Abstract
Importance
At present, the choice of noninvasive testing for a diagnosis of significant coronary artery disease (CAD) is ambiguous, but nuclear myocardial perfusion imaging with single-photon emission tomography (SPECT) or positron emission tomography (PET) and coronary computed tomography angiography (CCTA) is predominantly used for this purpose. However, to date, prospective head-to-head studies are lacking regarding the diagnostic accuracy of these imaging modalities. Furthermore, the combination of anatomical and functional assessments configuring a hybrid approach may yield improved accuracy.
Objectives
To establish the diagnostic accuracy of CCTA, SPECT, and PET and explore the incremental value of hybrid imaging compared with fractional flow reserve.
Design, Setting, and Participants
A prospective clinical study involving 208 patients with suspected CAD who underwent CCTA, technetium 99m/tetrofosmin–labeled SPECT, and [15O]H2O PET with examination of all coronary arteries by fractional flow reserve was performed from January 23, 2012, to October 25, 2014. Scans were interpreted by core laboratories on an intention-to-diagnose basis. Hybrid images were generated in case of abnormal noninvasive anatomical or functional test results.
Main Outcomes and Measures
Hemodynamically significant stenosis in at least 1 coronary artery as indicated by a fractional flow reserve of 0.80 or less and relative diagnostic accuracy of SPECT, PET, and CCTA in detecting hemodynamically significant CAD.
Results
Of the 208 patients in the study (76 women and 132 men; mean [SD] age, 58 [9] years), 92 (44.2%) had significant CAD (fractional flow reserve ≤0.80). Sensitivity was 90% (95% CI, 82%-95%) for CCTA, 57% (95% CI, 46%-67%) for SPECT, and 87% (95% CI, 78%-93%) for PET, whereas specificity was 60% (95% CI, 51%-69%) for CCTA, 94% (95% CI, 88%-98%) for SPECT, and 84% (95% CI, 75%-89%) for PET. Single-photon emission tomography was found to be noninferior to PET in terms of specificity (P < .001) but not in terms of sensitivity (P > .99) using the predefined absolute margin of 10%. Diagnostic accuracy was highest for PET (85%; 95% CI, 80%-90%) compared with that of CCTA (74%; 95% CI, 67%-79%; P = .003) and SPECT (77%; 95% CI, 71%-83%; P = .02). Diagnostic accuracy was not enhanced by either hybrid SPECT and CCTA (76%; 95% CI, 70%-82%; P = .75) or by PET and CCTA (84%; 95% CI, 79%-89%; P = .82), but resulted in an increase in specificity (P = .004) at the cost of a decrease in sensitivity (P = .001).
Conclusions and Relevance
This controlled clinical head-to-head comparative study revealed PET to exhibit the highest accuracy for diagnosis of myocardial ischemia. Furthermore, a combined anatomical and functional assessment does not add incremental diagnostic value but guides clinical decision-making in an unsalutary fashion.
This head-to-head comparative study evaluates the diagnostic accuracy of coronary computed tomography angiography, single-photon emission tomography, and positron emission tomography and explores the incremental value of hybrid imaging compared with fractional flow reserve.
Key Points
Question
What are the diagnostic performances of coronary computed tomography angiography, single-photon emission tomography, [15O]H2O positron emission tomography, and hybrid imaging for the diagnosis of myocardial ischemia using fractional flow reserve as a reference standard?
Findings
In this head-to-head comparative study of 208 adults, sensitivity was 90% for coronary computed tomography angiography, 57% for single-photon emission tomography, and 87% for positron emission tomography, whereas specificity was 60% for coronary computed tomography angiography, 94% for single-photon emission tomography, and 84% for positron emission tomography. Positron emission tomography exhibited the highest diagnostic accuracy compared with single-photon emission tomography and coronary computed tomography angiography.
Meaning
Coronary computed tomography angiography and [15O]H2O positron emission tomography are both useful in the diagnosis of myocardial ischemia, while single-photon emission tomography and hybrid imaging guide clinical decision making in an unsalutary fashion.
Introduction
An array of noninvasive tests is available for the diagnosis of coronary artery disease (CAD), including coronary computed tomography angiography (CCTA), single-photon emission computed tomography (SPECT), and positron emission tomography (PET). Coronary computed tomography angiography allows for the assessment of the severity of coronary stenosis, SPECT for the assessment of myocardial perfusion, and PET for absolute myocardial blood flow. Furthermore, hybrid techniques that allow for the fusion of SPECT and CCTA or PET and CCTA imaging have been recently reported.
For measures of hemodynamically significant CAD, prior prospective multicenter randomized clinical trials have established invasive fractional flow reserve (FFR) to be a prognostic criterion standard, guiding decisions of revascularization resulting in improved event-free survival vs that seen with stenosis-guided revascularization. To our knowledge, a systematic comparison of the diagnostic performances of SPECT, PET, CCTA, and hybrid imaging using invasive FFR as a reference standard has not been performed. We thus performed a prospective study to test the performances of noninvasive imaging modalities wherein CCTA, SPECT, PET, and hybrid imaging were performed for all individuals and compared against an FFR reference standard
Methods
Study Design
The Prospective Comparison of Cardiac PET/CT, SPECT/CT Perfusion Imaging and CT Coronary Angiography With Invasive Coronary Angiography (PACIFIC) study is a prospective controlled clinical single-center study conducted from January 23, 2012, to October 25, 2014, at the VU University Medical Center, Amsterdam, the Netherlands (NCT01521468). The study protocol was approved by the Medical Ethics Committee of the VU University Medical Center and all participants provided written informed consent.
