Key Points
Question
Can a patient-facing, interactive advance care planning website called PREPARE plus an easy-to-read advance directive increase advance care planning documentation compared with an advance directive alone?
Findings
In this randomized clinical trial that included 414 older veterans with chronic illness from multiple primary care clinics, PREPARE plus an easy-to-read advance directive resulted in statistically significant higher advance care planning documentation (35%) compared with an advance directive alone (25%).
Meaning
Patient-facing advance care planning tools, including the PREPARE website and the easy-to-read advance directive, increased advance care planning documentation and engagement without additional clinician- or system-level interventions.
This comparative effectiveness randomized clinical trial compares the efficacy of an interactive, patient-centered advance care planning website (PREPARE) with an easy-to-read advance directive to increase planning documentation.
Abstract
Importance
Documentation rates of patients’ medical wishes are often low. It is unknown whether easy-to-use, patient-facing advance care planning (ACP) interventions can overcome barriers to planning in busy primary care settings.
Objective
To compare the efficacy of an interactive, patient-centered ACP website (PREPARE) with an easy-to-read advance directive (AD) to increase planning documentation.
Design, Setting, and Participants
This was a comparative effectiveness randomized clinical trial from April 2013 to July 2016 conducted at multiple primary care clinics at the San Francisco VA Medical Center. Inclusion criteria were age of a least 60 years; at least 2 chronic and/or serious conditions; and 2 or more primary care visits; and 2 or more additional clinic, hospital, or emergency room visits in the last year.
Interventions
Participants were randomized to review PREPARE plus an easy-to-read AD or the AD alone. There were no clinician and/or system-level interventions or education. Research staff were blinded for all follow-up measurements.
Main Outcomes and Measures
The primary outcome was new ACP documentation (ie, legal forms and/or discussions) at 9 months. Secondary outcomes included patient-reported ACP engagement at 1 week, 3 months, and 6 months using validated surveys of behavior change process measures (ie, 5-point knowledge, self-efficacy, readiness scales) and action measures (eg, surrogate designation, using a 0-25 scale). We used intention-to-treat, mixed-effects logistic and linear regression, controlling for time, health literacy, race/ethnicity, baseline ACP, and clustering by physician.
Results
The mean (SD) age of 414 participants was 71 (8) years, 38 (9%) were women, 83 (20%) had limited literacy, and 179 (43%) were nonwhite. No participant characteristic differed significantly among study arms at baseline. Retention at 6 months was 90%. Advance care planning documentation 6 months after enrollment was higher in the PREPARE arm vs the AD-alone arm (adjusted 35% vs 25%; odds ratio, 1.61 [95% CI, 1.03-2.51]; P = .04). PREPARE also resulted in higher self-reported ACP engagement at each follow-up, including higher process and action scores; P <.001 at each follow-up).
Conclusions and Relevance
Easy-to-use, patient-facing ACP tools, without clinician- and/or system-level interventions, can increase planning documentation 25% to 35%. Combining the PREPARE website with an easy-to-read AD resulted in higher planning documentation than the AD alone, suggesting that PREPARE may increase planning documentation with minimal health care system resources.
Trial Registration
clinicaltrials.gov Identifier: NCT01550731
Introduction
Advance care planning (ACP) is a process whereby people communicate their goals and preferences for future medical care. The Institute of Medicine recommends ACP as a means to provide patient-centered, value-aligned medical care. In addition, Medicare and Medicaid Services (CMS) reimburse clinicians for ACP documentation because ACP conversations result in improved satisfaction with care, quality of life, and receipt of medical care aligned with patients’ wishes.
The ACP field has evolved to consider ACP as a process that involves a series of discussions over time in addition to advance directive (AD) completion. However, most older adults, even those with serious illness, have not engaged in ACP, and patients’ wishes are often not documented. Clinician barriers to ACP include a lack of training and system resources, especially in busy outpatient clinics. Patient barriers include difficulty understanding AD forms and feeling unprepared to make end-of-life medical decisions.
To help overcome some of these barriers, we first created an easy-to-read AD that significantly increased 6-month documentation. However, formative work among diverse populations demonstrated the need for more preparation for complex, ongoing medical decision making and communication of one’s wishes. Therefore, we created the PREPARE website (https://prepareforyourcare.org/), which has been shown to empower older adults to engage in ACP through the use of a simple 5-step process and “how-to” videos. Both of these patient-facing ACP tools were designed to help older adults begin to engage in ACP outside the medical environment.
