Key Points
Question
Does hospital inpatient treatment with electroconvulsive therapy reduce 30-day psychiatric readmission risk in individuals with severe affective disorders?
Findings
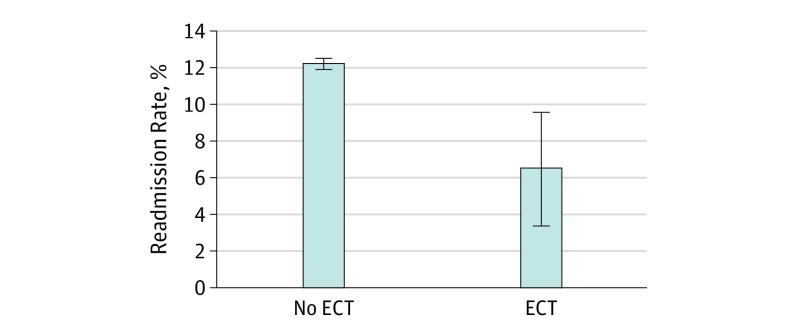
In this quasi-experimental study that included 162 691 inpatients with severe affective disorders in 9 states, the adjusted predicted proportion readmitted within 30 days was 6.6% among individuals who underwent electroconvulsive therapy and 12.3% among those who did not receive electroconvulsive therapy, which was a statistically significant difference.
Meaning
Electroconvulsive therapy may be associated with reduced short-term psychiatric inpatient readmissions among patients with severe affective disorders.
Abstract
Importance
Although electroconvulsive therapy (ECT) is considered the most efficacious treatment available for individuals with severe affective disorders, ECT’s availability is limited and declining, suggesting that information about the population-level effects of ECT is needed.
Objective
To examine whether inpatient treatment with ECT is associated with a reduction in 30-day psychiatric readmission risk in a large, multistate sample of inpatients with severe affective disorders.
Design, Setting, and Participants
A quasi-experimental instrumental variables probit model of the association correlation of ECT administration with patient risk of 30-day readmission was estimated using observational, longitudinal data on hospital inpatient discharges from US general hospitals in 9 states. From a population-based sample of 490 252 psychiatric inpatients, a sample was drawn that consisted of 162 691 individuals with a principal diagnosis of major depressive disorder (MDD), bipolar disorder, or schizoaffective disorder. The key instrumental variable used in the analysis was ECT prevalence in the prior calendar year at the treating hospital. To examine whether ECT’s association with readmissions was heterogeneous across population subgroups, analyses included interactions of ECT with age group, sex, race/ethnicity, and diagnosis group. The study was conducted from August 27, 2015, to March 7, 2017.
Main Outcome and Measures
Readmission within 30 days of being discharged.
Results
Overall, 2486 of the 162 691 inpatients (1.5%) underwent ECT during their index admission. Compared with other inpatients, those who received ECT were older (mean [SD], 56.8 [16.5] vs 45.9 [16.5] years; P < .001) and more likely to be female (65.0% vs 54.2%; P < .001) and white non-Hispanic (85.3% vs 62.1%; P < .001), have MDD diagnoses (63.8% vs 32.0%; P < .001) rather than bipolar disorder (29.0% vs 40.0%; P < .001) or schizoaffective disorder (7.1% vs 28.0%; P < .001), have a comorbid medical condition (31.3% vs 26.6%; P < .001), have private (39.4% vs 21.7%; P < .001) or Medicare (49.2% vs 39.4%; P < .001) insurance coverage, and be located in urban small hospitals (31.2% vs 22.3%; P < .001) or nonurban hospitals (9.0% vs 7.6%; P = .02). Administration of ECT was associated with a reduced 30-day readmission risk among psychiatric inpatients with severe affective disorders from an estimated 12.3% among individuals not administered ECT to 6.6% among individuals administered ECT (risk ratio [RR], 0.54; 95% CI, 0.28-0.81). Significantly larger associations with ECT on readmission risk were found for men compared with women (RR, 0.44; 95% CI, 0.20-0.69 vs 0.58; 95% CI, 0.30-0.88) and for individuals with bipolar disorder (RR, 0.42; 95% CI, 0.17-0.69) and schizoaffective disorder (RR, 0.44; 95% CI, 0.11-0.79) compared with those who had MDD (RR, 0.53; 95% CI, 0.26-0.81).
Conclusions and Relevance
Electroconvulsive therapy may be associated with reduced short-term psychiatric inpatient readmissions among psychiatric inpatients with severe affective disorders. This potential population health effect may be overlooked in US hospitals’ current decision making regarding the availability of ECT.
This population-based study compares psychiatric hospital readmission in patients with severe affective disorders based on receipt of electroconvulsive therapy.
