Key Points
Question
What are the progress and challenges toward universal health coverage in Afghanistan, Bangladesh, India, Nepal, and Pakistan?
Findings
In a population-based study including 335 373 households, coverage of essential health services and financial risk protection against catastrophic health expenditure and impoverishment was found to be low across all 5 South Asian countries. Inequality in coverage of health services and financial risk protection was common in the South Asian region.
Meaning
Reduction of inequality in access to care and expansion of risk-pooling mechanisms are essential in these countries to achieve universal health coverage.
Abstract
Importance
Achieving universal health coverage is one of the key targets in the newly adopted Sustainable Development Goals of the United Nations.
Objective
To investigate progress toward universal health coverage in 5 South Asian countries and assess inequalities in health services and financial risk protection indicators.
Design and Settings
In a population-based study, nationally representative household (335 373 households) survey data from Afghanistan (2014 and 2015), Bangladesh (2010 and 2014), India (2012 and 2014), Nepal (2014 and 2015), and Pakistan (2014) were used to calculate relative indices of health coverage, financial risk protection, and inequality in coverage among wealth quintiles. The study was conducted from June 2012 to February 2016.
Main Outcomes and Measures
Three dimensions of universal health coverage were assessed: access to basic services, financial risk protection, and equity. Composite and indicator-specific coverage rates, stratified by wealth quintiles, were then estimated. Slope and relative index of inequality were used to assess inequalities in service and financial indicators.
Results
Access to basic care varied substantially across all South Asian countries, with mean rates of overall prevention coverage and treatment coverage of 53.0% (95% CI, 42.2%-63.6%) and 51.2% (95% CI, 45.2%-57.1%) in Afghanistan, 76.5% (95% CI, 61.0%-89.0%) and 44.8% (95% CI, 37.1%-52.5%) in Bangladesh, 74.2% (95% CI, 57.0%-88.1%) and 83.5% (95% CI, 54.4%-99.1%) in India, 76.8% (95% CI, 66.5%-85.7%) and 57.8% (95% CI, 50.1%-65.4%) in Nepal, and 69.8% (95% CI, 58.3%-80.2%) and 50.4% (95% CI, 37.1%-63.6%) in Pakistan. Financial risk protection was generally low, with 15.3% (95% CI, 14.7%-16.0%) of respondents in Afghanistan, 15.8% (95% CI, 14.9%-16.8%) in Bangladesh, 17.9% (95% CI, 17.7%-18.2%) in India, 11.8% (95% CI, 11.8%-11.9%) in Nepal, and 4.4% (95% CI, 4.0%-4.9%) in Pakistan reporting incurred catastrophic payments due to health care costs. Access to at least 4 antenatal care visits, institutional delivery, and presence of skilled attendant during delivery were at least 3 times higher among the wealthiest mothers in Afghanistan, Bangladesh, Nepal, and Pakistan compared with the rates among poor mothers. Access to institutional delivery was 60 to 65 percentage points higher among wealthy than poor mothers in Afghanistan, Bangladesh, Nepal, and Pakistan compared with 21 percentage points higher in India. Coverage was least equitable among the countries for adequate sanitation, institutional delivery, and the presence of skilled birth attendants.
Conclusions and Relevance
Health coverage and financial risk protection was low, and inequality in access to health care remains a serious issue for these South Asian countries. Greater progress is needed to improve treatment and preventive services and financial security.
This population-based study evaluates the status of health coverage in 5 South Asian countries toward achievement of the United Nations’ Sustainable Development Goals.
Introduction
In the United Nations’ newly adopted Sustainable Development Goals, universal health coverage is promoted as an essential precondition for health and human security, particularly in low- and lower middle-income countries. The main goal of universal health coverage is to ensure that everyone who needs health care services is able to gain access to them without incurring financial hardship. The key targets of universal health coverage are to achieve at least 80% essential health service coverage and 100% protection from catastrophic health payment and impoverishment by 2030. Universal health coverage is now seen as an important component in the response to the global epidemic of noncommunicable diseases (NCDs), managing the epidemiologic transition and ensuring affordable and equitable access to care.
All World Health Organization member states have committed to universal health coverage and all developing countries are already pursuing universal health coverage policies with the intention of extending health coverage, but at the present only 20 developing countries have been identified as having made good progress toward universal health coverage. Effective and continuous monitoring and tracking are necessary to ensure that policymakers can manage new initiatives efficiently and program development continues in line with Sustainable Development Goal 3–related indicators.
The World Health Organization proposed 3 core dimensions of universal health coverage: the proportion of a population covered by existing health care systems, the range of health care services available to a population, and the extent of financial risk protection available to local populations. These dimensions are interdependent and can be measured in several ways. Assessing the services’ coverage and financial risk protection indicators is the most commonly recommended method by the World Health Organization to track the progress toward universal health coverage, as these indicators help to define where a country may best seek to improve its health care system. Assessment is particularly lacking in the South Asian region, where health systems are typically underfunded and poorly functioning, which can impede data gathering and tracking.
Many South Asian countries are simultaneously facing the double burden of disease and low health service coverage; patients’ out-of-pocket payments remain the most common source of funding for health care in these countries. Inequality is another concern in these countries, and disadvantaged populations are often unable to afford health care services. Inadequate public funding for health services, limited access to health insurance plans, and high out-of-pocket payments can trigger asset depletion, indebtedness, and reductions in essential consumption, leading to financial catastrophe, impoverishment, and reduced access to health care services.
To measure and track countries’ progress toward universal health coverage, we estimated a range of indicators of service coverage and financial risk protection using primary survey data from 5 South Asian countries: Afghanistan, Bangladesh, India, Nepal, and Pakistan. We examined service coverage indicators reflecting health promotion, disease prevention, and specific treatment areas. We assessed the extent of financial risk protection by measuring the incidence of catastrophic and impoverishing health expenditures associated with out-of-pocket payments. We also calculated measures of equity among wealth quintiles in each country, and composite indices were generated for country-level comparisons. The study was conducted from June 2012 to February 2016.
