Key Points
Question
How does vaccine hesitancy affect annual measles cases and economic costs in the United States?
Findings
In this modeling study of children (age 2-11 years), a 5% reduction in measles, mumps, and rubella vaccination coverage resulted in a 3-fold increase in annual measles cases with an additional US$2.1 million in public sector costs.
Meaning
Even small declines in vaccination coverage in children owing to vaccine hesitancy may have substantial public health and economic consequences that will be larger when considering unvaccinated infants, adolescents, and adults.
Abstract
Importance
Routine childhood vaccination is declining in some regions of the United States due to vaccine hesitancy, which risks the resurgence of many infectious diseases with public health and economic consequences. There are ongoing policy debates on the state and national level, including legislation around nonmedical (personal-belief) exemptions for childhood vaccination and possibly a special government commission on vaccine safety, which may affect vaccine coverage.
Objective
To estimate the number of measles cases in US children and the associated economic costs under scenarios of different levels of vaccine hesitancy, using the case example of measles, mumps, and rubella (MMR) vaccination and measles.
Design, Setting, and Participants
Publicly available data from the US Centers for Disease Control and Prevention were used to simulate county-level MMR vaccination coverage in children (age 2-11 years) in the United States. A stochastic mathematical model was adapted for infectious disease transmission that estimated a distribution for outbreak size as it relates to vaccine coverage. Economic costs per measles case were obtained from the literature. The predicted effects of increasing the prevalence of vaccine hesitancy as well as the removal of nonmedical exemptions were estimated. The model was calibrated to annual measles cases in US children over recent years, and the model prediction was validated using an independent data set from England and Wales.
Main Outcomes and Measures
Annual measles cases in the United States and the associated public sector costs.
Results
A 5% decline in MMR vaccine coverage in the United States would result in an estimated 3-fold increase in measles cases for children aged 2 to 11 years nationally every year, with an additional $2.1 million in public sector costs. The numbers would be substantially higher if unvaccinated infants, adolescents, and adult populations were also considered. There was variation around these estimates due to the stochastic elements of measles importation and sensitivity of some model inputs, although the trend was robust.
Conclusions and Relevance
This analysis predicts that even minor reductions in childhood vaccination, driven by vaccine hesitancy (nonmedical and personal belief exemptions), will have substantial public health and economic consequences. The results support an urgent need to address vaccine hesitancy in policy dialogues at the state and national level, with consideration of removing personal belief exemptions of childhood vaccination.
This population-based modeling study estimates the public health consequences associated with reduction of childhood MMR vaccination resulting from parents’ vaccine hesitancy.
Introduction
The routine vaccination of children is declining in Texas and other areas of the United States where they allow for personal belief and other nonmedical exemptions to childhood vaccination requirements. In these areas, there is growing vaccine hesitancy—defined as a delay or refusal to accept vaccination based on personal beliefs despite availability—that could accelerate gaps in vaccine coverage across the United States. The determinants of the parental decision-making process on whether to vaccinate their child are complex and context specific, but are often influenced by misinformation, false claims regarding vaccine safety, and a low perceived risk of infectious diseases among other factors. While the sources driving vaccine hesitancy (eg, the “anti-vaxxer” movement, celebrity endorsement, and online content) have historically been outside of science and government, there have recently been calls for a special government commission on vaccine safety, despite overwhelming scientific consensus on the safety and effectiveness of vaccinations. If the panel were to draft policies that relax childhood vaccinations requirements, the already declining trends in vaccination coverage in US children may decline further. The aim of this study was to estimate the potential public health and economic consequences of declining childhood vaccination, a result of a growing vaccine hesitancy movement, using the case example of measles, mumps, and rubella (MMR) vaccination and measles virus.
