [DOI] [Google Scholar]
- 22.Burkey ML, Bhadury J, Eiselt HA. A location-based comparison of health care services in four US states with efficiency and equity. Socioecon Plann Sci. 2012;46(2):157-163. doi: 10.1016/j.seps.2012.01.002 [DOI] [Google Scholar]
- 23.Cinnamon J, Schuurman N, Crooks VA. A method to determine spatial access to specialized palliative care services using GIS. BMC Health Serv Res. 2008;8:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khan JA, Casper M, Asimos AW, et al. Geographic and sociodemographic disparities in drive times to Joint Commission-certified primary stroke centers in North Carolina, South Carolina, and Georgia. Prev Chronic Dis. 2011;8(4):A79. [PMC free article] [PubMed] [Google Scholar]
- 25.Delmelle EM, Cassell CH, Dony C, et al. Modeling travel impedance to medical care for children with birth defects using Geographic Information Systems. Birth Defects Res A Clin Mol Teratol. 2013;97(10):673-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gesler WM, Hayes M, Arcury TA, Skelly AH, Nash S, Soward ACM. Use of mapping technology in health intervention research. Nurs Outlook. 2004;52(3):142-146. [DOI] [PubMed] [Google Scholar]
- 27.Curtis AB, Kothari C, Paul R, Connors E. Using GIS and secondary data to target diabetes-related public health efforts. Public Health Rep. 2013;128(3):212-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr. 2010;8:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dall T, West T, Chakrabarti R, Iacobucci W, Inc IHS. The Complexities of Physician Supply and Demand: Projections From 2013 to 2025. Washington, DC: Prepared for the Association of American Medical Colleges; 2015. [Google Scholar]