Key Points
Question
Does the presence/absence of a simulated surgical task affect the acquisition of teamwork skills among midlevel surgical residents?
Findings
In this study, surgical residents who were exposed to medium-fidelity simulation team training scenarios demonstrated greater gains in teamwork skills compared with the control group and equal gains in teamwork skills compared with high-fidelity simulation groups.
Meaning
Incorporating the use of relatively inexpensive, medium-fidelity synthetic anatomy in human patient simulators was as effective as using high-fidelity anatomy from deceased donors for promoting teamwork skills among this learning group.
Abstract
Importance
The human patient simulators that are currently used in multidisciplinary operating room team training scenarios cannot simulate surgical tasks because they lack a realistic surgical anatomy. Thus, they eliminate the surgeon’s primary task in the operating room. The surgical trainee is presented with a significant barrier when he or she attempts to suspend disbelief and engage in the scenario.
Objective
To develop and test a simulation-based operating room team training strategy that challenges the communication abilities and teamwork competencies of surgeons while they are engaged in realistic operative maneuvers.
Design, Setting, and Participants
This pre-post educational intervention pilot study compared the gains in teamwork skills for midlevel surgical residents at Wake Forest Baptist Medical Center after they participated in a standardized multidisciplinary team training scenario with 3 possible levels of surgical realism: (1) SimMan (Laerdal) (control group, no surgical anatomy); (2) “synthetic anatomy for surgical tasks” mannequin (medium-fidelity anatomy), and (3) a patient simulated by a deceased donor (high-fidelity anatomy).
Interventions
Participation in the simulation scenario and the subsequent debriefing.
Main Outcomes and Measures
Teamwork competency was assessed using several instruments with extensive validity evidence, including the Nontechnical Skills assessment, the Trauma Management Skills scoring system, the Crisis Resource Management checklist, and a self-efficacy survey instrument. Participant satisfaction was assessed with a Likert-scale questionnaire.
Results
Scenario participants included midlevel surgical residents, anesthesia providers, scrub nurses, and circulating nurses. Statistical models showed that surgical residents exposed to medium-fidelity simulation (synthetic anatomy for surgical tasks) team training scenarios demonstrated greater gains in teamwork skills compared with control groups (SimMan) (Nontechnical Skills video score: 95% CI, 1.06-16.41; Trauma Management Skills video score: 95% CI, 0.61-2.90) and equivalent gains in teamwork skills compared with high-fidelity simulations (deceased donor) (Nontechnical Skills video score: 95% CI, −8.51 to 6.71; Trauma Management Skills video score: 95% CI, −1.70 to 0.49).
Conclusions and Relevance
Including a surgical task in operating room team training significantly enhanced the acquisition of teamwork skills among midlevel surgical residents. Incorporating relatively inexpensive, medium-fidelity synthetic anatomy in human patient simulators was as effective as using high-fidelity anatomies from deceased donors for promoting teamwork skills in this learning group.
This study compares the teamwork skills surgical residents and experts gained from participating in a multidisciplinary team training scenario with 3 levels of surgical realism.
Introduction
When emergencies occur in the operating room (OR), surgical team members are expected to work together to prevent adverse patient outcomes. Effective communication and teamwork are essential, and breakdowns in these areas are associated with patient harm and errors. Surgical teams with low mortality rates communicate more effectively and frequently, and team training is associated with reduced mortality rates. Surgeons also report that their greatest personal deficit is communication skills. When combined, the evidence is strong that developing communication and teamwork skills among OR personnel is essential for ensuring patient safety.
Simulation scenarios with facilitated debriefings are a recognized method for effectively teaching teamwork and communication skills, but to our knowledge, few surgical residency programs incorporate them into their curricula. Even fewer provide interdisciplinary team training, despite research suggesting that educating surgical residents about teamwork in the presence of other members of the patient care team (ie, multidisciplinary team training) is preferred over training in isolation.
One barrier to broadly implementing teamwork training for surgical residents is a lack of knowledge about the most effective ways to improve these skills. High-fidelity simulations are a promising method for building teamwork skills because they mimic low-frequency, high-risk events in a safe, learner-friendly environment; however, many simulation-based team training and crisis resource management (CRM) models were developed from an anesthesia paradigm and later translated to the training of entire surgical teams. As a result, currently used mannequin simulators cannot simulate surgical tasks because they lack realistic anatomy, thus eliminating the surgeon’s primary role in the operating room. The surgical trainee is presented with an obstacle when he or she attempts to suspend disbelief and engage in the team scenario. To our knowledge, it is unknown how separating the learner from his/her primary task affects the acquisition of teamwork skills. It is also unknown how much anatomical fidelity is needed to effectively acquire teamwork skills. To address these questions, we developed an innovative patient simulator with Synthetic Anatomy for Surgical Tasks (SAST mannequin) to meet a perceived curricular deficiency regarding the engagement and task-loading of surgical residents during CRM scenarios (eFigure in the Supplement).
