Abstract
Importance
The Eighth Joint National Committee (JNC-8) recommended treating systolic blood pressure (SBP) to a target below 150 mm Hg in older adults, whereas data from the Systolic Blood Pressure Intervention Trial (SPRINT) suggested that a SBP level of lower than 120 mm Hg decreases cardiovascular event rates. Target SBP guidelines have not addressed the potential that black patients may have greater morbidity and mortality from hypertension, especially with regard to cognitive outcomes. The association of these discordant SBP targets with cognition and differences by race have not been systematically evaluated in the same population.
Objectives
To assess the long-term outcomes of the various recommended SBP levels and to determine if racial differences exist based on long-term cognitive trajectories.
Design, Setting, and Participants
A total of 1657 cognitively intact older adults receiving treatment for hypertension were studied from 1997 to 2007 in the Health Aging and Body Composition study. Data analysis was conducted from October 1, 2016, to January 1, 2017.
Main Outcomes and Measures
Cognition was assessed using the Modified Mini-Mental State Examination (3MSE) 4 times and the Digit Symbol Substitution Test (DSST) 5 times. At each visit, participants were classified as having an SBP level of 120 mm Hg or lower, 121 to 139 mm Hg, 140 to 149 mm Hg, or 150 mm Hg or higher based on the mean SBP level of 2 seated readings. Mixed models assessed the association of SBP levels with 10-year cognitive trajectories. The impact of race was tested using a race interaction term.
Results
During the 10-year study period, among the 1657 individuals (908 women and 784 black patients; mean [SE] age, 73.7 [0.1] years), there was a differential decrease in 3MSE and DSST scores by the SBP levels, with the greatest decrease in the group with SBP levels of 150 mm Hg or higher (adjusted decrease was 3.7 for 3MSE and 6.2 for DSST) and the lowest decrease in the group with SBP levels of 120 mm Hg or lower (adjusted decrease was 3.0 for 3MSE and 5.0 for DSST) (P < .001 for both). Compared with white patients, black patients had a greater difference between the higher and lower SBP levels in the decrease in cognition; adjusted differences between the group with SBP levels of 150 mm Hg or higher and the group with SBP levels of 120 mm Hg or lower were –0.05 in white patients and –0.08 in black patients for 3MSE (P = .03) and –0.07 in white patients and –0.13 in black patients for DSST (P = .05).
Conclusions and Relevance
For patients 70 years of age or older receiving treatment for hypertension, a SPRINT SBP level of 120 mm Hg or lower was not associated with worsening cognitive outcome and may be superior to the JNC-8 target for cognition. Lower SBP treatment levels may result in improved cognition in black patients.
This longitudinal study assesses the long-term outcomes of systolic blood pressure levels recommended by the Eighth Joint National Committee and by the Systolic Blood Pressure Intervention Trial and determines if racial differences exist based on long-term cognitive trajectories.
Key Points
Questions
How do various systolic blood pressure levels in persons 70 to 79 years of age receiving treatment for hypertension affect cognition, and do racial differences exist based on long-term cognitive trajectories?
Findings
The greatest decline in cognitive status was observed in persons with systolic blood pressure levels of 150 mm Hg or higher, whereas the least cognitive decline occurred in those with systolic blood pressure levels of 120 mm Hg or lower. A systolic blood pressure target of 120 mm Hg or lower was more beneficial for black patients than white patients.
Meaning
Systolic blood pressure levels of 120 mm Hg or lower in older adults receiving treatment for hypertension is advantageous for cognition, especially for black individuals.
Introduction
The Eighth Joint National Committee (JNC-8) hypertension guidelines recommended treating older adults with systolic blood pressure (SBP) levels of 150 mm Hg or higher. This recommendation represented a change from the earlier recommended cutoff of lower than 140 mm Hg by the JNC-7 panel. The main concern about the lower JNC-7 target in this population was that more aggressive treatment of hypertension may be associated with adverse effects such as falls, cognitive decline, and mortality. These concerns were based on analyses of observational data that may not have addressed the time-dependent blood pressure increases that occur with aging or the decreases that occur with the onset of cognitive symptoms. There is consistent evidence that higher blood pressure earlier in life is linked with cognitive decline later in life. This lack of accounting for the reverse association between blood pressure and cognition in older adults, especially those older than 75 to 80 years of age, has confounded much of the observational evidence.
