Abstract
Background
A marked increase in the number of cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection occurred in Jeddah, Saudi Arabia, in early 2014. We evaluated patients with MERS-CoV infection in Jeddah to explore reasons for this increase and to assess the epidemiologic and clinical features of this disease.
Methods
We identified all cases of laboratory-confirmed MERS-CoV infection in Jeddah that were reported to the Saudi Arabian Ministry of Health from January 1 through May 16, 2014. We conducted telephone interviews with symptomatic patients who were not health care personnel, and we reviewed hospital records. We identified patients who were reported as being asymptomatic and interviewed them regarding a history of symptoms in the month before testing. Descriptive analyses were performed.
Results
Of 255 patients with laboratory-confirmed MERS-CoV infection, 93 died (case fatality rate, 36.5%). The median age of all patients was 45 years (interquartile range, 30 to 59), and 174 patients (68.2%) were male. A total of 64 patients (25.1%) were reported to be asymptomatic. Of the 191 symptomatic patients, 40 (20.9%) were health care personnel. Among the 151 symptomatic patients who were not health care personnel, 112 (74.2%) had data that could be assessed, and 109 (97.3%) of these patients had had contact with a health care facility, a person with a confirmed case of MERS-CoV infection, or someone with severe respiratory illness in the 14 days before the onset of illness. The remaining 3 patients (2.7%) reported no such contacts. Of the 64 patients who had been reported as asymptomatic, 33 (52%) were interviewed, and 26 of these 33 (79%) reported at least one symptom that was consistent with a viral respiratory illness.
Conclusions
The majority of patients in the Jeddah MERS-CoV outbreak had contact with a health care facility, other patients, or both. This highlights the role of health care–associated transmission. (Supported by the Ministry of Health, Saudi Arabia, and by the U.S. Centers for Disease Control and Prevention.)
The Middle East respiratory syndrome coronavirus (MERS-CoV), an emerging novel betacoronavirus belonging to lineage C, is known to cause severe acute respiratory illness in humans. From the time the disease was first identified in 2012, mortality among patients with laboratory-confirmed infection has been reported to be approximately 30 to 40%.1,2 As of this writing, cases have been linked to seven countries in or near the Arabian Peninsula, and the majority of reported cases have been from Saudi Arabia.3,4
A zoonotic origin of MERS-CoV has been presumed on the basis of evidence to date. The reservoir, mechanism of transmission, and risk factors for transmission resulting in primary cases of infection remain elusive,5 although increasing evidence suggests that dromedary camels may be able to transmit the virus to humans through close contact.6-8 Infected camels may have mild, self-limited respiratory signs or inapparent infection.6,9 Primary cases of MERS-CoV infection that are probably associated with zoonotic exposures have been documented in community settings and can result in limited secondary transmission in households.10 Secondary transmission in health care settings, which also has been documented, has resulted in large outbreaks.11,12 Data on risk factors for transmission in households and health care settings are lacking.
Beginning in mid-March 2014, an increase in reported cases of MERS-CoV infection in Jeddah, Saudi Arabia, heightened international concern3,13 about the potential for global transmission of this virus.14 Amid intense speculation regarding the cause of the sudden increase in cases, several hypotheses emerged, including, either alone or in combination, genomic changes resulting in increased transmissibility of the virus, an unidentified seasonality component, an increase in testing to detect MERS-CoV infection, an increase in primary cases in the community as a result of changes in contacts between humans and potential animal reservoirs, an increase in cases because of sustained transmission in the community (unrelated to health care exposures), and health care–associated amplification. Subsequently, a laboratory-based study indicated that the outbreak was not associated with changes in the virus, and the investigators postulated a predominance of human-to-human transmission in Jeddah as an explanation.15
On May 10, 2014, the Saudi Arabian Ministry of Health, with assistance from the U.S. Centers for Disease Control and Prevention (CDC), began an investigation to determine the reasons for the increase in cases of MERS-CoV infection. Our primary objectives were to identify the cause of the increase in reported cases by characterizing the possible sources of exposure and to define the epidemiologic and clinical features of patients with the disease. Because data are lacking regarding asymptomatic patients with MERS-CoV infection, our secondary objective was to further characterize asymptomatic patients within our cohort.
