This study identifies sources of avoidable surgical intensive care unit days and determines strategies to minimize these days in preinterventional and postinterventional populations.
Key Points
Questions
What is the percentage of potentially avoidable admissions and disposition delays among patients admitted to a surgical intensive care unit, and can a portion of these avoidable days be eliminated?
Findings
In this study of 459 patients with 506 admissions, the initial rates of potentially avoidable surgical intensive care unit admissions and disposition delays were 152 (13%) and 138 (11.8%) of 1168 days, respectively; reductions to 118 (8.8%) and 97 (7.2%) of 1338 days, respectively, occurred after the implementation of targeted interventions.
Meaning
Although potentially avoidable surgical intensive care unit admissions and disposition delays are frequent, reductions may be attainable when interventions target the common sources.
Abstract
Importance
High health care costs encourage initiatives that avoid overuse of resources and identify opportunities to promote appropriate care.
Objective
To investigate the causes of potentially avoidable surgical intensive care unit (SICU) admissions and disposition delays to determine whether targeted interventions could decrease these stays.
Design, Setting, and Participants
This prospective, observational study focused on potentially avoidable SICU days, as determined by observers with input from the rounding intensivists at a 24-bed open SICU at an urban, academic hospital. The preintervention phase occurred from April 6 through June 21, 2015; after implementation of targeted interventions, the postintervention phase occurred from April 4 through June 28, 2016. Data collected included demographic characteristics, reason for admission, and length of stay. All patients admitted to the SICU during the preintervention and postintervention phases were included in the analysis.
Interventions
Based on results collected in the preintervention phase, targeted interventions were designed and implemented from July 1, 2015, through March 31, 2016, including (1) reducing SICU care for minor traumatic brain injury, (2) optimizing postoperative airway management, (3) enhancing communication between services regarding transfers to the SICU, (4) identifying and facilitating more timely end-of-life conversations and supportive care consultations, and (5) encouraging early disposition of patients to floor beds.
Main Outcomes and Measures
Changes in the proportion of potentially avoidable SICU days owing to potentially avoidable admissions and/or disposition delays.
Results
A total of 459 patients (253 men [55.1%] and 206 women [44.9%]; median age, 62 years [interquartile range, 46-75 years]) were admitted during the preintervention and postintervention phases. Of 261 patients admitted during the preintervention period and 245 during the postintervention period, median SICU and hospital length of stay remained unchanged. A reduction was noted in the percentage of postintervention SICU days owing to potentially avoidable admissions (152 of 1168 days [13%] vs 118 of 1338 days [8.8%]; P = .001) and disposition delays (138 of 1168 days [11.8%] vs 97 of 1338 days [7.2%]; P < .001). During the postintervention period, decreases were noted in the SICU days related to the most common sources of potentially avoidable admissions (SICU stay ≤24 hours, airway concerns, and somnolence) and disposition delays (end-of-life decisions and floor bed unavailable) as well as in the overall rate of potentially avoidable days (269 of 1168 days [23%] vs 205 of 1338 days [15.3%]; P < .001).
Conclusions and Relevance
Nearly one-fourth of SICU days could be categorized as potentially avoidable. Targeted interventions resulted in a significant reduction of potentially avoidable SICU days.
Introduction
In the United States, national health care expenditures for 2014 were estimated to be $3 trillion, with a mean of more than $9500 spent per capita. Unsustainable health care costs have prompted initiatives for cost containment, including identifying strategies to eliminate overtreatment, which accounts for up to $226 billion in spending. The intensive care unit (ICU) constitutes a disproportionate fraction of health care overtreatment, and efforts to achieve cost containment by decreasing avoidable care have been difficult. Physicians perceive ICU overtreatment to be common, with reasons that include clinical doubt, limited time for decision making, assessment error, and pressure from superiors, other clinicians, and patients’ families. Furthermore, overuse of limited ICU resources can result in delays in the care of other patients needing ICU admission. Intensive care unit overtreatment may be attributable to avoidable admissions, which in the case of pediatric trauma may occur one-third of the time, or to disposition delays, which may be the source of one-fourth of all patient-days and include delays related to challenges with patient transfer or end-of-life (EOL) decisions.
Overtreatment in the surgical ICU (SICU) has not been well described to date. Although the nature of what constitutes overtreatment varies from one ICU to another based on resources available, identifying reasons for avoidable SICU days may reveal opportunities to minimize overtreatment in most ICUs. Of importance, attempts to reduce overtreatment must be conducted in a safe manner to avoid any adverse consequences. The purpose of this study was to identify sources of avoidable SICU days and to determine strategies to minimize these days. We hypothesized that by first characterizing the reasons for the potentially avoidable admissions and disposition delays and then focusing on the surgical services and related challenges that accounted for the related potentially avoidable SICU days, we could target specific interventions aimed at reducing these days.