In contrast to these observational studies, clinical trials, including the Systolic Blood Pressure Intervention Trial (SPRINT), have suggested that a more aggressive SBP target for older adults may lower rates of cardiovascular disease without increasing falls. In SPRINT, a target SBP of lower than 120 mm Hg resulted in significant reductions in cardiovascular events and deaths compared with a target SBP of 140 mm Hg, which was true for persons younger than 75 years of age and those 75 years of age or older. There is also widespread concern based on observational studies that too much lowering of SBP, as in SPRINT, will adversely affect cognition. The cognitive outcomes have not yet been reported from SPRINT.
We sought to investigate the longitudinal outcomes of various SBP targets with regard to cognitive function in older adults receiving treatment for hypertension in the Health Aging and Body Composition (Health ABC) study. Our sample was composed only of patients receiving treatment for hypertension. We limited our analytical sample to patients receiving treatment for hypertension to render our results relevant to hypertension therapy. This design also minimizes bias introduced by prior observational studies by the inclusion in the analytical sample of both patients with and patients without hypertension and older adults receiving or not receiving treatment. The main bias concerns the outcome of hypertension treatment vs the reverse association between cognitive decline and blood pressure previously reported.
Target SBP guidelines have also not addressed the potential that black patients may have greater morbidity and mortality from hypertension, including cognitive outcomes, and hence may require a different set of targets. Hypertension is more prevalent in black individuals than in white individuals and is linked to greater vascular damage and morbidity; however, all guidelines have recommended the same SBP targets for both groups. A recent study based on a nationally representative sample reported that black patients are more likely to report cognitive symptoms related to hypertension and that these symptoms are related to increased mortality. Identifying the optimal treatment target in this population is of great necessity. This is especially critical since the JNC-8 guidelines for older adults were highly driven by the Hypertension in the Very Elderly Trial (HYVET), in which black individuals were underrepresented.
Therefore, the objective of our analysis is to investigate the outcome of different SBP levels with regard to cognition in older adults receiving treatment for hypertension and the differences by race in the associations between different SBP cutoffs and cognitive outcomes in the same population.
Methods
Sample
The Health ABC study is a prospective community-based study of 3075 well-functioning, cognitively intact participants 70 to 79 years of age. Participants were recruited to the Health ABC study between 1997 and 1998 from a random sample of white and black adults eligible for Medicare who were living in selected ZIP code areas in Pittsburgh, Pennsylvania, and Memphis, Tennessee. Of the sample, 1292 self-identified as black (42.0%) and 1599 were women (52.0%). For the present study, we only included participants being treated for hypertension (n = 1657). Cognitive trajectories were analyzed over a 10-year follow-up period from 1997 to 2007. The Health ABC study was approved by the institutional review boards at the University of Pittsburgh and the University of Tennessee Health Science Center, Memphis, and participants provided written informed consent.
Measures
The examiner-administered interview ascertained demographic characteristics (age, sex, educational level, income, and race/ethnicity) and health habits (smoking and alcohol use). Blood pressure recordings (taken while the participant was sitting after a 5-minute rest) were performed twice using a mercury sphygmomanometer. We used the mean SBP and mean diastolic blood pressure measured during each examination for this analysis. Weight (measured with a balance beam scale), height (measured with a stadiometer), and radial pulse were also obtained. Information on prevalent and incident health conditions was collected by self-report. Diagnoses of heart failure, hypertension, type 2 diabetes, and coronary artery disease were based on history, examination findings, and medication use. Data on current medications were collected using an inventory and included all prescription and nonprescription drugs taken in the last 2 weeks. The data were then coded according to the Iowa Drug Information System.
For this study, we used the findings from 2 cognitive tests obtained in the Health ABC study. The Digit Symbol Substitution Test (DSST), which requires an individual to rapidly write down symbols that are paired with numbers shown in an answer key, measures visuomotor speed, attention, set shifting, and memory. The DSST was performed in years 1, 5, 8, and 10. The Modified Mini-Mental State Examination (3MSE) assesses global cognitive function. This test was developed by Teng et al and is based on the original Mini-Mental State Examination with an expanded 100-point score to provide a lower floor and a higher test ceiling. The 3MSE was performed in years 1, 3, 5, 8, and 10.
Statistical Analysis
Statistical analysis was conducted from October 1, 2016, to January 1, 2017. Systolic blood pressure (mean level of 2 seated readings) at each visit was classified as 120 mm Hg or lower (SPRINT target), 121 to 139 mm Hg (JNC-7 target), 140 to 149 mm Hg (JNC-8 target), or 150 mm Hg or higher (reference group). The latter was used as a reference group because there is consensus that an SBP level of 150 mm Hg or higher is considered to result in an uncontrolled level of hypertension, as opposed to the 3 other SBP targets. We classified participants into 1 of these groups at each visit. We compared baseline characteristics between the 4 SBP target groups using analysis of variance or χ2 tests and between black and white participants using 2-tailed t tests or χ2 tests.