Introduction
The limited and regionally variable availability of electroconvulsive therapy (ECT) in US hospitals is a curious phenomenon in view of ECT’s unique clinical benefits. Electroconvulsive therapy is considered the most efficacious treatment available for individuals with severe affective disorders, yet ECT is not used during inpatient care in nearly 9 of 10 US hospitals, and its use in these settings has declined over the past 2 decades. Factors speculated to impede ECT’s availability include stringent regulatory restrictions on its use, limited graduate medical training, persistent concerns among mental health consumers about ECT’s safety and adverse effects despite contemporary improvements in the procedure’s safety and adverse effect profile, stigma, reluctance among medical professionals to recommend ECT, and cost considerations. Electroconvulsive therapy also may be comparatively less accessible to individuals who live in rural and low-income urban areas, patients from minority racial/ethnic backgrounds, and those who have Medicaid insurance coverage or are uninsured. However, despite recent evidence that greater use of ECT may have important population health benefits, little research has examined whether the limited availability of ECT has any adverse effects on population health.
Research studies that demonstrate how the availability of ECT may affect health outcomes in a population are needed to help policymakers contextualize the need for ECT to be more accessible. Ahmadi and colleagues used a matched case-control study to compare outcomes for 92 patients with both major depressive disorder (MDD) and posttraumatic stress disorder from a large urban US Department of Veterans Affairs hospital who underwent ECT to the outcomes 3393 patients with MDD and posttraumatic stress disorder who did not receive ECT. During an 8-year follow-up period, ECT was associated with a lower risk of all-cause mortality and suicidality independent of antidepressant therapy utilization. To our knowledge, that study is the only such comparative effectiveness study in an entire patient population. However, as a consequence of its sample being drawn from a single Veterans Affairs hospital, its results have limited generalizability. Further research on ECT’s effects in broader population samples of hospital patients are needed to address this gap.
The present study used hospital inpatient census data from 9 states to examine whether greater ECT utilization results in fewer 30-day psychiatric inpatient readmissions among patients with severe affective disorders (ie, MDD, bipolar disorder, and schizoaffective disorder). The rate of inpatient readmission within 30 days following discharge from psychiatric inpatient care is frequently used as a standardized metric of mental health system performance, with a higher rate indicating worse performance. Based on prior clinical studies’ results indicating that ECT treatment may reduce suicidal thinking and other symptoms of severe affective disorders, we hypothesized that, compared with similar psychiatric inpatients with severe affective disorders, those who were treated with ECT would have a lower probability of readmission within 30 days. We also examined heterogeneity in the magnitude of ECT’s effects on readmissions by patient age group, sex, race/ethnicity, and diagnosis group. A unique aspect of our study design compared with prior observational studies of ECT’s effects is that we used a quasi-experimental approach based on geographic, hospital, and insurance variation in access to inpatient treatment with ECT to minimize confounding from unmeasured patient-level characteristics that may affect both the likelihood of ECT treatment and study outcomes.
Methods
Data Source
The sample was drawn from the Health Care Utilization Project’s State Inpatient Databases (SID) from Arizona, Arkansas, California, Florida, Nevada, New York, North Carolina, Utah, and Washington for persons aged 18 years or older. The SID are statewide censuses of all hospital stays in private and public nonfederal, short-term general hospitals. SID contain hospitals’ electronic abstracts of inpatient stays, which include demographic information collected at admission, diagnoses, length of stay, procedure codes, and other information that is typically used for billing purposes. Although SID are available for most states, complete SID Revisit File data, which include a personal identification number needed to identify readmissions and hospital identification numbers needed to construct a measure of ECT availability, were available only for these 9 states. The most recent data year available for each state at the time of the study was used (2007: Arizona and Nevada; 2009: New York and Utah; and 2010: Arkansas, California, Florida, North Carolina, and Washington). The study was conducted from August 27, 2015, to March 7, 2017. The study data are fully deidentified, and consequently the study was deemed exempt from informed consent by study participants by the University of Maryland School of Medicine Institutional Review Board.
The initial sample contained inpatient admissions records for 490 252 unique patients who were hospitalized and then discharged at least once during the specified calendar year. We then selected all 171 970 patients who had a principal International Classification of Diseases, Ninth Revision (ICD-9) diagnosis code for a severe affective disorder, including MDD (ICD-9 codes 296.2 and 296.3), bipolar disorder (ICD-9 codes 296.4, 296.5, 296.6, 296.7, 296.8, and 296.9), and schizoaffective disorder (ICD-9 code 295.7). An additional 7655 patients with missing hospital identification numbers and 1624 patients who did not receive ECT and whose inpatient lengths-of-stay fell outside the range of lengths-of-stay among ECT cases were also excluded, leaving a final sample of 162 691 patients (2486 ECT cases and 160 205 non-ECT cases). Two-hundred fifty-eight ECT cases were among the excluded observations. Of these, 123 (47.7%) had missing hospital identification numbers, and 135 (52.3%) had various principal diagnoses not specifically indicated for ECT treatment (eg, dementia, substance use, sexual dysfunction, and depression not otherwise specified).