Study Population
The study population comprised 208 consecutively selected patients with stable new-onset chest pain and suspected CAD (see eFigure 1 and eTable 1 in the Supplement for detailed inclusion and exclusion criteria). Patients underwent CCTA, PET, and SPECT, followed by invasive coronary angiography (ICA) and FFR measurements of all coronary arteries within 2 weeks. No cardiac events were documented in the period between the scans and catheterization. A schematic overview of the imaging protocol is shown in Figure 1. Medication was not discontinued and was kept constant during the execution of the study protocol. A detailed description of the scan protocols is provided in the eAppendix in the Supplement.
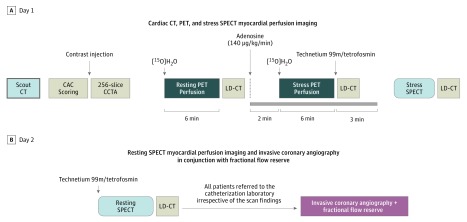
Figure 1. Schematic Illustration of the Study Protocol.
All patients underwent the imaging protocol at day 1 (A) and day 2 (B) and were subsequently referred to the catheterization laboratory for invasive coronary angiography in conjunction with fractional flow reserve measurements. CAC indicates coronary artery calcium; CCTA, coronary computed tomography angiography; LD-CT, low-dose computed tomography; PET, positron emission tomography; and SPECT, single-photon emission computed tomography.
Image Analysis and Data Interpretation
Raw image data from all scans were transferred to core laboratories. Interpretations by core laboratories were performed in a blinded fashion for CCTA (St Paul’s Hospital, Vancouver, British Columbia, Canada, and the Dalio Institute of Cardiovascular Imaging, New York–Presbyterian Hospital, New York), SPECT (Royal Brompton Hospital, London, England), and PET (Turku University Hospital, Turku, Finland) to ensure an unbiased grading of the scans.
Cardiac Computed Tomography
The 4 main vessels (right coronary artery, left main artery, left anterior descending artery, and circumflex artery) were assessed by use of CCTA. The primary threshold was defined as a visually estimated diameter of stenosis of 50% or more. Grading of the CCTA scans was on an intention-to-diagnose basis, with noninterpretable segments considered positive for obstructive CAD.
Single-Photon Emission Computed Tomography
For SPECT myocardial perfusion imaging (MPI), perfusion in each of 17 segments was classified as normal, mild reduction, moderate reduction, severe reduction, or absent perfusion, and the segmental scores were summed for the stress and resting images. Ischemia was defined by an inducible perfusion abnormality with a summed segmental difference score between stress and resting images of 2 or more. Scans were additionally quantitatively reported with the use of the total perfusion defect to assess the ischemic burden. The percentage of the myocardium that is ischemic was calculated by subtracting the resting total perfusion defect from the stress total perfusion defect.
[15O]H2O Positron Emission Tomography
On PET scans, myocardial segments with a hyperemic myocardial blood flow of 2.30 mL/min/g or less were considered to be abnormal. This cutoff value was predefined in a comparable population and published previously. Ischemia was defined by a perfusion defect of at least 2 adjacent myocardial segments with hyperemic flow of 2.30 mL/min/g or less.
Cardiac Hybrid Imaging
To allow for a hybrid interpretation, fusion images of CCTA with SPECT or PET were generated to allocate coronary arteries to their subtended vascular territories. Hybrid images were interpreted as follows. A vessel was considered abnormal when a matched SPECT/CCTA hybrid image or PET/CCTA hybrid image occurred, which was defined as ischemia (vide supra) on a SPECT or PET MPI vascular territory subtended by a coronary artery containing 50% or more stenosis. Lesion-specific ischemia was considered absent for all the other combinations of SPECT/CCTA or PET/CCTA findings.
Statistical Analysis
The end points of this study concerned the comparison of imaging modalities in terms of sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy in identifying patients with hemodynamically significant CAD, which was defined as stenosis in at least 1 coronary artery, as indicated by an FFR of 0.80 or less or a stenosis diameter of 90% or more if FFR was lacking. The total planned study sample size was fixed at 211 patients for whom paired PET and SPECT assessments were to be obtained (eAppendix in the Supplement). The McNemar test was used to test for differences between pairs of imaging modalities in terms of sensitivity, specificity, and diagnostic accuracy at the level of the individual patient. The PPV and NPV at the level of the individual patient were compared using the marginal regression approach as proposed by Leisenring et al. Secondary analyses concerned vessel-specific analyses (eAppendix in the Supplement). Furthermore, receiver operating characteristic curves were generated to determine the incremental value of noninvasive imaging above traditional risk factors. Finally, a comparison of the differences in radiation dose between different imaging modalities was performed using 1-way analysis of variance with a Bonferroni correction for multiple pairwise comparisons for localizing the source of the difference. P < .05 was considered statistically significant. All statistical analyses were performed by using IBM SPSS Statistics, version 20 (IBM Corp), except for the mixed effects logistic regression analyses, which were performed in STATA, version 14 (StataCorp LP).
Results
All 208 included patients underwent CCTA imaging, while 2 patients had incomplete or failed SPECT procedures owing to technical problems, and 4 patients failed to complete the cardiac PET protocol mainly because of claustrophobia or technical reasons. The baseline characteristics of the patients are listed in Table 1, and imaging examples are given in eFigure 2 in the Supplement.