Methods
Data Sources
For each country, we used the most recent country-specific, nationally representative, primary survey data to calculate estimates of health coverage and financial risk protection indicators based on previously described statistical methods of health coverage modeling: Afghanistan (2014 and 2015), Bangladesh (2010 and 2014), India (2012 and 2014), Nepal (2014 and 2015), and Pakistan (2014). The data sources used for intervention coverage and financial hardship estimates are presented in eTable 1 in the Supplement. Data were deidentified. Data were purchased from the selected countries, which had already obtained approval in conducting their surveys. In addition, we obtained data for gross domestic product, health expenditure, life expectancy, total fertility rate, and other demographic statistics from the World Bank.
Main Outcome Measures and Analysis
Indicators for each dimension of universal health coverage, along with measures of overall equitability, were calculated from the aforementioned survey database on standard techniques, which are summarized herein.
Health Service Coverage
Health service tracking is typically assessed through coverage of prevention measures and treatment measures. To be consistent with previous studies, we estimated a composite coverage index (CCI) for each country based on 8 interventions from 4 specialties (family planning, maternity care, child immunization, and case management).
where ANCS indicates antenatal care with a skilled attendant; BCG, BCG immunization; CPNM, care-seeking for pneumonia; DPT3, 3 doses of diphtheria-tetanus-pertussis immunization; FPS, family planning needs satisfied; MSL, measles immunization; ORT, oral rehydration therapy for children with diarrhea; and SBA, presence of a skilled birth attendant.
Similar to previous studies, we used random-effects meta-analysis (Stata command: metaprop_one) to estimate the mean proportion for the composite prevention index based on 11 prevention indicators and the composite treatment index based on 4 treatment indicators. We compared this pooled mean proportion from meta-analysis with the arithmetic mean proportion across health-related indicators, which is a commonly used alternative measurement of coverage, and found almost identical results. For comparison purposes, we did not include diabetes and hypertension treatment indicators in the composite treatment index estimation because these 2 indicators were available for only Bangladesh and India. We assessed the diabetes and hypertension treatment indicators separately. Specific definitions, as well as a complete list of these prevention and treatment indicators and data sources, along with details of the calculation method, are presented in eTable 2 and eMethods in the Supplement.
Financial Risk Protection
Financial risk protection was assessed through incidence of catastrophic and impoverishing out-of-pocket health payments. Household expenditure is treated as catastrophic if it exceeds a threshold of 10% of household total consumption expenditure. Health expenditure was defined as impoverishing when a non-poor household became poor due to out-of-pocket payments for health care. Impoverishment was estimated using total household consumption expenditure calculated separately with and without out-of-pocket payments for health care. A detailed description of the measurement of catastrophic payments and impoverishment can be found in the Supplement (see eMethods in the Supplement).
Measures of Inequality
To summarize wealth-based inequalities in health service coverage and financial risk, we used 2 indices: slope index of inequality (SII) and relative index of inequality (RII). We calculated both indices using logistic regression models that take into account the whole population distribution of wealth. The SII and RII were estimated by regressing health service and financial indicators outcomes against an individual’s relative rank in the cumulative distribution of wealth. The SII expresses the absolute difference in coverage in percentage points between the extremes of the wealth distribution (from top to bottom) and gives an idea of the actual effort that will be needed to close the gap. A positive value of SII indicates that intervention coverage is higher in wealthy households compared with poor ones; for example, measles vaccine coverage among the wealthy population is 60 percentage points higher than among the poor population. By contrast, the RII measures the ratio of intervention coverage for poor and wealthy households and provides an idea about the degree of inequity; for example, polio vaccine coverage in the wealthiest households is 1.3 ([1.3 − 1] • 100% = 30%) times higher than in the poorest households. A detailed description of these methods is presented in eMethods in the Supplement. We used Stata, version 14.1/MP (StataCorp) for all analyses.
Results
Sociodemographic Context
There were notable differences in wealth, health indicators, and health systems across South Asian countries (Table 1). The 5 included South Asian countries have a population of 1.72 billion, with the largest in India (1.31 billion) and smallest in Nepal (28 million). Poverty rate as a percentage of the population ranged from 21.9% (India) to 35.8% (Afghanistan). Gross domestic product spending on health varies: 8.2% in Afghanistan, 2.8% in Bangladesh, 4.7% in India, 5.8% in Nepal, and 2.6% in Pakistan. Women have a longer life expectancy than men in all 5 South Asian countries, ranging from 61.6 years in Afghanistan to 72.9 years in Bangladesh. A total of 335 373 households were included in this study.
Table 1. Key Socioeconomic and Population Characteristics of the Selected South Asian Countriesa.
| Indicator | Afghanistan | Bangladesh | India | Nepal | Pakistan |
|---|---|---|---|---|---|
| Socioeconomic | |||||
| Total population in 2015, millions, No. | 32.53 | 161.00 | 1311.05 | 28.51 | 188.92 |
| GDP, 2014, US$ billion | 12.9 | 119.0 | 1600.3 | 12.0 | 151.6 |
| GDP per person, 2014, US$ | 408.9 | 747.8 | 1235.5 | 425.7 | 819.3 |
| Literacy rate in 2011-2013, %b | |||||
| Female | 17.6 | 56.2 | 59.3 | 48.8 | 42.0 |
| Male | 45.4 | 63.2 | 78.9 | 71.7 | 67.0 |
| Age dependency ratio in 2014c | 89.8 | 53.7 | 53.1 | 63.7 | 65.8 |
| Poverty in 2011-2012, % of populationd | 35.8 | 31.5 | 21.9 | 25.2 | NA |
| Health expenditures in 2014 | |||||
| Percentage of GDP in THE | 8.2 | 2.8 | 4.7 | 5.8 | 2.6 |
| PHE, % of THE | 35.8 | 27.9 | 30.0 | 40.3 | 35.2 |
| PvtHE, % of THE | 64.2 | 72.1 | 70.0 | 59.7 | 64.8 |
| Out-of-pocket expenditure, % of THE | 63.9 | 67.0 | 62.4 | 47.7 | 56.3 |
| Private insurance, % of PvtHE | NA | NA | 5.0 | NA | 1.0 |
| Life, Birth, and Death | |||||
| Mean life expectancy at birth in 2014, y | |||||
| Men | 59.2 | 70.4 | 66.6 | 68.2 | 65.3 |
| Women | 61.6 | 72.9 | 69.5 | 71.1 | 67.2 |
| Mean births per woman in 2014, No. | 4.8 | 2.2 | 2.4 | 2.2 | 3.6 |
| NMR per 1000 live births in 2015, % | 35.5 | 23.3 | 27.7 | 22.2 | 45.5 |
| IMR per 1000 live births in 2015, % | 66.3 | 30.7 | 37.9 | 29.4 | 65.8 |
| U5MR per 1000 live births in 2015, % | 91.1 | 37.6 | 47.7 | 35.8 | 81.1 |
| MMR per 100 000 live births in 2013 | 400.0 | 170.0 | 190.0 | 190.0 | 170.0 |
Abbreviations: GDP, gross domestic product; IMR, infant mortality rate; MMR, maternal mortality ratio; NA, not applicable; NMR, neonatal mortality rate; PHE, public health expenditure; PvtHE, private health expenditure; THE, total health expenditure; U5MR, under age 5 years mortality rate.
