Key Points
Question
In patients who present to the emergency department with chest pain without evidence of ischemia, is cardiac testing—noninvasive testing or coronary angiography—associated with changes in revascularization or acute myocardial infarction (AMI) admissions?
Findings
In a retrospective cohort analysis of 926 633 patients, we used the day of presentation as an instrumental variable to adjust for potential selection bias. Cardiac testing was associated with increased revascularization without a significant change in AMI admissions.
Meaning
Routine testing may increase resource utilization without improving outcomes in patients who present to the emergency department with chest pain without evidence of ischemia.
Abstract
Importance
Noninvasive testing and coronary angiography are used to evaluate patients who present to the emergency department (ED) with chest pain, but their effects on outcomes are uncertain.
Objective
To determine whether cardiovascular testing—noninvasive imaging or coronary angiography—is associated with changes in the rates of coronary revascularization or acute myocardial infarction (AMI) admission in patients who present to the ED with chest pain without initial findings of ischemia.
Design, Setting, and Participants
This retrospective cohort analysis used weekday (Monday-Thursday) vs weekend (Friday-Sunday) presentation as an instrument to adjust for unobserved case-mix variation (selection bias) between 2011 and 2012. National claims data (Truven MarketScan) was used. The data included a total of 926 633 privately insured patients ages 18 to 64 years who presented to the ED with chest pain without initial diagnosis consistent with acute ischemia.
Exposures
Noninvasive testing or coronary angiography within 2 days or 30 days of presentation.
Main Outcomes and Measures
The primary end points were coronary revascularization (percutaneous coronary intervention or coronary artery bypass graft surgery) and AMI admission at 7, 30, 180, and 365 days. The secondary end points were coronary angiography and coronary artery bypass grafting in those who underwent angiography.
Results
The patients were ages 18 to 64 years with an average age of 44.4 years. A total of 536 197 patients (57.9%) were women. Patients who received testing (224 973) had increased risk at baseline and had greater risk of AMI admission than those who did not receive testing (701 660) (0.35% vs 0.14% at 30 days). Weekday patients (571 988) had similar baseline comorbidities to weekend patients (354 645) but were more likely to receive testing. After risk factor adjustment, testing within 30 days was associated with a significant increase in coronary angiography (36.5 per 1000 patients tested; 95% CI, 21.0-52.0) and revascularization (22.8 per 1000 patients tested; 95% CI, 10.6-35.0) at 1 year but no significant change in AMI admissions (7.8 per 1000 patients tested; 95% CI, −1.4 to 17.0). Testing within 2 days was also associated with a significant increase in coronary revascularization but no difference in AMI admissions.
Conclusions and Relevance
Cardiac testing in patients with chest pain was associated with increased downstream testing and treatment without a reduction in AMI admissions, suggesting that routine testing may not be warranted. Further research into whether specific high-risk subgroups benefit from testing is needed.
This cohort analysis evaluates clinical outcomes of the association of cardiovascular testing with patients who present to the emergency department with chest pain.
Introduction
Each year, more than 6 million patients present to emergency departments (EDs) in the United States with acute chest pain. Most—after initial evaluation with cardiac enzymes and an electrocardiogram—lack evidence of acute ischemia. However, given the morbidity of missed diagnoses, the American Heart Association (AHA) recommends noninvasive cardiac testing for inducible ischemia (exercise electrocardiogram [ECG], stress echocardiography, nuclear stress test) or anatomical coronary artery disease (coronary computed tomographic [CT] angiography) prior to discharge or within 72 hours. Patients with positive noninvasive testing typically undergo coronary angiography. High-risk patients may proceed directly to angiography even in the absence of objectively verified ischemia. Cardiovascular testing is costly and time-intensive. Moreover, it is unclear whether current practice reduces the risk of future cardiovascular events in patients without evidence of acute ischemia.
Past observational analyses have shown that noninvasive testing is associated with large increases in downstream testing and treatment without a reduction in subsequent acute myocardial infarction (AMI) admissions. Accordingly, some have suggested that the current practice should be modified. However, patients who receive testing are higher risk, raising concerns about residual confounding. In previous work, patients who underwent noninvasive testing were older with more comorbidities. Although the study adjusted for these differences, the 2 groups likely also differed in characteristics not captured in claims data, such as chest pain severity or electrocardiogram findings.
We used an instrumental-variables approach to reduce potential unmeasured confounding. Patients presenting on weekdays are more likely to receive testing owing to the resource-intensive nature of testing, but unmeasured patient characteristics—affecting treatment and outcomes—are less likely to vary across the week. This approach has been used to adjust for unobserved case-mix variation in other acute conditions in which the timing of presentation is unrelated to patient characteristics but predicts the receipt of intensive interventions. We used the day of the week of presentation—weekday vs weekend—as an instrumental variable to study the association between cardiovascular testing (noninvasive testing or coronary angiography) and the risk of revascularization and AMI admissions in patients who present to the ED with chest pain without initial evidence of acute ischemia.
Methods
Data
We analyzed MarketScan Commercial Claims and Encounters (Truven Health Analytics) data from January 1, 2010, to December 31, 2013. This database includes inpatient, outpatient, and pharmaceutical claims of more than 75 million employees, retirees, and dependents from more than 150 payers across all states. We selected all ED visits between 2011 and 2012 for those ages 18 to 64 years. Diagnoses and procedures were coded using International Classification of Diseases, Ninth Revision (ICD-9-CM), diagnosis-related groups (DRGs), and Current Procedural Terminology (CPT) (see eTable 1 in the Supplement for codes used).