Table 1. Baseline Patient Characteristics .
| Characteristic | No. (%) (N = 208) |
|---|---|
| Age, mean (SD), y | 58 (9) |
| Male sex | 132 (63.5) |
| BMI, mean (SD) | 27 (4) |
| Race/ethnicity | |
| White | 197 (94.7) |
| Black | 5 (2.4) |
| Asian | 6 (2.9) |
| Cardiovascular risk factors | |
| Type 2 diabetes | 33 (15.9) |
| Hypertension | 96 (46.2) |
| Hypercholesterolemia | 83 (39.9) |
| Current cigarette use | 40 (19.2) |
| History of tobacco use | 99 (47.6) |
| Family history of CAD | 107 (51.4) |
| Medication | |
| Statins | 161 (77.4) |
| Aspirin | 181 (87.0) |
| β-Blockers | 134 (64.4) |
| ACE inhibitors | 40 (19.2) |
| ARBs | 37 (17.8) |
| CCBs | 61 (29.3) |
| Long-acting nitrates | 21 (10.1) |
| Type of chest pain | |
| Typical angina | 71 (34.1) |
| Atypical angina | 80 (38.5) |
| Nonspecific chest discomfort | 57 (27.4) |
| Pretest likelihood of CAD | |
| Low | 17 (8.2) |
| Intermediate | 188 (90.4) |
| High | 3 (1.4) |
| Total CAC score, median (IQR) | 164 (14-487) |
Abbreviations: ACE, angiotensin-converting enzyme; ARBs, angiotensin II receptor blockers; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CAC, coronary artery calcium; CAD, coronary artery disease; CCBs, calcium channel blockers; IQR, interquartile range.
ICA and FFR
The prevalence of hemodynamically significant CAD in the study population was 44.2% (92 patients). Hemodynamically significant lesions were present in the left anterior descending artery in 81 patients (38.9%), in the right coronary artery in 39 patients (18.8%), and in the circumflex artery in 38 patients (18.3%). Among the 615 vessels analyzed, 160 (26.0%) contained hemodynamically significant stenosis (eFigure 3 in the Supplement). A total of 554 arteries (90.1%) were directly examined by FFR, corresponding to a total of 203 patients (97.6%) for whom FFR values were obtained. Intracoronary pressure values, measured as a ratio, ranged from 0.18 to 1.0 (mean [SD], 0.88 [0.15]) and correlated moderately (r = –0.64; P < .001) with diameter stenosis on quantitative coronary angiographic scans. The mean (SD) diameter stenosis of atherosclerotic plaques causing ischemia was 60% (18%). eTable 2 in the Supplement shows the angiographic findings and the prevalence of ischemia by FFR.
Diagnostic Accuracy of CCTA, SPECT, and PET Imaging for Diagnosis of Ischemia-Causing CAD as Indicated by FFR
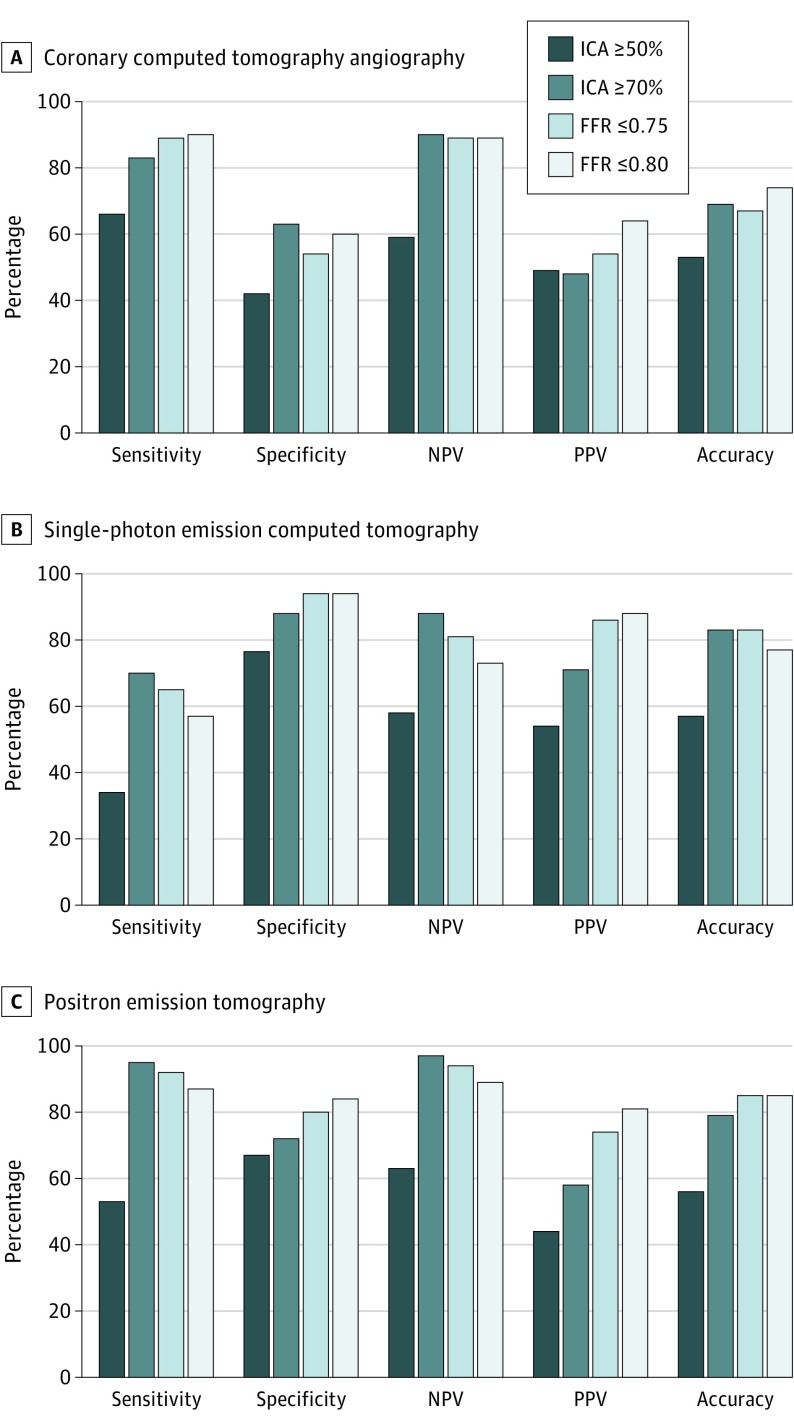
Image quality was judged as good or excellent in 183 of 208 CCTA studies (88.0%), 194 of 206 SPECT studies (94.2%), and 175 of 204 PET studies (85.8%). The diagnostic performances of all imaging modalities for the detection of hemodynamically significant CAD are summarized in Table 2 and shown in Figure 2. When analyzed on a per-patient level, the sensitivity of CCTA using the threshold of 50% diameter or greater stenosis was 90%, and the specificity was 60%. Coronary computed tomography angiography and PET exhibited a similar sensitivity (CCTA, 90%; and PET, 87%; P = .65) and NPV (CCTA, 89%; and PET, 89%; P = .95), while SPECT showed a significantly lower sensitivity (57%) and NPV (73%) when compared with CCTA (sensitivity, 90%; P < .001; and NPV, 89%; P = .002) and PET (sensitivity, 87%; and NPV, 89%, P < .001). Compared with CCTA, specificity and PPV were significantly in favor of SPECT (specificity, 94%; P < .001; and PPV, 88%; P = .01) and PET protocols (specificity, 84%; and PPV, 81%; P < .001). Overall, CCTA and SPECT showed similar accuracy (CCTA, 74%; and SPECT, 77%; P = .51). Positron emission tomography showed a significantly higher diagnostic accuracy (85%) when compared with CCTA (74%; P = .003) and SPECT (77%; P = .02). Similar trends have been observed on a per-vessel basis (eAppendix in the Supplement). The assessment of functional extent of CAD as identified by 1-, 2-, or 3-vessel disease according to an FFR of 0.80 or less has been shown in eTable 3 in the Supplement. The diagnostic performances of CCTA, SPECT, and PET when compared against anatomical reference standards (ie, ICA≥50% and ICA≥70%) and an FFR of 0.75 or less are shown in Figure 2. In addition, the association between noninvasive cardiac imaging findings and diameter stenosis as assessed by quantitative coronary angiography is shown in eFigure 4 in the Supplement. Coronary computed tomography angiography seems to overestimate the degree of stenosis, showing a high rate of positive findings for patients with nonobstructive CAD (ie, stenosis <50%), whereas the lowest percentage of abnormal scans is seen for SPECT even for patients with greater than 90% diameter stenosis (only 81% positive SPECT scans; eFigure 4 in the Supplement).
Table 2. Diagnostic Performance of CCTA, SPECT, PET, and Hybrid Cardiac Imaging for Diagnosis of Ischemia-Causing Coronary Artery Disease as Indicated by Fractional Flow Reserve .
| Characteristic | % (95% CI) | ||||
|---|---|---|---|---|---|
| CCTA | SPECT | PET | Hybrid SPECT and CCTA |
Hybrid PET and CCTA |
|
| Per patient | |||||
| Sensitivity | 90 (82-95) | 57 (46-67) | 87 (78-93) | 50 (39-61) | 74 (64-83) |
| Specificity | 60 (51-69) | 94 (88-98) | 84 (75-89) | 97 (93-99) | 92 (86-96) |
| PPV | 64 (55-73) | 88 (77-95) | 81 (72-89) | 94 (83-99) | 88 (79-94) |
| NPV | 89 (80-95) | 73 (65-80) | 89 (81-94) | 71 (63-78) | 82 (74-88) |
| Accuracy | 74 (67-79) | 77 (71-83) | 85 (80-90) | 76 (70-82) | 84 (79-89) |
| Per vessel | |||||
| Sensitivity | 72 (64-79) | 39 (32-48) | 81 (73-87) | 35 (27-43) | 64 (55-71) |
| Specificity | 78 (74-82) | 96 (94-98) | 75 (69-81) | 99 (98-100) | 97 (95-98) |
| PPV | 52 (44-59) | 80 (70-87) | 59 (51-66) | 87 (65-96) | 87 (79-92) |
| NPV | 87 (83-91) | 81 (76-85) | 92 (88-95) | 81 (76-85) | 88 (84-91) |
| Accuracy | 77 (73-80) | 82 (78-85) | 79 (75-83) | 83 (79-86) | 88 (85-91) |
Abbreviations: CCTA, coronary computed tomography angiography; NPV, negative predictive value; PET, positron emission tomography; PPV, positive predictive value; SPECT, single-photon emission computed tomography.
Figure 2. Diagnostic Performance of Coronary Computed Tomography Angiography, Single-Photon Emission Computed Tomography, and Positron Emission Tomography Imaging for Diagnosis of Significant Coronary Artery Disease as Defined by Different Standards.
FFR indicates fractional flow reserve; ICA, invasive coronary angiography; NPV, negative predictive value; and PPV, positive predictive value.
