Key Points
Question
Does an intervention that improves staff connections, information flow, and use of cognitive diversity in clinical problem solving boost uptake of an evidence-based fall prevention program?
Findings
This cluster-randomized trial found that although communication measures improved modestly among nursing home staff randomized to receive the intervention compared with staff in control facilities, no significant change was observed in documented fall risk reduction activities or recurrent fall rates in either group.
Meaning
Improving communication among nursing home staff did not facilitate uptake of complex interventions such as fall prevention programs. New approaches are needed to improve implementation of evidence-based care for geriatric syndromes.
This cluster-randomized trial tests whether a complexity science–based staff training intervention promoting high-quality staff interactions improves the impact of an evidence-based falls quality improvement program.
Abstract
Importance
New approaches are needed to enhance implementation of complex interventions for geriatric syndromes such as falls.
Objective
To test whether a complexity science–based staff training intervention (CONNECT) promoting high-quality staff interactions improves the impact of an evidence-based falls quality improvement program (FALLS).
Design, Setting, and Participants
Cluster-randomized trial in 24 nursing homes receiving either CONNECT followed by FALLS (intervention), or FALLS alone (control). Nursing home staff in all positions were asked to complete surveys at baseline, 3, 6, and 9 months. Medical records of residents with at least 1 fall in the 6-month pre- and postintervention windows (n = 1794) were abstracted for fall risk reduction measures, falls, and injurious falls.
Interventions
CONNECT taught staff to improve their connections with coworkers, increase information flow, and use cognitive diversity in problem solving. Intervention components included 2 classroom sessions, relationship mapping, and self-monitoring. FALLS provided instruction in the Agency for Healthcare Research and Quality’s Falls Management Program.
Main Outcomes and Measures
Primary outcomes were (1) mean number of fall risk reduction activities documented within 30 days of falls and (2) median fall rates among residents with at least 1 fall during the study period. In addition, validated scales measured staff communication quality, frequency, timeliness, and safety climate.
Results
Surveys were completed by 1545 staff members, representing 734 (37%) and 811 (44%) of eligible staff in intervention and control facilities, respectively; 511 (33%) respondents were hands-on care workers. Neither the CONNECT nor the FALLS-only facilities improved the mean count of fall risk reduction activities following FALLS (3.3 [1.6] vs 3.2 [1.5] of 10); furthermore, adjusted median recurrent fall rates did not differ between the groups (4.06 [interquartile range {IQR}, 2.03-8.11] vs 4.06 [IQR, 2.04-8.11] falls/resident/y). A modest improvement in staff communication measures was observed overall (mean, 0.03 [SE, 0.01] points on a 5-point scale; P = .03) and for communication timeliness (mean, 0.8 [SE, 0.03] points on a 5-point scale; P = .02). There was wide variation across facilities in intervention penetration.
Conclusions and Relevance
An intervention targeting gaps in staff communication and coordination did not improve the impact of a falls quality improvement program. New approaches to implementing evidence-based care for complex conditions in the nursing home are urgently needed.
Trial Registration
clinicaltrials.gov Identifier: NCT00636675
Introduction
Many common medical problems lack straightforward solutions that can be managed by a single individual and necessitate coordination among multiple people over time. This is especially true of geriatric syndromes that have multiple underlying causes and necessitate multifactorial interventions. Implementation of evidence-based interventions for geriatric syndromes in nursing homes has been particularly difficult. For example, fall prevention interventions that used external study staff to complete risk reduction activities for nursing home residents demonstrated substantial reductions in fall rates, whereas those that trained existing staff have not.
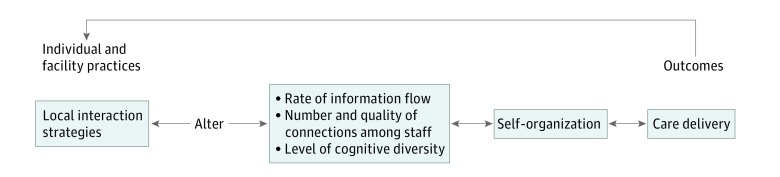
Complexity science may explain why care for patients with complex clinical problems often fails. Studies of high-reliability organizations demonstrate that the number and quality of connections among staff, the degree that information flows through the organization, and the level of cognitive diversity (different perspectives) used in decision making are critical determinants of how effectively staff are able to “self-organize” (Figure 1). Self-organization occurs during local interactions in the workplace, and it describes how staff mutually adjust their behaviors to provide care. Our previous work has found limited connections between staff in different roles, inconsistent information flow, and rare use of cognitive diversity. Common management approaches further limit interactions between staff by enforcing a chain of command for communication and creating an environment in which staff fear punishment if they report a clinical concern. As a result, important resident observations made by frontline staff are not shared with those who are trained to interpret and act on them, and care decisions from the interprofessional team are not communicated to and used by those delivering care. These issues are associated with worse resident outcomes; for example, nursing homes that report lower levels of frontline staff participation in decision making have higher rates of resident behavior problems, restraint use, and fractures. Unless communication barriers are addressed, implementation of multifactorial interventions is unlikely to succeed.
