Key Points
Question
To what degree do thyroidectomy rates vary among Medicare beneficiaries across US regions?
Findings
In this cross-sectional study of 15 888 thyroidectomies performed on Medicare beneficiaries in 2014, there was a 6.2-fold difference in thyroidectomy rates was observed across US regions.
Meaning
Wide variation in thyroidectomy rates observed among Medicare beneficiaries suggests widely divergent local beliefs and practice patterns surrounding the management of thyroid nodules and cancer because rates appeared to be unrelated to health care availability, regional socioeconomic status, or surgeons per capita.
This cross-sectional analysis of Medicaid data examines variability across US regions for rates of thyroid surgery among Medicaid beneficiaries.
Abstract
Importance
Research on variation in rates of procedures across otherwise similar geographic regions provides vital insight into practice patterns. It reveals the degree of consensus on how a particular condition is managed, shows areas where access to care may be inadequate, and other areas where the population may be receiving inappropriately high levels of care.
Objective
To test the hypothesis that rates of thyroid surgery vary across US geographic regions
Design, Setting, and Participants
A cross-sectional analysis of Medicare data for 15 888 beneficiaries aged 65 years or older from 2014 was carried out.
Main Outcome and Measures
Overall and hospital referral region-specific thyroidectomy rate per 100 000 Medicare beneficiaries.
Results
In 2014, 15 888 thyroidectomies were performed on Medicare beneficiaries in the United States (partial n = 7506, total n = 8382), representing a national average rate of 60 per 100 000 beneficiaries (median, 59 per 100 000 beneficiaries; IQR, 43-70 per 100 000). A 6.2-fold difference in thyroidectomy rates was observed across US regions (range, 22-139 per 100 000 Medicare beneficiaries).
Conclusions and Relevance
Thyroidectomy rates in the United States vary 6.2 fold, more than prostatectomy rates, which are usually held as the example of the procedure with the widest variation in the United States. This wide variation in thyroidectomy rates observed among Medicare beneficiaries suggests widely divergent local beliefs and practice patterns surrounding the management of thyroid nodules and cancer because rates appeared to be unrelated to health care availability, regional socioeconomic status, or surgeons per capita. A better understanding for the reasons underlying this variation is needed.
Introduction
Over the past 100 years, studies have demonstrated wide variation in the rates of common surgical procedures across geographical locations despite conditions being otherwise similar, with tonsillectomy being one of the most famous examples. Unfortunately, little evidence suggests that this variation is shrinking over time despite advances in medical science and the proliferation of practice guidelines. For example, as recently as 2012, rates of coronary artery bypass, tonsillectomy, and many other surgeries showed greater than 4-fold variation in rates across geographical locations with otherwise similar characteristics.
Rates tend to vary even more when there is not clear agreement about treatment strategies. Prostate cancer, the example used most commonly when describing extremes in surgical variation, shares similarities with thyroid cancer. Over the past 20 years, it has been recognized that selected prostate cancers may be managed by surveillance and other approaches without prostatectomy. This relates, in part, to the large reservoir of subclinical disease understood to exist for this disease, just as is known for thyroid cancer.
Variation in rates of procedures across otherwise similar geographic regions is problematic because it suggests that some people may not have adequate access to care, while others may be receiving inappropriately high levels of care. Some practice variation is expected, even in cases where practices are well agreed on, because unique circumstances may dictate alternative approaches. For instance, being admitted to the hospital after a hip fracture is accepted treatment, but rates do vary to some degree across the United States.
Over the past 25 years, the incidence of thyroid cancer has steadily increased. Most of the change in incidence has been recognized to be owing to the identification of subclinical cancers—small, asymptomatic tumors found through nonthyroid directed health care maneuvers and imaging studies. Thyroid cancer is both diagnosed and treated with surgery, and so not surprisingly, rates of thyroidectomy have increased with diagnosis rates during this period. We investigated how rates of thyroid surgery vary across the United States, and whether there were regional differences. Here, we use US Medicare claims data to test the hypothesis that rates of thyroid surgery vary across geographic regions. For perspective, we compare these rates to those of prostatectomy (known to vary widely), and hospitalization for hip fracture (known to vary little).
