Abstract
Adolescents with psychiatric disorders appear to be at increased risk for acquiring HIV and other sexually transmitted infections; however, little is known about the prevalence of behavioral risk factors in this population. This meta-analysis aimed to assess the prevalence of alcohol use and sexual risk behaviors among adolescents with psychiatric disorders. Electronic database searches identified studies sampling adolescents diagnosed with psychiatric disorders and assessing both alcohol and sexual risk behaviors. Fourteen studies sampling 3,029 adolescents with psychiatric disorders were included. The majority of adolescents with psychiatric disorders report alcohol use and sexual risk behaviors. Risk reduction interventions targeting these two behaviors are needed.
Keywords: adolescents, psychiatric disorders, alcohol, sexual behaviors, meta-analysis
Adolescents account for 50% of all newly diagnosed STIs, although they only account for 25% of the sexually active population (Centers for Disease Control and Prevention, 2016). Factors that place adolescents at greater risk of STIs include an early sexual debut, inconsistent use of condoms, and the use of alcohol or drugs before sex (Centers for Disease Control and Prevention, 2016). Although adolescents’ as a whole are at risk, specific subpopulations are particularly vulnerable. Recent research has highlighted that adolescents living with psychiatric disorders (PD) may be a uniquely vulnerable group for engaging in sexual risk behaviors and subsequent negative consequences (Brown, Danovsky, Lourie, DiClemente, & Ponton, 1997).
Approximately one in five adolescents living in the United States will experience a PD, and the rates of PD are increasing with the majority experiencing an anxiety (e.g., generalized anxiety) or behavioral disorder (e.g., oppositional defiant), followed by a mood (e.g., major depression) or substance use disorder (e.g., alcohol dependence; Merikangas et al., 2010). Growing evidence suggests that adolescents living with a PD—specifically those with mood or behavioral disorders—are at increased risk for engaging in sexual risk behaviors including unprotected sex, having multiple sex partners, and early onset of sex (Booth & Zhang, 1997; Shrier, Walls, Lops, Kendall, & Blood, 2012). The social and cognitive vulnerabilities that result from PD may influence the uptake of sexual risk behaviors (Donenberg et al., 2012; Reyna & Farley, 2006; Scott-Sheldon & Johnson, 2013); however, other behavioral factors such as co-occurring alcohol use might also contribute to this group’s increased risk.
Alcohol has been shown to be a prominent risk factor for sexual risk behaviors among several groups, including adolescents (Deas, 2006). Alcohol myopia theory—a primary theory accounting for this association—posits that alcohol use facilitates social interactions and behavioral disinhibition, thus increasing the likelihood of sexual activity and risk (Patrick, Maggs, & Lefkowitz, 2015; Steele & Josephs, 1990). Adolescents with a PD who consume alcohol appear even more likely to engage in sexual behavior. This increased likelihood of sexual activity may be due to the influence of alcohol compounding self-regulatory difficulties commonly found in individuals with PD (Brown, Danovsky, et al., 1997; Reyna & Farley, 2006; Smith, 2001). In addition, unique factors associated with treatment and severity of PD (e.g., treatment settings) and common factors (e.g., gender) may also influence prevalence and impact of these behaviors.
Taken together, the global alcohol-sexual risk behavior association is a common finding in the literature; however, subgroup differences may result in differing strength of this association (Shuper et al., 2010). Research findings suggest that adolescents living with PD are at increased risk for alcohol use, sexual risk behaviors, and STIs; however, a full examination of the prevalence of alcohol use, sexual risk behaviors, and STI/HIV among adolescents with a PD and the association among these factors has not been fully explored. Previous reviews have identified adolescents with PD as vulnerable to engaging in sexual risk behavior (Brown, Danovsky, et al., 1997; Donenberg, 2005), but these reviews have (a) broadly focused on HIV risks and (b) used narrative reviewing methods rather than meta-analytic methodology. Furthermore, these reviews are now dated and will benefit from the increase in the size and quality of the empirical literature. As such, the aims of the current review are to (1) assess the prevalence of alcohol use and sexual risk behaviors among adolescents with clinically diagnosed PD, (2) examine factors associated with the prevalence of alcohol and sexual risk behaviors across studies, and (3) evaluate the strength of the alcohol-risky sex association. In order to assess both prevalence and strength of the alcohol- sexual risk behavior association we conducted a meta-analytic review of the literature assessing both alcohol use and sexual risk behaviors among adolescents (age 10 to 19) with clinically diagnosed PD.
METHODS
The systematic review and meta-analysis was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses ([PRISMA]; Moher, Liberati, Tetzlaff, & Altman, 2009).
Information Sources and Search Strategy
Studies were retrieved from electronic bibliographic databases (PsycINFO, PubMed, ERIC, The Cochrane Library, CINAHL, Web of Science, Global Health, ProQuest Dissertation & Theses, and CORK) using a Boolean search strategy. The search string was developed with the assistance of a medical librarian. The searches consisted of these broad search terms: alcohol use, sex, HIV, STI, and PD. Search terms were modified using guidelines specified for each database searched. For example, the following search terms were used in PubMed: (binge drinking OR (binge AND (alcohol OR ethanol)) OR alcohol drinking OR alcohol abuse OR alcoholic OR alcohol OR “alcohol-related disorders”[MeSH] OR alcoholism OR intoxicat* OR drunk*) AND (“sexually transmitted diseases”[Mesh] OR “sexually transmitted” [tiab] OR STI OR STD OR AIDS[sb] OR condom OR unsafe sex OR sexual behavior OR (risk OR risk taking OR risk factor*) AND (sex OR sexu* OR sexual behavior)) AND (“mental illness” or “severe mental illness” or “mentally ill” or “psychiatric disorders” or “severely mentally ill”). No age or language restrictions were imposed. Relevant studies were also located by reviewing reference sections of relevant reviews and included studies. The search was finalized in February 2015 to ensure the inclusion of all studies available through December 2014.