Methods
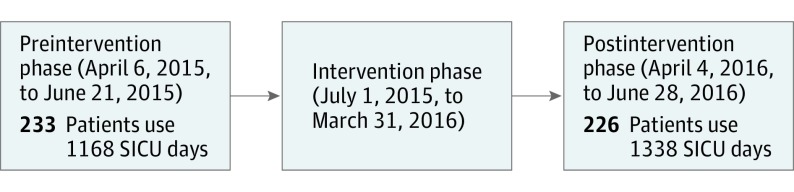
This prospective observational study was performed at an open 24-bed trauma and surgical ICU at an urban academic institution in the following 3 phases: a preintervention observational phase from April 6 through June 21, 2015; an intervention phase from July 1, 2015, through March 31, 2016; and a postintervention observational phase from April 4 through June 28, 2016 (Figure 1). All patients in the SICU discharged from April 6 through June 21, 2015, and from April 4 through June 28, 2016, were included in the study, and the same team of nurse observers (M.K. and J.C.) participated in the preintervention and postintervention observation phases. Information collected included patient demographic and clinical characteristics, surgical procedures performed, identification of the admitting service, consultations obtained, length of stay (LOS), discharge disposition, and mortality. Data were extracted from hospital electronic medical records, an internal institutional database from resource outcomes management, and observer interviews and interactions with clinicians. The observers, who were nurse members of the Cedars-Sinai Human-Centered Design team and trained in human factors design analysis, attended daily morning rounds with the SICU team and noted cases that were identified by the intensivists as potentially avoidable admissions and/or disposition delays. This study was approved by the institutional review board of Cedars-Sinai Medical Center, which waived the need for informed consent for the use of deidentified data.
Figure 1. Study Design.
SICU indicates surgical intensive care unit.
Data collection during the preintervention phase identified patient admissions that might not have required the SICU level of care, and these were labeled as potentially avoidable. Potentially avoidable admissions included stays less than 24 hours, often owing to a diagnosis of mild traumatic brain injury (TBI) in the context of an intact neurologic examination finding, and admissions for postoperative airway concerns or somnolence when postanesthesia care unit recovery may have been more appropriate. The observed types and reasons for avoidable admissions were described previously, and by labeling these stays as potentially avoidable, some stays may have been indicated. Our focus was on reducing a portion of potentially avoidable admissions while acknowledging that the percentage could not be zero. Likewise, data collected during the preintervention phase also identified previously defined disposition delays, similar to those previously published, including delays in de-escalation of care in patients who were determined to have a futile prognosis, where the availability of a floor bed was low, or surgeon refusal when the patient was considered to be stable for transfer by the SICU team. These delays were also considered to be potentially avoidable and targeted for reduction. Additional sources for potentially avoidable days due to admissions and disposition delays were identified by the rounding SICU team and categorized as other for this study. If an admission was potentially avoidable and a disposition delay was also noted, the overlapping days were subtracted from the total potentially avoidable days. An additional retrospective review of cases was conducted to better identify and quantify avoidable SICU days.
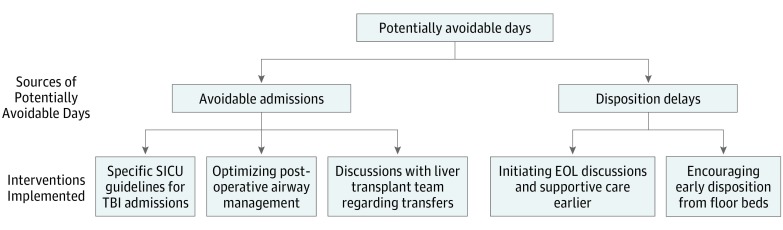
Based on preintervention data, specific targeted interventions were created and implemented during the intervention phase (Figure 2), specifically focusing on the 2 surgical services that consumed the most days. The following interventions targeted potentially avoidable admissions:
Figure 2. Interventions Designed and Implemented.
EOL indicates end of life; SICU, surgical intensive care unit; and TBI, traumatic brain injury.
We created specific SICU admission guidelines for patients being admitted from the trauma surgery service with TBI. These updated admission criteria for patients with TBI were based on modifications to the brain injury guidelines, which allowed the attending physician discretion in the admission of patients with TBI to the floor, when previously they were admitted to the SICU for short observation (eTable in Supplement).
We instituted feedback with anesthesia leadership for patients admitted to the SICU who were immediately extubated and ready for transfer out of the SICU. Postoperative airway management was specifically addressed by holding periodic meetings with the anesthesia department and reinforcing proper disposition and airway management before leaving the operating room or recovery in the postanesthesia care unit.
We initiated monthly group meetings with the SICU and liver transplant services that led to direct SICU communication before acceptance of patients from other hospitals.
Disposition delays with all services were addressed by initiating EOL discussions and mandating supportive care consultation. In addition, admitting surgical services were encouraged to transfer patients to the floor during morning rounds, and downstream floor beds were reviewed during weekly meetings with case managers and a physician representative to address sources for discharge delays.