Methods
Data Source
The Committee for the Protection of Human Subjects at Dartmouth College declared this project to be exempt from institutional review bord approval because all data used was deidentified. Data derived from 2014 Medicare and Medicaid Services (CMS) billing claims were analyzed. All beneficiaries enrolled in the traditional Medicare plan were included in the analysis. Those enrolled in Medicare Advantage were excluded. We identified the frequency of thyroidectomy procedures (both partial and total thyroidectomy), and for comparison, total prostatectomy and hospitalizations for hip fractures, using administrative billing codes stratified by hospital referral region (HRR) (Table). The HRRs are a way to examine geographic variation in health care practices and were developed by dividing the country into regional market areas based on the hospitals in each area that provide tertiary medical care. Tertiary care hospitals are defined as those that perform major cardiovascular procedures and neurosurgery.
Table. Administrative Codes Used to Define Procedures.
| Procedure | Administrative Codes |
|---|---|
| Thyroidectomya | Partial thyroidectomy: 60210, 60212, 60220, 60225; total thyroidectomy: 60240, 60260, 60270, 60271; total thyroidectomy with neck dissection: 60252, 60254 |
| Radical prostatectomyb | 60.5x |
| Hospitalizations for hip fractureb | 820-820.99 |
Common Procedural Terminology codes used.
International Classification of Diseases, Ninth Revision, Clinical Modification codes used.
Statistical Analysis
The adjusted number of thyroidectomies performed per 100 000 Medicare beneficiaries was calculated for each HRR and overall. Variance was assessed using a distribution plot and mapped across geographic regions. Regions with too few procedures to provide stable estimates were suppressed. For perspective, thyroidectomy variation was compared to rates of conditions known to vary little (hospitalization for hip fracture) and widely (total prostatectomy) across HRRs. Rates across procedures were normalized in the distribution plot using log transformation. All analyses were performed using STATA (version 12 MP, STATA Corp).
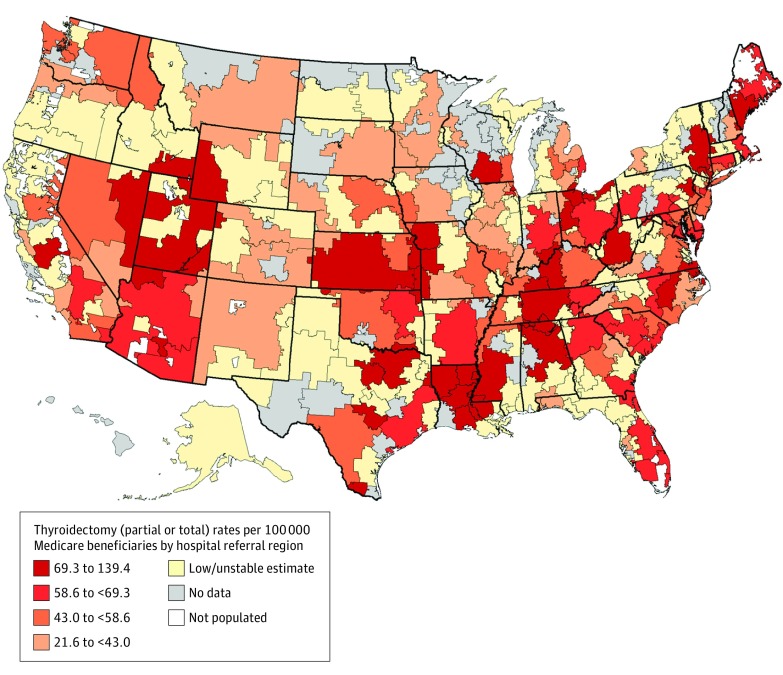
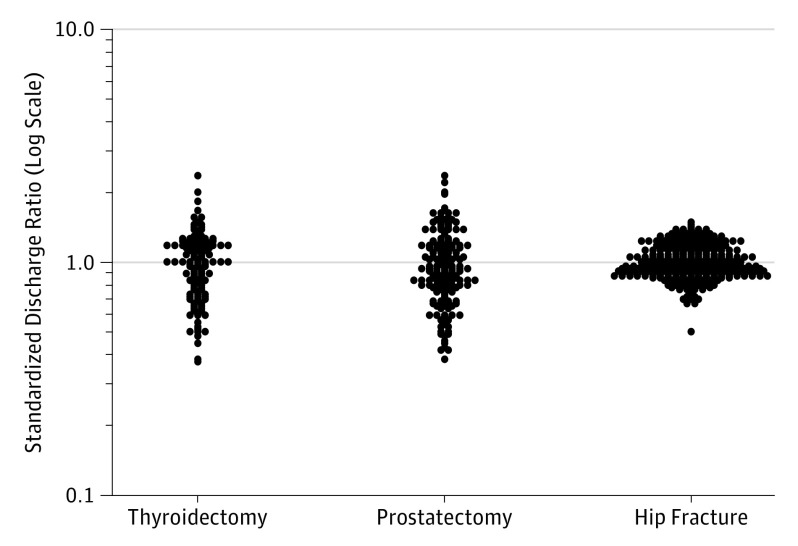
Results
In 2014, 15 888 thyroidectomies were performed on Medicare beneficiaries in the United States (partial n = 7506, total n = 8382), representing a national average rate of 60 per 100 000 beneficiaries (median, 59 per 100 000 beneficiaries; IQR, 43-70 per 100,000). A 6.2-fold difference in thyroidectomy rates was observed across US regions (range, 22-139 per 100 000 Medicare beneficiaries). In comparison, hip fracture hospitalization rates had only a 2.2-fold difference across HRRs, whereas radical prostatectomy rates varied 5.6 fold (Figure 1). Higher rates were observed in southern, central, and selected urban regions of the United States (Figure 2).