The objective of this randomized clinical trial was to compare the efficacy of PREPARE plus the easy-to-read AD (PREPARE plus AD) vs the AD alone (AD-only) on ACP documentation and engagement. We hypothesized that ACP documentation and engagement would increase in both arms but would be greater in the PREPARE plus AD arm.
Methods
This is a single-blind, parallel-group, randomized comparative effectiveness trial. The conceptual framework and the full trial protocol, including inclusion and exclusion criteria; the study flow diagram; recruitment procedures; sample size estimates; and validity, reliability, and response options of all outcome measures have been previously published. Using a modified informed consent process for vulnerable populations, written informed consent was obtained for all participants. Participants were compensated $50 for the baseline interview and $25 for all follow-up interviews. This study was approved by the University of California, San Francisco, and the San Francisco Veterans Affairs (VA) Medical Center institutional review boards. VA research audits were performed yearly.
Participants and Enrollment Criteria
Veterans were enrolled from a women’s, geriatrics, and several general medicine clinics at the San Francisco VA from April 2013 through July 2016. A full table of inclusion and exclusion criteria has been published. In brief, veterans were included if they were 60 years or older, had at least 2 chronic medical conditions defined by International Classification of Diseases, Ninth Revision (ICD-9), codes, had 2 or more visits with a primary care clinician in the past year (ie, a marker of established care) and had at least 2 additional VA clinic, emergency department, or hospital visits with any clinician in the past year (ie, a marker of frequent access). To be enrolled, veterans had to have an upcoming primary care appointment within 1 to 3 weeks. Exclusion criteria were determined by their clinician and study staff based on ICD-9 codes, medical record review, and in-person screening and included dementia, moderate-to-severe cognitive impairment, blindness, deafness, delirium, psychosis, active drug or alcohol abuse within the past 3 months, plans to be out of town during the study, no telephone, or inability to answer informed consent teach-back questions within 3 attempts. Because people may change their medical preferences over time, we did not exclude individuals who had previously engaged in ACP.
Recruitment and Data Collection
A Health Insurance Portability and Accountability Act (HIPAA) waiver was obtained to identify Veterans who met our inclusion and exclusion criteria and had upcoming appointments. As previously described, after clinicians gave permission for study staff to contact their patients, we sent recruitment letters and made phone calls to describe the study and assess eligibility and interest. Names were randomly listed to ensure random recruitment, with oversampling of women and nonwhite veterans. Staff screened participants prior to enrollment. Data were collected using Research Electronic Data Capture (REDCap); a secure, web-based application.
Interventions
Given the potential benefits of ACP, we decided with our VA stakeholders to perform a comparative effectiveness study and provide all veterans some form of ACP. Both PREPARE and the easy-to-read AD were designed with and vetted by older adults from several community and clinical settings and from diverse race/ethnicity and cultural backgrounds. Both tools are patient-facing, meaning their use does not require clinician or systems-level involvement to begin the ACP process. No clinician-, electronic health record–, or systems-level changes were implemented as part of this trial.
AD-Only Intervention
In the AD-only arm, veterans were asked to review the easy-to-read AD for 5 to 20 minutes within research offices. Participants were called 1 to 3 days prior to their upcoming primary care visit to remind them about their visit.
PREPARE Plus AD Intervention
The PREPARE plus AD arm included the literacy and culturally appropriate, HIPAA-compliant PREPARE website plus the easy-to-read AD. Briefly, we reconceptualized ACP as a process that evolves over time and includes many behaviors. Using video stories, modeling of behaviors, and a 5-step process, PREPARE was designed to motivate and prepare individuals to discuss their values and care preferences with their family, friends and clinicians. Through tailored algorithms, PREPARE asks individuals about their values and helps them make a commitment (ie, action plan) to do 1 ACP step. PREPARE then creates a unique, printed “Summary of My Wishes” and has the capacity to save individual’s preferences. Reviewing PREPARE takes an mean (SD) of 57 (16) minutes or approximately 10 minutes per step.
