Key Points
Question
What are the variables that contribute to interhospital cost variation in autologous free flap breast reconstruction?
Findings
In this nationwide, population-based secondary cross-sectional analysis that included 3302 women who underwent autologous free flap breast reconstruction in the United States, high-volume hospitals were more costly but had fewer complications. Compared with the Northeast, the West used more hospital resources, with longer length of stay, despite having patients with lower preoperative risk factors and similar complication rates.
Meaning
Further investigation is needed to uncover cost drivers for autologous free flap breast reconstruction; expedited discharge of patients with low preoperative risk factors may be an avenue to decrease expenditure, without compromising outcomes.
Abstract
Importance
Cost variation among hospitals has been demonstrated for surgical procedures. Uncovering these differences has helped guide measures taken to reduce health care spending. To date, the fiscal consequence of hospital variation for autologous free flap breast reconstruction is unknown.
Objective
To investigate factors that influence cost variation for autologous free flap breast reconstruction.
Design, Setting, and Participants
A secondary cross-sectional analysis was performed using the Healthcare Cost and Utilization Project National Inpatient Sample database from 2008 to 2010. The dates of analysis were September 2016 to February 2017. The setting was a stratified sample of all US community hospitals. Participants were female patients who were diagnosed as having breast cancer or were at high risk for breast cancer and underwent autologous free flap breast reconstruction.
Main Outcomes and Measures
Variables of interest included demographic data, hospital characteristics, length of stay, complications (surgical and systemic), and inpatient cost. The study used univariate and generalized linear mixed models to examine associations between patient and hospital characteristics and cost.
Results
A total of 3302 patients were included in the study, with a median age of 50 years (interquartile range, 44-57 years). The mean cost for autologous free flap breast reconstruction was $22 677 (interquartile range, $14 907-$33 391). Flap reconstructions performed at high-volume hospitals were significantly more costly than those performed at low-volume hospitals ($24 360 vs $18 918, P < .001). Logistic regression demonstrated that hospital volume correlated with increased cost (Exp[β], 1.06; 95% CI, 1.02-1.11; P = .003). Fewer surgical complications (16.4% [169 of 1029] vs 23.7% [278 of 1174], P < .001) and systemic complications (24.2% [249 of 1029] vs 31.2% [366 of 1174], P < .001) were experienced in high-volume hospitals compared with low-volume hospitals. Flap procedures performed in the West were the most expensive ($28 289), with a greater odds of increased expenditure (Exp[β], 1.53; 95% CI, 1.46-1.61; P < .001) compared with the Northeast. A significant difference in length of stay was found between the West and Northeast (odds ratio, 1.25; 95% CI, 1.17-1.33).
Conclusions and Relevance
There is significant cost variation among patients undergoing autologous free flap breast reconstruction. Experience, as measured by a hospital’s volume, provides quality health care with fewer complications but is more costly. Longer length of stay contributed to regional cost variation and may be a target for decreasing expenditure, without compromising care. In the era of bundled health care payment, strategies should be implemented to eliminate cost variation to condense spending while still providing quality care.
This secondary cross-sectional analysis, performed using the Healthcare Cost and Utilization Project National Inpatient Sample database from 2008 to 2010, investigates factors that influence cost variation for autologous free flap breast reconstruction.
Introduction
According to the Surveillance, Epidemiology, and End Results (SEER) database, approximately 12.4% of women are diagnosed as having breast cancer over the course of their lifetime. After implementation of the Women’s Health and Cancer Rights Act, insurance plans that provide coverage for mastectomies were required to offer coverage for postmastectomy breast reconstruction, leading to national increases in use. In 2015 alone, 106 338 women in the United States underwent breast reconstruction. These gains in access to breast reconstruction are vitally important because postmastectomy breast reconstruction has been shown to improve health-related quality of life and enhance psychosocial well-being.
In women undergoing mastectomy, reconstructive options range from implant-based to autologous breast reconstruction. The most advanced and technically challenging forms of autologous breast reconstruction involve free tissue transfers with microvascular anastomotic techniques. These free tissue transfers provide unique benefits ranging from durable natural-appearing results to superior long-term satisfaction from the patient’s perspective. Relative to implant-based reconstruction techniques, autologous free flap breast reconstructions are resource intensive. In the current political climate of affordable care, policy makers try to find ways to cut cost while still providing quality care. To minimize cost for breast reconstruction, findings have shown that microsurgical techniques increase expenditure compared with pedicled or implant-based techniques. Such studies have focused on patient-related and surgery-specific factors but have not examined hospital-related factors. Decreasing interhospital variation represents another possible avenue to standardize care and reduce cost. To date, little is known about interhospital variation of health care expenditure for autologous free flap breast reconstruction.
We aimed to evaluate interhospital cost variation for autologous free flap breast reconstruction. Our objective was to characterize hospital volume variations and regional differences to help target strategies to decrease health care expenditure.
Methods
Data Source
The Healthcare Cost and Utilization Project National Inpatient Sample (NIS) database from 2008 to 2010 was used to conduct a secondary cross-sectional analysis. The dates of analysis were September 2016 to February 2017. The NIS is a stratified database developed for the Healthcare Cost and Utilization Project (HCUP). A 20% stratified sample of all US community hospitals is randomly selected in the NIS database. The NIS contains a sample of all nonfederal, short-term hospitals, excluding rehabilitation facilities and long-term acute care hospitals. After adjustment by trend weights, it comprises more than 35 million hospitalizations per year. The database provides patient-level health care data, hospital-related information, and health care resource use data from the largest all-payer administrative database. The present study was assigned exempt status by the University of Michigan Institutional Review Board.