We then assessed the association of SBP levels with cognitive trajectories during the 10-year follow-up period using generalized mixed models. Mixed models are ideal because they account for within-subject correlations. We modeled these correlations using an autoregressive structure because the association between cognitive performances is typically stronger when the measures are conducted closer to each other. Cognition was assessed with variable times between the repeated measures.
Because participants may fluctuate from 1 group to another during the 10-year follow-up period, we modeled the SBP categorization as a time-dependent variable. Similarly, covariates were modeled as time-varying variables. For each cognitive measure, we tested the following 2 questions: (1) Is there a difference in cognitive change during the 10-year follow-up period between SBP levels when using an SBP group × year term in the model? (2) Within each SBP group, is there a significant change in cognition using SLICE and LSMESTIMATE statements? To assess the impact of race, we included a 3-way interaction term of race × SBP group × year. We calculated from the mixed models the unadjusted and covariate-adjusted differences in the rates of progression of the cognitive trajectories between white and black participants in the full analytical sample and within each SBP group. We calculated this difference as the disparity measure, which is the rate in white participants minus the rate in black participants (negative values meaning a greater decrease in the cognition of black participants), and we tested the hypothesis of whether the disparity measure differed by the SBP-target group. All models were adjusted for age, sex, race/ethnicity (except for the race comparisons), educational level, family income, stroke, diabetes, seated diastolic blood pressure, and the baseline performance on the corresponding cognitive measure. All analyses were conducted using SAS, version 9.4 (SAS Institute Inc). P < .05 was considered significant.
Results
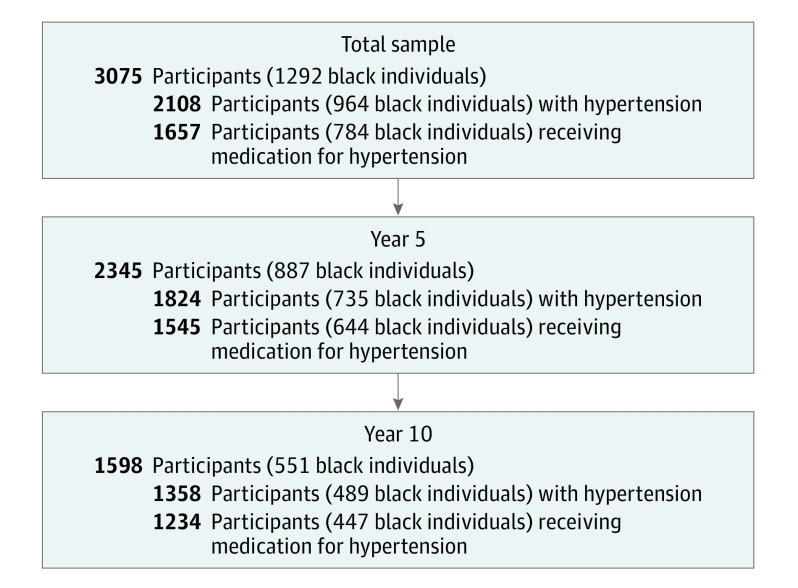
Our analytical sample included 1657 participants receiving treatment for hypertension. The follow-up rate was 93.2% in year 5 (n = 1545) and 74.5% in year 10 (n = 1234) (Figure 1). There was no significant difference in the mean number of follow-up visits across the 4 groups (2.5 visits in all groups except for those with a SBP level ≥150 mm Hg, where the mean number of visits was 2.4; P = .08). The baseline characteristics of the analytical sample by SBP level are presented in Table 1. The baseline distribution was as follows: 307 participants with a SBP level of 120 mm Hg or lower (18.5%), 627 participants with a SBP level of lower than 140 mm Hg (37.8%), 264 participants with a SBP level of lower than 150 mm Hg (15.9%), and 459 participants with a SPB level of 150 mm Hg or higher (57.7%). By year 10, a total of 309 of 1234 participants had a SBP level of 120 mm Hg or lower (25.0%), 457 had a SBP level of lower than 140 mm Hg (37.0%), 197 had a SBP level of lower than 150 mm Hg (16.0%), and 271 had a SBP level of 150 mm Hg or higher (22.0%). As shown in Table 1, those within the group with a SBP level of 150 mm Hg or higher were more likely to be black (248 [54.0%]; P = .004) and less likely to have had a myocardial infarction (56 [12.2%]; P < .001) and to be receiving thiazide diuretics (139 [30.3%]; P = .03).