Methods
Patients and Study Oversight
All patients from the Jeddah region who were reported to have laboratory-confirmed MERS-CoV infection between January 1 and May 16, 2014, were identified. In Saudi Arabia, before May 13, 2014, a person was considered to have a confirmed case of MERS-CoV infection if there was laboratory confirmation of MERS-CoV infection on the basis of a positive real-time reverse-tran-scriptase–polymerase-chain-reaction (RT-PCR) assay targeting two genes — the E gene and open-reading frame gene 1a. Persons with confirmed infection included reportedly asymptomatic persons who were identified by contact tracing, post-exposure screening of health care personnel, or both. The case definition was revised on May 13, 2014, after which a person with a confirmed case of MERS-CoV infection was defined as a person with laboratory confirmation as noted above and clinical or radiologic evidence consistent with the infection.16-18
In Saudi Arabia, real-time RT-PCR testing for MERS-CoV is performed at five Saudi Arabian Ministry of Health regional laboratories, one of which is located in Jeddah. In addition, at least three hospitals in Jeddah independently perform real-time RT-PCR testing for MERS-CoV in hospitalized patients with suspected infection.
We obtained a list of patients with laboratory-confirmed MERS-CoV cases from the Ministry of Health regional laboratory in Jeddah. We also obtained case information from the Communicable Diseases Control Department of the Ministry of Health in Riyadh, the Jeddah Health Affairs Directorate, and from local hospitals in Jeddah that were identified through these two aforementioned sources as having patients with laboratory-confirmed MERS-CoV infection.
Since this investigation was part of a public health response, it was not considered by the CDC and the Saudi Arabian Ministry of Health to be research that was subject to review by an institutional review board. Written informed consent was not required.
Possible Sources of Exposure
In order to identify possible sources of exposure among symptomatic patients, we first categorized all patients according to health status (symptomatic or asymptomatic) and employment status (health care personnel or not health care personnel) as coded by the Ministry of Health or admitting hospitals. We then attempted to contact the symptomatic patients who were not health care personnel at least four times by telephone. We obtained oral informed consent from these patients, and we conducted telephone interviews in Arabic or English. Proxies (i.e., the closest relative or friend) were interviewed if patients were deceased. Interviews were conducted from May 12 through June 9, 2014. Patients or their proxies were asked about demographic characteristics, occupation, underlying medical conditions, the clinical course of the infection, and exposure.
In addition, available hospital medical records were reviewed to characterize potential exposures and verify information obtained from telephone interviews. We categorized patients according to whether they had worked at, been admitted to, or visited a health care facility, as well as according to whether they reported contact with a patient with confirmed MERS-CoV infection or someone admitted to the hospital with severe respiratory illness of unknown cause during the 14 days before the onset of illness. These criteria addressed potential secondary exposures as specified in the revised World Health Organization (WHO) case–control protocol for assessment of potential risk factors for primary MERS-CoV infection.19
In patients in whom secondary exposures were identified, we did not collect information about primary exposure (e.g., contact with animals). The dates of onset of illness were extracted from hospital charts, telephone interviews, or Ministry of Health case lists. For patients in whom the date of onset of illness was unclear, we first used the date of onset of MERS-CoV–related symptoms.
Next, if that date was not available, we used the date of clinical deterioration (e.g., admission to an intensive care unit [ICU]), and finally, if neither of those dates were available, we used the date of testing for MERS-CoV. When information about exposure before the onset of illness was available, we characterized admissions to a health care facility according to the primary diagnosis and we characterized visits to a health care facility according to type (emergency or outpatient visit, or visits to hospitalized friends or family). Symptomatic patients who were not health care workers and who had none of the aforementioned exposures were considered to be potential primary cases.
Signs and Symptoms in Patients Reported to Have Been Asymptomatic
We conducted a telephone survey from May 26 through June 8, 2014, of patients who had been coded by the Ministry of Health and reported to the WHO as being asymptomatic. At least four attempts were made to contact patients with available telephone numbers. We obtained oral informed consent from these patients, and we conducted the telephone interviews in Arabic or English.