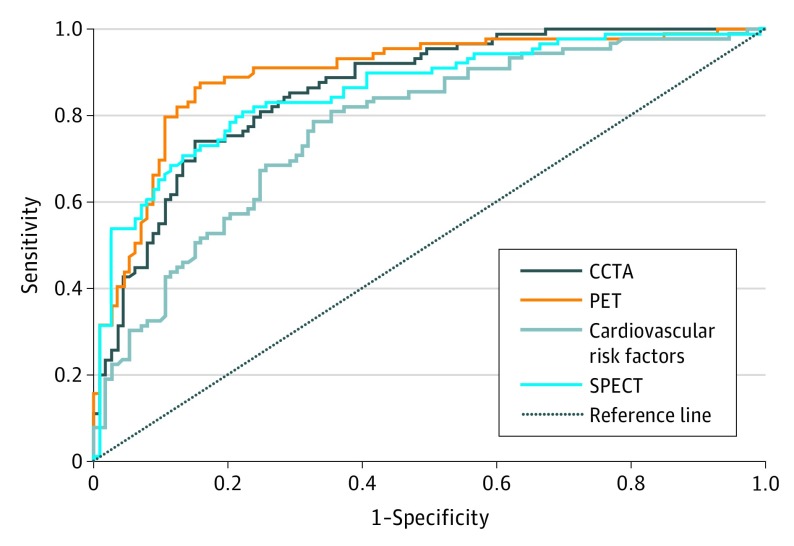
Notably, receiver operating characteristic curve analyses showed PET to possess the highest area under the curve (0.90; 95% CI, 0.85-0.94; P < .001); however, there was no statistically significant difference in the area under the curve compared with CCTA and SPECT (Figure 3). Logistic regression analyses revealed that CCTA, SPECT, and PET imaging has an incremental diagnostic value beyond traditional risk factors in assessing hemodynamic significant CAD, as indicated by FFR (eTable 4 in the Supplement).
Figure 3. Diagnostic Performance of Cardiac Imaging Methods and Traditional Cardiovascular Risk Factors for the Detection of Coronary Artery Disease (CAD) on a Patient-Based Level.
Area under the curve (AUC) calculated for coronary computed tomography angiography (CCTA), single-photon emission computed tomography (SPECT), positron emission tomography (PET), and cardiovascular risk factors for diagnosing ischemia (PET AUC = 0.90 [95% CI, 0.85-0.94; P < .001]; CCTA AUC = 0.86 [95% CI, 0.81-0.91; P < .001]; SPECT AUC = 0.86 [95% CI, 0.81-0.91; P < .001]; and cardiovascular risk factors AUC = 0.77 [95% CI, 0.71-0.84; P < .001]). Comparison of diagnostic performances of noninvasive cardiac imaging and traditional risk factors for the detection of hemodynamically significant CAD was determined by receiver operating characteristic curves (PET vs CCTA: AUC = 0.90 vs 0.86 [P = .18]; PET vs SPECT: AUC = 0.90 vs 0.86 [P = .10]; SPECT vs CCTA: AUC = 0.86 vs 0.86 [P = .98]; PET vs cardiovascular risk factors: AUC = 0.90 vs 0.77 [P < .001]; SPECT vs cardiovascular risk factors: AUC = 0.86 vs 0.77 [P < .001]; and CCTA vs cardiovascular risk factors: AUC = 0.86 vs 0.77 [P < .001]).
Noninferiority of SPECT Compared With PET for Diagnosis of Ischemia-Causing CAD
With regard to the primary end point, SPECT was shown to be noninferior in terms of its specificity (94%; P < .001) but not in terms of its sensitivity (57%; P > .99) using the predefined noninferiority margin of 10%. The absolute difference in specificity between SPECT and PET was 9.6% (95% CI, 1.6%-17.7%) in favor of SPECT, whereas the absolute difference in sensitivity was found to be 30.4% (95% CI, 20.9%-39.9%) in favor of PET.
Diagnostic Accuracy of Hybrid Cardiac Imaging for Diagnosis of Ischemia-Causing CAD as Indicated by FFR
The diagnostic performance of hybrid imaging for detecting hemodynamically significant lesions is listed in Table 2. The addition of either SPECT or PET to CCTA improved the specificity compared with CCTA (SPECT, 97%; and PET, 91%; P < .001) but lowered the sensitivity from 90% to 50% when SPECT was added to CCTA and decreased to 74% for hybrid PET/CCTA (P < .001). The addition of PET to CCTA improved the specificity (92%) compared with PET alone (84%; P = .004) but also lowered the sensitivity to 74% (P = .001). No differences in specificity and sensitivity were found when the addition of SPECT to CCTA was compared with SPECT only (specificity, 94%; P = .13; sensitivity, 57%; P = .03). Coronary computed tomography angiography yielded a false-negative result for 9 patients, while 46 patients were falsely identified as having nonhemodynamically significant CAD from hybrid SPECT/CCTA and 23 were falsely identified as having nonhemodynamically significant CAD from hybrid PET/CCTA. Compared with CCTA alone (89%), hybrid imaging yielded a significantly lower NPV from SPECT/CCTA (71%; P < .001) but not from PET/CCTA (82%; P = .06). On the other hand, hybrid imaging significantly improved PPV when compared with CCTA alone (SPECT/CCTA, 94%; P = .001; PET/CCTA, 88%; P < .001). Similar results were observed for per-artery analyses (Table 2 and eAppendix in the Supplement).
Radiation Dose of Noninvasive Cardiac Imaging
The mean (SD) radiation dose of CCTA was 5.31 (1.32) mSv. The mean (SD) dose (including low-dose CCTA) was 6.01 (0.70) mSv for SPECT and 3.10 mSv for PET MPI. The radiation dose for SPECT was significantly higher compared with that for CCTA and PET (both P < .001). Positron emission tomography was associated with a significantly lower radiation dose than was CCTA (P < .001). The hybrid SPECT/CCTA protocol yielded a mean (SD) effective radiation dose of 11.3 (1.48) mSv, and the PET/CCTA protocol yielded a mean (SD) effective radiation dose of 8.41 (1.32) mSv (P < .001).
