This cohort study assesses the association of expanded Medicaid eligibility under the Affordable Care Act with duration of hospitalization among patients with traumatic injury.
Key Points
Question
What was the association of the expansion of Medicaid eligibility under the Patient Protection and Affordable Care Act (ACA) with hospital length of stay after injury?
Findings
In this single-center cohort study of 2314 patients from 2 states and Washington, DC, with different levels of Medicaid expansion, expansion of Medicaid eligibility was associated with a significant reduction in length of stay after injury. Moreover, duration of hospitalization was significantly reduced in a graduated fashion in proportion to the degree that Medicaid eligibility was expanded.
Meaning
Expansion of Medicaid eligibility under the Affordable Care Act was associated with reductions in duration of hospitalization after injury; the potential cost savings should be further investigated.
Abstract
Importance
The expansion of Medicaid eligibility under the Affordable Care Act is a state-level decision that affects how patients with traumatic injury (trauma patients) interact with locoregional health care systems. Washington, DC; Maryland; and Virginia represent 3 unique payer systems with liberal, moderate, and no Medicaid expansion, respectively, under the Affordable Care Act. Characterizing the association of Medicaid expansion with hospitalization after injury is vital in the disposition planning for these patients.
Objective
To determine the association between expanded Medicaid eligibility under the Affordable Care Act and duration of hospitalization after injury.
Design, Setting, and Participants
This retrospective cohort study included patients admitted from Virginia, Maryland, and Washington, DC, to a single level I trauma center. Data were collected from January 1, 2013, through March 6, 2016, in Virginia and Washington, DC, and from May 1, 2013, through March 6, 2016, in Maryland. All patients with Medicare or Medicaid coverage and all uninsured patients were included. Patients with private insurance, patients with severe head or pelvic injuries, and those who died during hospitalization were excluded.
Main Outcomes and Measures
Hospital length of stay (LOS) and whether its association with patient insurance status varied by state of residence.
Results
A total of 2314 patients (1541 men [66.6%] and 773 women [33.4%]; mean [SD] age, 52.9 [22.8] years) were enrolled in the study. The uninsured rate in the Washington, DC, cohort (190 of 1699 [11.2%]) was significantly lower compared with rates in the Virginia (141 of 296 [47.6%]) or the Maryland (106 of 319 [33.2%]) cohort (P < .001). On multivariate regression controlling for injury severity and demographic variables, the difference in LOS for Medicaid vs non-Medicaid recipients varied significantly by state. For Medicaid recipients, mean LOS in Washington, DC, was significantly shorter (2.57 days; 95% CI, 2.36-2.79 days) than in Maryland (3.51 days; 95% CI, 2.81-4.38 days; P = .02) or Virginia (3.9 days; 95% CI, 2.79-5.45 days; P = .05).
Conclusions and Relevance
Expanded Medicaid eligibility is associated with shorter hospital LOS in mildly injured Medicaid recipients.
Introduction
With the passage of the Patient Protection and Affordable Care Act (ACA) in 2010, 32 states and Washington, DC, expanded Medicaid to include patients whose income is less than 133% above the federal poverty level (FPL). This change, in addition to expansion of parental health insurance coverage to 26 years of age, the creation of the individual mandate, and the formation of insurance exchanges, led to an overall decrease in the national uninsured rate from 16.0% in 2010 to 9.1% in 2015. States that expanded Medicaid have seen substantial reductions in their uninsured rates, and evidence suggests a correlation with improved outcomes.
The Supreme Court upheld the constitutionality of the ACA and retained the individual mandate but made Medicaid expansion a state-level decision. Subsequently, wide variability has ensued in the adoption of Medicaid expansion among states, with variable effects in Medicaid-associated benefits. Our level I trauma center receives patients from Washington, DC; Maryland; and Virginia. Within our region, a significant variability exists in Medicaid eligibility, from liberal Medicaid expansion in Washington, DC, to moderate expansion in Maryland and no expansion in Virginia.
Trauma centers are required to treat all patients, regardless of insurance status, but the same does not hold true for inpatient or outpatient rehabilitation and health service providers. Because of this requirement, uninsured patients are more likely to be discharged to home or to the community (ie, homeless), whereas insured patients are more likely to be discharged to a rehabilitation center or to receive home health services after their hospitalization. Patients who are not eligible for transfer to a rehabilitation center or who cannot be discharged to home with home services frequently have to spend additional days in the hospital to recover to a point where they can be discharged safely. Although studies have examined the association of insurance status with mortality rates, the association of Medicaid expansion eligibility with hospital length of stay (LOS) for injured patients remains poorly defined.