Figure 1. Complexity Science Conceptual Model of the Impact of Staff Interaction Quality on Resident Outcomes.
We designed an organization-level intervention, CONNECT, in which staff learned strategies to increase connections, information flow, and cognitive diversity in managing complex clinical problems. We hypothesized that CONNECT would enhance the impact of a fall prevention quality improvement program. A pilot study in 8 nursing homes showed improvement in measures of staff communication and lower fall rates (rate ratio, 0.81; 95% CI, 0.55-1.20). In this analysis, we report the results of a randomized trial of CONNECT in 16 additional nursing homes. Primary outcomes were fall risk reduction measures implemented in high-risk residents, and recurrent fall rates.
Methods
Design, Setting, and Randomization
This study was a cluster-randomized trial of 24 nursing homes with blinded outcomes assessment. Interventions took place over 6 months between 2012 and 2015, and resident falls were collected for the 6 months prior to and 6 months following the interventions. All 69 nursing homes with at least 90 beds participating in Medicare within 100 miles of Duke University were invited to participate, and the first 24 to respond were included. Nursing homes affiliated with hospitals and inpatient rehabilitation facilities were excluded. An investigator (K.C.) masked to nursing home name randomized within pairs matched on chain affiliation using a random number generator. All procedures were approved by the Duke University Institutional Review Board. The study protocol is available in Supplement 1.
Participants
Staff were invited to participate in intervention components as part of their facility’s quality improvement initiatives, but provided individual informed consent for data collection. All full-time staff able to understand English were eligible, regardless of role. Thus, our sample included staff who worked directly with residents (eg, registered nurses [RNs], licensed practical nurses [LPNs], nurse aides, social workers, dietary aides, activities staff, and physical and occupational therapists), administrative staff (eg, department directors), and other support staff (eg, environmental services, maintenance).
A waiver of informed consent for resident participation was obtained. Using a random number generator, random samples of 50 unique residents from each facility were selected for medical record abstraction in the 6 months before and 6 months following the intervention. Residents were included if they were 65 years or older, experienced at least 1 fall in either data collection window, and remained in the facility for at least 30 days after the fall. This sampling strategy allowed us to measure fall risk factor reduction activities completed for the highest-risk residents.
Interventions and Fidelity
The interventions were delivered by separate teams of trained interventionists over 3 months each, using standardized protocols and training tools. Intervention fidelity was assessed through investigator checklist audits of a random sample of interventionist observations and through qualitative review of staff interviews during structured mentoring.
A description of the CONNECT and fall prevention quality improvement program (FALLS) interventions is summarized in Table 1. CONNECT consisted of 3 main components. In the first month, staff attended 2 learning sessions about local interaction strategies found to increase connection, information flow, and cognitive diversity among nursing home staff. Sessions used adult learning strategies such as storytelling and role play to practice sharing information within and across disciplines; for example, in 1 scenario a nurse aide and LPN brought observations about fall risk to a medical clinician. In the second month, staff engaged in relationship-mapping sessions. Department leaders developed “group-to-group maps” depicting actual and desired interaction patterns between departments, ending with agreement on goals for improving cross-department communication. Each individual staff member drew a personal relationship map defining his or her ideal interactions with selected coworkers across disciplines. Participants received structured mentoring and feedback during 10-minute semistructured discussions of their experiences applying CONNECT concepts. In the third month, individuals used a standardized instrument to record interactions with coworkers, which were used to provide written feedback.
Table 1. CONNECT and FALLS Protocol Activities, Rationale, Who Is Involved, and Time Required.
| Activity | Rationale/Outcome | Who | Time |
|---|---|---|---|
| CONNECT Protocols | |||
| In-Class Protocols | |||
| CONNECT and Learn Protocols CONNECT Beginner. Introduces local interaction strategies using storytelling; practice strategies to improve connection and information exchange using role play. CONNECT Advanced. Brief review followed by focus on cognitive diversity, using storytelling and role play |
Introduce concepts; practice using local interaction strategies in interdisciplinary group setting. Outreach education | All staff | 30 min each |
| Relationship Map Protocols | |||
| (1) Group-to-group maps Session 1. Staff describe actual interactions between work groups. Session 2. Staff draw desired interaction map and develop goals for improved group-to-group interaction patterns |
Make facility interaction patterns explicit, and agree on guidelines for improved interactions. External facilitation | Mid-level managers, selected LPNs, nurse aides | 1 h each |
| (2) Individual-to-individual maps Staff draw an individual relationship map that defines his or her ideal interactions with selected coworkers (provided on laminated card). Participants record interactions with those individuals over 4 weeks |
Evaluate relationships, develop new connections, practice effective interaction strategies. External facilitation | All CONNECT participants | 30 min |
| Unit-Based Mentoring Protocols | |||
| Structured mentoring Researcher engages each participant twice in brief sessions to reflect on his or her experiences applying CONNECT concepts. Strategies for managing communication problems with specific individuals are developed |
Facilitates authentic learning, which occurs only when learners can directly apply concepts. External facilitation | All CONNECT participants | 20 min |
