Abstract
Importance
Clinical trials have documented that lowering blood pressure reduces cardiovascular disease and premature deaths. However, the optimal target for reduction of systolic blood pressure (SBP) is uncertain.
Objective
To assess the association of mean achieved SBP levels with the risk of cardiovascular disease and all-cause mortality in adults with hypertension treated with antihypertensive therapy.
Data Sources
MEDLINE and EMBASE were searched from inception to December 15, 2015, supplemented by manual searches of the bibliographies of retrieved articles.
Study Selection
Studies included were clinical trials with random allocation to an antihypertensive medication, control, or treatment target. Studies had to have reported a difference in mean achieved SBP of 5 mm Hg or more between comparison groups.
Data Extraction and Synthesis
Data were extracted from each study independently and in duplicate by at least 2 investigators according to a standardized protocol. Network meta-analysis was used to obtain pooled randomized results comparing the association of each 5–mm Hg SBP category with clinical outcomes after adjusting for baseline risk.
Main Outcomes and Measures
Cardiovascular disease and all-cause mortality.
Results
Forty-two trials, including 144 220 patients, met the eligibility criteria. In general, there were linear associations between mean achieved SBP and risk of cardiovascular disease and mortality, with the lowest risk at 120 to 124 mm Hg. Randomized groups with a mean achieved SBP of 120 to 124 mm Hg had a hazard ratio (HR) for major cardiovascular disease of 0.71 (95% CI, 0.60-0.83) compared with randomized groups with a mean achieved SBP of 130 to 134 mm Hg, an HR of 0.58 (95% CI, 0.48-0.72) compared with those with a mean achieved SBP of 140 to 144 mm Hg, an HR of 0.46 (95% CI, 0.34-0.63) compared with those with a mean achieved SBP of 150 to 154 mm Hg, and an HR of 0.36 (95% CI, 0.26-0.51) compared with those with a mean achieved SBP of 160 mm Hg or more. Likewise, randomized groups with a mean achieved SBP of 120 to 124 mm Hg had an HR for all-cause mortality of 0.73 (95% CI, 0.58-0.93) compared with randomized groups with a mean achieved SBP of 130 to 134 mm Hg, an HR of 0.59 (95% CI, 0.45-0.77) compared with those with a mean achieved SBP of 140 to 144 mm Hg, an HR of 0.51 (95% CI, 0.36-0.71) compared with those with a mean achieved SBP of 150 to 154 mm Hg, and an HR of 0.47 (95% CI, 0.32-0.67) compared with those with a mean achieved SBP of 160 mm Hg or more.
Conclusions and Relevance
This study suggests that reducing SBP to levels below currently recommended targets significantly reduces the risk of cardiovascular disease and all-cause mortality. These findings support more intensive control of SBP among adults with hypertension.
This systematic review and network meta-analysis assesses the association of mean achieved systolic blood pressure levels with the risk of cardiovascular disease and all-cause mortality in adults with hypertension treated with antihypertensive therapy.
Key Points
Question
What is the optimal target for reduction of systolic blood pressure among patients with hypertension?
Findings
In this systematic review and network meta-analysis of 42 trials, including 144 220 patients, linear associations were seen between mean achieved systolic blood pressure and risk of cardiovascular disease and mortality, with the lowest risk at a systolic blood pressure of 120 to 124 mm Hg.
Meaning
Reducing systolic blood pressure below currently recommended targets with commonly used antihypertensive medications may significantly reduce the risk of cardiovascular disease and all-cause mortality.
Introduction
Hypertension is the leading global preventable risk factor for cardiovascular disease (CVD) and premature death. Observational epidemiologic studies have shown a strong, independent, and log-linear association between usual systolic blood pressure (SBP) and mortality from CVD and all causes, with no evidence of a threshold down to at least 115 mm Hg. Randomized clinical trials have documented that lowering blood pressure (BP) with commonly used regimens reduces the risk of CVD and all-cause mortality. However, post hoc analyses based on achieved BP in some clinical trials, in which the results were not analyzed according to the randomized treatment assignment, identified a J-shaped association between achieved BP and risk of CVD and all-cause mortality, especially between achieved BP and coronary heart disease (CHD).
The uncertainty of optimal goals for treatment for patients with hypertension has resulted in inconsistent recommendations for BP targets in clinical practice guidelines. For example, compared with the 2003 Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, the 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults raised the recommended SBP treatment goal from less than 130 mm Hg to less than 140 mm Hg for patients with type 2 diabetes or chronic kidney disease and from less than 140 mm Hg to less than 150 mm Hg for individuals 60 years of age or older. Recently, the Systolic Blood Pressure Intervention Trial (SPRINT) reported that intensive treatment (targeting an SBP of <120 mm Hg), as compared with standard treatment (targeting an SBP of <140 mm Hg), significantly reduced CVD and all-cause mortality among adults with hypertension who were at high risk for CVD, but without diabetes or stroke. The data from SPRINT support a more intensive SBP treatment goal, although concerns remain regarding its generalizability to populations at large with hypertension.
