This meta-analysis quantifies the rates of suicide after discharge from psychiatric facilities and examines what moderates those rates.
Key Points
Questions
What is the suicide rate after discharge from psychiatric facilities, and what factors influence it?
Findings
In this meta-analysis of 100 studies of 183 patient samples, the postdischarge suicide rate was approximately 100 times the global suicide rate during the first 3 months after discharge and patients admitted with suicidal thoughts or behaviors had rates near 200 times the global rate. Even many years after discharge, previous psychiatric inpatients have suicide rates that are approximately 30 times higher than typical global rates.
Meaning
Although recently discharged patients and those who were admitted because of suicidal ideas and behaviors are at particular risk of suicide, all discharged patients have an enduring high suicide rate and should have ongoing access to health care resources.
Abstract
Importance
High rates of suicide after psychiatric hospitalization are reported in many studies, yet the magnitude of the increases and the factors underlying them remain unclear.
Objectives
To quantify the rates of suicide after discharge from psychiatric facilities and examine what moderates those rates.
Data Sources
English-language, peer-reviewed publications published from January 1, 1946, to May 1, 2016, were located using MEDLINE, PsychINFO, and EMBASE with the search terms ((suicid*).ti AND (hospital or discharg* OR inpatient or in-patient OR admit*).ab and ((mortality OR outcome* OR death*) AND (psych* OR mental*)).ti AND (admit* OR admis* or hospital* OR inpatient* OR in-patient* OR discharg*).ab. Hand searching was also done.
Study Selection
Studies reporting the number of suicides among patients discharged from psychiatric facilities and the number of exposed person-years and studies from which these data could be calculated.
Data Extraction and Synthesis
The meta-analysis adhered to Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) and Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines. A random-effects model was used to calculate a pooled estimate of postdischarge suicides per 100 000 person-years.
Main Outcomes and Measures
The suicide rate after discharge from psychiatric facilities was the main outcome, and the association between the duration of follow-up and the year of the sampling were the main a priori moderators.
Results
A total of 100 studies reported 183 patient samples (50 samples of females, 49 of males, and 84 of mixed sex; 129 of adults or unspecified patients, 20 of adolescents, 19 of older patients, and 15 from long-term or forensic discharge facilities), including a total of 17 857 suicides during 4 725 445 person-years. The pooled estimate postdischarge suicide rate was 484 suicides per 100 000 person-years (95% CI, 422-555 suicides per 100 000 person-years; prediction interval, 89-2641), with high between-sample heterogeneity (I2 = 98%). The suicide rate was highest within 3 months after discharge (1132; 95% CI, 874-1467) and among patients admitted with suicidal ideas or behaviors (2078; 95% CI, 1512-2856). Pooled suicide rates per 100 000 patients-years were 654 for studies with follow-up periods of 3 months to 1 year, 494 for studies with follow-up periods of 1 to 5 years, 366 for studies with follow-up periods of 5 to 10 years, and 277 for studies with follow-up periods longer than 10 years. Suicide rates were higher among samples collected in the periods 1995-2004 (656; 95% CI, 518-831) and 2005-2016 (672; 95% CI, 428-1055) than in earlier samples.
Conclusions and Relevance
The immediate postdischarge period is a time of marked risk, but rates of suicide remain high for many years after discharge. Patients admitted because of suicidal ideas or behaviors and those in the first months after discharge should be a particular focus of concern. Previously admitted patients should be able to access long-term care and assistance.
Introduction
Suicide is among the top 20 causes of death worldwide. The World Health Organization estimates that the global age-standardized suicide rate was 11.4 per 100 000 person-years in 2012. Most suicides occur in individuals with mental illness, and virtually all mental disorders are associated with increased suicide-associated mortality. Mentally ill persons who have been discharged from psychiatric hospitals and wards seem to have a greater risk for suicide than other mentally ill persons.
The rate of suicide after discharge from psychiatric hospitals and wards (referred to herein as postdischarge suicide) is very high. A recent US study reported a suicide rate of 178 per 100 000 person-years in the first 3 months after discharge, a figure that is approximately 15 times the US national suicide rate. Studies from the United Kingdom and Nordic countries with similar durations of follow-up after discharge have reported higher suicide rates. Currently, there are no accepted benchmarks for postdischarge suicide rates.
A synthesis of the existing literature about rates of postdischarge suicide would help quantify the extent of this issue and would complement an earlier meta-analysis of risk factors for postdischarge suicide by estimating expected base rates. A meta-analysis could help clarify the time course of postdischarge suicide risk and examine progress in reducing postdischarge suicide.
The first aim of this study was to calculate a pooled estimate and statistical dispersion (range, median, and interquartile range) of postdischarge suicide rates. The second aim was to explore whether the observed heterogeneity in postdischarge suicide rates was associated with the duration of follow-up after discharge and the year in which the samples were collected. We also explored potential associations between suicide rates and a predetermined set of moderator variables defined by demographic characteristics, clinical factors, and study methods.
Methods
We conducted a registered meta-analysis of rates of postdischarge suicides according to the Meta-analysis of Observational Studies in Epidemiology (MOOSE) and Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines.
Search Strategy
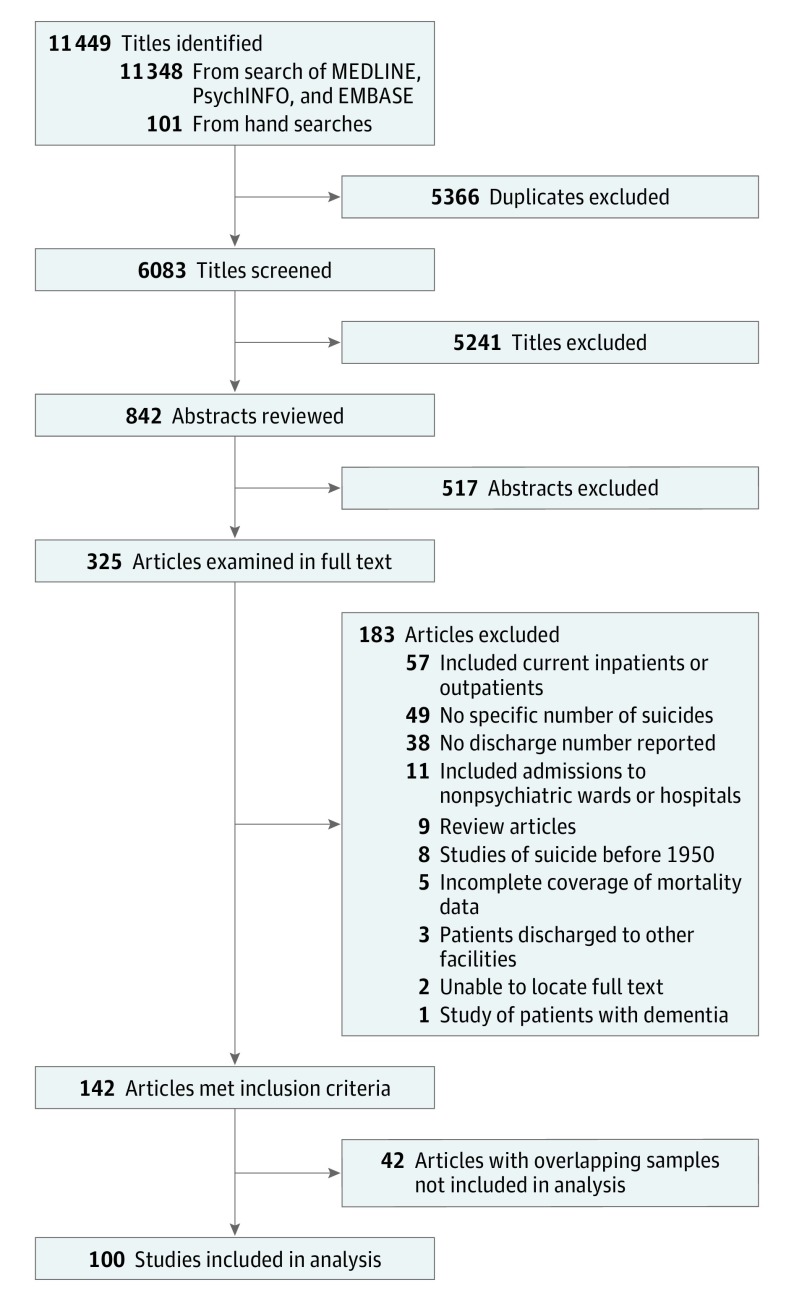
Two of us (D.T.C. and M.M.L.) independently searched MEDLINE, PsychINFO, and EMBASE for relevant articles published in English from January 1, 1946, to May 1, 2016, with the search terms ((suicid*).ti AND (hospital or discharg* OR inpatient or in-patient OR admit*).ab and ((mortality OR outcome* OR death*) AND (psych* OR mental*)).ti AND (admit* OR admis* or hospital* OR inpatient* OR in-patient* OR discharg*).ab (Figure 1). Electronic searches were supplemented by hand searches of the relevant review articles. Gray literature was not considered. Two of us (D.T.C., M.M.L.) independently winnowed titles, abstracts, and full-text publications.