Discussion
In this controlled clinical head-to-head comparative diagnostic performance study, PET demonstrated improved accuracy compared with CCTA and SPECT for the diagnosis of coronary ischemia, as measured by FFR, in symptomatic patients with suspected CAD. Furthermore, a hybrid diagnostic approach combining a functional and anatomical assessment by PET/CCTA or SPECT/CCTA yielded no incremental diagnostic value beyond stand-alone imaging. This study possesses the following unique design features: CCTA, SPECT, and PET were compared prospectively in a true head-to-head fashion; invasive FFR of all coronary arteries, irrespective of the imaging findings, was used as the reference standard; latest-generation techniques—such as CT-based attenuation correction in SPECT perfusion imaging—were used; and all scans were analyzed by core laboratory experts (8 of us: J.L., R.R., C.N., J.K., M.M., R.S.U., J.K.M., and K.E.) blinded to other imaging and clinical data. To our knowledge, these data represent the first comprehensive examination of commonly used noninvasive techniques to evaluate myocardial perfusion or severity of coronary artery stenosis.
At present, European and US guidelines do not advocate for any specific noninvasive imaging modality over another. Prior studies and empirical evidence have allowed for any initial noninvasive diagnostic test to be performed, depending on local availability and expertise, access to testing, costs of testing, radiation dose, ability to exercise, and the probability of obtaining a negative result. Current professional societal guidelines advocate for noninvasive imaging to be used for patients at intermediate risk of CAD, given the higher reclassification rates for these patients based on imaging findings. We observed the prevalence of ischemia-causing CAD to be 44%, reflecting an intermediate prevalence of significant CAD that is reflective of patients judged appropriate for noninvasive imaging by current guidelines. Although there is little consensus on the preferred imaging method, guidelines endorse the use of stress imaging given the solid evidence that ischemia-guided revascularizations improve symptoms and event-free survival when compared with a coronary stenosis–guided strategy. Paradoxically, prior studies evaluating the diagnostic performance of noninvasive imaging modalities have focused largely on an angiographic reference standard, with 50% stenosis or more at the time of invasive angiography considered as obstructive CAD. However, an array of investigations has revealed the inconsistency of high-grade stenosis and ischemia-causing coronary lesions. The Fractional Flow Reserve vs Angiography for Multivessel Evaluation (FAME) trial has demonstrated FFR to be a prognostic and clinical criterion standard, given its ability to guide decisions of revascularization in a manner that results in improvement in event-free survival over stenosis-guided revascularization. More important, in the FAME study, 47% of lesions were considered intermediate in stenosis severity, and approximately one-third of these lesions resulted in coronary ischemia, while two-thirds did not. In this regard, our study advances the understanding of the association of noninvasive testing and the use of FFR as a reference standard. To our knowledge, this is the first study in which all coronary arteries were examined by FFR, irrespective of the presence and severity of atherosclerosis, to discern the functional relevance of CAD.
In keeping with prior reports, CCTA exhibited high sensitivity (90%) and NPV (89%), even when compared directly with the FFR reference standard. Despite it being an excellent tool for ruling out hemodynamically significant CAD, CCTA performed poorly for identification of coronary lesions that cause ischemia, with 60% specificity and 64% PPV. In the recently published Evaluation of Integrated Cardiac Imaging for the Detection and Characterization of Ischemic Heart Disease (EVINCI) trial, the specificity of CCTA was much higher (92%), a disparity most likely attributable to the prevalence of CAD and the anatomical reference standard that was used. Naturally, CCTA will be closely associated with ICA and, as such, will yield high accuracy. However, CCTA is particularly hampered by the lack of functional information, resulting in overestimation of the significance of CAD when compared against FFR. The effect of different definitions of significant CAD, conceptualized as either the degree of luminal narrowing by ICA or the impairment in coronary flow reflected by FFR, on the evaluation of CCTA in diagnostic accuracy studies can be extracted from prior studies.
For measures of myocardial perfusion abnormalities, our results showed a higher diagnostic accuracy of PET vs SPECT MPI, as compared with FFR. Although, to our knowledge, there are no other prospective head-to-head comparative trials of PET vs SPECT using FFR as a reference standard, the sensitivity and specificity of PET are in keeping with 2 recently published meta-analyses of cardiac stress studies. The greater diagnostic accuracy of PET vs SPECT MPI has several potential explanations, but it has been suggested that its superior performance is largely owing to its higher spatial resolution that allows for better assessment of endocardial ischemia, as well as its ability to quantify perfusion in absolute terms. Of 21 patients with multivessel disease or left main disease (ie, left main coronary artery), 4 (19.0%) had normal perfusion results with SPECT, while quantitative PET correctly identified ischemia. A well-known limitation of SPECT, an imaging method dependent on relative rather than absolute perfusion assessment, is the presence of a normal study in the case of “balanced” ischemia observed in 3-vessel disease or left main disease. Prior studies have suggested a high rate of false negatives in this population that is negated by PET characteristics. These findings are supported by a recently published meta-analysis suggesting a low sensitivity of SPECT when it is compared with an FFR reference standard. In contrast, in our study, SPECT imaging exhibited a very high specificity. This performance characteristic has not been widely observed in prior studies and may be explained by interpretation by an expert core laboratory reader or, perhaps, by the use of CT attenuation–corrected SPECT images. Prior studies are in support of the latter, although FFR-comparison SPECT studies evaluating imaging with or without attenuation artifacts have not been performed to date.