Finding the optimal SBP target could have far-reaching implications for the reduction of CVD and premature death in general populations. By using a network meta-analysis to combine available data from randomized clinical trials, we compared the association of different levels of SBP reduction with the risk of major CVD, stroke, CHD, CVD mortality, and all-cause mortality.
Methods
Data Sources and Searches
We searched MEDLINE and EMBASE using the following search terms as medical subject headings and key words: (antihypertensive agents OR blood pressure lowering OR antihypertensive treatment) AND (cardiovascular disease OR coronary disease OR myocardial infarction OR stroke OR heart failure OR mortality). The searches were conducted without language or date restriction, from inception to December 15, 2015. We limited searches to randomized clinical trials in human adults. Additional trials were identified by hand-searching bibliographies from included studies, reviews, and meta-analyses.
Study Selection
Titles and abstracts of retrieved articles were independently screened by at least 2 of us (J.D.B., C.L., P.S., and X.B.). Articles deemed potentially eligible by either reviewer were retrieved for full-text review. Disagreements on full-text review were resolved by discussion and consensus.
Studies were included if they met the following criteria: (1) participants were randomly allocated to an antihypertensive medication, control, or treatment target; (2) the allocation to antihypertensive treatment was independent of other treatment regimens; (3) the sample size was 100 patients or more in each treatment group; (4) trial duration was 6 months or more; (5) one or more events for an outcome of interest were reported in each treatment group; (6) mean achieved SBP level was reported for each treatment group, and the difference in mean achieved SBP between the comparison groups was 5 mm Hg or more; and (7) outcomes included major CVD, stroke, CHD, CVD mortality, or all-cause mortality. Clinical trials with mean achieved SBP of 160 mm Hg or more in both comparison groups were excluded because they do not contribute information to the optimal target for SBP treatment. For studies with multiple publications, data from the article with the longest trial follow-up time were included.
Data Extraction and Quality Assessment
Data abstraction was conducted by 2 of us (J.D.B., C.L., P.S., and X.B.) who independently used a predefined, standardized protocol and data collection instrument. Information was recorded on sample size, demographic characteristics, and medical history of the trial participants; BP measurement methods; mean achieved BP during treatment; follow-up time; outcome ascertainment methods; and number of events for each outcome. The predefined outcomes were major CVD events (including CHD, stroke, heart failure, and CVD deaths), stroke, CHD, CVD mortality, and all-cause mortality.
Risk of bias was assessed by 2 of us (J.D.B., C.L., P.S., and X.B.) using the Cochrane Collaboration’s risk of bias tool, based on 7 domains: random sequence generation, allocation concealment, blinding of participants and outcome assessment, incomplete data, selective reporting, intention-to-treat analysis, and other sources of bias. Disagreement was resolved by consensus.
Data Synthesis and Analysis
Network meta-analysis allows pooling of results derived from direct and indirect evidence across multiple different treatments while preserving the benefits of randomized comparisons within each trial. We constructed network diagrams for each outcome and the overall network to visualize direct and indirect comparisons between SBP treatment levels. Treatment nodes were defined by categorizing SBP into the following 10 separate treatment levels: less than 120, 120 to 124, 125 to 129, 130 to 134, 135 to 139, 140 to 144, 145 to 149, 150 to 154, 155 to 159, and 160 mm Hg or more. We used a Bayesian hierarchical random-effects model with a binomial likelihood and complementary log-log link function to model the probability of events. Hazard ratios (HRs) for each possible comparison were calculated using Markov Chain Monte Carlo simulation.
For an individual trial, each randomization group was assigned to 1 category of achieved SBP according to the group’s mean SBP level during the trial, irrespective of medications used or initial treatment target. Thus, each trial contributed to 2 distinct achieved SBP categories based on randomization groups. Hazard ratios comparing the lower vs higher achieved SBP categories from each trial using intention-to-treat analysis results within specific SBP comparison groups (eg, 120-124 vs 130-134 mm Hg) were pooled. Therefore, randomized comparisons within each trial were preserved. The pooled HR for a given comparison is composed of direct evidence obtained from trials comparing the 2 SBP randomization groups and indirect evidence obtained from the association of all randomized SBP comparisons in the network. In addition, we conducted the following 2 sensitivity analyses: the first excluding SPRINT to assess its influence on the results, given its large sample size and treatment effects, and the second excluding trials with 4 or more categories deemed at “high” or “unclear” risk of bias.
To account for trial heterogeneity in the intervention duration and baseline risk of CVD or mortality, we adjusted for trial length and event rate (or mortality) of the reference groups for each trial in the model. The median of the posterior distribution was selected as the point estimate, bounded by the 2.5th and 97.5th percentiles to form a 95% CI. Heterogeneity was assessed by monitoring the posterior between-trial SD. We used inconsistency models, design-by-treatment interaction models, and the node-splitting method to evaluate the differences between direct and indirect comparisons.
Finally, publication bias was assessed using funnel plots and the Egger test for direct comparisons with 4 or more studies. All analyses were conducted using WinBUGS, version 1.4.3 (Medical Research Council Biostatistics Unit), R, version 3.2.1 (R Project for Statistical Computing), and Stata, version 12.1 (StataCorp LP). A detailed description of the methods is available in the eAppendix in the Supplement.