We sought to determine whether, in fact, any of the following signs or symptoms had been present during the 1 month before PCR testing to detect MERS-CoV (the period that was consistent with the presumed duration of viral shedding)20: cough, shortness of breath, rhinorrhea, sore throat, hemoptysis, fever, chills, muscle pain, abdominal pain, nausea, vomiting, diarrhea, rash, fatigue, chest pain, headache, night sweats, or other symptoms. The interview questions pertained to the patients’ demographic characteristics, occupation, and underlying medical conditions, as well as the clinical course of the infection, the reason for testing to detect MERS-CoV, and the history of defined symptoms. Patients were then characterized according to the presence or absence of symptoms and, among patients who were determined to have had symptoms, according to the type of symptoms.
Statistical Analysis
Descriptive analyses were performed for the following groups: all patients, all symptomatic patients who were not health care personnel, and asymptomatic patients. Results were reported as frequencies and proportions for categorical variables and as median values and interquartile ranges for continuous variables. In addition, the chi-square test, Fisher's exact test, and the F-test were used to compare prespecified subgroups of symptomatic patients (those who were not available for the assessment of potential exposure to MERS-CoV vs. those who were available for that assessment) and of asymptomatic patients (those who responded to the telephone survey vs. those who did not respond). A P value of less than 0.05 was considered to indicate statistical significance. All analyses were conducted with the use of SAS software, version 9.3 (SAS Institute).
Results
We identified 255 patients in Jeddah who had laboratory-confirmed MERS-CoV infection. The median age was 45 years (interquartile range, 30 to 59). A total of 174 patients (68.2%) were male, 78 (30.6%) were health care personnel, 140 (54.9%) were from Saudi Arabia, 93 (36.5%) were admitted to an ICU, and 93 died (case-fatality rate, 36.5%) (Table 1).
Table 1.
Characteristics of All Patients with Laboratory-Confirmed MERS-CoV Infection and of Symptomatic Patients Who Were Not Health Care Personnel.*
| Characteristic | All Patients with Laboratory-Confirmed Infection (N = 255) | Symptomatic Patients Who Were Not Health Care Personnel (N = 151) | |||
|---|---|---|---|---|---|
| All Patients (N = 151) | Data Not Assessed (N = 39) | Data Assessed (N = 112) | |||
| nonprimary case (N = 109) | Potential primary case (N = 3) | ||||
| Age — yr | |||||
| Median | 45 | 54 | 53 | 54 | 55 |
| Interquartile range† | 30-59 | 37-64 | 30-65 | 41-64 | 49-56 |
| Male sex — no. (%) | 174 (68) | 118 (78) | 33 (85) | 82 (75) | 3 (100) |
| Saudi Arabian — no. (%) | 140 (55) | 100 (66) | 27 (69) | 72 (66) | 1 (33) |
| Admission to intensive care unit — no. (%)‡ | 93 (36) | 78 (52) | 11 (28) | 66 (61) | 1 (33) |
| Died — no. (%) | 93 (36) | 89 (59) | 20 (51) | 68 (62) | 1 (33) |
| Asymptomatic — no. (%) | 64 (25) | NA | NA | NA | NA |
| Health care personnel — no. (%) | 78 (31) | NA | NA | NA | NA |
NA denotes not applicable.
The range for all patients was 3 months to 94 years, for patients with data that were not assessed 3 months to 90 years, for nonprimary cases 7 to 94 years, and for potential primary cases 49 to 56 years.
P<0.001 by the chi-square test for the comparison of the group of patients with data that were not assessed and the group of patients with data that were assessed.
Figure 1 shows an epidemic curve according to the date of onset of illness in symptomatic patients and according to the date of the test for MERS-CoV infection in asymptomatic patients. Of the 255 patients, 64 (25.1%) were reported to be asymptomatic, of whom 41 (64%) were health care personnel (Fig. 2). Of the 191 symptomatic patients, 40 (20.9%) were health care personnel. Among the 151 symptomatic patients who were not health care personnel, the median age was 54 years (interquartile range, 37 to 64), 118 (78.1%) were men, 100 (66.2%) were from Saudi Arabia, and 89 died (58.9%) (Table 1).
Figure 1. Laboratory-Confirmed Cases of MERS-CoV Infection.