The primary aim of this study was to determine whether expanded Medicaid eligibility under the ACA is correlated with a decrease in hospital LOS after injury, compared with payer systems that did not expand coverage. A secondary aim was to determine whether the degree of Medicaid expansion correlates with reductions in hospital LOS. We hypothesize that hospital LOS is reduced in states with Medicaid expansion after injury.
Methods
We performed a retrospective study of all adult patients with traumatic injury (hereinafter referred to as trauma patients) admitted to our level I urban trauma center from January 1, 2013, to March 6, 2016. In the case of Maryland, however, only patients admitted after May 1, 2013, were included because Maryland did not implement the ACA and Medicaid expansion until this time. Insurance information was obtained from hospital financial records at the time of discharge and cross-referenced with the trauma registry. All patients with Medicaid or Medicare insurance and those who were uninsured were enrolled in the study. Because Medicare benefits are constant across all states, whereas Medicaid benefits vary by state, Medicare recipients were enrolled to provide a comparison between public-based insurance programs and the Medicaid expansion. Patients with commercial insurance, those whose payer information was not known, who resided in states outside the Washington, DC, metropolitan area, or who died were excluded. In addition, patients with severe head or pelvic injuries (denoted by an Abbreviated Injury Score [AIS] of 4 or 5; range, 1-5, with higher scores indicating greater severity) were excluded because they were expected to have prolonged hospitalizations at baseline. The institutional review board of George Washington University approved this study and waived the need for informed consent for this retrospective data analysis.
The following data points were collected for each patient: age, sex, Injury Severity Score (ISS; range, 0-75, with higher scores indicating greater severity), AIS for head and for pelvis, location of residence (Washington, DC; Virginia; or Maryland), and home zip code. Socioeconomic status (SES) was calculated using zip code data from the Centers for Disease Control and Prevention, including percentage of unemployed population (reversed), median household income, and percentage of population below the FPL (reversed) to create a neighborhood SES variable. Each of these 3 variables were standardized, their mean was calculated, and this resulting score was rescaled to range from 0 (lowest SES) to 100 (highest SES). Insurance status was classified as Medicaid, Medicare, or uninsured.
The primary outcome measure was hospital LOS. The primary question was whether the association of insurance with LOS varied by state of residence. In particular, we wanted to know whether a stepwise increase occurred in the LOS of Medicaid compared with non-Medicaid recipients from the location with highest (Washington, DC) to the lowest (Virginia) ACA Medicaid expansion. Data are summarized as the mean (SD) for continuous variables and as a proportion for categorical variables. Univariate associations with state and insurance type were examined using the χ2 test or the Fisher exact test for categorical variables and the Kruskal-Wallis test or the 2-tailed t test for continuous variables, depending on the normalcy of the data distribution. Because several of the insurance, injury, and demographic variables were expected to be highly correlated, we tested for collinearity using weighted regression before running multivariate models and removed variables that were highly collinear; thus, in the final models, all predictive variables had a variance inflation factor of less than 2.0. After adjusting for patient demographic characteristics, ISS, penetrating injury, and AIS for the head and pelvis, a multivariate linear model was created to predict LOS. We focused on the state by insurance interaction term, which would indicate whether the association of insurance by LOS varied by state. Because LOS was positively skewed, the natural log of LOS was used as the dependent variable. Subgroup analyses were then conducted within states and within insurance types. Because sample sizes were smaller than in the full analysis, we used backward elimination to maximize power, eliminating variables with P > .10 from the final models. All data analysis was performed using SAS software (version 9.3; SAS Institute Inc), with P < .05 considered to be statistically significant.
Results
During the study period, 4883 patients were admitted to our trauma service, of whom 2314 were included in the study. Of these, 1699 (73.4%) resided in Washington, DC; 319 (13.8%) in Maryland; and 296 (12.8%) in Virginia (Table 1). Mean (SD) age was 52.9 (22.8) years, with 773 women (33.4%) and 1541 men (66.6%). The mean ISS was 6.5 (5.0), and 250 patients (10.8%) had penetrating injuries. Patients from Washington, DC, had a lower mean ISS (7.1 [6.0]) compared with residents of Virginia (8.0 [6.6]) or Maryland (8.1 [6.8]) (P = .02). A total of 923 patients in our study cohort (39.9%) were insured by Medicaid, whereas 954 (41.2%) were insured by Medicare and 437 (18.9%) were uninsured. States with Medicaid expansion had lower rates of uninsured patients (190 patients [11.2%] in Washington, DC; 106 [33.2%] in Maryland; and 141 [47.6%] in Virginia; P < .001).