Cohort
We identified a cohort of ED patients in 2011 to 2012 with a diagnosis of chest pain or angina pectoris among patients ages 18 to 64 (eFigure in the Supplement). We excluded patients with diagnoses that suggest evidence of acute ischemia: AMI, intermediate coronary syndrome, acute coronary syndrome without coronary occlusion, and other acute ischemic heart disease. We excluded patients with alternate cardiopulmonary diagnoses made in the ED that could explain chest pain (eFigure in the Supplement). Finally, we excluded patients with capitated health care plans who may have incomplete data capture. The study sample included 926 633 unique adult ED visits for chest pain in 2011 to 2012. The reasons for exclusion were similar on weekdays and weekends (eTable 2 in the Supplement). Because the analysis includes only analysis of secondary deidentified data, it does not meet the Stanford University or National Institutes of Health definition of human subject research requiring institutional review board approval.
Measures
We determined if patients underwent testing within 2 or 30 calendar days following their ED visit. We used a 2-day cutoff to analyze testing that would occur within 72 hours of the ED visit as per AHA guidelines. The 30-day cutoff was intended to include all testing that was performed as a result of the ED visit. Testing included coronary angiography or noninvasive testing: exercise electrocardiography, stress echocardiography, myocardial perfusion scan, or CT coronary angiography.
The primary outcomes were subsequent AMI admission and coronary revascularization—defined as either percutaneous coronary intervention or coronary artery bypass graft (CABG) surgery. We extracted outcome data at 7 days, 30 days, 180 days, and 1 year after the ED visit. Each time point was used as an outcome for testing within 2 days; outcomes at 180 and 365 days were used for testing within 30 days. We also assessed coronary angiography to determine if testing increased the use of angiography long-term or if those without initial testing underwent deferred angiography. Subsequent AMI admission is a measure of health outcomes, whereas angiography and revascularization are indicators of downstream resource use.
We established prior risk factors using claims from the year prior to ED presentation. We identified a history of diabetes, hypertension, hyperlipidemia, chronic kidney disease, peripheral vascular disease, cerebrovascular disease, or tobacco use based on their respective ICD-9-CM diagnoses or a claim for a disease-related medication using the databases’ therapeutic classes. We identified a history of ischemic heart disease with a prior diagnosis of MI or ischemic heart disease. We determined if patients were receiving antiplatelet therapy or antihyperlipidemic agents. We ascertained previous outpatient and inpatient cardiology evaluation using CPT codes from the year prior to presentation.
Statistical Analysis
We compared patient characteristics and unadjusted outcomes between cohorts using the 2-sample t test for continuous variables and the χ2 test for categorical variables. We performed 2-tailed hypothesis testing with an α = .05. We also used Cohen d (standardized mean difference) to evaluate the magnitude of cohort differences with a cutoff of 0.1 considered meaningful. We used STATA statistical software (version 14.1; StataCorp).
We used multivariable logistic regression to adjust for age, sex, hypertension, diabetes, hyperlipidemia, ischemic heart disease, chronic kidney disease, cerebrovascular disease, peripheral vascular disease, tobacco use, noninvasive testing in the preceding year, coronary angiography in the preceding year, previous antiplatelet medication use, and previous antihyperlipidemic medication use. We present the results as the average marginal effect of a change in testing in 1000 patients.
The instrumental variables analysis is intended to reduce residual confounding in the estimated treatment effect by comparing patients stratified by an instrument: a variable that predicts receipt of the treatment (cardiac testing) but is uncorrelated with observed and unobserved patient characteristics (ie, electrocardiogram changes). Acute chest pain is an emergent condition, so baseline risk is unlikely to affect the day of the week of presentation, as seen in similar acute conditions. Hospitals have decreased testing availability on weekends, causing some weekend patients to not receive testing that would be received on a weekday. We evaluated the validity of the instrument using 2 criteria: the day of presentation predicted testing (strength of instrument) and was independent of observable patient characteristics, suggesting independence of unobservable characteristics (exclusion restriction).
We performed 2-stage residual inclusion multivariable logistic regression with weekend (Friday-Sunday) presentation as an instrumental variable. This is an effective statistical approach when unobserved confounding is a potential problem. We first used multivariable logistic regression to model the effect of weekend presentation on testing—with the same covariates as the noninstrumented analysis—and calculated residuals. We then regressed each outcome on testing, including the residuals as an additional covariate. 95% Confidence intervals were estimated with 1000 bootstrap samples. The strength of the instrument was evaluated using the χ2 contrast for the instrument (weekend presentation) in the first-stage regression.