Measures
Dependent and Independent Variables
The readmission measure was a binary indicator of whether an individual had another inpatient admission to any hospital in the state with a primary psychiatric diagnosis ICD-9 code in the range 290-319 within 30 days of being discharged after the index admission. The independent variable of interest was an indicator of whether the patient was administered ECT during the hospital stay based on an ICD-9 procedure code of 94.27.
Covariates
Following the Andersen sociobehavioral model, the determinants of ECT use and readmission included predisposing factors, including age, sex (male/female), and race/ethnicity (white non-Hispanic, black non-Hispanic, Hispanic, and other); enabling factors, including whether the patient had a diagnosis of a medical comorbidity that increases the relative health risks of ECT (intracranial lesions, masses, inflammation, infection, or hemorrhage; hemorrhagic stroke; myocardial infarction; dysrhythmias; malfunctioning cardiac device; valvular disease; heart failure; epilepsy; dementia; and other contraindications to anesthesia), source of payment (private insurance, Medicare, Medicaid, other insurance, and uninsured), whether the stay was at a hospital that delivers ECT, hospital location (state) and size (urban medium or large, urban small, not urban, and unknown), and need for ECT, including primary psychiatric diagnosis, substance use disorder diagnosis, and the length-of-stay of the index admission. A binary indicator for December discharges, for which information on readmission was censored, was also included in regression analyses.
Statistical Analysis
Quasi-Experimental Model
In this observational study, the effects of unmeasured patient-level factors, such as treatment refractoriness, on the likelihood of treatment with ECT pose a significant challenge for accurately assessing the effectiveness of ECT in a large patient population. Most observational study designs, such as matched case-control, least squares, and propensity score matching, are vulnerable to confounding attributable to unmeasured characteristics that affect both treatment selection and treatment outcome. This study uses a quasi-experimental approach, an empirical approach to estimate the causal impact of an intervention on its target population without random assignment. An instrumental variables (IV) probit model based on geographic and hospital variation in the prevalence of inpatient treatment with ECT in a prior year was used in this study to minimize estimation bias from unmeasured patient-level selection (eAppendix 1 in the Supplement). The key instrumental variable was a hospital’s mean proportion of inpatients treated with ECT, which was estimated using data on a different sample of inpatient episodes at the same hospital in the prior calendar year. The validity of this instrument depends on whether access to ECT is affected predominantly by attributes of the treating hospital and its geographic location, with such billing requirements and regulations governing the use of ECT. These factors are presumed to be largely independent of a patient’s preexisting propensity for readmission. The estimated effects of ECT are reported as adjusted relative risk ratios (RRs) of psychiatric inpatient readmission for individuals who undergo ECT compared with those who do not receive ECT. Heteroskedasticity-robust variance estimators were used in all regression models.
Treatment Effect Heterogeneity
To examine whether the effects of ECT on readmissions were heterogeneous across population subgroups, supplemental regression analyses included interactions between ECT and indicators for age 65 years or older, sex, race/ethnicity, and diagnosis group.
Poststratification Weighting and Length of Stay
Poststratification weighting was used to calibrate the lengths of stay in the non-ECT group to the lengths-of-stay distribution in the ECT group. This adjustment was made to ensure valid mean comparisons of readmission risk because inpatient delivery of ECT is associated with longer-than-average stays, which in turn are associated with lower-than-average readmission risk. Poststratification weighting ensured that the weighted lengths-of-stay distributions in the non-ECT group closely resembled those in the ECT group. The weights were constructed by stratifying the lengths-of-stay distribution in the ECT group and then forming the ratios of the stratified sample proportions in the ECT and non-ECT groups. All analyses were conducted using the weighted sample. Statistical analysis was conducted using Stata, version 14. A 5% level of significance was used with unpaired, 2-tailed tests.
Results
Descriptive Analyses
Among all 162 691 inpatients, 2486 (1.5%) underwent ECT during their index admission. Compared with other inpatients, those who received ECT were older and more likely to be female and white non-Hispanic, to have MDD diagnoses rather than either bipolar disorder or schizoaffective disorder, to have private or Medicare insurance coverage, and to be located in urban small hospitals and nonurban hospitals (Table 1). Counterintuitively, ECT was administered more often to patients who had diagnoses indicating comorbid medical illnesses that may increase the relative health risks of ECT, possibly reflecting greater medical comorbidity in the group with ECT treatment or more frequent documentation of medical comorbidities among inpatients who are medically screened prior to ECT.
