This cohort study analyzes the proportion of and independent risk factors for survival to discharge after initiation of continuous renal replacement among patients in a surgical intensive care unit.
Key Points
Question
What is the observed mortality among patients in a surgical intensive care unit after initiation of continuous renal replacement therapy?
Findings
This cohort study examined mortality among 108 patients in a surgical intensive care unit who required continuous renal replacement therapy. When 7 or more days of therapy were required, patients preparing to undergo liver transplant had an in-hospital mortality of 59.1%; patients in a general surgical group had a mortality of 100%.
Meaning
Continuous renal replacement is valuable for patients admitted to a surgical service with an acute and correctable indication; however, survival decreases significantly with increasing duration of therapy among patients with multiple-system organ failure.
Abstract
Importance
Continuous renal replacement therapy (CRRT) benefits patients with renal failure who are too hemodynamically unstable for intermittent hemodialysis. The duration of therapy beyond which continued use is futile, particularly in a population of patients admitted to and primarily cared for by a surgical service (hereinafter referred to as surgical patients), is unclear.
Objective
To analyze proportions of and independent risk factors for survival to discharge after initiation of CRRT among patients in a surgical intensive care unit (SICU).
Design, Setting, and Participants
This retrospective cohort study included all patients undergoing CRRT from July 1, 2012, through January 31, 2016, in an SICU of an urban tertiary medical center. The population included patients treated before or after general surgery and patients admitted to a surgical service during inpatient evaluation and care before liver transplant. The pretransplant population was censored from further survival analysis on receipt of a transplant.
Exposures
Continuous renal replacement therapy.
Main Outcomes and Measures
Hospital mortality among patients in an SICU after initiation of CRRT.
Results
Of 108 patients (64 men [59.3%] and 44 women [40.7%]; mean [SD] age, 62.0 [12.7] years) admitted to the SICU, 53 were in the general surgical group and 55 in the pretransplant group. Thirteen of the 22 patients in the pretransplant group who required 7 or more days of CRRT died (in-hospital mortality, 59.1%); among the 12 patients in the general surgery group who required 7 or more days of CRRT, 12 died (in-hospital mortality, 100%). In the general surgical group, each day of CRRT was associated with an increased adjusted odds ratio of death of 1.39 (95% CI, 1.01-1.90; P = .04).
Conclusions and Relevance
Continuous renal replacement therapy is valuable for surgical patients with an acute and correctable indication; however, survival decreases significantly with increasing duration of CRRT. Duration of CRRT does not correlate with survival among patients awaiting liver transplant.
Introduction
Continuous renal replacement therapy (CRRT) is a valuable modality in the care of acutely ill patients with indications for hemodialysis who are too hemodynamically unstable to tolerate the physiologic and hemodynamic stresses of intermittent hemodialysis (IHD).1,2 Use of the modality has expanded in recent years, making it the most common modality of renal replacement therapy in acute kidney injury, which is used in 8% to 10% of critically ill patients.3,4,5 We hypothesized that a duration existed beyond which continued CRRT is futile in patients admitted to and primarily cared for by a surgical service (hereinafter referred to as surgical patients).
Continuous renal replacement therapy use has also been shown to be independently associated with mortality compared with conventional IHD in the treatment of patients with sepsis.6 The appropriate timing of CRRT in patients with acute kidney injury undergoing surgery, including those with sepsis, is an area of current clinical controversy. Studies to date have not specifically examined surgical patients.7,8 Acute kidney injury is common in the preoperative or postoperative period in surgical patients, particularly those with severe sepsis, those who experience periods of hypotension from blood loss, or those with acute tubular necrosis from myogloginuria after trauma, and thus is an important area to investigate.9,10,11,12,13,14,15 Our objective was to characterize survival to discharge after varying days of consecutive CRRT among patients admitted to a surgical intensive care unit (SICU).