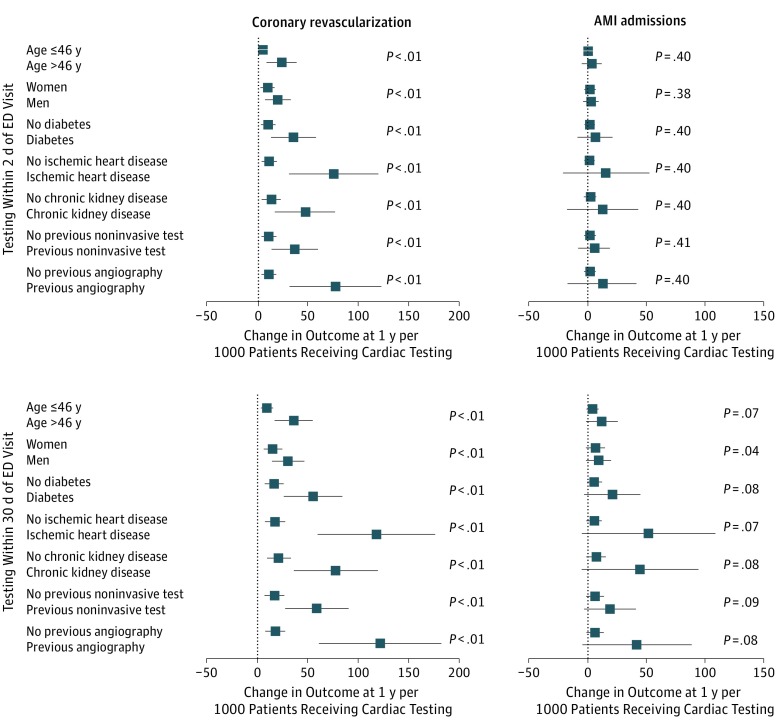
We tested whether the effect of cardiovascular testing on revascularization or AMI admissions at 1 year varied by patient characteristics (sex, diabetes, ischemic heart disease, chronic kidney disease, coronary angiography within the previous year, noninvasive testing in the previous year, and age older than 46 years or 46 years or younger, which was the median). We determined the marginal effect of testing in each subgroup and tested the difference in paired subgroups (eg, women with men) with 1000 bootstrapped samples.
We evaluated CABG surgery—typically reserved for patients with objectively worse coronary artery disease—in the subpopulation of patients who underwent angiography to determine if testing preferentially identified more severe disease.
Sensitivity Analyses
We adjusted for other potential differences in care over the weekend that may relate to our primary outcomes: cardiology consultation, admission to the hospital, or antiplatelet or antihyperlipidemic medication claims. To evaluate if uneven follow-up affected results, we performed the analysis while excluding patients without a full year of follow-up. We adjusted our exclusion criteria to include higher-risk patients with a diagnosis of “other acute or subacute ischemic heart disease.” Finally, we varied the definition of testing to include only those who underwent noninvasive testing within 30 days or angiography within 2 days of the ED visit.
Results
Baseline Characteristics
The data included a total of 926 633 privately insured patients ages 18 to 64 years, with an average age of 44.4 years; 536 197 patients (57.9%) were women. Patients presenting on Monday to Thursday were more likely to receive cardiovascular testing within 2 or 30 days (18.2% and 26.1%) than those presenting on Friday to Sunday (12.3% and 21.4%) (Table 1). Of those who underwent testing, 91.5% of weekday and 91.2% of weekend patients received noninvasive testing, with a similar distribution of modalities within each group.
Table 1. Cardiac Testing by Cohort and Time From ED Visit (%)a.
| Cardiac Test | Within 2 d of ED Visit | Within 30 d of ED Visit | ||||
|---|---|---|---|---|---|---|
| Overall (n = 26 633) |
Weekday Patients (n = 571 988) |
Weekend Patients (n = 354 645) |
Overall (n = 926 633) |
Weekday Patients (n = 571 988) |
Weekend Patients (n = 354 645) |
|
| Noninvasive/angiographyb,c,d | 15.93 | 18.18 | 12.30 | 24.28 | 26.10 | 21.35 |
| Noninvasive testc,d | 14.59 | 16.64 | 11.29 | 22.20 | 23.88 | 19.48 |
| Exercise ECG | 2.13 | 2.41 | 1.68 | 4.02 | 4.26 | 3.63 |
| Stress echocardiography | 3.32 | 3.88 | 2.42 | 5.21 | 5.66 | 4.50 |
| Myocardial perfusion scanc | 9.41 | 10.63 | 7.44 | 13.58 | 14.61 | 11.92 |
| Coronary CT angiography | 0.39 | 0.45 | 0.30 | 0.50 | 0.56 | 0.41 |
| Coronary angiography | 1.79 | 2.10 | 1.30 | 3.45 | 3.67 | 3.08 |
Abbreviations: CT, computed tomographic; ECG, electrocardiogram; ED, emergency department.
Data are given as percentages.
Patients who received either a noninvasive test or coronary angiography.
Cohen d > 0.1 for standardized mean differences of cardiac testing within 2 days of ED visit between weekday and weekend patients.
Cohen d > 0.1 for standardized mean differences of cardiac testing within 30 days of ED visit between weekday and weekend patients.
While patients who received testing had higher-risk characteristics than those who did not, there was minimal difference in risk factors between weekday and weekend patients (Table 2). Patients who received testing within 30 days were older (49.7 years vs 42.6), more likely men (47.5% vs 40.4%), and had higher rates of most traditional cardiac risk factors (for hypertension, 47.8% vs 38.2%) compared with the nontesting cohort. Patients presenting on weekdays had similar age (44.4 years vs 44.3 years), likelihood of being men (42.1% vs 42.3%), and traditional cardiac risk factors (for hypertension, 40.7% vs 40.3%) compared with patients presenting on weekends. There was a similar proportion of primary insurance beneficiaries on weekdays (65.2%) and weekends (63.5%). The standardized mean difference between weekday and weekend presenters was less than 0.1 for all characteristics.
