This study assesses whether a implementation of a hospital-driven improvement collaborative is associated with a reduction in acute asthma health care utilization in a population of Medicaid-insured pediatric patients.
Key Points
Question
Is implementation of a hospital-driven improvement collaborative associated with a reduction in acute asthma health care utilization in a population of Medicaid-insured pediatric patients?
Findings
In this study of Medicaid-insured pediatric patients with asthma from Hamilton County, Ohio, monthly asthma-related hospitalizations and emergency department visits decreased significantly with use of a hospital-driven improvement collaborative during a 5-year intervention period.
Meaning
An integrated, multilevel approach using quality improvement methods that extended from the hospital to the community was associated with improved asthma outcomes for a population of Medicaid-insured pediatric patients; similar models could be applied to other chronic conditions to improve outcomes and potentially reduce costs.
Abstract
Importance
Asthma is the most common chronic condition of childhood. Hospitalizations and emergency department (ED) visits for asthma are more frequently experienced by minority children and adolescents and those with low socioeconomic status.
Objective
To reduce asthma-related hospitalizations and ED visits for Medicaid-insured pediatric patients residing in Hamilton County, Ohio.
Design, Setting, and Participants
From January 1, 2010, through December 31, 2015, a multidisciplinary team used quality-improvement methods and the chronic care model to conduct interventions in inpatient, outpatient, and community settings in a large, urban academic pediatric hospital in Hamilton County, Ohio. Children and adolescents aged 2 to 17 years who resided in Hamilton County, had a diagnosis of asthma, and were Medicaid insured were studied.
Interventions
Interventions were implemented in 3 phases: hospital-based inpatient care redesign, outpatient-based care enhancements, and community-based supports. Plan-do-study-act cycles allowed for small-scale implementation of change concepts and rapid evaluation of how such tests affected processes and outcomes of interest.
Main Outcomes and Measures
The study measured asthma-related hospitalizations and ED visits per 10 000 Medicaid-insured pediatric patients. Data were measured monthly on a rolling 12-month mean basis. Data from multiple previous years were used to establish a baseline. Data were tracked with annotated control charts and with interrupted time-series analysis.
Results
Of the estimated 36 000 children and adolescents with asthma in Hamilton County (approximately 13 000 of whom are Medicaid insured and 6000 of whom are cared for in Cincinnati Children’s Hospital primary care practices), asthma-related hospitalizations decreased from 8.1 (95% CI, 7.7-8.5) to 4.7 (95% CI, 4.3-5.1) per 10 000 Medicaid patients per month by June 30, 2014, a 41.8% (95% CI, 41.7%-42.0%) relative reduction. Emergency department visits decreased from 21.5 (95% CI, 20.6-22.3) to 12.4 (95% CI, 11.5-13.2) per 10 000 Medicaid patients per month by June 30, 2014, a 42.4% (95% CI, 42.2%-42.6%) relative reduction. Improvements were sustained for the subsequent 12 months. The proportion of patients who were rehospitalized or had a return ED visit for asthma within 30 days of an index hospitalization was reduced from 12% to 7%. The proportion of patients with documented well-controlled asthma in this study’s primary care population increased from 48% to 54%.
Conclusions and Relevance
An integrated, multilevel approach focused on enhancing availability and accessibility of treatments, removing barriers to adherence, mitigating multidomain risks, augmenting self-management, and creating a collaborative relationship between the family and the health care system was associated with improved asthma outcomes for a population of Medicaid-insured pediatric patients. Similar models used in accountable care organizations or across patient panels and with other chronic conditions could be feasible and warrant evaluation.
Introduction
Pediatric asthma is a common, complex chronic condition. In 2010, asthma accounted for 14.2 million physician office visits and medical expenses of $50.1 billion per year. Hospitalizations and emergency department (ED) visits have historically been used to measure asthma morbidity. Risk factors for such potentially preventable health care use include minority race, low socioeconomic status, financial or social hardships, and living in a single-parent household. For example, minority children have hospitalization and ED visit rates 3 times greater than white children.
Successful long-term asthma management can be challenging; medications may be taken several times a day using complicated devices. Patients and caregivers may have difficulty comprehending instructions delivered during clinical care, complicating at-home implementation. Moreover, just 50% of patients keep appointments or fill prescriptions, perpetuating poor asthma control. Traditional care models do not adequately address underlying risk factors, propagating disparities and costly health care use. Within 12 months, approximately 40% of children and adolescents hospitalized for asthma are rehospitalized or revisit the ED.
Hamilton County, Ohio, the location of Cincinnati Children’s Hospital Medical Center (CCHMC), has more than 36 000 pediatric patients with asthma; more than 13 000 are Medicaid insured. With a global aim of improving the health of pediatric patients in the area, the CCHMC launched the Asthma Improvement Collaborative (AIC) in 2007; improvement efforts started in earnest in 2009. In 2010, the AIC was embedded within the CCHMC’s 2015 strategic plan, aiming to reduce asthma-related hospitalizations and ED visits for Medicaid-insured pediatric patients aged 2 to 17 years in Hamilton County by 20% by June 30, 2015. Specifically, the AIC sought to reduce the asthma-related hospitalization rate from a rolling 12-month mean of 7.2 to 5.8 per 10 000 patients per month and the ED visit rate from 20.9 to 16.7 per 10 000 patients per month.