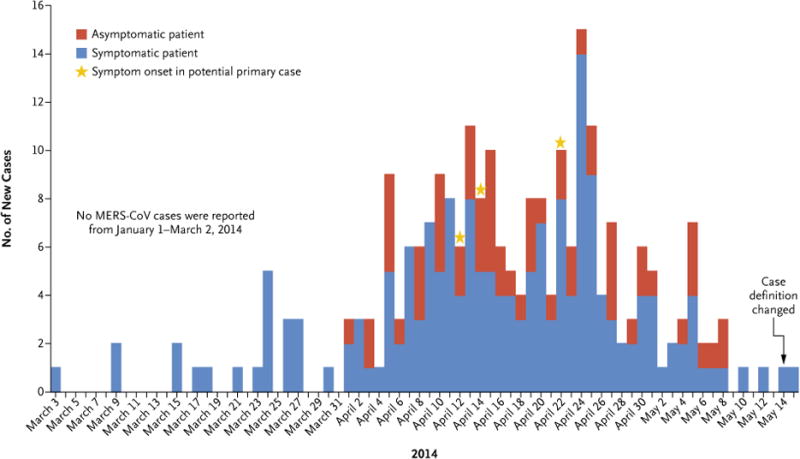
The date of onset of symptoms is shown for symptomatic patients, and the date of testing for MERS-CoV is shown for asymptomatic patients.
Figure 2. Characteristics of Patients with Confirmed MERS-CoV Infection.
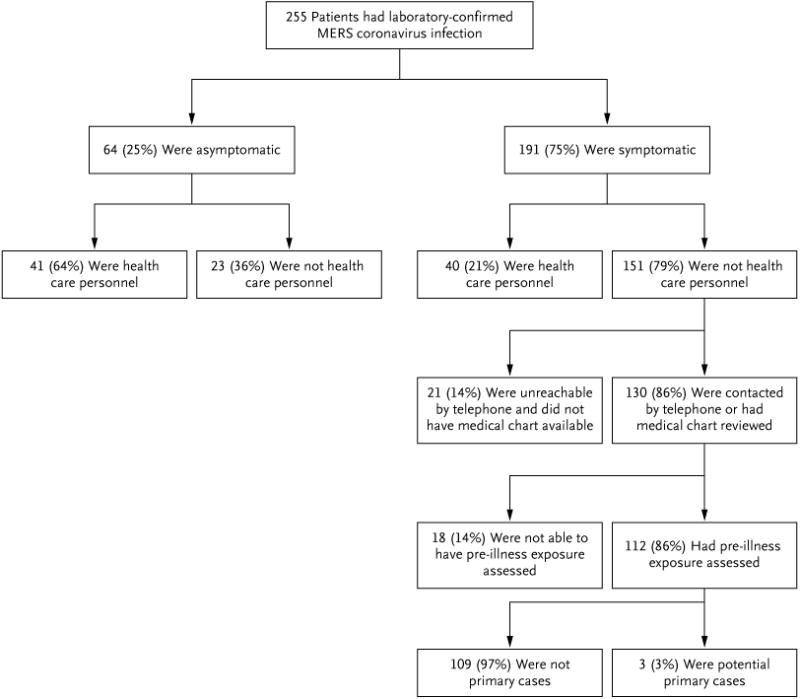
Of the 151 symptomatic patients who were not health care personnel, we obtained data on 130 (86.1%), by telephone interview (89 [58.9% ]), review of medical charts (122 [80.8% ]), or both (81 [53.6% ]). The inability to reach a patient by telephone was attributable to a lack of an available phone number or four unsuccessful calling attempts. Among the 130 symptomatic patients who were not health care personnel and who were called or had medical charts reviewed, exposures before the onset of illness could be assessed in 112 (86.2%). Exposures before the onset of illness were not assessed in 18 patients owing to insufficient medical history (Fig. 2). Patients who were contacted by telephone and for whom potential exposures were assessed were significantly more likely to have been admitted to an ICU than those for whom we could not assess exposure (P<0.001) (Table 1). Otherwise, the characteristics that were evaluated were similar in the two groups.
Of the 112 patients with data that could be assessed, 109 (97.3%) had one or more of the following types of secondary exposures during the 14 days before the onset of symptoms: admission to a health care facility (37 patients [33.9% ]), visits to a health care facility as a patient (68 patients [62.4% ]), contact with a patient who had confirmed MERS-CoV infection (22 patients [20.2% ]), or contact with someone with a severe respiratory illness of unknown cause (4 patients [3.7% ]) (Table 2). Only 3 of the 112 symptomatic patients who were not health care personnel (2.7%) reported no secondary exposures. Overall, 98 patients (87.5%) had exposure to a health care facility and 14 (12.5%) did not.