Methods
All patients admitted to a single SICU at the urban, academic tertiary care medical center from July 1, 2012, through January 31, 2016, and who required CRRT were included. The SICU at Cedars-Sinai Medical Center, Los Angeles, California, is the exclusive admitting unit for all critically ill patients undergoing trauma, general, gynecological, urologic, orthopedic, general (noncardiac) thoracic, vascular, and hepatobiliary surgery and patients in the abdominal transplant service who are older than 18 years, all of whom are candidates for CRRT when indicated. The study was approved by the institutional review board of Cedars-Sinai Medical Center, which waived the need for explicit patient consent because no direct contact with study participants was necessary.
The primary outcome of the study was survival to discharge among general surgical patients or survival to discharge or liver transplant among liver transplant candidates as a function of duration of CRRT. Patients who received CRRT only after liver transplant were excluded from analysis. Survival was censored from Kaplan-Meier and mortality analyses on receipt of a liver transplant in the pretransplant group only.
Institutional indications for initiating CRRT are acute or chronic renal failure meeting a criterion for initiation of hemodialysis, severe acidosis (pH, <7.2), refractory hyperkalemia, acute organ edema, uremia (serum urea nitrogen level of 40 mg/dL with symptoms [to convert to millimoles per liter, multiply by 0.357]), and/or extremity crush injury with a creatinine kinase level of greater than 20 000 U/L (to convert to microkatals per liter, multiply by 0.0167) in addition to inability to tolerate conventional IHD owing to hemodynamic instability. Criteria for cessation of therapy include terminal withdrawal of care, return of adequate renal function, resolution of underlying disorder, or improvement in hemodynamic status allowing transition to IHD. A global evaluation of the patient was conducted when deciding when to continue or to halt CRRT, and no specific hemodynamic data point was used when making the decision. The duration of CRRT was not considered when addressing the appropriateness of care during this study.
Patient age, sex, race/ethnicity, body mass index (calculated as weight in kilograms divided by height in meters squared), Acute Physiology and Chronic Health Evaluation IV score, preadmission stage IV chronic kidney disease, preadmission IHD, vasopressor use during CRRT, and consecutive number of days of CRRT were collected from the medical records. Outcomes measures included hospital mortality and, for Kaplan-Meier analysis, duration of hospital stay after initiation of CRRT.
Data were analyzed using SPSS statistical software (version 23; SPSS Inc) and are summarized as number and percentage for categorical variables and as mean (SD) for continuous variables. Comparisons of means used the paired t test or analysis of variance as appropriate. Categorical variables were compared using the Pearson χ2 test or Fisher exact test, with P < .05 considered to be statistically significant. Bivariate analysis of patient characteristics was performed between those who did or did not survive, and the characteristics differing significantly (P ≤ .20) between the survivors and deceased were incorporated into a stepwise forward logistic regression model. Kaplan-Meier analysis was used to compare survival to discharge between groups of patients based on duration of hospital stay after initiation of CRRT. The comparisons used a log-rank (Cox-Mantel) test. All P values are 2-sided.
Results
A total of 108 patients (64 men [59.3%] and 44 women [40.7%]; mean [SD] age, 62.0 [12.7] years) met the inclusion criteria (Table 1). Fifty-three patients were admitted to the SICU for general surgery (general surgical group); 55 were admitted to the SICU in anticipation of or for evaluation for liver transplant (pretransplant group).
Table 1. Patient Characteristics.