Table 1. Weighted Sample Characteristicsa.
| Characteristic | No. (%) | Fb | P Value | ||
|---|---|---|---|---|---|
| Overall (N = 162 691) |
No ECT (n = 160 205) |
ECT (n = 2486) |
|||
| Age, mean (SD), y | 46.1 (16.6) | 45.9 (16.5) | 56.8 (16.5) | 1024.5 | <.001 |
| Women | 90 655 (54.4) | 89 038 (54.2) | 1617 (65.0) | 112.1 | <.001 |
| Race/ethnicity | |||||
| White, non-Hispanic | 107 152 (62.4) | 105 031 (62.1) | 2121 (85.3) | 989.9 | <.001 |
| Black, non-Hispanic | 21 715 (15.8) | 21 632 (16.0) | 83 (3.3) | 1034.0 | <.001 |
| Hispanic | 18 376 (10.4) | 18 254 (10.5) | 122 (4.9) | 152.4 | <.001 |
| Other | 15 448 (11.4) | 15 288 (11.4) | 160 (6.4) | 96.0 | <.001 |
| Diagnosis group | |||||
| MDD | 68 287 (32.5) | 66 700 (32.0) | 1587 (63.8) | 507.0 | <.001 |
| Bipolar disorder | 65 961 (39.9) | 65 239 (40.0) | 722 (29.0) | 1056.0 | <.001 |
| Schizoaffective disorder | 28 443 (27.6) | 28 266 (28.0) | 177 (7.1) | 396.8 | <.001 |
| Substance use disorder | 64 265 (34.4) | 63 812 (34.7) | 453 (18.2) | 425.9 | <.001 |
| Medical comorbidityc | 39 978 (26.7) | 39 201 (26.6) | 777 (31.3) | 24.0 | <.001 |
| Length of stay, mean (SD), d | 20.6 (20.1) | 20.6 (20.1) | 20.7 (19.4) | 0.3 | .87 |
| Source of paymentd | |||||
| Private insurance | 48 633 (22.0) | 48 137 (21.7) | 979 (39.4) | 317.3 | <.001 |
| Medicare | 47 884 (39.5) | 46 982 (39.4) | 1223 (49.2) | 92.2 | <.001 |
| Medicaid | 38 531 (25.3) | 38 668 (25.6) | 186 (7.5) | 1050.2 | <.001 |
| Other insurance | 11 950 (5.9) | 12 024 (5.9) | 67 (2.7) | 92.9 | <.001 |
| Uninsured | 15 693 (7.3) | 16 018 (7.4) | 31 (1.2) | 634.0 | <.001 |
| Hospital type | |||||
| Urban, medium or large | 99 714 (67.7) | 98 235 (67.8) | 1479 (59.5) | 68.7 | <.001 |
| Urban, small | 44 771 (22.8) | 43 996 (22.3) | 775 (31.2) | 81.6 | <.001 |
| Nonurban | 15 173 (7.7) | 14 949 (7.6) | 224 (9.0) | 5.5 | .02 |
| Unknown location | 3033 (1.8) | 3025 (1.9) | 8 (0.3) | 155.4 | <.001 |
| Hospital delivers any inpatient ECT | 63 677 (40.8) | 61 191 (39.9) | 2486 (100) | NA | |
Abbreviations: ECT, electroconvulsive therapy; MDD, major depressive disorder; NA, not applicable.
Methods section describes the weighting procedure.
Indicates survey design–adjusted test statistics with df1 = 1, df2 = 162 672.
Equals 1 if the patient had an International Classification of Diseases, Ninth Revision diagnosis code in any position for intracranial lesions, masses, inflammation, infection, or hemorrhage; hemorrhagic stroke; myocardial infarction; dysrhythmias; malfunctioning cardiac device; valvular disease; heart failure; epilepsy; dementia; and other contraindications to anesthesia; for other categories, comorbidity equals 0.
Primary source of payment for index inpatient stay.
Poststratification weighting balanced the means of inpatient lengths of stay in the 2 groups (P = .87). The mean (SD) length of stay in the ECT group was 20.7 (19.4) days. By contrast, the mean length of stay in the no ECT group was 8.9 (13.2) days before weighting and 20.6 (20.1) days after weighting.
In bivariate analyses of the 30-day readmission rate (eTable 1 in the Supplement), a smaller proportion of the ECT group was readmitted within 30 days than in the non-ECT group (9.9% vs 12.2%; F1,162 672 = 14.6; P < .001).
