Key Points
Question
Which hospital services drive increases in cost following surgical complications?
Findings
In this single-institution retrospective analysis, major complications tripled normalized hospital costs following total gastrectomy for gastric adenocarcinoma. Most increased costs were related to attempts to correct morbidity and prevent mortality.
Meaning
Interventions that decrease the number or severity of postoperative complications may achieve substantial cost savings.
This study describes the effect of postoperative complications on hospital costs following total gastrectomy for gastric adenocarcinoma.
Abstract
Importance
Postoperative complications are associated with increased hospital costs following major surgery, but the mechanism by which they increase cost and the categories of care that drive this increase are poorly described.
Objective
To describe the association of postoperative complications with hospital costs following total gastrectomy for gastric adenocarcinoma.
Design, Setting, and Participants
This retrospective analysis of a prospectively collected gastric cancer surgery database at a single National Cancer Institute–designated comprehensive cancer center included all patients undergoing curative-intent total gastrectomy for gastric adenocarcinoma between January 2009 and December 2012 and was conducted in 2015 and 2016.
Main Outcomes and Measures
Ninety-day normalized postoperative costs. Hospital accounting system costs were normalized to reflect Medicare reimbursement levels using the ratio of hospital costs to Medicare reimbursement and categorized into major cost categories. Differences between costs in Medicare proportional dollars (MP $) can be interpreted as the amount that would be reimbursed to an average hospital by Medicare if it paid differentially based on types and extent of postoperative complications.
Results
In total, 120 patients underwent curative-intent total gastrectomy for stage I through III gastric adenocarcinoma between 2009 and 2012. Of these, 79 patients (65.8%) were men, and the median (interquartile range) age was 64 (52-70) years. The 51 patients (42.5%) who underwent an uncomplicated total gastrectomy had a mean (SD) normalized cost of MP $12 330 (MP $2500), predominantly owing to the cost of surgical care (mean [SD] cost, MP $6830 [MP $1600]). The 34 patients (28.3%) who had a major complication had a mean (SD) normalized cost of MP $37 700 (MP $28 090). Surgical care was more expensive in these patients (mean [SD] cost, MP $8970 [MP $2750]) but was a smaller contributor to total cost (24%) owing to increased costs from room and board (mean [SD] cost, MP $11 940 [MP $8820]), consultations (mean [SD] cost, MP $3530 [MP $2410]), and intensive care unit care (mean [SD] cost, MP $7770 [MP $14 310]).
Conclusions and Relevance
Major complications were associated with tripled normalized costs following curative-intent total gastrectomy. Most of the excess costs were related to the treatment of complications. Interventions that decrease the number or severity of postoperative complications could result in substantial cost savings.
Introduction
National discussions on the value of health care have resulted in increased interest in understanding the cost and quality of care. In surgery, this has resulted in an intense focus on studying postoperative complications and their cost in a variety of different surgical conditions. Whether from single institutions, hospital networks, or national databases, it has been consistently shown that surgical complications increase postoperative cost, often by multiples of the cost of an uncomplicated operation. However, these studies have failed to fully describe the components of hospital care that drive these higher costs. Increased length of stay following complications is a consistent driver, but the studies are hampered by inconsistent methods and reporting. Costs are also captured in disparate ways, including hospital reimbursement by payers, hospital charges to payers, or not otherwise specified costs. In most cases, it is unclear how these costs can be compared either between institutions or in relation to the cost to society. We are not aware of any studies with detailed descriptions of the source of increased costs following surgical complications.
Gastric cancer, the second leading cause of cancer-related deaths globally, is typically treated with surgery; in advanced cases, chemotherapy is often added. In the United States, approximately 30% of all gastric resections are total gastrectomies, which are performed for diffuse tumors or those occurring at either the gastroesophageal junction or the proximal one-third of the stomach.
In 2015, we completed a comprehensive review of our institutional experience with total gastrectomy and its common complications, prompting analysis of the associated costs. The aim of this study is to describe in detail the association of postoperative complications with hospital cost and to identify specific drivers of the cost differences between patients following total gastrectomy for gastric adenocarcinoma.
