This systematic review and meta-analysis estimates prevalence of fetal alcohol spectrum disorder among children and youth in the general population by country and international region.
Key Points
Question
What is the prevalence of fetal alcohol spectrum disorder among children and youth in the general population?
Findings
In this meta-analysis of 24 unique studies and 1416 unique children and youth with fetal alcohol spectrum disorder, approximately 8 of 1000 in the general population had fetal alcohol spectrum disorder, and 1 of every 13 pregnant women who consumed alcohol during pregnancy delivered a child with fetal alcohol spectrum disorder. The prevalence of fetal alcohol spectrum disorder was found to be notably higher among special populations.
Meaning
The prevalence of fetal alcohol spectrum disorder among children and youth in the general population exceeds 1% in 76 countries, which underscores the need for universal prevention initiatives targeting maternal alcohol consumption, screening protocols, and improved access to diagnostic services, especially in special populations.
Abstract
Importance
Prevalence estimates are essential to effectively prioritize, plan, and deliver health care to high-needs populations such as children and youth with fetal alcohol spectrum disorder (FASD). However, most countries do not have population-level prevalence data for FASD.
Objective
To obtain prevalence estimates of FASD among children and youth in the general population by country, by World Health Organization (WHO) region, and globally.
Data Sources
MEDLINE, MEDLINE in process, EMBASE, Education Resource Information Center, Cumulative Index to Nursing and Allied Health Literature, Web of Science, PsychINFO, and Scopus were systematically searched for studies published from November 1, 1973, through June 30, 2015, without geographic or language restrictions.
Study Selection
Original quantitative studies that reported the prevalence of FASD among children and youth in the general population, used active case ascertainment or clinic-based methods, and specified the diagnostic guideline or case definition used were included.
Data Extraction and Synthesis
Individual study characteristics and prevalence of FASD were extracted. Country-specific random-effects meta-analyses were conducted. For countries with 1 or no empirical study on the prevalence of FASD, this indicator was estimated based on the proportion of women who consumed alcohol during pregnancy per 1 case of FASD. Finally, WHO regional and global mean prevalence of FASD weighted by the number of live births in each country was estimated.
Main Outcomes and Measures
Prevalence of FASD.
Results
A total of 24 unique studies including 1416 unique children and youth diagnosed with FASD (age range, 0-16.4 years) were retained for data extraction. The global prevalence of FASD among children and youth in the general population was estimated to be 7.7 per 1000 population (95% CI, 4.9-11.7 per 1000 population). The WHO European Region had the highest prevalence (19.8 per 1000 population; 95% CI, 14.1-28.0 per 1000 population), and the WHO Eastern Mediterranean Region had the lowest (0.1 per 1000 population; 95% CI, 0.1-0.5 per 1000 population). Of 187 countries, South Africa was estimated to have the highest prevalence of FASD at 111.1 per 1000 population (95% CI, 71.1-158.4 per 1000 population), followed by Croatia at 53.3 per 1000 population (95% CI, 30.9-81.2 per 1000 population) and Ireland at 47.5 per 1000 population (95% CI, 28.0-73.6 per 1000 population).
Conclusions and Relevance
Globally, FASD is a prevalent alcohol-related developmental disability that is largely preventable. The findings highlight the need to establish a universal public health message about the potential harm of prenatal alcohol exposure and a routine screening protocol. Brief interventions should be provided, where appropriate.
Introduction
Alcohol consumption during pregnancy may cause a wide range of adverse health effects to the developing fetus, including but not limited to cognitive, behavioral, emotional, and adaptive functioning deficits, as well as congenital anomalies. The health effects of prenatal exposure to ethyl alcohol have been subsumed under the umbrella term fetal alcohol spectrum disorder (FASD), which consists of as many as 4 diagnostic entities, including fetal alcohol syndrome (FAS), partial FAS, alcohol-related neurodevelopmental disorder, and depending on the diagnostic guideline, alcohol-related birth defects. Alcohol can affect any organ or system in the developing fetus, and as such, individuals with FASD may experience a broad array of comorbid conditions. A recent study identified 428 comorbid conditions in individuals with FASD, with diagnoses from 18 of 22 chapters of the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Thus, clinicians from all specialties and other health service professionals will likely encounter cases of FASD. The effects of prenatal alcohol exposure have lifelong implications, and thus, FASD is costly for society. For example, the lifetime cost for a person with FASD in North America is estimated at more than $1 million.
Although human research has not been able to delineate the pattern, amount, and/or critical period of prenatal alcohol exposure necessary for structural and/or functional teratogenesis, animal models have demonstrated that all stages of embryonic development are vulnerable to the teratogenic effects of alcohol. Furthermore, the type and severity of birth defects induced by prenatal alcohol exposure are largely dependent on the pattern of exposure, the dose, and the developmental stage of the embryo at the time of exposure. Multiple animal models have also shown that even low levels of prenatal alcohol exposure can lead to brain dysfunction, which can lead to behavioral abnormalities. However, beyond the amount of alcohol consumed and the gestational timing of consumption, multiple factors (eg, variability in the metabolism and genetic background of the mother and fetus, environmental influences, maternal age, smoking, nutritional status, stress levels, and possibly paternal lifestyle) modify fetal susceptibility to the teratogenic effects of ethanol.
Updated prevalence estimates are essential to effectively prioritize, plan, and deliver health care to high-needs populations, such as children and youth with FASD. These estimates are also vital for assessing the population burden of disease and allocation of resources for health care and prevention. In much of the world, no prevalence estimates of FASD exist, which may influence prioritization of health care expenditures for care related to FASD. Until recently, a meaningful estimate of FASD prevalence was not possible. However, the publication of more representative rates of prenatal alcohol exposure and improved data on the prevalence of FASD in some settings now allows for estimates of the prevalence of FASD globally. Therefore, in the present study, we aimed to estimate the prevalence of FASD among children and youth in the general population globally, by World Health Organization (WHO) region, and by country. We then compared the global prevalence estimate of FASD among children and youth in the general population with the prevalence of FASD among special populations, such as aboriginal, correctional, and low socioeconomic status populations; those undergoing psychiatric care; and children in care (eg, in foster care, residing in orphanages, and adopted), obtained from select studies.