Table 1. Patient Characteristics and Insurance Status by State.
| Characteristic | All (N = 2314) |
Washington, DC (n = 1699) |
Maryland (n = 319) |
Virginia (n = 296) |
P Valuea |
|---|---|---|---|---|---|
| Age, mean (SD), y | 52.9 (22.8) | 53.4 (22.5) | 53.8 (23.9) | 52.9 (23.5) | .90 |
| Female, No. (%) | 773 (33.4) | 589 (34.7) | 94 (29.5) | 90 (30.4) | .10 |
| ISS, mean (SD)b | 6.5 (5.0) | 7.1 (6.0) | 8.1 (6.8) | 8.0 (6.6) | .02 |
| AIS for head, mean (SD)c | 0.76 (1.0) | 0.91 (1.25) | 1.09 (1.50) | 1.02 (1.28) | .14 |
| AIS for pelvis, mean (SD)c | 0.76 (1.1) | 0.76 (1.10) | 0.67 (1.07) | 0.72 (1.03) | .40 |
| Penetrating injury, No. (%) | 250 (10.8) | 191 (11.2) | 33 (10.3) | 26 (8.8) | .44 |
| Insurance type, No. (%) | |||||
| Medicaid | 923 (39.9) | 840 (49.4) | 59 (18.5) | 24 (8.1) | <.001 |
| Medicare | 954 (41.2) | 669 (39.4) | 154 (48.3) | 131 (44.3) | |
| Uninsured | 437 (18.9) | 190 (11.2) | 106 (33.2) | 141 (47.6) | |
| SES score, mean (SD)d | 39.5 (26.2) | 32.6 (26.0) | 56.8 (14.8) | 63.9 (10.8) | <.001 |
| Below the FPL, mean (SD), % | 20.4 (14.0) | 24.5 (13.8) | 7.6 (5.5) | 9.2 (5.3) | <.001 |
Abbreviations: AIS, Abbreviated Injury Score; FPL, federal poverty level; ISS, Injury Severity Score; SES, socioeconomic status.
Calculated using the 2-tailed t test for age; the χ2 test for sex, penetrating injury, and insurance type; and a nonparametric Kruskal-Wallis test for AIS and ISS.
Scores range from 0 to 75, with higher scores indicating greater severity.
Scores range from 1 to 5, with higher scores indicating greater severity.
Calculated as described in the Methods section with a range of 0 (lowest SES) to 100 (highest SES).
Patient variables that were significantly associated with state of residence included ISS, SES, and insurance type (Table 1). In Washington, DC, a mean of 24.5% (13.8%) of residents were below the FPL compared with 7.6% (5.5%) in Maryland and 9.2% (5.3%) in Virginia (P < .001).
Insurance type was significantly associated with age, sex, ISS, AIS for head and pelvis, rate of penetrating injury, and SES score (Table 2). Patients in the Medicaid and uninsured cohorts were younger compared with Medicare recipients; however, Medicare recipients also appeared to have more severe injuries with higher mean ISS and AIS. A notable finding was the difference in the SES score, which was nearly twice as high in uninsured patients compared with Medicaid recipients.
Table 2. Patient Variables Associated With Insurance Type.
| Patient Variable | Medicaid (n = 923) |
Medicare (n = 954) |
Uninsured (n = 437) |
P Valuea |
|---|---|---|---|---|
| Age, mean (SD), y | 40.2 (14.7) | 74.3 (15.1) | 35.7 (12.9) | <.001 |
| Female, No. (%) | 215 (23.3) | 498 (52.2) | 60 (13.7) | <.001 |
| ISS, mean (SD)b | 7.0 (6.3) | 8.0 (6.0) | 6.8 (6.3) | <.001 |
| AIS for head, mean (SD)c | 0.8 (1.2) | 1.1 (1.4) | 1.0 (1.2) | .003 |
| AIS for pelvis, mean (SD)c | 0.7 (1.0) | 0.9 (1.2) | 0.5 (0.9) | <.001 |
| Penetrating injury, No. (%) | 164 (17.8) | 17 (1.8) | 69 (15.8) | <.001 |
| SES score, mean (SD)d | 26.2 (22.9) | 49.7 (22.4) | 47.4 (22.4) | <.001b |
Abbreviations: AIS, Abbreviated Injury Score; ISS, Injury Severity Score; SES, socioeconomic status.