Methods
Following institutional board review approval and a waiver of informed consent from the Memorial Sloan Kettering Cancer Center Institutional Review Board, all patients who underwent curative-intent total gastrectomy for stage I through III gastric adenocarcinoma from 2009 to 2012 were identified from our prospectively maintained institutional gastric cancer database. Preoperative, perioperative, and postoperative data points were collected, and all medical records were manually reviewed by a dedicated surgeon reviewer to ensure capture of all postoperative complications. No patients were lost to follow-up within the 90 days of our study period. All complications were prospectively graded on our modification of the Clavien-Dindo classification and classified as minor or major complications. Grades 1 (an event requiring oral medication) and 2 (an event requiring intravenous medication or a bedside procedure) were considered minor; grades 3 (an event requiring intubation or operative, endoscopic, or radiologic intervention), 4 (an event resulting in prolonged disability or organ resection), and 5 (death) were considered major. For the purposes of this analysis, patients who experienced both minor (grades 1 and 2) and major (grades 3-5) complications were analyzed within the major complications cohort.
Hospital Costs
The costs for each patient’s index admission and all inpatient and outpatient care at our institution for 90 days following discharge were determined from itemized hospital costs from our hospital accounting database. Both direct costs (costs of specific goods and services including physician services) and indirect costs (overhead costs not attributable to a specific good or service) were included. This approach of using internal cost accounting numbers created “bottom-up” estimates that we assume are roughly proportional to components costs in health care more generally; in absolute terms, the numbers are likely unique within our institution.
To yield generalizable estimates, we converted our institutional-level findings to Medicare reimbursement levels by matching each patient to the amount Medicare would reimburse for their care and then calculated a conversion factor across all patients that we then applied across all the component costs. Although most hospitals receive add-ons to their Medicare reimbursement, our conversion factor assumes no add-ons or adjustments and can be interpreted as a base Medicare reimbursement. In many respects, our approach parallels the method Medicare uses to determine reimbursement levels for hospital care, a process that involves hospitals reporting costs using bottom-up accounting and their own cost to charge multipliers and has been used in prior publications. Although not all patients in our study were Medicare beneficiaries, Medicare’s payment rates are one window into the societal costs of care.
In more detail, we estimated the total hospital costs for each patient in the study for relevant visit types (ie, initial surgical admission, readmissions, and outpatient visits). We then determined the ratio of those costs to the reimbursement Medicare pays based on US mean diagnosis-related group level reimbursements for inpatient admissions and the resource-based relative value scale–based reimbursement for outpatient visits, less any hospital-specific add-on payments, such as the add-on for indirect graduate medical education. The ratio we then generated, which is specific to visit type (ie, index admission, subsequent readmission, or outpatient visits), was then applied to each individual item recorded in the cost-accounting database. For example, if the ratio of mean resource-based relative value scale–based Medicare payment to hospital-specific outpatient visits was 90%, then an individual outpatient visit costing $100 is reported as $90 Medicare proportional dollars (MP $). Thus, the cost estimates reported here are not the costs specific to a single institution but instead reflect a number generalizable to base Medicare reimbursement.
All costs were estimated based on 2012 US dollars using 2012 costs per unit for all services and categorized as 1 of 3 visit types: initial surgical admission, subsequent readmission, or outpatient visit. Final cost estimates were rounded to the nearest $10 and are reported as MP $. Costs from adjuvant chemotherapy (either consultation with a medical oncologist or the costs of medications themselves) were not included in this analysis.
Total patient cost was estimated by combining total normalized cost for each visit type. Differences in MP $ between patients with different complications can therefore be interpreted as the amount that would be reimbursed to an average hospital by Medicare if the US Center for Medicare and Medicaid Services paid differentially based on types of postoperative complications and did not include add-on payments.
Cost Categorization
Individual line-item costs were classified as belonging to 1 of the following mutually exclusive cost categories: surgery (all surgical equipment and outpatient visits with the primary surgeon), consultations (all inpatient and outpatient visits with other attending physicians), room and board (room costs for non–intensive care unit rooms), intensive care unit (critical care consultations, critical care medications, and intensive care unit room costs), emergency department (all visits to our institution’s emergency department), and hospital care (all medications, imaging, therapy, and laboratory tests not otherwise assigned). We were particularly interested in the interventions frequently used to treat patients with intra-abdominal complications (interventional radiology and endoscopy) and analyzed the cost of these services separately and within the consult category.