Eligibility Criteria and Selection of Studies
Studies were included if the study sampled (a) adolescents (ages 10 to 19) diagnosed with a PD, defined as a mental health problem that has a substantial impact on an individual’s ability to function socially, academically, and emotionally (Heger et al., 2014; Merikangas et al., 2010), (b) assessed alcohol use, and (c) assessed sexual risk behaviors (e.g., sexual activity, condom use, number of partners). Our search identified 2,540 reports. Records (2,303) were excluded because they did not meet the inclusion criteria and, in one case, because we did not have the expertise to translate the study (Tabrizi, Vatankhah, & Tabrizi, 2009). Of the remaining 237 studies, 188 were excluded because they sampled adults. The remaining 14 studies (and 35 supplemental manuscripts) sampled adolescents with PD and were included in this meta-analysis (Figure 1).
Figure 1.
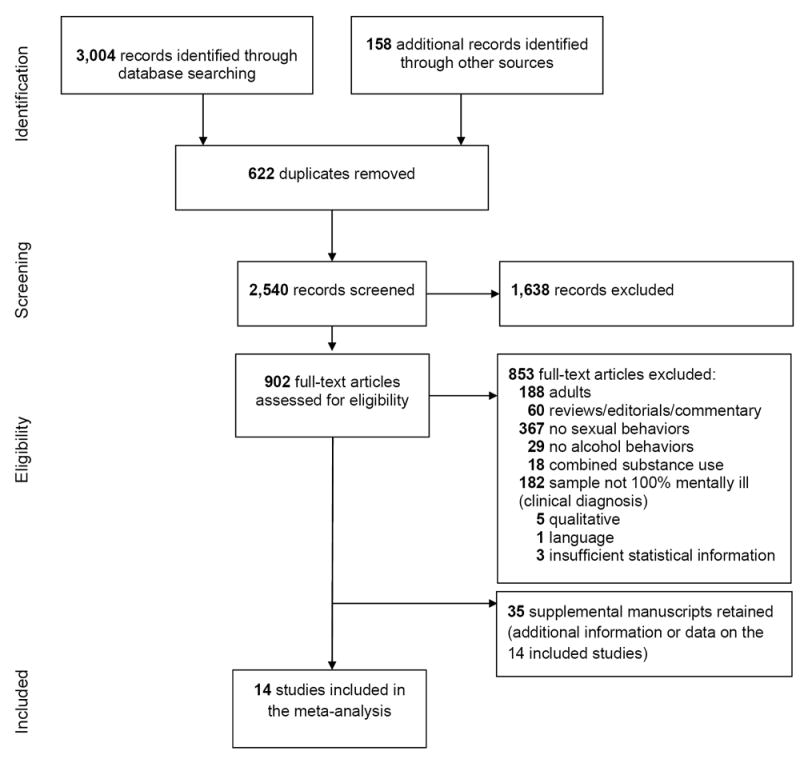
Selection Process for Study Inclusion in the Meta-Analysis
Coding and Reliability
Two trained coders extracted study information (e.g., publication year), sample characteristics (e.g., sex, ethnicity, age), risk characteristics (e.g., age at sexual debut, alcohol use), and mental health information (e.g., clinically diagnosed disorders, treatment setting). Methodological quality of the individual studies was assessed using items (e.g., appropriateness of study design, sampling method) adapted from validated measures (Downs & Black, 1998; Fowkes & Fulton, 1991; Miller et al., 1995). The mean percent agreement between coders was 76% (mean kappa = 0.48) for categorical variables and for continuous variables, the mean interclass correlation was 0.85, signifying moderate coding agreement. Coding discrepancies between the two independent coders were resolved through discussion and, due to the moderate reliability; a further review of the manuscript content was conducted with a code reviewer and the principal investigator of the project.
Study Outcomes
Outcomes included the prevalence of alcohol use, sexual activity, and sexual risk behaviors. Alcohol use included lifetime and current (i.e., prior 6 months) alcohol use and alcohol abuse and/or dependence. Sexual activity included ever or recently (i.e. prior 6 months) sexually active. Sexual risk behaviors included (a) multiple partners (e.g., ≥ 2 partners), (b) ever used a condom use, (c) consistent condom use, (d) condom use during the last sexual encounter, and (e) history of a STI.
Effect Size Calculations
Prevalence estimates (proportions) for alcohol use, sexual activity, and sexual risk behaviors were extracted from each study by two independent coders. Proportions represent the number of study participants out of the total number of study participants or the total number of sexually active participants for sexual risk behaviors who engaged in alcohol use, sexual activity, and sexual risk-taking. For studies with longitudinal or intervention designs, the prevalence was estimated from the baseline data. The analyses used were conducted using logits.