| Characteristic | General Surgical Group, Duration of CRRT | P Value | Pretransplant Group, Duration of CRRT | P Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All (N = 53) |
1-3 d (n = 26) |
4-6 d (n = 15) |
≥7 d (n = 12) |
All (N = 55) |
1-3 d (n = 22) |
4-6 d (n = 11) |
≥7 d (n = 22) |
|||
| Age, mean (SD), y | 67.2 (13.0) | 67 (12.7) | 66.8 (16.5) | 67.3 (11.9) | .99 | 57.2 (9.9) | 57.2 (10.2) | 52.9 (11.2) | 59.3 (8.8) | .23 |
| White, No. (%) | 38 (71.7) | 18 (69.2) | 9 (60) | 11 (91.7) | .18 | 48 (87.3) | 19 (86.4) | 10 (90.9) | 19 (86.4 | .92 |
| Male, No. (%) | 29 (54.7) | 15 (57.7) | 8 (53.3) | 6 (50) | .90 | 35 (63.6) | 12 (54.5) | 8 (72.7) | 15 (68.2) | .50 |
| BMI, mean (SD) | 24.9 (5.5) | 23.4 (5.1) | 26 (6.6) | 26.9 (4.1) | .11 | 27.9 (6.3) | 29.2 (6.4) | 27.5 (8.3) | 26.9 (4.9) | .45 |
| APACHE IV score, mean (SD)a | 42.2 (31.2) | 36 (32.2) | 44.3 (30.1) | 52.9 (29.8) | .32 | 31.4 (24.5) | 33.4 (24.9) | 22.1 (24.6) | 34.2 (23.9) | .37 |
| History of CKD, No. (%) | 20 (37.7) | 11 (42.3) | 1 (6.7) | 8 (66.7) | .005 | 10 (18.2) | 4 (18.2) | 1 (9.1) | 5 (22.7) | .63 |
| History of IHD, No. (%) | 20 (37.7) | 9 (34.6) | 4 (26.7) | 7 (58.3) | .22 | 7 (12.7) | 2 (9.1) | 1 (9.1) | 4 (18.2) | .61 |
| IHD preceding CRRT in SICU, No. (%) | 7 (13.2) | 1 (3.8) | 3 (20) | 3 (25) | .13 | 7 (12.7) | 3 (13.6) | 2 (18.2) | 2 (9.1) | .75 |
| Mechanical ventilation, No. (%) | 50 (94.3) | 25 (96.1) | 14 (93.3) | 11 (91.7) | .84 | 53 (96.4) | 20 (90.9) | 11 (100) | 22 (100) | .21 |
| Use of vasopressors during CRRT, No. (%) | 45 (84.9) | 22 (84.6) | 12 (80) | 11 (91.7) | .79 | 35 (63.6) | 7 (31.8) | 10 (90.9) | 18 (81.8) | <.001 |
Abbreviations: APACHE IV, Acute Physiology and Chronic Health Evaluation version IV; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CKD, chronic kidney disease; CRRT, continuous renal replacement therapy; IHD, intermittent hemodialysis; SICU, surgical intensive care unit.
Calculated using preexisting comorbidities, acute diagnosis, and variables related to acute physiology. Increases in the score are associated with increased risk of mortality (scores range from 0 to 286).
General Surgical Group
In the general surgical group, admissions were by a general, acute care, trauma, orthopedic, vascular, general thoracic (noncardiac), or gynecological surgical service. The mean (SD) age in this group was 67.2 (13.0) years; 29 of 53 (54.7%) were male, and 38 of 53 (71.7%) were white (Table 1). Patients were compared based on duration of CRRT for 1 to 3, 4 to 6, and 7 or more days. The only significantly different characteristic among these 3 groups was prevalence of chronic kidney disease (11 of 26 patients with 1-3 days of CRRT [42.3%], 1 of 15 with 4-6 days of CRRT [6.7%], and 8 of 12 with 7 or more days of CRRT [66.7%]; P = .005).
The mean number of consecutive days of CRRT for those surviving to discharge was lower than for those who did not survive (3.2 [1.5] vs 7.2 [6.8] days; P < .01). Bivariate analysis was performed comparing characteristics of those who did and did not survive (Table 2). Characteristics of survivors and nonsurvivors to discharge with a meaningful difference between groups were the proportion of patients who were white, who underwent IHD before CRRT during hospitalization, and who required vasopressor treatment during CRRT. These characteristics and days of continuous CRRT duration were incorporated into a forward regression analysis to determine independent risk factors for mortality. The only independent factor significantly associated with mortality was the number of days of continuous CRRT duration, with an adjusted odds ratio for mortality of 1.39 (95% CI, 1.01-1.90; P = .04) for each day of CRRT.