Table 2. Baseline Characteristics by Cohortsa.
| Characteristic | Within 2 d of ED Presentation | Within 30 d of ED Presentation | Weekday Patients (n = 571 988) |
Weekend Patients (n = 354 645) |
||
|---|---|---|---|---|---|---|
| No Testing (n = 779 012) |
Testing (n = 147 621) |
No Testing (n = 701 660) |
Testing (n = 224 973) |
|||
| Age, yb,c | 43.2 | 50.3 | 42.6 | 49.7 | 44.4 | 44.3 |
| Femaleb,c | 58.8 | 53.1 | 59.6 | 52.5 | 57.9 | 57.7 |
| Chronic kidney disease | 2.1 | 1.5 | 2.1 | 1.6 | 2.0 | 2.0 |
| Diabetes | 14.4 | 17.9 | 14.2 | 17.5 | 15.0 | 14.9 |
| Hyperlipidemiab,c | 31.8 | 44.1 | 30.6 | 43.4 | 33.8 | 33.6 |
| Hypertensionb,c | 39.1 | 48.4 | 38.2 | 47.8 | 40.7 | 40.3 |
| Ischemic heart disease | 4.7 | 4.7 | 4.5 | 5.2 | 4.7 | 4.7 |
| Peripheral vascular disease | 3.5 | 3.0 | 3.4 | 3.3 | 3.4 | 3.4 |
| Smoking history | 10.5 | 8.2 | 10.7 | 8.4 | 10.2 | 10.0 |
| Acute myocardial Infarction, previous year | 1.4 | 1.5 | 1.1 | 1.4 | 1.5 | 1.4 |
| Coronary angiography, previous year | 4.8 | 3.7 | 4.8 | 4.2 | 4.7 | 4.6 |
| Coronary revascularization, previous yeard | 2.0 | 2.6 | 1.8 | 2.9 | 2.1 | 2.1 |
| Cardiologist evaluation, previous year | 8.6 | 6.7 | 8.6 | 7.4 | 8.3 | 8.3 |
| Cerebrovascular accident, previous year | 4.1 | 3.6 | 4.1 | 3.9 | 4.1 | 4.1 |
| Noninvasive test, previous year | 12.8 | 12.4 | 13.1 | 11.8 | 12.8 | 12.7 |
| Antihyperlipidemic treatmentb,c,e | 15.8 | 23.7 | 15.1 | 23.2 | 17.2 | 16.9 |
| Antiplatelet treatmentc,f | 3.6 | 5.1 | 3.4 | 5.4 | 3.9 | 3.7 |
| Primary beneficiaryb,c,g | 63.5 | 70.2 | 62.9 | 69.7 | 65.2 | 63.5 |
| Total follow-up, dh | 291.6 | 294.8 | 290.6 | 297.1 | 292.2 | 292.1 |
Population of 926 633 patients divided into testing cohorts (no testing vs cardiac testing) in noninstrumented analysis and day of presentation cohorts (weekday and weekend patients) in instrumental variable analysis. Data are given as percentages.
Cohen d > 0.1 for standardized mean difference between testing within 2 days of ED visit and no testing within 2 day. Cohen d < 0.1 for standardized mean differences between weekday and weekend patients for all variables.
Cohen d > 0.1 for standardized mean difference between testing within 30 days of ED visit and no testing within 30 days. Cohen d < 0.1 for standardized mean differences between weekday and weekend patients for all variables.
Includes both percutaneous coronary intervention and coronary artery bypass graft surgery.
Claims for all medications in the therapeutic class of antihyperlipidemic drugs in the year preceding ED presentation.
Claims for aspirin or clopidogrel in the year preceding ED presentation.
Indicates whether patient is primary beneficiary of the insurance plan (as opposed to a dependent).
Number of days from the ED visit with enrollment in the health plan.
Unadjusted Outcomes
Patients who underwent testing within 2 or 30 days had higher rates of coronary angiography, revascularization, and AMI admission at each follow-up period (Table 3). Weekday patients underwent more angiography (5.5 per 1000 patients; 95% CI, 4.5-6.6) but had similar rates of revascularization (0.3 per 1000 patients; 95% CI, −0.2 to 0.8) and AMI admissions (−0.3 per 1000 patients; 95% CI, −0.6 to 0.1) as weekend patients at 1 year.
Table 3. Unadjusted Outcomes per 1000 Patientsa,b.
| Outcome | Follow-up, d | Testing Within 2 d (n = 157 587) |
Testing From 3-30 d (n = 77 352) |
No Testing Within 30 d (n = 701 660) |
Weekday Patients (n = 583 398) |
Weekend Patients (n = 363 753) |
|---|---|---|---|---|---|---|
| Coronary angiography | 7c | 123.7 | 44.7 | NA | 25.6 | 19.9 |
| 30c | 139.5 | 146.7 | NA | 36.7 | 30.8 | |
| 180c | 156.2 | 186.4 | 18.4 | 56.5 | 51.1 | |
| 365c | 164.7 | 197.4 | 31.2 | 68.4 | 62.9 | |
| Coronary revascularizationd | 7 | 18.6 | 13.5 | NA | 4.1 | 4.1 |
| 30 | 22.6 | 40.1 | NA | 7.0 | 6.9 | |
| 180 | 28.4 | 50.4 | 5.2 | 12.7 | 12.6 | |
| 365 | 31.6 | 54.5 | 9.0 | 16.5 | 16.2 | |
| Acute myocardial infarction admission | 7c | 2.8 | 4.2 | NA | 0.8 | 1.1 |
| 30c | 3.5 | 11.3 | NA | 1.6 | 2.0 | |
| 180c | 5.9 | 15.1 | 3.0 | 4.3 | 4.7 | |
| 365 | 7.8 | 17.7 | 5.4 | 6.7 | 7.0 |
Abbreviation: NA, not applicable.