Data are from the World Bank.
Literacy rate percentage in individuals aged 15 years or older.
Age dependency based on working-age population.
Poverty headcount ratio at national poverty line.
Health Service Coverage
Table 2 presents a set of tracer indicators with summary measures of prevention and treatment intervention coverage in the most recent survey year. Access to basic care varied substantially across all South Asian countries, with mean rates of overall prevention coverage of 53.0% (95% CI, 42.2%-63.6%) in Afghanistan, 76.5% (95% CI, 61.0%-89.0%) in Bangladesh, 74.2% (95% CI, 57.0%-88.1%) in India, 76.8% (95% CI, 66.5%-85.7%) in Nepal, and 69.8% (95% CI, 58.3%-80.2%) in Pakistan. Access to specific prevention services varied similarly, with mean rates of adequate sanitation and measles immunization of 33.7% (95% CI, 33.1%-34.3%) and 60.1% (95% CI, 58.8%-61.4%) in Afghanistan, 68.8% (95% CI, 68.1%-69.5%) and 86.2% (95% CI, 84.5%-87.9%) in Bangladesh, 57.9% (95% CI, 57.5%-58.3%) and 70.7% (95% CI, 70.4%-71.0%) in India, 74.4% (95% CI, 73.6%-75.2%) and 89.7% (95% CI, 87.8%-91.6%) in Nepal, and 74.0% (95% CI, 73.6%-74.3%) and 70.6% (95% CI, 69.6%-71.6%) in Pakistan.
Table 2. National Coverage of Health Services in 5 South Asian Countries.
| Indicator | Coverage, % (95% CI) | ||||
|---|---|---|---|---|---|
| Afghanistan | Bangladesh | India | Nepal | Pakistan | |
| Prevention | |||||
| Improved water | 65.3 (64.7-65.8) | 97.8 (97.5-98.0) | 97.9 (97.8-98.0) | 93.3 (92.8-93.7) | 93.3 (93.1-93.5) |
| Adequate sanitation | 33.7 (33.1-34.3) | 68.8 (68.1-69.5) | 57.9 (57.5-58.3) | 74.4 (73.6-75.2) | 74.0 (73.6-74.3) |
| FP needs satisfied | 47.9 (47.3-48.5) | 83.9 (83.3-84.6) | 38.5 (38.1-38.9) | 66.3 (65.3-67.3) | 65.1 (64.5-65.7) |
| ≥1 ANC visit | 57.6 (56.8-58.4) | 63.8 (62.4-65.1) | 96.5 (96.3-96.8) | 67.9 (65.9-69.9) | 77.9 (77.3-78.5) |
| ≥4 ANC visits | 17.3 (16.7-17.9) | 24.6 (23.4-25.9) | 84.2 (83.6-84.7)a | 48.4 (46.2-50.5) | 44.6 (43.9-45.4) |
| DPT3 immunization | 58.3 (57.0-59.6) | 91.3 (89.9-92.6) | 59.9 (59.5-60.2) | 87.1 (85.0-89.1) | 66.6 (65.6-67.6) |
| Measles immunization | 60.1 (58.8-61.4) | 86.2 (84.5-87.9) | 70.7 (70.4-71.0) | 89.7 (87.8-91.6) | 70.6 (69.6-71.6) |
| BCG immunization | 73.8 (72.7-74.9) | 97.9 (97.2-98.6) | 87.0 (86.7-87.2) | 95.4 (94.1-96.7) | 87.2 (86.5-87.9) |
| Polio3 immunization | 65.3 (64.1-66.6) | 91.5 (90.2-92.9) | 87.5 (87.3-87.8) | 90.8 (89.0-92.6) | 78.0 (77.1-78.9) |
| Care-seeking for pneumonia | 61.6 (60.0-63.1) | 42.0 (37.2-46.7) | 96.4 (96.1-96.7) | 50.1 (44.9-55.4) | 75.8 (74.2-77.4) |
| Exclusive breastfeeding | 43.3 (41.6-45.1) | 55.3 (51.5-59.1) | 59.0 (58.7-59.3) | 56.9 (52.3-61.4) | 21.7 (20.4-23.0) |
| Treatmentb | |||||
| ARI treatment | 54.4 (52.8-55.9) | 34.3 (29.9-39.0) | 96.1 (95.7-96.4) | 74.9 (70.4-79.4) | 34.4 (32.6-36.1) |
| Oral rehydration therapy | 40.7 (39.7-41.7) | 66.1 (61.6-70.5) | 94.8 (94.2-95.3) | 45.9 (42.0-49.7) | 39.9 (38.9-40.9) |
| Skilled birth attendance | 54.2 (53.5-54.9) | 42.1 (40.7-43.4) | 39.6 (38.7-40.4) | 55.6 (53.4-57.7) | 65.1 (64.4-65.8) |
| Institutional delivery | 52.0 (51.2-52.7) | 37.5 (36.1-38.8) | 82.2 (81.7-82.8) | 55.2 (53.0-57.3) | 61.9 (61.2-62.7) |
| Hypertension treatment | NA | 42.3 (39.4-45.2) | 70.4 (69.8-71.0) | NA | NA |
| Diabetes treatment | NA | 38.3 (34.0-42.8) | 82.4 (81.8-82.9) | NA | NA |
| Composite Indexesc | |||||
| Coverage | 54.2 (51.3-57.1) | 71.0 (68.9-73.1) | 68.9 (68.1-69.8) | 67.5 (65.6-69.4) | 67.7 (66.0-69.4) |
| Prevention | 53.0 (42.2-63.6) | 76.5 (61.0-89.0) | 74.2 (57.0-88.1) | 76.8 (66.5-85.7) | 69.8 (58.3-80.2) |
| Treatment | 51.2 (45.2-57.1) | 44.8 (37.1-52.5) | 83.5 (54.4-99.1) | 57.8 (50.1-65.4) | 50.4 (37.1-63.6) |
Abbreviations: ANC, antenatal care; ARI, acute respiratory infection; DPT3, 3 doses of diphtheria-tetanus-pertussis vaccine; FP, family planning; NA, not applicable; Polio3, 3 doses of polio vaccine.