Table 2. Bivariate Analysis of Risk Factors for Mortality.
| Risk Factor | Patient Group | |||||||
|---|---|---|---|---|---|---|---|---|
| General Surgical | Pretransplant | |||||||
| No. of Patients (N = 53) |
Mortality, No. (%) | OR (95% CI) | P Value | No. of Patients (N = 55) |
Mortality, No. (%) | OR (95% CI) | P Value | |
| Age ≥65 y | ||||||||
| Yes | 32 | 20 (62.53) | 1.83 (0.60-5.60) | .29 | 10 | 6 (60) | 1.56 (0.39-6.32) | .53 |
| No | 21 | 10 (47.6) | 45 | 22 (48.9) | ||||
| White | ||||||||
| Yes | 38 | 24 (63.2) | 2.57 (0.76-8.76) | .13 | 48 | 25 (52.1) | 1.45 (0.29-7.18) | .65 |
| No | 15 | 6 (40) | 7 | 3 (42.8) | ||||
| Male | ||||||||
| Yes | 29 | 16 (55.2) | 0.88 (0.30-2.62) | .82 | 35 | 18 (51.4) | 1.06 (0.35-3.18) | .92 |
| No | 24 | 14 (58.3) | 20 | 10 (50) | ||||
| BMI ≥30 | ||||||||
| Yes | 8 | 5 (62.5) | 1.33 (0.28-6.27) | .72 | 18 | 9 (50) | 0.95 (0.31-2.92) | .93 |
| No | 45 | 25 (55.6) | 37 | 19 (51.4) | ||||
| APACHE IV score ≥25a | ||||||||
| Yes | 30 | 15 (50) | 0.58 (0.18-1.89) | .37 | 26 | 14 (53.8) | 1.26 (0.43-3.70) | .68 |
| No | 19 | 12 (63.2) | 27 | 13 (48.2) | ||||
| History of CKD | ||||||||
| Yes | 20 | 12 (60) | 1.25 (0.41-3.86) | .70 | 10 | 4 (40) | 0.58 (0.15-2.34) | .45 |
| No | 33 | 18 (54.5) | 45 | 24 (53.3) | ||||
| History of IHD | ||||||||
| Yes | 20 | 11 (55) | 0.90 (0.29-2.76) | .85 | 7 | 2 (28.6) | 0.34 (0.06-1.92) | .21 |
| No | 33 | 19 (57.6) | 48 | 26 (54.2) | ||||
| IHD preceding CRRT in SICU | ||||||||
| Yes | 7 | 7 (100) | 1.30 (1.07-1.60) | .01 | 7 | 4 (57.1) | 1.33 (0.27-6.61) | .72 |
| No | 46 | 23 (50) | 48 | 24 (50) | ||||
| Mechanical ventilation | ||||||||
| Yes | 50 | 28 (56) | 0.64 (0.05-7.48) | .72 | 53 | 27 (50.9) | 1.04 (0.06-17.49) | .98 |
| No | 3 | 2 (66.7) | 2 | 1 (50) | ||||
| Use of vasopressors during CRRT | ||||||||
| Yes | 45 | 28 (62.2) | 4.94 (0.89-27.32) | .07 | 35 | 22 (62.9) | 3.95 (1.22-12.81) | .02 |
| No | 8 | 2 (25) | 20 | 6 (30) | ||||
Abbreviations: APACHE IV, Acute Physiology and Chronic Health Evaluation version IV; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CKD, chronic kidney disease; CRRT, continuous renal replacement therapy; IHD, intermittent hemodialysis; OR, odds ratio; SICU, surgical intensive care unit.
Calculated using preexisting comorbidities, acute diagnosis, and variables related to acute physiology. Increases in the score are associated with increased risk of mortality (scores range from 0 to 286).