| FALLS Protocols | |||
| FALLS Coordinator and Team Role | |||
| Training Session Researcher reviews (1) role of falls team members, (2) Falls Management Program rationale and main components, (3) toolkit materials, (4) study expectations |
Falls team members identify area to improve, set goals, collect data to monitor changes. Develop clinical champions | Falls team | 4 h |
| Weekly FALLS team teleconference Weekly teleconference over 3 mo highlighting a topic from the Fall Management Program in depth. Topics: (1) staff fall prevention education, (2) medications and falls, (3) patient and family education, (4) orthostatic hypotension, (5) vision assessment and intervention, (6) gait and balance assessment and intervention, (7) environmental assessment and intervention, (8) challenging behaviors, (9) establishing a culture of safety, (10) audit and feedback, and (11) wrap-up and resetting goals |
Reinforces key concepts of multifactorial risk reduction, supports falls team and maintains enthusiasm. Outreach education | Falls team, others at their invitation | 30 min each |
| Staff Education | |||
| Case-based modules 3 self-study modules tailored for nurses, nurse aides, or medical clinicians and pharmacists. Reviews multiple risk factor reduction strategies. Available online or in paper form; continuing education credits awarded |
Uses case-based learning to enhance multifactorial fall risk reduction. Outreach education | Individual staff | 30-60 min |
| Postfall Problem Solving | |||
| Academic detailing Falls coordinator and study falls expert lead 2 discussions with frontline staff regarding their most challenging residents with falls, modeling risk factor assessment and multifactorial interventions. Sessions occur at each nursing station during day and evening shifts |
Reinforces key concepts and promotes behavior change and interdisciplinary discussions | Nurses, nurse aides, others as interested | 20 min each |
| Audit and Feedback | |||
| Feedback report Report using visual and written depictions of the facility’s baseline fall risk reduction activities compared with peer facilities |
Identifies areas for improvement, promotes behavior change. External facilitation | Falls team, others at their invitation | 30 min |
| Toolbox | |||
| Morse Fall Scale, Nurse Fall Risk Reduction Worksheet, Prescriber/Pharmacist Medication Reduction Worksheet, Environmental Checklist, wheelchair maintenance log and stickers, fall fax communication form, patient and family brochure, physician/prescriber brochure | Provides modifiable tools to assist with communication and documentation of fall risk reduction | Falls team | Not applicable |
FALLS introduced the Agency for Healthcare Research and Quality (AHRQ)’s Falls Management Program for nursing homes. FALLS was delivered by interventionists not involved in CONNECT, and occurred immediately following CONNECT or the control period. In addition to the standard AHRQ program, we offered additional components as described in Table 1.
Measures
Timing of Measurement
Resident outcomes were assessed for the 180 days immediately preceding and immediately following the 6-month intervention period. Staff measures were collected during a 2-week period immediately before the CONNECT/control period (baseline), at the end of the CONNECT/control period (3 months), at the end of FALLS (6 months), and 3 months after all interventions were completed (9 months) (eFigure in Supplement 2).
Resident Outcomes
A count of fall risk reduction activities documented within 30 days of a fall was the primary end point. Fall risk reduction activities included the following: orthostatic blood pressure measurement and/or intervention, sensory impairment evaluation and/or intervention, change in footwear, exercise and/or assistive device intervention, toileting schedule implementation, environmental modification, psychoactive medication reduction, and vitamin D supplementation. Medical records were abstracted by trained nurses blinded to intervention status employed by the state Quality Improvement Organization. A random sample of 10% of records were abstracted by a second Quality Improvement Organization nurse and at least 90% agreement maintained. Fall risk reduction activities occurring after a fall, rather than proactive measures, were selected because such activities are less reliably documented in the absence of a trigger event such as a fall.
Median recurrent fall rates (falls per resident per year) among residents with at least 1 fall was a primary end point. To improve power, we calculated fall rates at an individual resident level rather than a facility level; we measured fall rates for residents with at least 1 fall during the 6-month study period (included in the aforementioned fall risk reduction activity measure), starting their observation period at the time of their first fall. Resident follow-up days were calculated censoring for hospital stays, discharge, and death. Rates of injurious falls, defined as those resulting in an emergency department visit, need for imaging, bruise, skin tear, or requirement for 72 hours or more of increased analgesia, were a secondary measure.
Staff Measures
Surveys included previously validated scales: communication openness, accuracy, and timeliness; the Participation in Decision-Making Instrument; the Safety Organizing Scale; and the Local Interaction Scale and Perceived Quality of Care Scale.
Covariates
Factors potentially affecting intervention delivery and outcomes were collected at the resident, staff, and facility levels as presented in Table 1.
Analysis
We used an intention-to-treat analysis, but in prespecified sensitivity analyses we deleted 3 facilities (2 intervention, 1 control) with staff turnover rates of 35% or greater, representing the highest 5%. Study power was estimated using algorithms for longitudinal models based on the formulae of Jung and Ahn, a type I error rate of .05 (2-tailed), and a 15% rate of attrition. We estimated that sample sizes of more than 1401 staff members and nearly 1800 residents, both clustered within 24 facilities, would provide 80% power to detect a 15% difference in fall risk reduction activities and 80% power to detect a 23% difference in the fall rate.