Data were analyzed using SPSS statistical software (version 23 for Windows; IBM Corp) and are summarized as numbers (percentages) for categorical variables and medians with interquartile range (IQR) for continuous variables. Comparisons of medians were conducted using the Mann-Whitney test. All variables were noted to be nonparametric. Categorical variables and proportions were compared using Pearson χ2 test or Fisher exact test where appropriate. P < .05 was considered statistically significant.
Results
A total of 459 patients (253 men [55.1%] and 206 women [44.9%]; median age, 62 years [IQR, 46-75 years]) with 506 admissions were included in the analysis. During the preintervention period, 233 patients (120 men [51.5%] and 113 women [48.5%]; median age, 62 years [IQR, 45-76 years]) had 261 admissions; during the postintervention period, 226 patients (133 men [58.8%] and 93 women [41.2%]; median age, 62 years [IQR, 46-73 years]) had 245 admissions. The preintervention and postintervention cohorts were comparable with respect to median age, sex, Acute Physiology and Chronic Health Evaluation IV scores, ventilator days, vasopressor use, mechanical ventilation, SICU mortality, and hospital mortality (Table 1). Median SICU LOS remained unchanged in the postintervention period (2 days [IQR, 1-4 days] vs 2 days [IQR, 1-6 days]; P = .07), as did median hospital LOS (9 days [IQR, 5-17 days] vs 9 days [IQR, 6-17 days]; P = .38). The readmission rate to the SICU within 48 hours after transfer and at any point during the patient’s hospital stay did not change.
Table 1. Characteristics of Preintervention and Postintervention Cohorts.
| Variable | Study Cohorta | P Valueb | |
|---|---|---|---|
| Preintervention (n = 233) |
Postintervention (n = 226) |
||
| Age, median (IQR), y | 62 (45-76) | 62 (46-73) | .67 |
| Male | 120 (51.5) | 133 (58.8) | .11 |
| APACHE IV score, median (IQR)c | 14.33 (4.09-33.23) | 14.38 (4.83-29.17) | .79 |
| Postoperative SICU stay | 173 (74.2) | 174 (77.0) | .49 |
| Required vasopressors | 58 (24.9) | 56 (24.8) | .98 |
| Required mechanical ventilation | 99 (42.5) | 87 (38.5) | .38 |
| Duration of ventilation, median (IQR), dd | 3 (1-7) | 3 (1-9) | .85 |
| Required readmission at any time | 17 (7.3) | 13 (5.8) | .50 |
| Required readmission within 48 h | 8 (3.4) | 4 (1.8) | .26 |
| SICU mortality | 18 (7.7) | 19 (8.4) | .79 |
| Hospital mortality | 18 (7.7) | 21 (9.3) | .55 |
| SICU LOS, median (IQR), de | 2 (1-4) | 2 (1-6) | .07 |
| Hospital LOS, median (IQR), d | 9 (5-17) | 9 (6-17) | .38 |
Abbreviations: APACHE IV, Acute Physiology and Chronic Health Evaluation; IQR, interquartile range; LOS, length of stay; SICU, surgical intensive care unit.
Unless otherwise indicated, data are expressed as number (percentage) of patients.
Comparisons of medians were conducted using the Mann-Whitney test; for categorical variables and proportions, Pearson χ2 test or Fisher exact test was used where appropriate.
Scores range from 0 to 286, with higher scores indicating a higher likelihood of mortality.
Includes those patients who required mechanical ventilation.
Readmissions to the SICU are included in this calculation.
A reduction was noted during the postintervention period (Table 2) in the rate of SICU days attributed to potentially avoidable admissions (152 of 1168 days [13%] vs 118 of 1338 days [8.8%]; P = .001) and disposition delays (138 of 1168 days [11.8%] vs 97 of 1338 days [7.2%]; P < .001). The 3 most common sources for SICU days due to potentially avoidable admissions decreased significantly during the postintervention period: ICU stay of 24 hours or less (84 of 1168 days [7.2%] vs 66 of 1338 days [4.9%]; P = .02), airway concerns (32 of 1168 days [2.7%] vs 9 of 1338 days [0.7%]; P < .001), and somnolence (7 of 1168 days [0.6%] vs 0 of 1138 days; P < .001). The 2 most common sources of SICU days due to potentially avoidable disposition delays also decreased in the postintervention period: EOL decisions (66 of 1168 days [5.7%] vs 0 of 1338 days; P < .001) and floor bed unavailability (46 of 1168 days [3.9%] vs 33 of 1338 days [2.5%]; P = .04). An increase was noted in the rate of potentially avoidable days due to surgeon preference that the patient remain in the SICU (12 of 1168 days [1%] vs 35 of 1338 days [2.6%]; P < .001). After accounting for the SICU days that were attributable to potentially avoidable admissions and disposition delays, an overall reduction was noted in the rate of potentially avoidable days during the postintervention period (269 of 1168 days [23.0%] vs 205 of 1338 days [15.3%]; P < .001).