Figure 1. Flowchart of Searches for Studies Reporting Rates of Suicide Among Discharged Psychiatric Patients.
Inclusion and Exclusion Criteria
We included studies that reported the number of suicides among patients discharged from psychiatric hospitals or wards and the number of person-years in which the suicides occurred. We also included studies from which these data could be calculated using the reported suicide rate, the mean length of patient follow-up, or the duration of follow-up.
Studies of suicide attempts, community patients, and current inpatients; conducted before 1950; and with discharge from nonpsychiatric settings were excluded. Studies were excluded if the number of suicides and number of person-years were not reported, could not be calculated, or could not be obtained by email from the authors. When 2 studies reported completely overlapping samples (eg, when one study was conducted at a national level and another study was from a single hospital in that country in the same period), the study with fewer person-years was excluded. When 2 studies had partial overlap, both studies were included if less than 20% of the participants in the smaller study were included in the larger study.
Data Extraction
Two of us (D.T.C., M.M.L.) independently extracted the data. When studies reported multiple samples, nonoverlapping samples were selected according to a hierarchy of sex, age group (adolescents, adults, and those >65 years of age), duration of follow-up, year of the suicide, and diagnostic group, such that no participant in any single study was included more than once. In some publications, the number of person-years could be calculated using the number of suicides and reported suicide rate. In other publications, the number of person-years was estimated using the reported duration of follow-up.
A predetermined list of moderator variables was extracted for each sample: the duration of follow-up, the year or midyear of data collection, the country in which the study was conducted, sex (male, female, or mixed), age at discharge (adolescent, adult, unspecified by age, >65 years of age), whether the patients were discharged from long-term or forensic facilities, whether the patients were defined by an admission for suicidality (defined as an admission associated with a suicide attempt or suicidal ideation), whether the samples were of patients followed up after their first psychiatric admission (first-admission patients), and the psychiatric diagnosis (psychosis, affective disorder, or mixed and other diagnoses). The corresponding national suicide rate in the country during the year of the study was obtained using World Health Organization data for each sample.
Strength of Reporting Scale
The strength of reporting of each study was assessed using a 5-point scale derived from the Newcastle-Ottawa Scale for assessing the quality of nonrandomized studies. One point was awarded if the study identified suicides by using coroners’ records or a national mortality database (rather than using hospital records), included all the postdischarge suicides in a defined geographic region (rather than suicides from a particular care setting), included open verdicts in suicide numbers, reported the number of individuals (rather than the number of discharges), or reported the number of person-years directly or the mean length of patient follow-up from which the number of person-years could be calculated directly. Studies that included open verdicts were regarded as being of higher quality because of evidence that open-verdict cases are often regarded as suicides by researchers.
Statistical Analysis
The suicide rate per patient-year was the effect size measure. The pooled effect size was calculated using a random-effects model because we considered that the different patient groups in different countries during different periods were unlikely to have a common effect size. The studies were weighted according to their inverse variance, τ2 was calculated using the Paule-Mandel method, and the suicide rates were log transformed and reported in rates per 100 000 person-years. The significance test of the pooled suicide rate was conducted with a null hypothesis of 11.4 events per 100 000 person-years. Between-study heterogeneity was assessed using the Cochran Q and I2 statistics. Possible publication bias was tested by examination of the funnel plot and by an Egger regression. The analysis was conducted using R packages meta and metafor.
Sources of between-sample heterogeneity were investigated using subgroup analysis with categorical moderators and meta-regression with continuous moderators. Continuous moderators examined by meta-regression and categorical moderators examined using subgroup analysis and Cochran Q that were significantly associated with heterogeneity in suicide rates (α<.05) were entered into a mixed-effects multiple meta-regression model. The length of follow-up was dichotomized (≤12 months coded as 1, >12 months coded as 0) for the purpose of the multiple meta-regression.
Results
Searches and Data Extraction
A total of 142 full-text peer-reviewed publications met our inclusion criteria before being examined for possible overlapping participants (Figure 1). Two of us (D.T.C., M.M.L.) identified 113 of the 142 publications (79.6%). A total of 100 publications were included after the removal of overlapping studies (eTable 1 in the Supplement). These studies reported 183 separate samples of discharged patients. Forty-two publications were excluded because of overlap with larger publications (eTable 2 in the Supplement). Of the 183 patient samples, 50 were of females, 49 were of males, and 84 were of mixed sex (eTable 3 in the Supplement). A total of 129 samples were of adults or unspecified patients, 20 were of adolescents (≤18 years of age at the time of discharge), and 19 samples were of older patients (≥65 years of age at the time of discharge). Fifteen samples were of patients discharged from long-term or forensic facilities, and 23 samples were of first-admission patients. Nine samples were of patients who had been admitted with suicidality. There were disagreements about 40 of the 366 data points relating to effect size. All disagreements were resolved by a second examination of the data (D.T.C., M.M.L.).
Sample Characteristics
The 100 studies with 183 samples reported 17 857 suicides during 4 725 445 person-years. The mean (SD) number of suicides per sample was 97.6 (321.6) (median, 12; range, 0-2822), and the mean (SD) number of person-years per sample was 25 822 (111 914) (median, 3534; range, 17-1 393 800). The median sample suicide rate was 461 per 100 000 person-years, with a range of 0 to 6259 per 100 000 person-years. The interquartile range was 207 to 919 per 100 000 person-years.
The median duration of follow-up was 60 months (range, 1-432 months; interquartile range, 12-112 months). The earliest study reported a sample with a midpoint in 1967, the median year of the samples was 1992, and the most recent study reported suicides that occurred in 2014.