Patient Selection
All female patients who were diagnosed as having breast cancer or were at high risk for breast cancer and underwent postmastectomy breast reconstruction with autologous free flaps comprised our study cohort. Autologous free flaps included in this study are listed in eTable 1 in the Supplement. Patients were identified using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes and the ICD-9-CM procedure codes. We ensured that the cohort had a diagnosis code for breast cancer or were at high risk for breast cancer and had an ICD-9-CM procedure code for autologous free flap breast reconstruction. All women who underwent breast reconstruction with latissimus dorsi flaps or pedicled flaps were excluded from this study (eFigure in the Supplement).
Explanatory and Outcome Variables
Dependent Variable
The total cost during each episode of care adjusted by the consumer price index and the area wage index was used as our outcome variable. We calculated the total cost during the hospital stay by the following equation:
| Total Cost = Total Charge × Group Average All-Payer Inpatient Cost-to-Charge Ratio. |
The group average all-payer inpatient cost-to-charge ratio, which is the weighted average for the hospitals in each group (defined based on state, urban vs rural, private vs public, and number of beds), was available from the cost-to-charge ratio files from 2008 to 2010 for the NIS database. The consumer price index from September 2016 was used to inflate all cost value to the most up-to-date US dollar value. We implemented the area wage index, a measure of the relative hospital wage level in a geographic area compared with the national average hospital wage level, provided in the cost-to-charge ratio files to adjust cost measures with the national standard average. This adjusted cost was our final cost value for all analyses in this study.
Explanatory Variables
The variables of interest consisted of patient and hospital characteristics. Patient characteristics included age, length of stay (LOS), insurance type, median household income national quartile, race/ethnicity, Charlson Comorbidity Index (CCI), surgical complications, and systemic complications. Age, measured as a continuous variable, was presented as the age of the patient at the time of breast reconstruction. Race/ethnicity was categorized into white, black, Hispanic, and other minorities. An unspecified group was created for race/ethnicity to include observations with missing values in our regression models. Insurance type comprised Medicare, Medicaid, private insurance, and other insurance. The median household income included 4 quartiles, with the fourth quartile representing the highest income level. Location encompassed Northeast, Midwest, South, and West. Surgical complications and systemic complications included are listed in eTable 2 in the Supplement. In this model, we coded surgical complications and systemic complications as being present or absent. The CCI was used to classify patient comorbidity, and 3 categories were used (CCI of 0, 1, or ≥2). The CCI, surgical complications, and systemic complications variables were defined by the ICD-9-CM codes listed in eTable 2 in the Supplement. In our model, we assessed for effect modification and collinearity and found no interaction between our predictors and hospital volume or hospital location.
Hospital characteristics collected included hospital location, teaching hospital status, hospital type (government or private), hospital bed size (small, medium, or large), and hospital autologous free flap breast reconstruction volume. Private hospitals are not for profit and investor owned (proprietary) and include several teaching hospitals. Government hospitals receive funding from the government and include public hospitals. The Veterans Administration, Department of Defense, and Indian Health Service hospitals are excluded from the NIS. Hospital bed size is determined by region in the United States, urbanization (urban vs rural), and teaching status. The NIS provides a unique identifier for each hospital, enabling us to calculate the procedure volume for each hospital included in our study. We separated the cohort into 3 groups based on hospital volume, which was defined as the number of autologous free flap breast reconstruction procedures performed annually. The low-volume group had 10 or fewer cases per year, the medium-volume group had 11 to 30 cases per year, and the high-volume group had 31 or more cases per year.
Statistical Analysis
We examined the association between hospital volume and cost of the autologous free flap breast reconstruction surgery and adjusted for patient and hospital characteristics. Patient and hospital characteristics and outcomes between low-, medium-, and high-volume hospitals were compared using the Wilcoxon rank sum test because our data were not normally distributed. Similar analyses were used to compare patient and hospital characteristics and outcomes between the most costly region and the least expensive region.
We used a generalized linear mixed model to examine the association between patient and hospital characteristics and cost. The primary outcome of the model was hospital cost. We controlled for patient characteristics and hospital characteristics. We adjusted for repeated measures within each hospital by putting the hospital identifier variable as a random effect. We assumed a gamma distribution for the cost variable and used a log link function for cost in the model. The data analysis was generated using statistical software (SAS, version 9.4; SAS Institute Inc). P values were calculated with 2-sided F test.
Results
During the study period (2008-2010), 3302 women underwent autologous free flap breast reconstruction. Patient characteristics are listed in Table 1. Of these patients, 1999 had immediate breast reconstruction, and 1303 had delayed breast reconstruction. The median cost of the hospital stay was $22 677 (interquartile range [IQR], $14 907-$33 391). A total of 2712 patients (82.1%) had private insurance. There were 750 surgical complications (22.7%) and 953 systemic complications (28.9%). In total, 362 hospitals were included in the cohort.