To estimate the impact of CONNECT on resident outcomes, we used 2-level generalized linear mixed models accounting for clustering of residents within facilities and for different shapes of the distributions. The intervention variable was modeled at the facility level. Because the baseline and follow-up periods included different residents, “time” was not modeled as another level but was controlled dichotomously. Postintervention fall rates were examined in separate generalized linear mixed models, controlling for baseline fall rates, baseline fall risk reduction score, and resident-, staff-, and facility-level variables. The Cohen d was used to estimate effect sizes.
For staff outcomes, we used 3-level linear mixed models. Time was modeled at the first level, staff was modeled at the second level, and facilities were modeled at the third level, which included the intervention variable. Staff outcomes were computed from available scale items unless more than 50% were missing, in which case the scale score was designated as missing. All missing data were imputed with maximum-likelihood and multiple-imputation techniques. We used plots and interaction terms to examine differences in the impact of CONNECT across staff roles. Intervention “dose” was modeled within intervention facilities as a continuous variable indicating the number of CONNECT intervention components that each staff member had completed (0-10).
Results
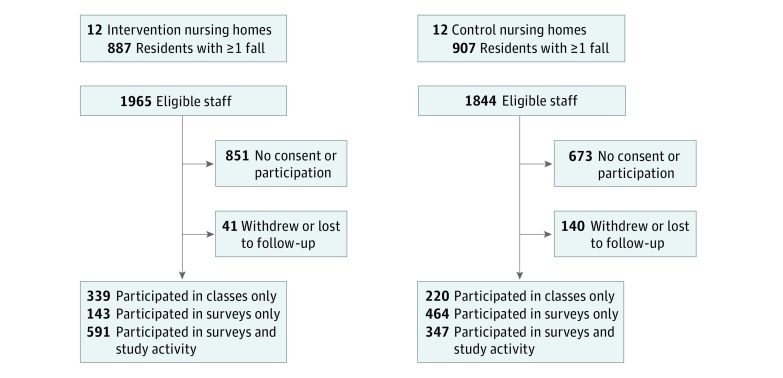
Characteristics of facilities, staff, and residents are described in Table 2. All facilities were for-profit, with a mixture of settings, payer mix, and quality ratings. Turnover among consented staff ranged from 0 to 46.4%. Residents were predominantly female (957 [53.5%]), white (1298 [72.3%]), and receiving long-term care (1022 [58.2%]); mean (SD) age was 81.9 (9.4) years. Staff represented the full range of job types, with a mean (SD) of 6.0 (6.2) years employment in the nursing home; notable differences between intervention and control facilities occurred in participation of RN staff (59 [9.0%] vs 51 [6.9%]), medical staff (10 [1.5%] vs 17 [2.3%]), and therapy staff (18 [2.7%] vs 24 [3.2%]). Staff participation is described in Figure 2; 930 (47.3%) of eligible staff completed at least 1 CONNECT activity and 567 (30.8%) completed at least 1 FALLS activity.
Table 2. Characteristics of Study Nursing Homes, Staff, and Residentsa.
| Nursing Home Characteristics | Intervention (n = 12) |
Control (n = 12) |
|---|---|---|
| Bed size, mean (SD) | 125 (20) | 121 (29) |
| Nonchain, No. (%) | 2 (17) | 4 (33) |
| Urban location, No. (%) | 7 (58) | 8 (67) |
| Staff turnover during study, mean (SD), % | 22 (14) | 25 (16) |
| Staff Characteristics at Baseline | (n = 658) | (n = 743) |
| Age, No. (%), y | ||
| 18-35 | 195 (29.6) | 233 (31.4) |
| 36-55 | 325 (49.4) | 394 (53.0) |
| >56 | 138 (21.0) | 116 (15.6) |
| Female sex, No. (%) | 586 (89.1) | 637 (85.7) |
| Race, No. (%) | ||
| Black or African American | 291 (44.2) | 344 (46.3) |
| White | 305 (46.4) | 321 (43.2) |
| Others | 47 (7.1) | 41 (5.5) |
| Unknown | 15 (2.3) | 37 (5.0) |
| College or associate degree, No. (%) | 265 (40.2) | 277 (37.3) |
| Role, No. (%) | ||
| Hands-on care (certified nursing assistant, physical therapist assistant, etc) | 243 (36.9) | 268 (36.1) |
| LPN | 66 (10.0) | 94 (12.7) |
| RN | 59 (9.0) | 51 (6.9) |
| Business office/administrative | 31 (4.7) | 36 (4.8) |
| Dietary | 55 (8.4) | 60 (8.1) |
| Environmental services | 45 (6.8) | 53 (7.1) |
| Therapy | 18 (2.7) | 24 (3.2) |
| Activities | 7 (1.1) | 11 (1.5) |
| Medical staff | 10 (1.5) | 17 (2.3) |
| Social work | 98 (14.9) | 104 (14.0) |
| Unknown | 26 (4.0) | 25 (3.4) |
| Employment in facility, mean (SD), y | 6.0 (6.3) | 6.0 (6.2) |
| Resident Characteristics at Time of First Fall | (n = 887) | (n = 907) |
| Age, mean (SD), y | 80.9 (9.6) | 80.7 (9.1) |
| Female sex, No. (%) | 476 (53.7) | 481 (53.0) |
| Race, No. (%) | ||
| White | 634 (71.4) | 664 (73.2) |
| Black | 233 (26.2) | 216 (23.8) |
| Other | 20 (2.3) | 27 (3.0) |
| Falls prior to index, No. (%) | 409 (46.1) | 457 (50.4) |
| Cognitive impairment, No. (%) | 571 (64.4) | 583 (64.3) |
| Parkinsonism, No. (%) | 82 (9.2) | 70 (7.7) |
| Neuropathy, No. (%) | 98 (11.0) | 125 (13.8) |
| Vision impairment, No. (%) | 290 (32.7) | 211 (23.3) |
| Ambulatory status, No. (%) | ||
| Independent | 650 (73.3) | 674 (74.3) |
| Dependent | 237 (26.7) | 233 (25.7) |
| Stroke, No. (%) | 215 (32.7) | 308 (34.0) |
Demographic characteristics were missing for 144 staff members who completed surveys.