Methods
The comprehensive systematic literature search and meta-analyses were conducted and reported according to the standards of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Meta-analysis of Observational Studies in Epidemiology (MOOSE) reporting guidelines. The full review protocol is available in the PROSPERO database.
Comprehensive Systematic Search Strategy
We performed a systematic literature search of MEDLINE, MEDLINE in process, EMBASE, Education Resource Information Center, Cumulative Index to Nursing and Allied Health Literature, Web of Science, PsychINFO, and Scopus to identify all studies that have reported the prevalence of FASD among the general population (keywords are given in eTable 1 in the Supplement). The search was not limited geographically or by language of publication and included studies published from November 1, 1973 (when FAS was first described), through June 30, 2015. Non–English-language studies deemed to be potentially relevant were translated by colleagues fluent in the respective language or using Google Translate (and subsequently cross-checked by a native speaker). In addition to the electronic search, we manually reviewed the content pages of the major epidemiologic journals and the citations in the relevant articles. Effort was also made to contact the leading international FASD experts and researchers to identify any pending publications on the prevalence of FASD.
Inclusion and Exclusion Criteria
Articles were included in the meta-analysis if they (1) consisted of original, quantitative research published in a peer-reviewed journal or scholarly report; (2) involved a measurement of FASD (or a combination of any of the diagnoses within the spectrum); (3) provided the prevalence of FASD with a measure of uncertainty (CI or SE) or the necessary information to calculate uncertainty (ie, sample size or number of cases); (4) specified the diagnostic guideline or case definition used to ascertain cases; and (5) used active case ascertainment (when researchers actively seek, assess, and identify cases; ie, the criterion standard) or clinic-based methods (prospectively conducted studies in prenatal clinics or hospitals). We excluded articles from the meta-analysis if they (1) reported a pooled estimate by combining several studies; (2) used passive surveillance (the use of existing record collections) to obtain the prevalence of FASD; or (3) were published in iteration. We placed no restriction on the age of participants (ie, articles were not excluded if they reported the prevalence of FASD among adults).
Critical Appraisal of Identified Studies
We critically appraised each study by using a tool recently developed specifically for use in systematic reviews addressing questions of prevalence. The following 7 criteria were used: (1) representative sample of the target population; (2) appropriate recruitment of participants; (3) adequate sample size (≥300); (4) detailed description of participants and setting; (5) sufficient coverage of the identified sample (ie, nonresponders were described and compared with those in the study); (6) use of objective, standard criteria for ascertaining FASD; and (7) appropriateness of statistical analysis.
Data Extraction
After the data were extracted from the identified articles, one of us (S.L.) checked extracted data for accuracy against the original articles. All discrepancies were reconciled by team discussion. We extracted the following variables from the identified articles: country, study year(s), sample size, number of cases, prevalence, 95% CI, age range, percentage of male participants in the sample, method of ascertainment, and the diagnostic guideline or case definition used.
Meta-analyses
To estimate the pooled prevalence of FASD, we performed a meta-analysis assuming a random-effects model for each country with 2 or more existing studies on the prevalence of FASD. As recommended for meta-analyses of prevalence and to prevent the overweighting of studies reporting extremely low prevalence (ie, a prevalence approaching zero), we transformed the data using the Freeman-Tukey double arcsine transformation. We assessed heterogeneity between prevalence estimates using the Cochrane Q test and the I2 statistic. We assessed publication bias by (1) visually inspecting the funnel plot (SE plotted against the point estimate) for a skewed distribution; (2) by using a ranked correlation test; and (3) a weighted regression test. However, we deemed publication bias to be unlikely because an observed prevalence of FASD that was substantially different than had previously been estimated would likely have been published. Therefore, if found to be present, we did not adjust for publication bias. All meta-analyses were performed using R software (version 3.2.2).
Prevalence Estimation
For countries with 1 or no empirical study, we estimated the prevalence of FASD by using country-specific data on the prevalence of alcohol use during pregnancy (obtained from Popova et al). First, we estimated a quotient of the mean number of women who consumed alcohol during pregnancy per 1 case of FASD by using the pooled estimates of the prevalence of FASD available from countries with a WHO drinking pattern score of 3 or less. A country’s drinking pattern score reflects how people in the respective country drink instead of how much they drink and is measured on a scale from 1 (least risky pattern of drinking) to 5 (most risky pattern of drinking); the higher the score, the greater the alcohol-attributable burden of disease. To produce the most conservative estimations, we excluded the estimates of the prevalence of FASD available from countries with a drinking pattern score of 4 or more, because it would have led to an unrealistically high ratio. These data were then linked to the prevalence of alcohol use during pregnancy for each respective country. Second, we applied this quotient to the country-specific prevalence of alcohol use during pregnancy to estimate the prevalence of FASD. To derive the CI for the FASD prevalence point estimate, we conducted Monte Carlo simulations, generating 1 million samples per country. We used the 2.5th and 97.5th percentiles of the resulting distribution as the CI. The Monte Carlo simulations were performed using Python software (version 2.7). Additional methodological details can be found in the eMethods in the Supplement and in the study by Popova and colleagues.
Global and Regional Estimates of the Prevalence of FASD Among Children and Youth in the General Population
To estimate the prevalence of FASD by WHO region and globally, we calculated a weighted mean prevalence of FASD, weighted by the number of live births in each country for the latest available year (2000-2014). We conducted Monte Carlo simulations to estimate the CI (as described above).
Comparison of the Global Prevalence of FASD Among Children and Youth in the General Population With the Prevalence in Special Populations
We compared the global prevalence estimate of FASD among children and youth in the general population with the prevalence of FASD in special populations of various countries, using select studies in the current literature. The associated CI was estimated based on an exact binomial distribution.
Results
Comprehensive Systematic Literature Search
A total of 24 unique studies including 1416 unique children and youth diagnosed with FASD (age range, 0-16.4 years) were retained and selected for data extraction. We identified no studies conducted among adults. Data on the prevalence of FASD among children and youth in the general population were available from the following 8 countries: Australia (2 studies), Canada (1 study), Croatia (2 studies), France (4 studies), Italy (2 studies), Norway (1 study), South Africa (6 studies), and the United States (6 studies) (eFigure 1 in the Supplement). Eighteen studies (75.0%) used active case ascertainment, 5 studies (20.8%) used a clinic-based method, and 1 study (4.2%) used a mixed-methods approach. Most of the studies (45.8%) used the clarification of the Institute of Medicine criteria for the diagnosis of FASD. Study characteristics and prevalence of FASD reported in the identified studies are given in Table 1; the diagnostic breakdown of FASD in the identified studies is provided in eTable 2 in the Supplement; and the critical appraisal of the identified studies is presented in eTable 3 in the Supplement.