Our study used this technology to compare gains in teamwork skills for midlevel surgical residents after participating in standardized multidisciplinary team training scenarios in which a simulated surgical task was performed with 3 possible levels of surgical realism: (1) SimMan (Laerdal Medical) (control group: no surgical task, no surgical anatomy), (2) SAST mannequin (surgical task, medium-fidelity anatomy); and (3) a deceased donor (surgical task, high-fidelity anatomy). The objectives were to investigate the effect of the presence/absence of a simulated surgical task and increasing levels of mannequin realism (medium- vs high-fidelity anatomy) on the acquisition of team skills among surgical residents. We hypothesized that surgical residents exposed to medium-fidelity simulation (SAST) team training would demonstrate greater gains in teamwork skills compared with the control group (SimMan) and equivalent gains in teamwork skills compared with high-fidelity simulations (deceased donors). The results provide insights concerning how simulated surgical tasks with varying degrees of realism affect team skill acquisition. They are valuable in identifying best practices for incorporating teamwork training in surgical residency curricula.
Methods
Study Participants
Scenario participants included midlevel surgical residents (postgraduate years 2 and 3), anesthesia providers, scrub nurses, and circulating nurses. All participants were recruited on a voluntary basis. Study protocols were reviewed and approved by the institutional review board of Wake Forest University Health Sciences. Fifteen surgical residents, the primary study participants, were randomized and unscripted; other participants were not randomized and were scripted to standardize the scenarios. The sample size was limited by the number of midlevel surgical residents in the general surgery residency program. Simulation-based training exercises were conducted 5 times in each experimental group, with each resident completing the training once. To investigate the ability of our metrics to discriminate between expertise levels, 6 additional training exercises (2 per group) were conducted with attending surgeons in place of surgical residents, with all other aspects unchanged.
Simulation Details and Study Design
The standardized multidisciplinary scenario simulated in this study was a blunt abdominal trauma with an exsanguinating injury requiring surgical hemorrhage control. This operative crisis scenario is associated with a high error risk, with the proper identification and treatment depending on teamwork and surgeon skill. Residents were randomly assigned to 1 of 3 groups (SimMan [control], SAST mannequin, or a deceased donor-based simulation). Because single-session training has not produced results of improved teamwork, surgical residents completed a 2-session multidisciplinary team training sequence simulating a blunt abdominal trauma operative crisis (hemorrhage from hepatic and splenic lacerations). Learning objectives, simulator settings/equipment details, the clinical data set, and discussion points were previously developed and used in our multidisciplinary CRM curriculum.
The study design was a pre-post educational intervention pilot study. The levels of teamwork competency of residents were assessed using several instruments with extensive validity evidence. The self-confidence (self-efficacy) of residents in their teamwork skills before and after the training was measured using a survey instrument. To measure the teamwork behaviors of residents during the simulated operative crisis, we used the Nontechnical Skills assessment (NOTECHS) and the Trauma Management Skills scoring system to investigate whether improvement occurred from one session to the next. The CRM checklist was used to clarify team behavior expectations, score the performance of all team members, and guide debriefings. We collected participant feedback on the training sessions using previously developed Likert-scale questionnaires (eTable 1 in the Supplement).
The detailed sequence of events for the team training exercise is given in Table 1. To enhance a sense of realism, a collaborating surgeon performed the role of a senior resident during the simulated surgery (with specific instructions regarding the limited types of assistance that they may provide to postgraduate year 2 or 3 residents), because residents at this level would not typically handle this type of case alone. The standardized team training exercise was used across all 3 experimental groups (Table 1). Residents completed the teamwork self-efficacy survey immediately before orientation and again following the case 2 debriefing. The responses were anonymous, and results were tabulated for data analysis and hypothesis testing. Two trained evaluators (attending surgeons) scored the teamwork behavior of residents during each session using the NOTECHS assessment and the Trauma Management Skills scoring system. One evaluator was present during the live session while the other viewed a videotape of the session. A third evaluator (an anesthesiologist/CRM expert) scored the performance of all team members during the scenario using the CRM checklist to provide formative feedback during debriefings.