Results
Searches of MEDLINE and EMBASE yielded 2721 records, and manual searches of bibliographies of reviews, meta-analyses, and other trial publications identified an additional 26 articles (Figure 1). After removal of duplicates, 2371 titles and abstracts were screened for eligibility, and 449 article texts were reviewed in full.
Figure 1. Study Selection Flow Diagram.
A total of 42 trials were included in the analyses, with a combined sample size of 144 220 individuals (eTable 1 in the Supplement). The mean achieved SBP levels ranged from 114 to 171 mm Hg among treatment groups. The trials were conducted in diverse study populations with various comorbidities, and 30 trials included participants with type 2 diabetes. Trial duration ranged from 6 months to more than 8 years, with a mean follow-up of 3.7 years across all trials. Most trials used standardized BP measurement methods (eTable 2 in the Supplement) and had a low risk of bias (eTable 3 in the Supplement).
The network of included trials was well connected, with many direct comparisons across the categories of mean achieved SBP levels (Figure 2; eFigure 1 in the Supplement). The group with an SPB of 130 to 134 mm Hg defined the center of the network, with 21 trials directly comparing a mean achieved SBP of 130 to 134 mm Hg with 7 other mean achieved SBP groups. A total of 31 trials contributed to network comparisons for major CVD, 27 trials for stroke, 27 trials for CHD, 41 trials for all-cause mortality, and 33 trials for CVD mortality. Descriptions of outcomes are available in eTable 4 in the Supplement.
Figure 2. Network of Treatment Comparisons for Cardiovascular Disease and Mortality According to Achieved Systolic Blood Pressure Categories Among 42 Clinical Trials.
Each node (blue circle) represents an achieved systolic blood pressure category. The size of the nodes corresponds to the number of trials of the categories. Comparisons are linked with a line, the thickness of which corresponds to the number of trials that assessed the comparison. Numbers next to every line indicate the number of trials directly comparing the categories.
In general, there were linear associations between mean achieved SBP levels and the risk of major CVD, stroke, CHD, all-cause mortality, and CVD mortality (Figure 3 and Figure 4; eFigure 2 and eTables 5-7 in the Supplement). The lowest risks for major CVD, CHD, all-cause mortality, and CVD mortality were at a mean achieved SBP of 120 to 124 mm Hg, whereas the lowest risk for stroke was at a mean achieved SBP of less than 120 mm Hg.
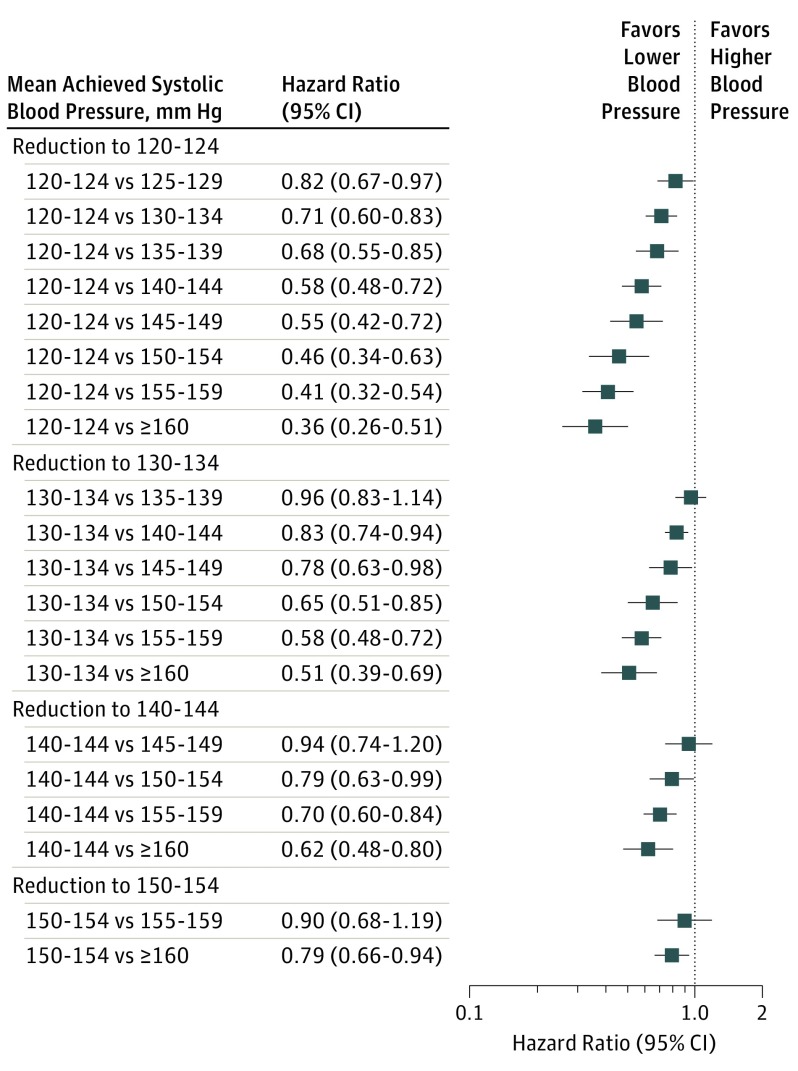
Figure 3. Hazard Ratios and 95% CIs for Major Cardiovascular Disease Associated With More Intensive Reductions in Systolic Blood Pressure.