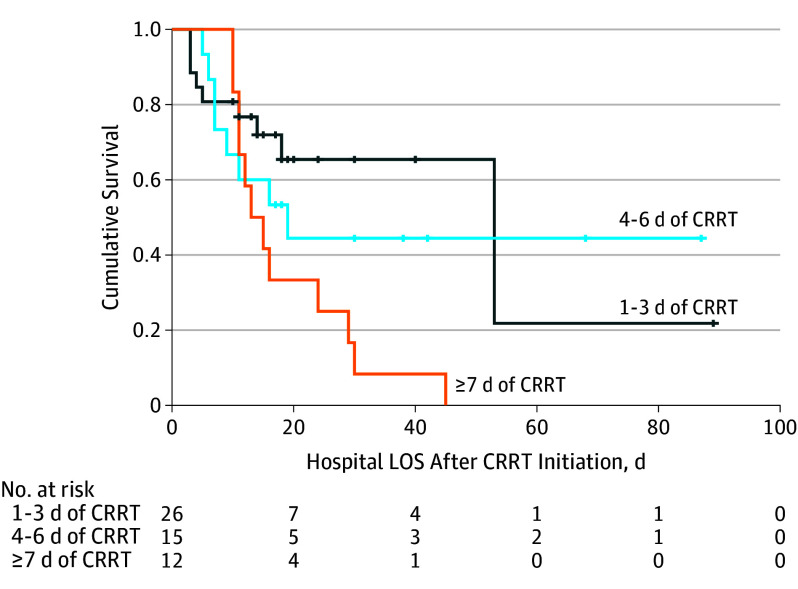
Analysis of patient survival to discharge based on duration of CRRT (Figure 1A) revealed in-hospital mortality of 38.5% (10 of 26) among patients undergoing 1 to 3 days of CRRT, 53.3% (8 of 15) among patients undergoing 4 to 6 days of CRRT, and 100% (12 of 12) among patients undergoing 7 or more days of CRRT. Kaplan-Meier analysis (Figure 2) established a significant difference in length of survival in the hospital after initiation of CRRT based on duration of therapy (log-rank test, P = .03). Estimated mean hospital survival after initiation of CRRT in the group with 7 or more consecutive days of CRRT was 18.8 days (95% CI, 13-25 days), with no survival to discharge from the hospital among these patients.
Figure 1. Analysis of In-Hospital Mortality by Duration of Continuous Renal Replacement Therapy (CRRT).
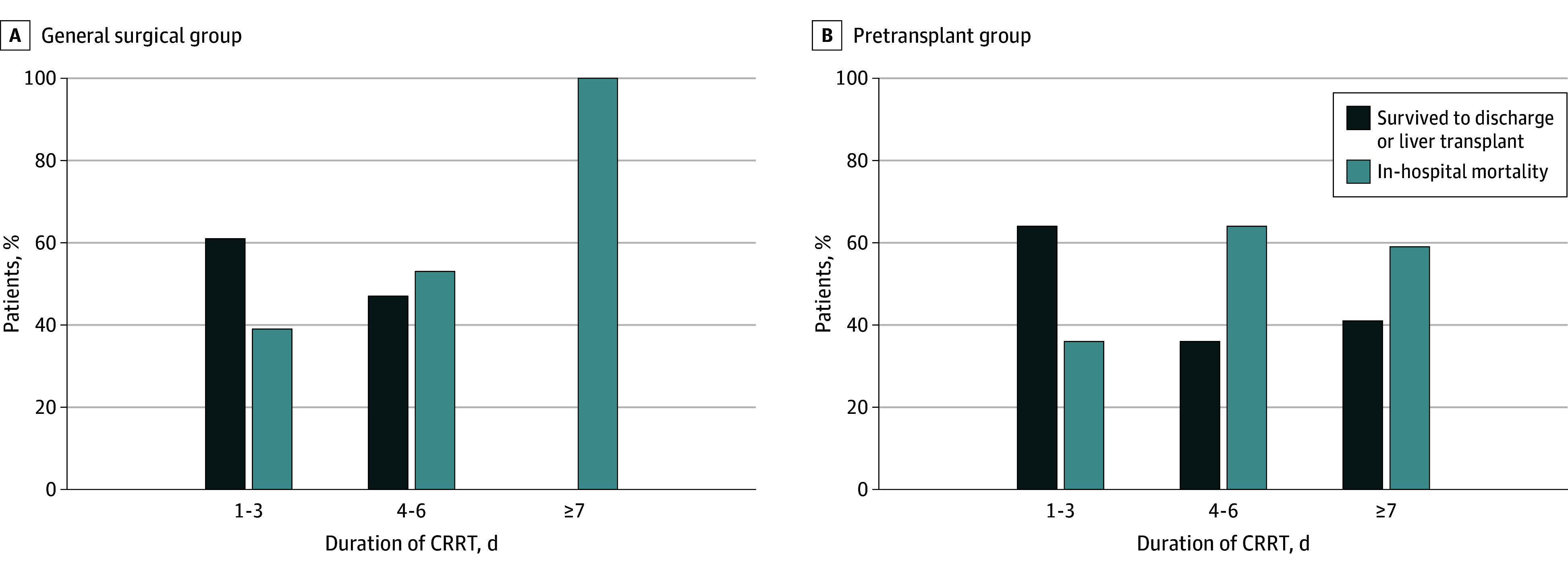
Patients included 53 in the general surgical group and 55 admitted to the surgical intensive care unit in anticipation of or for evaluation for liver transplant (pretransplant group).