Table 1. Outline of the Educational Intervention.
| Multidisciplinary Team Traininga | Training Activity | Training Objective | ||
| Orientiation (1 h) | Participant and faculty introductions | Orienting participants to simulation room (monitors, displays, equipment and medications available, capabilities, and the limitations of patient simulator) Completion of teamwork self-efficacy survey by study participants (completed by either a surgical resident or expert surgeon) |
Review CRM checklist to make learning objectives and expected behaviors and attitudes visible for learners and faculty members Review Plus/Delta method of constructive critique |
|
| Session 1 (1 h) | Blunt trauma scenario, liver injury (10-15 min) | During scenario, a surgical faculty member completes NOTECHS and Trauma Management Skills scoring system while observing residents. CRM checklist completed by CRM leader before debriefing. Debriefing (45 min): Team members offer reactions and feelings; faculty instructor clarifies clinical situation; participants share plusses and deltas; faculty instructor leads debriefing session by CRM checklist objectives; lessons summarized and generalized |
||
| Session 2 (1 h) | Blunt trauma scenario, spleen injury (10-15 min) | During scenario, a surgical faculty member completes NOTECHS and Trauma Management Skills scoring system while observing residents. CRM checklist completed by CRM leader before debriefing. Debriefing (45 min): Team members offer reactions and feelings; faculty instructor clarifies clinical situation; participants share Plusses and Deltas; faculty instructor leads debriefing session by CRM checklist objectives; final summary and lessons learned; completion of teamwork self-efficacy survey and participant feedback questionnaire by study participant (surgical resident or expert surgeon); completion of course evaluations |
||
| After the conclusion of the training exercise | NA | A second surgical faculty member completes NOTECHS and Trauma Management Skills scoring system while observing the video recording of the 2 sessions. | ||
| Simulation Sessions (21 Total Training Sessions) | ||||
| Training Session | Simulated Patient: SimMan (Control) | Simulated Patient: SAST Mannequin | Simulated Patient: Deceased Donor | |
| 2-Session training sequence | 1. Liver injury scenario 2. Splenic injury scenario |
1. Liver injury scenario 2. Splenic injury scenario |
1. Liver injury scenario 2. Splenic injury scenario |
|
| Teams with midlevel surgical residents (PGY 2 and PGY 3), No. | 5 | 5 | 5 | |
| Teams with expert surgeons, No. | 2 | 2 | 2 | |
Abbreviations: CRM, crisis resource management; NA, not applicable; NOTECHS, Nontechnical Skills assessment; PGY, postgraduate year; SAST, Synthetic Anatomy for Surgical Tasks.
A blunt abdominal trauma with an exsanguinating injury requiring surgical control of bleeding.
Statistical Analysis
All of the tests were 2-sided with significance level of .05. The post-training competency average and item scores for the 3 simulators were compared using analysis of covariance, adjusting for pre-training scores. Linear contrasts were used to conduct the pairwise comparison of the 3 simulators based on the analysis of covariance model results, and all tests were adjusted for multiple comparisons (Tukey method). For assessments conducted by multiple expert evaluators (live vs video), inter-rater reliability was evaluated by weighted Cohen κ. The reliability of assessments in measuring the construct of interest (internal consistency between questionnaire categories) was determined by Cronbach α.
Evaluators were necessarily familiar with residents before the educational intervention because of the available surgical faculty. The randomization of residents across groups was used to minimize the potential for bias from preconceived notions regarding resident communication strengths and weaknesses. In addition, using case 1 scores as a covariate was used to mitigate this potential, because any preconceived opinions would likely be present in both case 1 and 2, regardless of mannequin assignment.
To evaluate our results for evidence of validity, we compared 2 levels of surgical expertise (intermediate vs expert) on pre-post assessments and team behavior measures (Table 2). Contrasts were built from analysis of covariance models to detect differences between expertise levels, and Tukey adjustments were made for multiple comparisons.
Table 2. Multiple Comparisons for Treatment Groups (Deceased Donor, SAST) vs Control (SimMan).