Square markers indicate hazard ratios for major cardiovascular disease events comparing lower mean achieved systolic blood pressure with higher mean achieved systolic blood pressure. Error bars indicate 95% CIs.
Figure 4. Hazard Ratios and 95% CIs for All-Cause Mortality Associated With More Intensive Reductions in Systolic Blood Pressure.
Square markers indicate hazard ratios for all-cause mortality comparing lower mean achieved systolic blood pressure with higher mean achieved systolic blood pressure. Error bars indicate 95% CIs.
Randomized groups with a mean achieved SBP of 120 to 124 mm Hg had an HR for major CVD of 0.71 (95% CI, 0.60-0.83) compared with randomized groups with a mean achieved SBP of 130 to 134 mm Hg, an HR of 0.58 (95% CI, 0.48-0.72) compared with those with a mean achieved SBP of 140 to 144 mm Hg, an HR of 0.46 (95% CI, 0.34-0.63) compared with those with a mean achieved SBP of 150 to 154 mm Hg, and an HR of 0.36 (95% CI, 0.26-0.51) compared with those with a mean achieved SBP of 160 mm Hg or more (Figure 3; eTable 5 in the Supplement). Randomized groups with a mean achieved SBP of 120 to 124 mm Hg had an HR for stroke of 0.69 (95% CI, 0.40-1.07) compared with randomized groups with a mean achieved SBP of 130 to 134 mm Hg, an HR of 0.51 (95% CI, 0.26-0.87) compared with those with a mean achieved SBP of 140 to 144 mm Hg, an HR of 0.36 (95% CI, 0.17-0.68) compared with those with a mean achieved SBP of 150 to 154 mm Hg, and an HR of 0.27 (95% CI, 0.12-0.51) compared with those with a mean achieved SBP of 160 mm Hg or more (eFigure 2 and eTable 5 in the Supplement). A similar but weaker association between mean achieved SBP and CHD was observed (eFigure 2 and eTable 6 in the Supplement).
Randomized groups with a mean achieved SBP of 120 to 124 mm Hg had an HR for all-cause mortality of 0.73 (95% CI, 0.58-0.93) compared with randomized groups with a mean achieved SBP of 130 to 134 mm Hg, an HR of 0.59 (95% CI, 0.45-0.77) compared with those with a mean achieved SBP of 140 to 144 mm Hg, an HR of 0.51 (95% CI, 0.36-0.71) compared with those with a mean achieved SBP of 150 to 154 mm Hg, and an HR of 0.47 (95% CI, 0.32-0.67) compared with those with a mean achieved SBP of 160 mm Hg or more (Figure 4; eTable 7 in the Supplement). Randomized groups with a mean achieved SBP of 120 to 124 mm Hg had an HR for CVD mortality of 0.67 (95% CI, 0.40-1.22) compared with randomized groups with a mean achieved SBP of 130 to 134 mm Hg, an HR of 0.55 (95% CI, 0.30-1.07) compared with those with a mean achieved SBP of 140 to 144 mm Hg, an HR of 0.43 (0.22-0.93) compared with those with a mean achieved SBP of 150 to 154 mm Hg, and an HR of 0.34 (0.17-0.76) compared with those with a mean achieved SBP of 160 mm Hg or more (eFigure 2 and eTable 7 in the Supplement).
In a sensitivity analysis excluding SPRINT, HRs and 95% CIs were consistent with results from the main analyses for major CVD, CHD, and all-cause mortality, indicating the lowest risk at an SBP of 120 to 124 mm Hg for these outcomes (eTables 8-10 in the Supplement). However, in the sensitivity analysis, the lowest-risk group for stroke was the group with an SBP of 120 to 124 mm Hg, and the lowest-risk group for CVD mortality was the group with an SBP of less than 120 mm Hg. In the main analyses, the lowest-risk group for stroke was the group with an SBP of less than 120 mm Hg, and the lowest-risk group for CVD mortality was the group with an SBP of 120 to 124 mm Hg. A second sensitivity analysis excluding trials with 4 or more categories deemed at “high” or “unclear” risk of bias did not substantively change the results compared with the main analyses (eTables 11-13 in the Supplement).
Model fit for all outcomes was adequate according to the Bayesian deviance information criterion, and the baseline risk covariate did not significantly alter the models (eTables 14-18 in the Supplement). Heterogeneity was present for each outcome, with random-effects models fitting better than fixed-effects models according to the Bayesian deviance information criterion. The magnitude of heterogeneity was low to moderate, with a between-trial SD of 0.081 for major CVD and an SD ranging from 0.103 to 0.248 for the other outcomes (eTables 14-18 in the Supplement).