Figure 2. Kaplan-Meier Survival by Length of Hospital Stay (LOS) for the General Surgical Group.
Patients are stratified by duration of continuous renal replacement therapy (CRRT). Patients were censored from survival analysis after discharge.
Pretransplant Group
Among the 55 patients admitted by the transplant surgical service in anticipation of or for evaluation for liver transplant, the mean age was 57.2 (9.9) years; 35 of 55 (63.6%) were male, and 48 of 55 (87.3%) were white. Additional details about patient demographic characteristics can be found in Table 1. Patient characteristics were compared on the basis of duration of CRRT for 1 to 3, 4 to 6, and 7 or more days. The only significantly different characteristic among these 3 groups was the need for vasopressor treatment during CRRT in 7 of 22 patients (31.8%) with 1 to 3 days of CRRT, 10 of 11 (90.9%) with 4 to 6 days of CRRT, and 18 of 22 (81.8%) with 7 or more days of CRRT (P < .001).
Analysis of patient survival to discharge based on duration of therapy is given in Figure 1B. In-hospital mortality was 36.4% (8 of 22) among patients undergoing 1 to 3 days of CRRT, 63.6% (7 of 11) among patients undergoing 4 to 6 days of CRRT, and 59.1% (13 of 22) among patients undergoing 7 or more days of CRRT.
The mean number of consecutive days of CRRT for those who did not survive was not significantly higher compared with those who survived or underwent liver transplant (8.0 [6.6] vs 6.4 [5.9] days; P = .33). Bivariate analysis was performed comparing hospital mortality. Survivors and nonsurvivors to discharge differed only in the proportion of patients who required vasopressor treatment during CRRT (13 [37.1%] vs 14 [70.0%]; P < .02). These characteristics and duration of continuous CRRT were incorporated into a forward regression analysis to determine independent risk factors of mortality. The only significant independent predictor of mortality was the need for vasopressor treatment during CRRT, with an adjusted odds ratio for mortality of 3.73 (95% CI, 1.09-12.7; P = .04).
Discussion
Acute kidney injury due to sepsis, hemorrhagic shock, crush, or ischemic injuries is common in surgical patients, often making them too unstable for IHD. Continuous renal replacement therapy has become the predominant mode of renal replacement therapy used in caring for critically ill patients with renal failure in medical ICUs or SICUs worldwide.3 For this population in an SICU, we report an overall mortality of 53.7% (58 of 108 patients). Although this mortality rate does not consider the number of patients excluded from mortality analysis (23 of 108) owing to liver transplant, it is near the range reported in large studies in the literature that have generally not included patients awaiting liver transplant.9,16,17,18 Few studies include patients in an SICU, and when included, these patients are rarely treated as a separate population. A notable exception is a study conducted by the National Taiwan University Surgical ICU Associated Renal Failure Study Group (NSARF) from 2002 to 2006,19 which found a 40% rate of survival at 90 days after initiation of CRRT among 137 patients undergoing surgery. Herein we report the in-hospital mortality rate among patients admitted to an exclusively surgical ICU and characterize the survival to discharge in this patient group. In doing so, we attempt to establish a reference point beyond which further therapy has been futile in our practice.