Table 2.
Types of Secondary Exposure to MERS-CoV in 109 Patients within 14 days before Onset of Symptoms.*
| Source of Exposure | No. of Patients (%) |
|---|---|
| Admission to a health care facility for treatment | 37 (34) |
| Cardiopulmonary disease† | 9 (8) |
| Surgery | 5 (5) |
| Gastrointestinal disease‡ | 4 (4) |
| Bloodstream infection | 3 (3) |
| Endocrine disease | 3 (3) |
| Neurologic disease | 3 (3) |
| Cancer or immunosuppression | 3 (3) |
| Skin and soft-tissue infection | 3 (3) |
| Renal disease | 2 (2) |
| Vascular disease | 2 (2) |
| Outpatient visit to a health care facility for treatment | 68 (62) |
| Emergency department | |
| Cardiovascular disease | 3 (3) |
| Gastrointestinal disease | 3 (3) |
| Trauma | 2 (2) |
| Outpatient facility | |
| Renal dialysis | 35 (32) |
| Endocrine disease | 2 (2) |
| Cancer | 2 (2) |
| Cardiovascular disease | 1 (1) |
| Prenatal visit | 1 (1) |
| General clinic visit | 1 (1) |
| Visit to a patient at a health care facility | 18 (17) |
| Potential case contact not related to exposure at a health care facility | 26 (24) |
| Contact with a patient with a confirmed MERS-CoV infection | 22 (20) |
| Contact with a person with a severe respiratory illness of unknown cause | 4 (4) |
Patients may have had more than one type of exposure. No secondary exposures were detected in 3 of 112 symptomatic patients who were not health care personnel (2.7%) and who had confirmed infection.
Admissions related to the cardiopulmonary system included congestive heart failure, chronic obstructive pulmonary disease, cardiomyopathy, myocardial infarction, mitral stenosis, chest pain, and hypotension.
Admissions related to the gastrointestinal system included intestinal hemorrhage, perforated intestine, hepatic encephalopathy, and anorexia.
Among the 68 visits to a health care facility during the 14 days preceding the onset of illness, 35 (51%) were related to renal dialysis. Eighteen patients visited family members or friends in a health care facility, and 11 of these patients reported that this visitation was their only health care–related exposure. Among the 37 admissions to a health care facility during the 14 days preceding the onset of illness, the median interval between admission and the onset of MERS-CoV symptoms was 11 days (interquartile range, 7 to 23).
Of the 64 patients who were originally identified as being asymptomatic, 33 (52%) were available for the telephone survey. There were no significant differences in demographic characteristics between the 33 patients who responded to the telephone survey and the 31 patients who did not respond. Table 3 lists the demographic characteristics of these patients, reasons for testing, and symptoms reported. Of note, 73% of the patients were health care personnel. Twenty-six of the 33 asymptomatic patients who were reached by telephone (79%) reported at least one symptom in the month before testing, and 23 (70%) reported more than one symptom. Unexpectedly, 12 of the 33 patients surveyed (36%) reported the presence of signs and symptoms as the reason for MERS-CoV testing, even though they had been identified as being asymptomatic (Table 3).
Table 3.
Demographic Characteristics, Reasons for Testing, and Signs and Symptoms Reported within 1 Month before Testing among 33 Patients Initially Reported as Being Asymptomatic.