Table 1. Study Characteristics and Prevalence of FASD Among Children and Youth in the General Population Reported in the Identified Studies by Country and WHO Region.
| Source | Country (State, Province, or Territory) | Study Period | Sample Size | No. of FASD Cases | Prevalence of FASD per 1000 Population | Diagnostic Guidelines or Case Definition | Male Participants, % | Age Range, y | Method |
|---|---|---|---|---|---|---|---|---|---|
| African Region | |||||||||
| Chersich et al, 2012 | South Africa (Northern Cape, De Aar, and Upington) | 2003-2010 | 809 | 72 | 89.0 | Clarification of the IOM criteria | 49.5 | 9.5-11.0 | ACA |
| May et al, 2007 | South Africa (Western Cape) | 2002-2003 | 818 | 73 | 89.2 | Clarification of the IOM criteria | 51.5 | 6-7 | ACA |
| May et al, 2013 | South Africa (Western Cape) | 2008-2009 | 747 | 155 | 207.5 | Clarification of the IOM criteria | 49.0 | 6-7 | ACA |
| Olivier et al, 2013 | South Africa (rural Western Cape) | 2008 | 160 | 28 | 175.0 | Clarification of the IOM criteria | 50.0 | 4.8-16.4 | ACA |
| Urban et al, 2008 | South Africa (Northern Cape, De Aar, and Upington) | 2001-2004 | 1830 | 161 | 88.0 | IOM criteria | 49.7 | 6-7 | ACA |
| Urban et al, 2015 | South Africa (Northern Cape) | 2012-2013 | 1503 | 96 | 63.9 | Clarification of the IOM criteria | 52.6 | 6-7 | ACA |
| European Region | |||||||||
| Petković and Barišić, 2010 | Croatia (urban) | NA | 466 | 19 | 40.8 | Clarification of the IOM criteria | 46.1 | 6.6-11.1 | ACA |
| Petković and Barišić, 2013 | Croatia (rural) | NA | 824 | 55 | 66.8 | Clarification of the IOM criteria | NA | 7.0-11.9 | ACA |
| Bloch et al, 2008 | France (Alsace, Isère, Paris, Puy de Dôme, and Rhône) | 2008 | 45 919 | 18 | 0.4 | Case definition provided | NA | 0-1 (Newborns) | Clinic based |
| Dehaene et al, 1981 | France (Roubaix) | 1977-1979 | 8284 | 45 | 5.4 | Case definition provided | NA | 0-1 (Newborns) | Clinic based |
| Serreau et al, 2002 | France (Saint-Pierre, Reunion Island) | 1996 | 1320 | 75 | 66.0 | IOM criteria | NA | NA | ACA |
| Toutain and Lejeune, 2008 | France | 1995-2003 | 5000 | 28 | 5.6 | Guidelines established by the Fetal Alcohol Study Group of the RSA | NA | 0-1 (Newborns) | Clinic based |
| May et al, 2006 | Italy (Lazio) | 2004 | 543 | 22 | 40.5 | Clarification of the IOM criteria | 51.0 | 6-7 | ACA |
| May et al, 2011 | Italy (Lazio) | 2005-2007 | 976 | 46 | 47.1 | Clarification of the IOM criteria | 50.6 | 6-7 | ACA |
| Elgen et al, 2007 | Norway (Hordaland) | 1999-2004 | 29 091 | 32 | 1.1 | CDC diagnostic guidelines | NA | NA | ACA |
| Region of the Americas | |||||||||
| Asante and Nelms-Matzke, 1985 | Canada (Northwest British Columbia and Yukon) | 1983-1984 | 33 485 | 176 | 5.3 | Guidelines established by the Fetal Alcohol Study Group of the RSA | 63.0 | 0-16 | ACA |
| Barr and Streissguth, 2001 | United States (Washington State) | 1974-1975 | 1439 | 36 | 25.0 | Case definitions provided | NA | 0-7 | Clinic based |
| Clarren et al, 2001 | United States (Washington State) | NA | 3740 | 26 | 7.0 | 4-Digit diagnostic code | NA | 6-7 | ACA |
| Hingson et al, 1982 | United States (Boston, Massachusetts) | 1977-1979 | 1690 | 37 | 21.9 | Guidelines established by the Fetal Alcohol Study Group of the RSA | NA | 0 (Live births) | Clinic based |
| May et al, 2014 | United States (Midwestern) | 2010-2011 | 1433 | 48 | 33.5 | Clarification of the IOM criteria | 51.8 | 6-7 | ACA |
| May et al, 2015 | United States (Northern Plains) | 2007-2009 | 2334 | 26 | 11.1 | Clarification of the IOM criteria | 54.5 | 6-7 | ACA |
| Poitra et al, 2003 | United States | 1992-2000 | 1384 | 7 | 5.1 | Criteria by Sokol and Clarren | NA | 5-6 | ACA |
| Western Pacific Region | |||||||||
| Elliott et al, 2008 | Australia | 2001-2004 | 1 533 333 | 92 | 0.1 | IOM criteria | NA | 0-15 | ACA |
| Harris and Bucens, 2003 | Australia (Northern Territory) | 1990-2000 | 25 209 | 43 | 1.7 | Adapted 4-digit diagnostic code and the criteria by the AAP | NA | 0-10 | Mixed methods (passive surveillance and clinic based) |
Abbreviations: ACA, active case ascertainment; AAP, American Academy of Pediatrics; CDC, Centers for Disease Control and Prevention; FASD, fetal alcohol spectrum disorder; IOM, Institute of Medicine; NA, not available; RSA, Research Society on Alcoholism; WHO, World Health Organization.