The SICU in this study cares primarily for patients admitted to a surgical service before or after surgery or trauma and a second group of patients admitted for treatment and workup of end-stage liver disease in anticipation of liver transplant. Table 1 gives the differences in patient characteristics between these 2 groups. The aforementioned Kaplan-Meier analysis given in Figure 2 further reveals that survival after initiation of CRRT is different (P = .03) in the general surgical group based on duration of therapy—an association that is not seen among patients awaiting liver transplant. These findings have implications for the duration of therapy that clinicians should be willing to provide patients awaiting liver transplant, erring on the side of continued therapy because duration did not independently correlate with mortality. In contrast, for the patients in the SICU who were not awaiting a liver transplant, duration of therapy directly correlated with in-hospital mortality. Our results in the general surgical sample suggest futility in continuing CRRT beyond 6 days because none of these patients survived to discharge despite a sometimes prolonged hospital stay and even after cessation of CRRT as indicated in the Kaplan-Meier analysis for survival after initiation of CRRT (Figure 2).
A general surgical patient may survive after 6 or more days of CRRT, and this survival is likely based on the presence of a correctable problem. We do not encourage the blanket statement that all general surgical patients with multiple-system organ failure should not be allowed to continue CRRT after 6 days. Instead, we suggest that our data indicate that mortality will likely be close to 100% after 6 days, and withholding CRRT should be considered when discussing the patient’s prognosis with their family.
Limitations
This study has multiple limitations. As a retrospective cohort study, it has no control group, and the specifics of underlying disease process, organ systems in failure, primary surgical treatment, or comorbidities are unavailable. Small sample size limits the power of the study and inhibits our ability to perform more robust statistics modeling. The surgical disciplines that admit critically ill patients to an exclusively surgical ICU vary between institutions and may affect the generalizability of these findings. At many institutions, patients admitted for workup for liver transplant are treated in medical ICUs by medical critical care specialists. We have controlled for the nongeneralizability of this population’s presence in our SICU by examining them separately from the other surgical patients in this study.
Conclusions
The decision to withhold or withdraw medical care in the critically ill population, even when the prognosis is poor, creates substantial challenges in patient care and family relations. Families and physicians often support the idea that any possible care that can be provided should be provided when there is a small chance of survival. Among general surgical patients admitted to an SICU, the proportion of patients surviving to discharge rapidly decreased with each additional day of CRRT, and no patient in our population survived to discharge after receiving more than 6 days of CRRT. After 6 days of CRRT, daily consideration should be given to withdrawing the therapy for this population. In addition, our findings suggest that it is futile to continue aggressive therapy in a patient who requires 7 or more days of CRRT. Among patients with an identifiable and rapidly reversible problem, such as hepatic failure before liver transplant, we found no significant association between duration of CRRT and mortality, providing an argument that supports the prolonged use of CRRT in patients who are admitted in anticipation of liver transplant. At present, to our knowledge, no similar studies have demonstrated mortality after CRRT among similar patients, and we therefore look forward to additional research on this topic, especially as related to the delivery of appropriate care.