Twenty-seven samples were from Asian countries, 10 samples were from Australasia, 30 from mainland Europe, 40 from Nordic countries, 32 from North America, and 42 from the United Kingdom or Ireland. There was 1 sample each from Israel and Brazil.
Meta-analysis
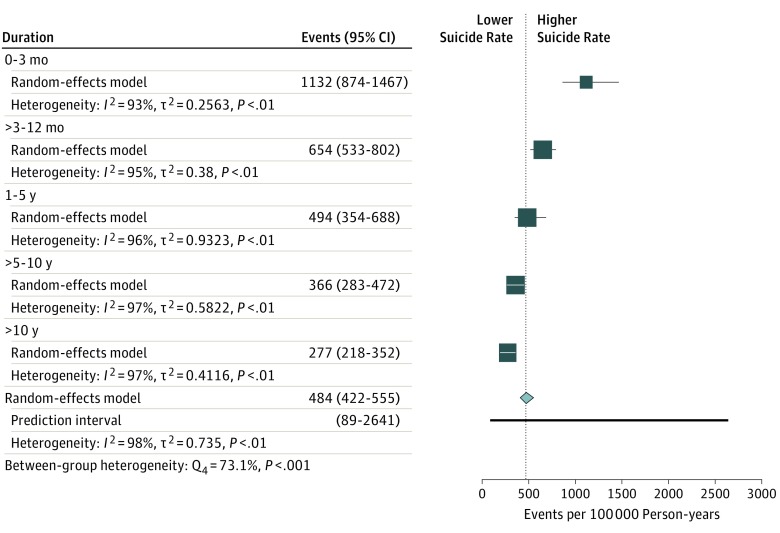
The pooled rate of suicide after discharge was 484 per 100 000 person-years (95% CI, 422-555 per 100 000 person-years; prediction interval, 89-2641; P < .001, assuming a null hypothesis of 11.4 per 100 000 person-years) with very high between-sample heterogeneity (n = 183, Q182 = 9768, P < .001, I2 = 98%, τ2 = 0.86). The pooled suicide rate among 18 samples with a follow-up of 3 months or less was 1132 per 100 000 person-years (95% CI, 874-1467 per 100 000 person-years; I2 = 93%) and decreased thereafter in studies with follow-up of 3 to 12 months (654 [95% CI, 533-802]; 43 samples; I2 = 95%), 1 to 5 years (494 [95% CI, 354-688]; 44 samples; I2 = 96%), 5 to 10 years (366 [95% CI, 283-472]; 44 samples; I2 = 97%), and greater than 10 years (277 [95% CI, 218-352]; 34 samples; I2 = 97%). The duration of follow-up was significantly associated with between-group heterogeneity (Q4 = 73.1; P < .001) (Figure 2).
Figure 2. Suicide Rates According to Duration of Follow-up.
Error bars indicate 95% CIs.
More recently conducted studies had higher rates of suicide per 100 000 person-years than older studies (2005-2016: 672 [95% CI, 428-1055]; 27 samples; I2 = 98%; 1995 to 2004: 656 [95% CI, 518-831]; 51 samples; I2 = 99%; 1985 to 1994: 404 [95% CI, 322-508]; 46 samples; I2 = 98%; 1975 to 1984; 373 [95% CI, 279-498]; 47 samples; I2 = 96%; before 1975; 423 [95% CI, 316-567]; 12 samples; I2 = 75%). The period of sample collection was significantly associated with between-sample heterogeneity (Q4 = 14.7; P = .005).
Difference in postdischarge suicide rates according to geographic region were not statistically significant (Q6 = 10.6; P = .10) (Asia: 632 [95% CI, 434-921]; 27 samples; I2 = 95%; Australasia: 423 [95% CI, 164-1090]; 10 samples; I2 = 96%; Mainland Europe: 502 [95% CI, 375-672]; 30 samples; I2 = 96%; Nordic countries: 562 [95% CI, 430-735]; 40 samples; I2 = 97%; North America: 308 [95% CI, 220-430]; 32 samples; I2 = 94%; United Kingdom and Ireland: 513 [95% CI, 410-642]; 42 samples; I2 = 98%; other: 261 [95% CI, 7-9940]; 2 samples; I2 = 98%).
The suicide rate was lower among cohorts of adolescents (158 per 100 000 person-years) compared with samples of adults (555 per 100 000 person-years), patients from long-term or forensic discharge facilities (487 per 100 000 person-years), and older patients (496 per 100 000 person-years) (Table 1). Samples of persons discharged after an admission for suicidality (2078 per 100 000 person-years) had more than 4 times the suicide rate of other samples (452 per 100 000 person-years) (Table 1). Rates of suicide were lower among first-admission patients (305 per 100 000 person-years) (Table 1). Samples of patients with psychosis (599 per 100 000 person-years), affective disorder (524 per 100 00 person-years), and mixed and other diagnoses (463 per 100 000 person-years) had similar suicide rates (P = .40). There was no significant difference in suicide rates according to sex (533 for males, 412 for females, and 503 for mixed per 100 000 person-years; P = .34) or total strength of reporting scores (488 for lower scores and 526 for higher scores per 100 000 person-years; P = .30) (Table 1).
Table 1. Main Results and Analyses of Subgroups.
| Variable | No. of Samples | No. of Suicides | Total No. of Person-years | Estimated Suicide Rate per 100 000 Person-years (95% CI) | I2, % | Cochran Q | P Value |
|---|---|---|---|---|---|---|---|
| Effects | 17 857 | 4 725 445 | 98 | 9768 | <.001a | ||
| Random | 183 | 484 (422-555) | |||||
| Fixed | 183 | 509 (502-517) | |||||
| Sex | |||||||
| Female | 50 | 3335 | 948 434 | 412 (318-534) | 95 | 2.2 | .34 |
| Male | 49 | 4024 | 810 071 | 533 (415-685) | 96 | ||
| Mixed | 84 | 10 498 | 2 966 941 | 503 (407-622) | 99 | ||
| Age | |||||||
| Adolescent | 20 | 106 | 80 490 | 158 (112-225) | 54 | 41.5 | <.001 |
| Adults and unspecified by age | 129 | 17 221 | 4 506 808 | 555 (474-650) | 99 | ||
| ≥65 y | 19 | 296 | 85 504 | 496 (353-695) | 76 | ||
| Long-term or forensic discharge facility | 15 | 95 | 21 819 | 487 (376-632) | 21 | ||
| Diagnosis | |||||||
| Affective disorder | 18 | 3394 | 620 690 | 524 (370-742) | 95 | 2.0 | .40 |
| Psychosisb | 24 | 437 | 75 812 | 599 (430-834) | 88 | ||
| Mixed and other | 141 | 14 026 | 4 028 943 | 463 (393-545) | 99 | ||
| Sample type | |||||||
| Suicidal patients | 9 | 45 | 2479 | 2078 (1512-2856) | 16 | 75.0 | <.001 |
| Not selected on the basis of suicidality | 174 | 17 812 | 4 722 966 | 452 (396-517) | 98 | ||
| Postdischarge follow-up status | |||||||
| First admission | 23 | 3684 | 1 904 192 | 305 (193-481) | 98 | 75.0 | <.001 |
| Mixed first and earlier admitted | 160 | 14 173 | 2 821 253 | 517 (449-595) | 97 | ||
| Reporting strength | |||||||
| Lower ≤3 | 103 | 6836 | 2 827 162 | 448 (369-543) | 96 | 1.3 | .30 |
| Higher ≥4 | 80 | 11 020 | 1 898 283 | 526 (433-639) | 98 |
Null hypothesis: effect is equal to 11.4 events per 100 000 person-years.