PREPARE was administered within research offices, and participants were asked to review PREPARE in its entirety. Participants were instructed to complete PREPARE on their own. Research staff intervened only if there were technological issues and the study could not move forward. After viewing PREPARE, participants were given a copy of their action plan; the AD; their website login; and a PREPARE pamphlet, booklet, and DVD to take home. Participants were called 1 to 3 days prior to their upcoming primary care visit and reminded to bring the “Summary of My Wishes” and action plan to their medical visit.
Outcomes
Our primary outcome was any new ACP documentation in the electronic medical record (EMR) 9 months after study enrollment. Because legal forms (eg, ADs, living wills, a durable power of attorney for healthcare, and physicians’ orders for life-sustaining treatment [POLST] forms) and documented discussions can be used to direct medical care, we created a composite variable of any ACP documentation (forms and/or discussions). All medical review data were double-coded by 2 independent research assistants. Discrepancies were adjudicated by the principal investigator (R.L.S.).
Secondary outcomes, measured at 1 week, 3 months, and 6 months, included the validated, patient-reported ACP Engagement Survey. This questionnaire includes both process measures of knowledge, contemplation, self-efficacy, and readiness assessed on an average 5-point Likert scale and action measures such as discussing and documenting ACP wishes using “yes” or “no” response options on a 0- to 25-point scale. All questions are published. Clinically meaningful effect sizes were defined based on commonly used criteria (ie, 0.50-0.79 was considered a moderate effect). We also measured ease of use, “How easy was it to use this guide?” on a 1 (very hard) to 10 (very easy) point scale, and satisfaction, “How comfortable were you reviewing this guide?”, “How helpful was this guide?”, and “How likely are you to recommend this guide to others?” using “not-at-all” to “extremely” 5-point Likert scale after viewing the interventions.
Other Measures
We assessed participant characteristics using self-report at baseline including age, gender they most identified with (male, female, other), race/ethnicity, and validated measures of health status, health literacy, social support, and social standing. We also assessed the presence of a possible surrogate decision maker (yes or no), whether they had funeral plans or a will, and whether they had internet access in the home (yes or no). Two research assistants conducted independent medical record review to determine prior ACP documentation up to 5 years before the baseline interview. We also administered the Patient Health Questionnaire (PHQ)-4 at baseline and at each follow-up interview. The PHQ-4 includes the PHQ-2 for depression and the Generalized Anxiety Disorder (GAD)-2 anxiety screening tool. A score of 3 or greater on a 0 to 6 scale suggests possible depression or anxiety.
Sample Size
We estimated that 350 veterans would provide 92% power with a 2-tailed α = .05 to detect ACP documentation (primary outcome) from 15% in the AD-only arm to 30% in the PREPARE plus AD arm. We oversampled to 415 veterans to account for up to 15% attrition.
Randomization, Allocation Concealment, Blinding, and Fidelity
Because we hypothesized that literacy and cultural differences may be important determinants of ACP engagement, participants were block randomized, using a computer-based random number generator, by health literacy (adequate vs limited), and race/ethnicity (nonwhite vs white) in random block sizes of 4, 6, and 8 by a statistician (J.B.) who was not involved in recruitment. The initial visit included consent, baseline assessments, and the interventions, which were longer in the PREPARE plus AD arm. Because of the need to schedule interview rooms to accommodate longer PREPARE plus AD interviews, randomization occurred at the time of scheduling.
Although participants could not be blinded to the intervention, they were told during the consent process that they had a “50/50 chance” of getting 1 of 2 different ACP guides. However, the nonassigned intervention was not described. The staff member who administered the intervention and baseline interview was not blinded. However, all follow-up outcome ascertainment was conducted by different staff blinded to group allocation. Research staff asked participants at each follow-up to not disclose the materials they reviewed, and staff documented whether they became unblinded. If unblinding occurred, a third blinded staff member conducted all subsequent interviews. Clinicians were blinded to patient group assignment; we obtained clinicians’ permission to recruit their patients, but the interventions were not described, and no clinician education was provided.
To ensure fidelity, staff followed study scripts and used checklists for every study phase. Staff had to demonstrate an ability to adhere to the protocol in role-playing exercises, 10% of all interviews and data capture were observed for accuracy, and ongoing training was provided.