Data Analyses
The overall weighted mean (logits) effect size (and 95% confidence intervals), using random-effects assumptions, were calculated for each outcome. The homogeneity statistic, Q, was also computed to determine whether the effect sizes (logits) estimated a common population mean. We quantified the inconsistency across studies using the I2 index and 95% confidence interval (Higgins & Thompson, 2002; Huedo-Medina, Sanchez-Meca, Marin-Martinez, & Botella, 2006). The I2 index is the proportion of variability in the weighted mean (logits) effect sizes due to heterogeneity vs. sampling error. The weighted mean (logits) effect sizes were transformed back to prevalence estimates (proportions) to ease interpretation of the findings.
Predictor Analyses
Meta-regression analyses, using random-effects assumptions, were conducted to assess the effects of the hypothesized predictors of alcohol use, sexual risk behaviors, and STIs. Given the variability in the specificity of diagnoses reported across studies, broader diagnostic categories (e.g., mood disorders) were used in analyses. Predictors included the proportion of participants out of the total number diagnosed with a mood disorder and attention-deficit and disruptive disorders (e.g., ADHD, conduct disorder). Additional predictors included gender, mean age, ethnicity and setting. Analyses for continuous predictors (i.e., proportion female, mean age, proportion White, proportion diagnosed with a mood disorder or attention-deficit and disruptive disorders) and categorical moderators (setting: 1 = inpatient, 0 = outpatient) were conducted using published macros (Harbord & Higgins, 2008; Lipsey & Wilson, 2001). Meta-regression was also used to test the association beween alcohol use, sexual risk behaviors and STIs. Meta-regression analyses were only completed using outcomes with sufficient studies (i.e., > 5).
RESULTS
Table 1 provides a description of the 14 studies. Details regarding the study characteristics, methodological quality, and sample are summarized below.
Table 1.
Description of the 14 Studies Included in the Systematic Review and Meta-Analysis
| Citation | Sample | Setting | Alcohol Use | Sexual Behaviors | Diagnostic Tool and Psychiatric Diagnosis |
|---|---|---|---|---|---|
|
| |||||
| Abrantes et al. (2006)† | N = 239; 61% F; 94% White; Mage = 15 | Inpatient psychiatric hospital; Providence, RI | 50% CD | 67% sexually active (lifetime) | C-DISC:54% anxiety disorders; 45% mood disorders; ≥44% attention-deficit and disruptive behavior disorders |
| 42% AA/D | 52% sexually active (recent) | ||||
| 50% condom use (last event) | |||||
| 45% multiple partners (past 3M) | |||||
| 29% ≥4 partners (lifetime) | |||||
|
| |||||
| Aruffo et al. (1994)† | N = 100; 44% F; 71% White; Mage = 15 | Inpatient psychiatric hospital; Little Rock, AR | 64% CD | 79% sexually active (lifetime) | Medical Chart/Record:100% emotional and behavioral problems (unspecified) |
| 44% condom use (lifetime) | |||||
| 47% condom use (last event) | |||||
|
| |||||
| Bodison (1998) | N = 170 [89]; 30% F; 69% White, Mage = 15 | Partial hospital day treatment programs; PA and MD | 72% LD | 58% sexually active (recent) | Medical Chart/Record: 3% anxiety disorders; 48% mood disorders; 32% attention-deficit and disruptive behavior disorders; 1% psychotic disorders |
| Psychiatric disorder subsample only (n = 89) | 30% ≥2 partners (past 6M) | ||||
|
| |||||
| Brawner et al. (2012) | N = 131 [64]; 100% F; 100% Black, American; Mage = 16 | Outpatient mental health treatment programs; USA | 16% CD | 78% sexually active (lifetime) | PHQ- 9: 100% mood disorders |
| Clinically depressed subsample only (n = 64) | 73% LD | 50% condom use (last event) | |||
|
| |||||
| Brown et al. (2014)† | N = 893; 56% F; 67% Black, non-African; Mage = 15 | Outpatient mental health treatment; Atlanta, GA; Chicago, IL; Providence, RI | 22% CD | 55% sexually active (lifetime) | DISC:34% anxiety disorders; 32% mood disorders; 66% attention-deficit and disruptive behavior disorders |
| 31% sexually active (recent) | |||||
| 71% condom use (last event) | |||||
| 42%≥2 partners (past 90 days) | |||||
| 15%≥4 partners (past 90 days) | |||||
|
| |||||
| Brown et al. (1997) | N = 102; 63% F; 93% White; Mage = 15 | Inpatient psychiatric unit; Providence, RI | 29% CD | 71% sexually active (lifetime) | Medical Chart/Record:51% mood disorders; 13% attention-deficit and disruptive behavior disorders |
| 55% sexually active (recent) | |||||
| 33% condom use (past 6M) | |||||
| 27% ≥5 partners (past 12M) | |||||
|
| |||||
| Brown et al. (2000)† | N = 307; 40% F; 83% White; Mage = 15 | Psychiatric day schools and residential programs; Providence, RI | 74% LD | 68% sexually active (lifetime) | Admission intake record: |
| 80% condom use (12M) | 8% anxiety disorders | ||||
| 43% consistent condom use | 33% mood disorders | ||||
| 59% ≥2 partners (past 12M) | 7% attention-deficit and disruptive behavior disorders | ||||