Calculated using the 2-tailed t test for age; the χ2 test for sex, penetrating injury, and insurance type; and a nonparametric Kruskal-Wallis test for AIS, ISS, and SES.
Scores range from 0 to 75, with higher scores indicating greater severity.
Scores range from 1 to 5, with higher scores indicating greater severity.
Calculated as described in the Methods section with a range of 0 (lowest SES) to 100 (highest SES).
We found no significant difference in postdischarge disposition between states (Table 3). Seventy-three patients of 923 Medicaid recipients (7.9%) needed some form of postdischarge rehabilitation (including subacute rehabilitation, skilled nursing, or acute rehabilitation facility). In all states analyzed, most patients were discharged to home (754 [89.8%] in Washington, DC; 21 [87.5%] in Virginia 88%; and 55 [93.2%] in Maryland). However, our data do not evaluate which patients required, obtained, or used home physical or occupational therapy, required home equipment such as walkers, or needed home health aide visits.
Table 3. Disposition Status at Discharge and State for Medicaid Patients.
| Disposition | Medicaid Patients, No. (%) | ||
|---|---|---|---|
| Washington, DC (n = 840) |
Virginia (n = 24) |
Maryland (n = 59) |
|
| Home | 754 (89.8) | 21 (87.5)a | 55 (93.2)b |
| Inpatient | 20 (2.4) | 0 | 0 |
| SAR, SNF, or acute rehabilitation facility | 66 (7.9) | 3 (12.5) | 4 (6.8) |
Abbreviations: SAR, subacute rehabilitation facility; SNF, skilled nursing facility.
P = .75, compared with Washington, DC.
P = .68, compared with Washington, DC.
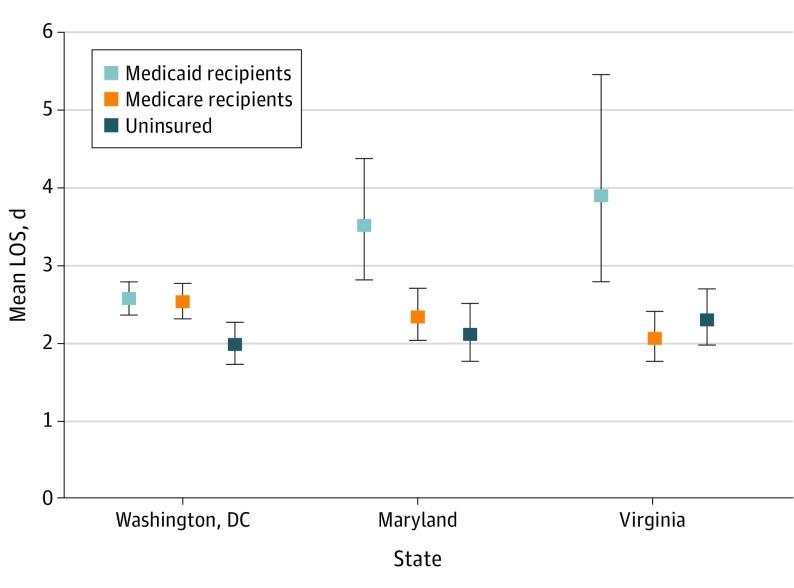
Finally, we developed a multivariable linear model to compare LOS among states with adjustment for age, sex, AIS score, ISS, mechanism of injury, and SES score (Table 4 and Figure). After adjusting for covariates, the interaction between state and type of insurance had a significant association with LOS (P < .001), indicating that the association between a patient’s insurance status and their LOS varied by state. Because Medicaid eligibility is a function of the percentage below the FPL and because this figure is state dependent, differences in LOS are likely to be a function of differences in the Medicaid eligibility. Length of stay for Medicaid patients from Washington, DC, was significantly shorter (2.57 days; 95% CI, 2.36-2.79 days) than for patients from Maryland (3.51 days; 95% CI, 2.81-4.38 days; P = .02) or Virginia (3.90 days; 95% CI, 2.79-5.45 days; P = .05) (Table 4). We found no significant differences in LOS for uninsured patients between states; however, Virginia Medicare recipients had a significantly shorter LOS (2.06 days; 95% CI, 1.77-2.41 days) compared with Washington, DC, Medicare recipients (2.53 days; 95% CI, 2.31-2.77 days; P = .008). The mean LOS was 1.33 days shorter for Medicaid patients in Washington, DC, vs Virginia (P = .05), and 0.94 days shorter in Washington, DC, vs Maryland (P = .02). Compared with Medicaid recipients, uninsured patients had an LOS shorter by 0.6 days in Washington, DC (P < .001), and by 1.6 days in Virginia (P = .003).