Includes one sample of patients with affective psychosis.
Publication Bias, Meta-regression, and Multiple Meta-regression
The funnel plot was symmetrical and the Egger regression was not significant (intercept, −0.27; t181 = −38; P = .70), suggesting an absence of publication bias. Samples with longer durations of follow-up were more likely to report lower suicide rates (coefficient = −0.0049; 95% CI, −0.0064 to −0.0034; z = −6.34; P < .001). Samples reporting suicides from more recent studies reported higher suicide rates than older studies (coefficient = 0.02; 95% CI, 0.008-0.031; z = 3.40; P = .007). The general population suicide rate was not associated with rates of suicide among discharged patients (coefficient = 0.0064; 95% CI, −0.019 to 0.032; z = 0.49; P = .60).
Five moderators that were associated with between-sample heterogeneity were included in a mixed-effects multiple meta-regression model (Table 2). More recent samples, samples with follow-up of a year or less, and samples of suicidal patients were independently associated with higher postdischarge suicide rates. Samples of adolescent patients were independently associated with lower rates. This model accounted for 39% of the observed between-sample variance.
Table 2. Multiple Meta-regression Using Covariates Associated With Between-Sample Heterogeneity in Postdischarge Suicide Ratesa.
| Covariate | Coefficient (SE) [95% CI] | z Score | P Value | |
|---|---|---|---|---|
| Midyear of sample | 0.011 (0.005) [0.0007 to 0.020] | 2.10 | .04 | |
| Follow-up ≤12 mo | 0.63 (0.12) [0.39 to 0.87] | 5.15 | <.001 | |
| Suicidal patients | 1.46 (0.29) [0.89 to 2.02] | 5.02 | <.001 | |
| Adolescent | −0.86 (0.21) [−1.27 to −0.44] | −4.05 | <.001 | |
| First admission | −0.10 (0.17) [−0.45 to 0.24] | −0.59 | .56 | |
| Intercept | −26.40 (9.93) [−45.86 to −6.93] | −2.66 | .008 |
n = 183, Q5 = 100.8, R2 analog = 0.39.
Discussion
This study synthesizes more than half a century of research into postdischarge suicide rates. We identified a large number of studies reporting more than 17 000 suicides in almost 5 million person-years at a pooled rate of 484 per 100 000 person-years. This figure is more than 3 times the suicide rate estimated in a comparable study of the suicide rate among inpatients and 44 times the global suicide rate of 11.4 per 100 000 patients per year in 2012. The suicide rate of studies that followed up patients for no more than 3 months was 100 times the global suicide rate. Studies with follow-up periods of 3 to 12 months had almost 60 times the global suicide rates, and the suicide rate among discharged patients was more than 30 times that in the general population even for periods of follow-up of 5 to 10 years.
Nordentoft et al recently described the phenomenon of postdischarge suicide as a “nightmare and disgrace.”(p 1) We agree; however, they formed this view in the light of a recent study that found a rate of suicide of 178 per 100 000 patients per year during the first 3 months after discharge. Of note, our meta-analytic estimate during the same duration of follow-up is more than 6 times higher.
Our data suggest that the suicide rates among discharged patients have not decreased in the past 50 years. This is a disturbing finding considering the increase in community psychiatry and the availability of a range of new treatments during this period. The increase that we observed in postdischarge suicides can be seen in the context of the recent finding of a more extreme increase in the suicide rate among current inpatients from 68 per 100 000 person-years in the 1960s and 1970s to 646 per 100 000 person-years since 2000. An increase in the suicide rate of admitted and discharged patients might be attributable to multiple factors, including changing legal and other criteria for admission, shorter lengths of inpatient treatment, increased prevalence of substance use, and a greater acuity of illness among those admitted in the era of deinstitutionalization. Publication bias in favor of recent studies from regions with a higher suicide rate might have also contributed to the observed increase in suicide rates over time.
The marked variation in postdischarge suicide rates was not fully explained by the duration of follow-up or the year of the sample. Studies with similar periods of follow-up and studies conducted in the same or similar years have between-study heterogeneity that is similar to that of the whole sample.
Limitations
Our study has a number of limitations, most relating to the high between-sample heterogeneity. Although we were able to explain some heterogeneity by using moderator variables, further unexplained heterogeneity might be attributable to factors that were not reported in the primary research. Few of the included studies reported comparisons of those who committed suicide with those who survived, and information about the psychiatric care that the patients received in hospital or after discharge was absent. For example, the included studies did not report on the extent of any association between readmission and suicide. The association between readmission and suicide might matter because we found that samples of first-admission patients had a lower postdischarge suicide rate than samples of patients with a mix of first-time and previous patients. This finding suggests that readmission might be an important suicide risk factor.
Other limitations relate to the representativeness of the included studies. Almost all the research came from high-income economies of Asia, Australasia, North America, and Europe, and our results might not be representative of postdischarge suicide in low- and middle-income countries. Even the pooled results that we obtained from our 6 regions were heterogeneous and should not be considered to be a generalizable benchmark for all psychiatric hospital settings in high-income countries.
Furthermore, factors that are associated with increased suicide risk at an aggregate level should be interpreted cautiously and are not necessarily applicable to individual patients. For example, we found that samples of older patients had a higher suicide rate than samples of adolescents, whereas a meta-analysis of risk factors for suicide after discharge found that older age was not associated with an increased suicide risk. Likewise, we found that samples of patients with affective disorders did not have a particularly high suicide rate, whereas the earlier meta-analysis found an association between suicide and depressive symptoms and disorders.
Finally, our study did not estimate the suicide rate in the days immediately after discharge. Some studies have suggested that the days immediately after discharge are the period of the highest suicide risk, but our methods yielded insufficient numbers of samples to robustly estimate suicide rates during periods of less than 3 months. It is likely that rates of suicide in the initial period after discharge are substantially higher than the rate we report during the 3 months.
Conclusions
It has been argued that a way of combatting postdischarge suicide is to focus on individual patients with clinical characteristics that signify a high suicide risk. However, the very high suicide rates calculated in this study and the known limitations of suicide risk assessment suggest that a focus on clinical risk assessment might mislead clinicians into thinking that some patients can be regarded as having low risk after discharge. Our findings better support the views of authors who believe in a more universal approach to suicide prevention that might focus on periods of high risk but that extends for periods of years. However, the findings should curb enthusiasm for restrictive interventions directed at patients labeled as having high risk of suicide by virtue of demographic or clinical variables. Our figures suggest that 0.28% of all discharged patients can be expected to commit suicide during the first 3 months after discharge. The modest statistical strength of suicide risk assessment means that even patients who are classified as having high risk because of their suicide risk factors will have a low absolute probability of suicide over clinically meaningful time frames, whereas patients with a low risk for suicide will still have a probability of suicide that is many times that in the general community.