| 3% psychotic disorders | |||||
|
| |||||
| Brown &Reynolds (1997) | N = 24; 54% F; 89% White; Mage = 14 | Inpatient psychiatric unit; Providence, RI | 23% CD | 75% sexually active (lifetime) | Medical Chart/Record: |
| 45% condom use (lifetime) | 9% anxiety disorder | ||||
| 51% mood disorders | |||||
| 9% attention-deficit and disruptive behavior disorders | |||||
|
| |||||
| Bryant et al. (1995)† | N = 83; 30% F; 58% White; Mage = 16 | State continuum of care program; Columbia, SC | 30% CD | 79% sexually active (lifetime) | Medical Chart/Record:100% severely emotionally disturbed (i.e., anxiety, mood, attention-deficit and disruptive behavior, or psychotic disorders) |
| 7% condom use (last event) | |||||
| 18% ≥4 partners (lifetime) | |||||
|
| |||||
| Cropsey et al. (2008)† | N = 636; 51% F; 58% White; Mage = 15 | Inpatient psychiatric units; VA | 55% LD | 46% sexually active (lifetime) | Medical Chart/Record:26% anxiety disorders; 73% mood disorders; 40% attention-deficit and disruptive behavior disorders; 4% psychotic disorders; 22% personality disorders |
| 12% AA/D | |||||
|
| |||||
| Deas et al. (2000) | N = 51; 33% F; 75% White; Mage = 16 | Inpatient substance abuse program; Charleston, SC | 27% AD | sexual risk composite:
|
KSADS:27% anxiety disorders; 68% mood disorders; 79% attention-deficit and disruptive behavior disorders |
| 25% AA | |||||
|
| |||||
| Donenberg et al. (2011)† | N = 218; 100% F; 100% Black, American; Mage = 14 | Outpatient mental health clinicsa; Chicago, IL | 33% CD | 32% sexually active (lifetime) | DISC: 5% anxiety disorders; 4% mood disorders; 11% attention-deficit and disruptive behavior disorders |
| 65% condom use (last event) | |||||
| 57% consistent condom use | |||||
| 24% ≥2 partners (past 6M) | |||||
|
| |||||
| Riggs et al. (2007)† | N = 106; 33% F; 48% White, Mage = 17 | Community and juvenile and social agencies; Denver, CO | ≥ 53% LD | 94% sexually active (lifetime) | Semi-structured diagnostic interview administered by study physician:100% mood disorders; 100% attention-deficit and disruptive behavior disorders |
| 53% ADb | 30% consistent condom use | ||||
| 13% AAb | |||||
|
| |||||
| Teplin et al. (2005)† | N = 1,829 [117]; 36% F; 55% Black, American; Mage = 15 | Juvenile detention center; Chicago, IL | 57% CDc | 88% sexually active (lifetime) | DISC:100% mood or psychotic disorders |
| Psychiatric disorder subsampleonly with or without a substance use disorder (n = 117) | 89% LDc | 46% condom use (past 1M) | |||
| 29% AA/Dbc | 51% ≥2 partners (past 3M) | ||||
| 23% ≥4 partners (past 3M) | |||||
Note. If studies included clinical and non-clinical populations, only the clinical samples are reported in this meta-analysis. F, female; CD, current drinkers; LD, lifetime drinkers; AA, alcohol abuse; AD, alcohol dependence; AA/D, alcohol abuse/dependence; M, month; NR, not reported; C-DISC, Columbia-Diagnostic Interview Schedule for Children (Costello, Edelbrock, Dulcan, Kalas, & Klaric, 1984); PHQ-9, The Patient Health Questionnaire (Kroenke & Spitzer, 2002); DISC, Diagnostic Interview Schedule for Children (Schwab-Stone et al., 1996); KSADS, Child Schedule for Affective Disorders and Schizophrenia (Kaufman et al., 1997).
Participants were recruited from inpatient and outpatient mental health clinics but were outpatients at the time of the study.
Participants were selected if they had a substance use disorder; excluded from AA/AD analyses.
Information drawn from the sample who received the HIV/AIDS survey (N = 689) because this information was not reported separately for the subsample who had a a psychiatric disorder (n = 117).
Details of the study were obtained from the primary paper and linked papers (see References).
Study Characteristics
Thirteen of the 14 studies were published in peer-reviewed journals (93%) between 1994 and 2014; data collection occurred between 1989 and 2008. Most studies (79%) were supported by a federal grant. All studies were conducted in the U. S.: northeast (4), south (4), midwest (2), west (1), and multiple regions (3). Samples were primarily recruited through clinical settings (86%; 43% inpatient, 36% outpatient, 7% both). One study recruited from community and juvenile and social agencies and another recruited from a juvenile detention facility. Psychiatric diagnoses were based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 1994, [8 studies]) or the DSM-III Revised (American Psychiatric Association, 1987, [2 studies]); four studies did not report this information. An intervention was evaluated in five of the 14 studies; three assessed a behavioral risk reduction intervention compared to a control condition, one included a single-group pilot behavioral intervention, and one assessed the effects of fluoxetine hydrochloride with or without cognitive behavioral therapy for major depressive, conduct, and substance use disorders. Only the baseline data from these studies were used in the analysis.