Methods
Setting
From January 1, 2010, through December 31, 2015, a multidisciplinary team used quality improvement methods and the chronic care model to conduct interventions in inpatient, outpatient, and community settings in the CCHMC. The CCHMC is a 628-bed, urban pediatric academic center that cares for more than 90% of Hamilton County children and adolescents who require hospitalization and 65% or more of those seeking emergency care. The CCHMC general pediatric clinics provide primary care for approximately 34 000 Medicaid-insured children and adolescents, including those cared for at a primary care center opened during improvement efforts that increased to serve approximately 6000 pediatric patients. In addition, more than 7000 patients receive long-term asthma care in the CCHMC pulmonary or general pediatrics clinics each year. There are approximately 1000 hospitalizations and approximately 2500 ED visits annually for asthma for in-county children and adolescents. This project was reviewed by the CCHMC Institutional Review Board and deemed to be nonhuman subject research; therefore, informed consent was not required. Because this study used population-based data, no patient identifiers or patient-level data were used.
Planning the Study of the Intervention
The AIC was framed using the chronic care model and executed using quality improvement (QI) methods. The multidisciplinary improvement team consisted of hospitalist, primary care, and community pediatricians; pediatric pulmonologists and allergists; ED physicians; pediatric residents; social workers; respiratory therapists; nurses; care coordinators; pharmacists; project managers; QI consultants; and representatives from Medicaid managed care organizations and the Cincinnati Health Department school health program.
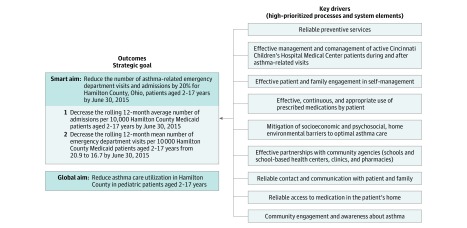
A key driver diagram was developed to frame elements believed to affect use by the target population (Figure 1). Interventions were implemented in and continued through 3 phases (hospital-based inpatient care redesign, outpatient-based care enhancements, and community-based supports and partnerships) and were tested using plan-do-study-act cycles.
Figure 1. Key Driver Diagram Used as Conceptual Framework Through Which Team Members Could Develop, Implement, and Evaluate Interventions.
Improvement Activities
Because current hospitalization predicts future hospitalization, phase 1 targeted redesign of inpatient processes for acute asthma management (Table and eTable in the Supplement). Hospitalization was recognized as a sentinel event, and focus was placed on identifying and mitigating relevant medical, social, and environmental risks. Interventions included the following:
Table. Intervention Timeline Used for the Interrupted Time-Series Analysis.
| Phase, Period | Intervention |
|---|---|
| Preintervention | |
| May 2008 | Medication-in-hand work began in primary asthma unit |
| January 2009 | Implemented metered-dose inhaler checklist in CCHMC primary care |
| May 2009 | Care coordination program started with single care coordinator |
| August 2009 | Use of standardized paper asthma history and physical examination form and paper CARAT-R testing in inpatient unit began |
| Phase 1 | |
| November 2009 | Use of home health pathway began |
| April 2010 | Medication-in-hand implemented in all inpatient units |
| September 2010 | CARAT-R implemented in inpatient units |
| December 2010 | External funding grant started |
| Phase 2 | |
| March 2011 | Intervention for low ACT scores in CCHMC primary care |
| May 2011 | Transition of primary care EHR from Logician to Epic; asthma history and physical examination form built and implemented in EHR |
| July 2011 | Medication home delivery program started for care coordination patients; Collaborating to Lessen Environmental Asthma Risks, an environmental health pathway and program began |
| August 2011 | Testing workflow related to receipt of regional alerts for admissions and ED visits from Health Information Exchange began |
| September 2011 | New electronic history and physical examination template and CARAT-R implemented |
| December 2011 | Outpatient clinic workflows for ACT scores completed in EHR |
| April 2012 | Web-based registry for CCHMC primary care implemented |
| October 2012 | ACT collected on tablet computer in largest primary care clinic |
| November 2012 | Care coordination program established at all CCHMC primary care sites |
| Phase 3 | |
| October 2013 | Collection of ACT scores from CPS began with support of Cincinnati Health Department nurses in pilot schools |
| November 2013 | EHR asthma registry launched for primary care and asthma specialists |
| March 2014 | EHR-based revisions to primary care asthma flow sheets |
| April 2014 | Asthma registry reports available to close gaps in care |
| May 2014 | Previsit planning tool live in EHR |
| August-September 2014 | Enterovirus D68 outbreak |
| August 2015 | All CPS school nurses granted read-only access to EHR |
| December 2015 | CPS and Cincinnati Health Department ACT process implemented across district |
Abbreviations: ACT, Asthma Control Test; CARAT-R, Childhood Asthma Risk Assessment Tool–Revised; CCHMC, Cincinnati Children’s Hospital Medical Center; CPS, Cincinnati public schools; ED, emergency department; EHR, electronic health record.