Table 2. Sources for Potentially Avoidable Admissions and Disposition Delays in Preintervention and Postintervention Cohorts.
| Source of Potentially Avoidable Days | SICU Days, No. (%)a | P Valueb | |
|---|---|---|---|
| Preintervention Cohort (n = 1168) |
Postintervention Cohort (n = 1338) |
||
| Potentially avoidable admissions | 152 (13.0) | 118 (8.8) | .001 |
| SICU stay ≤24 h | 84 (7.2) | 66 (4.9) | .02 |
| Airway concerns | 32 (2.7) | 9 (0.7) | <.001 |
| Somnolence | 7 (0.6) | 0 | <.001 |
| Other | 29 (2.5) | 43 (3.2) | .28 |
| Disposition delays | 138 (11.8) | 97 (7.2) | <.001 |
| EOL decisions | 66 (5.7) | 1 (0.07) | <.001 |
| Floor bed unavailable | 46 (3.9) | 33 (2.5) | .04 |
| Surgeon preference | 12 (1.0) | 35 (2.6) | <.001 |
| Other | 14 (1.2) | 28 (2.1) | .003 |
| Potentially avoidable admissions and disposition delays | 21 (1.8) | 10 (0.7) | .02 |
| Totalc | 269 (23.0) | 205 (15.3) | <.001 |
Abbreviations: EOL, end of life; SICU, surgical intensive care unit.
All percentages are reported relative to total intensive care unit days (appropriate and potentially avoidable).
Calculated using Pearson χ2 test or Fisher exact test where appropriate.
Calculated by adding potentially avoidable days due to potentially avoidable admissions and potentially avoidable days due to disposition delays and then subtracting overlapping days (those potentially avoidable days due to potentially avoidable admissions and disposition delays) to avoid overcounting.
The trauma and liver transplant surgical services were responsible for most SICU days (Table 3). Although the percentage of days for the trauma surgical service associated with potentially avoidable admissions was unchanged in postintervention compared with preintervention phases (24 of 376 days [6.4%] vs 17 of 248 days [6.9%]; P = .82), the percentage of days due to potentially avoidable disposition delays decreased (57 of 376 preintervention days [15.2%] vs 23 of 248 postintervention days [9.3%]; P = .03). During the postintervention period, the liver transplant surgical service noted decreases in the rate of SICU days attributed to potentially avoidable admissions (14 of 242 days [5.8%] vs 2 of 319 days [0.6%]; P < .001) and disposition delays (20 of 242 days [8.3%] vs 9 of 319 days [2.8%]; P = .004). In comparison, the general surgical service was not directly targeted for reducing potentially avoidable SICU days. No change was observed in SICU days due to potentially avoidable disposition delays (3 of 88 days [3.4%] vs 2 of 154 days [1.3%]; P = .36), whereas those attributed to potentially avoidable admissions decreased (25 of 88 days [28.4%] vs 15 of 154 days [9.7%]; P < .001).
Table 3. Comparison of Potentially Avoidable Admissions and Disposition Delays in Preintervention and Postintervention Cohorts by Surgical Service.
| Surgical Service | Preintervention Cohort | Postintervention Cohort | P Valuea |
|---|---|---|---|
| Trauma | |||
| Total SICU days | 376 | 248 | NA |
| SICU LOS, median (IQR), d | 2 (1-4) | 2 (1-6) | .55 |
| No. of SICU admissions | 82 | 54 | NA |
| Potentially avoidable admissions, No. (%) | 28 (34.1) | 16 (29.6) | .58 |
| Potentially avoidable days due to potentially avoidable admissions, No. (%) | 24 (6.4) | 17 (6.9) | .82 |
| Potentially avoidable days due to disposition delays, No. (%) | 57 (15.2) | 23 (9.3) | .03 |
| Liver transplant | |||
| Total SICU days, d | 242 | 319 | NA |
| SICU LOS, median (IQR), d | 5 (2-8) | 6 (3-14) | .31 |
| No. of SICU admissions | 30 | 31 | NA |
| Potentially avoidable admissions, No. (%) | 7 (23.3) | 2 (6.5) | .08 |
| Potentially avoidable days due to potentially avoidable admissions, No. (%) | 14 (5.8) | 2 (0.6) | <.001 |
| Potentially avoidable days due to disposition delays, No. (%) | 20 (8.3) | 9 (2.8) | .004 |
| Thoracic | |||
| Total SICU days, d | 153 | 87 | NA |
| SICU LOS, median (IQR), d | 2.5 (1-5) | 2 (1-5) | .86 |
| No. of SICU admissions | 26 | 24 | NA |
| Potentially avoidable admissions, No. (%) | 14 (53.8) | 8 (33.3) | .14 |
| Potentially avoidable days due to potentially avoidable admissions, No. (%) | 22 (14.4) | 9 (10.3) | .37 |
| Potentially avoidable days due to disposition delays, No. (%) | 15 (9.8) | 10 (11.5) | .68 |
| General | |||
| Total SICU days, d | 88 | 154 | NA |