Table 1. Characteristics of Patients Who Underwent Autologous Free Flap Breast Reconstruction From 2008 to 2010 in the United Statesa.
| Variable | Value |
|---|---|
| No. of patients | 3302 |
| Cost of hospital stay, median (IQR), $US | 22 677 (14 907-33 391) |
| Age at time of breast reconstruction, median (IQR), y | 50 (44-57) |
| Timing of free flap, No. (%) | |
| Immediate | 1999 (60.5) |
| Delayed | 1303 (39.5) |
| Radiotherapy, No. (%) | |
| No | 2944 (89.2) |
| Yes | 308 (9.3) |
| Length of stay, median (IQR), d | 4 (3-5) |
| Insurance type, No. (%) | |
| Medicare | 245 (7.4) |
| Medicaid | 218 (6.6) |
| Private | 2712 (82.1) |
| Other | 116 (3.5) |
| Median household income national quartile, No. (%) | |
| First | 453 (13.7) |
| Second | 572 (17.3) |
| Third | 844 (25.6) |
| Fourth, richest | 1346 (40.8) |
| Race/ethnicity, No. (%) | |
| White | 2029 (61.4) |
| Black | 282 (8.5) |
| Hispanic | 311 (9.4) |
| Other minorities | 210 (6.4) |
| Unspecified | 470 (14.2) |
| Hospital location, No. (%) | |
| Northeast | 617 (18.7) |
| Midwest | 766 (23.2) |
| South | 1121 (33.9) |
| West | 798 (24.2) |
| Charlson Comorbidity Index, No. (%) | |
| 0 | 1629 (49.3) |
| 1 | 227 (6.9) |
| ≥2 | 1446 (43.8) |
| Teaching hospital, No. (%) | |
| Yes | 2576 (78.0) |
| No | 679 (20.6) |
| Hospital type, No. (%) | |
| Government | 2868 (86.9) |
| Private | 434 (13.1) |
| Surgical complications, No. (%) | |
| Yes | 750 (22.7) |
| No | 2552 (77.3) |
| Systemic complications, No. (%) | |
| Yes | 953 (28.9) |
| No | 2349 (71.1) |
| Hospital bed size, No. (%) | |
| Small | 375 (11.4) |
| Medium | 441 (13.4) |
| Large | 2439 (73.9) |
Abbreviation: IQR, interquartile range.
From the 2008 to 2012 Healthcare Cost and Utilization Project National Inpatient Sample database. Some numbers do not sum to heading totals because of missing values.
Patient characteristics, hospital data, and cost are listed in Table 2 after categorizing our cohort into 3 groups by hospital volume. There were 322 hospitals in the low-volume group, 31 hospitals in the medium-volume group, and 9 hospitals in the high-volume group. High-volume hospitals had significantly increased expenditure. The median cost at high-volume hospitals was $24 360 (IQR, $15 167-$34 619) compared with $18 918 (IQR, $12 856-$29 186) at low-volume hospitals (P < .001). Fewer surgical complications were present in the high-volume group compared with the low-volume group (16.4% [169 of 1029] vs 23.7% [278 of 1174], P < .001). Systemic complications followed a similar pattern, with high-volume hospitals having the lowest systemic complication rate (24.2% [249 of 1029] vs 31.2% [366 of 1174], P < .001). Hospital factors, including teaching hospital status, hospital type, and hospital bed size were also different between high-volume hospitals and low-volume hospitals. High-volume hospitals were more likely to be teaching hospitals and government hospitals and have large bed size. Differences in cost, patient factors, and hospital factors between procedure volumes are listed in eTable 3 in the Supplement. There was a significant difference in cost between high-volume and low-volume hospitals and between medium-volume and low-volume hospitals, with high-volume and medium-volume hospitals being more expensive.
Table 2. Characteristics of Patients Who Underwent Autologous Free Flap Breast Reconstruction by Hospital Volume From 2008 to 2010 in the United Statesa.
| Variable | Low, ≤10 Cases | Medium, 11-30 Cases | High, ≥31 Cases | P Value |
|---|---|---|---|---|
| No. of patients | 1174 | 1099 | 1029 | NA |
| Dependent Variable | ||||
| Cost of hospital stay, median (IQR), $US | 18 918 (12 856-29 186) | 24 205 (17 163-35 501) | 24 360 (15 167-34 619) | <.001b |
| Explanatory Variables | ||||
| Age at time of breast reconstruction, median (IQR), y | 51 (45-57) | 51 (44-57) | 49 (43-56) | .005b |
| Length of stay, median (IQR), d | 4 (3-5) | 4 (4-5) | 4 (4-5) | <.001 |
| Insurance type, No. (%) | ||||
| Medicare | 117 (10.0) | 70 (6.4) | 58 (5.6) | <.001b |
| Medicaid | 121 (10.3) | 75 (6.8) | 22 (2.1) | |
| Private | 869 (74.0) | 900 (81.9) | 943 (91.6) | |
| Other | 65 (5.5) | 45 (4.1) | 6 (0.6) | |
| Median household income national quartile, No. (%) | ||||
| First | 201 (17.1) | 108 (9.8) | 144 (14.0) | <.001b |
| Second | 216 (18.4) | 196 (17.8) | 160 (15.5) | |
| Third | 326 (27.8) | 280 (25.5) | 238 (23.1) | |
| Fourth | 381 (32.5) | 491 (44.7) | 474 (46.1) | |
| Race/ethnicity, No. (%) | ||||
| White | 741 (63.1) | 695 (63.2) | 593 (57.6) | <.001b |
| Black | 141 (12.0) | 84 (7.6) | 57 (5.5) | |
| Hispanic | 102 (8.7) | 67 (6.1) | 142 (13.8) | |
| Other minorities | 70 (6.0) | 59 (5.4) | 81 (7.9) | |
| Unspecified | 120 (10.2) | 194 (17.7) | 156 (15.2) | |
| Hospital location, No. (%) | ||||
| Northeast | 284 (24.2) | 202 (18.4) | 131 (12.7) | <.001b |
| Midwest | 213 (18.1) | 333 (30.3) | 220 (21.4) | |
| South | 480 (40.9) | 275 (25.0) | 366 (35.6) | |
| West | 197 (16.8) | 289 (26.3) | 312 (30.3) | |
| Charlson Comorbidity Index, No. (%) | ||||
| 0 | 539 (45.9) | 543 (49.4) | 547 (53.2) | .02b |
| 1 | 91 (7.8) | 75 (6.8) | 61 (5.9) | |
| ≥2 | 544 (46.3) | 481 (43.8) | 421 (40.9) | |
| Teaching hospital, No. (%) | ||||
| Yes | 697 (59.4) | 916 (83.3) | 963 (93.6) | <.001b |
| No | 430 (36.6) | 183 (16.7) | 66 (6.4) | |
| Hospital type, No. (%) | ||||
| Government | 906 (77.2) | 999 (90.9) | 963 (93.6) | <.001b |
| Private | 268 (22.8) | 100 (9.1) | 66 (6.4) | |
| Hospital bed size, No. (%) | ||||
| Small | 131 (11.2) | 115 (10.5) | 129 (12.5) | <.001b |
| Medium | 243 (20.7) | 198 (18.0) | 0 | |
| Large | 753 (64.1) | 786 (71.5) | 900 (87.5) | |
| Surgical complications, No. (%) | ||||
| Yes | 278 (23.7) | 303 (27.6) | 169 (16.4) | <.001b |
| No | 896 (76.3) | 796 (72.4) | 860 (83.6) | |
| Systemic complications, No. (%) | ||||
| Yes | 366 (31.2) | 338 (30.8) | 249 (24.2) | <.001b |
| No | 808 (68.8) | 761 (69.2) | 780 (75.8) | |
Abbreviations: IQR, interquartile range; NA, not applicable.