| Response Variable | 95% CI | |||
|---|---|---|---|---|
| Deceased Donor–Control | SAST-Control | Deceased Donor–SAST | Expert-Resident | |
| Participant feedback score | 16.79-35.21a | 10.21-28.64a | −2.64 to 15.79 | −2.48 to 11.22 |
| Self-efficacy score (post-case 2) | −7.78 to 13.39 | −12.68 to 8.49 | −5.69 to 15.49 | −6.84 to 10.82 |
| NOTECHS live score (case 2) | −4.35 to 5.78 | −3.10 to 7.04 | −6.31 to 3.80 | −5.05 to 3.76 |
| NOTECHS video score (case 2) | 0.62-15.05a | 1.06-16.41a | −8.51 to 6.71 | −7.82 to 6.60 |
| Trauma Management Skills live score (case 2) | −1.37 to 1.54 | −1.11 to 2.00 | −1.89 to 1.17 | −0.34 to 2.49 |
| Trauma Management Skills video score (case 2) | 0.02-2.28a | 0.61-2.90a | −1.70 to 0.49 | −0.77 to 1.39 |
| CRM checklist score (case 2) | −0.88 to 2.91 | −0.68 to 3.07 | −2.08 to 1.72 | −0.52 to 2.48 |
Abbreviations: CRM, crisis resource management; NOTECHS, Nontechnical Skills assessment; SAST, Synthetic Anatomy for Surgical Tasks.
Statistically significant differences, corresponding to 95% CIs that do not contain zero.
Results
Statistical results show that for 3 assessment metrics (participant feedback, NOTECHS video, Trauma Management Skills video) the control group (SimMan) had worse results compared with the other 2 groups while the 2 treatment groups (SAST, deceased donor) were not statistically different from each other for any metric (Table 2). Specifically, for 3 metrics (participant feedback, NOTECHS video, Trauma Management Skills video), the 95% CIs did not contain zero for deceased donor vs control group comparisons (16.79-35.21, 0.62-15.05, and 0.02-2.28, respectively) or for SAST vs control group comparisons (10.21-28.64, 1.06-16.41, and 0.61-2.90, respectively), with Tukey adjustments for multiple comparisons. These findings support the study hypotheses that surgical residents exposed to medium-fidelity simulation (SAST) team training scenarios would demonstrate greater gains in teamwork skills compared with the control group (SimMan) and equal gains in teamwork skills compared with high-fidelity simulations (deceased donors).
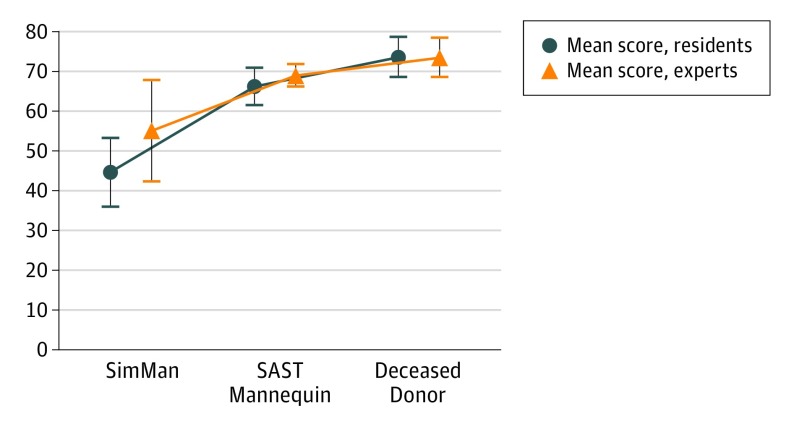
Total participant feedback scores from surgical residents and expert surgeons were tabulated and grouped by simulation type (maximum possible score = 80) (Figure 1). Results showed significantly higher participant feedback scores among groups in simulations with SAST and deceased donors compared with the control group (Table 2). The highest scores were from residents in high-fidelity simulations with deceased donors and the lowest scores were from the simulations with the low-fidelity control mannequin.
Figure 1. Average Scores From the Participant Feedback Questionnaire.
The questionnaire assessed the satisfaction of participants with the simulation. The maximum score was 80 points. The error bars are ±1 SD. SAST indicates synthetic anatomy for surgical tasks.