Statistical Methods
Variables were assessed for distributional and outlier values using standard summary statistics. Baseline participant characteristics were compared between arms using unpaired t tests, χ2, or Fisher exact tests. Using t tests or χ2 tests, we also compared, by intervention group, veterans’ age, race/ethnicity, and gender between those who refused vs those who enrolled and between those who withdrew vs those who remained in the study. We used intention-to-treat analysis using SAS statistical software (version 9.4; SAS Institute Inc). All P values were 2-tailed and set at a significance level of .05. We used mixed-effects logistic and linear regression with fixed effects for time (baseline and 9 months for ACP documentation and 1 week, 3 months, and 6 months for secondary outcomes of the ACP Engagement Survey modeled using dummy variables), group (AD-only vs PREPARE plus AD) and group × time interaction as well as blocking variables of literacy (adequate or limited) and race/ethnicity (white or nonwhite). We also adjusted all models for prior ACP documentation and potential clustering by physician. We tested for interactions by adding interaction terms to the group × time variable for age (<65 years and ≥65 years), gender (women and men), race/ethnicity (white and nonwhite), health literacy (adequate and limited), presence of a possible surrogate decision maker (yes or no), health status (fair-to-poor or good-to-excellent), and internet access at home (yes or no). A P value for interaction <.05 was considered statistically significant. Ease-of-use, satisfaction, depression, and anxiety measures were assessed using the Wilcoxon rank test.
Missing Data
There were no missing data for the primary outcome (ie, all medical records were reviewed). For secondary outcomes, less than 10% of interviews were missing at any time point, and all available data were included in the mixed-effects models. No individual ACP Engagement Survey question was missing greater than 10%; therefore, we used a mean imputation approach. If bias were to occur using this conservative approach, it would tend toward the null. We conducted sensitivity analysis and excluded data for veterans whose research assistants became unblinded.
Results
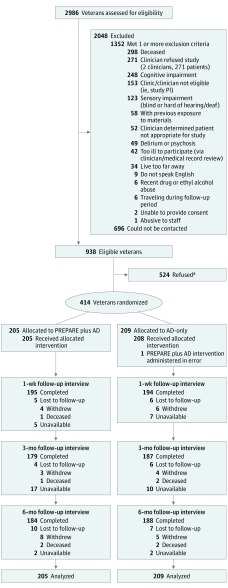
Of 938 eligible veterans, 414 (44%) enrolled; 205 were randomized to the PREPARE plus AD and 209 to the AD-only arm (Figure 1). There were no differences in gender or race/ethnicity of veterans who refused; however, those who refused were older than those who enrolled (mean [SD], 74.6 [9.1] years vs 71.1 [7.8] years; P < .001. The mean age of enrolled participants was 71.1 (7.8) years, 38 (9%) were women, 179 (43%) were nonwhite, 120 (29%) reported fair-to-poor health status, and 212 (51%) had evidence of prior ACP documentation (Table). The mean ACP documentation rate 6 months prior to intervention exposure was 0.8% (0.6%) for both groups. There were no differences in participant characteristics between arms (Table), and the number of enrolled veterans per clinician was 5 (6) [range, 1-28]. At 6 months, 184 participants in the PREPARE plus AD arm and 188 in the AD-only arm completed follow-up interviews (a 90% retention rate). There were no significant differences between groups in the rates of, or reasons for, withdrawal (9 patients [7%] in each arm) (see the eTable in the Supplement).
Figure 1. CONSORT Flow Diagram.
AD indicates advance directive; PI, principal investigator; PREPARE, patient-centered, advance care planning website.
aOne person consented but did not undergo any study procedures and was excluded from the analysis.
Table. Baseline Participant Characteristics.