From the 2008 to 2012 Healthcare Cost and Utilization Project National Inpatient Sample database. Some numbers do not sum to heading totals because of missing values.
Statistically significant at 95% level.
We then compared the most costly region, the West, with the least expensive region, the Northeast. A total of 798 patients in the West and 617 patients in the Northeast underwent autologous free flap breast reconstruction. Table 3 lists patient-specific and hospital-related differences between these 2 regions. The Northeast had more teaching hospitals (91.9% [567 of 617] in the Northeast and 69.2% [552 of 798] in the West), more government hospitals (100% [617 of 617] in the Northeast and 70.4% [562 of 798] in the West), and smaller bed size (71.8% [443 of 617] large bed size in the Northeast and 82.0% [654 of 798] large bed size in the West). Hospital cost was significantly higher in the West ($28 289) compared with the Northeast ($16 461) (P < .001). Differences in cost, patient factors, and hospital factors between the West and Northeast are listed in eTable 4 in the Supplement. Patients in the West had a median LOS of 4 nights (IQR, 4-5 nights), and patients in the Northeast had a median LOS of 4 nights (IQR, 3-5 nights) (Table 3). The LOS was significantly different between the 2 geographic groups (odds ratio [OR], 1.25; 95% CI, 1.17-1.33). In addition, more high-volume hospitals were present in the West compared with the Northeast (39.1% [312 of 798] vs 21.2% [131 of 617]). Hospital costs in the West were higher than in the Northeast across all surgical volume categories ($32 913 vs $21 704 for high volume, $33 310 vs $17 339 for medium volume, and $29 229 vs $16 539 for low volume). Patients in the Northeast had more comorbidities than those in the West. There were no differences in surgical complications (OR, 0.90; 95% CI, 0.70-1.16; P = .38) or systemic complications (OR, 0.89; 95% CI, 0.70-1.14; P = .20) between the 2 regions.
Table 3. Characteristics of Patients Who Underwent Autologous Free Flap Breast Reconstruction by Region (Highest vs Lowest Cost) From 2008 to 2010 in the United Statesa.
| Variable | West | Northeast | P Value |
|---|---|---|---|
| No. of patients | 798 | 617 | NA |
| Cost of hospital stay, median (IQR), $US | 28 289 (21 226-38 568) | 16 461 (11 276-22 019) | <.001b |
| Age at time of breast reconstruction, median (IQR), y | 51 (45-57) | 50 (44-56) | .39 |
| Length of stay, median (IQR), d | 4 (4-5) | 4 (3-5) | <.001b |
| Insurance type, No. (%) | |||
| Medicare | 63 (7.9) | 45 (7.3) | .01b |
| Medicaid | 52 (6.5) | 46 (7.5) | |
| Private | 668 (83.7) | 496 (80.4) | |
| Other | 15 (1.9) | 30 (4.9) | |
| Median household income national quartile, No. (%) | |||
| First | 65 (8.1) | 57 (9.2) | <.001b |
| Second | 125 (15.7) | 58 (9.4) | |
| Third | 192 (24.1) | 116 (18.8) | |
| Fourth | 402 (50.4) | 352 (57.1) | |
| Race/ethnicity, No. (%) | |||
| White | 573 (71.8) | 442 (71.6) | <.001b |
| Black | 27 (3.4) | 59 (9.6) | |
| Hispanic | 76 (9.5) | 61 (9.9) | |
| Other minorities | 73 (9.1) | 48 (7.8) | |
| Unspecified | 49 (6.1) | 7 (1.1) | |
| Hospital volume, No. (%) | |||
| ≤10 | 197 (24.7) | 284 (46.0) | <.001b |
| 11-30 | 289 (36.2) | 202 (32.7) | |
| ≥31 | 312 (39.1) | 131 (21.2) | |
| Charlson Comorbidity Index, No. (%) | |||
| 0 | 445 (55.8) | 223 (36.1) | <.001b |
| 1 | 60 (7.5) | 30 (4.9) | |
| ≥2 | 293 (36.7) | 364 (59.0) | |
| Teaching hospital, No. (%) | |||
| Yes | 552 (69.2) | 567 (91.9) | <.001b |
| No | 246 (30.8) | 50 (8.1) | |
| Hospital type, No. (%) | |||
| Government | 562 (70.4) | 617 (100) | <.001b |
| Private | 236 (29.6) | 0 | |
| Surgical complications, No. (%) | |||
| Yes | 182 (22.8) | 153 (24.8) | .38 |
| No | 616 (77.2) | 464 (75.2) | |
| Systemic complications, No. (%) | |||
| Yes | 201 (25.2) | 174 (28.2) | .20 |
| No | 597 (74.8) | 443 (71.8) | |
| Hospital bed size, No. (%) | |||
| Small | 71 (8.9) | 83 (13.5) | <.001b |
| Medium | 73 (9.1) | 91 (14.7) | |
| Large | 654 (82.0) | 443 (71.8) |
Abbreviations: IQR, interquartile range; NA, not applicable.