Figure 1. Standardized Discharge Ratios For Major Procedures With High and Low Variation Across The United States .
Data are derived from the 306 hospital referral regions in the United States and based on national Medicare data. Surgical rates were logarithmically transformed and divided by national averages in order to standardize estimates of variation. Thyroidectomy: mean 60/100 000 beneficiaries, interquartile ratio 1.62 (75th percentile divided by 25th percentile), extremal ratio 6.20 (highest rate divided by lowest rate); radical prostatectomy: mean 95/100 000 beneficiaries, interquartile ratio 1.58, extremal ratio 5.58; hip fracture hospitalization: 585/100 000 beneficiaries, interquartile ratio 1.27, extremal ratio 2.18.
Figure 2. Distribution of Adjusted Thyroidectomy Rates Per 100 000 Medicare Beneficiaries Across US Hospital Referral Regions.
Discussion
Thyroidectomy rates among Medicare beneficiaries varied more than 6 fold across US HRRs. Rates did not align with health care availability, regional socioeconomic status, or surgeons per capita, suggesting variation is owing to causes other than disease burden. Comparison of similar sized and resourced cities provides an illustrative example. The thyroidectomy rate is 76 per 100 000 in Manhattan, whereas in San Francisco the rate is so low that estimates are unstable. Similarly, a Medicare beneficiary in Joplin, Missouri, is 6 times more likely to undergo thyroidectomy than if living in Hackensack, New Jersey. These data suggest that thyroidectomy does not enjoy broad agreement surrounding treatment indications. The dramatic variation in rates is even higher than the patterns seen for prostate cancer, which has a similar subclinical reservoir of asymptomatic disease and where the option of surveillance rather than immediate intervention has been discussed for over 20 years. Our data show that rates of thyroidectomy vary even more than prostatectomy, which until now has been held as the standard bearer for wide variation in surgical rates.
It is notable that in Figure 2 there are some regions in the United States that register as having no data. These might be interpreted as areas having limited or no access to surgical services, such as northern Montana, North Dakota, Wisconsin, and portions of Vermont and New Hampshire. This is not necessarily the case. The lack of data is owing to the combination of low population density and the relatively low rate of thyroid surgery compared with other Medicare procedures on the population level. For example, the median rate of back surgery among Medicare beneficiaries in the United States is 450 per 100,000, compared with the 60 per 100 000 rate for thyroidectomy. The combination of low procedure rates with low population density makes it hard to obtain stable statistical estimates; however, this does not necessarily equate to inadequate services. Thus, this mapping method may be less useful in more sparsely populated, rural regions.
Although, to our knowledge, this is the first report to describe geographic variations in thyroidectomy rates, the study of geographic variation in health care as a whole is a well-developed field. Variations research is an effective tool for identifying disparities in care. Recognition of differences is a crucial first step, and this predictably leads to the question: why is there variation? Many reasons for variation exist. One commonality that has been noted in variations research is that high rates of variation occur when care is “preference sensitive”—there are a number of options available for treatment and reasonable people might choose differently. Thyroid surgery appears to be preference sensitive, based on what we have shown herein.