References
- 1.Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. 2012;2(suppl 1):1-138. [Google Scholar]
- 2.Brochard L, Abroug F, Brenner M, et al. ; ATS/ERS/ESICM/SCCM/SRLF Ad Hoc Committee on Acute Renal Failure . An official ATS/ERS/ESICM/SCCM/SRLF statement: prevention and management of acute renal failure in the ICU patient: an international consensus conference in intensive care medicine. Am J Respir Crit Care Med. 2010;181(10):1128-1155. [DOI] [PubMed] [Google Scholar]
- 3.Prowle JR, Bellomo R. Continuous renal replacement therapy: recent advances and future research. Nat Rev Nephrol. 2010;6(9):521-529. [DOI] [PubMed] [Google Scholar]
- 4.Rewa OG, Villeneuve P-M, Lachance P, et al. Quality indicators of continuous renal replacement therapy (CRRT) care in critically ill patients: a systematic review [published online October 11, 2016]. Intensive Care Med. doi: 10.1007/s00134-016-4579-x [DOI] [PubMed] [Google Scholar]
- 5.Hoste EAJ, Bagshaw SM, Bellomo R, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41(8):1411-1423. [DOI] [PubMed] [Google Scholar]
- 6.Elseviers MM, Lins RL, Van der Niepen P, et al. ; SHARF Investigators . Renal replacement therapy is an independent risk factor for mortality in critically ill patients with acute kidney injury. Crit Care. 2010;14(6):R221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Payen D, Mateo J, Cavaillon JM, Fraisse F, Floriot C, Vicaut E; Hemofiltration and Sepsis Group of the Collège National de Réanimation et de Médecine d’Urgence des Hôpitaux extra-Universitaires . Impact of continuous venovenous hemofiltration on organ failure during the early phase of severe sepsis: a randomized controlled trial. Crit Care Med. 2009;37(3):803-810. [DOI] [PubMed] [Google Scholar]
- 8.Oh HJ, Kim MH, Ahn JY, et al. Can early initiation of continuous renal replacement therapy improve patient survival with septic acute kidney injury when enrolled in early goal-directed therapy? J Crit Care. 2016;35:51-56. [DOI] [PubMed] [Google Scholar]
- 9.Thakar CV. Perioperative acute kidney injury. Adv Chronic Kidney Dis. 2013;20(1):67-75. [DOI] [PubMed] [Google Scholar]
- 10.Morgan DJ, Ho KM. Acute kidney injury in bariatric surgery patients requiring intensive care admission: a state-wide, multicenter, cohort study. Surg Obes Relat Dis. 2015;11(6):1300-1306. [DOI] [PubMed] [Google Scholar]
- 11.Ishikawa S, Griesdale DEG, Lohser J. Acute kidney injury after lung resection surgery: incidence and perioperative risk factors. Anesth Analg. 2012;114(6):1256-1262. [DOI] [PubMed] [Google Scholar]
- 12.Abelha FJ, Botelho M, Fernandes V, Barros H. Determinants of postoperative acute kidney injury. Crit Care. 2009;13(3):R79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lim SY, Lee JY, Yang JH, et al. Predictive factors of acute kidney injury in patients undergoing rectal surgery. 2016;35(3):160-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Romagnoli S, Zagli G, Tuccinardi G, et al. Postoperative acute kidney injury in high-risk patients undergoing major abdominal surgery. J Crit Care. 2016;35:120-125. [DOI] [PubMed] [Google Scholar]
- 15.Brown CV, Dubose JJ, Hadjizacharia P, et al. Natural history and outcomes of renal failure after trauma. J Am Coll Surg. 2008;206(3):426-431. [DOI] [PubMed] [Google Scholar]
- 16.De Corte W, Dhondt A, Vanholder R, et al. Long-term outcome in ICU patients with acute kidney injury treated with renal replacement therapy: a prospective cohort study. Crit Care. 2016;20(1):256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prasad B, Urbanski M, Ferguson TW, Karreman E, Tangri N. Early mortality on continuous renal replacement therapy (CRRT): the Prairie CRRT study. Can J Kidney Health Dis. 2016;3(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oh HJ, Shin DH, Lee MJ, et al. Early initiation of continuous renal replacement therapy improves patient survival in severe progressive septic acute kidney injury. J Crit Care. 2012;27(6):743.e9-743.e18. [DOI] [PubMed] [Google Scholar]
- 19.Lin Y-F, Ko W-J, Chu T-S, et al. ; NSARF Study Group . The 90-day mortality and the subsequent renal recovery in critically ill surgical patients requiring acute renal replacement therapy. Am J Surg. 2009;198(3):325-332. [DOI] [PubMed] [Google Scholar]