| SICU LOS, median (IQR), d | 2 (1-3.5) | 2.5 (1-8) | .24 |
| No. of SICU admissions | 21 | 24 | NA |
| Potentially avoidable admissions, No. (%) | 12 (57.1) | 9 (37.5) | .19 |
| Potentially avoidable days due to potentially avoidable admissions, No. (%) | 25 (28.4) | 15 (9.7) | <.001 |
| Potentially avoidable days due to disposition delays, No. (%) | 3 (3.4) | 2 (1.3) | .36 |
| Hepatobiliary | |||
| Total SICU days, d | 62 | 269 | NA |
| SICU LOS, median (IQR), d | 2 (1-3) | 3 (2-8) | .049 |
| No. of SICU admissions | 23 | 31 | NA |
| Potentially avoidable admissions, No. (%) | 9 (39.1) | 7 (22.6) | .19 |
| Potentially avoidable days due to potentially avoidable admissions, No. (%) | 11 (17.7) | 9 (3.3) | <.001 |
| Potentially avoidable days due to disposition delays, No. (%) | 7 (11.3) | 21 (7.8) | .37 |
| Orthopedic | |||
| Total SICU days, d | 29 | 30 | NA |
| SICU LOS, median (IQR), d | 1 (1-3) | 1.5 (1-4) | .82 |
| No. of SICU admissions | 12 | 10 | NA |
| Potentially avoidable admissions, No. (%) | 8 (66.7) | 3 (30.0) | .09 |
| Potentially avoidable days due to potentially avoidable admissions, No. (%) | 9 (31) | 3 (10) | .045 |
| Potentially avoidable days due to disposition delays, No. (%) | 7 (24.1) | 1 (3.3) | .03 |
| Vascular | |||
| Total SICU days, d | 25 | 62 | NA |
| SICU LOS, median (IQR), d | 1 (1-4) | 2 (1-3) | .45 |
| No. of SICU admissions | 11 | 20 | NA |
| Potentially avoidable admissions, No. (%) | 6 (54.5) | 12 (60.0) | >.99 |
| Potentially avoidable days due to potentially avoidable admissions, No. (%) | 5 (20.0) | 24 (38.7) | .09 |
| Potentially avoidable days due to disposition delays, No. (%) | 2 (8.0) | 11 (17.7) | .33 |
| Plastic | |||
| Total SICU days, d | 16 | 11 | NA |
| SICU LOS, median (IQR), d | 1 (1-3) | 1 (1-4) | >.99 |
| No. of SICU admissions | 9 | 5 | NA |
| Potentially avoidable admissions, No. (%) | 6 (66.7) | 4 (80.0) | >.99 |
| Potentially avoidable days due to potentially avoidable admissions, No. (%) | 8 (50.0) | 5 (45.5) | .82 |
| Potentially avoidable days due to disposition delays, No. (%) | 2 (12.5) | 0 | .50 |
| Otherb | |||
| Total SICU days, d | 177 | 158 | NA |
| SICU LOS, median (IQR), d | 2 (1-3) | 2 (1-3) | .65 |
| No. of SICU admissions | 47 | 46 | NA |
| Potentially avoidable admissions, No. (%) | 24 (51.1) | 22 (47.8) | .76 |
| Potentially avoidable days due to potentially avoidable admissions, No. (%) | 34 (19.2) | 34 (21.5) | .60 |
| Potentially avoidable days due to disposition delays, No. (%) | 25 (14.1) | 20 (12.7) | .69 |
Abbreviations: IQR, interquartile range; LOS, length of stay; NA, not applicable; SICU, surgical intensive care unit.
Calculated using Pearson χ2 test or Fisher exact test where appropriate for categorical variables and Mann-Whitney test for continuous variables.
Includes colorectal surgery, interventional radiology, kidney transplant surgery, obstetrics and gynecology, otolaryngology, pancreas transplant surgery, surgical oncology, and urology.
Discussion
To better understand the reasons for an extended patient LOS in the SICU, we created the term potentially avoidable SICU days to define admission or disposition delays that might be preventable. Potentially avoidable rather than avoidable reduces the emphasis on whether the SICU day should be defined as unnecessary and instead encourages the review of any SICU day that might not have been required. In the initial observation period, we determined that 23.0% of patient days in the SICU were considered potentially avoidable, and we were able to reduce this proportion to 15.3% during the postintervention period by identifying their sources and then targeting them for improvement. These interventions focused on reducing potentially avoidable admissions and disposition delays and included (1) reducing SICU care for minor TBI, (2) optimizing postoperative airway management, (3) enhancing communication between services regarding transfers to the SICU, (4) identifying and facilitating more timely EOL conversations and supportive care consultations, and (5) encouraging early disposition of patients to floor beds. The specific interventions were tailored to the services that used the most SICU days initially and the common reasons for potentially avoidable admissions or disposition delays.