Methodological Quality
The methodological quality for the studies was assessed using 8 items derived from validated methodological quality rating scales (Downs & Black, 1998; Fowkes & Fulton, 1991; Miller et al., 1995). Studies satisfied an average of 66% (SD = 0.11) of the methodological quality criteria, indicating moderate to strong methodological quality. All studies described the objective of the study and used a design (e.g., cross-sectional surveys, randomized controlled trial) that was appropriate for the stated objective. We were unable to determine if the samples recruited for the study were representative of the population in 12 of the 14 studies or if a random sample of participants was selected in 13 of the 14 studies. Objective measures were used in four of the 14 studies; all studies used accurate (i.e., reliable and valid) self-report measures. All studies used statistical methods that were appropriate for their design.
Sample Characteristics
Only adolescents (N = 3,029) with a diagnosed PD were included in the analyses. Study samples were on average 53% female with a mean age of 15 years (SD = 0.75; range = 14 to 17); predominately White (56%) or non-African Black (41%; k = 11) with 8% identified as Latino/Latina (k = 10). The remaining participants were Asian (2%), Pacific Islander (2%), and American Indian (1%). Most adolescents were sexually active (69%), and of the four studies reporting age at sexual debut, adolescents were on average 14 years of age (SD = 0.42) at the time of their first sexual encounter. Of the two studies reporting sexual orientation, 92% and 3% of adolescents self-identified as heterosexual and bisexual, respectively.
Psychiatric Diagnoses of the Samples
Of the samples for which psychiatric diagnosis data were provided, 21% had some type of anxiety disorder (e.g., 10% PTSD), 55% had some type of mood disorder (e.g., 52% major depressive disorder; 2% bipolar disorder), 40% had some type of attention deficit or disruptive behavior disorder (e.g., 32% conduct disorder, 26% ADHD), and 3% had some type of psychotic disorder. A single study reported that 22% of their sample was diagnosed with a personality disorder (Cropsey, Weaver, & Dupre, 2008). Three studies reported that 100% of their samples had emotional and behavioral problems (Aruffo, Gottlieb, Webb, & Neville, 1994), severe emotional disturbance (Bryant, Garrison, Valois, Rivard, & Hinkle, 1995), or mood and/or psychotic disorders (Teplin et al., 2005). For studies that allowed participants to carry multiple diagnoses, each diagnosis was counted separately in totals.
Prevalence of Alcohol Use, Sexual Risk Behaviors, and STIs
The weighted mean prevalence estimates of alcohol use, sexual risk behaviors, and STIs among adolescents with a PD are found in Table 2. Most adolescents reported lifetime alcohol use (78%; 95% CI = 35, 96), and many were current users (36%; 95% CI = 19, 58). On average, 24% also met criteria for alcohol abuse and/or dependence (95% CI = 7, 58). Most adolescents reported ever being sexual active (70%; 95% CI = 44, 88) and 49% (95% CI = 17, 82) reported current sexual activity. Regarding sexual risk behaviors, 41% reported two or more recent sexual partners (41%; 95% CI = 17, 70), 21% reported four or more recent sexual partners (95% CI = 4, 66), and 23% reported four or more lifetime sexual partners (95% CI = 3, 75). On average, approximately half of the sexually active adolescents reported ever using a condom (51%; 95% CI = 20, 81) and 43% (95% CI = 12, 81) reported consistent condom use. For studies assessing condom use at last sex event (k= 7), 60% (95% CI = 23, 78) reported condom use at their last sexual encounter. Of the five studies assessing STIs, 15% (95% CI = 3, 50) of the patients self-reported a lifetime STI. A single study (k = 2) tested adolescents for STIs; 9% of those sub-samples were diagnosed with a STI (95% CI = 1, 72).
Table 2.
Prevalence estimates for alcohol, sexual behaviors, and sexually transmitted diseases among adolescents with a psychiatric disorder
| Outcome | k | Prevalence Estimate (95% CI) | Q (p-value) | I2 (95% CI) |
|---|---|---|---|---|
| Alcohol use | ||||
| Alcohol use (lifetime) | 6 | 78% (35, 96) | 189.77*** | 97 (96, 98) |
| Alcohol use (current) | 11 | 36% (19, 58) | 238.84*** | 96 (94,97) |
| Alcohol abuse/dependence | 5 | 24% (7, 58) | 90.06 | 96 (92, 97) |
| Sexual activity | ||||
| Sexual activity (lifetime) | 13 | 70% (44, 88) | 227.22*** | 95 (93, 96) |
| Sexual activity (recent) | 4 | 49% (17, 82) | 50.90*** | 94 (88, 97) |
| Sexual risk behaviors | ||||
| Condom Use, % of participants | 5 | 51% (20, 81) | 71.10*** | 94 (90, 97) |
| Condom Use, consistent | 4 | 43% (14, 77) | 82.91*** | 93 (88, 96) |
| Condom Use, last sex event | 7 | 60% (23, 78) | 9.07* | 67 (3, 89) |
| Multiple Partners, 2 or more (recent) | 6 | 41% (17, 70) | 38.06*** | 87 (74, 93) |
| Multiple Partners, 4 or more (recent) | 3 | 21% (4, 66) | 6.77* | 70 (0, 90) |
| Multiple Partners, 4 or more (lifetime) | 2 | 23% (3, 75) | 2.45 | 59 (0, 90) |
| Sexually transmitted infections (STIs) | ||||
| Any STI, self-reported | 5 | 15 (3, 50) | 69.70*** | 94 (89, 97) |
| Any STI, diagnosed | 2 | 09 (1, 72) | 21.24*** | 95 (86, 98) |
Note. Prevalence values were estimated using random-effects assumptions.