Statistical Analysis
Descriptive statistics were calculated to examine cohort characteristics and estimated cost. Mean 90-day and postdischarge costs were calculated by surgical complication severity (ie, uncomplicated, minor, and major), number of complications, and complication grade. Mean postoperation cost was calculated for each specific cost category. The percentage of costs attributed to readmission was calculated by complication severity. All analyses were performed using Stata version 13.1 (StataCorp).
Results
Between January 1, 2009, and December 31, 2012, 120 patients underwent curative-intent total gastrectomy for stage I through III gastric adenocarcinoma at our institution. Patient, clinical, and pathologic characteristics are shown in Table 1. Our patients were predominantly male (79 of 120 [65.8%]), the median age was 64 years, and the most common medical comorbidity was hypertension. While most of our patients (102 [85.0%]) underwent open gastrectomy, the percentage of minimally invasive gastrectomy (18 [15.0%]) was twice as high as it was during our prior series (7.9%), reflecting an increase in our minimally invasive practice over time. Most of our patients (115 [95.8%]) had their esophageal-jejunal anastomosis reconstructed with surgical staplers; circular staplers (64 [53.3%]) were more common than linear staplers (51 [42.5%]). The remaining patients (5 [4.2%]) received a hand-sewn anastomosis.
Table 1. Clinical, Operative, and Pathologic Characteristics for All Patients in the Cohort.
| Characteristic | Cohort, No. (%) (N = 120) |
|---|---|
| Age, median (IQR), y | 64 (52-70) |
| Preoperative BMI, median (IQR) | 26 (23-30) |
| Male sex | 79 (65.8) |
| Diabetes | 19 (15.8) |
| Receiving oral medicine | 17 (14.2) |
| Receiving insulin | 2 (1.7) |
| Hypertension requiring medication | 53 (44.2) |
| Hypercholesterolemia requiring medication | 42 (35.0) |
| Active smoker | 12 (10.0) |
| Previous cardiac event | 14 (11.7) |
| Received neoadjuvant chemotherapy | 64 (53.3) |
| Received adjuvant chemotherapy | 40 (33.3) |
| Operative approach | |
| Open | 102 (85.0) |
| Minimally invasive | 18 (15.0) |
| Reconstruction method | |
| Circular stapler | 64 (53.3) |
| Linear stapler | 51 (42.5) |
| Hand sewn | 5 (4.2) |
| Final pathologic stage | |
| T stage | |
| T0a | 4 (3.3) |
| T1 | 38 (31.7) |
| T2 | 13 (10.8) |
| T3 | 38 (31.7) |
| T4 | 27 (22.5) |
| N stage | |
| N0 | 68 (56.7) |
| N1 | 21 (17.5) |
| N2 | 15 (12.5) |
| N3 | 16 (13.3) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); IQR, interquartile range; N, node; T, tumor.
All patients received neoadjuvant chemotherapy and had a complete pathological response.