| Participant Characteristic | No. | No. (%) | |
|---|---|---|---|
| AD-only (n = 209) |
PREPARE Plus AD (n = 205) |
||
| Demographics | |||
| Age, mean (SD) | 414 | 71.5 (7.9) | 70.7 (7.7) |
| Women | 414 | 19 (9) | 19 (9) |
| Race/ethnicity | 413 | ||
| White | 122 (59) | 113 (55) | |
| African American | 42 (20) | 46 (22) | |
| Latino/Hispanic | 17 (8) | 16 (8) | |
| Native American | 2 (1) | 3 (1) | |
| Asian/Pacific Islander | 13 (6) | 13 (6) | |
| Multiethnic/other | 12 (6) | 14 (7) | |
| Education ≤high school | 413 | 40 (20) | 34 (16) |
| Limited health literacy | 411 | 44 (21) | 39 (19) |
| Finances, not enough to make ends meet | 412 | 25 (12) | 24 (12) |
| Social standing 1-10 score, mean (SD) | 407 | 6.6 (2.0) | 6.5 (2.0) |
| Religious, fairly to extremely | 410 | 77 (37) | 75 (37) |
| Spiritual, fairly to extremely | 412 | 130 (63) | 125 (61) |
| Social support | |||
| In a married/long-term relationship | 414 | 100 (48) | 87 (42) |
| Have adult children | 413 | 141 (67) | 133 (65) |
| Have a potential surrogate | 414 | 198 (95) | 184 (90) |
| Health status | |||
| Self-rated health, fair-to-poor | 412 | 55 (27) | 65 (32) |
| IADL difficulty score 0-8, mean (SD) | 413 | 1.1 (1.8) | 1.0 (1.5) |
| ADL difficulty score 0-7, mean (SD) | 412 | 1.1 (1.4) | 1.1 (1.3) |
| Depression, PHQ2 score 0-6, mean (SD) | 413 | 0.8 (1.3) | 1.0 (1.5) |
| Anxiety, GAD2 PHQ2 score, 0-6, mean (SD) | 413 | 1.1 (1.6) | 1.2 (1.7) |
| Prior planning activities | |||
| Completed a will | 407 | 104 (51) | 94 (46) |
| Made funeral arrangements | 408 | 62 (30) | 65 (32) |
| Prior ACP documentation | 414 | 109 (52) | 103 (50) |
| Legal forms (ie, advance directives) and orders (ie, POLST) | 89 (43) | 73 (36) | |
| Documented discussions about ACP | 61 (29) | 63 (31) | |
| Internet access | |||
| Access to the internet | 414 | 79 (38) | 87 (42) |
Abbreviations: ACP, advance care planning; AD, advance directive; ADLs, activities of daily living; GAD2, generalized anxiety disorder 2-question anxiety screening measure; IADL, instrumental activities of daily living; PHQ2, Patient Health Questionnaire, 2-question depression screening measure; POLST, physician’s orders for life-sustaining treatment; PREPARE, patient-centered, advance care planning website.
At 9 months, in mixed-effects adjusted analysis, new overall ACP documentation was higher in the PREPARE plus AD vs the AD-only arm (unadjusted analyses, 37% vs 27%, P = .04; and adjusted analyses, 35% vs 25%, adjusted odds ratio [OR], 1.61; 95% CI, 1.03-2.51, P = .04), including higher documentation for legal forms and orders (20% vs 13%; P = .04) and for documented discussions (26% vs 20%; P = .13).
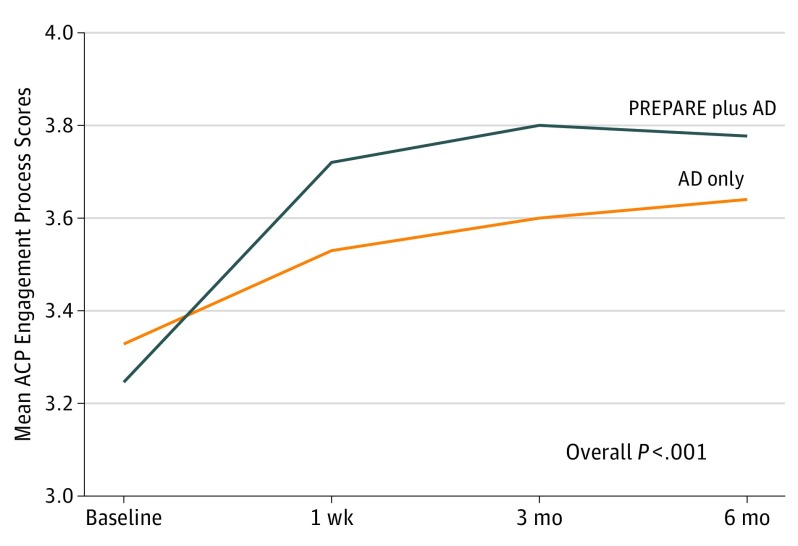
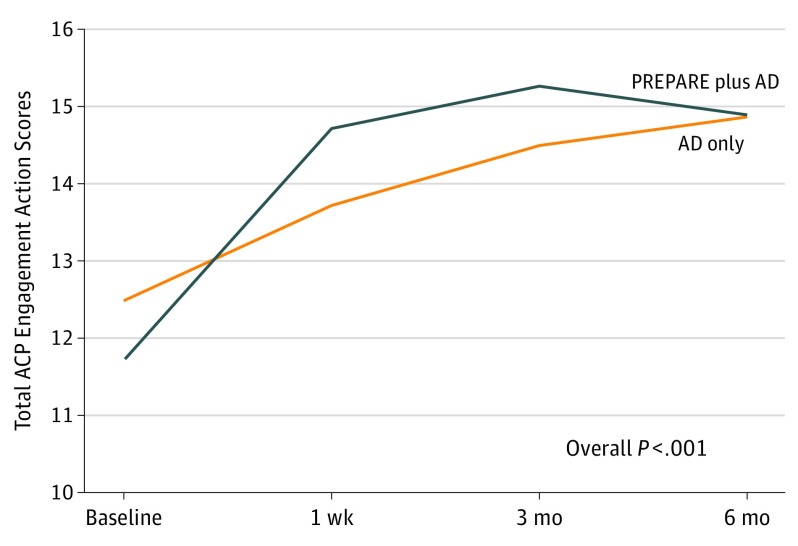
Self-reported ACP engagement including mean process and action scores increased significantly more in the PREPARE plus AD arm compared with the AD-only arm, group × time P < .001 (Figure 2 and Figure 3). Effect size estimates were moderate for PREPARE plus AD (0.59 to 0.68 SDs for process scores, 0.49 to 0.59 SDs for action scores) and were small for the AD-only arm (0.24 to 0.39 for process scores, 0.20 to 0.39 SDs for action scores).