Three or more ANC visits.
Diabetes and hypertension were not included to estimate the composite treatment index because these 2 indicators were not available in Afghanistan, Nepal, and Pakistan.
Composite prevention index was developed based on 11 prevention indicators, and composite treatment index was based on 4 treatment indicators by random-effects meta-analysis. Composite coverage index was a weighted mean of 8 interventions (FP needs satisfied, skilled birth attendant, ANC with skilled attendant, DPT3 immunization, measles immunization, BCG immunization, oral rehydration therapy for children with diarrhea, and care-seeking for pneumonia) from 4 specialties (FP, maternity care, child immunization, and case management).
The mean treatment coverage also varied across all 5 South Asian countries, with a coverage rate of 51.2% (95% CI, 45.2%-57.1%) in Afghanistan, 44.8% (95% CI, 37.1%-52.5%) in Bangladesh, 83.5% (95% CI, 54.4%-99.1%) in India, 57.8% (95% CI, 50.1%-65.4%) in Nepal, and 50.4% (95% CI, 37.1%-63.6%) in Pakistan. The national coverage of institutional delivery and skilled birth attendance had rates of 52.0% (95% CI, 51.2%-52.7%) and 54.2% (95% CI, 53.5%-54.9%) in Afghanistan, 37.5% (95% CI, 36.1%-38.8%) and 42.1% (95% CI, 40.7%-43.4%) in Bangladesh, 82.2% (95% CI, 81.7%-82.8%) and 39.6% (95% CI, 38.7-40.4) in India, 55.2% (95% CI, 53.0%-57.3%) and 55.6% (95% CI, 53.4%-57.7%) in Nepal, and 61.9% (95% CI, 61.2%-62.7%) and 65.1% (95% CI, 64.4%-65.8%) in Pakistan, respectively. The composite coverage index related to maternal and child health interventions ranged from 54.2% (95% CI, 51.3%-57.1%) (Afghanistan) to 71.0% (95% CI, 68.9%-73.1%) (Bangladesh).
Financial Risk Protection
In all of the study countries, a large proportion of total health expenditures comes from private sources, and out-of-pocket payments are the main sources of funding for health care in Afghanistan, Bangladesh, and India (Table 1). A total of 15.3% (95% CI, 14.7%-16.0%) of households in Afghanistan, 15.8% (95% CI, 14.9%-16.8%) in Bangladesh, 17.9% (95% CI, 17.7%-18.2%) in India, 11.8% (95% CI, 11.8%-11.9%) in Nepal, and 4.4% (95% CI, 4.0%-4.9%) in Pakistan incurred catastrophic health payments (Table 3). Of nonpoor households in Afghanistan, Bangladesh, India, and Nepal, 2.9% to 4.9% became poor due to health care costs; this occurred in only 1.4% of households in Pakistan (Table 3).
Table 3. Inequality in Catastrophic Health Payments in 5 South Asian Countries.
| Country (Year of Survey) | % (95% CI) | ||||
|---|---|---|---|---|---|
| Financial Burden | Inequality in Catastrophic Payments | Relative Index of Inequality | |||
| Catastrophic Paymentsa | Impoverishment | Poorest Quintile | Wealthiest Quintile | ||
| Afghanistan (2014) | 15.3 (14.7-16.0) | 2.9 (2.6-3.2) | 13.4 (12.0-14.9) | 17.1 (15.7-18.6) | 1.2 (1.0-1.4) |
| Bangladesh (2010) | 15.8 (14.9-16.8) | 4.9 (4.5-5.4) | 10.9 (9.5-12.5) | 22.0 (19.5-24.7) | 2.5 (2.0-3.0) |
| India (2012) | 17.9 (17.7-18.2) | 3.4 (3.3-3.6) | 13.3 (12.9-13.8) | 24.1 (23.5-24.7) | 2.1 (1.9-2.3) |
| Nepal (2015) | 11.8 (11.8-11.9) | 3.5 (3.5-3.6) | 8.3 (8.3-8.4) | 17.1 (23.5-24.7) | 2.3 (1.6-3.0) |
| Pakistan (2014) | 4.4 (4.0-4.9) | 1.4 (1.0-1.7) | 4.9 (4.0-6.0) | 4.7 (3.9-5.7) | 1.2 (1.0-1.4) |
Catastrophic payments at 10% threshold of total consumption.