Cost of Complications
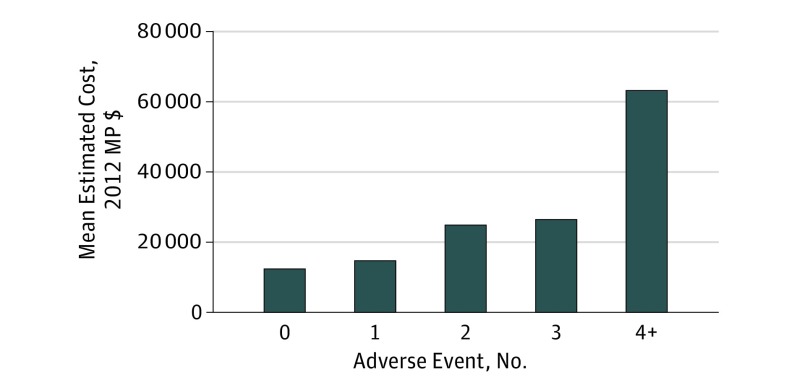
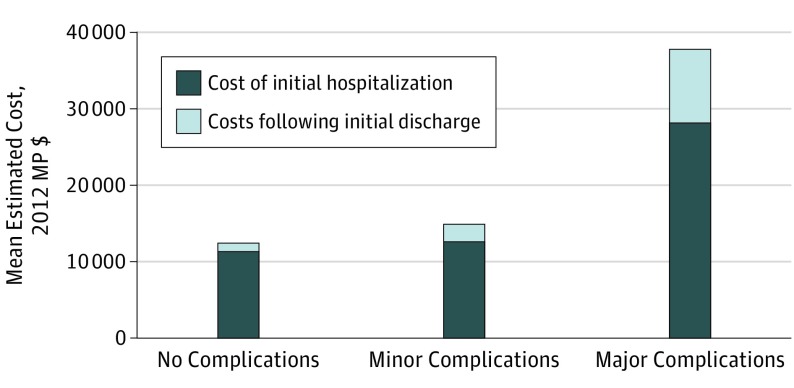
Overall, an uncomplicated total gastrectomy had a mean (SD) normalized 90-day cost of MP $12 330 (MP $2500), compared with an estimated mean (SD) normalized 90-day cost of MP $14 830 (MP $3470) for patients with minor complications and MP $37 700 (MP $28 090) for patients with major complications (Table 2). Table 2 shows the mean 90-day costs and clinical resource use as well as the breakdown of costs by categorized complication grade (ie, no complications, patients with minor complications only, and patients with at least 1 major complication). Increasing complication number, regardless of grade, was associated with an increase in 90-day costs (Figure 1). Though the initial surgical admission accounted for most costs for all groups, increasing complication grade resulted in increased postdischarge spending (Figure 2). Mean (SD) postdischarge costs for uncomplicated gastrectomies were MP $1000 (MP $1730), while mean (SD) postdischarge costs for patients with a major complication were MP $9530 (MP $10 390) (Table 2; Figure 2). In patients with minor complications, readmission costs (mean [SD] cost, MP $1260 [MP $2430]) accounted for approximately 56% of all postdischarge costs (mean [SD] cost, MP $2260 [MP $2750]), while readmission costs in patients with major complications (mean [SD] cost, MP $7970 [MP $10 350]) accounted for approximately 84% of all postdischarge costs (mean [SD] cost, MP $9530 [MP $10 390]). Postdischarge costs reflect all care provided at our institution, including outpatient visits with attending physicians, visits in our emergency department, and readmissions, but do not include postdischarge admissions to inpatient rehabilitation facilities, visiting nurse services, outpatient medications, or readmissions at other facilities.
Table 2. Estimated Mean 90-Day Cost (in 2012 Medicare Proportional Dollars) and Resource Use Following Curative-Intent Total Gastrectomy.
| Characteristic | Complications, Mean (SD), 2012 MP $a | ||
|---|---|---|---|
| None (n = 51 [42.5%]) | Minor (n = 35 [29.2%]) | Major (n = 34 [28.3%]) | |
| Total 90-d cost | 12 330 (2500) | 14 830 (3470) | 37 700 (28 090) |
| Initial hospitalization cost | 11 330 (2000) | 12 570 (2340) | 28 180 (24 150) |
| Postdischarge cost | 1000 (1730) | 2260 (2750) | 9530 (10 390) |
| Cost of all readmissions | 0 | 1260 (2430) | 7970 (10 350) |
| Categorized costs | |||
| Surgeryb | 6830 (1600) | 6950 (880) | 8970 (2750) |
| Consultationsc | 750 (950) | 960 (790) | 3530 (2410) |
| Interventional radiology | 0 | 0 | 930 (1000) |
| Endoscopy | 0 | 0 | 770 (1280) |
| ICU care | 0 | 0 | 7770 (14 310) |
| Room and board | 3620 (1070) | 5210 (2230) | 11 940 (8820) |
| Hospital servicesd | 1110 (340) | 1590 (600) | 5070 (4690) |
| ED care | 0 | 110 (180) | 430 (730) |
| Hospitalization characteristics, No. (%) | |||
| Length of stay, median (IQR), d | 6 (6-8) | 9.5 (7-15)e | 21 (12-29)f |
| Reoperation | 0 | 0 | 10 (29) |
| Interventional radiology | 0 | 0 | 22 (65) |
| Endoscopy | 0 | 0 | 12 (35) |
| Any ICU admission | 0 | 0 | 12 (35) |
| Total readmissions | 0 | 10 (29) | 9 (26) |
Abbreviations: ED, emergency department; ICU, intensive care unit; IQR, interquartile range; MP $, Medicare proportional dollars.