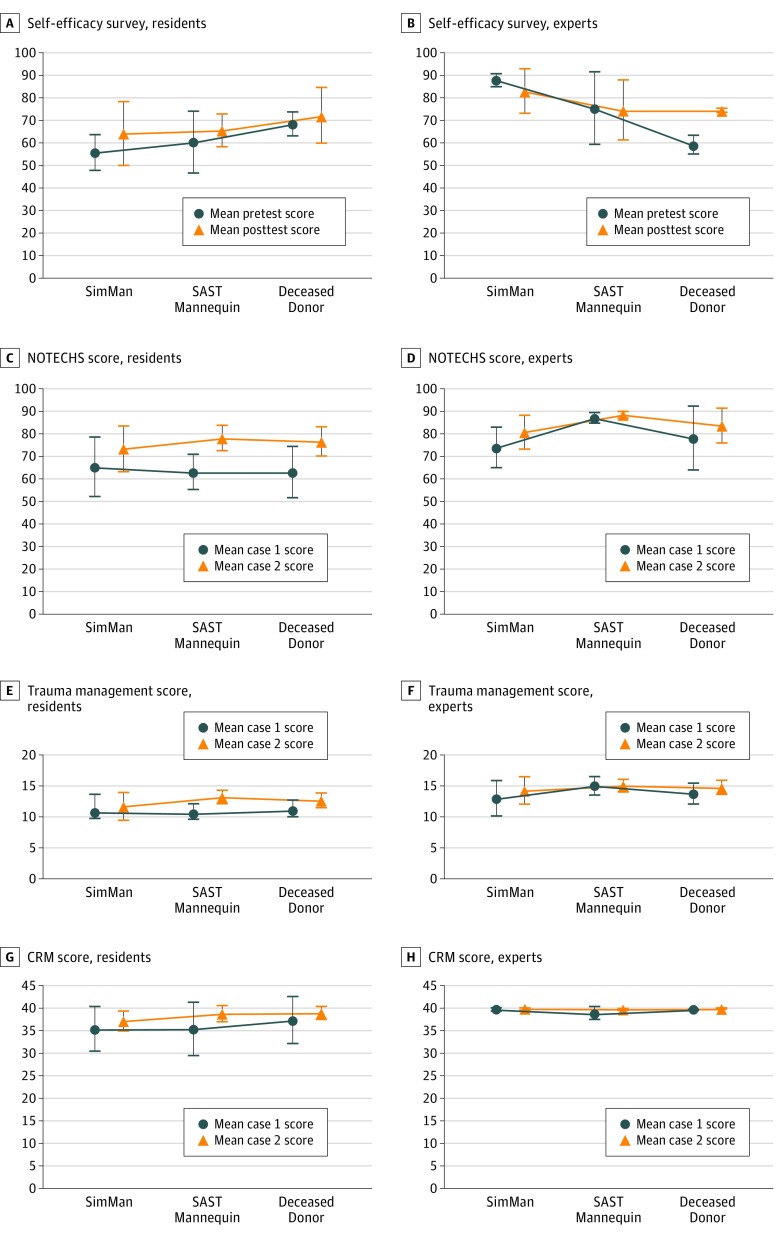
For the Surgeon Self-Efficacy questionnaire, the mean pre- and posttraining results of 90 possible points are given in Figure 2A and B. Surgical residents showed lower scores overall than expert surgeons, as expected. There were no statistically significant differences between treatment groups.
Figure 2. Results From the Teamwork Competency Assessment Instruments.
All error bars are ±1 SD. Mean scores from the Surgeon Self-efficacy questionnaire among residents (A) and experts (B), used to assess a participant’s confidence in his or her teamwork skills before and after training. Mean scores from Nontechnical Skills Assessment (NOTECHS) questionnaire for residents (C) and experts (D) and mean scores from the Trauma Management Skills assessment for residents (E) and experts (F). Scores from in-person and video-based evaluations are pooled in these plots. Mean scores from crisis resource management (CRM) checklist for residents (G) and experts (H) are used for a formative assessment of team performance. SAST indicates synthetic anatomy for surgical tasks.
For the NOTECHS assessment, mean total scores of 90 possible points are shown in Figure 2C and D. Statistical comparisons showed significantly higher NOTECHS case 2 video scores among groups in simulations with SAST and deceased donors compared with the control group, with the case 1 score serving as a numerical covariate (Table 2). Thus, the groups in simulations with SAST and deceased donors showed significantly greater gains in teamwork skills from case 1 to case 2 compared with the control (SimMan) group. It was noted that the control group scored poorly on the vigilance and leadership subscales of the NOTECHS instrument. No statistically significant difference was observed between gains in teamwork skills for the groups in simulations with SAST and deceased donors. In general, expert surgeons scored higher than residents; however, the difference between experts and residents was not statistically significant (Table 2).
For the Trauma Management Skill assessment, the mean results of 15 possible points are shown in Figure 2E and F. Statistical results again showed significantly higher Trauma Management case 2 video scores in groups in simulations with SAST and deceased donors as compared with the control group, with the case 1 score serving as a numerical covariate (Table 2). Thus, this assessment metric also found that the groups in simulations with SAST and deceased donors showed significantly greater gains in teamwork skills from case 1 to case 2 compared with the control (SimMan) group. No statistically significant difference was observed between gains in teamwork skills for the groups in simulations with SAST and deceased donors. Expert surgeons scored higher overall than residents, as expected, but the difference between expert and resident was not statistically significant (Table 2).