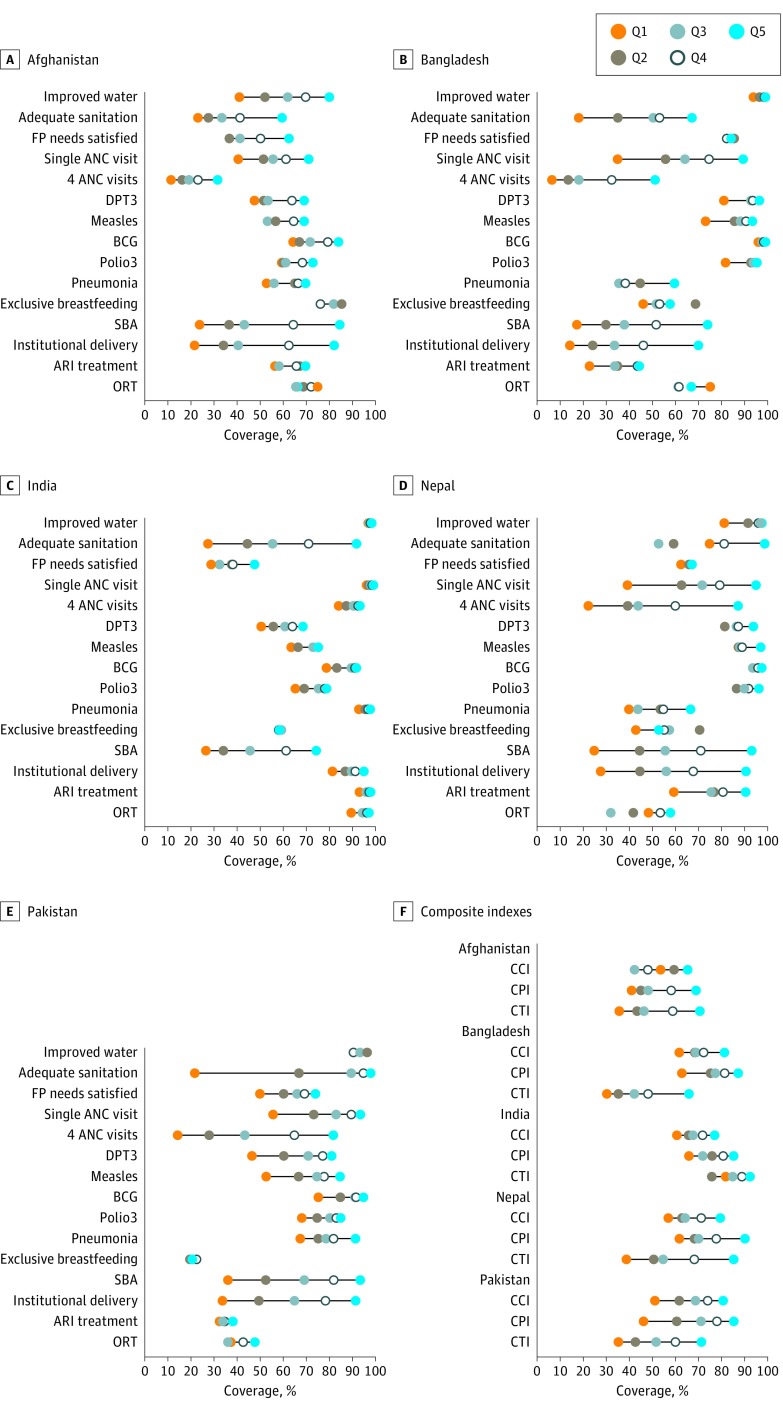
Inequalities in Universal Health Coverage Indicators
The country-specific coverage of prevention and treatment interventions for each quintile in the 5 selected countries is presented in the Figure, and the magnitude of inequality as assessed by the RII for each intervention is presented in Table 4. Among the prevention and treatment interventions, the most inequitable interventions in most South Asian countries were adequate sanitation, presence of a skilled birth attendant during delivery, institutional delivery, and at least 4 antenatal care visits (except India). Coverage of at least 4 antenatal care visits among wealthy mothers was approximately 11 times higher in Bangladesh, 9 times higher in Pakistan, and 5 times higher in both Afghanistan and Nepal than that among poor mothers. Access to institutional delivery among wealthy mothers was at least 4 times higher in Bangladesh, Afghanistan, and Nepal than poor mothers. Greater inequalities were also observed for skilled birth attendance coverage, where women in the wealthy population were at least 5 times more likely to have received this service than were women in the poor population in Afghanistan, Bangladesh, and Nepal. The slope index of inequalities of prevention and treatment interventions is presented in more detail in eTable 3 in the Supplement. Access to institutional delivery was 60 to 65 percentage points higher among wealthy than poor mothers in Afghanistan, Bangladesh, Nepal, and Pakistan compared with 21 percentage points higher in India.
Figure. Quintile-Specific Health Service Indicators.
Noncommunicable disease indicators, especially diabetes and hypertension, were available only for Bangladesh and India, so these indicators were excluded here for comparison. The range of measures was from Q1 (poorest quintile) to Q5 (wealthiest quintile). ANC indicates antenatal care; ARI, acute respiratory infection; CCI, composite coverage index; CPI, prevention coverage index; CTI, treatment coverage index; DPT3, 3 doses of diphtheria-tetanus-pertussis vaccine; FP, family planning; ORT, oral rehydration therapy; Pneumonia, care-seeking for pneumonia; Polio3, 3 doses of polio vaccine; and SBA, skilled birth attendant.
Table 4. Magnitude of Inequalities by Intervention in 5 South Asian Countries.