| Characteristic | All Patients R (N = 33) | eported No Symptoms (N = 7) | Reported Symptoms (N = 26) |
|---|---|---|---|
| Demographic characteristics and medical history | |||
| Age — yr | |||
| Median | 35 | 29 | 36 |
| Interquartile range* | 27-51 | 28-37 | 26-52 |
| Male sex — no. (%) | 20 (61) | 2 (29) | 18 (69) |
| Saudi Arabian — no. (%) | 14 (42) | 3 (43) | 11 (42) |
| Health care personnel — no. (%) | 24 (73) | 6 (86) | 18 (69) |
| Underlying illness — no. (%) | 14 (42) | 1 (14) | 13 (50) |
| Reason for test — no. (%) | |||
| Contact investigation | 5 (15) | 3 (43) | 2 (8) |
| Screening of health care worker | 15 (45) | 4 (57) | 11 (46) |
| Presence of signs and symptoms | 12 (36) | 0 | 12 (46) |
| Signs and symptoms — no. (%) | |||
| Fever | 16 (48) | NA | 16 (62) |
| Cough | 13 (39) | NA | 13 (50) |
| Shortness of breath | 11 (33) | NA | 11 (42) |
| Fatigue | 9 (27) | NA | 9 (35) |
| Nausea and vomiting | 6 (18) | NA | 6 (23) |
| Rhinorrhea | 5 (15) | NA | 5 (19) |
| Sore throat | 5 (15) | NA | 5 (19) |
| Diarrhea | 4 (12) | NA | 4 (15) |
| Chills | 3 (9) | NA | 3 (12) |
| Muscle pain | 3 (9) | NA | 3 (12) |
| Headache | 3 (9) | NA | 3 (12) |
| Chest pain | 2 (6) | NA | 2 (8) |
| Loss of appetite | 2 (6) | NA | 2 (8) |
| Abdominal pain | 1 (3) | NA | 1 (4) |
| Conjunctivitis | 1 (3) | NA | 1 (4) |
| Night sweats | 1 (3) | NA | 1 (4) |
| Rash | 1 (3) | NA | 1 (4) |
| More than one sign or symptom | 23 (70) | NA | 23 (88) |
| Fever, cough, and shortness of breath | 7 (21) | NA | 7 (27) |
The range for all patients was 1 to 71 years, for patients who reported no symptoms 26 to 43 years, and for patients who reported symptoms 1 to 71 years.
Discussion
The outbreak of MERS-CoV infections in Jeddah raised international concern and led to widespread speculation regarding possible causes. We found that the marked increase in the number of patients with MERS-CoV infection in Jeddah could be explained by secondary human-to-human transmission and amplification in health care facilities, rather than by a sudden increase in primary cases in the community. We determined that the vast majority of patients with reported MERS-CoV infection in the Jeddah region from January 1 through May 16, 2014, had potential exposure to other patients with MERS-CoV infection, mostly in health care settings. We could not identify these exposures in 3 of 112 symptomatic patients who were not health care personnel (2.7%) and who had data that could be assessed. Efforts to identify risk factors for community transmission, including exposure to animals, are ongoing in Saudi Arabia and were not part of this investigation. We provide a further description of reportedly asymptomatic MERS-CoV patients, the majority of whom were health care personnel in clinical settings. We were able to elicit a history of symptoms in a majority of patients, and a substantial proportion reported the presence of symptoms as the reason for testing for MERS-CoV infection. These findings warrant further investigation.
Our study had several limitations. On the basis of the epidemiology of MERS-CoV to date, we considered the risk of MERS-CoV transmission to be higher in health care facilities than in the community. We thus designated cases as being potentially health care–associated if we could document an exposure to a health care setting or a patient with MERS-CoV infection during the 14 days before the onset of illness.19 Given this, it is possible that among patients with frequent visits to health care facilities, some cases that we designated as health care–associated could have been primary cases. In addition, because MERS-CoV testing is ordered at the discretion of the treating health care personnel, the decision to test could be biased toward certain features such as access to health care, demographic characteristics, or underlying disease. Second, for patients in whom the onset of illness was unclear, we used the date of MERS-CoV testing, the date of clinical deterioration (e.g., admission to an ICU), or the date of onset of MERS-CoV–related symptoms. Although the onset of illness was unclear in a small number of patients, these patients had frequent health care–related exposures that could have provided multiple opportunities for MERS-CoV transmission.
Third, some symptomatic patients were not reached by telephone, although assessed variables indicated that these patients were similar to those who were reached (Table 1). In addition, although medical histories were supplemented by hospital chart review in most cases, poor recall may have limited the accuracy of some responses. Fourth, asymptomatic patients were identified through a variety of methods (e.g., investigation of contacts and screening of health care workers) and not through routine surveillance. Among health care personnel, the decision to seek testing may have been influenced by knowledge or perception of high-risk exposures. However, because we restricted our analysis of secondary exposures to persons who were not health care personnel, this is unlikely to have affected our results. Finally, no controls were enrolled for comparison with cases; therefore, we could not assess the frequency of respiratory symptoms or exposure to health care facilities in this population.