Discharged patients have suicide rates many times that in the general community. Efforts aimed at suicide prevention should start while patients are in hospital, and the period shortly after discharge should be a time of increased clinical focus. However, our study also suggests that previously admitted patients, particularly those with prior suicidality, remain at a markedly elevated risk of suicide for years and should be a focus of efforts to decrease suicide in the community.
eTable 1. Included Studies
eTable 2. Excluded Studies
eTable 3. Sample-Level Data, Strength of Reporting, and Study Characteristics
References
- 1.World Health Organization Suicide Data. http://www.who.int/gho/mental_health/en/. Accessed July 30, 2016.
- 2.Cho SE, Na KS, Cho SJ, Im JS, Kang SG. Geographical and temporal variations in the prevalence of mental disorders in suicide: systematic review and meta-analysis. J Affect Disord. 2016;190:704-713. [DOI] [PubMed] [Google Scholar]
- 3.Harris EC, Barraclough B. Suicide as an outcome for mental disorders: a meta-analysis. Br J Psychiatry. 1997;170:205-228. [DOI] [PubMed] [Google Scholar]
- 4.Hjorthøj CR, Madsen T, Agerbo E, Nordentoft M. Risk of suicide according to level of psychiatric treatment: a nationwide nested case-control study. Soc Psychiatry Psychiatr Epidemiol. 2014;49(9):1357-1365. [DOI] [PubMed] [Google Scholar]
- 5.Olfson M, Wall M, Wang S, et al. Short-term suicide risk after psychiatric hospital discharge. JAMA Psychiatry. 2016;73(11):1119-1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldacre M, Seagroatt V, Hawton K. Suicide after discharge from psychiatric inpatient care. Lancet. 1993;342(8866):283-286. [DOI] [PubMed] [Google Scholar]
- 7.Geddes JR, Juszczak E, O’Brien F, Kendrick S. Suicide in the 12 months after discharge from psychiatric inpatient care, Scotland 1968-92. J Epidemiol Community Health. 1997;51(4):430-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Madsen T, Nordentoft M. Changes in inpatient and postdischarge suicide rates in a nationwide cohort of Danish psychiatric inpatients, 1998-2005. J Clin Psychiatry. 2013;74(12):e1190-e1194. [DOI] [PubMed] [Google Scholar]
- 9.Pirkola S, Sohlman B, Heilä H, Wahlbeck K. Reductions in postdischarge suicide after deinstitutionalization and decentralization: a nationwide register study in Finland. Psychiatr Serv. 2007;58(2):221-226. [DOI] [PubMed] [Google Scholar]
- 10.Large M, Sharma S, Cannon E, Ryan C, Nielssen O. Risk factors for suicide within a year of discharge from psychiatric hospital: a systematic meta-analysis. Aust N Z J Psychiatry. 2011;45(8):619-628. [DOI] [PubMed] [Google Scholar]
- 11.Stroup DF, Berlin JA, Morton SC, et al. ; Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group . Meta-analysis of Observational Studies in Epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008-2012. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006-1012. [DOI] [PubMed] [Google Scholar]
- 13.Wells GA, Shea B, O’Connnell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed January 6, 2016.
- 14.Palmer BS, Bennewith O, Simkin S, et al. Factors influencing coroners’ verdicts: an analysis of verdicts given in 12 coroners’ districts to researcher-defined suicides in England in 2005. J Public Health (Oxf). 2015;37(1):157-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Linsley KR, Schapira K, Kelly TP. Open verdict v. suicide—importance to research. Br J Psychiatry. 2001;178:465-468. [DOI] [PubMed] [Google Scholar]
- 16.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629-634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.R Core Team R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/. 2013. Accessed February 28, 2017.
- 18.Ajetunmobi O, Taylor M, Stockton D, Wood R. Early death in those previously hospitalised for mental healthcare in Scotland: a nationwide cohort study, 1986-2010. BMJ Open. 2013;3(7):e002768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Angst F, Stassen HH, Clayton PJ, Angst J. Mortality of patients with mood disorders: follow-up over 34-38 years. J Affect Disord. 2002;68(2-3):167-181. [DOI] [PubMed] [Google Scholar]
- 20.Avery D, Winokur G. Mortality in depressed patients treated with electroconvulsive therapy and antidepressants. Arch Gen Psychiatry. 1976;33(9):1029-1037. [DOI] [PubMed] [Google Scholar]
- 21.Barbato A, Terzian E, Saraceno B, De Luca L, Tognoni G. Outcome of discharged psychiatric patients after short inpatient treatment: an Italian collaborative study. Soc Psychiatry Psychiatr Epidemiol. 1992;27(4):192-197. [DOI] [PubMed] [Google Scholar]
- 22.Bergen J, Hunt G, Armitage P, Bashir M. Six-month outcome following a relapse of schizophrenia. Aust N Z J Psychiatry. 1998;32(6):815-822. [DOI] [PubMed] [Google Scholar]
- 23.Berglund M, Nilsson K. Mortality in severe depression: a prospective study including 103 suicides. Acta Psychiatr Scand. 1987;76(4):372-380. [DOI] [PubMed] [Google Scholar]
- 24.Best KM, Hauser ST, Gralinski-Bakker JH, Allen JP, Crowell J. Adolescent psychiatric hospitalization and mortality, distress levels, and educational attainment: follow-up after 11 and 20 years. Arch Pediatr Adolesc Med. 2004;158(8):749-752. [DOI] [PubMed] [Google Scholar]
- 25.Björkenstam C, Björkenstam E, Hjern A, Bodén R, Reutfors J. Suicide in first episode psychosis: a nationwide cohort study. Schizophr Res. 2014;157(1-3):1-7. [DOI] [PubMed] [Google Scholar]
- 26.Black DW, Warrack G, Winokur G. The Iowa record-linkage study, I: suicides and accidental deaths among psychiatric patients. Arch Gen Psychiatry. 1985;42(1):71-75. [DOI] [PubMed] [Google Scholar]
- 27.Blumenthal S, Bell V, Neumann N-U, Schüttler R, Vogel R. Mortality and rate of suicide of first admission psychiatric patients: a 5-year follow-up of a prospective longitudinal study. Psychopathology. 1989;22(1):50-56. [DOI] [PubMed] [Google Scholar]
- 28.Brent DA, Kolko DJ, Wartella ME, et al. Adolescent psychiatric inpatients’ risk of suicide attempt at 6-month follow-up. J Am Acad Child Adolesc Psychiatry. 1993;32(1):95-105. [DOI] [PubMed] [Google Scholar]
- 29.Brodaty H, MacCuspie-Moore CM, Tickle L, Luscombe G. Depression, diagnostic sub-type and death: a 25 year follow-up study. J Affect Disord. 1997;46(3):233-242. [DOI] [PubMed] [Google Scholar]
- 30.Burvill PW, Hall WD. Predictors of increased mortality in elderly depressed patients. Int J Geriatr Psychiatry. 1994;9(3):219-227. [Google Scholar]