Population of 926 633 patients divided by time of testing and day of presentation. Number of patients in each cohort included in parentheses. Results presented as the number of events per 1000 patients.
Statistical testing only included for difference between weekday and weekend patients.
Includes both percutaneous coronary intervention and coronary artery bypass graft surgery.
P < .05 for difference between weekday and weekend patients.
Adjusted Analyses
With a multivariable model adjusted for observable risk factors, testing 1000 patients within 2 days of the ED visit was associated with 92.1 more coronary angiograms (95% CI, 90.5- 93.7) and 11.6 more revascularizations (95% CI, 9.4-13.8) but no significant difference in AMI admissions (0.1; 95% CI, −0.5 to 0.7) at 1 year (Table 4). Testing within 30 days of presentation was associated with a significant increase in angiography, revascularizations, and AMI admissions.
Table 4. Adjusted Change in Outcome With Cardiovascular Testing Compared with No Testing per 1000 Patients (SE)a,b,c.
| Outcome | Follow-up Period, d | Time From ED Visit to Testing | |||
|---|---|---|---|---|---|
| Within 2 d | Within 30 d | ||||
| Multivariable Analysis | Instrumented Analysisd | Multivariable Analysis | Instrumented Analysise | ||
| Coronary angiography | 7 | 103.4 (1.1) | 42.3 (5.4) | NA | NA |
| 30 | 104.2 (0.8) | 29.2 (5.2) | NA | NA | |
| 180 | 97.6 (0.8) | 18.2 (6.0) | 128.8 (2.5) | 60.1 (7.9) | |
| 365 | 92.1 (0.8) | 7.7 (6.2) | 122.8 (2.2) | 36.5 (7.9) | |
| Coronary revascularizationf | 7 | 13.2 (1.0) | -0.2 (1.7) | NA | NA |
| 30 | 13.6 (1.1) | 1.5 (2.1) | NA | NA | |
| 180 | 13.0 (1.1) | 12.2 (4.3) | 24.1 (0.3) | 20.6 (5.8) | |
| 365 | 11.6 (1.1) | 15.0 (4.8) | 22.7 (0.3) | 22.8 (6.2) | |
| Acute myocardial infarction admission | 7 | 1.7 (0.1) | -11.3 (10.7) | NA | NA |
| 30 | 1.6 (0.0) | -3.9 (2.8) | NA | NA | |
| 180 | 1.0 (0.2) | 0.0 (1.9) | 4.9 (0.2) | 2.6 (2.9) | |
| 365 | 0.1 (0.3) | 2.3 (2.8) | 4.1 (0.3) | 7.8 (4.7) | |
Abbreviations: NA, not applicable; SE, standard error.
Results presented as the change in outcome associated with performing testing in 1000 patients (SE). Estimated using the average marginal effect of testing.
In the first stage-residual, the odds ratio of weekend presentation on testing within 2 days of ED visit was 0.61 (95% CI, 0.61-0.62) with an incremental χ2 test statistic of 6166.9 with P < .001.
Adjusted for age, sex, comorbid conditions (diabetes, hypertension, hyperlipidemia, chronic kidney disease, cerebrovascular disease, peripheral vascular disease, smoking), history of ischemic heart disease, history of noninvasive test in the previous year, history of coronary angiography in the previous year, antiplatelet medication use, and antihyperlipidemic medication use.
In the first stage-residual, the odds ratio of weekend presentation on testing within 30 days of ED visit was 0.75 (95% CI, 0.74-0.77) with an incremental χ2 test statistic of 2916.4 with P < .001.
Either percutaneous coronary intervention or coronary artery bypass graft surgery.
Using weekday vs weekend as an instrument for cardiovascular testing, we found a smaller increase in coronary angiography and no significant difference in AMI admissions (Table 4). Testing within 2 days was not associated with a significant increase in angiography at 1 year. Testing was associated with 15.0 additional revascularizations per 1000 patients tested (95% CI, 5.6-24.4) at 1 year. Testing was not associated with a significant change in AMI admissions at 1 year (2.3 per 1000 patients; 95% CI, −3.2 to 7.8).
With a 30-day testing cutoff, there was a significant increase in angiography (36.5 per 1000 patients; 95% CI, 21.1-52.0) at 1 year that was smaller than seen in the multivariable analysis. There was also a significant increase in coronary revascularization at 1 year but no significant change in AMI admissions (7.8 per 1000 patients; 95% CI, −1.4 to 17.0).
Testing was consistently associated with more revascularization in patient subgroups with higher baseline cardiac risk (Figure; eTables 3 and 4 in the Supplement). However, there were no subgroups in which testing was associated with a reduction in AMI admissions. Among patients who eventually underwent angiography, those who received early testing were less likely to undergo CABG surgery (eTable 5 in the Supplement).
Figure. Subgroup Analyses of Effect of Cardiac Testing Per 1000 Patients at 1 Year.