The literature on appropriate placement of patients indicates a high frequency of avoidable admissions in varied ICU settings. Inappropriate admissions to the ICU appear to stem from external factors, such as pressure from superiors, referring clinicians, and administrators. This finding suggests that factors other than the clinician’s perception of a patient’s condition may contribute to the inflow of potentially avoidable admissions. At ICU admission, many patients do not require an ICU level of care. For example, in an audit of postoperative ICU admissions, 35.8% of patients did not receive any ICU-specific interventions. Disposition delays are also common and occur in up to two-thirds of ICU admissions, with the most common cause being lack of downstream resources, such as surgical floor beds. Other factors reflecting organizational infrastructure, such as a lack of communication or coordination, appear to play a role. Intensive care unit disposition delays lead to an overall increase in hospital LOS.
In our study, we did not observe a reduction in SICU or hospital LOS related to our research, although this decrease was neither expected nor a focus of our project. By concentrating on potentially avoidable SICU admissions and disposition delays, we reduced admissions for patients who had short stays and the disposition delays for patients with long stays. When patients who require short stays in the SICU are admitted instead to ward beds, the median ICU length of the SICU stay will increase. Because we also reduced disposition delays, the overall outcome of our research was that no net change in the median SICU stay was observed. Had the aim of this research been reduction of the median SICU stay, the focus might have been only on reducing disposition delays. Because SICU mortality (7.7% [18 patients] in the preintervention phase vs 8.4% [19 patients] in the postintervention phase; P = .79), hospital mortality (7.7% [18 patients] in the preintervention phase vs 9.3% [21 patients] in the postintervention phase; P = .55), and readmission rates (7.3% [17 patients] in the preintervention phase vs 5.8% [13 patients] in the postintervention phase; P = .50) were not affected by the interventions, earlier disposition did not appear to alter patient mortality or readmission rates.
Patients with TBI who were admitted to the SICU constituted a substantial number of admissions by the trauma service during the preintervention phase. Because the SICU is staffed by intensivists who are also members of the trauma service, changes regarding TBI admission pathways were readily accepted. Members of the neurosurgery team also provided input regarding the appropriate placement of patients with brain injury in the trauma service. During the postintervention period, fewer patients from the trauma service required SICU admission; however, no reduction in the rate of potentially avoidable admissions was observed. This lack of significance may be attributable to how TBI admissions were categorized. An admission to the SICU of a patient with TBI was considered justifiable if the stay lasted more than 24 hours, but it would then be considered a disposition delay if no bed was available when the patient was cleared for transfer. During the preintervention period, many patients admitted for TBI were ready for transfer soon after 24 hours, and these admissions generated potentially avoidable SICU days due to a disposition delay rather than potentially avoidable admissions. Because fewer patients with TBI were admitted during the postintervention period, a significant reduction in potentially avoidable SICU days was observed because of a decrease in disposition delays.
Our analysis revealed that a major source of potentially avoidable disposition delays stemmed from EOL decision making. A disproportionate share of health care costs are attributed to the care of patients shortly before their deaths, and costs for these patients correlate with the duration that they remain in the ICU. The SUPPORT (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment) results demonstrate that despite applying interventions that were intended to improve EOL care, patients often spent several days in the ICU in a comatose state before death, despite do-not-resuscitate orders often being written, on average, 2 days before death. This finding suggests some degree of inconsistency between a patient’s status and how the prognosis is perceived by clinicians, family members, or both. Palliative care screening has been proposed to ameliorate this issue. Zalenski et al suggest that hospitals can decrease ICU LOS and reduce costs when all patients in the ICU undergo palliative care screening with subsequent consultation. Preintervention analysis in our study revealed that many of our patients who required EOL discussions came from the liver transplant surgical service; thus, communication between this service and the SICU team helped identify specific patients who warranted supportive care consultations. During the postintervention period, most patients had supportive care consultation, including all patients admitted before liver transplant, which reduced the percentage of potentially avoidable days due to disposition delays that were categorized as related to EOL decisions.
Limitations
Our investigation has some limitations, as revealed by its design and results. The interventions created were customized to our patient population and their associated diagnoses. Thus, the effect of the interventions executed in our study may not be similar when applied to other settings in which the patient population and ICU staffing may differ. The open model in our ICU also may have undermined efforts to reduce potentially avoidable days, as evidenced by the increase in potentially avoidable days secondary to disposition delays due to surgeon preference. One may speculate that different results may have been observed in a closed unit. Conversely, much of the decrease in the rate of potentially avoidable admissions and disposition delays may have been attributable to the institution’s open SICU model. A closed SICU where the intensivist has authority over all admissions and discharges might have different results. In addition, although a large tertiary center may be able to accommodate patients with unique or critical illness in ward beds or step-down units, smaller community hospitals may not be able to make such accommodations. Restricting ICU access to smaller hospitals may be associated with adverse events.