A medications-in-hand program that ensured that all patients received a 30-day supply of medications for use at home, an asthma action plan, and standardized inhaler training.
An asthma-specific history and physical examination form that prompted in-depth assessment of chronic asthma control, severity, and triggers.
Administration of an adapted Childhood Asthma Risk Assessment Tool–Revised (CARAT-R).
Decision support embedded in the electronic history and physical examination and CARAT-R that suggested consultation with pulmonary or allergy specialists if the diagnosis was in question, if symptoms were hard to treat, or for questions about optimal management. Similar prompts suggested referrals to social workers, environmental assessments by Cincinnati Health Department sanitarians, or a newly developed home health pathway.
A home health pathway consisting of up to 5 in-home nurse visits. Visits were tailored to families’ needs and included education on medications and trigger avoidance. Nurses also administered the Asthma Control Test (ACT), ensured that an asthma action plan and prescribed medications were in the home, reinforced proper device use, conducted informal environmental assessments, and supported needs related to self-management. Findings were shared with primary care practitioners.
Partnerships with Medicaid managed care organizations to support care transitions and leverage resources (medical equipment, transportation).
Because primary care access and continuity improve asthma outcomes, phase 2 focused on outpatient care processes (Table and eTable in the Supplement). Routine asthma visits were enhanced and standardized to focus on long-term control and acute exacerbation follow-up. Electronic health record (EHR)–based prompts facilitated determination of asthma control, severity, and triggers. Refined processes promoted families’ scheduling and keeping ambulatory asthma appointments. Interventions included the following:
Care coordination in the CCHMC primary care sites for children with 1 or more asthma-related hospitalizations and/or 2 or more ED visits in the preceding 12 months. Care coordinators, master’s-level social workers certified as asthma educators, applied an intervention bundle, including risk assessment, education, medication home delivery, collaboration with a Medicaid managed care practitioner, and improved access to community resources. Children graduated from care coordination if they had no hospitalizations or ED visits for 365 consecutive days after enrollment.
Standardized assessment of barriers to access, adherence, and environmental exposures with direct linkages to care modifications, including medication changes, referrals to subspecialists, and/or community-based resources (eg, medicolegal partnership).
Enhanced previsit screening, including use of a standardized metered-dose inhaler checklist, ACT, and EHR-based previsit planning tool.
Expanding the home health pathway to accept referrals from outpatient sources.
External funding in December 2010 allowed the CCHMC primary care practices to implement a web-based registry and improved alert system through the local health information exchange. Alerts notified practices of hospitalizations or ED visits by a patient at any regional hospital system. This registry was replaced in November 2013 by an EHR-embedded registry codeveloped by the CCHMC primary care and subspecialty practices to improve cross-divisional tracking.
Because asthma is influenced by community-based social determinants of health, phase 3 focused on enhancing connections between the CCHMC and community resources (Table and eTable in the Supplement). Interventions included the following:
Partnership with Cincinnati public schools and the Cincinnati Health Department School Nursing Program to deliver bundled asthma-related services, including ACT collection, protocols on how to access medication delivery services and home health pathway, and facilitated referrals to asthma subspecialists.
To build QI capacity within schools, 2 teams of school-based health staff completed a CCHMC-sponsored QI course. Teams worked on increasing rates of ACT completion (and sharing results with primary care physicians) and ensuring that students had completed asthma action plans on file at school. Successes were spread to additional schools, and more teams were enrolled in QI courses, first spreading to schools with high rates of asthma morbidity.
Read-only access to the CCHMC EHR system by school nurses was tested to improve communication of ACT scores, asthma action plans, primary care and subspecialty visits, and information on hospitalizations and ED visits.
Methods of Evaluation
Primary outcomes were the rates of asthma-related hospitalizations and ED visits by Medicaid-insured children and adolescents aged 2 to 17 years living in Hamilton County. The baseline period for primary outcome measures was defined as 2007 to 2009, the 3 years before the launch of the 2015 strategic plan. This period was chosen because accurate and complete data on enrollment from the state Medicaid office (denominators) only became available in 2007. Although tests of change began during the preintervention or baseline period, these interventions focused in the CCHMC on rehospitalizations and ED revisits (Table). Broader work targeting children and adolescents across Hamilton County commenced in 2010.
Hospitalization and ED data were obtained from hospital administrative databases and reported per 10 000 total Medicaid enrollees. Asthma-related visits were identified using International Classification of Diseases, Ninth Revision (ICD-9) codes: asthma as the primary diagnosis (493.**) or a specified set of respiratory diagnoses as primary diagnosis (034.**, 460.**-466.**, 472.**, 473.**, 475.**, 477.**- 493.**, 495.**, 496.**, 510.**-513.**, 786.**, and 995.**) with asthma as a secondary diagnosis.
Secondary outcomes were the percentage of patients with an asthma-related rehospitalization or ED revisit within 30 days of a hospital discharge and the percentage of CCHMC primary care patients with well-controlled asthma, defined as an ACT score greater than 19. Process measures were assessed using data collected at the point of care or extracted from the EHR daily, weekly, or monthly.