IV Probit Regressions
The IV probit coefficient estimate for ECT (eAppendix 2 and eTable 2 in the Supplement) corresponded to an RR of 0.54 (95% CI, 0.28-0.81) for readmission within 30 days if a patient received ECT compared with not receiving ECT (Table 2) or, alternatively, with a 46% reduction in 30-day readmission risk (Figure). These RRs were formed using the adjusted predicted probabilities of readmission, which were 6.6% with ECT and 12.3% without ECT. There were no significant moderator interactions between ECT and either age or race/ethnicity (Table 2). However, the interaction with female sex indicated a larger ECT impact among men (RR, 0.44; 95% CI, 0.20-0.69) than among women (RR, 0.58; 95% CI, 0.30-0.88; moderator χ21 = 7.1; P = .01), and the interaction with diagnosis group implied a larger ECT impact among individuals with bipolar disorder (RR, 0.42; 95% CI, 0.17-0.69; moderator χ21 = 8.5; P = .004) and schizoaffective disorder (RR, 0.44; 95% CI, 0.11-0.79; moderator χ21 = 4.4; P = .04) than among those with MDD (RR, 0.53; 95% CI, 0.26-0.81; reference category for moderator test).
Table 2. IV Probit–Adjusted Estimates of ECT Effect on 30-Day Readmission Risk.
| Category | 95% CI | Moderator Test | |||
|---|---|---|---|---|---|
| % No ECT | % ECT | Risk Ratioa | χ21 | P Value | |
| Overall | 12.3 (12.0-12.6) | 6.6 (3.5-9.7) | 0.54 (0.28-0.81) | ||
| Age, y | |||||
| <65 | 12.7 (12.4-13.0) | 6.2 (3.1-9.2) | 0.49 (0.24-0.74) | 1 [Reference] | .21 |
| ≥65 | 10.0 (9.2-10.8) | 4.7 (2.3-7.1) | 0.47 (0.21-0.77) | 1.6 | |
| Sex | |||||
| Men | 13.1 (12.6-13.5) | 5.7 (2.7-8.7) | 0.44 (0.20-0.69) | 1 [Reference] | .008 |
| Women | 11.6 (11.2-12.0) | 6.7 (3.6-9.9) | 0.58 (0.30-0.88) | 7.1 | |
| Racial/ethnic group | |||||
| White, non-Hispanic | 12.7 (12.3-13.1) | 6.8 (3.7-9.9) | 0.54 (0.28-0.80) | 1 [Reference] | |
| Black, non-Hispanic | 12.1 (11.4-12.8) | 5.4 (0.2-10.5) | 0.45 (0.02-0.92) | 0.2 | .70 |
| Hispanic | 12.2 (11.4-13.0) | 4.6 (0.7-8.6) | 0.38 (0.05-0.75) | 1.0 | .32 |
| Other | 10.5 (9.7-11.3) | 4.8 (1.0-8.6) | 0.46 (0.09-0.89) | <0.1 | .91 |
| Diagnosis group | |||||
| MDD | 9.8 (9.4-10.3) | 5.2 (2.7-7.6) | 0.53 (0.26-0.81) | 1 [Reference] | |
| Bipolar disorder | 12.6 (12.1-13.0) | 5.3 (2.2-8.3) | 0.42 (0.17-0.69) | 8.5 | .004 |
| Schizoaffective disorder | 14.7 (14.1-15.3) | 6.4 (1.7-11.2) | 0.44 (0.11-0.79) | 4.4 | .04 |
Abbreviations: ECT, electroconvulsive therapy; IV, instrumental variables; MDD, major depressive disorder.
Risk ratios calculated as the ratio of the adjusted means for ECT and No ECT, respectively.
Figure. Estimated 30-Day Inpatient Readmission Rates Without and With Electroconvulsive Therapy (ECT).
Error bars indicate 95% CI.
In sensitivity analyses (eAppendix 2 in the Supplement), the ordinary probit model estimate of the ECT coefficient was positive in sign and not statistically significant (coefficient, 0.020; z = 0.53; P = .60). Also, the IV probit estimate of the correlation between the unmeasured determinants of ECT administration and the likelihood of 30-day readmission was positive and significant (coefficient = 0.193; z = 2.89; P = .004), suggesting that the individuals who were selected for ECT had an above-average baseline readmission risk compared with other inpatients in the sample. In other sensitivity analyses that used state variation and patients’ insurance coverage type (not ECT prevalence) as the identifying IVs, the ECT coefficient estimate was consistently negative in sign and similar in magnitude to the IV estimate from the main analysis (z = −2.53; P = .01). Finally, among 308 848 inpatients who did not have an MDD, bipolar disorder, or schizoaffective disorder diagnosis and did not receive ECT, the Pearson correlation coefficient for correlation between hospital prevalence of ECT use and 30-day readmission risk was not significantly different from zero (ρ < .01; P = .74) (eTable 3 and eTable 4 in the Supplement). Collectively, the results of these sensitivity analyses support the validity of the IV probit model.