Prevalence of FASD Among Children and Youth in the General Population
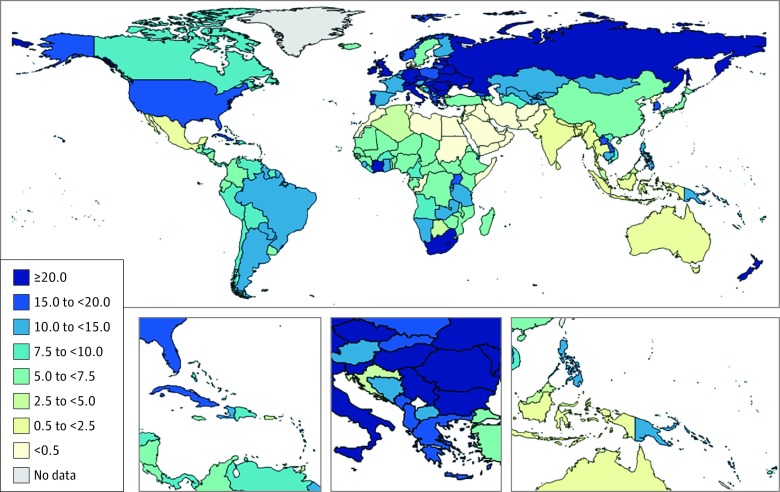
The 5 countries with the highest prevalence of FASD were South Africa at 111.1 per 1000 population (95% CI, 71.1-158.4 per 1000 population), obtained via meta-analysis; Croatia at 53.3 per 1000 population (95% CI, 30.9-81.2 per 1000 population), obtained via meta-analysis; Ireland at 47.5 per 1000 population (95% CI, 28.0-73.6 per 1000 population), obtained via prediction model; Italy at 45.0 per 1000 population (95% CI, 35.1-56.1 per 1000 population), obtained via meta-analysis; and Belarus at 36.6 per 1000 population (95% CI, 23.7-53.2 per 1000 population), obtained via prediction model. Seventy-six countries (of 187 for which observed or predicted estimates were available) had a prevalence of FASD of greater than 1%. The global prevalence of FASD was estimated to be 7.7 per 1000 population (95% CI, 4.9-11.7 per 1000 population), with the European Region having the highest overall prevalence at 19.8 per 1000 population (95% CI, 14.1-28.0 per 1000 population) and the Eastern Mediterranean Region having the lowest overall prevalence at 0.1 per 1000 population (95% CI, 0.1-0.5 per 1000 population). Furthermore, 1 of 13 pregnant women who consumed alcohol while pregnant was estimated to deliver a child with FASD. This estimation would result in a cohort of 630 000 children born with FASD globally every year. Figure 1 and eTable 4 in the Supplement provide the prevalence of FASD by country based on actual and estimated data, and Table 2 provides the global and regional prevalence. A forest plot of the country-specific meta-analyses is presented in eFigure 2 in the Supplement. The results of the tests of heterogeneity and publication bias for the meta-analyses on the prevalence of FASD among children and youth in the general population by country and region are presented in eTable 5 in the Supplement.
Figure 1. Global Prevalence of Fetal Alcohol Spectrum Disorder Among Children and Youth in the General Population in 2012.
Data are expressed as number per 1000 population.
Table 2. Global Prevalence of FASD Among Children and Youth in the General Population by WHO Region in 2012.
| WHO Region | Prevalence Estimate (95% CI) per 1000 Population |
|---|---|
| African Region | 7.8 (5.4-10.7) |
| Eastern Mediterranean Region | 0.1 (0.1-0.5) |
| European Region | 19.8 (14.1-28.0) |
| Region of the Americas | 8.8 (6.4-13.2) |
| Southeast Asia Region | 1.4 (0.6-5.3) |
| Western Pacific Region | 6.7 (4.5-11.7) |
| Globally | 7.7 (4.9-11.7) |
Abbreviations: FASD, fetal alcohol spectrum disorder; WHO, World Health Organization.
Comparison of the Global Prevalence of FASD Among Children and Youth in the General Population With the Prevalence in Special Populations
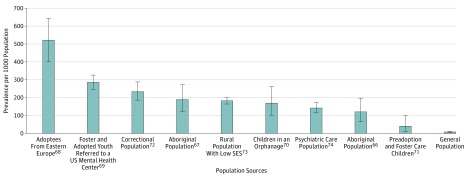
The prevalence of FASD in special populations, based on select studies, was found to be notably higher than the estimated global prevalence among children and youth in the general population (eTable 6 in the Supplement). Specifically, the prevalence of FASD among special populations was 15.6 to 24.6 times higher among aboriginal populations, 5.2 to 67.7 times higher among children in care, 30.3 times higher in a correctional population, 23.7 times higher in a population with low socioeconomic status, and 18.5 times higher among a population in psychiatric care compared with the global prevalence among children and youth in the general population (Figure 2).
Figure 2. Comparison of the Prevalence of Fetal Alcohol Spectrum Disorder in Special Populations With the Global Prevalence Among Children and Youth in the General Population.
Data in special populations are obtained from select studies. Special populations include adoptees from Eastern Europe in Sweden (521.1 per 1000 population; Landgren et al), foster and adopted youth referred to a US children’s mental health center (285.2 per 1000 population; Chasnoff et al), a correctional population in Canada (233.5 per 1000 population; Fast et al), an aboriginal population in Canada (189.7 per 1000 population; Robinson et al), a rural population with low socioeconomic status (SES) in South Africa (182.4 per 1000 population; de Vries et al), children in an orphanage in Brazil (170.2 per 1000 population; Strömland et al), a US population in psychiatric care (142.4 per 1000 population; Bell and Chimata), an aboriginal population in Australia (120.4 per 1000 population; Fitzpatrick et al), and children before adoption or in foster care in Israel (40.0 per 1000 population; Tenenbaum et al). Prevalence in the general population is described in Table 2. Error bars indicate 95% CI.
Discussion
This study identified several important public health issues. First, based on the existing data, 1 of every 13 pregnant women who consumed alcohol during pregnancy is estimated to have had a child with FASD. Second, this finding leads to an estimate that more than 1700 infants with FASD are born every day (630 000 every year) globally. Third, FASD is notably more frequent among special populations (eg, aboriginal populations, children in care, incarcerated populations, and those in psychiatric care). The higher prevalence emphasizes that these high-risk populations deserve special attention for the planning and organization of targeted screening strategies, improved access to diagnostic services, and prevention of maternal alcohol consumption. Fourth, the burden of FASD is elevated in 76 of the 187 countries included in this study, as demonstrated by having a prevalence of FASD that exceeds 1%. In these countries, the prevalence of FASD among children and youth in the general population is higher than the prevalence of some common birth defects in the United States, such as anencephaly, Down syndrome, spina bifida, and trisomy 18.