Finally, we observed no improved accuracy for combined physiological and anatomical imaging by hybrid methods. Several investigators have advocated for this method, contending that this combined approach may allow for retention of the high sensitivity of CCTA while improving its specificity. Previous studies have shown that hybrid imaging may mitigate the limitations of each separate imaging modality, strengthening diagnostic certainty. Nevertheless, while such hybrid imaging was performed for this study, the widespread use of CCTA coupled with SPECT or PET will result in increased radiation exposure to the patient and may mitigate its utility in a clinical setting. We observed no incremental diagnostic value of hybrid imaging compared with stand-alone testing. Although the addition of functional imaging to CCTA improved specificity, the increase in false-negative findings affects clinical decision making in an unfavorable manner. It is expected that the addition of CT perfusion or FFR CT to CCTA for patients with an intermediate pretest likelihood of CAD will likely increase specificity at the cost of sensitivity. However, future studies are needed to determine whether hybrid CT imaging for patients at the lower spectrum of pretest probability of CAD, relying primarily on the high sensitivity and NPV of noninvasive testing, will improve accuracy and clinical decision making. However, others have argued for CT as an initial diagnostic test, maintaining the importance of ruling out CAD by CT and assessing the presence of functionally irrelevant coronary atherosclerosis, which may harbor important prognostic information, as the foremost information to be garnered from the study. In this regard, the landmark Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) trial revealed that the addition of information related to angiographic severity of stenosis and atherosclerosis may not be superior to stress testing for improving outcomes. In addition, the recently published Cardiovascular Magnetic Resonance and Single-Photon Emission Computed Tomography for Diagnosis of Coronary Heart Disease (CE-MARC 2) trial showed that the type of functional testing (ie, SPECT vs cardiac magnetic resonance) yields comparable outcome results.
Limitations
This study has some limitations. It was powered for noninferiority testing of SPECT compared with PET, whereas secondary end points of hybrid imaging should be interpreted with caution given the limited sample size. The prevalence of disease in this study was generally higher than reported in other trials of the diagnostic accuracy of noninvasive imaging to detect CAD; these results should be interpreted in the context of this particular patient population. The present findings can be extrapolated to patients at low risk of CAD in whom specificity of a test is less important. It is expected that with increasing prevalence, the NPV of imaging will increase at the cost of specificity and PPV. Patients with a low ischemic burden at nuclear imaging (ie, <10% of myocardium) could very well initially be treated conservatively with optimal medical therapy to control symptoms. Furthermore, we used [15O]H2O as a tracer agent for PET with solely quantitative flow analysis for the diagnosis of myocardial ischemia because this has proven superior over qualitative image analysis. This result has only been demonstrated, however, for this particular tracer, and these results may not be extrapolated to the more commonly used tracers [13N] ammonia and rubidium 82 in which visual grading and quantitative flow interpretation are often combined for diagnostic purposes.
Conclusions
This controlled clinical head-to-head comparative study revealed PET to exhibit the highest accuracy for diagnosis of myocardial ischemia. Furthermore, a combined anatomical and functional assessment does not add incremental diagnostic value and guides clinical decision making in an unsalutary fashion.
eAppendix. Methods
eFigure 1. Study Enrollment
eFigure 2. Three Examples of CCTA, SPECT, PET, Hybrid PET/CCTA and Angiographic Findings
eFigure 3. Flow Chart Showing the Number of Arteries Interrogated by Fractional Flow Reserve
eFigure 4. Association Between Noninvasive Cardiac Imaging and Diameter Stenosis as Assessed by Quantitative Coronary Angiography
eTable 1. Detailed Inclusion and Exclusion Criteria
eTable 2. Patient Characteristics (n = 208) by ICA, FFR, CCTA, SPECT and PET
eTable 3. Association Between Functional Extent of Coronary Artery Disease and Noninvasive Imaging
eTable 4. Cardiovascular Risk Factors, Type of Chest Pain and CCTA (A), SPECT (B), and PET (C) as Predictors of Myocardial Ischemia as Indicated by FFR
eReferences.
References
- 1.Di Carli MF, Hachamovitch R. New technology for noninvasive evaluation of coronary artery disease. Circulation. 2007;115(11):1464-1480. [DOI] [PubMed] [Google Scholar]
- 2.Gaemperli O, Bengel FM, Kaufmann PA. Cardiac hybrid imaging. Eur Heart J. 2011;32(17):2100-2108. [DOI] [PubMed] [Google Scholar]
- 3.Kajander S, Joutsiniemi E, Saraste M, et al. . Cardiac positron emission tomography/computed tomography imaging accurately detects anatomically and functionally significant coronary artery disease. Circulation. 2010;122(6):603-613. [DOI] [PubMed] [Google Scholar]
- 4.Danad I, Raijmakers PG, Appelman YE, et al. . Hybrid imaging using quantitative H215O PET and CT-based coronary angiography for the detection of coronary artery disease. J Nucl Med. 2013;54(1):55-63. [DOI] [PubMed] [Google Scholar]
- 5.Tonino PA, De Bruyne B, Pijls NH, et al. ; FAME Study Investigators . Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360(3):213-224. [DOI] [PubMed] [Google Scholar]
- 6.De Bruyne B, Pijls NH, Kalesan B, et al. ; FAME 2 Trial Investigators . Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease [published correction appears in N Engl J Med. 2012;367(18):1768]. N Engl J Med. 2012;367(11):991-1001. [DOI] [PubMed] [Google Scholar]