Discussion
To our knowledge, this is the first study to examine how initiation of ECT during inpatient stays in US hospitals affects the likelihood of 30-day psychiatric inpatient readmission in a large, multisite sample of hospital inpatients diagnosed with severe affective disorders. Previous studies have found that treatment with ECT is associated with remission from depressive disorders and reductions in mortality in individuals with MDD and posttraumatic stress disorder. The results of the present study add evidence that wider availability of ECT may result in up to 46% fewer inpatient readmissions within 30 days of discharge among individuals with severe affective disorders. The effect of ECT on 30-day readmission risk did not differ significantly by age or race/ethnicity but was relatively larger among men than women and among individuals with bipolar disorder and schizoaffective disorder than among those with MDD.
Despite being an effective treatment for patients with severe affective disorders, ECT is either not available or not used as an inpatient procedure in nearly 9 of 10 US hospitals, and there are disparities in ECT’s use based on race/ethnicity and insurance coverage. In this study’s sample, ECT was administered among only 1.5% of inpatients with severe affective disorders. Many factors may contribute to ECT’s inconsistent availability, including clinical recommendations not to use the procedure as first-line therapy, managed care preauthorization requirements, limited graduate medical training in ECT, and public ambivalence toward the ECT procedure and its adverse effects. However, reimbursements that hospitals receive for inpatient treatment with ECT, which, in Medicare, are approximately $310 per treatment, also may provide insufficient financial incentive to offer ECT given the procedure’s indirect costs resulting from longer inpatient lengths of stay, screening required for medical risks, and anesthesia.
Evidence that ECT reduces the likelihood of inpatient readmission for patients with severe affective disorders suggests that hospitals may have added incentive to offer ECT since many hospitals now bear financial risks for inpatient readmissions under value-based payment arrangements that shift the costs of readmissions from payers to hospitals and accountable care organizations. Moreover, the Centers for Medicare & Medicaid Services uses a standardized 30-day readmissions metric for inpatient psychiatric facility performance benchmarking, quality improvement, and payment purposes. This metric raises the prospect that Medicare and other health care payers may someday link psychiatric readmission rates with financial penalties for hospitals that have “excess” readmissions, analogous to the current Centers for Medicare & Medicaid Services Readmissions Reduction Program incentives for nonpsychiatric conditions. When hospitals bear some of the financial costs of unplanned readmissions, they may reassess the value of ECT and other interventions that may be beneficial for patients at risk for multiple hospitalizations.
Limitations
The potential limitations of this study’s design and approach should be considered when interpreting its findings. The internal validity of our correlational estimates of ECT’s effects depends on the assumption that individuals with greater measured access to ECT (ie, higher prior-year ECT prevalence at the same hospital) have a similar natural propensity for readmission within 30 days than individuals with worse access to ECT. Among inpatients with affective disorders, the likelihood of being treated in a hospital that offers ECT is lower in rural areas, in hospitals located in geographic areas with lower mean incomes, among inpatients from minority racial/ethnic backgrounds, and among inpatients who have Medicaid insurance coverage or are uninsured. These associations suggest that individuals who have greater access to ECT might also have more access to community supports that reduce readmission risks and, consequently, that our IV estimates may overstate ECT’s effects on readmission risk.
However, prior research studies have documented greater (>20-fold) variability in ECT prevalence among US metropolitan areas. This variation is associated with hospital system-level factors that affect the costs of providing ECT, such as regulatory restrictions, postgraduate medical training opportunities, and insurance-based payment amounts and preapproval requirements. Consequently, geographic variability in ECT’s prevalence may be largely independent of individuals’ propensity for readmission. Moreover, inpatients treated with ECT are older, have a history of medication-resistant mood problems, and are more likely to have had another inpatient episode within the 30 days prior to their current episode; these characteristics suggest unfavorable risk prediction for ECT. We also found no correlation between hospitals’ ECT prevalence and readmission risk among inpatients with conditions that are not appropriate for ECT (eAppendix 2 in the Supplement). We further estimated IV probit models using only state indicators and insurance coverage as IVs and found similar results. Consequently, although additional studies are needed to understand the factors affecting access to ECT, the hypothesis that favorable patient risk prediction into ECT explains our findings is inconsistent with empirical findings in this study and with prior research.
Other potential limitations of the study include insufficient clinical information, exclusion of state and federal hospitals, and lack of data on administration of ECT in outpatient hospital settings. However, the lack of clinical information had no bearing on IV analyses. The lack of information on outpatient ECT means that our estimated effects of ECT might overstate the importance of starting ECT while an individual is an inpatient, as our estimates may partially reflect the effects of ambulatory ECT administered after hospital discharge, which was not measured. Finally, although this study used a large sample across 9 states—to our knowledge, a far larger sample than in any prior study of ECT—the results might not generalize to patients in other states. The 3 largest states in the sample—California, Florida, and New York—accounted for most of the observations and consequently may have disproportionately influenced the results. Studies of a broader national sample could help to confirm the generalizability of these findings in other states.