From the 2008 to 2012 Healthcare Cost and Utilization Project National Inpatient Sample database. Some numbers do not sum to heading totals because of missing values.
Statistically significant at 95% level.
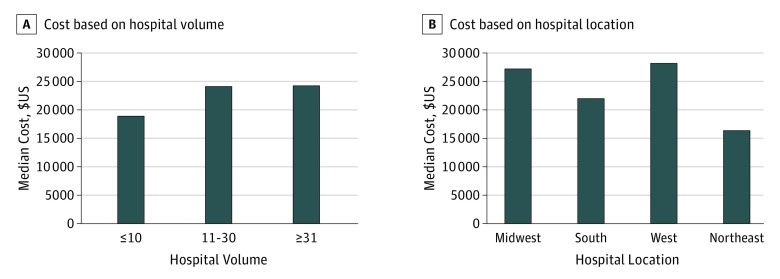
On multivariable analysis, hospital volume, hospital location, comorbidities (CCI), longer LOS, and the presence of complications were predictors of increased hospital expenditure (Table 4). Patients with a CCI of 1 or more compared with a CCI of 0 had significantly increased cost (Exp[β], 1.09; 95% CI, 1.03-1.16; P = .004). Exp[β] indicates the ratio of the average cost between the reference group and each category. For example, 1.09 is the ratio of the average cost of care for patients with a CCI of 1 or more and the average cost of care for patients with a CCI of 0. Longer LOS was associated with increased expenditure (Exp[β], 1.11; 95% CI, 1.10-1.11; P < .001), and complications increased resource use. The median cost for a patient with a surgical complication was $29 399 (IQR, $20 778-$42 359) (compared with $20 616 [IQR, $13 975-$30 488] without), and the median cost for a patient with a systemic complication was $24 525 (IQR, $15 819-$35 149) (compared with $21 922 [IQR, $14 605-$32 500] without). High-volume hospitals (Exp[β], 1.06; 95% CI, 1.02-1.11; P = .003) and medium-volume hospitals (Exp[β], 1.07; 95% CI, 1.03-1.11; P < .001) predicted greater expenditure (Table 4 and Figure, A). Geographic variation was also associated with disparate resource use, with the West being the most expensive region (Exp[β], 1.53; 95% CI, 1.46-1.61; P < .001) (Table 4 and Figure, B).
Table 4. Results of the Generalized Linear Mixed Model for Cost Variation for Autologous Free Flap Breast Reconstruction From 2008 to 2010 in the United Statesa.
| Variable | Exp[β] (95% CI) | P Value |
|---|---|---|
| Age at time of breast reconstruction | 1.00 (0.99-1.00) | <.001b |
| Insurance type | ||
| Medicare | 0.95 (0.90-1.01) | .10 |
| Medicaid | 0.92 (0.86-0.98) | .007b |
| Other | 0.94 (0.87-1.02) | .13 |
| Private | 1 [Reference] | NA |
| Race/ethnicity | ||
| Black | 1.08 (1.02-1.14) | .006b |
| Hispanic | 0.83 (0.79-0.87) | <.001b |
| Other minorities | 0.99 (0.93-1.05) | .78 |
| Unspecified | 1.02 (0.96-1.07) | .56 |
| White | 1 [Reference] | NA |
| Median household income national quartile | ||
| First | 0.96 (0.91-1.00) | .07 |
| Second | 0.99 (0.95-1.03) | .53 |
| Third | 1.01 (0.97-1.05) | .57 |
| Fourth | 1 [Reference] | NA |
| Hospital volume | ||
| 11-30 | 1.07 (1.03-1.11) | <.001b |
| ≥31 | 1.06 (1.02-1.11) | .003b |
| ≤10 | 1 [Reference] | NA |
| Hospital location | ||
| Midwest | 1.63 (1.54-1.72) | <.001b |
| South | 1.12 (1.07-1.17) | <.001b |
| West | 1.53 (1.46-1.61) | <.001b |
| Northeast | 1 [Reference] | NA |
| Charlson Comorbidity Index | ||
| 1 | 1.09 (1.03-1.16) | .004b |
| ≥2 | 1.03 (0.99-1.06) | .11 |
| 0 | 1 [Reference] | |
| Length of stay | 1.11 (1.10-1.11) | <.001b |
| Teaching hospital | ||
| Yes | 1.14 (1.08-1.22) | <.001b |
| No | 1 [Reference] | NA |
| Hospital type | ||
| Private | 1.34 (1.25-1.44) | <.001b |
| Government | 1 [Reference] | NA |
| Surgical complications | ||
| Yes | 1.18 (1.13-1.22) | <.001b |
| No | 1 [Reference] | NA |
| Systemic complications | ||
| Yes | 1.04 (1.01-1.08) | .02b |
| No | 1 [Reference] | NA |
| Hospital bed size | ||
| Medium | 0.82 (0.77-0.88) | <.001b |
| Large | 0.82 (0.78-0.86) | <.001b |
| Small | 1 [Reference] | NA |
Abbreviation: NA, not applicable.