Estimated costs are 2012 MP $ expressed as mean (SD) and rounded to the nearest $10.
Surgery costs include the cost of the surgical procedure as well as all outpatient visits with the operative surgeon.
Consultation costs include the cost of all inpatient and outpatient visits with other attending surgeons, inclusive of interventional radiology and endoscopy.
Hospital costs include all medications, imaging, laboratory tests, and therapy (eg, physical therapy and occupational therapy) not specifically associated with another cost category.
In patients who had a minor complication prior to discharge.
In patients who had a major complication prior to discharge.
Figure 1. Estimated Cost in 2012 Medicare Proportional Dollars (MP $) Associated With Number of Complications Following Curative-Intent Total Gastrectomy.
Figure 2. Estimated Costs in 2012 Medicare Proportional Dollars (MP $) Occurring During or Following Index Hospitalization for Curative-Intent Total Gastrectomy by Complication Severity.
Minor complications: grades 1 and 2. Major complications: grades 3 through 5.
Cost Within Categories
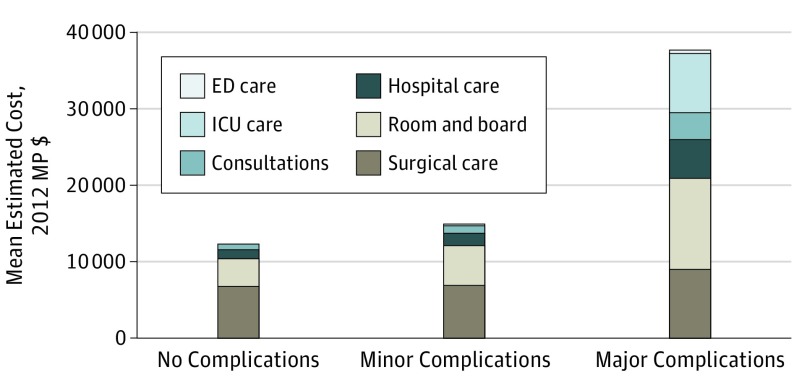
For the 51 patients (42.5%) without a postoperative complication, most of their estimated cost was owing to surgery (mean [SD] cost, MP $6830 [MP $1600]) and their initial hospitalization room and board (mean [SD] cost, MP $3620 [MP $1070]). Consultations from other services (mean [SD] cost, MP $750 [MP $950]) and the cost of other hospital services (median [SD] cost, MP $1110 [MP $340]) accounted for the remainder of their costs.
The total estimated cost of care in the 34 patients (28.3%) who experienced a major complication (mean [SD] cost, MP $37 700 [MP $28 090]) was substantially more than the total cost of care in patients who did not experience any complications (mean [SD] cost, MP $12 330 [MP $2500]) or those who experienced only minor complications (mean [SD] cost, MP $14 830 [MP $3470]), driven mostly by increases in supportive care for the patient. The small difference in the cost of surgical care between patients with major complications (mean [SD] cost, MP $8970 [MP $2750]) and those without complications (mean [SD] cost, MP $6830 [MP $1600]) reflects emergent reoperations. In contrast to the small increased cost of surgical care, there were large costs differences in the other categories of care across groups. Mean (SD) room and board costs increased from MP $3620 (MP $1070) for an uncomplicated gastrectomy to MP $11 940 (MP $8820) following a major complication, consultation costs increased from MP $750 (MP $950) to MP $3530 (MP $2410), and hospital care costs (medications, imaging, laboratory tests, and physical or occupation therapy) increased from MP $1110 (MP $340) to MP $5070 (MP $4690) (Table 2; Figure 3).
Figure 3. Categorized Estimated Costs in 2012 Medicare Proportional Dollars (MP $) Following Curative-Intent Total Gastrectomy by Complication Severity.