- 7.De Bruyne B, Fearon WF, Pijls NH, et al. ; FAME 2 Trial Investigators . Fractional flow reserve–guided PCI for stable coronary artery disease. N Engl J Med. 2014;371(13):1208-1217. [DOI] [PubMed] [Google Scholar]
- 8.Cerqueira MD, Weissman NJ, Dilsizian V, et al. ; American Heart Association Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging . Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Int J Cardiovasc Imaging. 2002;18(1):539-542. [PubMed] [Google Scholar]
- 9.Danad I, Uusitalo V, Kero T, et al. . Quantitative assessment of myocardial perfusion in the detection of significant coronary artery disease: cutoff values and diagnostic accuracy of quantitative [15O]H2O PET imaging. J Am Coll Cardiol. 2014;64(14):1464-1475. [DOI] [PubMed] [Google Scholar]
- 10.Leisenring W, Alonzo T, Pepe MS. Comparisons of predictive values of binary medical diagnostic tests for paired designs. Biometrics. 2000;56(2):345-351. [DOI] [PubMed] [Google Scholar]
- 11.Montalescot G, Sechtem U, Achenbach S, et al. ; Task Force Members; ESC Committee for Practice Guidelines; Document Reviewers . 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34(38):2949-3003. [DOI] [PubMed] [Google Scholar]
- 12.Fihn SD, Blankenship JC, Alexander KP, et al. . 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2014;130(19):1749-1767. [DOI] [PubMed] [Google Scholar]
- 13.Tonino PA, Fearon WF, De Bruyne B, et al. . Angiographic versus functional severity of coronary artery stenoses in the FAME study: fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010;55(25):2816-2821. [DOI] [PubMed] [Google Scholar]
- 14.Abdulla J, Abildstrom SZ, Gotzsche O, Christensen E, Kober L, Torp-Pedersen C. 64-Multislice detector computed tomography coronary angiography as potential alternative to conventional coronary angiography: a systematic review and meta-analysis. Eur Heart J. 2007;28(24):3042-3050. [DOI] [PubMed] [Google Scholar]
- 15.Neglia D, Rovai D, Caselli C, et al. ; EVINCI Study Investigators . Detection of significant coronary artery disease by noninvasive anatomical and functional imaging. Circ Cardiovasc Imaging. 2015;8(3):e002179. [DOI] [PubMed] [Google Scholar]
- 16.Nørgaard BL, Leipsic J, Gaur S, et al. ; NXT Trial Study Group . Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (analysis of coronary blood flow using CT angiography: next steps). J Am Coll Cardiol. 2014;63(12):1145-1155. [DOI] [PubMed] [Google Scholar]
- 17.Min JK, Leipsic J, Pencina MJ, et al. . Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA. 2012;308(12):1237-1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mc Ardle BA, Dowsley TF, deKemp RA, Wells GA, Beanlands RS. Does rubidium-82 PET have superior accuracy to SPECT perfusion imaging for the diagnosis of obstructive coronary disease?: a systematic review and meta-analysis. J Am Coll Cardiol. 2012;60(18):1828-1837. [DOI] [PubMed] [Google Scholar]
- 19.Takx RA, Blomberg BA, El Aidi H, et al. . Diagnostic accuracy of stress myocardial perfusion imaging compared to invasive coronary angiography with fractional flow reserve meta-analysis. Circ Cardiovasc Imaging. 2015;8(1):e002666. [DOI] [PubMed] [Google Scholar]
- 20.Schindler TH, Dilsizian V. PET-determined hyperemic myocardial blood flow: further progress to clinical application. J Am Coll Cardiol. 2014;64(14):1476-1478. [DOI] [PubMed] [Google Scholar]
- 21.Berman DS, Kang X, Slomka PJ, et al. . Underestimation of extent of ischemia by gated SPECT myocardial perfusion imaging in patients with left main coronary artery disease. J Nucl Cardiol. 2007;14(4):521-528. [DOI] [PubMed] [Google Scholar]
- 22.Danad I, Szymonifka J, Twisk JW, et al. . Diagnostic performance of cardiac imaging methods to diagnose ischaemia-causing coronary artery disease when directly compared with fractional flow reserve as a reference standard: a meta-analysis. Eur Heart J. 2017;38(13):991-998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Masood Y, Liu YH, Depuey G, et al. . Clinical validation of SPECT attenuation correction using x-ray computed tomography–derived attenuation maps: multicenter clinical trial with angiographic correlation. J Nucl Cardiol. 2005;12(6):676-686. [DOI] [PubMed] [Google Scholar]
- 24.Genovesi D, Giorgetti A, Gimelli A, et al. . Impact of attenuation correction and gated acquisition in SPECT myocardial perfusion imaging: results of the multicentre SPAG (SPECT Attenuation Correction vs Gated) study. Eur J Nucl Med Mol Imaging. 2011;38(10):1890-1898. [DOI] [PubMed] [Google Scholar]
- 25.Douglas PS, Hoffmann U, Patel MR, et al. ; PROMISE Investigators . Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med. 2015;372(14):1291-1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Greenwood JP, Ripley DP, Berry C, et al. ; CE-MARC 2 Investigators . Effect of care guided by cardiovascular magnetic resonance, myocardial perfusion scintigraphy, or NICE guidelines on subsequent unnecessary angiography rates: the CE-MARC 2 randomized clinical trial. JAMA. 2016;316(10):1051-1060. [DOI] [PubMed] [Google Scholar]
- 27.Kajander SA, Joutsiniemi E, Saraste M, et al. . Clinical value of absolute quantification of myocardial perfusion with 15O-water in coronary artery disease. Circ Cardiovasc Imaging. 2011;4(6):678-684. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Methods
eFigure 1. Study Enrollment
eFigure 2. Three Examples of CCTA, SPECT, PET, Hybrid PET/CCTA and Angiographic Findings
eFigure 3. Flow Chart Showing the Number of Arteries Interrogated by Fractional Flow Reserve
eFigure 4. Association Between Noninvasive Cardiac Imaging and Diameter Stenosis as Assessed by Quantitative Coronary Angiography
eTable 1. Detailed Inclusion and Exclusion Criteria
eTable 2. Patient Characteristics (n = 208) by ICA, FFR, CCTA, SPECT and PET
eTable 3. Association Between Functional Extent of Coronary Artery Disease and Noninvasive Imaging
eTable 4. Cardiovascular Risk Factors, Type of Chest Pain and CCTA (A), SPECT (B), and PET (C) as Predictors of Myocardial Ischemia as Indicated by FFR
eReferences.