From the 2008 to 2012 Healthcare Cost and Utilization Project National Inpatient Sample database.
Statistically significant at 95% level.
Figure. Cost Variation for Autologous Free Flap Breast Reconstruction.
A, Based on hospital volume. B, Based on hospital location. From the 2008 to 2012 Healthcare Cost and Utilization Project National Inpatient Sample database.
Discussion
Using a nationwide, generalizable estimate of surgical performance and cost, this study demonstrates significant interhospital cost variation for autologous free flap breast reconstruction. High procedure volume was associated with increased hospital spending. However, this elevated cost was coupled with improved surgical outcomes. Geographic cost variation was also present, with the West having the greatest expenditure. Given the current political environment of cost containment, interhospital variation has substantial fiscal and policy implications.
Health care spending continues to rise, despite attempts to contain cost. Over the past few years, health care costs in the inpatient setting contributed the most to health care expenses. The principal inpatient spending drivers are health care labor shortages, technology, and hospital market characteristics. With this scenario in mind, policy makers try to find ways to minimize cost. The quantity of health care delivered, as measured by the number of tests and procedures, and the use of specialists are scrutinized as explanations for increased expenditure. Therefore, the Centers for Medicare & Medicaid Services initiated reforms to transition care from volume-based pricing of services to quality of services. Bundling of payment will impart one disbursement for all care under a specific diagnosis or procedure code. These adjustments in health care push hospitals and clinicians to deliver high-quality care at a lower price.
In this study, higher-volume hospitals were more expensive than lower-volume hospitals but had fewer complications. Substantial literature within different surgical fields confirms an association between surgical volume and improved outcomes. These studies have been performed for high-risk procedures, such as coronary artery bypass graft surgery, esophagectomy, oncologic resections, and abdominal aortic aneurysm repairs. Recently, outcomes and surgical volume for breast reconstruction have been studied. In 2013, Albornoz et al investigated this trend and concluded that higher-volume hospitals had improved surgical and systemic outcomes. Our study corroborates these findings. However, improved outcomes at high-volume hospitals came with increased cost. Beyond the initial procedure for breast reconstruction, patients are managed for many months, and autologous free flap breast reconstruction complications over time lead to increased expenditure. Although impossible to ascertain with the NIS database, there might be financial benefits gained from fewer complications over the entire period of care for breast reconstruction. Higher-volume hospitals were more likely to be teaching hospitals and government hospitals and have larger bed size, and these underlying hospital characteristics may also contribute to expenditure.
Regional disparities in care have been identified as one possible solution to decrease health care costs. Regional variation for autologous free flap breast reconstruction was predictive of increased health care use. The highest cost difference was seen in the West ($28 289) compared with the Northeast ($16 461). Regional differences have been seen in other medical and surgical fields. Obirieze et al observed significant regional variations in trauma care, with the West having an increased relative cost of liver and splenic injuries, pneumothoraces, tibial fractures, and traumatic brain injuries compared with the Northeast. Rettenmaier and Wang examined regional variations of medical expenditure on the state level and concluded that fee-for-service reimbursement contributes greatly to regional variation. Reasons behind this trend include discrepancies in efficiency of care and health status of patients. We also found a significant difference in LOS in the West compared with the Northeast. These differences were in spite of caring for patients with fewer comorbidities in the West and in the absence of differences in postoperative complications. However, in this study, the severity of postoperative complications within the different regions is unknown and may have contributed to discrepancies in LOS. Nonetheless, in efforts to decrease expenditure, expedited discharge of patients with low preoperative risk may help contain costs, without compromising outcomes. The fact that there were more high-volume hospitals in the West may have contributed to increased expenditure; however, low-, medium-, and high-volume hospitals were more expensive in the West. Consequently, increased cost in the West cannot be completely explained by hospital volume. Differences in practice patterns must be further studied as an avenue to reduce spending.
Limitations
Our study has some limitations. The complications studied herein are only based on one episode of care, namely, the episode associated with the autologous free flap breast reconstruction. Therefore, late complications, such as fat necrosis, late flap failure, abdominal hernia and bulge formation, late surgical site infections, wound dehiscence, and revision surgical procedures, could not be evaluated. In addition, cost beyond the one episode of care could not be studied. Furthermore, this study is a cross-sectional analysis, making it difficult to establish causality. We can only comment on associations between certain variables. Furthermore, this data set includes a unique hospital identifier but does not provide the identity of a specific hospital or the clinician; consequently, we cannot make conclusions about specific hospitals or surgeons. For cost, the NIS contains the total inpatient hospital charges and does not include physician fees. The physician fees for autologous free flap breast reconstruction vary nationally. For instance, “carve-out” arrangements with insurance companies provide much better surgeon payments and may further contribute to disparities in cost. However, these disparities cannot be studied using the NIS owing to these limitations. Furthermore, the NIS database lacks the granularity to determine the exact finances of the hospitals that may allow for alternative interpretations of the data. In addition, we separated our cohort into 3 groups based on surgical volume. The definition of high volume is based on the 90th percentile of the number of free flaps performed and has been used in studies investigating hospital volume and free flap reconstruction. However, these volume cutoffs have not been validated and may be a source of bias. In addition, in the current political climate, the fate of health care is unknown, and health care reimbursement is different from the cost structure in place during the study period. Given these changing policies, the generalizability of our study is restricted. Last, the NIS only includes data on insured patients, limiting the generalizability of our findings to the uninsured.