Minor complications: grades 1 and 2. Major complications: grades 3 through 5. ED indicates emergency department; ICU, intensive care unit.
Discussion
Postoperative complications were associated with substantial increases in the cost of total gastrectomy performed for stage I through III gastric adenocarcinoma. Experiencing a major postoperative complication was associated with a tripling in the cost of care, an increase that comes not only from a more expensive initial hospital stay but also from increased costs postdischarge. Costs following an uncomplicated total gastrectomy were primarily related to the surgery and room and board; most costs were incurred during the initial hospitalization (Table 2; Figure 2 and Figure 3). This is in stark contrast to costs following total gastrectomy with major complications; costs were more evenly divided between the different cost categories, and one-third of all costs were incurred following discharge, most of which occurred during readmission.
Although every complication resulted in incremental cost, patients who experienced multiple complications had substantially more expensive admissions than patients who did not experience a complication or experienced only 1 (Figure 1). Similarly, initial hospitalization costs do not differ substantially between patients without any complications and those who only experience minor complications, while patients who experience major complications have substantially more costly admissions (Table 2; Figure 2). This difference is caused by their increased length of stay (with a corresponding increase in the cost of hospital care and room and board) and also reflects the severity of their complication and the resources required to rescue those patients from mortality. Patients with major complications often require either intensive care unit care, endoscopic, or radiologic intervention; these services account for a substantial portion of the increased cost following major complications.
In this analysis, estimated hospital costs were analyzed instead of hospital charges or reimbursement because using itemized costs allows examination of the most granular cost information available. Costs are determined identically for all patients regardless of their insurance status or provider. In contrast, hospital reimbursement is significantly influenced by a patient’s insurance status and is nearly always bundled into amalgams of unrelated components of care, whether reimbursement is based on Diagnosis Related Groups or per diem rates. Had we used our own hospital costs, that would have created a different problem in that the underlying cost structure of a single institution may not be generalizable, even when use within categories is. Costs are also typically handled as proprietary data. To overcome these challenges, this analysis used a method described by Bochner et al. By normalizing estimated institutional costs to MP $ (without Medicare add-ons), we are able to present data that maintain the level of detail found in internal cost data that can easily be compared with normalized costs from other institutions.
Strengths and Limitations
Our study had limitations. One limitation of our study is that it represents a single institutional experience and only captures inpatient costs and costs incurred in our outpatient departments. Although no patients were lost to follow-up during our study period, there may have been some costs incurred outside our institution (ie, leakage) that we did not identify. We did not capture the cost of postdischarge rehabilitation, such as postdischarge acute or subacute rehabilitation facility admissions or postoperative visits with physical therapists, nor did we capture outpatient visiting nurse services. The use of these services following major surgery can be substantial. However, their omission was a conscious decision because we were interested in unveiling the root causes of increased hospital cost following complications. Additionally, it is known that services such as postdischarge rehabilitation, physical therapy, and home health nurses account for a small proportion of the total cost of postsurgical care compared with the cost of inpatient hospitalization.
To our knowledge, our method of determining costs and mapping them to representative Medicare reimbursement levels is novel and has several advantages compared with previously reported methods. Historically, medical costs are reported as either hospital reimbursement, hospital charges, or hospital costs. Hospital reimbursement is a direct representation of the cost of complications to a payer but is often not specific enough to determine the smaller components of that cost. Both hospital charges and hospital cost are much more granular than hospital reimbursement. However, hospital charges are not a direct representation of the hospital’s cost of care and also do not represent the payer’s cost because there are significant differences (the magnitude of which vary by payer and by institution and are unknown to the public) between what a hospital charges for care and what it receives. Hospital costs also vary significantly by hospital structure and geographic location.
By normalizing our internal costs to publically available Medicare reimbursement levels (which do not include Medicare add-ons), we have maintained the granularity available in internal accounting systems while also producing generalizable results. The method we used allows any institution (regardless of whether their actual costs are similar to ours) to compare the magnitude of cost differences between patients who experience postoperative complications and those who do not. In other words, we think that this is an early step toward understanding both components of “value”: clinical outcomes and the magnitude of cost associated with them.