The mean CRM checklist scores (of 40 possible points) for resident- and expert-led simulation sessions are shown in Figure 2G and H. Surgical residents showed lower scores overall than expert surgeons, as expected. There were no statistically significant differences between treatment groups (Table 2).
The internal consistency of each instrument was evaluated using Cronbach α (Table 3). Of 13 α values, 12 were good (0.7 ≤α <0.9) to excellent (α ≥ 0.9), and 1 was low (α < 0.6) (Table 3). The low α value (CRM checklist, case 2) could be because of the instrument having a small number of possible categories per item, which can deflate the α value. Overall, the results show a good assessment reliability and a sound basis for confidence in the internal consistency of the scores.
Table 3. Evaluation of Internal Consistency (Cronbach α) and Interrater Reliability (Cohen κ).
| Assessment | Cronbach α |
|---|---|
| Internal Consistency for Different Assessments | |
| Pre self-efficacy scores | .88 |
| Case 1 Trauma Management Skills scores, live | .81 |
| Case 1 Trauma Management Skills scores, video | .83 |
| Case 1 NOTECHS scores, live | .94 |
| Case 1 NOTECHS scores, video | .97 |
| Case 1 CRM checklist scores | .88 |
| Post self-efficacy scores | .97 |
| Case 2 Trauma Management Skills scores, live | .86 |
| Case 2 Trauma Management Skills scores, video | .78 |
| Case 2 NOTECHS scores, live | .93 |
| Case 2 NOTECHS scores, video | .96 |
| Case 2 CRM checklist scores | .57 |
| Participant feedback scores | .92 |
| Interrater Reliability for Live vs Video Scores | |
| Assessment | Weighted Cohen κ |
| Case 1 Trauma Management Skills scores | .33 |
| Case 1 NOTECHS scores | .35 |
| Case 2 Trauma Management Skills scores | .28 |
| Case 2 NOTECHS scores | .35 |
Abbreviations: CRM, crisis resource management; NOTECHS, Nontechnical Skills assessment.
As described earlier, 2 trained evaluators (attending surgeons) scored each participant’s teamwork behavior during each session using the NOTECHS assessment and the Trauma Management Skills scoring system. One evaluator was present while the other viewed a videotape. Therefore, the inter-rater consistency of live vs video scores was evaluated using weighted Cohen κ, in which κ values of 0 to 0.20 represent “slight” agreement, values between 0.21 and 0.40 are “fair,” values between 0.41 and 0.60 are “moderate,” values between 0.61 and 0.80 are “good,” and values between 0.81 and 1.0 are “excellent.” The results indicate a fair consistency between live and video scores (Table 3).
Discussion
Previous research indicates a positive relationship between technical and nontechnical performance in surgeons. For example, Black and colleagues showed significant correlation between technical skills and nontechnical skills using a commercially available benchtop model of a carotid bifurcation combined with trained actors portraying an awake carotid endarterectomy. Recently published results of a simulator–based curriculum for surgical residents and multidisciplinary trauma team members demonstrated significant improvements in teamwork as well as speed and completing blunt trauma resuscitations in the emergency department. This study showed improvements in nontechnical and technical skills over the course of the 4-hour simulation curriculum. We hypothesized that the relationship goes both ways, meaning that a surgical task would allow surgeons to be more effectively engaged in their role and better develop their decision making, situational awareness, communication, and other team skills. Teamwork and communication skills are context specific, but our results indicate that having full realism, like a deceased donor, may not be mandatory. Hybrid models such as this one can achieve gains in team performance while providing an appropriate context for the surgical trainee.
Our results showed that surgical residents exposed to medium-fidelity simulation (SAST) team training demonstrated greater gains in teamwork skills compared with the control group (SimMan) and equivalent gains in teamwork skills compared with those in high-fidelity simulations (deceased donors). Two main findings can be drawn from these results. First, including a surgical task in multidisciplinary OR team training significantly enhanced the acquisition of teamwork skills among midlevel surgical residents. Second, incorporating relatively inexpensive, medium-fidelity synthetic anatomy in human patient simulators was as effective as using high-fidelity anatomies from deceased donors for promoting teamwork skills in this learning group. This knowledge will be beneficial in identifying the best strategies for building teamwork skills in surgical residents and OR team members. The Accreditation Council for Graduate Medical Education Common Program Requirements for training residents are currently under revision. The proposed revised requirements in Section VI.A.1.a)(3).b. require that “the program director must design and maintain a program that has a structure that promotes team-based care” and that “residents must participate as team members in real and/or simulated interprofessional clinical site-sponsored patient safety activities.” Our results may help guide surgical programs in satisfying these requirements and training residents to work safely in interprofessional teams by including models and scenarios that simulate a surgical task while not requiring the use of deceased donors, which might be cost-prohibitive for some smaller programs.