Figure 2. Enrollment and Participation in Study Activities.
CONNECT offered activities to all staff in the facility whereas FALLS activities were targeted primarily to the fall team and nursing staff. Therefore, more staff in the control facilities participated in surveys only.
Surveys were completed by 1545 unique staff members, 734 (37%) and 811 (44%) of eligible staff in intervention and control facilities, respectively. Mean communication scores in intervention facilities at baseline were lower than controls in 5 of 6 scales (statistically significant difference for 3 scales). Table 3 shows the change in communication scores at 6 months attributable to CONNECT, after accounting for staff-, facility-, and patient-level covariates. CONNECT was associated with small increases in all communication measures, but the findings were significant only for communication timeliness (with an adjusted mean increase of 0.08 [SE, 0.03] points on a 5-point Likert scale; P = .02). A factor analysis confirmed that responses loaded on a single factor; thus, we performed linear mixed modeling on the weighted average on a 1-to-5 Likert scale. This showed a 0.03 (SE, 0.01)-point improvement attributable to the intervention at 6 months (P = .03), although statistical significance was lost when nesting within facilities was modeled. Interaction plots suggested that LPNs, environmental services workers, and dietary workers had greater improvements with CONNECT than other groups of workers. A higher “dose” of CONNECT (ie, number of intervention components received) was associated with small incremental increases in communication variables that were not statistically significant. Staff-level variables, especially job position, had far more impact on scores than did facility, intervention, or time. For example, nurse aides across facilities rated communication quality variables a mean of 0.14 to 0.40 points lower than RNs in 5 of 6 scales (P < .001).
Table 3. Impact of CONNECT on Measures of Staff Communication and Interaction, and Fall Ratesa.
| Outcome Measure | Adjusted Score, Mean (SE) | P Value | ||
|---|---|---|---|---|
| Staff Communication Scale (Range) | Control Baseline | Intervention Baseline | 6-mo Change Attributable to Intervention | |
| Communication openness (0-5) | 4.11 (0.11) | 3.95 (0.08) | 0.04 (0.03) | .12 |
| Communication accuracy (0-5) | 2.95 (0.07) | 2.80 (0.05) | 0.04 (0.03) | .33 |
| Communication timeliness (0-5) | 3.96 (0.09) | 3.82 (0.08) | 0.08 (0.03) | .02 |
| Nurse aide participation in decision making (0-7) | 5.66 (0.24) | 5.47 (0.15) | 0.05 (0.08) | .52 |
| Local interaction strategies (0-5) | 4.01 (0.09) | 3.88 (0.06) | 0.03 (0.02) | .26 |
| Safety climate (0-7) | 5.08 (0.22) | 4.91 (0.14) | 0.00 (0.05) | .97 |
| Staff perceptions of quality (0-7) | 5.25 (0.56) | 5.18 (0.04) | 0.03 (0.02) | .30 |
| Weighted average response (1-5) | 3.56 (0.08) | 3.42 (0.06) | 0.03 (0.02) | .10 |
| Resident Fall Rates, Falls/Resident/y | ||||
| Recurrent fall rate | ||||
| Median (IQR) | 4.06 (2.04-8.11) | 4.06 (2.03-8.11) | 0 | .96 |
| Mean (SD) | 7.11 (11.14) | 6.70 (8.42) | ||
| Injurious fall rate | ||||
| Median (IQR) | 0 (0-2.12) | 0 (0-2.21) | 0 | .39 |
| Mean (SD) | 2.07 (4.56) | 2.25 (5.45) | ||
Abbreviation: IQR, interquartile range.
Staff measures are adjusted for facility-level (bed size, turnover rate), staff-level (age, race, position, years at facility, licensure), and resident-level (mean number of comorbidities) covariates. Resident measures are additionally adjusted for preintervention fall rates and resident fall risk factors.