Methods
Data Source
We used publicly available data from the US Centers for Disease Control and Prevention (CDC) to simulate county-level MMR vaccine coverage for children aged 2 to 11 years in the United States for the present day. For primary school children (kindergarten to fifth grade; age 5-11 years), we used state-level data from SchoolVaxView from 2010 to 2015. For younger children (age 2-5 years), we used state-level data from ChildVaxView from 2013 to 2015. These age groups were chosen based on availability of data, role in transmission, and strength of social mixing patterns. To simulate county-level vaccine coverage, we used the most recent publicly available data for 257 counties in the United States from the CDC (2007-2008 survey) to compute state-specific variance for MMR vaccine coverage. These counties were chosen as a subset of the estimated 3141 counties in the United States, based on their sufficient reporting during the National Immunization Survey, and provide a sampling of multiple counties per state. We then applied the state-specific variances to current state-level coverage estimates to simulate counties in the United States, assuming coverage was normally distributed. The simulation of county-level coverage estimates is important because of the heterogeneity in vaccine coverage and the corresponding implication to outbreaks in highly immunized populations. Although historical, our county-level variances estimates are likely to be conservative since variance is expected to have increased over time given focal regions of vaccine hesitancy. When vaccine coverage data were unavailable, we used the mean of neighboring years. Data on the state-level prevalence of vaccine hesitancy, defined as nonmedical (eg, personal belief) exemptions of childhood vaccination, were sourced from the CDC SchoolVaxView.
We estimated a cost (2016 US$) of $20 000 per case of measles from the perspective of the public sector (ie, local and state public health institutions) based on the literature. These costs included state and local expenses to the public sector, including personnel wages and salaries, contact tracing, transportation, laboratory analysis, vaccination, overhead, and other costs. These estimates did not account for costs of illness, loss productivity to the parent, hospitalization (common in the prevaccine era), or other societal aspects, and our base case cost may represent a conservative estimate.
This study was not human subject research as determined by the Stanford University School of Medicine Institutional Review Board.
Statistical Analysis
We estimated the annual number of measles cases in the United States and the associated public sector costs under increasing levels of vaccine hesitancy. We modeled a measles outbreak following 2 chance events. First, we simulated importation of measles cases into US counties (often a US traveler returning from an endemic country) with the possibility for multiple introductions within the same county. We used a calibrated number of individuals with imported measles interacting with children in the United States, which can be thought of as a static force of infection. We weighted the probability of introduction by the state’s population, where more populated states had a higher probability of receiving an imported measles case (eMethods in the Supplement).
Second, in scenarios where an imported measles case was successfully introduced in a county with contact of a child, we simulated the ensuing size of the outbreak. We adapted a stochastic mathematical model that estimated a probability distribution for the size of a measles outbreak following introduction of an imported case as it relates to vaccine coverage in a population (eMethods in the Supplement). The model implemented a simple random walk, which is a mathematical approach to simulating a series of random events (ie, interaction of children and subsequent transmission of an infectious disease). In this model, we computed the probability of an infectious child transmitting the virus to another child based on the effective reproductive number, which is the mean number of secondary cases caused by 1 infectious person in a population with some level of immunity (eMethods in the Supplement). We computed the effective reproductive number as a simple function of both the calibrated basic reproductive number (R0) for measles and the proportion of children who are immune (accounting for both county-level vaccine coverage and imperfect vaccine efficacy). The model assumed that the outbreak is small relative to the entire population (ie, no population-wide outbreaks) and the overall proportion of susceptible individuals will not be significantly changed with respect to the effective reproductive number (eMethods in the Supplement). This assumption is supported by disease surveillance data from developed countries with high vaccine coverage.
We simulated increasing vaccine hesitancy (ie, nonmedical exemptions) to estimate the predicted effect of declining childhood vaccination coverage in the study population on measles outbreaks. We simulated hypothetical reductions in vaccination coverage in the entire study population of children aged 2 to 11 years and computed measles outbreaks over the time horizon of 1 year following traditional reporting of annual case counts. We estimated the predicted effect of reducing mean vaccine coverage for each state by 1% to 8%, which represented a corresponding increase in the prevalence of nonmedical exemptions across the entire study population. This percentage change in vaccine hesitancy was atop the current 2% national prevalence of nonmedical exemptions. Using CDC data on current state-level estimates for nonmedical exemptions, we also quantified the predicted effect of removing nonmedical exemptions for children. Removal of all nonmedical exemptions equated with estimated national vaccine coverage of only 95% in eligible children; this gap in coverage was likely due to children who are not required to follow school vaccination policy (eg, home schooling). There was a small subset of children who were ineligible owing to medical exemptions (eg, immunocompromised, receiving chemotherapy; <0.1% of the population), and these children were modeled as fully susceptible. The data and model code are available online.