Figure 2. Values Reflect Mean Advance Care Planning (ACP) Engagement Process Scores From Repeated Measures, Mixed-Effects Linear Regression Models Adjusted for Race, Literacy, Baseline ACP Documentation, and Clustering by Physician.
P values reflect significance for overall group × time interactions. AD indicates advance directive; PREPARE, patient-centered, advance care planning website.
Figure 3. Values Reflect Total Advance Care Planning (ACP) Engagement Action Scores From Repeated Measures, Mixed-Effects Linear Regression Models Adjusted for Race, Literacy, Baseline ACP Documentation, and Clustering by Physician.
P values reflect significance for overall group × time interactions. AD indicates advance directive; PREPARE, patient-centered, advance care planning website.
There were no significant interaction effects observed for ACP documentation or ACP engagement as a function of age, gender, race/ethnicity, US acculturation, health literacy, presence of a surrogate decision maker, health status, access to or confidence using the internet, or prior ACP documentation.
There were no significant differences in the 10-point self-reported ease-of-use scales for PREPARE plus AD vs the AD-only intervention (9.0 [1.4] vs 8.7 [1.7]; P = .31) or for the 5-point satisfaction scales including comfort reviewing the interventions (4.5 [0.7] vs 4.4 [0.8]; P = .57); helpfulness (4.4 [0.8] vs 4.3 [0.9]; P = .19); and likelihood of recommending the guides (4.4 [0.9] vs 4.2 [1.1]; P = .10).
No adverse events were reported. After controlling for baseline scores, there were no differences in depression or anxiety between arms at 6 months. One participant assigned to the AD-only arm was given PREPARE plus AD; however, this individual was analyzed in their assigned group. Outcomes did not differ after excluding 7 individuals whose research assistants became unblinded (5 PREPARE plus AD, 2 AD-only).
Discussion
In the absence of clinician- or systems-level interventions, the easy-to-read AD (AD-only) increased new ACP documentation to 25%. PREPARE plus AD increased ACP documentation to 35%. Both tools were rated highly in terms of ease-of-use, satisfaction, and helpfulness, suggesting that PREPARE and the easy-to-read AD could serve as scalable, easy-to-disseminate tools to improve the ACP process, especially in busy and resource-poor primary care clinics.
Prior studies have shown that passive ACP education with written materials is less effective than ongoing education by a trained health care professional. One reason may be the use of ADs and other materials written beyond a 12th grade reading level. The success of both PREPARE and the easy-to-read AD may be explained by their attention to both literacy and cultural considerations designed with and for diverse communities. The PREPARE website may also help patients engage in ACP owing to the inclusion of “how-to” videos that model behavior based on behavior change and social cognitive theories. In addition, videos have been shown to help patients make end-of-life medical decisions.