Results are presented as the change in outcome associated with performing testing in 1000 patients (standard error) in each subgroup, estimated using the average marginal effect for each subgroup. Presented P values are the difference between the average marginal effects in paired subgroups (ie, women and men) in 1000 bootstrapped samples. Cardiac testing includes either noninvasive test (exercise electrocardiography, stress echocardiography, myocardial perfusion scan, and cardiac computed tomographic angiography) or coronary angiography. Analyses were adjusted for age; sex; comorbid conditions (diabetes, hypertension, hyperlipidemia, chronic kidney disease, cerebrovascular disease, peripheral vascular disease, tobacco use); and history of ischemic heart disease, noninvasive test in the previous year, coronary angiography in the previous year, antiplatelet medication use, and antihyperlipidemic medication use. Revascularization is either coronary artery bypass graft surgery or percutaneous coronary intervention. AMI indicates acute myocardial infarction; ED, emergency department. Error bars indicate standard error.
Sensitivity Analyses
We evaluated if the effects of testing are due to additional variations in treatment. The standardized mean difference for each additional potential variation in initial treatment—cardiology evaluation, hospital admission, or antiplatelet or antihyperlipidemic medication claims—was less than 0.1 between weekday and weekend cohorts (eTables 6-8 in the Supplement). After adjusting for these interventions, testing was still associated with an increase in revascularizations without a reduction in AMI admissions (eTables 9 and 10 in the Supplement).
Weekday presentation was associated with a small increase in coronary angiography without noninvasive testing in the first 2 days with similar rates for the remainder of the month. Including only those who underwent noninvasive testing within 30 days or angiography within 2 days (excluding angiography alone from 3 to 30 days) did not change our results (eTable 11 in the Supplement).
Neither excluding the 370 544 patients with less than 1 year of follow-up nor including the additional 17 518 patients with a diagnosis of “other acute and subacute forms of ischemic heart disease” substantially changed the effect of testing (eTables 9 and 10 in the Supplement).
Discussion
We evaluated the association between cardiac testing and subsequent clinical outcomes in patients presenting to the ED with acute chest pain. Previous observational analyses suggested that noninvasive testing of ED patients is associated with increased rates of coronary angiography and revascularization without affecting AMI admissions. However, unmeasured risk factors may be associated with more noninvasive testing and worse clinical outcomes, potentially obscuring benefits and undermining the analyses. We also found that testing is associated with increased revascularization without a decrease in AMI admissions with both traditional analyses and an instrumental variable analysis using the day of presentation as an instrument to reduce potential selection bias.
The day of presentation seems to be a strong and valid instrument: predicting receipt of cardiac testing and only affecting outcomes via testing. Acute chest pain leads to urgent presentation, so patients who present to the ED are similar on weekdays and weekends. We believe the remarkable balance in all tested observable patient characteristics between cohorts provides compelling support to our assumption that unobserved risk factors were also likely independent of the day of presentation.
The primary difference in treatment between weekday and weekend presentation was the increased use of cardiovascular testing on weekdays; there was 47% more testing within 2 days and 22% more within 30 days. Other differences in care were much smaller and potentially effect mediators downstream to the decision and outcome of cardiac testing. Adjusting for these differences did not change our results.
In patients with AMI, observational studies have demonstrated worse outcomes on weekends. These findings likely do not apply to our lower-risk cohort given differences in treatment and treatment effect. Furthermore, if there were a bias it would be toward finding a clinical benefit for cardiac testing because on weekends, the time historically associated with worse outcomes, less cardiac testing is performed. However, our study found no significant difference in AMI admissions between weekday and weekend presentation.
We found testing was associated with increased downstream testing and treatment, but the instrumented analysis demonstrated a smaller increase in angiography compared with the noninstrumented analysis. Analyses that do not adequately adjust for selection bias can overestimate the effect on downstream resource utilization; this accounts for the differences in the effect size of testing on angiography. The increase in angiography decreased with longer follow-up; testing after ED presentation may sometimes lead to an earlier evaluation that would otherwise be later performed. Our analysis suggests testing deferral is not associated with increased AMI admissions. Further analysis of the effect of testing on health care utilization and costs will refine future practice recommendations and guide patient-physician shared decision-making.
Testing led to more revascularization in those with greater baseline risk but did not decrease AMI admissions in any subgroups or preferentially selected patients with more severe disease—those requiring CABG surgery. However, we evaluated the benefit in patients who are variably tested depending on the day of presentation. The results would not be directly applicable to a higher-risk subgroup that always receives testing regardless of day of presentation. Our results show that cardiac testing is overused and reinforces the need to evaluate which, if any, patients with chest pain without evidence of ischemia benefit from noninvasive testing.
American College of Cardiology/American Heart Association guidelines include a moderate recommendation that benefits outweigh the risks for noninvasive testing before discharge or within 72 hours in troponin-negative patients with a nondiagnostic ECG. This recommendation is based on observational studies that negative testing indicates a patient’s subsequent risk for cardiac events is low enough for outpatient follow-up. However, this risk is low before testing in such patients. As EDs transition to increasingly sensitive troponin assays, troponin-negative patients’ risk will decrease further. The value of any testing is tied to the benefit of treating test-positive patients, and—despite increasing revascularization—testing did not reduce subsequent AMI admissions in our analysis.