| Indicator | Relative Index of Inequality (95% CI) | ||||
|---|---|---|---|---|---|
| Afghanistan | Bangladesh | India | Nepal | Pakistan | |
| Prevention | |||||
| Improved water | 3.2 (2.6-3.8) | 1.1 (1.0-1.1) | 1.0 (1.0-1.0) | 1.2 (1.2-1.3) | 0.9 (0.9-1.0) |
| Adequate sanitation | 15.7 (9.7-21.8) | 3.2 (2.7-3.7) | 4.7 (4.4-5.1) | 1.7 (1.5-1.9) | 6.4 (5.9-6.8) |
| FP needs satisfied | 2.0 (1.5-2.4) | 1.0 (0.9-1.1) | 1.8 (1.7-1.9) | 1.1 (1.0-1.1) | 1.6 (1.2-1.9) |
| ≥1 ANC visit | 1.7 (1.5-1.9) | 3.0 (2.6-3.5) | 1.1 (1.0-1.1) | 3.0 (2.5-3.6) | 2.0 (1.9-2.1) |
| ≥4 ANC visits | 5.1 (3.6-6.6) | 10.8 (7.3-14.4) | 1.2 (1.1-1.3)a | 4.8 (3.6-6.1) | 8.7 (7.8-9.5) |
| DPT3 immunization | 1.7 (1.4-1.9) | 1.2 (1.1-1.4) | 1.4 (1.4-1.5) | 1.1 (1.0-1.2) | 1.9 (1.3-2.6) |
| Measles immunization | 1.2 (1.1-1.4) | 1.3 (1.2-1.5) | 1.2 (1.2-1.3) | 1.1 (1.0-1.2) | 1.7 (1.2-2.2) |
| BCG immunization | 1.5 (1.3-1.6) | 1.1 (1.0-1.1) | 1.2 (1.2-1.2) | 1.0 (1.0-1.1) | 1.3 (1.1-1.5) |
| Polio3 immunization | 1.2 (1.1-1.3) | 1.2 (1.1-1.3) | 1.2 (1.3-1.2) | 1.1 (1.0-1.2) | 1.3 (1.1-1.5) |
| Care-seeking for pneumonia | 1.3 (1.0-1.7) | 1.3 (0.5-2.2) | 1.1 (1.0-1.2) | 1.6 (0.8-2.4) | 1.4 (1.2-1.5) |
| Exclusive breastfeeding | 1.1 (0.8-1.4) | 1.0 (0.6-1.5) | 1.0 (1.0-1.0) | 1.0 (0.4-1.6) | 1.0 (0.8-1.3) |
| Treatmentb | |||||
| ARI treatment | 1.2 (0.8-1.5) | 0.5 (0.3-0.8) | 1.1 (1.0-1.2) | 1.6 (1.2-2.0) | 1.1 (0.8-1.4) |
| Oral rehydration therapy | 0.9 (0.7-1.2) | 0.9 (0.5-1.2) | 1.1 (1.0-1.1) | 1.2 (0.8-1.6) | 1.3 (1.1-1.5) |
| Skilled birth attendance | 5.1 (4.2-5.9) | 5.5 (4.4-6.7) | 4.4 (3.8-5.0) | 4.7 (3.7-5.8) | 3.4 (3.2-3.7) |
| Institutional delivery | 4.8 (4.0-5.6) | 6.8 (5.2-8.4) | 1.3 (1.2-1.4) | 4.1 (3.1-5.1) | 3.6 (3.3-3.9) |
| Hypertension treatment | NA | 2.2 (1.7-2.6) | 1.3 (1.2-1.3) | NA | NA |
| Diabetes treatment | NA | 5.8 (3.2-8.5) | 1.2 (1.2-1.3) | NA | NA |
| Composite Indexesc | |||||
| Coverage | 1.7 (1.5-2.0) | 1.4 (1.0-1.9) | 1.3 (1.3-1.4) | 1.5 (1.4-1.6) | 1.7 (1.6-1.8) |
| Prevention | 1.8 (1.4-2.3) | 1.4 (1.0-1.9) | 1.3 (1.0-1.6) | 1.5 (1.1-1.8) | 1.8 (1.3-2.3) |
| Treatment | 2.2 (1.1-3.4) | 2.3 (0.5-4.2) | 1.3 (0.7-2.0) | 2.5 (1.3-3.8) | 2.3 (1.1-3.5) |
Abbreviations: ANC, antenatal care; ARI, acute respiratory infection; DPT3, 3 doses of diphtheria-tetanus-pertussis vaccine; FP, family planning; NA, not applicable; Polio3, 3 doses of polio vaccine.
Three or more ANC visits.
Diabetes and hypertension were not included to estimate the composite treatment index because these 2 indicators were not available in Afghanistan, Nepal, and Pakistan.
Composite prevention index was developed based on 11 prevention indicators, and composite treatment index was based on 4 treatment indicators by random-effects meta-analysis. Composite coverage index was a weighted mean of 8 interventions (FP needs satisfied, skilled birth attendant, ANC with skilled attendant, DPT3 immunization, measles immunization, BCG immunization, oral rehydration therapy for children with diarrhea, and care-seeking for pneumonia) from 4 specialties (FP, maternity care, child immunization, and case management).
A greater pro-wealthy inequality was also observed for the composite prevention index, composite treatment index, and composite coverage index in all 5 countries (Figure). The overall mean treatment coverage among wealthy households was higher by 49 percentage points in Nepal, 40 percentage points in Pakistan and Afghanistan, 36 points in Bangladesh, and 23 points in India than among poor households (eTable 3 in the Supplement). In the composite prevention index, a greater pro-wealthy inequality was found in Pakistan (37 percentage points), followed by Afghanistan (31 points), Nepal (27 points), Bangladesh (26 points), and India (18 points) (eTable 3 in the Supplement). Wide inequality was observed in the management of NCDs (Table 4 and eTable 3 in the Supplement) among the 2 countries for which data were available. Approximately 42% of persons with hypertension received medication to control their blood pressure in Bangladesh compared with 70% in India. In both countries, the poor population was less likely to receive diabetes and hypertension treatment than the wealthy population.
The proportion of financial catastrophe varied substantially across household socioeconomic profiles. On average, wealthy households were more likely to incur catastrophic health expenditures compared with poor households in all South Asian countries except Pakistan, where almost equal proportions of poor and wealthy families incurred financial catastrophe (Table 3 and eTable 4 in the Supplement).
Discussion
To our knowledge, this study is the first attempt to assess the progress toward universal health coverage in select South Asian countries through a comprehensive range of indicators. Our findings show that the mean coverage of populations with essential health care services and financial risk protection against catastrophic health expenditure and impoverishment is low. Inequality in coverage of health services, especially maternal health interventions and financial risk protection, is common in all 5 South Asian countries.
The present study showed that indicators with similar levels of overall coverage often have very different degrees of inequality. The overall prevention coverage ranged from 53.0% in Afghanistan to 76.8% in Nepal and 76.5 % in Bangladesh, while the mean treatment coverage ranged from 44.8% in Bangladesh to 83.5% in India. A composite coverage index related to reproductive, maternal, and child health interventions was the lowest in Afghanistan and highest in Bangladesh. Greater inequality was seen in both prevention and treatment indicators. Consistent with previous studies, the most inequitable health service indicators in the present study were adequate sanitation, at least 4 antenatal care visits with skilled health personnel, institutional delivery, and the presence of skilled health personnel at birth in most South Asian countries. In all of these indicators, the mean coverage was substantially lower in the poorest population than the wealthy population.