Figure 1. Flowchart for the Health Aging and Body Composition Study.
The analytical sample is the group that received medication for hypertension.
Table 1. Baseline Characteristics of the Analytical Sample by Systolic Blood Pressure (SBP) Targets .
| Characteristic | Patients, No. (%) | P Valuea | ||||
|---|---|---|---|---|---|---|
| Total Sample (N = 1657) |
SBP ≤ 120 mm Hg (n = 307) |
SBP = 121-139 mm Hg (n = 627) |
SBP = 140-149 mm Hg (n = 264) |
SBP ≥ 150 mm Hg (n = 459) |
||
| Demographic | ||||||
| Age, mean (SE), y | 73.7 (0.1) | 73.6 (0.2) | 73.6 (0.1) | 73.5 (0.2)b | 73.9 (0.1)b | .14 |
| Female sex | 908 (54.8) | 144 (46.9) | 285 (45.5) | 117 (44.3) | 203 (44.2) | .89 |
| White race | 873 (52.7) | 179 (58.3) | 345 (55.0)b | 138 (52.3) | 211 (46.0)b | .004 |
| Postsecondary education | 664 (40.1) | 141 (45.9)b | 243 (38.8) | 109 (41.3) | 170 (37.0)b | .10 |
| Income $10 000-$25 000 | 701 (42.3) | 108 (35.2) | 230 (36.7) | 99 (37.5) | 180 (39.2) | .32 |
| BMI, mean (SE) | 28.20 (0.12) | 27.94 (0.26) | 28.00 (0.26) | 28.66 (0.32) | 28.38 (0.25) | .19 |
| Diagnosis | ||||||
| Congestive heart failure | 85 (5.3) | 25 (8.6)b | 27 (4.4) | 14 (5.3) | 19 (4.2)b | .04 |
| Type 2 diabetes, ever | 324 (19.5) | 51 (16.6) | 120 (19.1) | 52 (19.7) | 101 (22.0) | .32 |
| Diabetes, medication | 279 (16.8) | 46 (15.0) | 97 (15.5) | 46 (27.4) | 90 (19.6) | .24 |
| Myocardial infarction | 269 (16.2) | 74 (24.2)b | 106 (16.9) | 33 (12.5) | 56 (12.2)b | <.001 |
| Stroke | 57 (3.5) | 12 (3.9) | 23 (3.7) | 5 (1.9) | 17 (3.7) | .52 |
| Dementia | 331 (20.0) | 61 (19.9) | 125 (19.9) | 42 (15.9) | 96 (20.9) | .45 |
| Death ratec | 1143 (69.0) | 209 (68.1) | 420 (67.0) | 180 (68.2) | 326 (71.0) | .51 |
| Medication | ||||||
| ACE inhibitors | 465 (28.1) | 81 (26.4) | 168 (26.8)b | 68 (25.8) | 148 (32.2)b | .13 |
| α-Adrenergic blockers | 130 (7.9) | 23 (7.5) | 50 (8.0) | 30 (11.4)b | 27 (5.9)b | .07 |
| Angiotensin II receptor blockers | 70 (4.2) | 14 (4.6) | 22 (3.5) | 8 (3.0) | 26 (5.7) | .25 |
| β-Adrenergic blockers | 413 (24.9) | 84 (27.4) | 148 (23.6) | 58 (22.0) | 123 (26.8) | .30 |
| Calcium channel blockers | 705 (42.3) | 117 (38.1) | 269 (42.9) | 118 (44.7) | 201 (43.8) | .35 |
| Central hypotensives | 128 (7.7) | 14 (4.6)b | 48 (7.7) | 17 (6.4) | 49 (10.7)b | .02 |
| Hydralazine | 33 (2.0) | 7 (2.3) | 12 (1.9) | 6 (2.3) | 8 (1.7) | .94 |
| Potassium-sparing diuretics | 266 (16.1) | 60 (19.5)b | 119 (19.0) | 33 (12.5) | 54 (11.8)b | .001 |
| Loop diuretics | 192 (11.6) | 52 (16.9)b | 53 (8.4) | 26 (9.9)b | 61 (13.3) | .001 |
| Thiazide diuretics | 554 (33.4) | 95 (30.9) | 237 (37.8)b | 83 (31.4) | 139 (30.3)b | .03 |
| Antihypertensive medications, mean (SE), No. | 1.8 (0.02) | 1.78 (0.04) | 1.79 (0.04) | 1.69 (0.05) | 1.82 (0.04) | .33 |
| Cognitive assessment score, mean (SE) | ||||||
| 3MSE | 89.80 (0.20) | 90.21 (0.49) | 90.23 (0.29)b | 89.69 (0.49) | 89.00 (0.39)b | .07 |
| DSST | 34.28 (0.36) | 35.43 (0.82)b | 34.33 (0.56) | 35.48 (0.93) | 32.72 (0.71)b | .03 |
| Follow-up, median, y | 7 | 7 | 7 | 9 | 7 | .05 |
Abbreviations: 3MSE, Modified Mini-Mental State Examination; ACE, angiotensin converting enzyme; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); DSST, Digit Symbol Substitution Test.