p ≤ .05;
p ≤ .01;
p ≤ .001
Predictors of Alcohol Use, Sexual Activity, and Sexual Risk Behavior
Meta-regression was used to examine whether sample characteristics (i.e., proportion women, age [continuous and categorical (≤14 years vs. ≥15 years)], proportion White, proportion with mood disorders, proportion with attention-deficit and disruptive behavior, and study setting [inpatient vs. outpatient]) was associated to the variability in prevalence estimates. Due to the limited number of studies, meta-regression analyses were conducted only for alcohol use (current, lifetime), alcohol abuse/dependence, lifetime sexual activity, proportion condom use, multiple sexual partners, and self-reported STIs (see Table 3).
Table 3.
Continous perdictors of alcohol, sexual behaviors, and sexually transmitted diseases among adolescents with a psychiatric disorder
| Outcome | Predictor | k | β (SE) | 95% CI | p |
|---|---|---|---|---|---|
| Alcohol use (lifetime) | Female | 6 | -0.23 (0.97) | -2.92, 2.46 | .83 |
| Age | 6 | -0.34 (0.83) | -2.65, 1.98 | .71 | |
| White | 6 | -1.26 (0.95) | -3.91, 1.39 | .26 | |
| Mood Disorders | 6 | -0.37 (1.03) | -4.79, 4.05 | .75 | |
| ADDB | 3 | -2.17 (1.58) | -22.31, 17.97 | .40 | |
| Alcohol use (current) | Female | 11 | -0.51 (0.62) | -1.91, 0.88 | .43 |
| Age | 11 | -0.23 (0.47) | -1.28, 0.83 | .64 | |
| White | 11 | 0.11 (0.63) | -1.33, 1.54 | .87 | |
| Mood Disorders | 7 | -0.88 (0.80) | -2.94, 1.17 | .32 | |
| ADDB | 6 | -0.03 (1.03) | -2.88, 2.82 | .98 | |
| Alcohol Abuse/Dependence | Female | 5 | 3.02 (4.36) | -10.85, 16.88 | .54 |
| Age | 5 | 1.10 (1.01) | -2.11, 4.30 | .36 | |
| White | 5 | 4.64 (0.49) | 3.07, 6.21 | <.01 | |
| Mood Disorders | 5 | -2.11 (1.94) | -8.28, 4.04 | .35 | |
| ADDB | 5 | 0.36 (1.37) | -4.01, 4.72 | .81 | |
| Sexual activity (lifetime) | Female | 13 | -1.79 (1.03) | -3.98, 0.40 | .10 |
| Age | 13 | 0.76 (0.31) | 0.08, 1.41 | .03 | |
| White | 13 | 0.43 (0.77) | -1.27, 2.14 | .59 | |
| Mood Disorders | 10 | 2.02 (0.74) | 0.32, 3.73 | .03 | |
| ADDB | 9 | 1.04 (1.05) | -1.44, 3.52 | .35 | |
| Condom use, % of participants | Female | 5 | -4.14 (3.68) | -15.86, 7.59 | .34 |
| Age | 5 | 1.03 (1.68) | -4.32, 6.39 | .58 | |
| White | 5 | 0.22 (1.49) | -4.53, 4.97 | .89 | |
| Mood Disorders | 3 | -10.44 (1.66) | -31.55, 10.67 | .10 | |
| ADDB | 3 | -33.60 (18.52) | -268.92, 201.73 | .32 | |
| Condom Use, last sex event | Female | 7 | 2.04 (1.65) | -2.21, 6.29 | .27 |
| Age | 7 | -1.17 (0.84) | -3.33, 1.00 | .22 | |
| White | 7 | -1.20 (1.46) | -4.95, 2.54 | .45 | |
| Mood Disorders | 5 | -0.93 (0.97) | -4.03, 2.17 | .41 | |
| ADDB | 4 | 0.96 (1.74) | -6.54, 8.45 | .64 | |
| Multiple Partners, ≥ 2 (recent) | Female | 6 | -0.84 (0.76) | -2.95, 1.27 | .33 |
| Age | 6 | 0.44 (0.57) | -1.13, 2.02 | .48 | |
| White | 6 | 0.16 (0.55) | -1.35, 1.68 | .78 | |
| Mood Disorders | 5 | 1.35 (1.08) | -2.08, 4.78 | .30 | |
| ADDB | 5 | 0.84 (0.63) | -1.17, 2.86 | .28 | |
| Any STI, self-reported | Female | 5 | 3.16 (1.01) | -0.05, 6.37 | .05 |
| Age | 5 | 0.08 (0.69) | -2.12, 2.29 | .91 | |
| White | 5 | -3.16 (0.56) | -4.95, -1.37 | .01 | |
| Mood Disorders | 4 | 0.69 (1.86) | -7.31, 8.69 | .75 | |
| ADDB | 3 | 0.27 (2.24) | -28.15, 28.68 | .92 |
Note. Female, proportion of sample female. Age, mean age of sample. White, proportion sample white. Mood, proportion of sample with mood disorder. ADDB, proportion of sample with Attention Deficit or Disruptive Behavior disorder. STI, proportion of sample reporting a sexually transmitted infection.