The easy-to-read AD-alone increased ACP documentation similar to a 52-page ACP workbook used among veterans (easy-to-read AD, 25%; workbook, 23%), although the workbook study included mostly educated, white men compared with our diverse sample. In addition, in general, facilitator-based models have shown marked improvement in clinical communication and ACP documentation, well over 50%. In the VA workbook study, the addition of a social worker intervention increased documentation to 48%, while the addition of PREPARE increased documentation to 35%. While all care plans should eventually be reviewed by a clinician regardless of whether they are initiated by patient-facing or facilitator-level interventions, these studies suggest that some individuals may need a facilitator to begin to engage in the ACP process. However, because it may not be feasible to provide a facilitator for all patients, especially in resource-limited health systems, the ACP documentation gains demonstrated in this patient-facing only intervention study of 25% (AD-alone) and 35% (PREPARE plus AD) could have large public health implications. While combining the patient-facing tools with clinician-, facilitator-, and system-level models would likely be highly synergistic, further research is needed.
Limitations
Older veterans, including only 9% women, were recruited from several clinics from the San Francisco VA, potentially limiting generalizability. However, the sample was diverse. We did not collect reasons for refusal, and it was not possible to blind patients to treatment. However, all staff conducting follow-up interviews were blinded to group allocation, and sensitivity analysis did not change our findings. Also, the materials were viewed in study offices with computer access, potentially limiting generalizability to viewing at home. Furthermore, study interviews and reminder calls may be activating. Although reminder calls are a routine part of primary care at the VA, other programs may need to include reminders to obtain similar results, specifically reminders to bring in ADs.
Conclusions
Easy-to-use, patient-facing ACP tools, without clinician- and system-level interventions, can increase ACP documentation by 25% to 35%. Combining PREPARE plus an easy-to-read AD resulted in higher ACP documentation and engagement than the AD alone. This study suggests that PREPARE and the easy-to-read AD may be useful ACP interventions on a population level, especially in resource-limited health systems. Although these tools are likely to be synergistic with other clinician- and system-level interventions, more research is needed.
eTable. Reasons for Withdrawal
References
- 1.Sudore RL, Lum HD, You JJ, et al. . Defining advance care planning for adults: a consensus definition from a multidisciplinary Delphi panel. J Pain Symptom Manage. 2017;S0885-3924(16)31232-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Academies of Science, Engineering, and Medicine. Dying in America: improving quality and honoring individual preferences near the end of life. September, 2014. http://www.nationalacademies.org/hmd/Reports/2014/Dying-In-America-Improving-Quality-and-Honoring-Individual-Preferences-Near-the-End-of-Life.aspx. Accessed July 2016.
- 3.Tierney WM, Dexter PR, Gramelspacher GP, Perkins AJ, Zhou XH, Wolinsky FD. The effect of discussions about advance directives on patients’ satisfaction with primary care. J Gen Intern Med. 2001;16(1):32-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wright AA, Zhang B, Ray A, et al. . Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665-1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211-1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340:c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pope TM. Legal briefing: Medicare coverage of advance care planning. J Clin Ethics. 2015;26(4):361-367. [PubMed] [Google Scholar]
- 8.Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med. 2010;153(4):256-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramsaroop SD, Reid MC, Adelman RD. Completing an advance directive in the primary care setting: what do we need for success? J Am Geriatr Soc. 2007;55(2):277-283. [DOI] [PubMed] [Google Scholar]
- 10.Heyland DK, Barwich D, Pichora D, et al. ; ACCEPT (Advance Care Planning Evaluation in Elderly Patients) Study Team; Canadian Researchers at the End of Life Network (CARENET) . Failure to engage hospitalized elderly patients and their families in advance care planning. JAMA Intern Med. 2013;173(9):778-787. [DOI] [PubMed] [Google Scholar]
- 11.Schickedanz AD, Schillinger D, Landefeld CS, Knight SJ, Williams BA, Sudore RL. A clinical framework for improving the advance care planning process: start with patients’ self-identified barriers. J Am Geriatr Soc. 2009;57(1):31-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.You JJ, Downar J, Fowler RA, et al. ; Canadian Researchers at the End of Life Network . Barriers to goals of care discussions with seriously ill hospitalized patients and their families: a multicenter survey of clinicians. JAMA Intern Med. 2015;175(4):549-556. [DOI] [PubMed] [Google Scholar]