Among residents with at least 1 fall during the observation period, median subsequent fall rates were not different between intervention and control facilities (4.06 [interquartile range {IQR}, 2.03-8.11] vs 4.06 [IQR, 2.04-8.11] falls/resident/y). Median injurious fall rates were 0 in both groups (IQR, 0-2.21 falls/resident/y in the intervention group vs 0-2.12 falls/resident/y in the control group), with a mean (SD) of 2.25 (5.45) falls/resident/y in the intervention group vs 2.07 (4.56) falls/resident/y in the control group (Table 3). Fall rates did not improve after the FALLS intervention in either group.
Medical records in intervention and control facilities documented a mean (SD) of 3.3 (1.6) and 3.2 (1.5) fall risk reduction activities, respectively (of a possible 10) within 30 days of a fall. The most commonly documented activities were vision assessment (1381 [77%]), exercise and/or assistive device intervention (1345 [75%]), and footwear change (915 [51%]). The number of fall risk reduction activities did not change following FALLS in either group. Adjusting for staff turnover and eliminating the 3 facilities with turnover exceeding 35% did not change the results for either the staff or resident outcomes.
Discussion
Complex, multifactorial interventions are the benchmark for preventing adverse outcomes including delirium, urinary incontinence, and falls in older people, but translation of clinical trials into clinical practice has been elusive. Our work and that of others suggests that a lack of staff collaboration is associated with poor resident outcomes. In this context, we conducted what we believe to be the first randomized trial of an intervention explicitly designed to improve collaboration among staff by focusing on enhanced connections, information flow, and cognitive diversity. Despite inclusion of 47% of eligible staff, we observed only a small impact on measures of communication and no impact on fall risk reduction activities or recurrent fall rates.
There are several potential explanations for our findings. First, we had lower power than anticipated for the communication measures because responses were more strongly influenced by job role than facility, reducing the potential to detect differences in facility-level communication resulting from the intervention. Power issues also arose with higher-than-expected variability in fall rates; however, the small magnitude of the observed changes suggests that insufficient power alone does not explain the findings. Second, CONNECT did not appear to be clinically potent. Intervention penetration varied across facilities (mean number of intervention components received by staff ranged 2.3-4.2 out of 10 possible), with challenges including varying levels of administrative support, high turnover, and competing clinical responsibilities. We used a number of strategies to mitigate these expected issues, including requiring administrators to attend the first CONNECT session, development of a modified classroom session that could be provided to small groups of staff at the nursing station, use of participant incentives, and training new staff during the intervention period. Third, the indicator condition and population that we chose might have been problematic. Whereas falls are highly prevalent with a good evidence base supporting risk reduction activities, our design targeting residents with at least 1 fall resulted in the inclusion of a high number of residents who fell frequently and whose falls may be the most difficult to prevent. We tested differences in median fall rates, which are less sensitive to outliers, and sensitivity analyses excluding residents with 10 or more falls in the study period did not change findings. Finally, fall risk reduction activities may not be recorded reliably in the medical record. We developed a fall prevention clinical vignette measure completed by staff before and after the intervention as an alternative process measure for this study, but results were not different between the study groups.
Our study has several implications for researchers. First, additional studies are needed to determine optimal ways of improving connection, information flow, and cognitive diversity within health care organizations.(pp140-146) Whereas complexity science supported our approach to deliver the intervention broadly across the organization, recent work by Norton and colleagues also supports targeting workgroups with focused interactions around small groups of residents; their recent study indicated that Minimum Data Set quality indicators such as pressure ulcers and pain vary by work group unit, referred to as clinical microsystems, and thus facility-level measures might mask unit-level improvements. An alternative design would target smaller networks of individuals that require high-quality interactions to self-organize effectively. Targeting smaller work groups with interventions also was suggested after disappointing results of the INTERACT trial. A second implication for future nursing home research is to consider randomization stratified on baseline measures rather than facility characteristics.
Our study also has implications for clinicians. While CONNECT had limited impact at the nursing-home level, focus groups indicated that staff are hungry to discuss communication problems that they are encountering, and welcome practicing strategies to improve them. The present analysis demonstrated that CONNECT had the greatest impact with LPNs, dietary, and environmental services workers—groups who are often overlooked. Nursing home administrators should consider whether select work groups may particularly benefit from communication interventions such as CONNECT as part of their culture change initiatives. Second, quality improvement programs may require more substantial process changes than are typically provided. In contrast to previous reports, the AHRQ falls management program (enhanced by learning modules, academic detailing, and audit and feedback reports) did not result in a measurable change in process or outcome measures. New models are needed to radically alter care for complex geriatric syndromes, for example, using trained volunteers to deliver a daily walking program, or doing routine bedside team evaluations for at-risk residents that include their direct care workers and family.
Limitations
Our study results should be interpreted considering its strengths and weaknesses. While randomized, the relatively small number of nursing homes (N = 24) likely resulted in imbalances in facility-, staff-, and resident-level factors by chance alone, as evidenced by the lower baseline staff survey response rate in intervention facilities. While our facility characteristics are generally similar to the US average, we were limited to 1 geographic region. As noted, unexpected measurement variability in both staff and resident outcomes resulted in lower-than-anticipated power to detect a meaningful difference; however, the magnitude of the observed changes is small.