There was no network-wide evidence of inconsistency between direct and indirect comparisons in any of the outcomes based on inconsistency models and design-by-treatment interaction analyses (eTables 19-23 in the Supplement). However, inconsistency was present in a few individual comparisons based on node-splitting analyses (major CVD, 125-129 vs 130-134 mm Hg; CHD, 125-129 vs 130-134 mm Hg; and CVD mortality, 120-124 vs 130-134 mm Hg, and 120-124 vs 135-139 mm Hg). There was no evidence of publication bias.
Discussion
This network meta-analysis of randomized clinical trials documented significant and linear associations between mean achieved SBP and the risk of CVD and all-cause mortality. The lowest risks for CVD and all-cause mortality were among randomized groups with a mean achieved SBP of 120 to 124 mm Hg. These findings support recently published results from SPRINT and suggest a benefit of reducing SBP below the currently recommended target among adults with hypertension.
The SPRINT trial randomly assigned 9361 persons 50 years of age or older with an SBP of 130 to 180 mm Hg who had an increased risk of CVD, but without diabetes or stroke, to receive intensive treatment or standard treatment of SBP. Blood pressure was measured in accordance with a prespecified, standardized protocol. The mean achieved SBP was 121.5 mm Hg in the intensive-treatment group and 134.6 mm Hg in the standard-treatment group during the intervention. During a median follow-up of 3.26 years, a significant 25% reduction in the primary composite outcome of CVD events (HR, 0.75; 95% CI, 0.64-0.89; P < .001) and a 27% reduction in all-cause mortality (HR, 0.73; 95% CI, 0.60-0.90; P = .003) were reported.
In our network meta-analysis, compared with randomized groups with a mean achieved SBP of 130 to 134 mm Hg, CVD was reduced by 29% (HR, 0.71; 95% CI, 0.60-0.83), and all-cause mortality was reduced by 27% (HR, 0.73; 95% CI, 0.58-0.93), among randomized groups with a mean achieved SBP of 120 to 124 mm Hg. This agreement persisted even after excluding SPRINT in a sensitivity analysis. The findings from SPRINT and our network meta-analysis suggest that a more intensive treatment target than currently recommended (eg, SBP of 120-124 mm Hg) provides additional benefits for prevention of CVD complications and all-cause mortality.
Our study contributes additional information on SBP management strategies beyond SPRINT. First, our study included 42 clinical trials conducted for 144 220 patients with various comorbidities (including diabetes and stroke), age ranges, and mean BP levels at baseline. Therefore, these results are generalizable to populations at large with hypertension. Second, our study compared multiple levels of achieved SBP on the risk of CVD and all-cause mortality and found positive and linear associations between achieved SBP and clinical outcomes. Our findings do not support the existence of a J-shaped association between achieved SBP and the risk of CVD and all-cause mortality. Furthermore, our study indicates that there is a linear association between the magnitudes of SBP reduction and the risk of CVD and all-cause mortality. For example, by lowering SBP by 10 mm Hg to achieve the treatment goal of 120 to 124 mm Hg, the risk of CVD was reduced by 29% (95% CI, 17%-40%), by lowering SBP by 20 mm Hg, the risk of CVD was reduced by 42% (95% CI, 28%-52%), by lowering SBP by 30 mm Hg, the risk of CVD was reduced by 54% (95% CI, 37%-66%), and by lowering SBP by 40 mm Hg or more, the risk of CVD was reduced by 64% (95% CI, 49%-74%). These data support a more intensive SBP management approach to achieve a lower SBP goal.
Several meta-analyses have examined the association with CVD and mortality of more intensive vs less intensive treatment of BP. Recently, Xie and colleagues reported an updated meta-analysis of 19 clinical trials, including 44 989 participants, on the association of intensive BP reduction with CVD outcomes. The mean achieved SBP was 133 mm Hg (range, 118-144 mm Hg) in the more intensive treatment group and 140 mm Hg (range, 124-154 mm Hg) in the less intensive treatment group. Intensive BP-lowering treatment was associated with a reduction of 14% (95% CI, 4%-22%) for major CVD, 13% (95% CI, 0%-24%) for myocardial infarction, and 22% (95% CI, 10%-32%) for stroke. However, more intensive treatment had no significant association with CVD mortality (9%; 95% CI, –11% to 26%) or all-cause mortality (9%; 95% CI, –3% to 19%). Another recent meta-analysis conducted by Ettehad and colleagues suggested that every 10–mm Hg reduction in SBP, including to levels less than 130 mm Hg, significantly reduced the risk of major CVD and CHD. Our network meta-analysis results complement and expand on the findings from these traditional meta-analyses. Our analyses, based on many achieved SBP categories while maintaining randomized treatment assignments, show a beneficial linear association between more intensively reduced mean achieved SBPs and clinical outcomes, and identify the lowest risk at a mean SBP of 120 to 124 mm Hg.