Both noninvasive testing and coronary angiography were performed more frequently with weekday presentation; with a single instrumental variable, the interventions could not be analyzed separately. However, fewer than 10% of tested patients underwent angiography without noninvasive testing. In the 2-day analysis, this subgroup represents a small group of high-risk patients with clinical symptoms suggestive of acute ischemia with negative cardiac enzyme testing (unstable angina). These patients are more likely to benefit and their inclusion should bias results toward a positive treatment effect. The 30-day analysis also included an additional subgroup—those who underwent delayed angiography without noninvasive testing (2.9% of the testing cohort)—but did not demonstrate a reduction in AMI admissions with or without this subgroup.
Limitations
This analysis has several limitations. First, there may be untested subgroups that may benefit from testing. Second, there may be benefits that were not analyzed, such as patient reassurance or decreased symptoms. Third, we evaluated privately insured patients younger than 65 years; our results may not be generalizable to other populations. Fourth, we did not have mortality data, although AMI admissions are robust surrogate outcomes. Finally, our analysis estimated the local average treatment effect, and hence applies to those patients for whom day of presentation may change whether testing is performed.
Conclusions
Appropriate treatment of ED patients with chest pain without evidence of ischemia remains controversial. The cornerstone of treatment has been risk stratification with noninvasive testing. We found that testing was not associated with a reduction in subsequent AMI admissions and further research is needed to evaluate whether a benefit is present in higher risk subgroups. We believe the current evidence supports a shift in the treatment of these patients; shared decision-making with patients should be considered a viable alternative to routine cardiac testing in the absence of robust evidence to support its benefit.
eFigure. Patient Flow Diagram
eTable 2. Exclusion Criteria by Day of Presentation
eTable 3. Subgroup Analyses: Change in Outcome at 365 days with Cardiovascular Testing within 2 days of ED Visit per 1,000 patients
eTable 4. Subgroup Analyses: Change in Outcome at 365 days with Cardiovascular Testing within 30 days of ED Visit per 1,000 patients
eTable 5. Association Between Cardiac Testing and CABG Surgery in Patients who Underwent Coronary Angiography (change/1,000 patients)
eTable 6. Differences in Management within 2 days of ED visit
eTable 7. Differences in Management within 30 days of ED Visit
eTable 8. Claims for Antiplatelet and Antihyperlipidemic Medications
eTable 9. Sensitivity Analyses of the Change in Outcome per 1,000 patients with Cardiac Testing vs. No Testing within 2 days of the ED visit
eTable 10. Sensitivity Analyses of the Change in Outcome per 1,000 patients (SE) with Cardiac Testing vs. No Testing within 30 days of the ED visit
eTable 11. Adjusted Change in Outcome With Non-Invasive Testing within 30 days or Coronary Angiography within 2 days of ED Visit Compared with No Testing per 1,000 patients
References
- 1.Center for Disease Control and Prevention National Hospital Ambulatory Medical Care Survey: 2013. https://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2013_ed_web_tables.pdf. Accessed February 3, 2016.
- 2.Mozaffarian D, Benjamin EJ, Go AS, et al. ; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics: 2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29-e322. [DOI] [PubMed] [Google Scholar]
- 3.Pope JH, Aufderheide TP, Ruthazer R, et al. . Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med. 2000;342(16):1163-1170. [DOI] [PubMed] [Google Scholar]
- 4.Amsterdam EA, Kirk JD, Bluemke DA, et al. ; American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Interdisciplinary Council on Quality of Care and Outcomes Research . Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010;122(17):1756-1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amsterdam EA, Wenger NK, Brindis RG, et al. ; American College of Cardiology; American Heart Association Task Force on Practice Guidelines; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons; American Association for Clinical Chemistry . 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-e228. [DOI] [PubMed] [Google Scholar]
- 6.Prasad V, Cheung M, Cifu A. Chest pain in the emergency department: the case against our current practice of routine noninvasive testing. Arch Intern Med. 2012;172(19):1506-1509. [DOI] [PubMed] [Google Scholar]
- 7.Chou R; High Value Care Task Force of the American College of Physicians . Cardiac screening with electrocardiography, stress echocardiography, or myocardial perfusion imaging: advice for high-value care from the American College of Physicians. Ann Intern Med. 2015;162(6):438-447. [DOI] [PubMed] [Google Scholar]
- 8.Foy AJ, Liu G, Davidson WR Jr, Sciamanna C, Leslie DL. Comparative effectiveness of diagnostic testing strategies in emergency department patients with chest pain: an analysis of downstream testing, interventions, and outcomes. JAMA Intern Med. 2015;175(3):428-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Safavi KC, Li SX, Dharmarajan K, et al. . Hospital variation in the use of noninvasive cardiac imaging and its association with downstream testing, interventions, and outcomes. JAMA Intern Med. 2014;174(4):546-553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Redberg RF. Coronary CT angiography for acute chest pain. N Engl J Med. 2012;367(4):375-376. [DOI] [PubMed] [Google Scholar]
- 11.Redberg RF. Stress testing in the emergency department: not which test but whether any test should be done. JAMA Intern Med. 2015;175(3):436. [DOI] [PubMed] [Google Scholar]
- 12.Foy AJ, Sciamanna C, Davidson WR. Noninvasive testing in emergency department patients with low-risk chest pain: does the evidence support current guidelines? Cardiol Rev. 2016;24(6):268-272. [DOI] [PubMed] [Google Scholar]
- 13.Hartlage GR. Noninvasive testing in patients with chest pain. JAMA Intern Med. 2015;175(10):1727-1728. [DOI] [PubMed] [Google Scholar]
- 14.Bhattacharya J, Shaikh AM, Vytlacil E; National Bureau of Economic Research . Treatment Effect Bounds an Application to Swan-Ganz Catheterization. NBER Working Paper Series Working Paper 11263. Cambridge, MA: National Bureau of Economic Research; 2005, http://www.nber.org/papers/w11263. Accessed August 26, 2016. [Google Scholar]
- 15.Ryan JW, Peterson ED, Chen AY, et al. ; CRUSADE Investigators . Optimal timing of intervention in non-ST-segment elevation acute coronary syndromes: insights from the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines) Registry. Circulation. 2005;112(20):3049-3057. [DOI] [PubMed] [Google Scholar]
- 16.Hansen L. The MarketScan Databases for Life Sciences Researchers. Truven Health Analytics. 2016. http://truvenhealth.com/markets/life-sciences/products/data-tools/marketscan-databases. Accessed February 3, 2016.