Testing the hypothesis that there is an association between factor and SBP classification.
Significant differences exist between designated subgroups at α = .05.
Death rate is based on the adjudication release of June 1, 2015.
SBP Groups and Cognition
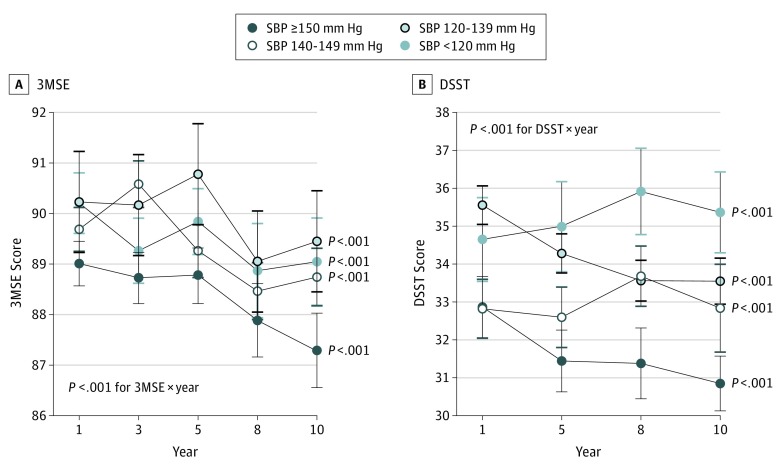
During the 10-year follow-up period, there was a differential decrease in 3MSE and DSST scores by SBP level in patients receiving treatment for hypertension. As shown in Figure 2, the greatest decrease in 3MSE and DSST scores was in the reference group (the covariate-adjusted 10-year decrease in score was 3.7 for the 3MSE and 6.2 for the DSST), and the least was in the group with SBP of 120 mm Hg or lower (the covariate-adjusted 10-year decrease in score was 3.0 for the 3MSE and 5.0 for the DSST). These results of the final multivariate mixed model adjusting for multiple covariates and potential confounders are presented in Table 2.
Figure 2. Cognitive Scores During the 10-Year Study Period by Systolic Blood Pressure (SBP) Levels for Participants Treated for Hypertension in the Health Aging and Body Composition Study.
A, Modified Mini-Mental State Examination (3MSE). B, Digit Symbol Substitution Test (DSST). Statistical significance was tested using the multivariate mixed models adjusted for covariates. The within-group P value test hypothesis, the significance of change within the SBP target group, was obtained from the SLICE statements of the multivariate models.
Table 2. Results of the Mixed Model for the Modified Mini-Mental State Examination and Digit Symbol Substitution Test .
| Characteristic | Modified Mini-Mental State Examination | Digit Symbol Substitution Test | ||
|---|---|---|---|---|
| F Score | P Value | F Score | P Value | |
| Study year | 84.06 | <.001 | 129.47 | <.001 |
| SBP target | 20.82 | <.001 | 7.39 | <.001 |
| SBP group × year | 5.29 | <.001 | 4.30 | <.001 |
| Race | 19.92 | <.001 | 14.35 | <.001 |
| Age | 30.28 | <.001 | 28.03 | <.001 |
| Sex | 0.91 | .34 | 14.23 | <.001 |
| BMI | 0.15 | .70 | 2.38 | .12 |
| Educational level | 28.88 | <.001 | 12.74 | <.001 |
| Income | 2.11 | .10 | 0.20 | .90 |
| Stroke | 1.44 | .23 | 1.38 | .24 |
| Diabetes | 0.08 | .78 | 0.12 | .73 |
| Baseline score | 2505.13 | <.001 | 4845.48 | <.001 |
| Seated DBP | 0.12 | .73 | 0.64 | .43 |
Abbreviations: BMI, body mass index; DBP, diastolic blood pressure; DSST, Digit Symbol Substitution Test; SBP, systolic blood pressure.