The association of intensive treatment in subgroups of patients with certain comorbidities, especially type 2 diabetes, have been of particular interest. The Action to Control Cardiovascular Risk in Diabetes trial examined the association of an intensive SBP target (<120 mm Hg) compared with a standard SBP target (<140 mm Hg) for patients with diabetes, finding a nonsignificant benefit on reducing risk for CVD events, which could be a consequence of reduced statistical power or use of a factorial design. A 2012 meta-analysis conducted by McBrien and colleagues reported a small reduction in the risk of stroke associated with more intensive BP reduction in adults with type 2 diabetes but found inconclusive results for mortality and CHD. Another recent meta-analysis by Brunström and Carlberg reported increased risk of CVD mortality among patients with diabetes who had a baseline SBP of less than 140 mm Hg and reduced their level of SBP via treatment, suggesting a J-shaped association. We were able to include many trials of patients with diabetes and other comorbidities. Our findings do not support the existence of a J-shaped association among populations at large with hypertension.
Strengths and Limitations
There are several strengths in this network meta-analysis compared with the previous meta-analyses that used traditional analysis methods. Network meta-analysis methods offer a unique advantage compared with traditional meta-regression techniques by allowing the simultaneous comparison of multiple achieved SBP levels on clinical outcomes while preserving trial-level treatment randomization and its associated protection against bias. Our study allowed for comparisons of a wider range of mean achieved SBP levels than has been possible in traditional meta-analyses, with a spread from less than 120 mm Hg to more than 160 mm Hg, and identified the lowest risks for CVD and all-cause mortality at a mean achieved SBP of 120 to 124 mm Hg. Another strength of our network meta-analysis is that it uses all available information (direct and indirect comparisons) to compare the association of each mean achieved SBP level with clinical outcomes. Therefore, it was possible to base the comparisons between various SBP levels on a much larger number of clinical trials compared with similar meta-analyses limited to trials examining more intensive compared with less intensive therapy; our study included 42 trials compared with the traditional analysis from Xie et al that included 19 trials. Our data indicate that there was no significant difference between direct and indirect comparisons at the network level. In addition, we used a systematic and comprehensive search strategy to identify a wide coverage of available antihypertensive clinical trials. Most of the included trials had low risk of bias; a sensitivity analysis indicated that trials with unclear risk of bias did not substantially influence our results. Finally, our analyses included a large number of trials conducted in diverse patient populations and were adjusted for differences in intervention duration and baseline risk among trials, which increases the generalizability of our findings.
Our findings should be interpreted in light of several limitations, most of which have been common to all meta-analyses conducted in this topic area. First, we had limited sample size in some mean achieved SBP comparisons. For example, only 3 trials achieved mean SBP levels below 120 mm Hg, with a combined sample size of 7333. Thus, most of the evidence in our analyses is based on trials treating participants to achieve SBP levels above 120 mm Hg. Second, few trials reported heart failure outcomes, which resulted in an insufficiently connected network to analyze this outcome. Similarly, we were unable to assess the association of intensive SBP reduction with kidney disease outcomes, dementia, or adverse events such as hypotension or falling, which have been concerns with intensive treatment of BP. Furthermore, we were unable to conduct subgroup analyses by age, race/ethnicity, history of CVD, stroke, chronic kidney disease, or diabetes owing to insufficient data. Finally, we defined treatment nodes according to the mean achieved SBP in each randomization group, which does not consider the distribution of individual SBP levels within groups. Thus, mean achieved SBP groups may represent a range of SBPs. In addition, analysis of mean achieved SBP does not guide treatment decisions regarding diastolic BP.
There are several implications for clinicians based on findings from SPRINT, other meta-analyses, and our network meta-analysis. First, data suggest that treatment to achieve an SBP below currently recommended guidelines reduces the risk for major CVD and all-cause mortality in adults with hypertension. However, there may be a tradeoff between these benefits and potential adverse effects of intensive SBP reduction, including hypotension, electrolyte abnormalities, and kidney injury. Thus, clinicians should continue to monitor acute adverse effects in individual patients and make treatment decisions based on accurate BP measurements, according to standardized protocols similar to those used in clinical trials. Second, although our analysis suggests that intensive SBP reduction reduces risk for major CVD and all-cause mortality in populations at large with hypertension, including in those with diabetes, the outcomes of intensive SBP reduction for patients with diabetes warrant further exploration. Clinicians should be particularly vigilant when treating patients with comorbidities, including diabetes. Finally, the most effective strategies for implementing more intensive SBP reduction in general clinical practice remain to be established. Future research should consider the best practices for treating patients to reduce SBP levels below current guidelines in the routine clinical management of hypertension.