Statistically significant differences in resident performance, as measured by the NOTECHS and Trauma Management Skills assessment metrics, were detected only in video evaluations and not in live evaluations. Since the statistically significant differences appeared in the same pattern for multiple assessment metrics (Table 2), it is unlikely that these differences are because of chance. Our findings suggest that a genuine difference exists between data contained in the video evaluations vs live evaluations. This reasoning is supported by the fact that the agreement between the live vs video evaluations was only “fair” according to a weighted Cohen κ analysis (Table 3). It is possible that when surgical faculty evaluators conducted video assessments they had more time to complete the assessment and fewer demands for their attention. Other authors argued that while debriefing at the time of the event is necessary to provide immediate feedback, a delayed review via videotape allows more time for discussion and self-assessment by the learner and frees raters to evaluate residents on demand. Further research is needed to investigate the comparative benefits and limitations of live vs video review.
There were no statistically significant differences between surgical expertise levels (expert vs resident), which suggests that the educational intervention in this study was unable to distinguish between expertise levels (Table 2). However, in most cases the surgical residents scored lower than the expert surgeons on the self-efficacy survey, the NOTECHS assessment, the Trauma Management Skill assessment, and the CRM checklist (Figure 2). It is possible that the inability to detect significant differences between expertise levels was because of the relatively small number of study participants (n = 5 residents and n = 2 experts per group).
The evaluation instruments were chosen to assess teamwork using multiple measurement tools. Participant feedback questionnaires were used to gauge the reaction and degree of satisfaction of participants, surgeon self-efficacy questionnaires were used to measure changes in the attitudes of participants, and the NOTECHS assessment, Trauma Management Skill assessment, and CRM checklist were used to evaluate behavior changes. Together, these measurement tools span levels 1 to 3 of the Kirkpatrick hierarchy of training evaluation, and this breadth of evaluation drove the selection of these assessments (eTable 2 in the Supplement). In practice, all but 1 of the assessments had good to excellent reliability scores as measured by Cronbach α (Table 3). Reliability has been defined as the ability of an instrument to measure consistently, and Cronbach α is the most widely used objective measure of reliability. It describes the internal consistency of an assessment tool, or the extent to which all items in a test measure the same concept or construct. Therefore, there is a sound basis for confidence in the assessment instruments used in this study.
Limitations
This study had several limitations. It was a single-institution study, limiting its applicability in other settings. The sample size was limited by the available surgical resident population, and inte-rater reliability between video and in-person assessments was lower than expected. Lastly, while team factors were controlled to the largest extent possible by using scripting and standardized scenarios, it is possible that team factors played a role in the suspension of disbelief and engagement.
Conclusions
This work provides valuable new information about the importance of including a surgical task in multidisciplinary OR team training. Medium-fidelity synthetic surgical anatomy was sufficient to produce significantly greater gains in team skills for surgical residents, and this finding has implications for future efforts to define optimal teamwork training regimes in surgical residency curricula.
eFigure. SAST Mannequin Design.
eTable 1. Participant Feedback Questionnaire.
eTable 2. Kirkpatrick’s Hierarchy of Evaluation
References
- 1.Catchpole K, Mishra A, Handa A, McCulloch P. Teamwork and error in the operating room: analysis of skills and roles. Ann Surg. 2008;247(4):699-706. [DOI] [PubMed] [Google Scholar]
- 2.Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care. 2004;13(suppl 1):i85-i90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Christian CK, Gustafson ML, Roth EM, et al. A prospective study of patient safety in the operating room. Surgery. 2006;139(2):159-173. [DOI] [PubMed] [Google Scholar]
- 4.Neily J, Mills PD, Young-Xu Y, et al. Association between implementation of a medical team training program and surgical mortality. JAMA. 2010;304(15):1693-1700. [DOI] [PubMed] [Google Scholar]
- 5.Young GJ, Charns MP, Daley J, Forbes MG, Henderson W, Khuri SF. Best practices for managing surgical services: the role of coordination. Health Care Manage Rev. 1997;22(4):72-81. [DOI] [PubMed] [Google Scholar]
- 6.Arriaga AF, Gawande AA, Raemer DB, et al. ; Harvard Surgical Safety Collaborative . Pilot testing of a model for insurer-driven, large-scale multicenter simulation training for operating room teams. Ann Surg. 2014;259(3):403-410. [DOI] [PubMed] [Google Scholar]
- 7.Rudolph JW, Simon R, Dufresne RL, Raemer DB. There’s no such thing as “nonjudgmental” debriefing: a theory and method for debriefing with good judgment. Simul Healthc. 2006;1(1):49-55. [DOI] [PubMed] [Google Scholar]
- 8.Association of American Medical Colleges Trauma team training: multidisciplinary training for trauma management. https://www.mededportal.org/publication/8267. Accessed July 28, 2016.