Changes over time were tracked on annotated run charts and statistical process control charts and displayed using Excel. When possible, standard industry criteria were used to distinguish random, common-cause variation from significant, special-cause changes attributable to the interventions. Primary statistical process control charts revealed a rolling 12-month mean for the rate of asthma-related hospitalizations and ED visits. We opted for this type of chart to blunt potential effects of seasonality. This approach, however, incorporated nonindependent historical data. Although each chart could depict what would look to be special cause (8 consecutive points above or below the established center line, 6 consecutive increasing or decreasing points, or points outside control limits), center lines could not be moved because of data autocorrelation.
To compensate for autocorrelation, we pursued a segmented regression analysis, modeling interrupted time-series data to draw conclusions about the effect across phases. A change in trend was defined as a change in the slope after the intervention (or phase) compared with before the intervention. To facilitate model development, interventions were grouped according to the timing of the 3 phases. Autoregressive models using the maximum likelihood method were built using SAS statistical software (SAS Institute Inc). The Durbin-Watson test for autocorrelation was performed on final regression models.
Because data were autocorrelated, conventional methods for estimating absolute change, relative change, and CIs would lead to biased results. Thus, predicted values were obtained from respective autoregressive models instead.
Two additional models were built to estimate the number of hospitalizations and ED visits avoided because of the interventions. To overcome the issue of overdispersion, a negative binomial regression model was built instead of a Poisson regression model. The preintervention trend and slope after each intervention phase were independent variables (eMethods in the Supplement).
Results
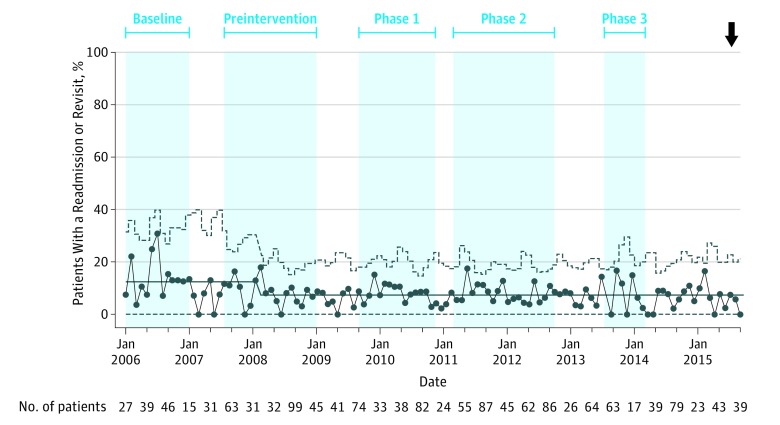
The study consisted of an estimated 36 000 children and adolescents with asthma in Hamilton County (approximately 13 000 of whom are Medicaid insured and 6000 of whom are cared for in primary care practices). Key process and outcome measures were tracked throughout each phase (Table and eFigures 1-6 in the Supplement). The main inpatient (phase 1) process measure was associated with the medications-in-hand intervention. The percentage of patients discharged with a 30-day supply of inhaled controller medications increased from 50% in May 2008 to 90% by May 2010 (eFigure 1 in the Supplement). The percentage of patients discharged with a short course of oral corticosteroids increased from 0% to 70% by March 2011 (eFigure 2 in the Supplement). The key secondary outcome, the 30-day rate at which hospitalized patients were rehospitalized or revisited the ED, decreased by 41% within 3 years of implementation of the inpatient care interventions, from 12% to 7% (Figure 2).
Figure 2. Proportion of Medicaid-Insured Patients From Hamilton County, Ohio, Who Had an Asthma-Related Hospital Readmission or Emergency Department Revisit Within 30 Days After the Index Hospital Admission for Asthma.
See the Table for interventions in each phase. The baseline period for this outcome was January 1, 2006, to May 1, 2008. Arrow indicates desired direction of change.
Outpatient processes (phase 2) focused on baseline asthma control of the CCHMC primary care patients. These processes included ensuring that ACT scores were collected and patients were provided asthma action plans (eFigure 3 and eFigure 4 in the Supplement). This phase also included our care coordination program. By the end of June 2015, a total of 763 patients with high-risk asthma had been enrolled in asthma care coordination and 394 had graduated; 345 were offered and received medication delivery. After implementation of phase 2 interventions, the percentage of primary care patients with well-controlled asthma increased from 48% to 54% (eFigure 5 in the Supplement).
In the community setting (phase 3), efforts focused on enhancing screenings and communication. By the end of the study period, more than 80% of Cincinnati public school students with asthma were screened using the ACT (eFigure 6 in the Supplement). Those with suboptimal scores, indicative of poorly controlled asthma, were referred to their existing or a new medical home.