Racial Disparity, SBP Levels, and Cognition
At baseline 784 participants were black (47.3%). Compared with the white participants, they were more likely to be women and have a lower educational level and income, a higher body mass index, and a greater prevalence of diabetes and stroke. Baseline cognitive scores (3MSE and DSST) were also lower among black participants than white participants.
There were significant racial differences in the progression of cognitive function, with black participants having a greater mean (SE) 10-year decrease in 3MSE scores (–4.1 [0.4]; P < .001) than white participants (–2.6 [0.3]; P < .001) (P < .001 for race × year) after adjusting for covariates and baseline performances. However, that was not the case for the DSST; the mean (SE) 10-year decrease in DSST scores was –5.8 (0.4) for white participants (P < .001) and –4.7 (0.4) for black participants (P < .001) (P = .09 for race × year).
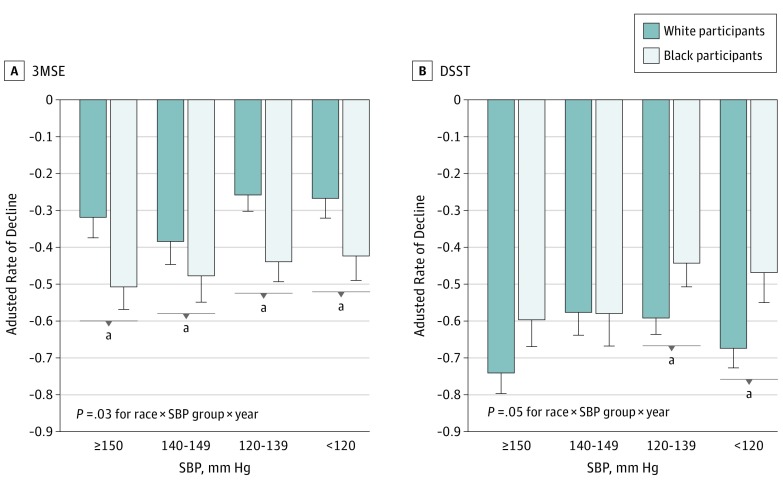
There were also racial differences in the association between SBP levels and cognitive progression, in which lower SBP levels were associated with a slower decrease in 3MSE scores relative to the higher SBP levels in black participants compared with white participants. Compared with white participants, black participants had a greater difference between the higher and lower SBP levels in cognitive decline; adjusted differences between the groups with SBP levels of 150 mm Hg or higher and 120 mm Hg or lower were –0.05 for white participants and –0.08 for black participants for the 3MSE (P = .03 for race × SBP group × year) and –0.07 for white participants and –0.13 for black participants for the DSST (P = .05). Within each SBP group, the covariate-adjusted decrease in 3MSE score was higher and the covariate-adjusted decrease in the DSST score was lower for black participants than for white participants (Figure 3).
Figure 3. Ten-Year Rates of Decrease in Cognitive Scores by Target Systolic Blood Pressure (SBP) and Racial Groups in Treated for Hypertension in the Health Aging and Body Composition Study.
A, Modified Mini-Mental State Examination (3MSE). B, Digit Symbol Substitution Test (DSST). Rates are the covariate-adjusted rates of the trajectories during the 10-year follow-up within each race and SBP group calculated from the overall mixed models. Statistical significance was tested using the multivariate mixed models adjusted for covariates. The P values for the SBP group × year within black and white participants were less than .001 for both cognitive tests. aIndicates if there was a difference in the rates of decline within the SBP group between the 2 races.
Discussion
The findings of this study suggest that lower SBP targets, such as those recommended by JNC-7 or used in SPRINT, are overall superior from the cognitive perspective to the higher targets of JNC-8. As opposed to prior observational studies in which a heterogeneous group was included (treated or untreated and individuals with hypertension and those without hypertension), our analysis supports the finding that higher SBP is not associated with better cognitive outcomes. This study highlights that when important methodological issues are considered (such as limiting sample heterogeneity, accounting for time-varying blood pressures, and addressing the reverse-association confounder of hypertension and cognition), observational studies provide more consistent results with clinical trials.