Prior research has shown that the geographic disparities in preference-sensitive care can be attributed to patient and physician factors. Specifically, it is known that a patient’s likelihood of undergoing such care depends to a great degree on: (1) where they reside, (2) patient and physician knowledge and beliefs about the disease and indications for surgery, and (3) the extent to which each parties’ preferences are incorporated into treatment decisions. Based on this knowledge, we surmise that variability in thyroid surgery rates in areas with similar access to surgical services largely relates to local beliefs and practice patterns.
To be sure, there are other reasons for thyroid surgery besides known or suspected cancer that could contribute to the variation in rates. However, goiter, a dominant indication for surgery historically, has reduced in prevalence since table salt was iodinated in the 1920s, and iodine deficiency in the United States is now very uncommon, even as iodine intake has decreased in recent years. Sometimes variations in rates are explained by referral to higher-volume tertiary care centers owing to case complexity—pancreatic surgery is a good example. However, data presented herein reflect the experience of Medicare patients based on where they live, not where the care was actually delivered. Furthermore, this supposition is less pertinent to thyroid surgery where lower volume surgeons (<10/y) perform most thyroidectomies, and regions with well-known cancer centers did not routinely have higher rates (eg, Seattle, Washington).
Limitations
Medicare claims are administrative billing data, so we cannot comment on relationships with important clinical information (eg, final pathological findings, cancer size). These types of data also may not clearly identify indications for surgery. This is important because thyroid surgery has multiple indications of which cancer and nodules are the most common. However, regardless of indication, the wide variation seen in thyroid surgery is surprising whether or not discussing benign disease or malignant abnormality, and total or partial thyroidectomy. Finally, Medicare data only capture those 65 years and older, therefore findings may not be fully generalizable to younger patients, who comprise over half of all thyroidectomies performed in the United States.
Conclusions
Thyroidectomy rates among Medicare beneficiaries vary more than 6 fold across US HRRs. Wide variation in thyroidectomy rates observed among Medicare beneficiaries suggests widely divergent local beliefs and practice patterns surrounding the management of thyroid cancer because rates appear to be unrelated to health care availability, regional socioeconomic status, or surgeons per capita. Variation research provides vital insight into disparities in care and the degree of consensus on how to manage a particular condition. A better understanding for the reasons underlying variation in thyroidectomy is needed.
References
- 1.Wennberg J, Gittelsohn. Small area variations in health care delivery. Science. 1973;182(4117):1102-1108. [DOI] [PubMed] [Google Scholar]
- 2.Glover JA. The incidence of tonsillectomy in school children: (section of epidemiology and state medicine). Proc R Soc Med. 1938;31(10):1219-1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boss EF, Marsteller JA, Simon AE. Outpatient tonsillectomy in children: demographic and geographic variation in the United States, 2006. J Pediatr. 2012;160(5):814-819. [DOI] [PubMed] [Google Scholar]
- 4.Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, Wennberg JE. Understanding of regional variation in the use of surgery. Lancet. 2013;382(9898):1121-1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg. 2014;140(4):317-322. [DOI] [PubMed] [Google Scholar]
- 6.Davies L, Ouellette M, Hunter M, Welch HG. The increasing incidence of small thyroid cancers: where are the cases coming from? Laryngoscope. 2010;120(12):2446-2451. [DOI] [PubMed] [Google Scholar]
- 7.Sun GH, DeMonner S, Davis MM. Epidemiological and economic trends in inpatient and outpatient thyroidectomy in the United States, 1996-2006. Thyroid. 2013;23(6):727-733. [DOI] [PubMed] [Google Scholar]
- 8.The Dartmouth Atlas of Healthcare - definition of HRR. http://www.dartmouthatlas.org/data/region/. Accessed April 25, 2017.
- 9.The Dartmouth Atlas of Healthcare - Back surgery. http://www.dartmouthatlas.org/data/table.aspx?ind=73. Accessed April 21, 2017.
- 10.Caldwell KL, Makhmudov A, Ely E, Jones RL, Wang RY. Iodine status of the U.S. population, National Health and Nutrition Examination Survey, 2005–2006 and 2007–2008. Thyroid. 2011;21(4):419-427. [DOI] [PubMed] [Google Scholar]
- 11.Pearce EN, Andersson M, Zimmermann MB. Global iodine nutrition: Where do we stand in 2013? Thyroid. 2013;23(5):523-528. [DOI] [PubMed] [Google Scholar]
- 12.Loyo M, Tufano RP, Gourin CG. National trends in thyroid surgery and the effect of volume on short-term outcomes. Laryngoscope. 2013;123(8):2056-2063. [DOI] [PubMed] [Google Scholar]