Alcohol use
Lifetime alcohol use was more prevalent among studies conducted in outpatient (73%; 95% CI = 69, 77; k = 3) compared to inpatient settings (55%; 95% CI = 51, 59, k = 1), QB (1) = 36.45, p < .001. Current alcohol use was more prevalent in studies conducted in inpatient (40%; 95% CI = 29, 52;k = 5) compared to outpatient settings (25%, 95% CI = 17, 36; k = 4), QB (1) = 3.86, p = .005. None of the other potential moderators explained variability in prevalence estimates for lifetime or current alcohol use (ps > .05).
Alcohol abuse and/or dependence
A diagnosis of alcohol abuse and/or dependence was more prevalent among studies that sampled a greater proportion of Whites (B = 4.64, p = .003, k = 5). Alcohol abuse and/or dependence was more prevalent among adolescents aged ≥15 years (33%; 95% CI = 21, 48;k = 3) compared to adolescents aged ≤ 14 years (15%; 95% CI = 8, 26, k = 2), QB (1) = 4.57, p< .05. Proportion women, mean age, proportion with mood disorder, proportion with attention-deficit and disruptive behaviors, and setting did not moderate the variability in prevalence estimates for alcohol abuse/dependence (ps > .05).
Sexual activity
Lifetime sexual activity was more prevalent in studies that sampled older adolescents (B = 0.76, p = .003, k = 13) and among adolescents aged ≥15 years (79%; 95% CI = 66, 88;k = 5) compared to adolescents aged ≤14 years (64%; 95% CI = 53, 73, k = 9), QB (1) = 3.78, p = .05. Lifetime sexual activity was also more prevalent when studies included a higher proportion of adolescents with mood disorders (B = 2.02, p = .03, k = 10). Proportion women, proportion White, proportion with attention-deficit and disruptive behaviors, and setting did not moderate the variability in prevalence estimates for lifetime sexual activity (ps > .05).
Condom use
The proportion of adolescents using condoms was higher in studies conducted in outpatient (80%; 95% CI = 75, 84; k = 1) compared to those conducted in inpatient settings (41%, 95% CI = 52, 86;k = 4), QB (1) = 58.49, p< .001. Condom use at the last sexual event was more prevalent among adolescents aged ≤14 years (66%; 95% CI = 49, 80; k = 4) compared to adolescents aged ≥15 years (34%; 95% CI = 18, 53, k = 3), QB (1) = 5.42, p< .05. Proportion women, mean age, proportion White, proportion with mood disorder, and proportion with attention-deficit and disruptive behaviors was not a significant moderator of the proportion of participants who used condoms or condom use at the last sex event (ps > .05).
Multiple partners
The proportion women, mean age, proportion White, proportion with mood disorder, and proportion with attention-deficit and disruptive behaviors did not moderate the number of sexual partners (ps > .05). There were no differences in the proportion of participants with multiple sexual partners by setting or age group (≥15 vs. ≤14 years of age).
Self-reported STIs
Self-reported STIs were more prevalent in studies that sampled more women (B = 3.16, p = .05, k = 5) and fewer Whites (B = -3.16, p = .01, k = 5). Age, proportion with mood disorder, proportion with attention-deficit and disruptive behaviors, and setting was not a significant moderator of self-reported STIs (ps > .05).
Association between Alcohol, Sex, and HIV/STI
Only a single study assessed the association between alcohol consumption (yes, no) and sexual behaviors/STIs ([yes/no]; Brown et al., 2010). Alcohol use was associated with sexual activity (OR = 4.39; 95% CI = 2.99, 6.45) and unprotected sex at the last sex event (OR= 1.66, 95% CI = 1.09, 2.52), but not STIs (OR = 0.62; 95% CI = 0.33, 1.15).
DISCUSSION
This is the first meta-analysis to assess the prevalence of alcohol use, sexual risk behaviors, STIs, and their association among adolescents with a PD. Our meta-analysis shows that (a) adolescents with a PD report high rates of alcohol use, sexual activity, and sexual risk-taking and (b) these prevalence rates differ as a function of sex, age, racial/ethnic minority status, and treatment setting.
The prevalence of lifetime alcohol use (78%) among adolescents with a PD was found to be higher than rates found in other representative national sample of U.S. adolescents (45%-63%);however, the prevalence of current alcohol use was similar to national estimates (22%-33%) (Kann et al., 2016; Johnston, Miech, O’Malley, Bachman, & Schulenberg, 2016). Moderator tests indicate that lifetime use was more prevalent in studies that sampled adolescents in outpatient settings, but current alcohol use was more prevalent in studies that sampled adolescents in inpatient settings. These setting differences may reflect differences in the severity of illness; including comorbidity (cf. Berkson’s bias; Berkson, 1946; Du Fort, Newman, & Bland, 1993). Motivations for drinking (e.g., social vs. coping) may also differ among adolescents being seen in an outpatient (vs. inpatient) setting (cf. Kuntsche, Knibbe, Engels, & Gmel, 2010). Because the available studies did not consistently assess (or report) on drinking motives or severity of PD, future research to investigate these hypotheses is encouraged.