Calibration and Validation
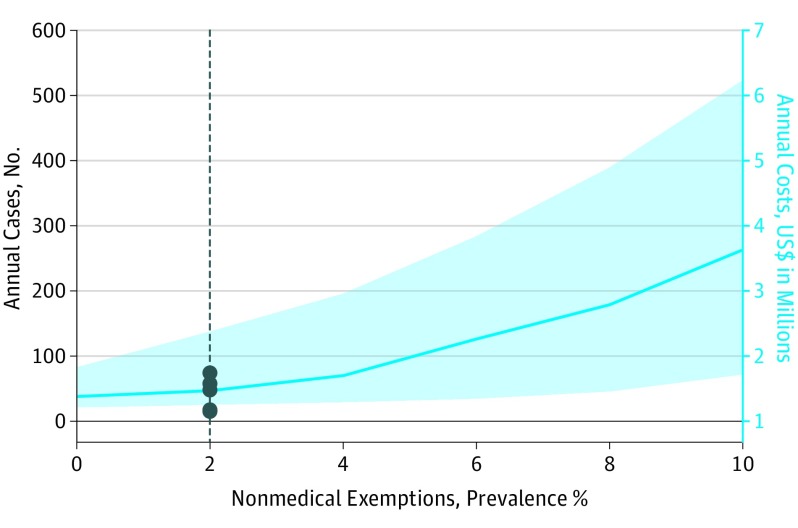
We calibrated the model to annual measles cases in US children in recent years and fitted 2 model parameters: the R0 for measles (for the study population of children age 2-11 years) and number of imported measles cases with successful contact of a child (eMethods in the Supplement). We calibrated the median model output to annual measles cases in children (age 2-11 years) from recent years (an estimated 48 cases annually) (Table 1) and number of outbreaks in this group (4 based on CDC definition of a transmission chain of ≥3) in the United States. The stochastic mathematical model reproduced the observed data and provided a 90% prediction interval that captured the wide range of recent measles case counts in children (Figure).
Table 1. Model Variables for Measles Epidemiology, Vaccination, and Public Sector Costs.
| Variable | Base Case Value | Comments |
|---|---|---|
| Fixed model parameters | ||
| Estimated annual cases in US children in recent years | 48 | 28% Total cases were in ages 2-11 y |
| Estimated annual No. of outbreaks in US children (≥3 cases) | 4 | |
| MMR efficacy for measles, % | 95 | Assume some with 2 doses |
| Cost per measles case, $ | 20 000 | |
| Fitted model parameters | ||
| Basic R0, measles in children | 5.7a | |
| No. of measles importations in US children | 16b |
Abbreviations: CDC, Centers for Disease Control and Prevention; MMR, measles, mumps, and rubella; R0, reproductive number.
The model accounts for transmission among children who represent approximately 30% of the cases.
The CDC estimates approximately 35 cases of imported measles per year, which broadly aligns with our findings because children account for approximately 30% of the cases.
Figure. Public Health Consequences and Public Sector Costs of Childhood Measles in the United States With Increasing Prevalence of Vaccine Hesitancy.
The line indicates the predicted number of annual measles cases in US children (ages 2-11 years) and the associated public sector costs across a range of prevalences for vaccine hesitancy (ie, nonmedical exemptions). The shaded area provides the 90% prediction interval. The vertical dashed line indicates the predicted annual measles cases in children for present day (2% prevalence of vaccine hesitancy). The datapoints represent the observed number of annual cases in recent years. We estimated the consequence of increasing national nonmedical exemptions from 2% to 10% prevalence, and the removal of nonmedical exemptions (0% prevalence).
We validated the model prediction using an independent data set on national MMR vaccine coverage and annual measles cases from England and Wales (eMethods in the Supplement). Most notably, this data set allowed for characterization of the model validity across the broad range of vaccine coverage and across the range of vaccine coverage evaluated in the main analysis in a highly immunized population comparable to that of the United States.