Table 4. Comparison of Adjusted Mean Hospital LOS by Insurance and State.
| Insurance Type | LOS, Mean (95% CI), da | ||
|---|---|---|---|
| Washington, DC | Maryland | Virginia | |
| Medicaid | 2.57 (2.36-2.79) | 3.51 (2.81-4.38)b | 3.90 (2.79-5.45)c |
| Medicare | 2.53 (2.31-2.77) | 2.34 (2.03-2.71)d | 2.06 (1.77-2.41)e |
| Uninsured | 1.98 (1.72-2.27) | 2.11 (1.77-2.50)f | 2.30 (1.97-2.70)g |
| Medicaid vs uninsured, P value | <.001 | <.001 | .003 |
Abbreviation: LOS, length of stay.
P values are adjusted for age, sex, Injury Severity Score, Abbreviated Injury Score for head and pelvis, penetrating injury, and socioeconomic status.
P = .02, compared with Washington, DC.
P = .05, compared with Washington, DC.
P = .008, compared with Washington, DC.
P = .68, compared with Washington, DC.
P = .92, compared with Washington, DC.
P = .09, compared with Washington, DC.
Figure. Adjusted Mean Length of Stay (LOS) by Insurance Coverage and State.
Data are adjusted for age, sex, Injury Severity Score, Abbreviated Injury Score for head and pelvis, penetrating injury, and socioeconomic status variable (calculated as described in the Methods section). Error bars show the 95% CI.
Discussion
In this study, the patient’s type of insurance coverage and their state of residence was significantly associated with hospital LOS, with reductions in LOS for Medicaid recipients in states that expanded Medicaid eligibility under the ACA. This finding is in line with those of previous studies, which demonstrated strong correlations between insurance status and clinical outcomes, including duration of hospitalization. We also found that states with Medicaid expansion had lower uninsured rates compared with nonexpansion states, an important finding because lack of insurance coverage has been associated with reduced access to rehabilitation facilities after discharge and less favorable patient outcomes.
Because the trauma patient population is disproportionately dependent on government-based health insurance programs compared with other patient populations, an understanding of the influences that federal- and state-level legislation have on patient outcomes is critical. Medicaid expansion and the cutoff for Medicaid eligibility is a state-dependent decision. Medicaid eligibility for states participating in Medicaid expansion under the ACA is set at a minimum of 133% of the FPL, which is a measure of income established by the 2016 poverty level guidelines for the 48 contiguous states and Washington, DC. The Washington, DC, metropolitan area represents a unique patient catchment that encompasses payer systems with liberal, moderate, or no adoptions of the ACA. Specifically, Virginia did not participate in Medicaid expansion and retains restrictive Medicaid eligibility requirements such that all nonelderly, nondisabled adults without dependents are ineligible for Medicaid regardless of income. Conversely, Maryland expanded Medicaid to include all adults earning less than 133% of the FPL, and Washington, DC, raised eligibility to 210% of the FPL for single, nonelderly, nondisabled adults without dependents. In effect, this makes Virginia a natural control against which we were able to measure the effects of moderate or liberal Medicaid expansion in Maryland and Washington, DC, respectively.
One of the key goals of the ACA was to decrease the number of uninsured persons by providing easier avenues to private and public health insurance. Although in our study cohort, the uninsured rate in Washington, DC, was 11.2% compared with 47.6% in Virginia, the uninsured rate compared with all patients admitted during our study period was approximately 8.9%, which is consistent with rates in previous literature.
Our key finding of shorter hospitalization for Medicaid recipients in Medicaid expansion states is provocative, but these findings may be circumstantial to the particular states represented in our cohorts. To test this possibility, we evaluated Medicare recipients and the uninsured to provide some comparison between public-based insurance programs and the effects of Medicaid expansion. Because Medicare is entirely funded by the federal government, the LOS of Medicare recipients should be unaffected by the implementation of Medicaid expansion and the legislation of the ACA. Similarly, alterations to Medicaid eligibility should not affect LOS for uninsured patients. We found no pattern of reductions in LOS among states as a function of altered Medicaid eligibility in the uninsured or Medicare cohorts. The mean LOS for uninsured trauma patients was significantly lower than the LOS for those with public health insurance in Washington, DC, and Virginia, a finding that has been published elsewhere. The reason for the discrepancy in uninsured LOS is unclear and likely to be multifactorial. The mean ISS among patients in our study was low, and few patients needed postdischarge rehabilitation regardless of insurance type, but often even mildly injured patients need postdischarge home services or equipment (eg, ambulatory assistance devices such as rolling walkers), which would have taken time to arrange and prolonged hospitalization. These services are paid for by Medicaid but are typically optional benefits for which patients qualify based on income level (ie, as a function of percentage of FPL). Uninsured patients opted or were recommended for earlier discharge in the wake of being ineligible for Medicaid-associated benefits. In comparison, patients who qualified for Medicaid and therefore had easier access to outpatient services may have incurred longer hospitalizations in the pursuit of these resources. A secondary hypothesis could be that because the SES score of the uninsured cohort was nearly double that of Medicaid recipients, uninsured patients may have been able to arrange postdischarge needs more easily than Medicaid recipients. Studies identifying the effect of postinjury rehabilitation and home health services on quality of life, even for patients with low-acuity injuries, are needed to optimize use of resources and delineate disparities in care between the publicly insured and uninsured.