- 31.Castelein S, Liemburg EJ, de Lange JS, et al. Suicide in recent onset psychosis revisited: significant reduction of suicide rate over the last two decades—a replication study of a dutch incidence cohort. PLoS One. 2015;10(6):e0129263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Charrel CL, Plancke L, Genin M, et al. Mortality of people suffering from mental illness: a study of a cohort of patients hospitalised in psychiatry in the north of France. Soc Psychiatry Psychiatr Epidemiol. 2015;50(2):269-277. [DOI] [PubMed] [Google Scholar]
- 33.Chen WJ, Huang Y-J, Yeh L-L, Rin H, Hwu H-G. Excess mortality of psychiatric inpatients in Taiwan. Psychiatry Res. 1996;62(3):239-250. [DOI] [PubMed] [Google Scholar]
- 34.Choi JW, Park S, Yi KK, Hong JP. Suicide mortality of suicide attempt patients discharged from emergency room, nonsuicidal psychiatric patients discharged from emergency room, admitted suicide attempt patients, and admitted nonsuicidal psychiatric patients. Suicide Life Threat Behav. 2012;42(3):235-243. [DOI] [PubMed] [Google Scholar]
- 35.Clark DC, Young MA, Scheftner WA, Fawcett J, Fogg L. A field test of Motto’s risk estimator for suicide. Am J Psychiatry. 1987;144(7):923-926. [DOI] [PubMed] [Google Scholar]
- 36.Coid JW, Hickey N, Yang M. Comparison of outcomes following after-care from forensic and general adult psychiatric services. Br J Psychiatry. 2007;190(6):509-514. [DOI] [PubMed] [Google Scholar]
- 37.Craig TJ, Ye Q, Bromet EJ. Mortality among first-admission patients with psychosis. Compr Psychiatry. 2006;47(4):246-251. [DOI] [PubMed] [Google Scholar]
- 38.Crisanti AS, Love EJ. Mortality among involuntarily admitted psychiatric patients: a survival analysis. Soc Psychiatry Psychiatr Epidemiol. 1999;34(12):627-633. [DOI] [PubMed] [Google Scholar]
- 39.Curtis JL, Millman EJ, Struening E, D’Ercole A. Deaths among former psychiatric inpatients in an outreach case management program. Psychiatr Serv. 1996;47(4):398-402. [DOI] [PubMed] [Google Scholar]
- 40.Davies S, Clarke M, Hollin C, Duggan C. Long-term outcomes after discharge from medium secure care: a cause for concern. Br J Psychiatry. 2007;191(1):70-74. [DOI] [PubMed] [Google Scholar]
- 41.De Leo D, Heller T. Intensive case management in suicide attempters following discharge from psychiatric care. Aust J Prim Health. 2007;13(3):49-58. [Google Scholar]
- 42.Deisenhammer EA, Behrndt EM, Kemmler G, Haring C, Miller C. A comparison of suicides in psychiatric in-patients, after discharge and in not recently hospitalized individuals. Compr Psychiatry. 2016;69:100-105. [DOI] [PubMed] [Google Scholar]
- 43.Desai RA, Dausey D, Rosenheck RA. Suicide among discharged psychiatric inpatients in the Department of Veterans Affairs. Mil Med. 2008;173(8):721-728. [DOI] [PubMed] [Google Scholar]
- 44.Donnelly M, McGilloway S, Mays N, et al. Leaving hospital: one and two-year outcomes of long-stay psychiatric patients discharged to the community. J Ment Health. 1996;5(3):245-256. [Google Scholar]
- 45.Donnelly M, McGilloway S, Mays N, Perry S, Lavery C. A 3- to 6-year follow-up of former long-stay psychiatric patients in Northern Ireland. Soc Psychiatry Psychiatr Epidemiol. 1997;32(8):451-458. [DOI] [PubMed] [Google Scholar]
- 46.Eastwood MR, Stiasny S, Meier HM, Woogh CM. Mental illness and mortality. Compr Psychiatry. 1982;23(4):377-385. [DOI] [PubMed] [Google Scholar]
- 47.Engqvist U, Rydelius PA. Death and suicide among former child and adolescent psychiatric patients. BMC Psychiatry. 2006;6:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Furlan PM, Zuffranieri M, Stanga F, Ostacoli L, Patta J, Picci RL. Four-year follow-up of long-stay patients settled in the community after closure of Italy’s psychiatric hospitals. Psychiatr Serv. 2009;60(9):1198-1202. [DOI] [PubMed] [Google Scholar]
- 49.Goldston DB, Daniel SS, Reboussin BA, Reboussin DM, Frazier PH, Harris AE. Cognitive risk factors and suicide attempts among formerly hospitalized adolescents: a prospective naturalistic study. J Am Acad Child Adolesc Psychiatry. 2001;40(1):91-99. [DOI] [PubMed] [Google Scholar]
- 50.Hansen V, Jacobsen BK, Arnesen E. Cause-specific mortality in psychiatric patients after deinstitutionalisation. Br J Psychiatry. 2001;179(5):438-443. [DOI] [PubMed] [Google Scholar]
- 51.Hayashi N, Igarashi M, Imai A, et al. Post-hospitalization course and predictive signs of suicidal behavior of suicidal patients admitted to a psychiatric hospital: a 2-year prospective follow-up study. BMC Psychiatry. 2012;12(1):186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Healy D, Harris M, Tranter R, et al. Lifetime suicide rates in treated schizophrenia: 1875-1924 and 1994-1998 cohorts compared. Br J Psychiatry. 2006;188(3):223-228. [DOI] [PubMed] [Google Scholar]
- 53.Herpertz-Dahlmann B, Müller B, Herpertz S, Heussen N, Hebebrand J, Remschmidt H. Prospective 10-year follow-up in adolescent anorexia nervosa: course, outcome, psychiatric comorbidity, and psychosocial adaptation. J Child Psychol Psychiatry. 2001;42(5):603-612. [PubMed] [Google Scholar]
- 54.Ho TP. The suicide risk of discharged psychiatric patients. J Clin Psychiatry. 2003;64(6):702-707. [DOI] [PubMed] [Google Scholar]
- 55.Hobbs C, Newton L, Tennant C, Rosen A, Tribe K. Deinstitutionalization for long-term mental illness: a 6-year evaluation. Aust N Z J Psychiatry. 2002;36(1):60-66. [DOI] [PubMed] [Google Scholar]
- 56.Hoffmann H, Modestin J. Completed suicide in discharged psychiatric inpatients. Soc Psychiatry. 1987;22(2):93-98. [DOI] [PubMed] [Google Scholar]
- 57.Høye A, Jacobsen BK, Hansen V. Increasing mortality in schizophrenia: are women at particular risk? a follow-up of 1111 patients admitted during 1980-2006 in Northern Norway. Schizophr Res. 2011;132(2-3):228-232. [DOI] [PubMed] [Google Scholar]
- 58.Høye A, Jacobsen BK, Hansen V. Sex differences in mortality of admitted patients with personality disorders in North Norway: a prospective register study. BMC Psychiatry. 2013;13:317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jamieson L, Taylor PJ. Patients leaving English high security hospitals: do discharge cohorts and their progress change over time? Int J Forensic Ment Health. 2005;4(1):71-87. [Google Scholar]
- 60.Jones RM, Hales H, Butwell M, Ferriter M, Taylor PJ. Suicide in high security hospital patients. Soc Psychiatry Psychiatr Epidemiol. 2011;46(8):723-731. [DOI] [PubMed] [Google Scholar]