Sensitivity Analysis
We conducted a series of 1-way sensitivity analyses to measure the influence of varying individual model parameters on the overall study outcomes to assess the robustness of our findings. We evaluated a range of alternative values around the calibrated parameters, including the R0 for measles and number of imported measles cases in, and also the per-case public sector cost of a measles case, and other model assumptions (Table 2). We examined modeling an expanded age group (0-11 years) that added children 0 to 2 years (eMethods in the Supplement). While the mixing structure in this group is more complex than our primary study population, we evaluated this alternative age specification to understand the robustness of study conclusions. We also modeled a slow phase-in of vaccine hesitancy in the youngest age group alone over a 10-year period (eMethods in the Supplement).
Table 2. One-Way Sensitivity Analysis of Measles Cases and Public Sector Costs.
| Description | Base Case | Range of Values | Outcome With 5% Decline in Vaccine Coverage, Range |
|---|---|---|---|
| No. of Cases (fold increase) | |||
| Measles cases | |||
| Base case | 3.1 | ||
| Basic R0 | 5.7 | 5-8 | 2.2-4.5 |
| No. of measles importations in US children | 16 | 10-25 | 1.5-4.0 |
| Expanded age group, range, y | 2-11 | 0-11a | 2.7 |
| Additional Cost, US$ million | |||
| Public sector costs | |||
| Base case | 2.1 | ||
| Basic R0 | 5.7 | 5-8 | 1.2-3.2 |
| No. of measles importations in US children | 16 | 10-25 | 0.5-2.7 |
| Per-case cost, US$ | 20 000 | 5000-30 000 | 0.5-3.1 |
| Expanded age group, y | 2-11 | 0-11a | 2.5 |
Abbreviation: R0, reproductive number.
Only the age group 0 to 11 years was tested in the analysis; thus, there is no range for the outcomes.
Results
For the United States, the baseline national coverage for MMR vaccination in children aged 2 to 11 years was 93% prevalence (state variation, 87%-97%), and nonmedical exemptions were a 2% prevalence (state variation, 0.4%-6.2%). We estimated an R0 for measles of 5.7 for transmission within US children (age 2-11 years), with 48 annual measles cases under current vaccine coverage estimates. Reduction in MMR vaccine coverage due to increasing vaccine hesitancy increased the annual measles incidence and associated economic costs (Figure).
We found that a 5% decline in MMR vaccine coverage in US children would result in a 3-fold increase in national measles cases in this age group, for a total of 150 cases and an additional $2.1 million in economic costs to the public sector (Figure). With declining vaccination coverage, the size of outbreaks increased. Increased MMR vaccine coverage in children, through elimination of children with nonmedical exemptions or other mechanisms, increased national MMR coverage to 95% prevalence (state variation, 91%-98%). We predicted that this strategy would reduce annual cases of measles by 20% (from 48 to 38 cases) and was an effective strategy to mitigate annual measles cases and costs.
For validation, we used independent data from England and Wales and found that the model prediction for rise in measles incidence with declining vaccine coverage correlated well with the observed data within the constraints of the stochastic nature of measles outbreaks and wide prediction intervals (eMethods and eTable 1 in the Supplement).
There was variation around these estimates due to the stochastic elements of measles importation, although the relationship between declining MMR vaccine coverage and increasing measles cases was robust and model assumptions were conservative. The 1-way sensitivity analyses found that varying individual model parameters, including the R0 (from R0 5-8), public sector costs per measles case (from US$5000-US$30 000), and expanded age groups (0-11 years), resulted in a range of values for increases in measles cases and economic costs associated with a 5% reduction in MMR vaccine coverage (Table 2, eFigure in the Supplement). We also evaluated a slow phase-in of a 5% reduction in MMR vaccine coverage in the youngest age group over 10 years and found a 2-fold increase in total measles cases, with an additional 480 cases costing $7.9 million over this period. Overall, the study conclusion that minor reductions in vaccine coverage resulted in multifold increases in measles cases with large public sector costs remained robust in most cases.