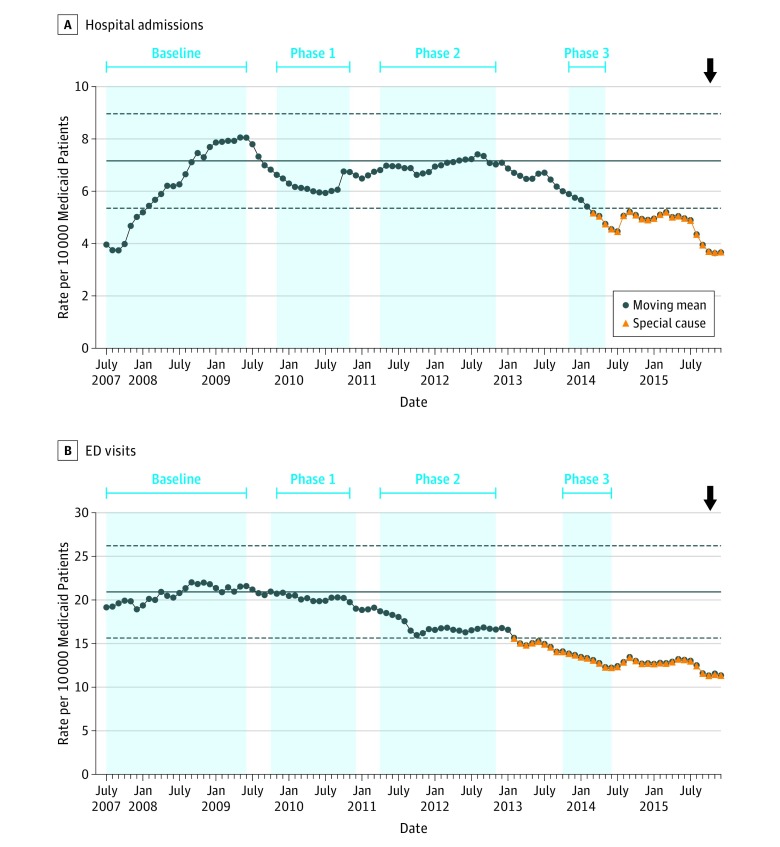
Our phased approach contributed to outcome improvement. Asthma-related hospitalizations decreased from 8.1 (95% CI, 7.7-8.5) to 4.7 (95% CI, 4.3-5.1) per 10 000 in-county Medicaid patients per month by June 30, 2014, a 41.8% (95% CI, 41.7%-42.0%) relative reduction (Figure 3). Asthma-related ED visits decreased from 21.5 (95% CI, 20.6-22.3) to 12.4 (95% CI, 11.5-13.2) per 10 000 in-county Medicaid patients per month, a 42.4% (95% CI, 42.2%-42.6%) relative reduction (Figure 3). The absolute decreases in the rolling 12-month mean (rate per 10 000 Medicaid enrollees) were 3.4 (95% CI, 3.3-3.5) for asthma-related hospitalizations and 9.1 (95% CI, 9.0-9.2) for ED visits. From the regression model, we estimate that during the last year of the project (2015), the improvements were associated with a reduction of 153 hospitalizations and 318 ED visits (eMethods in the Supplement). The improvement in health care utilization was sustained for the subsequent 12 months, apart from a transient increase in hospitalizations and ED visits coinciding with an enterovirus 68 outbreak in late summer to early fall of 2014.
Figure 3. Rolling 12-Month Means for Additional Asthma-Related Visits per 10 000 Medicaid-Insured Patients From Hamilton County, Ohio.
Patients were aged 2 through 17 years. The emergency department (ED) visits that resulted in hospitalization are not included in the hospital readmissions data. See the Table for interventions in each phase. The control limits (dashed lines) are based on data for the preintervention period (July 2007 through June 2009) using billing data. Conversion to International Statistical Classification of Diseases and Health-Related Problems, Tenth Revision coding occurred in October 2015. Arrow indicates desired direction of change.
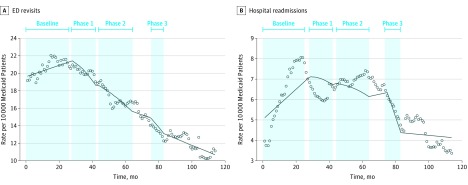
Interrupted time-series analyses confirmed these findings, revealing the change in slope for key outcome measures across all phases (Figure 4). For ED visit rates, a significant change occurred in postintervention slopes across all phases (Figure 4). Before the intervention, the slope was positive, implying an increase in ED visits. After implementation of interventions, for each phase and cumulatively after all phases, the slope significantly decreased, indicating a decrease in the number of ED visits. Findings were similar for hospitalization rates, with a significant change in slope after phase 3 (Figure 4). There was no autocorrelation in final regression models.
Figure 4. Interrupted Time-Series Analysis of Change in Additional Asthma-Related Visits Across the Intervention Phases.
See the Table for interventions in each phase. ED indicates emergency department.
Discussion
Implementation of an integrated, multilevel approach focused on enhancing availability and accessibility of treatments, removing barriers to adherence, mitigating risks related to adverse exposures, and augmenting self-management and collaborative relationships between the family and the health care system was associated with improved asthma outcomes. During the initiative, Medicaid-insured children had a more than 40% relative decrease in asthma-related hospitalizations and ED visits, whereas the number of 30-day return visits to the hospital or ED after an index hospitalization decreased by 41%. Thus, patient health improved and there was a potential reduction in cost, 2 critical arms of the Triple Aim Initiative.