- 13.Ahluwalia SC, Bekelman DB, Huynh AK, Prendergast TJ, Shreve S, Lorenz KA. Barriers and strategies to an iterative model of advance care planning communication. Am J Hosp Palliat Care. 2015;32(8):817-823. [DOI] [PubMed] [Google Scholar]
- 14.Spoelhof GD, Elliott B. Implementing advance directives in office practice. Am Fam Physician. 2012;85(5):461-466. [PubMed] [Google Scholar]
- 15.Sudore RL, Landefeld CS, Barnes DE, et al. . An advance directive redesigned to meet the literacy level of most adults: a randomized trial. Patient Educ Couns. 2007;69(1-3):165-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McMahan RD, Knight SJ, Fried TR, Sudore RL. Advance care planning beyond advance directives: perspectives from patients and surrogates. J Pain Symptom Manage. 2013;46(3):355-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sudore RL, Schickedanz AD, Landefeld CS, et al. . Engagement in multiple steps of the advance care planning process: a descriptive study of diverse older adults. J Am Geriatr Soc. 2008;56(6):1006-1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sudore RL, Knight SJ, McMahan RD, et al. . A novel website to prepare diverse older adults for decision making and advance care planning: a pilot study. J Pain Symptom Manage. 2014;47(4):674-686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sudore R, Le GM, McMahan R, Feuz M, Katen M, Barnes DE. The advance care planning PREPARE study among older veterans with serious and chronic illness: study protocol for a randomized controlled trial. Trials. 2015;16(16):570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sudore RL, Landefeld CS, Williams BA, Barnes DE, Lindquist K, Schillinger D. Use of a modified informed consent process among vulnerable patients: a descriptive study. J Gen Intern Med. 2006;21(8):867-873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 2004;42(4):355-360. [DOI] [PubMed] [Google Scholar]
- 22.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-619. [DOI] [PubMed] [Google Scholar]
- 23.Fried TR, Van Ness PH, Byers AL, Towle VR, O’Leary JR, Dubin JA. Changes in preferences for life-sustaining treatment among older persons with advanced illness. J Gen Intern Med. 2007;22(4):495-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sudore RL, Stewart AL, Knight SJ, et al. . Development and validation of a questionnaire to detect behavior change in multiple advance care planning behaviors. PLoS One. 2013;8(9):e72465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sudore RL, Heyland DK, Barnes DE, et al. . Measuring advance care planning: optimizing the advance care planning engagement survey. J Pain Symptom Manage. 2017;53(4):669-681.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 28.Löwe B, Wahl I, Rose M, et al. . A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122(1-2):86-95. [DOI] [PubMed] [Google Scholar]
- 29.Sudore RL, Landefeld CS, Pérez-Stable EJ, Bibbins-Domingo K, Williams BA, Schillinger D. Unraveling the relationship between literacy, language proficiency, and patient-physician communication. Patient Educ Couns. 2009;75(3):398-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chew LD, Griffin JM, Partin MR, et al. . Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23(5):561-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schlomer GL, Bauman S, Card NA. Best practices for missing data management in counseling psychology. J Couns Psychol. 2010;57(1):1-10. [DOI] [PubMed] [Google Scholar]
- 32.Mueller LA, Reid KI, Mueller PS. Readability of state-sponsored advance directive forms in the United States: a cross sectional study. BMC Med Ethics. 2010;11:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.El-Jawahri A, Paasche-Orlow MK, Matlock D, et al. . Randomized, controlled trial of an advance care planning video decision support tool for patients with advanced heart failure. Circulation. 2016;134(1):52-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pearlman RA, Starks H, Cain KC, Cole WG. Improvements in advance care planning in the Veterans Affairs System: results of a multifaceted intervention. Arch Intern Med. 2005;165(6):667-674. [DOI] [PubMed] [Google Scholar]
- 35.Hammes BJ, Rooney BL, Gundrum JD. A comparative, retrospective, observational study of the prevalence, availability, and specificity of advance care plans in a county that implemented an advance care planning microsystem. J Am Geriatr Soc. 2010;58(7):1249-1255. [DOI] [PubMed] [Google Scholar]
- 36.Bays AM, Engelberg RA, Back AL, et al. . Interprofessional communication skills training for serious illness: evaluation of a small-group, simulated patient intervention. J Palliat Med. 2014;17(2):159-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Reasons for Withdrawal