Conclusions
Our study indicates that treating patients to reduce SBP below currently recommended targets may significantly reduce risk of CVD and all-cause mortality. These findings support more intensive SBP control among adults with hypertension and suggest the need for revising the current clinical guidelines for management of hypertension.
eAppendix. Methods
eFigure 1. Networks of Treatment Comparisons for Cardiovascular Disease and Mortality According to Randomization Groups With Various Mean Levels of Achieved Systolic Blood Pressure
eFigure 2. Hazard Ratios and 95% CIs for Stroke, Coronary Heart Disease, and Cardiovascular Disease Mortality Associated With More Intensive Reductions in Systolic Blood Pressure
eTable 1. Characteristics of 42 Clinical Trials With 144,220 Participants
eTable 2. Description of Blood Pressure Measurement Methods for All Included Trials
eTable 3. Quality Assessment and Risk of Bias for All Included Trials
eTable 4. Description of Cardiovascular Disease, Coronary Heart Disease, Stroke, and Cardiovascular Disease Mortality Outcomes for All Included Trials
eTable 5. Hazard Ratios and 95% CIs for Major Cardiovascular Disease and Stroke Associated With More Intensive Reductions in Systolic Blood Pressure
eTable 6. Hazard Ratios and 95% CIs for Coronary Heart Disease Associated With More Intensive Reductions in Systolic Blood Pressure
eTable 7. Hazard Ratios and 95% CIs for All-Cause Mortality and Cardiovascular Disease Mortality Associated With More Intensive Reductions in Systolic Blood Pressure
eTable 8. Hazard Ratios and 95% CIs for Major Cardiovascular Disease and Stroke Associated With More Intensive Reductions in Systolic Blood Pressure in Sensitivity Analysis Excluding SPRINT
eTable 9. Hazard Ratios and 95% CIs for Coronary Heart Disease Associated With More Intensive Reductions in Systolic Blood Pressure in Sensitivity Analysis Excluding SPRINT
eTable 10. Hazard Ratios and 95% CIs for All-Cause Mortality and Cardiovascular Disease Mortality Associated With More Intensive Reductions in Systolic Blood Pressure in Sensitivity Analysis Excluding SPRINT
eTable 11. Hazard Ratios and 95% CIs for Major Cardiovascular Disease and Stroke Associated With More Intensive Reductions in Systolic Blood Pressure in Sensitivity Analysis Excluding Trials With High or Unclear Risk of Bias
eTable 12. Hazard Ratios and 95% CIs for Coronary Heart Disease Associated With More Intensive Reductions in Systolic Blood Pressure In Sensitivity Analysis Excluding Trials With High or Unclear Risk of Bias
eTable 13. Hazard Ratios and 95% CIs for All-Cause Mortality and Cardiovascular Disease Mortality Associated With More Intensive Reductions in Systolic Blood Pressure in Sensitivity Analysis Excluding Trials With High or Unclear Risk of Bias
eTable 14. Model Fit Characteristics for Major Cardiovascular Disease
eTable 15. Model Fit Characteristics for Stroke
eTable 16. Model Fit Characteristics for All-Cause Mortality
eTable 17. Model Fit Characteristics for Cardiovascular Disease Mortality
eTable 18. Model Fit Characteristics for Coronary Heart Disease
eTable 19. Node-Splitting Results of Testing Consistency for Major Cardiovascular Disease
eTable 20. Node-Splitting Results of Testing Consistency for Stroke
eTable 21. Node-Splitting Results of Testing Consistency for All-Cause Mortality
eTable 22. Node-Splitting Results of Testing Consistency for Cardiovascular Disease Mortality
eTable 23. Node-Splitting Results of Testing Consistency for Coronary Heart Disease
eReferences.
References
- 1.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217-223. [DOI] [PubMed] [Google Scholar]
- 2.GBD 2013 Mortality and Causes of Death Collaborators Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration . Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903-1913. [DOI] [PubMed] [Google Scholar]
- 4.Chobanian AV, Bakris GL, Black HR, et al. ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee . Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206-1252. [DOI] [PubMed] [Google Scholar]
- 5.Turnbull F; Blood Pressure Lowering Treatment Trialists’ Collaboration . Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-1535. [DOI] [PubMed] [Google Scholar]
- 6.Messerli FH, Panjrath GS. The J-curve between blood pressure and coronary artery disease or essential hypertension: exactly how essential? J Am Coll Cardiol. 2009;54(20):1827-1834. [DOI] [PubMed] [Google Scholar]
- 7.Mancia G, Grassi G. Aggressive blood pressure lowering is dangerous: the J-curve: pro side of the argument. Hypertension. 2014;63(1):29-36. [DOI] [PubMed] [Google Scholar]
- 8.James PA, Oparil S, Carter BL, et al. . 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520. [DOI] [PubMed] [Google Scholar]
- 9.Weber MA, Schiffrin EL, White WB, et al. . Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich). 2014;16(1):14-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wright JT Jr, Williamson JD, Whelton PK, et al. ; SPRINT Research Group . A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins JPT, Altman DG, Gøtzsche PC, et al. ; Cochrane Bias Methods Group; Cochrane Statistical Methods Group . The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23(20):3105-3124. [DOI] [PubMed] [Google Scholar]
- 13.Multi-parameter Evidence Synthesis Research Group Mixed treatment comparisons: network meta-analysis. http://www.bristol.ac.uk/social-community-medicine/projects/mpes/mtc/. Accessed September 25, 2015.