Among prevention indicators, coverage of all child immunization and access to improved drinking water reached the 80% universal health coverage target both at the national and quintile-specific levels only in Bangladesh and Nepal. Despite the large investment in maternal and child health programs in low- and middle-income countries, coverage of most maternal health interventions among the poor population was still low and far from the 80% threshold across all 5 South Asian countries. Similar to another study, professional antenatal care visits and skilled birth attendance at time of birth in the present study had the lowest coverage in Afghanistan compared with the other South Asian countries. In Sustainable Development Goal 3, health intervention coverage of 80% of targets for the poorest population remains out of reach in the immediate future. Therefore, particular efforts should be made to expand the provision of cost-effective priority services to provide a foundation for future developments of low- and middle-priority services.
In Sustainable Development Goal 3, prevention and promotion of NCDs are also given top priority. However, our study found that approximately 58% of the hypertensive patients in Bangladesh and 30% of those in India were not receiving medication to control hypertension. This percentage contrasts sharply with that in the United States, where 62% of patients with hypertension were receiving antihypertensive treatment and 50% had control of their condition in 2007-2008. In the case of diabetes management, approximately 57% of diabetic patients in the United States received oral antidiabetic drugs in 2003-2004 and 57% had controlled glycemic levels. Our study found that approximately 38% of patients with diabetes in Bangladesh and 82% in India were receiving antidiabetic treatment. However, our study found greater pro-wealthy inequality in diabetes and hypertension management in these 2 countries.
The low coverage of NCD treatment might be due to high treatment costs. One study found that approximately 12% of households with a patient who had hypertension or diabetes were borrowing money or selling household assets to cope with treatment costs. The US population also experiences significant out-of-pocket spending on NCDs, and diabetes, heart disease, back pain, and hypertension dominate US health care spending. The most expensive condition, diabetes, accounted for the highest personal health care spending in 2013 in the United States ($101.4 billion), followed by ischemic health disease ($88.1 billion), low back and neck pain ($87.6 billion), and hypertension ($83.9 billion) treatment. Therefore, the increasing burden of high treatment cost will also increase national health expenditure and put a substantial burden on the health system unless the health system incorporates an effective strategy to protect households from such high-cost diseases.
On average, more than 1 in 10 households in most of the South Asian region incurred financial catastrophe, and 3% of nonpoor households became poor due to health care costs. Wealthy households in the South Asian countries were more likely to incur catastrophic health payment compared with disadvantaged households. The major reasons for this lower financial risk among the poor population may be due to the low ability to pay and decisions by a significant proportion of poor populations to forego available health care because of financial constraints. In India, some health insurance plans target poor populations; however, reimbursements are lacking for outpatient services and medicines, which is the major reason that people incur high out-of-pocket payments in India. Nepalese community-based health insurance also offers a special subsidized rate to the extremely poor population. Despite this special attention, disadvantaged populations in Nepal still face significant financial risk. Similarly, Afghanistan and Bangladesh lack a formal social safety net, and citizens remain financially insecure. Consequently, approximately 15% of households in Afghanistan and Bangladesh were facing financial catastrophe. This level represents a significant challenge for the universal health coverage goal of ensuring 100% financial protection against catastrophic and impoverishing health care payments by 2030.
Although health services coverage is high among wealthy populations in all 5 South Asian countries, the existing health systems fail to ensure equitable access to essential health services and protect households from financial risk associated with health care costs. Health systems reform is therefore essential. Reforms should include strong political commitment, increased government spending on health through budget reallocation, improved service delivery, proper monitoring of subsidized programs, ensuring standardized costs for both official and unofficial fees across all public facilities, and reconsidering both the demand side (committing to proper risk-pooling mechanisms for the whole population, expanding benefits, and reducing cost-sharing) and the supply side (expansion of infrastructure, human resources for health, and health services).
Limitations
Our study has some weaknesses. The first of these is that NCD treatment-related indicators, including diabetes and hypertension, are lacking in Afghanistan, Nepal, and Pakistan. Although NCDs are now the leading cause of the burden of disease, the availability of data to measure access to basic interventions was limited, at least in these surveys, and did not permit accurate characterization of access. Development of ongoing monitoring systems for the prevalence of NCDs, NCD risk factors, access to NCD care, and quality of care is a challenge for measurement of progress toward universal health coverage. It was also not possible to assess the quality or effectiveness of services available in the countries analyzed. Data availability and quality issues resulted in certain countries being excluded from parts of the analysis, which may limit generalizability. However, our study benefited from the use of a wide range of metrics, including treatment indicators as well as typical prevention and promotion indicators, where data permitted.
Conclusions
Universal health coverage is a crucial step forward for South Asian countries seeking to ensure access to essential health services without imposing financial risk upon citizens. Recent improved service provision in certain key areas is encouraging and highlights the increasing enthusiasm and momentum behind the universal health coverage movement. However, the ultimate challenge for policymakers is not merely to improve clinical services but also to ensure equity in service and treatment coverage and protection against health care–related financial hardship. The journey toward universal health coverage is far from complete, but with proper attention to access and equity in health, even the poorest nations in South Asia can make steady progress toward achieving health care for all.
eTable 1. Description of the Included Surveys by Country
eTable 2. List of Intervention Coverage and Financial Risk Indicators and Data Sources
eTable 3. Slope Index of Inequality by Intervention in Five South Asian Countries
eTable 4. Slope Index of Inequality in Catastrophic Health Payments in Five South Asian Countries
eMethods. Measurement of Indices and Indicators
References
- 1.United Nations Sustainable Development knowledge platform. Sustainable Development goal. https://sustainabledevelopment.un.org/. Accessed October 7, 2015.