Conclusions
This study found that ECT administration may prevent many short-term inpatient readmissions to general hospitals among US patients with severe affective disorders. Despite the lower prevalence of treatment with ECT among inpatients who are black, the study’s results suggest that ECT’s effects on readmission risk are largely independent of race/ethnicity. However, a moderately larger effect of ECT treatment on readmission risk was found for men compared with women and individuals with bipolar disorder and schizoaffective disorder diagnoses compared with those diagnosed with MDD. These results provide evidence suggesting that broader ECT availability may result in fewer readmissions among psychiatric inpatients with severe affective disorders. This population health effect may be overlooked in US hospitals’ current decision making regarding the availability of ECT.
eAppendix 1. Bivariate Probit Model
eAppendix 2. Sensitivity Analyses
eTable 1. Bivariate Results
eTable 2. Probit Regression Estimates of the Likelihood of 30-Day Readmission
eTable 3. One-to-One Propensity Score Matching Estimate of the Average Treatment Effect of ECT on 30-Day Readmission Risk (N=4,940)
eTable 4. Thirty-Day Readmission Risk by Hospital ECT Prevalence Among Inpatients Who Were Not Administered ECT and Did Not Have a Major Depressive Disorder, Bipolar Disorder, or Schizoaffective Disorder Diagnosis
References
- 1.Hermann RC, Dorwart RA, Hoover CW, Brody J. Variation in ECT use in the United States. Am J Psychiatry. 1995;152(6):869-875. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association The Practice of Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging: A Task Force Report of the American Psychiatric Association. Washington, DC: American Psychiatric Association; 2001. [Google Scholar]
- 3.Greenhalgh J, Knight C, Hind D, Beverley C, Walters S. Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies. Health Technol Assess. 2005;9(9):1-156, iii-iv. [DOI] [PubMed] [Google Scholar]
- 4.UK ECT Review Group Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet. 2003;361(9360):799-808. [DOI] [PubMed] [Google Scholar]
- 5.Fink M, Taylor MA. Electroconvulsive therapy: evidence and challenges. JAMA. 2007;298(3):330-332. [DOI] [PubMed] [Google Scholar]
- 6.Schoeyen HK, Kessler U, Andreassen OA, et al. Treatment-resistant bipolar depression: a randomized controlled trial of electroconvulsive therapy versus algorithm-based pharmacological treatment. Am J Psychiatry. 2015;172(1):41-51. [DOI] [PubMed] [Google Scholar]
- 7.Avery D, Winokur G. Mortality in depressed patients treated with electroconvulsive therapy and antidepressants. Arch Gen Psychiatry. 1976;33(9):1029-1037. [DOI] [PubMed] [Google Scholar]
- 8.Ahmadi N, Moss L, Simon E, Nemeroff CB, Atre-Vaidya N. Efficacy and long-term clinical outcome of comorbid posttraumatic stress disorder and major depressive disorder after electroconvulsive therapy. Depress Anxiety. 2016;33(7):640-647. [DOI] [PubMed] [Google Scholar]
- 9.Weiner RD, Prudic J. Electroconvulsive therapy in the United States: how often is it used? Biol Psychiatry. 2013;73(2):105-106. [DOI] [PubMed] [Google Scholar]
- 10.Case BG, Bertollo DN, Laska EM, et al. Declining use of electroconvulsive therapy in United States general hospitals. Biol Psychiatry. 2013;73(2):119-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bailine S. Reimbursement and documentation issues in an ambulatory ECT program. J ECT. 1998;14(4):255-258. [PubMed] [Google Scholar]
- 12.Kellner CH, Li EH. Electroconvulsive therapy from both sides now: perspectives from late and early career. J ECT. 2016;32(1):1-2. [DOI] [PubMed] [Google Scholar]
- 13.Kellner CH. Electroconvulsive therapy: the second-most controversial medical procedure. Psychiatr Times http://www.psychiatrictimes.com/major-depressive-disorder/electroconvulsive-therapy-second-most-controversial-medical-procedure Published February 8, 2011. Accessed June 20, 2016.
- 14.Nauert R. Decline in use of electroconvulsive therapy. PsychCentral. https://psychcentral.com/news/2012/11/26/decline-in-use-of-electroconvulsive-therapy/48130.html. Published November 26, 2012. Accessed January 2, 2017.