The patients who might have been admitted to the SICU during the preintervention phase but were diverted to other areas during the postintervention phase were not tracked, and therefore, no preventable morbidity or mortality can be provided for this population. Our results also indicate that the median LOS in the SICU did not change after the application of our interventions. This lack of change may in part be attributable to the reduction in patients who were admitted to the SICU for less than 24 hours, such that a significant reduction in median LOS might not be realized. How potentially avoidable days were characterized could differ between observer or rounding intensivist on a day-to-day basis and during the preintervention and postintervention periods. Sources of potentially avoidable days, in addition to avoidable admission or disposition delay, were not accounted for in the study methods. Further analysis is required to explore these limitations.
Conclusions
Although nearly one-quarter of SICU days could be categorized as potentially avoidable, a reduction was noted through targeted interventions focused on short anesthesia-related admissions, service-dependent challenges, downstream bed availability, and EOL care. Addressing potentially avoidable admissions and disposition delays by creating specific admission guidelines, improving hand-off communication with various teams, and encouraging earlier EOL conversations and disposition of floor patients may reduce inappropriate SICU use.
eTable. Criteria for Admission for Patients With Traumatic Brain Injury
References
- 1.Centers for Medicare & Medicaid Services. NHE Fact Sheet. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet.html. Published August 10, 2016. Accessed October 5, 2016.
- 2.Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513-1516. [DOI] [PubMed] [Google Scholar]
- 3.Hammond DA, Kathe N, Shah A, Martin BC. Cost-effectiveness of histamine2 receptor antagonists vs proton pump inhibitors for stress ulcer prophylaxis in critically ill patients [published online December 20, 2016]. Pharmacotherapy. doi: 10.1002/phar.1859 [DOI] [PubMed] [Google Scholar]
- 4.Morgan DJ, Dhruva SS, Wright SM, Korenstein D. 2016 update on medical overuse: a systematic review. JAMA Intern Med. 2016;176(11):1687-1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colla CH, Kinsella EA, Morden NE, Meyers DJ, Rosenthal MB, Sequist TD. Physician perceptions of Choosing Wisely and drivers of overuse. Am J Manag Care. 2016;22(5):337-343. [PubMed] [Google Scholar]
- 6.Kirton OC, Civetta JM, Hudson-Civetta J. Cost effectiveness in the intensive care unit. Surg Clin North Am. 1996;76(1):175-200. [DOI] [PubMed] [Google Scholar]
- 7.Baigelman W, Bellin SJ, Cupples LA, Dombrowski D, Coldiron J. Overutilization of serum electrolyte determinations in critical care units: savings may be more apparent than real but what is real is of increasing importance. Intensive Care Med. 1985;11(6):304-308. [DOI] [PubMed] [Google Scholar]
- 8.Jordan KG. Continuous EEG and evoked potential monitoring in the neuroscience intensive care unit. J Clin Neurophysiol. 1993;10(4):445-475. [DOI] [PubMed] [Google Scholar]
- 9.Vlayen A, Verelst S, Bekkering GE, Schrooten W, Hellings J, Claes N. Exploring unplanned ICU admissions: a systematic review. JBI Libr Syst Rev. 2011;9(25):925-959. [DOI] [PubMed] [Google Scholar]
- 10.Luce JM, Rubenfeld GD. Can health care costs be reduced by limiting intensive care at the end of life? Am J Respir Crit Care Med. 2002;165(6):750-754. [DOI] [PubMed] [Google Scholar]
- 11.Giannini A, Consonni D. Physicians’ perceptions and attitudes regarding avoidable admissions and resource allocation in the intensive care setting. Br J Anaesth. 2006;96(1):57-62. [DOI] [PubMed] [Google Scholar]
- 12.Chang DW, Shapiro MF. Association between intensive care unit utilization during hospitalization and costs, use of invasive procedures, and mortality. JAMA Intern Med. 2016;176(10):1492-1499. [DOI] [PubMed] [Google Scholar]
- 13.Hernu R, Cour M, de la Salle S, Robert D, Argaud L; Costs in French ICU Study Group . Cost awareness of physicians in intensive care units: a multicentric national study [published correction appears in Intensive Care Med. 2016;42(8):1312]. Intensive Care Med. 2015;41(8):1402-1410. [DOI] [PubMed] [Google Scholar]