We saw evidence of improvement across each phase. Although QI methods make it difficult to isolate the most influential intervention, we expect that certain interventions were particularly influential. Our first interventions targeted hospitalized pediatric patients because, at baseline, 12-month asthma rehospitalization rates at the CCHMC were approximately 20% and ED revisit rates were approximately 40%. Inpatient interventions shifted the focus to long-term management by identifying barriers to asthma control. Previous research has found that 38% to 70% of patients do not obtain prescribed medications at hospital discharge despite evidence that adherence to inhaled and oral corticosteroid treatment after acute exacerbations reduces the risk of additional acute asthma episodes. Having asthma controller and rescue medications and systemic corticosteroids in hand at discharge likely obviated a major barrier (getting to a neighborhood pharmacy) for the urban, indigent families in our study. Thus, we believe that providing a 30-day supply of all daily asthma medications at discharge was key to observed improvements.
Successful asthma management requires medical and nonmedical strategies that may be difficult for families to implement. Phases 2 and 3 applied and expanded inpatient-focused interventions to outpatient and community settings. Use of a care coordinator in primary care to facilitate deployment of an evidence-based care bundle led to reduced acute care service use by some of the highest-risk patients in our study. We believe that the bundle, which included in-depth risk assessment, directed education, medication delivery, and robust connections with hospital- and community-based partners, including schools, promoted lasting relationships with families and extended the reach of primary care.
To our knowledge, this is one of the largest population-based improvement efforts to successfully reduce asthma-related health care utilization by Medicaid-insured pediatric patients. Other investigators have found similar improvements in asthma symptoms and health care utilization with multidimensional interventions. However, most have used a randomized clinical trial design or have focused on small, select cohorts. We believe that using elements derived from the chronic care model to structure the framework and interventions was key to the success of our approach. Moreover, the QI frame with which interventions were developed and tested allowed for real-world, sustainable improvements to occur.
Our multidisciplinary, cross-divisional, community-inclusive team was bolstered by trusting relationships and a shared vision. We focused on supporting capacity building and skill acquisition among frontline hospital- and community-based health care professionals by using knowledge expansion and QI training that was practical and translatable to the workplace. Identifying neighborhoods with high rates of asthma hospitalizations helped the teams and community to understand and begin to tackle the problem. Sharing data across systems promoted communication, shared decision making, and improved health-condition management and prompted interventions that support risk assessment, population segmentation, and subsequent action. Focusing on transitions from hospital to primary care and to and from the community minimized lapses in continuity and provided more opportunities to intervene before crises occurred.
Limitations
Our study has some limitations. First, although the observed improvement could, in part, have been attributable to regression to the mean or reflect overall improvement in health across the studied community, this is unlikely given the long-term baseline data and evidence of sustained improvement. The most recent statewide data from the Ohio Hospital Association indicates that hospitalization rates for patients aged 5 to 14 years increased slightly and then stabilized from 2007 through 2009 (26.2 to 29.3 per 10 000 population). Moreover, national data indicate that hospitalization and ED visit rates for children were stable between 2001 and 2010; data beyond 2010 were not available nationally. More recent data, although limited, suggest continued stability during the subsequent years. In Ohio, pediatric patients covered through Medicaid had a stable rate of hospitalizations and ED visits between 2011 and 2015. California had a relatively flat rate of pediatric asthma hospitalizations between 2010 and 2014, whereas children in Missouri experienced an increase in acute asthma hospital visits between 2005 and 2014. Second, although the observed decrease in hospitalizations and ED visits in our study may have resulted in cost savings, a formal economic evaluation of this program was not conducted and would be needed to understand the actual economic effect. Third, because many interventions occurred simultaneously, we are unable to identify the individual benefit of any single change. Fourth, this project took place in 1 county; our findings and interventions may not be generalizable to other communities.
Conclusions
Children and adolescents with asthma experience considerable morbidity marked by persistent disparities. A multidisciplinary approach to improving family-centered care delivery may reduce the rate of health care utilization for high-risk patients. Our success has broad implications for management of asthma and other chronic conditions. Under evolving care provision and payment models, use of a multidisciplinary team approach to long-term disease management is feasible, with cost savings to potentially help sustain the program.
eTable. Intervention Details
eMethods. Analysis and Data Interpretation of Estimated Reduction in Emergency Department (ED) Visits and Hospitalizations in Last Year of Project (2015)
eFigure 1. Proportion of Patients Who Received a 30-Day Supply of Controller (Multidose) Medications at Hospital Discharge
eFigure 2. Proportion of Patients Who Received Oral Steroid Dose for Home Completion at Discharge
eFigure 3. Proportion of CCHMC Primary Care Patients Who Had an Asthma Control Test Completed
eFigure 4. Proportion of CCHMC Primary Care Patients Who Were Given an Asthma Action Plan
eFigure 5. Proportion of CCHMC Primary Care Patients Whose Asthma Was Rated as Well-Controlled (Asthma Control Test Score >19)
eFigure 6. Proportion of Asthma Control Test Scores Collected in Cincinnati Public Schools
References
- 1.Centers for Disease Control and Prevention Asthma facts—CDC's National Asthma Control Program grantees. July 2013. https://www.cdc.gov/asthma/pdfs/asthma_facts_program_grantees.pdf. Accessed February 20, 2017.