Our finding that persons with SBP levels of 150 mm Hg or higher may have poorer cognitive outcomes is consistent with the findings of a recent study examining participants enrolled in the National Institutes of Health–National Institute on Aging Alzheimer Disease Centers. In that study, persons 60 years of age or older with normal cognition at baseline and a consistently elevated SBP of 150 mm Hg or higher had a steeper decline on the Mini-Mental State Examination during a 3-year follow-up period than did persons with lower SBP targets. The present study extends that to a longer follow-up and demonstrates the importance of lower treatment targets in an even older segment of the population.
Conflicting guidelines have been issued regarding the management of hypertension in older adults, with the main concern being that lower targets are linked to poorer cognitive performance. These concerns have led to a higher SBP target recommendation for elderly patients. However, the results of SPRINT have suggested that, from a cardiovascular perspective, this link may not be completely accurate. The present study suggests that target SBP levels of lower than 140 mm Hg and possibly 120 mm Hg or lower extend to cognitive outcomes as well. These issues are critical for defining the concept of blood pressure control, for clinical guidelines and recommendations as well as for quality-based assessments of health care.
The findings of the present study suggest that a lower SBP target for black patients is linked to greater cognitive benefit. Almost all guidelines have recommended that target blood pressures be similar for black and white patients. A recent study reported that, for the same blood pressure level, self-reported cognitive limitations are higher in black patients. That study also identified an association between cognitive symptoms and increased mortality. Future recommendations for the management of hypertension and cognitive outcomes need to take this racial disparity into consideration. Our finding was independent of cardiovascular disease, stroke, and other risk factors. Although statistical adjustment does not completely discount the role these factors played in the associations between hypertension and cognition, these data suggest a race-specific risk for the development of cognitive decline from hypertension beyond these factors. Further investigations into other mechanisms based on prior literature, such as cerebrovascular changes, inflammation, or oxidative stress, may be warranted in black patients with hypertension. We unexpectedly observed a slower rate of decreasing DSST scores among black participants, especially among those with lower SBP levels after adjusting for other risk factors. These trends may be related to the greater impact of lower SBP levels in this group. These observations need to be replicated in other cohorts and confirmed by clinical trials.
Although we found statistical significance in these analyses, the magnitude of the change over the 10-year period was small. Nevertheless, we did not observe an association between lower targets and cognition that was significantly detrimental. This analysis, which was specifically conducted for older adults receiving treatment for hypertension, provides the additional suggestion that the potential for a detrimental cognitive outcome of a target SBP lower than 140 or 120 mm Hg is not substantiated with appropriately designed analyses of observational data.
Strengths and Limitations
The advantages of this study are the long-term follow-up; the statistical modeling of the change over time in blood pressure, covariates, and cognition; and the large number of black participants in the sample, allowing us to test for racial differences. A limitation of these analyses is the observational nature of the study design. Differences in classes of antihypertensive medications and the degree of blood-pressure lowering that physicians might pursue, especially in the racial comparisons, are important factors to consider when interpreting these results. Also, observational studies of drug effects have a significant bias by indication related to the initiation of treatment. We have minimized that bias by excluding untreated individuals. Nevertheless, residual confounding is a limitation that is unavoidable in any observational analysis. Furthermore, in our analyses, we adjusted for baseline cognition. This adjustment minimizes the effect of baseline differences in cognition on our results but also introduces bias into the interpretation because it is conceivable that participants may have been experiencing cognitive decline even before the study started.
Other limitations include the lack of additional cognitive biomarkers such as neuroimaging and the limited number of cognitive tests conducted on the sample. Finally, it is important to note that, in contrast to clinical trial data, in which the intention-to-treat analysis classifies people based on their initial assignment at randomization, our analysis by design classified participants into groups based on their blood-pressure levels at each visit. This difference is important when interpreting these results with the SPRINT targets; SPRINT was a randomized clinical trial that evaluated the effects of intensive (<120 mm Hg) vs standard (<140 mm Hg) SBP targets for individuals 75 years of age or older with hypertension but without diabetes. It was stopped after approximately 3 years. Our study uses observational data with no randomization or specific target SBP definitions, which were managed by the participants’ clinicians. This issue needs to be considered when interpreting the results of our analysis. Furthermore, because of the small number of individuals with diabetes or kidney disease within each subgroup, we did not have the power to assess the association of SBP targets relevant to diabetes or kidney disease status.