The large proportion of reported cases associated with exposure to health care facilities highlights the importance of implementation of infection-control practices to limit transmission. Our results show a wide range of clinical presentations associated with MERS-CoV in various locations within health care facilities. These findings underscore the need to strengthen infection prevention and control practices throughout health care facilities, including early recognition and care of patients who are potentially infected with MERS-CoV and who present with mild disease. Saudi Arabia has recently revised its Ministry of Health MERS-CoV surveillance case definitions and infection-control guidance.18 This revision has been accompanied by intensive efforts to improve case detection, testing, and reporting. Efforts are ongoing to strengthen infection-control practices throughout Saudi Arabia.
Acknowledgments
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Supported by the Ministry of Health, Saudi Arabia, and the U.S. Centers for Disease Control and Prevention.
We thank the following persons who assisted with identifying patients, abstracting medical records, and reporting case data: Ministry of Health, Saudi Arabia: Dr. Banan M. Alamoudi, Dr. Ghadi F. Subahi, Dr. Maram Al Mohammadi, Dr. Mohammed S. Kutbi, Dr. Omima Shabouni, Dr. Ziad Bin-Saad, and Nahed Batarfi; King Fahd General Hospital: Dr. Imad A. Al-Jahdali, Dr. Mohammed A. Garout, Dr. Areej Bin-Sadiq, Dr. Kholoud Alsulaimani, Dr. Reham M. Gandeh, and Arwa A. Sebaih; King Faisal Specialist Hospital: Dr. Bakr Bin-Sadiq, Ms. Hanadi S. Al-Salmi, and Richard Sanvictores; King Abdulaziz General Hospital: Dr. Mohammad F. Al-Mobarak and Dr. Aisha Mutwalli; King Abdulaziz University Hospital: Dr. Nabeela A. Al-Abdullah and Dr. Anees Sindi; King Saud Hospital: Dr. Batool M.S. Ali and Dr. Dalya M. Atallah; Erfan Hospital: Dr. Azza Khattab; United Doctors Hospital: Dr. Nuha Mirza; Saudi German Hospital: Dr. Khaled Batterjee, Dr. Wael Alganaini, Dr. Jehan Ibrahim, Sally Barr, and Mostafa Nasar; International Medical Center: Dr. Mujahed Abbas and Dr. Raya Jabar; Fakeeh Hospital: Dr. Samar A. Badreddine; National Guard Hospital: Dr. Abdulhakeem Al-Thaqafi; Bakhsh Hospital: Suseela Koruthu; Al-Jedani Hospital: Dr. Ibrahim Hassan and Sally Diwa; Centers for Disease Control and Prevention: Dr. Rima Khabbaz, Dr. John Jernigan, Dr. Allison Arwady, Dr. Colin Basler, Dr. Andrew Geller, Dr. Concepcion Estivariz, and Dr. Glen Abedi. We also thank Miss Fadwa Mushtag for assistance with preparation of an earlier version of the manuscript.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.The WHO MERS-CoV Research Group. State of knowledge and data gaps of Middle East respiratory syndrome coronavirus (MERS-CoV) in humans. PLOS Currents Outbreaks. 2013 doi: 10.1371/currents.outbreaks.0bf719e352e7478f8ad85fa30127ddb8. ( http://currents.plos.org/outbreaks/article/state-of-knowledge-and-data-gaps-of-middle-east-respiratory-syndrome-coronavirus-mers-cov-in-humans-2) [DOI] [PMC free article] [PubMed]
- 2.Middle East respiratory syndrome coronavirus (MERS-CoV) — update. World Health Organization; Jun 11, 2014. ( http://www.who.int/csr/don/2014_06_11_mers/en) [Google Scholar]
- 3.Middle East respiratory syndrome coronavirus (MERS-CoV) summary and literature update — as of 9 May 2014. World Health Organization; 2014. ( http://www.who.int/csr/disease/coronavirus_infections/MERS_CoV_Update_09_May_2014pdf?ua=1) [Google Scholar]
- 4.Middle East respiratory syndrome coronavirus (MERS-CoV) summary and literature update — as of 11 June 2014. World Health Organization; 2014. ( http://www.who.int/csr/disease/coronavirus_infections/MERS-CoV_summary_update_20140611.pdf) [Google Scholar]