- 17.Center for Medicare and Medicaid Services ICD-9-CM Diagnosis and Procedure Codes: Abbreviated and Full Code Titles. https://www.cms.gov/medicare/coding/ICD9providerdiagnosticcodes/codes.html. Accessed January 1, 2016.
- 18.Center for Medicare and Medicaid List of MS-DRGs. Version 28.0. https://www.cms.gov/icd10manual/fullcode_cms/P0368.html. Accessed March 1, 2016.
- 19.Center for Medicare and Medicaid Physician Fee Schedule. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/index.html?redirect=/PhysicianFeeSched/. Accessed March 1, 2016.
- 20.Terza JV, Basu A, Rathouz PJ. Two-stage residual inclusion estimation: addressing endogeneity in health econometric modeling. J Health Econ. 2008;27(3):531-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chan GW, Sites FD, Shofer FS, Hollander JE. Impact of stress testing on 30-day cardiovascular outcomes for low-risk patients with chest pain admitted to floor telemetry beds. Am J Emerg Med. 2003;21(4):282-287. [DOI] [PubMed] [Google Scholar]
- 22.Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE; Myocardial Infarction Data Acquisition System (MIDAS 10) Study Group . Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007;356(11):1099-1109. [DOI] [PubMed] [Google Scholar]
- 23.Kumar G, Deshmukh A, Sakhuja A, et al. ; Milwaukee Initiative in Critical Care Outcomes Research (MICCOR) Group of Investigators . Acute myocardial infarction: a national analysis of the weekend effect over time. J Am Coll Cardiol. 2015;65(2):217-218. [DOI] [PubMed] [Google Scholar]
- 24.Amsterdam EA, Kirk JD, Diercks DB, Lewis WR, Turnipseed SD. Immediate exercise testing to evaluate low-risk patients presenting to the emergency department with chest pain. J Am Coll Cardiol. 2002;40(2):251-256. [DOI] [PubMed] [Google Scholar]
- 25.Bholasingh R, Cornel JH, Kamp O, et al. . Prognostic value of predischarge dobutamine stress echocardiography in chest pain patients with a negative cardiac troponin T. J Am Coll Cardiol. 2003;41(4):596-602. [DOI] [PubMed] [Google Scholar]
- 26.Kontos MC, Jesse RL, Schmidt KL, Ornato JP, Tatum JL. Value of acute rest sestamibi perfusion imaging for evaluation of patients admitted to the emergency department with chest pain. J Am Coll Cardiol. 1997;30(4):976-982. [DOI] [PubMed] [Google Scholar]
- 27.Hamm CW, Goldmann BU, Heeschen C, Kreymann G, Berger J, Meinertz T. Emergency room triage of patients with acute chest pain by means of rapid testing for cardiac troponin T or troponin I. N Engl J Med. 1997;337(23):1648-1653. [DOI] [PubMed] [Google Scholar]
- 28.Than M, Cullen L, Aldous S, et al. . 2-Hour accelerated diagnostic protocol to assess patients with chest pain symptoms using contemporary troponins as the only biomarker: the ADAPT trial. J Am Coll Cardiol. 2012;59(23):2091-2098. [DOI] [PubMed] [Google Scholar]
- 29.Angrist JD, Imbens GW, Rubin DB. Identification of causal effects using instrumental variables. J Am Stat Assoc. 1996;91(434):444-455. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Patient Flow Diagram
eTable 2. Exclusion Criteria by Day of Presentation
eTable 3. Subgroup Analyses: Change in Outcome at 365 days with Cardiovascular Testing within 2 days of ED Visit per 1,000 patients
eTable 4. Subgroup Analyses: Change in Outcome at 365 days with Cardiovascular Testing within 30 days of ED Visit per 1,000 patients
eTable 5. Association Between Cardiac Testing and CABG Surgery in Patients who Underwent Coronary Angiography (change/1,000 patients)
eTable 6. Differences in Management within 2 days of ED visit
eTable 7. Differences in Management within 30 days of ED Visit
eTable 8. Claims for Antiplatelet and Antihyperlipidemic Medications
eTable 9. Sensitivity Analyses of the Change in Outcome per 1,000 patients with Cardiac Testing vs. No Testing within 2 days of the ED visit
eTable 10. Sensitivity Analyses of the Change in Outcome per 1,000 patients (SE) with Cardiac Testing vs. No Testing within 30 days of the ED visit
eTable 11. Adjusted Change in Outcome With Non-Invasive Testing within 30 days or Coronary Angiography within 2 days of ED Visit Compared with No Testing per 1,000 patients