- 9.Knudson MM, Khaw L, Bullard MK, et al. Trauma training in simulation: translating skills from SIM time to real time. J Trauma. 2008;64(2):255-263. [DOI] [PubMed] [Google Scholar]
- 10.Larkin AC, Cahan MA, Whalen G, et al. Human Emotion and Response in Surgery (HEARS): a simulation-based curriculum for communication skills, systems-based practice, and professionalism in surgical residency training. J Am Coll Surg. 2010;211(2):285-292. [DOI] [PubMed] [Google Scholar]
- 11.Pronovost PJ, Freischlag JA. Improving teamwork to reduce surgical mortality. JAMA. 2010;304(15):1721-1722. [DOI] [PubMed] [Google Scholar]
- 12.Paige JT, Kozmenko V, Yang T, et al. Attitudinal changes resulting from repetitive training of operating room personnel using of high-fidelity simulation at the point of care. Am Surg. 2009;75(7):584-590. [PubMed] [Google Scholar]
- 13.Paige J, Kozmenko V, Morgan B, et al. From the flight deck to the operating room: an initial pilot study of the feasibility and potential impact of true interdisciplinary team training using high-fidelity simulation. J Surg Educ. 2007;64(6):369-377. [DOI] [PubMed] [Google Scholar]
- 14.Carter JE, Chang MC, Bodin SG, et al. Team training in the operating room: the development of a multidisciplinary curriculum. J Am Coll Surg. 2008;207(3):S94. dx.doi.org/ 10.1016/j.jamcollsurg.2008.06.237 [DOI] [Google Scholar]
- 15.Zausig YA, Grube C, Boeker-Blum T, et al. Inefficacy of simulator-based training on anesthesiologists’ non-technical skills. Acta Anaesthesiol Scand. 2009;53(5):611-619. [DOI] [PubMed] [Google Scholar]
- 16.Sevdalis N, Davis R, Koutantji M, Undre S, Darzi A, Vincent CA. Reliability of a revised NOTECHS scale for use in surgical teams. Am J Surg. 2008;196(2):184-190. [DOI] [PubMed] [Google Scholar]
- 17.Marshall RL, Smith JS, Gorman PJ, Krummel TM, Haluck RS, Cooney RN. Use of a human patient simulator in the development of resident trauma management skills. J Trauma. 2001;51(1):17-21. [DOI] [PubMed] [Google Scholar]
- 18.Black SA, Nestel DF, Kneebone RL, Wolfe JHN. Assessment of surgical competence at carotid endarterectomy under local anaesthesia in a simulated operating theatre. Br J Surg. 2010;97(4):511-516. [DOI] [PubMed] [Google Scholar]
- 19.Steinemann S, Berg B, Skinner A, et al. In situ, multidisciplinary, simulation-based teamwork training improves early trauma care. J Surg Educ. 2011;68(6):472-477. [DOI] [PubMed] [Google Scholar]
- 20.Accreditation Council for Graduate Medical Education ACGME common program requirements: section VI: proposed major revisions. http://www.acgme.org/Portals/0/PFAssets/ReviewandComment/CPR_SectionVI_ChangesTracked.pdf. Accessed February 20, 2017.
- 21.House JB, Dooley-Hash S, Kowalenko T, et al. Prospective comparison of live evaluation and video review in the evaluation of operator performance in a pediatric emergency airway simulation. J Grad Med Educ. 2012;4(3):312-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kirkpatrick DL. Evaluation of training In: Craig R, Mittel I, eds. Training and Development Handbook. New York, NY: McGraw Hill; 1967. [Google Scholar]
- 23.Tavakol M, Mohagheghi MA, Dennick R. Assessing the skills of surgical residents using simulation. J Surg Educ. 2008;65(2):77-83. [DOI] [PubMed] [Google Scholar]
- 24.Tavakol M, Dennick R. Making sense of Cronbach’s α. Int J Med Educ. 2011;2:53-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. SAST Mannequin Design.
eTable 1. Participant Feedback Questionnaire.
eTable 2. Kirkpatrick’s Hierarchy of Evaluation