Conclusions
Despite these limitations, this nationwide study of interhospital cost variation for autologous free flap breast reconstruction provides insight into ways to minimize expenditure while still providing high-quality health care. Although hospital volume was associated with increased cost, fewer surgical complications emphasize the importance of procedure volume and outcomes. This study only considers the index procedure episode of care, and long-term financial benefits from fewer complications may be realized when accounting for the entire period of care for breast reconstruction. This study also uncovered regional variation in expenditure for free tissue transfer for breast reconstruction. In the West, we found increased LOS and expenditure, despite comparable preoperative risk and complications rates. Measures to expedite patient discharge while still maintaining quality care need to be investigated to diminish this regional variation. With changes in health care reimbursement, it is imperative to recognize interhospital variation and to target avenues to decrease spending. This study highlights the need for additional investigation into drivers of interhospital variation for autologous free flap breast reconstruction.
eTable 1. Diagnosis and Procedure Codes for Breast Cancer and Free Flap Breast Reconstruction
eTable 2. Code List for Surgical Complications, Systemic Complications, and Charlson Comorbidity Index
eTable 3. Effect Estimates of Patients Who Underwent Autologous Free Flap Breast Reconstruction by Hospital Volume From 2008 to 2010 in the U.S.
eTable 4. Effect Estimates of Patients Who Underwent Autologous Free Flap Breast Reconstruction by Region From 2008 to 2010 in the U.S.
eFigure. Flow Diagram of Patients Undergoing Free Flap Breast Reconstruction Using National Inpatient Sample Database, 2008-2010
References
- 1.Howlader N, Noone AM, Krapcho M, et al. , eds. SEER Cancer Statistics Review, 1975-2013 Bethesda, MD: National Cancer Institute; based on November 2015 SEER data. https://seer.cancer.gov/csr/1975_2013/. Published April 2016. Accessed November 20, 2016.
- 2.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131(1):15-23. [DOI] [PubMed] [Google Scholar]
- 3.Sisco M, Du H, Warner JP, Howard MA, Winchester DP, Yao K. Have we expanded the equitable delivery of postmastectomy breast reconstruction in the new millennium? evidence from the National Cancer Data Base. J Am Coll Surg. 2012;215(5):658-666. [DOI] [PubMed] [Google Scholar]
- 4.American Society of Plastic Surgeons 2015 Plastic surgery statistics. http://www.plasticsurgery.org/news/plastic-surgery-statistics.html. Accessed November 2016.
- 5.Silberfarb PM, Maurer LH, Crouthamel CS. Psychosocial aspects of neoplastic disease, I: functional status of breast cancer patients during different treatment regimens. Am J Psychiatry. 1980;137(4):450-455. [DOI] [PubMed] [Google Scholar]
- 6.Ueda S, Tamaki Y, Yano K, et al. Cosmetic outcome and patient satisfaction after skin-sparing mastectomy for breast cancer with immediate reconstruction of the breast. Surgery. 2008;143(3):414-425. [DOI] [PubMed] [Google Scholar]
- 7.Wilkins EG, Cederna PS, Lowery JC, et al. Prospective analysis of psychosocial outcomes in breast reconstruction: one-year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2000;106(5):1014-1025. [DOI] [PubMed] [Google Scholar]
- 8.Zhong T, McCarthy C, Min S, et al. Patient satisfaction and health-related quality of life after autologous tissue breast reconstruction: a prospective analysis of early postoperative outcomes. Cancer. 2012;118(6):1701-1709. [DOI] [PubMed] [Google Scholar]
- 9.Jagsi R, Li Y, Morrow M, et al. Patient-reported quality of life and satisfaction with cosmetic outcomes after breast conservation and mastectomy with and without reconstruction: results of a survey of breast cancer survivors. Ann Surg. 2015;261(6):1198-1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atisha DM, Rushing CN, Samsa GP, et al. A national snapshot of satisfaction with breast cancer procedures. Ann Surg Oncol. 2015;22(2):361-369. [DOI] [PubMed] [Google Scholar]
- 11.Alderman AK, Kuhn LE, Lowery JC, Wilkins EG. Does patient satisfaction with breast reconstruction change over time? two-year results of the Michigan Breast Reconstruction Outcomes Study. J Am Coll Surg. 2007;204(1):7-12. [DOI] [PubMed] [Google Scholar]
- 12.Fischer JP, Fox JP, Nelson JA, Kovach SJ, Serletti JM. A longitudinal assessment of outcomes and healthcare resource utilization after immediate breast reconstruction: comparing implant- and autologous-based breast reconstruction. Ann Surg. 2015;262(4):692-699. [DOI] [PubMed] [Google Scholar]
- 13.Sando IC, Chung KC, Kidwell KM, Kozlow JH, Malay S, Momoh AO. Comprehensive breast reconstruction in an academic surgical practice: an evaluation of the financial impact. Plast Reconstr Surg. 2014;134(6):1131-1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kulkarni AR, Sears ED, Atisha DM, Alderman AK. Use of autologous and microsurgical breast reconstruction by U.S. plastic surgeons. Plast Reconstr Surg. 2013;132(3):534-541. [DOI] [PubMed] [Google Scholar]
- 15.Alderman AK, Storey AF, Nair NS, Chung KC. Financial impact of breast reconstruction on an academic surgical practice. Plast Reconstr Surg. 2009;123(5):1408-1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Albornoz CR, Cordeiro PG, Mehrara BJ, et al. Economic implications of recent trends in U.S. immediate autologous breast reconstruction. Plast Reconstr Surg. 2014;133(3):463-470. [DOI] [PubMed] [Google Scholar]
- 17.Healthcare Cost and Utilization Project. NIS database documentation. http://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp. Published 2011. Accessed November 20, 2016.