- 2.World Health Organization Monitoring Progress Towards Universal Health Coverage at Country and Global Levels: Framework, Measures and Targets Geneva, Switzerland: World Health Organization and International Bank for Reconstruction and Development, World Bank; 2014. [Google Scholar]
- 3.Boerma T, Eozenou P, Evans D, Evans T, Kieny M-P, Wagstaff A. Monitoring progress towards universal health coverage at country and global levels. PLoS Med. 2014;11(9):e1001731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization Tracking Universal Health Coverage: First Global Monitoring Report. Geneva, Switzerland: World Health Organization; 2015. [Google Scholar]
- 5.Schmidt H, Gostin LO, Emanuel EJ. Public health, universal health coverage, and Sustainable Development goals: can they coexist? Lancet. 2015;386(9996):928-930. [DOI] [PubMed] [Google Scholar]
- 6.Atun R, Aydın S, Chakraborty S, et al. Universal health coverage in Turkey: enhancement of equity. Lancet. 2013;382(9886):65-99. [DOI] [PubMed] [Google Scholar]
- 7.Atun R, de Andrade LO, Almeida G, et al. Health-system reform and universal health coverage in Latin America. Lancet. 2015;385(9974):1230-1247. [DOI] [PubMed] [Google Scholar]
- 8.Lagomarsino G, Garabrant A, Adyas A, Muga R, Otoo N. Moving towards universal health coverage: health insurance reforms in nine developing countries in Africa and Asia. Lancet. 2012;380(9845):933-943. [DOI] [PubMed] [Google Scholar]
- 9.Reeves A, Gourtsoyannis Y, Basu S, McCoy D, McKee M, Stuckler D. Financing universal health coverage—effects of alternative tax structures on public health systems: cross-national modelling in 89 low-income and middle-income countries. Lancet. 2015;386(9990):274-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reich MR, Harris J, Ikegami N, et al. Moving towards universal health coverage: lessons from 11 country studies. Lancet. 2016;387(10020):811-816. [DOI] [PubMed] [Google Scholar]
- 11.Stuckler D, Feigl AB, Basu S, McKee M The political economy of universal health coverage. http://www.pacifichealthsummit.org/downloads/UHC/the%20political%20economy%20of%20uhc.PDF. World Health Organization paper HSR/BCKGRT/8/2010/. Published 2010. Accessed January 25, 2017.
- 12.Vos T, Allen C, Arora M, et al. ; GBD 2015 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study, 2015. Lancet. 2016;388(10053):1545-1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang H, Naghavi M, Allen C, et al. ; GBD 2015 Mortality and Causes of Death Collaborators . Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459-1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scammell K, Noble DJ, Rasanathan K, et al. A landscape analysis of universal health coverage for mothers and children in South Asia. BMJ Glob Health. 2016;1(1):e000017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wehrmeister FC, Restrepo-Mendez MC, Franca GV, Victora CG, Barros AJ. Summary indices for monitoring universal coverage in maternal and child health care. Bull World Health Organ. 2016;94(12):903-912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Doorslaer E, O’Donnell O, Rannan-Eliya RP, et al. Catastrophic payments for health care in Asia. Health Econ. 2007;16(11):1159-1184. [DOI] [PubMed] [Google Scholar]
- 17.Requejo JH, Bryce J, Barros AJ, et al. Countdown to 2015 and beyond: fulfilling the health agenda for women and children. Lancet. 2015;385(9966):466-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McIntyre D, Thiede M, Dahlgren G, Whitehead M. What are the economic consequences for households of illness and of paying for health care in low- and middle-income country contexts? Soc Sci Med. 2006;62(4):858-865. [DOI] [PubMed] [Google Scholar]
- 19.World Bank DataBank: world development indicators. http://databank.worldbank.org/data/reports.aspx?source=world-development-indicators. Accessed January 25, 2017.
- 20.Boerma T, AbouZahr C, Evans D, Evans T. Monitoring intervention coverage in the context of universal health coverage. PLoS Med. 2014;11(9):e1001728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barros AJ, Ronsmans C, Axelson H, et al. Equity in maternal, newborn, and child health interventions in Countdown to 2015: a retrospective review of survey data from 54 countries. Lancet. 2012;379(9822):1225-1233. [DOI] [PubMed] [Google Scholar]
- 22.Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Stat. 1950:607-611. [Google Scholar]
- 23.Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Obare V, Brolan CE, Hill PS. Indicators for universal health coverage: can Kenya comply with the proposed post-2015 monitoring recommendations? Int J Equity Health. 2014;13:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lim S, Kate A, Bhutta Z, et al. ; GBD 2015 SDG Collaborators . Measuring the health-related Sustainable Development Goals in 188 countries: a baseline analysis from the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1813-1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O’Donnell O, Van Doorsslaer E, Wagstaff A, Lindelöw M. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and Their Implementation. Vol 434 Washington, DC: World Bank Publications; 2008. [Google Scholar]
- 27.Barros AJ, Victora CG. Measuring coverage in MNCH: determining and interpreting inequalities in coverage of maternal, newborn, and child health interventions. PLoS Med. 2013;10(5):e1001390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Regidor E. Measures of health inequalities: part 2. J Epidemiol Community Health. 2004;58(11):900-903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.United Nations General Assembly Transforming Our World: the 2030 Agenda for Sustainable Development. New York: United Nations; 2015. [Google Scholar]
- 30.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303(20):2043-2050. [DOI] [PubMed] [Google Scholar]
- 31.Ong KL, Cheung BM, Wong LY, Wat NM, Tan KC, Lam KS. Prevalence, treatment, and control of diagnosed diabetes in the US: National Health and Nutrition Examination Survey 1999-2004. Ann Epidemiol. 2008;18(3):222-229. [DOI] [PubMed] [Google Scholar]
- 32.Rahman MM, Gilmour S, Saito E, Sultana P, Shibuya K. Self-reported illness and household strategies for coping with health-care payments in Bangladesh. Bull World Health Organ. 2013;91(6):449-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dieleman JL, Baral R, Birger M, et al. US spending on personal health care and public health, 1996-2013. JAMA. 2016;316(24):2627-2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Selvaraj S, Karan AK. Deepening health insecurity in India: evidence from national sample surveys since 1980s. Econ Polit Wkly. 2009;40:55-60. [Google Scholar]
- 35.Stoermer M, Fuerst F, Rijal K, et al. Review of community-based health insurance initiatives in Nepal. Kathmandu, Nepal: Deutsche Gesellschaft fur internationale Zusammenarbeit (GIZ) Gmbh; December 2012.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Description of the Included Surveys by Country
eTable 2. List of Intervention Coverage and Financial Risk Indicators and Data Sources
eTable 3. Slope Index of Inequality by Intervention in Five South Asian Countries
eTable 4. Slope Index of Inequality in Catastrophic Health Payments in Five South Asian Countries
eMethods. Measurement of Indices and Indicators