- 14.Achana FA, Cooper NJ, Dias S, et al. . Extending methods for investigating the relationship between treatment effect and baseline risk from pairwise meta-analysis to network meta-analysis. Stat Med. 2013;32(5):752-771. [DOI] [PubMed] [Google Scholar]
- 15.Jackson D, Barrett JK, Rice S, White IR, Higgins JPT. A design-by-treatment interaction model for network meta-analysis with random inconsistency effects. Stat Med. 2014;33(21):3639-3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29(7-8):932-944. [DOI] [PubMed] [Google Scholar]
- 17.Jones DW, Weatherly L, Hall JE. SPRINT: what remains unanswered and where do we go from here? Hypertension. 2016;67(2):261-262. [DOI] [PubMed] [Google Scholar]
- 18.Xie X, Atkins E, Lv J, et al. . Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387(10017):435-443. [DOI] [PubMed] [Google Scholar]
- 19.Ettehad D, Emdin CA, Kiran A, et al. . Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387(10022):957-967. [DOI] [PubMed] [Google Scholar]
- 20.Cushman WC, Evans GW, Byington RP, et al. ; ACCORD Study Group . Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575-1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Margolis KL, O’Connor PJ, Morgan TM, et al. . Outcomes of combined cardiovascular risk factor management strategies in type 2 diabetes: the ACCORD randomized trial. Diabetes Care. 2014;37(6):1721-1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McBrien K, Rabi DM, Campbell N, et al. . Intensive and standard blood pressure targets in patients with type 2 diabetes mellitus: systematic review and meta-analysis. Arch Intern Med. 2012;172(17):1296-1303. [DOI] [PubMed] [Google Scholar]
- 23.Brunström M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses. BMJ. 2016;352:i717. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Methods
eFigure 1. Networks of Treatment Comparisons for Cardiovascular Disease and Mortality According to Randomization Groups With Various Mean Levels of Achieved Systolic Blood Pressure
eFigure 2. Hazard Ratios and 95% CIs for Stroke, Coronary Heart Disease, and Cardiovascular Disease Mortality Associated With More Intensive Reductions in Systolic Blood Pressure
eTable 1. Characteristics of 42 Clinical Trials With 144,220 Participants
eTable 2. Description of Blood Pressure Measurement Methods for All Included Trials
eTable 3. Quality Assessment and Risk of Bias for All Included Trials
eTable 4. Description of Cardiovascular Disease, Coronary Heart Disease, Stroke, and Cardiovascular Disease Mortality Outcomes for All Included Trials
eTable 5. Hazard Ratios and 95% CIs for Major Cardiovascular Disease and Stroke Associated With More Intensive Reductions in Systolic Blood Pressure
eTable 6. Hazard Ratios and 95% CIs for Coronary Heart Disease Associated With More Intensive Reductions in Systolic Blood Pressure
eTable 7. Hazard Ratios and 95% CIs for All-Cause Mortality and Cardiovascular Disease Mortality Associated With More Intensive Reductions in Systolic Blood Pressure
eTable 8. Hazard Ratios and 95% CIs for Major Cardiovascular Disease and Stroke Associated With More Intensive Reductions in Systolic Blood Pressure in Sensitivity Analysis Excluding SPRINT
eTable 9. Hazard Ratios and 95% CIs for Coronary Heart Disease Associated With More Intensive Reductions in Systolic Blood Pressure in Sensitivity Analysis Excluding SPRINT
eTable 10. Hazard Ratios and 95% CIs for All-Cause Mortality and Cardiovascular Disease Mortality Associated With More Intensive Reductions in Systolic Blood Pressure in Sensitivity Analysis Excluding SPRINT
eTable 11. Hazard Ratios and 95% CIs for Major Cardiovascular Disease and Stroke Associated With More Intensive Reductions in Systolic Blood Pressure in Sensitivity Analysis Excluding Trials With High or Unclear Risk of Bias
eTable 12. Hazard Ratios and 95% CIs for Coronary Heart Disease Associated With More Intensive Reductions in Systolic Blood Pressure In Sensitivity Analysis Excluding Trials With High or Unclear Risk of Bias
eTable 13. Hazard Ratios and 95% CIs for All-Cause Mortality and Cardiovascular Disease Mortality Associated With More Intensive Reductions in Systolic Blood Pressure in Sensitivity Analysis Excluding Trials With High or Unclear Risk of Bias
eTable 14. Model Fit Characteristics for Major Cardiovascular Disease
eTable 15. Model Fit Characteristics for Stroke
eTable 16. Model Fit Characteristics for All-Cause Mortality
eTable 17. Model Fit Characteristics for Cardiovascular Disease Mortality
eTable 18. Model Fit Characteristics for Coronary Heart Disease
eTable 19. Node-Splitting Results of Testing Consistency for Major Cardiovascular Disease
eTable 20. Node-Splitting Results of Testing Consistency for Stroke
eTable 21. Node-Splitting Results of Testing Consistency for All-Cause Mortality
eTable 22. Node-Splitting Results of Testing Consistency for Cardiovascular Disease Mortality
eTable 23. Node-Splitting Results of Testing Consistency for Coronary Heart Disease
eReferences.