Conclusions
In summary, although we achieved small improvements in connections, information flow, and use of cognitive diversity, we found no overall benefit for reducing falls. Furthermore, there was no difference in fall rates before and after the introduction of an established falls quality improvement intervention. Future research should focus on targeting meaningful work units/clusters and engagement of supervisors and administrators. Alternative models for falls quality improvement are needed.
Trial Protocol
eFigure. Intervention and data collection timeline
References
- 1.Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55(5):780-791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk factors for falls, incontinence, and functional dependence: unifying the approach to geriatric syndromes. JAMA. 1995;273(17):1348-1353. [PubMed] [Google Scholar]
- 3.Becker C, Kron M, Lindemann U, et al. Effectiveness of a multifaceted intervention on falls in nursing home residents. J Am Geriatr Soc. 2003;51(3):306-313. [DOI] [PubMed] [Google Scholar]
- 4.Dyer CAE, Taylor GJ, Reed M, Dyer CA, Robertson DR, Harrington R. Falls prevention in residential care homes: a randomised controlled trial. Age Ageing. 2004;33(6):596-602. [DOI] [PubMed] [Google Scholar]
- 5.Jensen J, Lundin-Olsson L, Nyberg L, Gustafson Y. Fall and injury prevention in older people living in residential care facilities.: a cluster randomized trial. Ann Intern Med. 2002;136(10):733-741. [DOI] [PubMed] [Google Scholar]
- 6.Rubenstein LZ, Robbins AS, Josephson KR, Schulman BL, Osterweil D. The value of assessing falls in an elderly population: a randomized clinical trial. Ann Intern Med. 1990;113(4):308-316. [DOI] [PubMed] [Google Scholar]
- 7.McMurdo ME, Millar AM, Daly F. A randomized controlled trial of fall prevention strategies in old peoples’ homes. Gerontology. 2000;46(2):83-87. [DOI] [PubMed] [Google Scholar]
- 8.Kerse N, Butler M, Robinson E, Todd M. Fall prevention in residential care: a cluster, randomized, controlled trial. J Am Geriatr Soc. 2004;52(4):524-531. [DOI] [PubMed] [Google Scholar]
- 9.Neyens JCL, Dijcks BPJ, Twisk J, et al. A multifactorial intervention for the prevention of falls in psychogeriatric nursing home patients, a randomised controlled trial (RCT). Age Ageing. 2009;38(2):194-199. [DOI] [PubMed] [Google Scholar]
- 10.Sutcliffe KM, Paine L, Pronovost PJ. Re-examining high reliability: actively organising for safety. BMJ Qual Saf. 2017;26(3):248-251. [DOI] [PubMed] [Google Scholar]
- 11.Sullivan JL, Rivard PE, Shin MH, Rosen AK. Applying the high reliability health care maturity model to assess hospital performance: a VA case study. Jt Comm J Qual Patient Saf. 2016;42(9):389-411. [DOI] [PubMed] [Google Scholar]
- 12.Anderson RA, Issel LM, McDaniel RR Jr. Nursing homes as complex adaptive systems: relationship between management practice and resident outcomes. Nurs Res. 2003;52(1):12-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Colón-Emeric CS, Lekan D, Utley-Smith Q, et al. Barriers to and facilitators of clinical practice guideline use in nursing homes. J Am Geriatr Soc. 2007;55(9):1404-1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Colón-Emeric CS, Lekan-Rutledge D, Utley-Smith Q, et al. Connection, regulation, and care plan innovation: a case study of four nursing homes. Health Care Manage Rev. 2006;31(4):337-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Colón-Emeric C, Ammarell N, Bailey D, et al. Care planning in skilled nursing facilities through a complexity science lens. Paper presented at: American Geriatric Society 2005 Annual Scientific Meeting; May 11-15, 2005; Orlando, Florida. [Google Scholar]
- 16.Colón-Emeric CS, Ammarell N, Bailey D, et al. Patterns of medical and nursing staff communication in nursing homes: implications and insights from complexity science. Qual Health Res. 2006;16(2):173-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Colón-Emeric CS, Plowman D, Bailey D, et al. Regulation and mindful resident care in nursing homes. Qual Health Res. 2010;20(9):1283-1294. doi: 10.1177/1049732310369337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Toles M, Anderson RA. State of the science: relationship-oriented management practices in nursing homes. Nurs Outlook. 2011;59(4):221-227. [DOI] [PubMed] [Google Scholar]
- 19.Barry TT, Brannon D, Mor V. Nurse aide empowerment strategies and staff stability: effects on nursing home resident outcomes. Gerontologist. 2005;45(3):309-317. [DOI] [PubMed] [Google Scholar]
- 20.Anderson RA, McDaniel RR Jr. Intensity of registered nurse participation in nursing home decision making. Gerontologist. 1998;38(1):90-100. [DOI] [PubMed] [Google Scholar]
- 21.Corazzini-Gomez K, Anderson R, McDaniel R. Quality of care and nurse aide participation in decision-making about resident care. Gerontologist. 2002;42:74. [Google Scholar]