Discussion
In this study, we estimated the public health and economic consequences of increasing vaccine hesitancy based on nonmedical and personal-belief exemptions on childhood measles in the United States. We found that even a modest 5% decline in MMR vaccine coverage could result in a 3-fold increase in annual measles cases, with an additional US$2.1 million in economic costs in children aged 2 to 11 years. These estimates would be substantially higher if unvaccinated infants, adolescents, and adult populations are also considered. We predict that removal of nonmedical (eg, personal belief) vaccine exemptions for childhood vaccination will mitigate this trend and substantially reduce measles and other infectious diseases in the United States.
Vaccine hesitancy in the United States and globally has historically reflected a number of complex and context-specific determinants that are often vaccine specific. In the case of MMR vaccination in the United States, parental refusal to vaccinate their child may be largely influenced by misinformation on vaccine safety and the low perceived risk of measles in the United States. Our study conclusions find that measles still poses a substantial threat for large outbreaks in children, despite public perception that measles is no longer a risk to children in the United States, especially under scenarios with further decline in vaccine coverage. Furthermore, the safety of MMR and other vaccines is well established in the scientific literature, including the finding that MMR vaccination has no association with the development of autism.
The recent declines in vaccine coverage in the United States are increasingly driven by parental nonmedical exemptions of vaccine recommendations. Presently, 18 states allow for nonmedical personal belief exemptions to childhood vaccination. In addition, all but 2 states offer nonmedical exemption on religious or philosophical grounds. Given trends in declining vaccine coverage, our study predicts that removal of nonmedical personal belief exemptions would substantially reduce the risk of measles in the United States. This conclusion is further supported by a recent study that examined the association between vaccine coverage and measles outbreaks in Denver, Colorado, and found that a reduction in nonmedical exemptions through stricter policy would reduce measles cases and economic consequences.
Measles is a highly infectious viral illness that requires high vaccine coverage (>90%-95%) to achieve herd immunity and prevent large outbreaks, based on an estimated 95% vaccine efficacy. The current empirical data on state-level vaccine coverage suggest that many settings are on the border of the desired threshold for herd immunity. Substantial within-state variation means that there are likely “hot spots” where vaccine coverage is especially low compared with the state average and outbreaks will be large following importation of a measles case (commonly from a returning US citizen after traveling internationally). This geographic clustering of low vaccine coverage (hot spot) and outbreaks in the United States is supported by data on low diphtheria, tetanus, and acellular pertussis vaccine coverage and outbreaks of pertussis, which provides further evidence for the study conclusions.
The mechanism of measles outbreaks in the United States, which are driven by importation of cases from outside the country, is a stochastic process with substantial variation around the number of annual cases. This variation can be readily seen in recent annual case counts for measles in the United States, ranging from 55 to 667 annual cases across all age groups in recent years, across a time period with relatively similar vaccine coverage (eTable 2 in the Supplement). The wide range of annual measles cases from recent years is captured in our model through the large prediction interval for present-day vaccine coverage (Figure; see present-day prevalence of 2% vaccine hesitancy). Beyond the stochastic nature of measles importation and outbreaks, the model prediction was sensitive to some input parameters that may be heterogeneous between settings, but the overall conclusion remained robust. We validated our model with independent data from England and Wales over a similar vaccine coverage range, which increases our confidence in the model trend prediction. Furthermore, the historical data from England and Wales found a comparable relation between declining vaccine coverage and a rise in measles cases.
This modeling analysis likely predicts a conservative estimate for a rise in measles cases associated with declining immunization status because of foundational model assumptions and since we limited our analysis to US children (age 2-11 years). The model is designed to simulate outbreaks in highly immunized population and nonendemic settings. However, large reductions in MMR vaccine coverage could allow for measles to become endemic again, which is not accounted for in this model, and would likely result in thousands of annual measles cases. Owing to constraints on data for immunization status in the adult population and social mixing structures, we limited our analysis to children ages 2-11 years who contribute approximately 30% of the annual measles cases. However, the number of cases of measles would be much larger when accounting for other age groups, such as infants, adolescents, and adults. This increased number would be, in part, driven by infants younger than 12 months who are not yet eligible to receive measles vaccines, as illustrated in the sensitivity analysis modeling an expanded age group (0-11 years). Finally, the upper limit of the prediction interval in the base case analysis (Figure) demonstrated substantial nonlinearity, suggesting the possibility for large outbreaks due to random chance with small reductions in vaccine coverage.