- 2.Beck AF, Huang B, Simmons JM, et al. . Role of financial and social hardships in asthma racial disparities. Pediatrics. 2014;133(3):431-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cincinnati Children’s, James M. Anderson Center for Health Systems Excellence 2005 Child Well-Being Survey. http://www.cincinnatichildrens.org/service/j/anderson-center/health-policy/well-being/. Accessed February 28, 2017.
- 4.Moorman JE, Akinbami LJ, Bailey CM, et al. . National surveillance of asthma: United States, 2001-2010. Vital Health Stat 3. 2012;(35):1-58. [PubMed] [Google Scholar]
- 5.Akinbami LJ, Moorman JE, Simon AE, Schoendorf KC. Trends in racial disparities for asthma outcomes among children 0 to 17 years, 2001-2010. J Allergy Clin Immunol. 2014;134(3):547-553.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akinbami LJ, Simon AE, Rossen LM. Changing trends in asthma prevalence among children. Pediatrics. 2016;137(1):e20152354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Makaryus AN, Friedman EA. Patients’ understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80(8):991-994. [DOI] [PubMed] [Google Scholar]
- 8.Maniaci MJ, Heckman MG, Dawson NL. Functional health literacy and understanding of medications at discharge. Mayo Clin Proc. 2008;83(5):554-558. [DOI] [PubMed] [Google Scholar]
- 9.Engel KG, Heisler M, Smith DM, Robinson CH, Forman JH, Ubel PA. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand? Ann Emerg Med. 2009;53(4):454-461. [DOI] [PubMed] [Google Scholar]
- 10.Riekert KA, Butz AM, Eggleston PA, Huss K, Winkelstein M, Rand CS. Caregiver-physician medication concordance and undertreatment of asthma among inner-city children. Pediatrics. 2003;111(3):e214-e220. [DOI] [PubMed] [Google Scholar]
- 11.Bloomberg GR, Trinkaus KM, Fisher EB Jr, Musick JR, Strunk RC. Hospital readmissions for childhood asthma: a 10-year metropolitan study. Am J Respir Crit Care Med. 2003;167(8):1068-1076. [DOI] [PubMed] [Google Scholar]
- 12.Database INSIGHT. [online database] Columbus: Ohio Hospital Association; 2009. [Google Scholar]
- 13.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775-1779. [DOI] [PubMed] [Google Scholar]
- 14.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. JAMA. 2002;288(15):1909-1914. [DOI] [PubMed] [Google Scholar]
- 15.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2-4. [PubMed] [Google Scholar]
- 16.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff (Millwood). 2001;20(6):64-78. [DOI] [PubMed] [Google Scholar]
- 17.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74(4):511-544. [PubMed] [Google Scholar]
- 18.Langley GJ, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. San Francisco, CA: Jossey-Bass; 1996. [Google Scholar]
- 19.Haselkorn T, Zeiger RS, Chipps BE, et al. . Recent asthma exacerbations predict future exacerbations in children with severe or difficult-to-treat asthma. J Allergy Clin Immunol. 2009;124(5):921-927. [DOI] [PubMed] [Google Scholar]
- 20.Teach SJ, Gergen PJ, Szefler SJ, et al. . Seasonal risk factors for asthma exacerbations among inner-city children. J Allergy Clin Immunol. 2015;135(6):1465-1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beck AF, Sauers HS, Kahn RS, Yau C, Weiser J, Simmons JM. Improved documentation and care planning with an asthma-specific history and physical. Hosp Pediatr. 2012;2(4):194-201. [DOI] [PubMed] [Google Scholar]
- 22.Mitchell H, Senturia Y, Gergen P, et al. . Design and methods of the National Cooperative Inner-City Asthma Study. Pediatr Pulmonol. 1997;24(4):237-252. [DOI] [PubMed] [Google Scholar]
- 23.Beck AF, Simmons JM, Sauers HS, et al. . Connecting at-risk inpatient asthmatics to a community-based program to reduce home environmental risks: care system redesign using quality improvement methods. Hosp Pediatr. 2013;3(4):326-334. [DOI] [PubMed] [Google Scholar]
- 24.Nathan RA, Sorkness CA, Kosinski M, et al. . Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113(1):59-65. [DOI] [PubMed] [Google Scholar]
- 25.The Office of the National Coordinator for Health Information Technology The Beacon Community Program. February 2012. https://www.healthit.gov/sites/default/files/beacon-communities-lessons-learned.pdf. Accessed February 20, 2017.