Conclusions
This analysis of 10-year data from older adults receiving treatment for hypertension in the Health ABC study suggests that lower SBP levels are associated with greater cognitive protection. The lower targets may offer greater protection for older black adults with hypertension. Future guidelines need to consider this racial difference when reviewing or providing recommendations for management of hypertension.
References
- 1.James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520. [DOI] [PubMed] [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, et al. ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee . Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206-1252. [DOI] [PubMed] [Google Scholar]
- 3.Oates DJ, Berlowitz DR, Glickman ME, Silliman RA, Borzecki AM. Blood pressure and survival in the oldest old. J Am Geriatr Soc. 2007;55(3):383-388. [DOI] [PubMed] [Google Scholar]
- 4.Skoog I, Lernfelt B, Landahl S, et al. 15-Year longitudinal study of blood pressure and dementia. Lancet. 1996;347(9009):1141-1145. [DOI] [PubMed] [Google Scholar]
- 5.Kivipelto M, Helkala EL, Hänninen T, et al. Midlife vascular risk factors and late-life mild cognitive impairment: a population-based study. Neurology. 2001;56(12):1683-1689. [DOI] [PubMed] [Google Scholar]
- 6.Gottesman RF, Schneider AL, Albert M, et al. Midlife hypertension and 20-year cognitive change: the Atherosclerosis Risk in Communities Neurocognitive study. JAMA Neurol. 2014;71(10):1218-1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wright JT Jr, Williamson JD, Whelton PK, et al. ; SPRINT Research Group . A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Molander L, Gustafson Y, Lövheim H. Low blood pressure is associated with cognitive impairment in very old people. Dement Geriatr Cogn Disord. 2010;29(4):335-341. [DOI] [PubMed] [Google Scholar]
- 9.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988-1994 and 1999-2004. Hypertension. 2008;52(5):818-827. [DOI] [PubMed] [Google Scholar]
- 10.Lackland DT. Racial differences in hypertension: implications for high blood pressure management. Am J Med Sci. 2014;348(2):135-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Douglas JG, Thibonnier M, Wright JT Jr. Essential hypertension: racial/ethnic differences in pathophysiology. J Assoc Acad Minor Phys. 1996;7(1):16-21. [PubMed] [Google Scholar]
- 12.Calhoun DA, Oparil S. Racial differences in the pathogenesis of hypertension. Am J Med Sci. 1995;310(suppl 1):S86-S90. [DOI] [PubMed] [Google Scholar]
- 13.Summerson JH, Bell RA, Konen JC. Racial differences in the prevalence of microalbuminuria in hypertension. Am J Kidney Dis. 1995;26(4):577-579. [DOI] [PubMed] [Google Scholar]
- 14.Hajjar I, Wharton W, Mack WJ, Levey AI, Goldstein FC. Racial disparity in cognitive and functional disability in hypertension and all-cause mortality. Am J Hypertens. 2016;29(2):185-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beckett NS, Peters R, Fletcher AE, et al. ; HYVET Study Group . Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887-1898. [DOI] [PubMed] [Google Scholar]
- 16.Hall WD. Representation of blacks, women, and the very elderly (aged > or = 80) in 28 major randomized clinical trials. Ethn Dis. 1999;9(3):333-340. [PubMed] [Google Scholar]
- 17.Wechsler D. WMS-R: Wechsler Memory Scale–Revised: manual. San Antonio, TX: Psychological Corp.: Harcourt Brace Jovanovich; 1987. [Google Scholar]
- 18.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48(8):314-318. [PubMed] [Google Scholar]
- 19.Littell RC, Henry PR, Ammerman CB. Statistical analysis of repeated measures data using SAS procedures. J Anim Sci. 1998;76(4):1216-1231. [DOI] [PubMed] [Google Scholar]
- 20.Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. 2nd ed Hoboken, NJ: Wiley; 2011. [Google Scholar]
- 21.Padgett LV. Practical Statistical Methods: A SAS Programming Approach. Boca Raton, FL: CRC Press; 2011. [Google Scholar]
- 22.Brown H, Prescott R. Applied Mixed Models in Medicine. 3rd ed Hoboken, NJ: John Wiley & Sons Inc.; 2015. [Google Scholar]
- 23.Goldstein FC, Hajjar IM, Dunn CB, Levey AI, Wharton W. The relationship between cognitive functioning and the JNC-8 guidelines for hypertension in older adults. J Gerontol A Biol Sci Med Sci. 2017;72(1):121-126. [DOI] [PMC free article] [PubMed] [Google Scholar]