Limitations
The study findings should be understood within the limitation of the model assumptions and data. We simulated county-level differences in vaccine coverage and assumed homogeneous mixing of children within this ecologic zone, although there are important spatial and age-based heterogeneities in measles transmission that were not accounted for in the model owing to limitations in data. We estimated an R0 for measles of 5.7, which is lower than historically estimated values of 10 to 18, although we only modeled children who account for approximately 30% of the cases, so the R0 is intuitively lower since we did not include transmission with adolescents and adults (reducing the population for transmission). Although our estimate aligns with outbreaks in school children, we caution against overinterpretation of this R0 value that may be underestimated because of the ecologic nature of the estimate. Finally, there are key limitations in CDC data for vaccination coverage, including variation in reporting standards from individual states and that vaccine exemption estimates may include children who were partially vaccinated.
Conclusions
The results of our study find substantial public health and economic consequences with even minor reductions in MMR coverage due to vaccine hesitancy and directly confront the notion that measles is no longer a threat in the United States. Removal of the nonmedical personal belief exemptions for childhood vaccination may mitigate these consequences. These findings should play a key role in any policies adapted by state or national governments that relate to childhood vaccination.
eMethods. Additional Description of the Methodology
eTable 1. Model Calibration in United States and Validation in England and Wales
eTable 2. Number of Annual Measles Cases in the United States for the Overall Population and Children
eFigure. Public Health Impact and Public Sector Costs of Childhood Measles in the United States With Increasing Prevalence of Vaccine Hesitancy in Expanded Age Group (Ages 0-11 Years)
References
- 1.Hotez PJ. Texas and its measles epidemics. PLoS Med. 2016;13(10):e1002153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Conference of State Legislatures. States with religious and philosophical exemptions from school immunization requirements http://www.ncsl.org/research/health/school-immunization-exemption-state-laws.aspx. Published August 23, 2016. Accessed February 6, 2017.
- 3.VaxView. United States Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/vaxview/. Accessed February 6, 2017.
- 4.Omer SB, Enger KS, Moulton LH, Halsey NA, Stokley S, Salmon DA. Geographic clustering of nonmedical exemptions to school immunization requirements and associations with geographic clustering of pertussis. Am J Epidemiol. 2008;168(12):1389-1396. [DOI] [PubMed] [Google Scholar]
- 5.Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. 2014;32(19):2150-2159. [DOI] [PubMed] [Google Scholar]
- 6.Report of the SAGE Working Group on Vaccine Hesitancy. World Health Organization. http://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf. Published October 1, 2014. Accessed June 12, 2017.
- 7.American Academy of Pediatrics. Vaccine safety : examine the evidence. https://www.aap.org/en-us/Documents/immunization_vaccine_studies.pdf. Updated April 2013. Accessed March 25, 2017.