Most affected children and youth will require lifelong care for the ever-changing phenotype of FASD. The demands for this care will affect virtually every specialty in medicine. The present findings suggest that prenatal alcohol exposure should be a public health priority. With the current level of awareness and extremely limited access to diagnostic services, very few of these alcohol-affected children and youth will ever be diagnosed with FASD. As a result, the focus of their care will often be on a comorbid condition (eg, attention-deficit/hyperactivity disorder or conduct disorder). This focus diminishes the likelihood of care organized around their developmental course, prevention of exposure in their younger siblings, and anticipation of the long-term impairments likely to occur in children and youth with FASD.
A diagnosis of FASD has several potentially important benefits for affected children and youth, namely, early access to developmental interventions, improved quality of life, and ultimately a more prosperous developmental trajectory in terms of social functioning. Currently, several clinical guidelines are available for diagnosing FASD, and although the current criteria overlap with one another, they lack diagnostic reliability owing to low convergent validity. Furthermore, the specificity, sensitivity, and accuracy of the various diagnostic criteria are unknown because, at present, no external standard against which a diagnostic systems classification function can be measured exists.
The absence of widely accepted standardized criteria can ultimately lead to diagnostic misclassification. Thus, a need exists for a common diagnostic approach to be developed. Ideally, novel and reliable biomarkers for detecting fetal effects of alcohol and low and moderate levels of alcohol consumption during pregnancy will be identified. Accurate diagnosis is complicated by the fact that children and youth with FASD have increased rates of comorbidities. Recently, Popova and colleagues reported that more than 9 in 10 of those with FAS had co-occurring problems with conduct, approximately 8 in 10 had communication disorders related to understanding or expressing language, and more than half had attention-deficit/hyperactivity disorder. In addition, more than 50% had hearing loss, more than 60% had problems with vision, and approximately 5 in 10 had congenital malformations of the spine. However, most comorbid conditions found to occur among children and youth with FASD were in those chapters of the ICD-10 pertaining to congenital malformations and mental disorders. This finding highlights the need for expanded attention to FASD and prenatal alcohol exposure in medical education generally and especially for clinicians who provide prenatal care, pediatricians, and psychiatric and mental health care professionals. The finding also stresses the need for improved prevention programs and access to early interventions to minimize the severity of FASD in affected children and youth.
Strengths and Limitations
The strengths of this study include the comprehensive search strategy, strict inclusion and exclusion criteria, critical appraisal of identified studies, rigorous identification of dual publications (thereby avoiding any potential of double counting cases), analytic strategy, use of country-specific indicators to predict the prevalence of alcohol use during pregnancy, and innovative evidence-based statistical analysis. Although the present study used the best available data and provides, to our knowledge, the first estimates of FASD globally, by WHO region, and for 187 countries, several limitations support the need for further research in this area. First, the prevalence of FASD in those countries with 1 or no empirical study was estimated using self-report data on the prevalence of alcohol use during pregnancy, which is vulnerable to reporting and recall biases. As such, the prevalence of alcohol use during pregnancy may be an underestimate. Second, the identified studies used different diagnostic guidelines and case definitions to ascertain cases of FASD, which may have affected the estimated pooled prevalence of FASD in the present study (the direction of this effect depends on the sensitivity and specificity of the diagnostic system). Third, not all studies included in the meta-analyses were conducted on nationally representative population-based samples (eg, clinic-based studies); therefore, some regionally confined studies may have been conducted where FASD was more prevalent. Fourth, the estimated predicted prevalence may differ from the true prevalence owing to the fact that the data from which the values were estimated carry measurement error and uncertainty. Fifth, examination of the effect of timing, dose, and frequency of prenatal alcohol exposure on the risk of FASD was not possible.
In addition, not many countries have actual data on the prevalence of FASD. Thus, the results of the present study highlight the need for countries to conduct their own cross-sectional active case ascertainment studies to obtain their own prevalence data on FASD. When such data become available, the present estimates can be refined. For example, 2 recent studies from South Africa (not included in the current analysis, because they were published outside the time frame covered) reported a prevalence of FASD that ranged from 170 to 259 per 1000 population, which is higher than previously reported.
Conclusions
Our data indicate that FASD is a relatively prevalent alcohol-related developmental disability. However, FASD is a largely preventable condition. Because the present study was restricted to the general population, the current findings emphasize that FASD is not restricted to disadvantaged groups but rather occurs throughout society, regardless of socioeconomic status, educational attainment, or ethnicity. Given the current trend in unplanned pregnancies in developing and developed countries (39% and 47%, respectively), efforts should be made to educate all women of childbearing age about the potential detrimental effects of prenatal alcohol exposure on the developing fetus. Health care professionals are in the best position to do this. Development of a universal screening protocol to detect problematic drinking before and during pregnancy is a potentially inexpensive strategy that can be widely implemented. Last, detection of drinking during pregnancy and successful intervention can eliminate alcohol exposure in subsequent pregnancies, which eliminates risk for FASD in younger siblings.