- 22.Anderson RA, McDaniel RR Jr. RN participation in organizational decision making and improvements in resident outcomes. Health Care Manage Rev. 1999;24(1):7-16. [DOI] [PubMed] [Google Scholar]
- 23.Anderson RA, Ammarell N, Bailey D Jr, et al. Nurse assistant mental models, sensemaking, care actions, and consequences for nursing home residents. Qual Health Res. 2005;15(8):1006-1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anderson RA, Corazzini K, Porter K, Daily K, McDaniel RR Jr, Colón-Emeric C. CONNECT for quality: protocol of a cluster randomized controlled trial to improve fall prevention in nursing homes. Implement Sci. 2012;7(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Colon-Emeric CS, McConnell E, Pinheiro SO, et al. CONNECT for better fall prevention in nursing homes: results from a pilot intervention study. J Am Geriatr Soc. 2013;61(12):2150-2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kamimura A, Banaszak-Holl J, Berta W, Baum JA, Weigelt C, Mitchell W. Do corporate chains affect quality of care in nursing homes? the role of corporate standardization. Health Care Manage Rev. 2007;32(2):168-178. [DOI] [PubMed] [Google Scholar]
- 27.Resnick B, Inguito P, Orwig D, et al. Treatment fidelity in behavior change research: a case example. Nurs Res. 2005;54(2):139-143. [DOI] [PubMed] [Google Scholar]
- 28.Anderson RA, Toles MP, Corazzini K, McDaniel RR, Colón-Emeric C. Local interaction strategies and capacity for better care in nursing homes: a multiple case study. BMC Health Serv Res. 2014;14(1):244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor JA, Parmelee P, Brown H, Strothers HS III, Capezuti E, Ouslander JG. A model quality improvement program for the management of falls in nursing homes. J Am Med Dir Assoc. 2007;8(3)(suppl):S26-S36. [DOI] [PubMed] [Google Scholar]
- 30.O’Reilly C, Roberts K. Task group structure, communication, and effectiveness in three organizations. J Appl Psychol. 1977;62(6):674-681. [Google Scholar]
- 31.Shortell SM, Zimmerman JE, Rousseau DM, et al. The performance of intensive care units: does good management make a difference? Med Care. 1994;32(5):508-525. [DOI] [PubMed] [Google Scholar]
- 32.Anderson RA, Plowman D, Corazzini K, et al. Participation in decision making as a property of complex adaptive systems: developing and testing a measure. Nurs Res Pract. 2013;2013:706842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vogus TJ, Sutcliffe KM. The Safety Organizing Scale: development and validation of a behavioral measure of safety culture in hospital nursing units. Med Care. 2007;45(1):46-54. [DOI] [PubMed] [Google Scholar]
- 34.Jung S-H, Ahn C. Sample size estimation for GEE method for comparing slopes in repeated measurements data. Stat Med. 2003;22(8):1305-1315. [DOI] [PubMed] [Google Scholar]
- 35.Collins LM, Schafer JL, Kam CM. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychol Methods. 2001;6(4):330-351. [PubMed] [Google Scholar]
- 36.Zwarenstein M, Reeves S. Knowledge translation and interprofessional collaboration: where the rubber of evidence-based care hits the road of teamwork. J Contin Educ Health Prof. 2006;26(1):46-54. [DOI] [PubMed] [Google Scholar]
- 37.Ferlie E, Fitzgerald L, Wood M, Hawkins C. The nonspread of innovations: the mediating role of professionals. Acad Manage J. 2005;48(1):117-134. [Google Scholar]
- 38.Tjia J, Mazor KM, Field T, Meterko V, Spenard A, Gurwitz JH. Nurse-physician communication in the long-term care setting: perceived barriers and impact on patient safety. J Patient Saf. 2009;5(3):145-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Colón-Emeric CS, Corazzini K, McConnell E, et al. Study of individualization and bias in nursing home fall prevention practices. J Am Geriatr Soc. 2017;65(4):815-821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stacey RD. Complexity and Creativity in Organizations. San Francisco, CA: Berrett-Koehler; 1996. [Google Scholar]
- 41.Norton PG, Murray M, Doupe MB, et al. Facility versus unit level reporting of quality indicators in nursing homes when performance monitoring is the goal. BMJ Open. 2014;4(2):e004488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kane RL, Huckfeldt P, Tappen R, et al. Effects of an intervention to reduce hospitalizations from nursing homes: a randomized implementation trial of the interact program [published online July 3, 2017]. JAMA Intern Med. doi: 10.1001/jamainternmed.2017.2657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Colón-Emeric CS, Pinheiro SO, Anderson RA, et al. Connecting the learners: improving uptake of a nursing home educational program by focusing on staff interactions. Gerontologist. 2014;54(3):446-459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rask K, Parmelee PA, Taylor JA, et al. Implementation and evaluation of a nursing home fall management program. J Am Geriatr Soc. 2007;55(3):342-349. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eFigure. Intervention and data collection timeline