- 5.WHO risk assessment: Middle East respiratory syndrome coronavirus. World Health Organization; Apr 24, 2014. ( http://www.who.int/csr/disease/coronavirus_infections/MERS_CoV_RA_20140424.pdf?ua=1) [Google Scholar]
- 6.Azhar EI, El-Kafrawy SA, Farraj SA, et al. Evidence for camel-to-human transmission of MERS coronavirus. N Engl J Med. 2014;370:2499–505. doi: 10.1056/NEJMoa1401505. [DOI] [PubMed] [Google Scholar]
- 7.Haagmans BL, Al Dhahiry SH, Re-usken CB, et al. Middle East respiratory syndrome coronavirus in dromedary camels: an outbreak investigation. Lancet Infect Dis. 2014;14:140–5. doi: 10.1016/S1473-3099(13)70690-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Update on MERS-CoV transmission from animals to humans, and interim recommendations for at-risk groups. World Health Organization; Jun 13, 2014. ( http://www.who.int/csr/disease/coronavirus_infections/MERS_CoV_RA_20140613.pdf) [Google Scholar]
- 9.Middle East respiratory syndrome coronavirus summary and literature update — as of 27 March 2014. World Health Organization; 2014. ( http://www.who.int/csr/disease/coronavirus_infections/MERS_CoV_Update_27_March_2014.pdf?ua=1) [Google Scholar]
- 10.Memish ZA, Zumla AI, Al-Hakeem RF, Al-Rabeeah AA, Stephens GM. Family cluster of Middle East respiratory syndrome coronavirus infections. N Engl J Med. 2013;368:2487–94. doi: 10.1056/NEJMoa1303729. [DOI] [PubMed] [Google Scholar]
- 11.Assiri A, McGeer A, Perl TM, et al. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med. 2013;369:4, 07–16. doi: 10.1056/NEJMoa1306742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Abdallat MM, Payne DC, Alqasrawi S, et al. Hospital-associated outbreak of Middle East respiratory syndrome corona-virus: a serologic, epidemiologic, and clinical description. Clin Infect Dis. 2014;59:1225–33. doi: 10.1093/cid/ciu359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gulland A. WHO voices concern over rising numbers of MERS-CoV cases. BMJ. 2014;348:g2968. doi: 10.1136/bmj.g2968. [DOI] [PubMed] [Google Scholar]
- 14.Soaring MERS cases cause pandemic jitters, but causes are unclear. Science Insider. 2014 ( http://news.sciencemag.org/health/2014/04/soaring-mers-cases-cause-pandemic-jitters-causes-are-unclear)
- 15.Drosten C, Muth D, Corman VM, et al. An observational, laboratory-based study of outbreaks of Middle East respiratory syndrome coronavirus in Jeddah and Riyadh, Kindom of Saudi Arabia. Clin Infect Dis. 2015;60:369–77. doi: 10.1093/cid/ciu812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Madani TA, Althaqafi AO, Alraddadi BM. Infect ion prevent ion and control guidelines for patients with Middle East respiratory syndrome coronavirus (MERS-CoV) infection. Saudi Med J. 2014;35:897–913. [PubMed] [Google Scholar]
- 17.Madani TA. Case definition and management of patients with MERS coronavirus in Saudi Arabia. Lancet Infect Dis. 2014;14:911–3. doi: 10.1016/S1473-3099(14)70918-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Case definition and surveillance guidance for MERS-CoV testing in Saudi Arabia. Kingdom of Saudi Arabia Ministry of Health. 2014 May 13; ( http://www.moh.gov.sa/en/CoronaNew/Regulations/MoHCaseDefinitionMERSCoVVersionMay132014.pdf)
- 19.Case-control study to assess potential risk factors related to human illness caused by Middle East respiratory syndrome coronavirus (MERS-CoV) World Health Organization; Jul 15, 2014. ( http://www.who.int/csr/disease/coronavirusinfections/MERSCoVCaseControlStudyofExposures.pdf?ua=1) [Google Scholar]
- 20.Poissy J, Goffard A, Parmentier-Decrucq E, et al. Kinetics and pattern of viral excretion in biological specimens of two MERS-CoV cases. J Clin Virol. 2014;61:275–8. doi: 10.1016/j.jcv.2014.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