- 61.Kessler RC, Warner CH, Ivany C, et al. ; Army STARRS Collaborators . Predicting suicides after psychiatric hospitalization in US Army soldiers: the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). JAMA Psychiatry. 2015;72(1):49-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kittirattanapaiboon P, Mahatnirunkul S, Booncharoen H, Thummawomg P, Dumrongchai U, Chutha W. Long-term outcomes in methamphetamine psychosis patients after first hospitalisation. Drug Alcohol Rev. 2010;29(4):456-461. [DOI] [PubMed] [Google Scholar]
- 63.Kjelsberg E, Neegaard E, Dahl AA. Suicide in adolescent psychiatric inpatients: incidence and predictive factors. Acta Psychiatr Scand. 1994;89(4):235-241. [DOI] [PubMed] [Google Scholar]
- 64.Kuo CJ, Tsai SY, Liao YT, Lee WC, Sung XW, Chen CC. Psychiatric discharge against medical advice is a risk factor for suicide but not for other causes of death. J Clin Psychiatry. 2010;71(6):808-809. [DOI] [PubMed] [Google Scholar]
- 65.Kuperman S, Black DW, Burns TL. Excess mortality among formerly hospitalized child psychiatric patients. Arch Gen Psychiatry. 1988;45(3):277-282. [DOI] [PubMed] [Google Scholar]
- 66.Lawrence DM, Holman CD, Jablensky AV, Fuller SA. Suicide rates in psychiatric in-patients: an application of record linkage to mental health research. Aust N Z J Public Health. 1999;23(5):468-470. [DOI] [PubMed] [Google Scholar]
- 67.Lee HC, Lin HC. Are psychiatrist characteristics associated with postdischarge suicide of schizophrenia patients? Schizophr Bull. 2009;35(4):760-765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lindelius R, Salum I, Ågren G. Mortality among male and female alcoholic patients treated in a psychiatric unit. Acta Psychiatr Scand. 1974;50(6):612-618. [DOI] [PubMed] [Google Scholar]
- 69.Links P, Nisenbaum R, Ambreen M, et al. Prospective study of risk factors for increased suicide ideation and behavior following recent discharge. Gen Hosp Psychiatry. 2012;34(1):88-97. [DOI] [PubMed] [Google Scholar]
- 70.Luxton DD, Trofimovich L, Clark LL. Suicide risk among US Service members after psychiatric hospitalization, 2001-2011. Psychiatr Serv. 2013;64(7):626-629. [DOI] [PubMed] [Google Scholar]
- 71.Maden A, Rutter S, McClintock T, Friendship C, Gunn J. Outcome of admission to a medium secure psychiatric unit, I: short- and long-term outcome. Br J Psychiatry. 1999;175(4):313-316. [DOI] [PubMed] [Google Scholar]
- 72.Mastroeni A, Bellotti C, Pellegrini E, Galletti F, Lai E, Falloon IR. Clinical and social outcomes five years after closing a mental hospital: a trial of cognitive behavioural interventions. Clin Pract Epidemiol Ment Health. 2005;1:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.McGlashan TH, Heinssen RK. Hospital discharge status and long-term outcome for patients with schizophrenia, schizoaffective disorder, borderline personality disorder, and unipolar affective disorder. Arch Gen Psychiatry. 1988;45(4):363-368. [DOI] [PubMed] [Google Scholar]
- 74.Meloni D, Miccinesi G, Bencini A, et al. Mortality among discharged psychiatric patients in Florence, Italy. Psychiatr Serv. 2006;57(10):1474-1481. [DOI] [PubMed] [Google Scholar]
- 75.Menezes PR, Mann AH. Mortality among patients with non-affective functional psychoses in a metropolitan area of south-eastern Brazil. Rev Saude Publica. 1996;30(4):304-309. [DOI] [PubMed] [Google Scholar]
- 76.Miller BJ, Paschall CB III, Svendsen DP. Mortality and medical comorbidity among patients with serious mental illness. Psychiatr Serv. 2006;57(10):1482-1487. [DOI] [PubMed] [Google Scholar]
- 77.Möller H-J, von Zerssen D, Werner-Eilert K, Wüschner-Stockheim M. Outcome in schizophrenic and similar paranoid psychoses. Schizophr Bull. 1982;8(1):99-108. [DOI] [PubMed] [Google Scholar]
- 78.Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv. 2001;52(6):828-833. [DOI] [PubMed] [Google Scholar]
- 79.Naik PC, Davies S, Buckley AM, Lee AS. Long-term mortality after first psychiatric admission. Br J Psychiatry. 1997;170(1):43-46. [DOI] [PubMed] [Google Scholar]
- 80.Ng R, Leung S. A 5-year outcome study of chronically ill psychiatric patients in Hong Kong. Hong Kong J Psychiatry. 2000;10(3):27-36. [Google Scholar]
- 81.Opjordsmoen S, Friis S, Melle I, et al. A 2-year follow-up of involuntary admission’s influence upon adherence and outcome in first-episode psychosis. Acta Psychiatr Scand. 2010;121(5):371-376. [DOI] [PubMed] [Google Scholar]
- 82.Ösby U, Brandt L, Correia N, Ekbom A, Sparén P. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry. 2001;58(9):844-850. [DOI] [PubMed] [Google Scholar]
- 83.Owen C, Rutherford V, Jones M, Tennant C, Smallman A. Psychiatric rehospitalization following hospital discharge. Community Ment Health J. 1997;33(1):13-24. [DOI] [PubMed] [Google Scholar]
- 84.Park S, Choi JW, Kyoung Yi K, Hong JP. Suicide mortality and risk factors in the 12 months after discharge from psychiatric inpatient care in Korea: 1989-2006. Psychiatry Res. 2013;208(2):145-150. [DOI] [PubMed] [Google Scholar]
- 85.Park S, Kim CY, Hong JP. Unnatural causes of death and suicide among former adolescent psychiatric patients. J Adolesc Health. 2013;52(2):207-211. [DOI] [PubMed] [Google Scholar]
- 86.Park S, Kim JW, Kim BN, et al. Clinical characteristics and precipitating factors of adolescent suicide attempters admitted for psychiatric inpatient care in South Korea. Psychiatry Investig. 2015;12(1):29-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Park S, Kim SY, Hong JP. Cause-specific mortality of psychiatric inpatients and outpatients in a general hospital in Korea. Asia Pac J Public Health. 2015;27(2):164-175. [DOI] [PubMed] [Google Scholar]
- 88.Pedersen CG, Jensen SOW, Gradus J, Johnsen SP, Mainz J. Systematic suicide risk assessment for patients with schizophrenia: a national population-based study. Psychiatr Serv. 2014;65(2):226-231. [DOI] [PubMed] [Google Scholar]
- 89.Peuskens J, De Hert M, Cosyns P, Pieters G, Theys P, Vermote R. Suicide in young schizophrenic patients during and after inpatient treatment. Int J Ment Health. 1996;25(4):39-44. [Google Scholar]
- 90.Pokorny AD. Prediction of suicide in psychiatric patients. Report of a prospective study. Arch Gen Psychiatry. 1983;40(3):249-257. [DOI] [PubMed] [Google Scholar]
- 91.Politi P, Piccinelli M, Klersy C, et al. Mortality in psychiatric patients 5 to 21 years after hospital admission in Italy. Psychol Med. 2002;32(2):227-237. [DOI] [PubMed] [Google Scholar]
- 92.Qurashi I, Kapur N, Appleby L. A prospective study of noncompliance with medication, suicidal ideation, and suicidal behavior in recently discharged psychiatric inpatients. Arch Suicide Res. 2006;10(1):61-67. [DOI] [PubMed] [Google Scholar]