Conclusions
This analysis reports detailed information on hospital costs following curative-intent total gastrectomy for gastric adenocarcinoma, a complex and potentially morbid surgical procedure. In an uncomplicated operation, most of the hospital cost is driven by the procedure and the subsequent hospitalization. Major complications triple the cost of care; increases in cost are driven by clinical resources used to treat patients’ complications and increased lengths of stay. Detailed cost analyses, such as this, can also be used as a mechanism to identify novel quality-improvement targets and to track the effectiveness of interventions on decreasing the frequency and severity of postoperative complications. Interventions that decrease the frequency or severity of complications will decrease the cost of care, as will strategies that prevent readmission following complications.
References
- 1.Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA Jr. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199(4):531-537. [DOI] [PubMed] [Google Scholar]
- 2.Hemmila MR, Jakubus JL, Maggio PM, et al. Real money: complications and hospital costs in trauma patients. Surgery. 2008;144(2):307-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khan NA, Quan H, Bugar JM, Lemaire JB, Brant R, Ghali WA. Association of postoperative complications with hospital costs and length of stay in a tertiary care center. J Gen Intern Med. 2006;21(2):177-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vonlanthen R, Slankamenac K, Breitenstein S, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg. 2011;254(6):907-913. [DOI] [PubMed] [Google Scholar]
- 5.Dimick JB, Pronovost PJ, Cowan JA, Lipsett PA. Complications and costs after high-risk surgery: where should we focus quality improvement initiatives? J Am Coll Surg. 2003;196(5):671-678. [DOI] [PubMed] [Google Scholar]
- 6.Enestvedt CK, Diggs BS, Cassera MA, Hammill C, Hansen PD, Wolf RF. Complications nearly double the cost of care after pancreaticoduodenectomy. Am J Surg. 2012;204(3):332-338. [DOI] [PubMed] [Google Scholar]
- 7.Regenbogen SE, Gust C, Birkmeyer JD. Hospital surgical volume and cost of inpatient surgery in the elderly. J Am Coll Surg. 2012;215(6):758-765. [DOI] [PubMed] [Google Scholar]
- 8.Nathan H, Atoria CL, Bach PB, Elkin EB. Hospital volume, complications, and cost of cancer surgery in the elderly. J Clin Oncol. 2015;33(1):107-114. [DOI] [PubMed] [Google Scholar]
- 9.Birkmeyer JD, Gust C, Dimick JB, Birkmeyer NJ, Skinner JS. Hospital quality and the cost of inpatient surgery in the United States. Ann Surg. 2012;255(1):1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Papenfuss WA, Kukar M, Oxenberg J, et al. Morbidity and mortality associated with gastrectomy for gastric cancer. Ann Surg Oncol. 2014;21(9):3008-3014. [DOI] [PubMed] [Google Scholar]
- 11.National Comprehensive Cancer Network NCCN clinical practice guideline in oncology: gastric cancer: version 1.2015. https://www.nccn.org/professionals/physician_gls/PDF/gastric.pdf. Accessed February 18, 2015.
- 12.Selby LV, Vertosick EA, Sjoberg DD, et al. Morbidity after total gastrectomy: analysis of 238 patients. J Am Coll Surg. 2015;220(5):863-871.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Strong VE, Selby LV, Sovel M, et al. Development and assessment of Memorial Sloan Kettering Cancer Center’s Surgical Secondary Events grading system. Ann Surg Oncol. 2015;22(4):1061-1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.US Government Accountability Office MEDICARE: legislative modifications have resulted in payment adjustments for most hospitals. http://www.gao.gov/products/GAO-13-334. Accessed March 1, 2015.
- 15.Center for Medicare and Medicaid Services Medicare data for the geographic variation public use file: a methodological overview. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Geographic-Variation/Downloads/Geo_Var_PUF_Methods_Paper.pdf. Accessed May 21, 2015.
- 16.Bochner BH, Dalbagni G, Sjoberg DD, et al. Comparing open radical cystectomy and robot-assisted laparoscopic radical cystectomy: a randomized clinical trial. Eur Urol. 2015;67(6):1042-1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Center for Medicare and Medicaid Services 1st Quarter 2012 values for hospital outpatient prospective payment system payment amounts (addendum B). http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Addendum-A-and-Addendum-B-Updates.html. Accessed September 18, 2014.