eTable 1. Keywords Used in the Comprehensive Systematic Literature Search
eTable 2. Diagnostic Breakdown of FASD in the Identified Studies
eTable 3. Critical Appraisal of the Identified Studies Reporting on the Prevalence of FASD Among Children and Youth in the General Population
eTable 4. Prevalence of FASD Among Children and Youth in the General Population by Country and WHO Region in 2012
eTable 5. Pooled Prevalence of FASD Among Children and Youth in the General Population and the Results of the Heterogeneity and Publication Bias Tests by Country and WHO Region
eTable 6. Comparison of the Prevalence of FASD Among Special Populations, Based on Select Studies, to the Global Prevalence Among Children and Youth in the General Population
eMethods. Estimation of the Quotient of the Average Number of Women Who Consumed Alcohol During Pregnancy per 1 Case of FASD
eFigure 1. Schematic Diagram Depicting the Search Strategy Used
eFigure 2. Forest Plot of the Prevalence of FASD Among Children and Youth in the General Population in Australia, Croatia, France, Italy, South Africa, and the United States
References
- 1.Chudley AE, Conry J, Cook JL, Loock C, Rosales T, LeBlanc N; Public Health Agency of Canada’s National Advisory Committee on Fetal Alcohol Spectrum Disorder . Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. CMAJ. 2005;172(5)(suppl):S1-S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoyme HE, May PA, Kalberg WO, et al. . A practical clinical approach to diagnosis of fetal alcohol spectrum disorders: clarification of the 1996 Institute of Medicine criteria. Pediatrics. 2005;115(1):39-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stratton K, Howe C, Battaglia F. Fetal Alcohol Syndrome: Diagnosis, Epidemiology, Prevention, and Treatment. Washington, DC: National Academy Press; 1996. [Google Scholar]
- 4.Popova S, Lange S, Shield K, et al. . Comorbidity of fetal alcohol spectrum disorder: a systematic review and meta-analysis. Lancet. 2016;387(10022):978-987. [DOI] [PubMed] [Google Scholar]
- 5.Lupton C, Burd L, Harwood R. Cost of fetal alcohol spectrum disorders. Am J Med Genet C Semin Med Genet. 2004;127C(1):42-50. [DOI] [PubMed] [Google Scholar]
- 6.Popova S, Lange S, Burd L, Rehm J. Economic burden of fetal alcohol spectrum disorder in Canada in 2013. Alcohol Alcohol. 2016;51(3):367-375. [DOI] [PubMed] [Google Scholar]
- 7.Thanh NX, Jonsson E. Costs of fetal alcohol spectrum disorder in Alberta, Canada. Can J Clin Pharmacol. 2009;16(1):e80-e90. [PubMed] [Google Scholar]
- 8.Weeks M. Economic impact of fetal alcohol syndrome, IR 89-100015: memorandum to Senator Johne Binkeley. Juneau, Alaska: Senate Advisory Council, Alaska State Legislature; February 17, 1989.
- 9.Sulik KK. Fetal alcohol spectrum disorder: pathogenesis and mechanisms. Handb Clin Neurol. 2014;125:463-475. [DOI] [PubMed] [Google Scholar]
- 10.Jacobson JL, Jacobson SW. Prenatal alcohol exposure and neurobehavioral development: where is the threshold? Alcohol Health Res World. 1994;18(1):30-36. [PMC free article] [PubMed] [Google Scholar]
- 11.Jacobson JL, Jacobson SW. Drinking moderately and pregnancy: effects on child development. Alcohol Res Health. 1999;23(1):25-30. [PMC free article] [PubMed] [Google Scholar]
- 12.O’Leary-Moore SK, Parnell SE, Lipinski RJ, Sulik KK. Magnetic resonance-based imaging in animal models of fetal alcohol spectrum disorder. Neuropsychol Rev. 2011;21(2):167-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sood B, Delaney-Black V, Covington C, et al. . Prenatal alcohol exposure and childhood behavior at age 6 to 7 years, I: dose-response effect. Pediatrics. 2001;108(2):E34. [DOI] [PubMed] [Google Scholar]
- 14.Hamilton DA, Barto D, Rodriguez CI, et al. . Effects of moderate prenatal ethanol exposure and age on social behavior, spatial response perseveration errors and motor behavior. Behav Brain Res. 2014;269:44-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Day J, Savani S, Krempley BD, Nguyen M, Kitlinska JB. Influence of paternal preconception exposures on their offspring: through epigenetics to phenotype. Am J Stem Cells. 2016;5(1):11-18. [PMC free article] [PubMed] [Google Scholar]
- 16.Eberhart JK, Parnell SE. The genetics of fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2016;40(6):1154-1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.May PA, Gossage JP. Maternal risk factors for fetal alcohol spectrum disorders: not as simple as it might seem. Alcohol Res Health. 2011;34(1):15-26. [PMC free article] [PubMed] [Google Scholar]
- 18.Liberati A, Altman DG, Tetzlaff J, et al. . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stroup DF, Berlin JA, Morton SC, et al. ; Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group . Meta-analysis of Observational Studies in Epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008-2012. [DOI] [PubMed] [Google Scholar]
- 20.Global prevalence of fetal alcohol spectrum disorder (FASD). CRD42016033837. http://www.crd.york.ac.uk/PROSPERO/. Accessed January 31, 2016.
- 21.Jones KL, Smith DW. Recognition of the fetal alcohol syndrome in early infancy. Lancet. 1973;302(7836):999-1001. [DOI] [PubMed] [Google Scholar]
- 22.Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag. 2014;3(3):123-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177-188. [DOI] [PubMed] [Google Scholar]
- 24.Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67(11):974-978. [DOI] [PubMed] [Google Scholar]
- 25.Rücker G, Schwarzer G, Carpenter J, Olkin I. Why add anything to nothing? the arcsine difference as a measure of treatment effect in meta-analysis with zero cells. Stat Med. 2009;28(5):721-738. [DOI] [PubMed] [Google Scholar]
- 26.Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Stat. 1950;21(4):607-611. [Google Scholar]
- 27.Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10(1):101-129. [Google Scholar]
- 28.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539-1558. [DOI] [PubMed] [Google Scholar]
- 29.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088-1101. [PubMed] [Google Scholar]
- 30.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629-634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.R Core Team R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2015. [Google Scholar]