We excluded the privately or commercially insured from our analysis for several reasons. First, Medicaid and Medicare are relatively uniform within states, but Medicaid and its associated benefits may differ among states depending on the optional benefits offered to eligible recipients. Private insurance plans, however, can vary widely in breadth and scope of coverage among patients regardless of state of residence, and therefore including the privately insured would introduce confounding biases that would make data analysis and interpretation difficult. Second, although the ACA created health insurance exchanges (also known as insurance marketplaces) to facilitate patient access to private insurance plans, differences in marketplace competition and variability in coverage between plans would likely confound results. On a prospective basis, measuring the effects of the ACA among the privately insured and accounting for differences in coverage would yield interesting results on the interaction between government legislation and the private sector in trauma patients.
Previous work has shown that the geographic distribution of trauma centers and prolonged transport times after severe injury may affect patient care and clinical outcomes. Evidence from the Medicare population has demonstrated that in patients who have undergone major surgery and are subsequently readmitted, an increased postdischarge travel distance more often leads to readmission to facilities other than the index hospital and fragmentation in care. In the trauma population, the effect of postdischarge distance on readmission rates and outcomes has not been well defined. In our cohorts, the maximal possible distance that any resident of Washington, DC, can travel from our center is 16 km, and the mean distance traveled was 20.6 (7.1) km for Virginia Medicaid recipients and 31.8 (29.1) km for Maryland Medicaid recipients. We did not calculate the mean travel distance for Washington, DC, patients because the size of the cohort made the calculation impractical, and overall postdischarge travel distance was not included in our multivariate analysis. This decision may have biased our results to longer LOS for patients who lived further from our hospital, namely, Maryland and Virginia residents. However, in subgroup analysis of Virginia and Maryland patients, the Pearson correlation coefficients between LOS and distance from our center were −0.14 and −0.08, respectively, indicating no meaningful correlation. Therefore, the contribution of travel distance to our findings was likely to have been small.
Finally, our multivariable linear model found that mildly injured patients in states that did not adopt the ACA had longer LOS. Moreover, this increase appears to have been graduated, mirroring the degree to which a state adopts and implements Medicaid expansion. Although the mean ISS in our study cohort was less than 7, we found significant differences in LOS among states. One would expect that in less injured patient populations, overall LOS would be relatively short, differences in LOS would be minimal, and the effect of health policy legislation on this patient population would be small. However, the ACA altered multiple components of Medicaid, including the interactions between postacute care rehabilitation services and reimbursement. The difference in LOS among Medicaid recipients is likely to be attributable to the unique package of Medicaid benefits, known as optional benefits, offered by each state. Although these benefits must be the same throughout a state, the breadth and scope of these packages often differ among states. A patient’s ability to qualify for these benefits is based on their income relative to the FPL and depends entirely on the eligibility criteria set by the state. Therefore, the differences found in Medicaid recipient LOS likely reflect these state-dependent optional benefit packages and therefore reflect changes in Medicaid eligibility set by the ACA.
Limitations
All studies are subject to limitations, and ours is no exception. First, our study design was retrospective in nature, with limitations inherent to its design, and represents the experience of a single institution. Our data analysis grouped all Medicaid recipients by state; however, as noted before, Medicaid and its associated benefits differ among states and among recipients within states. This subgroup heterogeneity may have skewed our results in unaccounted ways. Furthermore, our registry only captures insurance status at discharge, and some patients may have arrived at the hospital while uninsured and gained Medicaid coverage during their hospitalization. The difference in LOS may have been attributable to additional days that were spent obtaining some form of financial coverage to allow safe patient discharge. However, this possibility would be expected to have a negative effect on our results and would skew the result toward the null hypothesis. Our sample sizes in the Medicaid and uninsured cohorts in Virginia and Maryland were small, which is reflective of more restrictive Medicaid eligibility criteria; however, our small cohort sizes may have affected power and introduced type II error into our results. Finally, our data do not allow us to determine how many patients received and used home health services, such as physical, occupational, and/or speech therapies; home health aide visits; or access to equipment, and therefore we cannot address how use of those benefits affect postdischarge quality of life in the mildly injured population.