- 14.Huynh TN, Kleerup EC, Raj PP, Wenger NS. The opportunity cost of futile treatment in the ICU. Crit Care Med. 2014;42(9):1977-1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fenton SJ, Campbell SJ, Stevens AM, Zhang C, Presson AP, Lee JH. Preventable pediatric intensive care unit admissions over a 13-year period at a level 1 pediatric trauma center. J Pediatr Surg. 2016;51(10):1688-1692. [DOI] [PubMed] [Google Scholar]
- 16.Almoosa KF, Luther K, Resar R, Patel B. Applying the New Institute for Healthcare Improvement Inpatient Waste Tool to identify “waste” in the intensive care unit. J Healthc Qual. 2016;38(5):e29-e38. [DOI] [PubMed] [Google Scholar]
- 17.Khandelwal N, Benkeser D, Coe NB, Engelberg RA, Teno JM, Curtis JR. Patterns of cost for patients dying in the intensive care unit and implications for cost savings of palliative care interventions. J Palliat Med. 2016;19(11):1171-1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daly B, Hantel A, Wroblewski K, et al. No exit: identifying avoidable terminal oncology intensive care unit hospitalizations. J Oncol Pract. 2016;12(10):e901-e911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shine NP, Coates HL, Lannigan FJ, Duncan AW. Adenotonsillar surgery in morbidly obese children: routine elective admission of all patients to the intensive care unit is unnecessary. Anaesth Intensive Care. 2006;34(6):724-730. [DOI] [PubMed] [Google Scholar]
- 20.Mirghani HM, Hamed M, Ezimokhai M, Weerasinghe DSL. Pregnancy-related admissions to the intensive care unit. Int J Obstet Anesth. 2004;13(2):82-85. [DOI] [PubMed] [Google Scholar]
- 21.Davison G, Suchman AL, Goldstein BJ. Reducing unnecessary coronary care unit admissions: a comparison of three decision aids. J Gen Intern Med. 1990;5(6):474-479. [DOI] [PubMed] [Google Scholar]
- 22.Joseph B, Friese RS, Sadoun M, et al. The BIG (Brain Injury Guidelines) Project: defining the management of traumatic brain injury by acute care surgeons. J Trauma Acute Care Surg. 2014;76(4):965-969. [DOI] [PubMed] [Google Scholar]
- 23.Osinaike BB, Olusanya O. Inappropriate intensive care unit admissions: Nigerian doctors’ perception and attitude. Niger J Clin Pract. 2016;19(6):721-724. [DOI] [PubMed] [Google Scholar]
- 24.Swann D, Houston P, Goldberg J. Audit of intensive care unit admissions from the operating room. Can J Anaesth. 1993;40(2):137-141. [DOI] [PubMed] [Google Scholar]
- 25.Peltonen L-M, McCallum L, Siirala E, et al. An integrative literature review of organisational factors associated with admission and discharge delays in critical care. Biomed Res Int. 2015;2015:868653. [DOI] [PMC free article] [PubMed]
- 26.Johnson DW, Schmidt UH, Bittner EA, Christensen B, Levi R, Pino RM. Delay of transfer from the intensive care unit: a prospective observational study of incidence, causes, and financial impact. Crit Care. 2013;17(4):R128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lubitz JD, Riley GF. Trends in Medicare payments in the last year of life. N Engl J Med. 1993;328(15):1092-1096. [DOI] [PubMed] [Google Scholar]
- 28.Maltoni M, Scarpi E, Dall’Agata M, et al. ; Early Palliative Care Italian Study Group (EPCISG) . Systematic versus on-demand early palliative care: a randomised clinical trial assessing quality of care and treatment aggressiveness near the end of life. Eur J Cancer. 2016;69:110-118. [DOI] [PubMed] [Google Scholar]
- 29.Bramley T, Antao V, Lunacsek O, Hennenfent K, Masaquel A. The economic burden of end-of-life care in metastatic breast cancer. J Med Econ. 2016;19(11):1075-1080. [DOI] [PubMed] [Google Scholar]
- 30.Chaix C, Durand-Zaleski I, Alberti C, Brun-Buisson C. A model to compute the medical cost of patients in intensive care. Pharmacoeconomics. 1999;15(6):573-582. [DOI] [PubMed] [Google Scholar]
- 31.The SUPPORT Principal Investigators A controlled trial to improve care for seriously ill hospitalized patients: the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT). JAMA. 1995;274(20):1591-1598. [PubMed] [Google Scholar]
- 32.Waite K, Rhule J, Bush D, Meisenberg B. End-of-life care patterns at a community hospital: the rest of the story [published online October 2016]. Am J Hosp Palliat Care. doi: 10.1177/1049909116673300 [DOI] [PubMed] [Google Scholar]
- 33.Zalenski RJ, Jones SS, Courage C, et al. Impact of palliative care screening and consultation in the ICU: a multi-hospital quality improvement project. J Pain Symptom Manage. 2017;53(1):5-12.e3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Criteria for Admission for Patients With Traumatic Brain Injury