- 8.Jain A, Marshall J, Buikema A, Bancroft T, Kelly JP, Newschaffer CJ. Autism occurrence by MMR vaccine status among US children with older siblings with and without autism. JAMA. 2015;313(15):1534-1540. [DOI] [PubMed] [Google Scholar]
- 9.Taylor LE, Swerdfeger AL, Eslick GD. Vaccines are not associated with autism: an evidence-based meta-analysis of case-control and cohort studies. Vaccine. 2014;32(29):3623-3629. [DOI] [PubMed] [Google Scholar]
- 10.Uno Y, Uchiyama T, Kurosawa M, Aleksic B, Ozaki N. Early exposure to the combined measles-mumps-rubella vaccine and thimerosal-containing vaccines and risk of autism spectrum disorder. Vaccine. 2015;33(21):2511-2516. [DOI] [PubMed] [Google Scholar]
- 11.Smith PJ, Singleton JA; National Center for Immunization and Respiratory Diseases; Centers for Disease Control and Prevention (CDC) . County-level trends in vaccination coverage among children aged 19-35 months—United States, 1995-2008. MMWR CDC Surveill Summ. 2011;60(4):1-86. [PubMed] [Google Scholar]
- 12.Keeling MJ, Rohani P. Modeling Infectious Diseases in Humans and Animals. Princeton, NJ: Princeton University Press; 2008. [Google Scholar]
- 13.Glasser JW, Feng Z, Omer SB, Smith PJ, Rodewald LE. The effect of heterogeneity in uptake of the measles, mumps, and rubella vaccine on the potential for outbreaks of measles: a modelling study. Lancet Infect Dis. 2016;16(5):599-605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atwell JE, Van Otterloo J, Zipprich J, et al. . Nonmedical vaccine exemptions and pertussis in California, 2010. Pediatrics. 2013;132(4):624-630. [DOI] [PubMed] [Google Scholar]
- 15.Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med. 2009;360(19):1981-1988. [DOI] [PubMed] [Google Scholar]
- 16.Ortega-Sanchez IR, Vijayaraghavan M, Barskey AE, Wallace GS. The economic burden of sixteen measles outbreaks on United States public health departments in 2011. Vaccine. 2014;32(11):1311-1317. [DOI] [PubMed] [Google Scholar]
- 17.Sugerman DE, Barskey AE, Delea MG, et al. . Measles outbreak in a highly vaccinated population, San Diego, 2008: role of the intentionally undervaccinated. Pediatrics. 2010;125(4):747-755. [DOI] [PubMed] [Google Scholar]
- 18.Orenstein WA, Papania MJ, Wharton ME. Measles elimination in the United States. J Infect Dis. 2004;189(suppl 1):S1-S3. [DOI] [PubMed] [Google Scholar]
- 19.Strebel PM, Papania MJ, Fiebelkorn AP, Halsey NA Measles vaccine. In: Plotkin SA, Orenstein WA, Offit PA. Vaccines. 6th ed. New York: Elsevier Saunders; 2013:352-387. [Google Scholar]
- 20.Jansen VA, Stollenwerk N, Jensen HJ, Ramsay ME, Edmunds WJ, Rhodes CJ. Measles outbreaks in a population with declining vaccine uptake. Science. 2003;301(5634):804. [DOI] [PubMed] [Google Scholar]
- 21.Yap P, Wu FW, Du ZW, et al. . Effect of deworming on physical fitness of school-aged children in Yunnan, China: a double-blind, randomized, placebo-controlled trial. PLoS Negl Trop Dis. 2014;8(7):e2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Measles cases and outbreaks: 2010-2015. https://www.cdc.gov/measles/cases-outbreaks.html. Updated June 2, 2017. Accessed June 12, 2017.
- 23.Lo N. Publication codes. https://github.com/NathanLo3/Publication-codes. May 2017. Accessed June 19, 2017.
- 24.Parker AA, Staggs W, Dayan GH, et al. . Implications of a 2005 measles outbreak in Indiana for sustained elimination of measles in the United States. N Engl J Med. 2006;355(5):447-455. [DOI] [PubMed] [Google Scholar]
- 25.Whittington MD, Kempe A, Dempsey A, Herlihy R, Campbell JD. Impact of nonmedical vaccine exemption policies on the health and economic burden of measles. Acad Pediatr. 2017;S1876-2859(17)30068-2. [DOI] [PubMed] [Google Scholar]
- 26.Durrheim DN, Crowcroft NS, Strebel PM. Measles—the epidemiology of elimination. Vaccine. 2014;32(51):6880-6883. [DOI] [PubMed] [Google Scholar]
- 27.Wallinga J, Heijne JC, Kretzschmar M. A measles epidemic threshold in a highly vaccinated population. PLoS Med. 2005;2(11):e316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mossong J, Muller CP. Estimation of the basic reproduction number of measles during an outbreak in a partially vaccinated population. Epidemiol Infect. 2000;124(2):273-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Additional Description of the Methodology
eTable 1. Model Calibration in United States and Validation in England and Wales
eTable 2. Number of Annual Measles Cases in the United States for the Overall Population and Children
eFigure. Public Health Impact and Public Sector Costs of Childhood Measles in the United States With Increasing Prevalence of Vaccine Hesitancy in Expanded Age Group (Ages 0-11 Years)