- 93.Remberk B, Bażyńska AK, Krempa-Kowalewska A, Rybakowski F. Adolescent insanity revisited: course and outcome in early-onset schizophrenia spectrum psychoses in an 8-year follow-up study. Compr Psychiatry. 2014;55(5):1174-1181. [DOI] [PubMed] [Google Scholar]
- 94.Robling SA, Paykel ES, Dunn VJ, Abbott R, Katona C. Long-term outcome of severe puerperal psychiatric illness: a 23 year follow-up study. Psychol Med. 2000;30(6):1263-1271. [DOI] [PubMed] [Google Scholar]
- 95.Ruengorn C, Sanichwankul K, Niwatananun W, Mahatnirunkul S, Pumpaisalchai W, Patumanond J. Incidence and risk factors of suicide reattempts within 1 year after psychiatric hospital discharge in mood disorder patients. Clin Epidemiol. 2011;3:305-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Rydelius PA. Deaths among child and adolescent psychiatric patients. Acta Psychiatr Scand. 1984;70(2):119-126. [DOI] [PubMed] [Google Scholar]
- 97.Sani G, Tondo L, Koukopoulos A, et al. Suicide in a large population of former psychiatric inpatients. Psychiatry Clin Neurosci. 2011;65(3):286-295. [DOI] [PubMed] [Google Scholar]
- 98.Schneider B, Philipp M, Müller MJ. Psychopathological predictors of suicide in patients with major depression during a 5-year follow-up. Eur Psychiatry. 2001;16(5):283-288. [DOI] [PubMed] [Google Scholar]
- 99.Seemüller F, Meier S, Obermeier M, et al. Three-year long-term outcome of 458 naturalistically treated inpatients with major depressive episode: severe relapse rates and risk factors. Eur Arch Psychiatry Clin Neurosci. 2014;264(7):567-575. [DOI] [PubMed] [Google Scholar]
- 100.Simpson AI, Jones RM, Evans C, McKenna B. Outcome of patients rehabilitated through a New Zealand forensic psychiatry service: a 7.5 year retrospective study. Behav Sci Law. 2006;24(6):833-843. [DOI] [PubMed] [Google Scholar]
- 101.Skeem JL, Silver E, Aippelbaum PS, Tiemann J. Suicide-related behavior after psychiatric hospital discharge: Implications for risk assessment and management. Behav Sci Law. 2006;24(6):731-746. [DOI] [PubMed] [Google Scholar]
- 102.Tabita B, de Santi MG, Kjellin L. Criminal recidivism and mortality among patients discharged from a forensic medium secure hospital. Nord J Psychiatry. 2012;66(4):283-289. [DOI] [PubMed] [Google Scholar]
- 103.Tejedor MC, Díaz A, Castillón JJ, Pericay JM. Attempted suicide: repetition and survival: findings of a follow-up study. Acta Psychiatr Scand. 1999;100(3):205-211. [DOI] [PubMed] [Google Scholar]
- 104.Thomsen PH. A 22- to 25-year follow-up study of former child psychiatric patients: a register-based investigation of the course of psychiatric disorder and mortality in 546 Danish child psychiatric patients. Acta Psychiatr Scand. 1996;94(6):397-403. [DOI] [PubMed] [Google Scholar]
- 105.Thornicroft G, Sartorius N. The course and outcome of depression in different cultures: 10-year follow-up of the WHO Collaborative Study on the Assessment of Depressive Disorders. Psychol Med. 1993;23(4):1023-1032. [DOI] [PubMed] [Google Scholar]
- 106.Thornicroft G, Bebbington P, Leff J. Outcomes for long-term patients one year after discharge from a psychiatric hospital. Psychiatr Serv. 2005;56(11):1416-1422. [DOI] [PubMed] [Google Scholar]
- 107.Trieman N, Leff J, Glover G. Outcome of long stay psychiatric patients resettled in the community: prospective cohort study. BMJ. 1999;319(7201):13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tseng MC, Cheng IC, Lee YJ, Lee MB. Intermediate-term outcome of psychiatric inpatients with major depression. J Formos Med Assoc. 2006;105(8):645-652. [DOI] [PubMed] [Google Scholar]
- 109.Welner A, Welner Z, Fishman R. Psychiatric adolescent inpatients: eight- to ten-year follow-up. Arch Gen Psychiatry. 1979;36(6):698-700. [DOI] [PubMed] [Google Scholar]
- 110.Wiersma D, Nienhuis FJ, Slooff CJ, Giel R. Natural course of schizophrenic disorders: a 15-year followup of a Dutch incidence cohort. Schizophr Bull. 1998;24(1):75-85. [DOI] [PubMed] [Google Scholar]
- 111.Winkler P, Mladá K, Csémy L, Nechanská B, Höschl C. Suicides following inpatient psychiatric hospitalization: A nationwide case control study. J Affect Disord. 2015;184:164-169. [DOI] [PubMed] [Google Scholar]
- 112.Zilber N, Schufman N, Lerner Y. Mortality among psychiatric patients: the groups at risk. Acta Psychiatr Scand. 1989;79(3):248-256. [DOI] [PubMed] [Google Scholar]
- 113.Zubenko GS, Mulsant BH, Sweet RA, Pasternak RE, Tu XM. Mortality of elderly patients with psychiatric disorders. Am J Psychiatry. 1997;154(10):1360-1368. [DOI] [PubMed] [Google Scholar]
- 114.Walsh G, Sara G, Ryan CJ, Large M. Meta-analysis of suicide rates among psychiatric in-patients. Acta Psychiatr Scand. 2015;131(3):174-184. [DOI] [PubMed] [Google Scholar]
- 115.Nordentoft M, Erlangsen A, Madsen T. Postdischarge suicides: nightmare and disgrace. JAMA Psychiatry. 2016;73(11):1113-1114. [DOI] [PubMed] [Google Scholar]
- 116.Olfson M, Marcus SC, Bridge JA. Focusing suicide prevention on periods of high risk. JAMA. 2014;311(11):1107-1108. [DOI] [PubMed] [Google Scholar]
- 117.Qin P, Nordentoft M. Suicide risk in relation to psychiatric hospitalization: evidence based on longitudinal registers. Arch Gen Psychiatry. 2005;62(4):427-432. [DOI] [PubMed] [Google Scholar]
- 118.Meehan J, Kapur N, Hunt IM, et al. Suicide in mental health in-patients and within 3 months of discharge: national clinical survey. Br J Psychiatry. 2006;188:129-134. [DOI] [PubMed] [Google Scholar]
- 119.Berman AL, Silverman MM. Suicide risk assessment and risk formulation part II: suicide risk formulation and the determination of levels of risk. Suicide Life Threat Behav. 2014;44(4):432-443. [DOI] [PubMed] [Google Scholar]
- 120.Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. 2016;387(10024):1227-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ryan CJ, Large MM. Suicide risk assessment: where are we now? Med J Aust. 2013;198(9):462-463. [DOI] [PubMed] [Google Scholar]
- 122.Large M, Kaneson M, Myles N, Myles H, Gunaratne P, Ryan C. Meta-analysis of longitudinal cohort studies of suicide risk assessment among psychiatric patients: heterogeneity in results and lack of improvement over time. PLoS One. 2016;11(6):e0156322. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Included Studies
eTable 2. Excluded Studies
eTable 3. Sample-Level Data, Strength of Reporting, and Study Characteristics