- 15.Olfson M, Marcus S, Sackeim HA, Thompson J, Pincus HA. Use of ECT for the inpatient treatment of recurrent major depression. Am J Psychiatry. 1998;155(1):22-29. [DOI] [PubMed] [Google Scholar]
- 16.Durbin J, Lin E, Layne C, Teed M. Is readmission a valid indicator of the quality of inpatient psychiatric care? J Behav Health Serv Res. 2007;34(2):137-150. [DOI] [PubMed] [Google Scholar]
- 17.Angrist J, Imbens G, Rubin D. Identification of causal effects using instrumental variables. J Am Stat Assoc. 1996;91:444-455. [Google Scholar]
- 18.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: MIT Press; 2002. [Google Scholar]
- 19.Hogan JW, Lancaster T. Instrumental variables and inverse probability weighting for causal inference from longitudinal observational studies. Stat Methods Med Res. 2004;13(1):17-48. [DOI] [PubMed] [Google Scholar]
- 20.Stukel TA, Fisher ES, Wennberg DE, Alter DA, Gottlieb DJ, Vermeulen MJ. Analysis of observational studies in the presence of treatment selection bias: effects of invasive cardiac management on AMI survival using propensity score and instrumental variable methods. JAMA. 2007;297(3):278-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project (HCUP): overview of the State Inpatient Databases. AHRQ website. https://www.ahrq.gov/research/data/hcup/index.html. Published 2013. Accessed May 19, 2017.
- 22.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9(3):208-220. [PMC free article] [PubMed] [Google Scholar]
- 23.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10. [PubMed] [Google Scholar]
- 24.Angrist JD, Krueger AB. Instrumental variables and the search for identification: from supply and demand to natural experiments. J Econ Perspect. 2001;15(4):69-85. doi:10.1257/jep.15.4.69 [Google Scholar]
- 25.Pippard J. Audit of electroconvulsive treatment in two national health service regions. Br J Psychiatry. 1992;160:621-637. [DOI] [PubMed] [Google Scholar]
- 26.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55(2):652-659. [DOI] [PubMed] [Google Scholar]
- 27.Huber PJ. The behavior of maximum likelihood estimates under non-standard conditions In: Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability. Berkeley: University of California Press; 1967;1:221-233. [Google Scholar]
- 28.White H. A heteroskedastic consistent covariance matrix estimator and a direct test of heteroskedasticity. Econometrica. 1980;48:817-838. [Google Scholar]
- 29.Deville JC, Särndal CE, Sautory O. Generalized raking procedures in survey sampling. J Am Stat Assoc. 1993;88:1013-1020. [Google Scholar]
- 30.Wilson KG, Kraitberg NJ, Brown JH, Bergman JN. Electroconvulsive therapy in the treatment of depression: the impact on length of stay. Compr Psychiatry. 1991;32(4):345-354. [DOI] [PubMed] [Google Scholar]
- 31.Herr BE, Abraham HD, Anderson W. Length of stay in a general hospital psychiatric unit. Gen Hosp Psychiatry. 1991;13(1):68-70. [DOI] [PubMed] [Google Scholar]
- 32.Mark TL, Tomic KS, Kowlessar N, Chu BC, Vandivort-Warren R, Smith S. Hospital readmission among Medicaid patients with an index hospitalization for mental and/or substance use disorder. J Behav Health Serv Res. 2013;40(2):207-221. [DOI] [PubMed] [Google Scholar]
- 33.Prudic J, Olfson M, Marcus SC, Fuller RB, Sackeim HA. Effectiveness of electroconvulsive therapy in community settings. Biol Psychiatry. 2004;55(3):301-312. [DOI] [PubMed] [Google Scholar]
- 34.Thompson JW, Weiner RD, Myers CP. Use of ECT in the United States in 1975, 1980, and 1986. Am J Psychiatry. 1994;151(11):1657-1661. [DOI] [PubMed] [Google Scholar]
- 35.Medicare Payment Advisory Commission Report to the Congress: Aligning Incentives in Medicare. Washington, DC: Medicare Payment Advisory Commission; June 2010. [Google Scholar]
- 36.VanLare JM, Conway PH. Value-based purchasing—national programs to move from volume to value. N Engl J Med. 2012;367(4):292-295. [DOI] [PubMed] [Google Scholar]
- 37.CMS.gov. Centers for Medicare & Medicaid Services Measure methodology. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. Updated April 14, 2017. Accessed March 6, 2017.
- 38.CMS.gov. Centers for Medicare & Medicaid Services Readmissions Reduction Program (HRRP). https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Updated April 18, 2016. Accessed March 7, 2017.
- 39.Breakey WR, Dunn GJ. Racial disparity in the use of ECT for affective disorders. Am J Psychiatry. 2004;161(9):1635-1641. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Bivariate Probit Model
eAppendix 2. Sensitivity Analyses
eTable 1. Bivariate Results
eTable 2. Probit Regression Estimates of the Likelihood of 30-Day Readmission
eTable 3. One-to-One Propensity Score Matching Estimate of the Average Treatment Effect of ECT on 30-Day Readmission Risk (N=4,940)
eTable 4. Thirty-Day Readmission Risk by Hospital ECT Prevalence Among Inpatients Who Were Not Administered ECT and Did Not Have a Major Depressive Disorder, Bipolar Disorder, or Schizoaffective Disorder Diagnosis