- 32.Popova S, Lange S, Probst C, Gmel G, Rehm J. Estimation of national, regional, and global prevalence of alcohol use during pregnancy and fetal alcohol syndrome: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(3):e290-e299. [DOI] [PubMed] [Google Scholar]
- 33.Graham C, Talay D. Stochastic Simulation and Monte Carlo Methods: Mathematical Foundations of Stochastic Simulation. Berlin, Germany: Springer; 2013. [Google Scholar]
- 34.Python Software Foundation Python Language Reference, Version 2.7. Wilmington, Delaware: Python Software Foundation; 2016. [Google Scholar]
- 35.United Nations Population and Vital Statistics Report: Statistical Papers, Series A. Vol LXVII New York, NY: United Nations, Department of Economic and Social Affairs, Statistics Division; 2016. [Google Scholar]
- 36.Elliott EJ, Payne J, Morris A, Haan E, Bower C. Fetal alcohol syndrome: a prospective national surveillance study. Arch Dis Child. 2008;93(9):732-737. [DOI] [PubMed] [Google Scholar]
- 37.Harris KR, Bucens IK. Prevalence of fetal alcohol syndrome in the top end of the Northern Territory. J Paediatr Child Health. 2003;39(7):528-533. [DOI] [PubMed] [Google Scholar]
- 38.Asante KO, Nelms-Maztke J. Report on the Survey of Children With Chronic Handicaps and Fetal Alcohol Syndrome in the Yukon and Northwest British Columbia. Whitehorse, YT: Council for Yukon Indians; 1985. [Google Scholar]
- 39.Petković G, Barisić I. FAS prevalence in a sample of urban schoolchildren in Croatia. Reprod Toxicol. 2010;29(2):237-241. [DOI] [PubMed] [Google Scholar]
- 40.Petković G, Barišić I. Prevalence of fetal alcohol syndrome and maternal characteristics in a sample of schoolchildren from a rural province of Croatia. Int J Environ Res Public Health. 2013;10(4):1547-1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bloch J, Cans C, de Vigan C, et al. Feasibility of the foetal alcohol syndrome surveillance [in French]. Arch Pediatr. 2008;15(5):507-509. [DOI] [PubMed] [Google Scholar]
- 42.Dehaene P, Crépin G, Delahousse G, et al. Epidemiological aspects of the foetal alcoholism syndrome: 45 cases [in French]. Nouv Presse Med. 1981;10(32):2639-2643. [PubMed] [Google Scholar]
- 43.Serreau R, Maillard T, Verdier R, et al. Clinical study and prevalence of fetal alcohol syndrome in medico-social institutions of the Reunion Island [in French]. Arch Pediatr. 2002;9(1):14-20. [DOI] [PubMed] [Google Scholar]
- 44.Toutain S, Lejeune C. Family management of infants with fetal alcohol syndrome or fetal alcohol spectrum disorders. J Dev Phys Disabil. 2008;20:425-436. [Google Scholar]
- 45.May PA, Fiorentino D, Phillip Gossage J, et al. . Epidemiology of FASD in a province in Italy: prevalence and characteristics of children in a random sample of schools. Alcohol Clin Exp Res. 2006;30(9):1562-1575. [DOI] [PubMed] [Google Scholar]
- 46.May PA, Fiorentino D, Coriale G, et al. . Prevalence of children with severe fetal alcohol spectrum disorders in communities near Rome, Italy: new estimated rates are higher than previous estimates. Int J Environ Res Public Health. 2011;8(6):2331-2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Elgen I, Bruaroy S, Laegreid LM. Lack of recognition and complexity of foetal alcohol neuroimpairments. Acta Paediatr. 2007;96(2):237-241. [DOI] [PubMed] [Google Scholar]
- 48.Chersich MF, Urban M, Olivier L, Davies LA, Chetty C, Viljoen D. Universal prevention is associated with lower prevalence of fetal alcohol spectrum disorders in Northern Cape, South Africa: a multicentre before-after study. Alcohol Alcohol. 2012;47(1):67-74. [DOI] [PubMed] [Google Scholar]
- 49.May PA, Gossage JP, Marais AS, et al. . The epidemiology of fetal alcohol syndrome and partial FAS in a South African community. Drug Alcohol Depend. 2007;88(2-3):259-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.May PA, Blankenship J, Marais AS, et al. . Approaching the prevalence of the full spectrum of fetal alcohol spectrum disorders in a South African population-based study. Alcohol Clin Exp Res. 2013;37(5):818-830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Olivier L, Urban M, Chersich M, Temmerman M, Viljoen D. Burden of fetal alcohol syndrome in a rural West Coast area of South Africa. S Afr Med J. 2013;103(6):402-405. [DOI] [PubMed] [Google Scholar]
- 52.Urban M, Chersich MF, Fourie LA, Chetty C, Olivier L, Viljoen D. Fetal alcohol syndrome among grade 1 schoolchildren in Northern Cape Province: prevalence and risk factors. S Afr Med J. 2008;98(11):877-882. [PubMed] [Google Scholar]
- 53.Urban MF, Olivier L, Viljoen D, et al. . Prevalence of fetal alcohol syndrome in a South African city with a predominantly Black African population. Alcohol Clin Exp Res. 2015;39(6):1016-1026. [DOI] [PubMed] [Google Scholar]
- 54.Barr HM, Streissguth AP. Identifying maternal self-reported alcohol use associated with fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2001;25(2):283-287. [PubMed] [Google Scholar]
- 55.Clarren SK, Randels SP, Sanderson M, Fineman RM. Screening for fetal alcohol syndrome in primary schools: a feasibility study. Teratology. 2001;63(1):3-10. [DOI] [PubMed] [Google Scholar]
- 56.Hingson R, Alpert JJ, Day N, et al. . Effects of maternal drinking and marijuana use on fetal growth and development. Pediatrics. 1982;70(4):539-546. [PubMed] [Google Scholar]
- 57.May PA, Baete A, Russo J, et al. . Prevalence and characteristics of fetal alcohol spectrum disorders. Pediatrics. 2014;134(5):855-866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.May PA, Keaster C, Bozeman R, et al. . Prevalence and characteristics of fetal alcohol syndrome and partial fetal alcohol syndrome in a Rocky Mountain Region City. Drug Alcohol Depend. 2015;155:118-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Poitra BA, Marion S, Dionne M, et al. . A school-based screening program for fetal alcohol syndrome. Neurotoxicol Teratol. 2003;25(6):725-729. [DOI] [PubMed] [Google Scholar]
- 60.Hoyme HE, Kalberg WO, Elliott AJ, et al. . Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics. 2016;138(2):e20154256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rosett HL. A clinical perspective of the fetal alcohol syndrome. Alcohol Clin Exp Res. 1980;4(2):119-122. [DOI] [PubMed] [Google Scholar]
- 62.Bertrand J, Floyd RL, Weber MK, et al. ; National Task Force on FAS/FAE. Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. Atlanta, GA: Centers for Disease Control and Prevention; 2004. [Google Scholar]