Conclusions
Expanded Medicaid eligibility under the ACA is associated with shorter hospital LOS in mildly injured Medicaid recipients. Moreover, our findings suggest a graduated reduction in LOS as Medicaid eligibility is increased. Future work investigating the disposition of trauma patients under the ACA on a national scale is needed to further illuminate the full association of Medicaid expansion with overall cost of care after injury.
References
- 1.Blavin F. Association between the 2014 Medicaid expansion and US hospital finances. JAMA. 2016;316(14):1475-1483. doi: 10.1001/jama.2016.14765 [DOI] [PubMed] [Google Scholar]
- 2.Ward B, Clarke T, Nugent C, Schiller J Early release of selected estimates based on data from the 2015 National Health Interview Survey. 2015. https://www.cdc.gov/nchs/nhis/releases/released201605.htm. May 24, 2016. Accessed August 5, 2016.
- 3.Benitez JA, Creel L, Jennings J. Kentucky’s Medicaid expansion showing early promise on coverage and access to care. Health Aff (Millwood). 2016;35(3):528-534. doi: 10.1377/hlthaff.2015.1294 [DOI] [PubMed] [Google Scholar]
- 4.Joseph B, Haider AA, Azim A, et al. The impact of patient protection and Affordable Care Act on trauma care: a step in the right direction. J Trauma Acute Care Surg. 2016;81(3):427-434. doi: 10.1097/TA.0000000000001082 [DOI] [PubMed] [Google Scholar]
- 5.Cheslik TG, Bukkapatnam C, Markert RJ, Dabbs CH, Ekeh AP, McCarthy MC. Initial impact of the Affordable Care Act on an Ohio level I trauma center. J Trauma Acute Care Surg. 2016;80(6):1010-1014. doi: 10.1097/TA.0000000000001052 [DOI] [PubMed] [Google Scholar]
- 6.Obama B. United States health care reform: progress to date and next steps. JAMA. 2016;316(5):525-532. doi: 10.1001/jama.2016.9797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mashaw JL. Legal, imagined, and real worlds: reflections on National Federation of Independent Business v. Sebelius. J Health Polit Policy Law. 2013;38(2):255-266. doi: 10.1215/03616878-1966243 [DOI] [PubMed] [Google Scholar]
- 8.Perkins J. Implications of the Supreme Court’s ACA Medicaid decision. J Law Med Ethics. 2013;41(suppl 1):77-79. doi: 10.1111/jlme.12045 [DOI] [PubMed] [Google Scholar]
- 9.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE III. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143(10):945-949. doi: 10.1001/archsurg.143.10.945 [DOI] [PubMed] [Google Scholar]
- 10.Haas JS, Goldman L. Acutely injured patients with trauma in Massachusetts: differences in care and mortality, by insurance status. Am J Public Health. 1994;84(10):1605-1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asemota AO, George BP, Cumpsty-Fowler CJ, Haider AH, Schneider EB. Race and insurance disparities in discharge to rehabilitation for patients with traumatic brain injury. J Neurotrauma. 2013;30(24):2057-2065. doi: 10.1089/neu.2013.3091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Metcalfe D, Davis WA, Olufajo OA, et al. Access to post-discharge inpatient care after lower limb trauma. J Surg Res. 2016;203(1):140-144. doi: 10.1016/j.jss.2016.02.036 [DOI] [PubMed] [Google Scholar]
- 13.Sawhney JS, Stephen AH, Nunez H, et al. Impact of type of health insurance on infection rates among young trauma patients. Surg Infect (Larchmt). 2016;17(5):541-546. doi: 10.1089/sur.2015.210 [DOI] [PubMed] [Google Scholar]
- 14.Alghnam S, Schneider EB, Castillo RC. Insurance status and health-related quality-of-life disparities after trauma: results from a nationally representative survey in the US. Qual Life Res. 2016;25(4):987-995. doi: 10.1007/s11136-015-1126-0 [DOI] [PubMed] [Google Scholar]
- 15.Gerry JM, Weiser TG, Spain DA, Staudenmayer KL. Uninsured status may be more predictive of outcomes among the severely injured than minority race. Injury. 2016;47(1):197-202. doi: 10.1016/j.injury.2015.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heffernan DS, Vera RM, Monaghan SF, et al. Impact of socioethnic factors on outcomes following traumatic brain injury. J Trauma. 2011;70(3):527-534. doi: 10.1097/TA.0b013e31820d0ed7 [DOI] [PubMed] [Google Scholar]