- 26.Trudnak T, Mansour M, Mandel K, et al. . A case study of pediatric asthma alerts from the beacon community program in cincinnati: technology is just the first step. EGEMS (Wash DC). 2014;2(1):1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amin SG. Control charts 101: a guide to health care applications. Qual Manag Health Care. 2001;9(3):1-27. [DOI] [PubMed] [Google Scholar]
- 28.Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12(6):458-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Provost LP, Murray SK. The Health Care Data Guide: Learning from Data for Improvement. San Francisco, CA: Jossey-Bass; 2011. [Google Scholar]
- 30.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299-309. [DOI] [PubMed] [Google Scholar]
- 31.SAS SAS/ETS User’s Guide, Version 6. 2nd ed Cary, NC: SAS Institute Inc; 1993. [Google Scholar]
- 32.Institute for Healthcare Improvement The Triple Aim Initiative. http://www.ihi.org/Engage/Initiatives/TripleAim/pages/default.aspx. Accessed February 28, 2017.
- 33.Cooper WO, Hickson GB. Corticosteroid prescription filling for children covered by Medicaid following an emergency department visit or a hospitalization for asthma. Arch Pediatr Adolesc Med. 2001;155(10):1111-1115. [DOI] [PubMed] [Google Scholar]
- 34.Herndon JB, Mattke S, Evans Cuellar A, Hong SY, Shenkman EA. Anti-inflammatory medication adherence, healthcare utilization and expenditures among Medicaid and children’s health insurance program enrollees with asthma. Pharmacoeconomics. 2012;30(5):397-412. [DOI] [PubMed] [Google Scholar]
- 35.Kenyon CC, Rubin DM, Zorc JJ, Mohamad Z, Faerber JA, Feudtner C. Childhood asthma hospital discharge medication fills and risk of subsequent readmission. J Pediatr. 2015;166(5):1121-1127. [DOI] [PubMed] [Google Scholar]
- 36.Camargo CA Jr, Ramachandran S, Ryskina KL, Lewis BE, Legorreta AP. Association between common asthma therapies and recurrent asthma exacerbations in children enrolled in a state Medicaid plan. Am J Health Syst Pharm. 2007;64(10):1054-1061. [DOI] [PubMed] [Google Scholar]
- 37.Williams LK, Peterson EL, Wells K, et al. . Quantifying the proportion of severe asthma exacerbations attributable to inhaled corticosteroid nonadherence. J Allergy Clin Immunol. 2011;128(6):1185-1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McCarthy D, Cohen A; The Cincinnati Children’s Hospital Medical Center’s Asthma Improvement Collaborative Enhancing Quality of Care. January 2013. http://www.commonwealthfund.org/publications/case-studies/2013/jan/cincinnati-childrens. Accessed February 28, 2017.
- 39.Bryant-Stephens T, Kurian C, Guo R, Zhao H. Impact of a household environmental intervention delivered by lay health workers on asthma symptom control in urban, disadvantaged children with asthma. Am J Public Health. 2009;99(suppl 3):S657-S665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Woods ER, Bhaumik U, Sommer SJ, et al. . Community asthma initiative: evaluation of a quality improvement program for comprehensive asthma care. Pediatrics. 2012;129(3):465-472. [DOI] [PubMed] [Google Scholar]
- 41.Beck AF, Moncrief T, Huang B, et al. . Inequalities in neighborhood child asthma admission rates and underlying community characteristics in one US county. J Pediatr. 2013;163(2):574-580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fingar K, Washington R.. Potentially Preventable Pediatric Hospital Inpatient Stays for Asthma and Diabetes, 2003-2012. Rockville, MD: Agency for Healthcare Research and Quality; February 2006 to June 2015. Healthcare Cost and Utilization Project Statistical Brief 192. [PubMed]
- 43.Ohio Department of Health Asthma Program The Burden of Asthma in Ohio. Columbus: Ohio Dept of Health Asthma Program; 2012. [Google Scholar]
- 44.Centers for Medicare & Medicaid Services Chronic conditions. January 18, 2017. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/CC_Main.html. Accessed April 26, 2017.
- 45.Kidsdata.org: A Program of Lucile Packard Foundation for Children's Health. Data by topic, asthma hospitalizations, by age group. April 2016. http://www.kidsdata.org/topic/239/asthma-hospitalizations/trend#fmt=2378&loc=2&tf=10,79&ch=788,789&pdist=7. Accessed April 26, 2017.
- 46.Reidhead M. Hospital utilization for pediatric asthma in Missouri. June 2015. https://www.mhanet.com/mhaimages/hidihealthstats/Asthma_HealthStats_0615.pdf. Accessed April 26, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Intervention Details
eMethods. Analysis and Data Interpretation of Estimated Reduction in Emergency Department (ED) Visits and Hospitalizations in Last Year of Project (2015)
eFigure 1. Proportion of Patients Who Received a 30-Day Supply of Controller (Multidose) Medications at Hospital Discharge
eFigure 2. Proportion of Patients Who Received Oral Steroid Dose for Home Completion at Discharge
eFigure 3. Proportion of CCHMC Primary Care Patients Who Had an Asthma Control Test Completed
eFigure 4. Proportion of CCHMC Primary Care Patients Who Were Given an Asthma Action Plan
eFigure 5. Proportion of CCHMC Primary Care Patients Whose Asthma Was Rated as Well-Controlled (Asthma Control Test Score >19)
eFigure 6. Proportion of Asthma Control Test Scores Collected in Cincinnati Public Schools