- 63.Astley SJ, Clarren SK. Diagnostic Guide for Fetal Alcohol Syndrome and Related Conditions: The 4-Digit Diagnostic Code. 2nd ed Washington, DC: University of Washington Publication Services; 1999. [Google Scholar]
- 64.Sokol RJ, Clarren SK. Guidelines for use of terminology describing the impact of prenatal alcohol on the offspring. Alcohol Clin Exp Res. 1989;13(4):597-598. [DOI] [PubMed] [Google Scholar]
- 65.American Academy of Pediatrics Committee on Substance Abuse and Children With Disabilities. Fetal alcohol syndrome and alcohol-related neurodevelopmental disorders. Pediatrics. 2000;106(2, pt 1):358-361. [PubMed] [Google Scholar]
- 66.Fitzpatrick JP, Latimer J, Carter M, et al. . Prevalence of fetal alcohol syndrome in a population-based sample of children living in remote Australia: the Lililwan Project. J Paediatr Child Health. 2015;51(4):450-457. [DOI] [PubMed] [Google Scholar]
- 67.Robinson GC, Conry JL, Conry RF. Clinical profile and prevalence of fetal alcohol syndrome in an isolated community in British Columbia. CMAJ. 1987;137(3):203-207. [PMC free article] [PubMed] [Google Scholar]
- 68.Landgren M, Svensson L, Strömland K, Andersson Grönlund M. Prenatal alcohol exposure and neurodevelopmental disorders in children adopted from eastern Europe. Pediatrics. 2010;125(5):e1178-e1185. [DOI] [PubMed] [Google Scholar]
- 69.Chasnoff IJ, Wells AM, King L. Misdiagnosis and missed diagnoses in foster and adopted children with prenatal alcohol exposure. Pediatrics. 2015;135(2):264-270. [DOI] [PubMed] [Google Scholar]
- 70.Strömland K, Ventura LO, Mirzaei L, et al. . Fetal alcohol spectrum disorders among children in a Brazilian orphanage. Birth Defects Res A Clin Mol Teratol. 2015;103(3):178-185. [DOI] [PubMed] [Google Scholar]
- 71.Tenenbaum A, Hertz P, Dor T, Castiel Y, Sapir A, Wexler ID. Fetal alcohol spectrum disorder in Israel: increased prevalence in an at-risk population. Isr Med Assoc J. 2011;13(12):725-729. [PubMed] [Google Scholar]
- 72.Fast DK, Conry J, Loock CA. Identifying fetal alcohol syndrome among youth in the criminal justice system. J Dev Behav Pediatr. 1999;20(5):370-372. [DOI] [PubMed] [Google Scholar]
- 73.de Vries MM, Marais AS, Buckley D. Epidemiology of fetal alcohol spectrum disorders in rural communities in South Africa: prevalence, child characteristics, and maternal risk factors. Alcohol Clin Exp Res. 2014;38(s1):251A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bell CC, Chimata R. Prevalence of neurodevelopmental disorders among low-income African Americans at a clinic on Chicago’s South Side. Psychiatr Serv. 2015;66(5):539-542. [DOI] [PubMed] [Google Scholar]
- 75.Parker SE, Mai CT, Canfield MA, et al. ; National Birth Defects Prevention Network . Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res A Clin Mol Teratol. 2010;88(12):1008-1016. [DOI] [PubMed] [Google Scholar]
- 76.Clarren SK, Lutke J, Sherbuck M. The Canadian guidelines and the interdisciplinary clinical capacity of Canada to diagnose fetal alcohol spectrum disorder. J Popul Ther Clin Pharmacol. 2011;18(3):e494-e499. [PubMed] [Google Scholar]
- 77.Burd L. Fetal alcohol spectrum disorder: complexity from comorbidity. Lancet. 2016;387(10022):926-927. [DOI] [PubMed] [Google Scholar]
- 78.Coles CD, Gailey AR, Mulle JG, Kable JA, Lynch ME, Jones KL. A comparison among 5 methods for the clinical diagnosis of fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2016;40(5):1000-1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Burd L, Klug MG, Li Q, Kerbeshian J, Martsolf JT. Diagnosis of fetal alcohol spectrum disorders: a validity study of the fetal alcohol syndrome checklist. Alcohol. 2010;44(7-8):605-614. [DOI] [PubMed] [Google Scholar]
- 80.Astley SJ, Clarren SK. Diagnosing the full spectrum of fetal alcohol-exposed individuals: introducing the 4-digit diagnostic code. Alcohol Alcohol. 2000;35(4):400-410. [DOI] [PubMed] [Google Scholar]
- 81.O’Leary CM, Nassar N, Zubrick SR, Kurinczuk JJ, Stanley F, Bower C. Evidence of a complex association between dose, pattern and timing of prenatal alcohol exposure and child behaviour problems. Addiction. 2010;105(1):74-86. [DOI] [PubMed] [Google Scholar]
- 82.May PA, Marais AS, de Vries MM, et al. . The continuum of fetal alcohol spectrum disorders in a community in South Africa: Prevalence and characteristics in a fifth sample. Drug Alcohol Depend. 2016;168:274-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.May PA, de Vries MM, Marais AS, et al. . The continuum of fetal alcohol spectrum disorders in four rural communities in South Africa: prevalence and characteristics. Drug Alcohol Depend. 2016;159:207-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann. 2014;45(3):301-314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Floyd RL, Decouflé P, Hungerford DW. Alcohol use prior to pregnancy recognition. Am J Prev Med. 1999;17(2):101-107. [DOI] [PubMed] [Google Scholar]
- 86.Tough S, Tofflemire K, Clarke M, Newburn-Cook C. Do women change their drinking behaviors while trying to conceive? an opportunity for preconception counseling. Clin Med Res. 2006;4(2):97-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Keywords Used in the Comprehensive Systematic Literature Search
eTable 2. Diagnostic Breakdown of FASD in the Identified Studies
eTable 3. Critical Appraisal of the Identified Studies Reporting on the Prevalence of FASD Among Children and Youth in the General Population
eTable 4. Prevalence of FASD Among Children and Youth in the General Population by Country and WHO Region in 2012
eTable 5. Pooled Prevalence of FASD Among Children and Youth in the General Population and the Results of the Heterogeneity and Publication Bias Tests by Country and WHO Region
eTable 6. Comparison of the Prevalence of FASD Among Special Populations, Based on Select Studies, to the Global Prevalence Among Children and Youth in the General Population
eMethods. Estimation of the Quotient of the Average Number of Women Who Consumed Alcohol During Pregnancy per 1 Case of FASD
eFigure 1. Schematic Diagram Depicting the Search Strategy Used
eFigure 2. Forest Plot of the Prevalence of FASD Among Children and Youth in the General Population in Australia, Croatia, France, Italy, South Africa, and the United States