- 17.Duron VP, Monaghan SF, Connolly MD, et al. Undiagnosed medical comorbidities in the uninsured: a significant predictor of mortality following trauma. J Trauma Acute Care Surg. 2012;73(5):1093-1098. doi: 10.1097/TA.0b013e31826fc844 [DOI] [PubMed] [Google Scholar]
- 18.Taghavi S, Jayarajan SN, Duran JM, et al. Does payer status matter in predicting penetrating trauma outcomes? Surgery. 2012;152(2):227-231. doi: 10.1016/j.surg.2012.05.039 [DOI] [PubMed] [Google Scholar]
- 19.Chikani V, Brophy M, Vossbrink A, et al. Association of insurance status with health outcomes following traumatic injury: statewide multicenter analysis. West J Emerg Med. 2015;16(3):408-413. doi: 10.5811/westjem.2015.1.23560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Department of Health and Human Services. Annual Update of the HHS Poverty Guidelines. 2016. https://www.federalregister.gov/documents/2016/01/25/2016-01450/annual-update-of-the-hhs-poverty-guidelines. January 5, 2016. Accessed July 1, 2016.
- 21.Social Security Administration. Medicaid Information. https://www.ssa.gov/disabilityresearch/wi/medicaid.htm. Accessed July 21, 2016.
- 22.The White House. The consequences of state decisions note to expand Medicaid. https://obamawhitehouse.archives.gov/the-press-office/2014/07/02/white-house-report-missed-opportunities-and-consequences-state-decisions. Accessed November 21, 2016.
- 23.Medicaid eligibility criteria. 2016. https://www.medicaid.gov/medicaid/. Accessed November 20, 2016.
- 24.Gallup. In US, uninsured rate sinks to 13.4% in second quarter. http://www.gallup.com/poll/172403/uninsuredratesinkssecondquarter.aspx. July 10, 2014. Accessed November 21, 2016.
- 25.Toussaint RJ, Bergeron SG, Weaver MJ, Tornetta P III, Vrahas MS, Harris MB. The effect of the Massachusetts healthcare reform on the uninsured rate of the orthopaedic trauma population. J Bone Joint Surg Am. 2014;96(16):e141. doi: 10.2106/JBJS.M.00740 [DOI] [PubMed] [Google Scholar]
- 26.Englum BR, Hui X, Zogg CK, et al. Association between insurance status and hospital length of stay following trauma. Am Surg. 2016;82(3):281-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.HealthCare.gov. What Marketplace health insurance plans cover. https://www.healthcare.gov/coverage/what-marketplace-plans-cover/. Accessed March 19, 2017.
- 28.Ciesla DJ, Pracht EE, Cha JY, Langland-Orban B. Geographic distribution of severely injured patients: implications for trauma system development. J Trauma Acute Care Surg. 2012;73(3):618-624. doi: 10.1097/TA.0b013e3182509132 [DOI] [PubMed] [Google Scholar]
- 29.Crandall M, Sharp D, Unger E, et al. Trauma deserts: distance from a trauma center, transport times, and mortality from gunshot wounds in Chicago. Am J Public Health. 2013;103(6):1103-1109. doi: 10.2105/AJPH.2013.301223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tsai TC, Orav EJ, Jha AK. Care fragmentation in the postdischarge period: surgical readmissions, distance of travel, and postoperative mortality. JAMA Surg. 2015;150(1):59-64. doi: 10.1001/jamasurg.2014.2071 [DOI] [PubMed] [Google Scholar]
- 31.Zogg CK, Payró Chew F, Scott JW, et al. Implications of the Patient Protection and Affordable Care Act on insurance coverage and rehabilitation use among young adult trauma patients[published online December 21, 2016]. JAMA Surg. doi: 10.1001/jamasurg.2016.3609 [DOI] [PubMed] [Google Scholar]
- 32.Boninger JW, Gans BM, Chan L. Patient Protection and Affordable Care Act: potential effects on physical medicine and rehabilitation. Arch Phys Med Rehabil. 2012;93(6):929-934. doi: 10.1016/j.apmr.2012.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]