- 18.Healthcare Cost and Utilization Project. Cost-to-charge ratio files. https://hcup-us.ahrq.gov/db/state/costtocharge.jsp. Accessed November 20, 2016. [Google Scholar]
- 19.Mooney JJ, Raimundo K, Chang E, Broder MS. Hospital cost and length of stay in idiopathic pulmonary fibrosis. J Med Econ. 2017;20(5):518-524. [DOI] [PubMed] [Google Scholar]
- 20.Faiena I, Dombrovskiy VY, Modi PK, et al. Regional cost variations of robot-assisted radical prostatectomy compared with open radical prostatectomy. Clin Genitourin Cancer. 2015;13(5):447-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Obirieze AC, Gaskin DJ, Villegas CV, et al. Regional variations in cost of trauma care in the United States: who is paying more? J Trauma Acute Care Surg. 2012;73(2):516-522. [DOI] [PubMed] [Google Scholar]
- 22.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. [DOI] [PubMed] [Google Scholar]
- 23.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-619. [DOI] [PubMed] [Google Scholar]
- 24.Albornoz CR, Cordeiro PG, Hishon L, et al. A nationwide analysis of the relationship between hospital volume and outcome for autologous breast reconstruction. Plast Reconstr Surg. 2013;132(2):192e-200e. [DOI] [PubMed] [Google Scholar]
- 25.Tuggle CT, Patel A, Broer N, Persing JA, Sosa JA, Au AF. Increased hospital volume is associated with improved outcomes following abdominal-based breast reconstruction. J Plast Surg Hand Surg. 2014;48(6):382-388. [DOI] [PubMed] [Google Scholar]
- 26.Hay JW. Hospital cost drivers: an evaluation of 1998-2001 state-level data. Am J Manag Care. 2003;9(spec No 1):SP13-SP24. [PubMed] [Google Scholar]
- 27.Goetghebeur MM, Forrest S, Hay JW. Understanding the underlying drivers of inpatient cost growth: a literature review. Am J Manag Care. 2003;9(spec No 1):SP3-SP12. [PubMed] [Google Scholar]
- 28.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending, part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273-287. [DOI] [PubMed] [Google Scholar]
- 29.Hackbarth G, Reischauer R, Mutti A. Collective accountability for medical care: toward bundled Medicare payments. N Engl J Med. 2008;359(1):3-5. [DOI] [PubMed] [Google Scholar]
- 30.Burwell SM. Setting value-based payment goals: HHS efforts to improve U.S. health care. N Engl J Med. 2015;372(10):897-899. [DOI] [PubMed] [Google Scholar]
- 31.Press MJ, Rajkumar R, Conway PH. Medicare’s new bundled payments: design, strategy, and evolution. JAMA. 2016;315(2):131-132. [DOI] [PubMed] [Google Scholar]
- 32.Cutler DM, Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med. 2012;366(12):1075-1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Birkmeyer JD, Dimick JB, Staiger DO. Operative mortality and procedure volume as predictors of subsequent hospital performance. Ann Surg. 2006;243(3):411-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kohn GP, Galanko JA, Meyers MO, Feins RH, Farrell TM. National trends in esophageal surgery–are outcomes as good as we believe? J Gastrointest Surg. 2009;13(11):1900-1910. [DOI] [PubMed] [Google Scholar]
- 35.Birkmeyer JD, Finlayson SR, Tosteson AN, Sharp SM, Warshaw AL, Fisher ES. Effect of hospital volume on in-hospital mortality with pancreaticoduodenectomy. Surgery. 1999;125(3):250-256. [PubMed] [Google Scholar]
- 36.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364(22):2128-2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Israeli R, Funk S, Reaven NL. Comparative analysis of 18-month outcomes and costs of breast reconstruction flap procedures. Plast Reconstr Surg. 2014;133(3):471-479. [DOI] [PubMed] [Google Scholar]
- 38.Rettenmaier AJ, Wang Z. Regional variations in medical spending and utilization: a longitudinal analysis of US Medicare population. Health Econ. 2012;21(2):67-82. [DOI] [PubMed] [Google Scholar]
- 39.Makarov DV, Loeb S, Landman AB, et al. Regional variation in total cost per radical prostatectomy in the Healthcare Cost and Utilization Project Nationwide Inpatient Sample database. J Urol. 2010;183(4):1504-1509. [DOI] [PubMed] [Google Scholar]
- 40.Sun GH, Auger KA, Aliu O, Patrick SW, DeMonner S, Davis MM. Variation in inpatient tonsillectomy costs within and between US hospitals attributable to postoperative complications. Med Care. 2013;51(12):1048-1054. [DOI] [PubMed] [Google Scholar]
- 41.Sirovich B, Gallagher PM, Wennberg DE, Fisher ES. Discretionary decision making by primary care physicians and the cost of U.S. health care. Health Aff (Millwood). 2008;27(3):813-823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zuckerman S, Waidmann T, Berenson R, Hadley J. Clarifying sources of geographic differences in Medicare spending. N Engl J Med. 2010;363(1):54-62. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Diagnosis and Procedure Codes for Breast Cancer and Free Flap Breast Reconstruction
eTable 2. Code List for Surgical Complications, Systemic Complications, and Charlson Comorbidity Index
eTable 3. Effect Estimates of Patients Who Underwent Autologous Free Flap Breast Reconstruction by Hospital Volume From 2008 to 2010 in the U.S.
eTable 4. Effect Estimates of Patients Who Underwent Autologous Free Flap Breast Reconstruction by Region From 2008 to 2010 in the U.S.
eFigure. Flow Diagram of Patients Undergoing Free Flap Breast Reconstruction Using National Inpatient Sample Database, 2008-2010