The prevalence of alcohol abuse and/or dependence (24%) was high among adolescents with PD. Results from a national sample of U.S. adolescents aged 12-17 suggests a prevalence of approximately 5% for alcohol or illicit drug dependence/abuse in the past year (Substance Abuse and Mental Health Services Administration, 2014); however, direct comparisons cannot be made given the current study’s slightly older sample. Diagnoses of alcohol abuse and/or dependence were more common when studies sampled a higher proportion of White and older adolescents (≥15 years of age). Relative to other racial or ethnic groups, White youth report higher levels of alcohol use during mid- and late-adolescence making them more likely to meet criteria for abuse or dependence (Chen & Jacobson, 2012). Additionally, typical age of onset for substance use disorders is 15 years old (Merikangas et al., 2010). Our findings reflect these overall patterns.
A significantly high proportion (69%) of adolescents reported ever having sex, with a sizeable subset reporting having had multiple sexual partners in their lifetime (2 or more: 39% and 4 or more: 22%). All of these rates are higher than those observed in the general adolescent population (41% report ever having sex and, of these, only 11% report ≥ 4 sexual partners in their lifetime; Kann et al., 2016). Adolescents with mood disorders were more likely to report lifetime sexual activity and having had four or more sexual partners. This is consistent with the evidence suggesting that adolescents with mood disorders tend to engage in more sexual risk behaviors (e.g., early initiation) compared to adolescents without a mood disorder (Nijjar, Ellenbogen, & Hodgins, 2014), perhaps in an effort to cope with negative emotions (Cooper, Agocha, & Sheldon, 2000; Langer & Tubman, 1997; Tubman, Gil, Wagner, & Artigues, 2003).
Prevalence of reported condom use varied across studies depending on its measurement. For studies that assessed lifetime condom use, approximately 50% of these study participants reported using condoms and 43% reporting consistent condom use. When studies asked about condom use at last sex, approximately 60% of adolescents reported using a condom at their last sexual encounter. Unlike the previously reported risk behaviors, condom use during the last sex event was similar to the national average of 57% (Kann et al., 2016); however, this prevalence varied depending on contextual factors. More participants reported using condoms in studies that sampled from outpatient (80%) vs. inpatient (41%) settings. Again, treatment setting may reflect differences in symptom severity. Adolescents in outpatient settings may have more resources (e.g., cognitive capacity) that enable them to use condoms during sex (DiClemente & Ponton, 1993). Condoms may also be more readily accessible to adolescents in outpatient (vs. inpatient) settings. Finally, studies that sampled younger adolescents (aged ≤14 years) had higher prevalence rates of condom use during the last sex event (66% vs. 33%). Younger adolescents (who are often less sexually experienced) generally report more consistent condom use compared to older adolescents (Bonar et al., 2015).
Few studies reported on STIs, and only two studies used laboratory tests to document the prevalence of STIs. Self-reported STIs were more prevalent in studies that sampled more females and studies that sampled fewer Whites. These findings corroborate prior research showing that females report more STIs and Whites have lower prevalence of STIs compared to non-Whites (Bonar et al., 2015; Bonar et al., 2014). More research is needed to establish the prevalence of STIs in adolescents with a PD and to confirm self-reported rates biologically. Nonetheless, our meta-analysis provides evidence that adolescents with a PD engage in high-risk behaviors that put them at risk for STIs, including HIV.
Only a single study examined the association between alcohol use and sexual risk behaviors or HIV/STIs (Brown et al., 2010). They found that adolescents with PD who endorsed recent alcohol use (i.e. last 30 days) were also more likely to endorse sexual activity and unprotected last sex. This pattern did not hold for the presence of a current STI. Additional research assessing alcohol use, sexual risk behaviors, and STIs among adolescents living with a PD is needed to better elucidate this association.
Limitations
There are five limitations of this meta-analysis. First, studies were primarily identified using electronic databases. Thus, manuscripts that did not contain indicated keywords could have been omitted from the meta-analysis. Second, we identified a small number of studies, which may limit the generalizability of the findings. The limited number of studies also significantly limited our ability to evaluate associations between variables of interest. Additional research on the association between alcohol and sexual risk behaviors is needed within this population. Third, our analyses were limited due to the non-assessment and/or inconsistent reporting of alcohol, sexual, STIs, and PD information across studies. Primary level studies should assess and report specific alcohol use and sexual risk behaviors, including alcohol use prior to sex. Fourth, many samples were recruited from clinical settings; prevalence may differ among non-treatment seeking adolescents with PD. Finally, greater specificity regarding diagnosis and severity (e.g., using structured clinical interviews) would allow for better understanding of the risks associated with specific disorders.
CONCLUSION
Our findings highlight that adolescents with PD are a group whose behavior place them at risk for HIV and other STIs. Higher prevalence of specific alcohol and sexual risk behaviors among these adolescents indicate the need for interventions to reduce both sexual and alcohol risk behaviors. Clinicians should incorporate empirically validated assessments for alcohol and sexual risk as well as use evidence-based practices when targeting these behaviors in conjunction with the primary presenting diagnosis. The careful use of evidence-based assessments and practice in clinical settings will enable further research examining the association of alcohol and sexual risk in this important population. Differences in prevalence of alcohol and sexual risk behaviors according to treatment setting also suggests a need to provide interventions that are targeted to the unique needs of hospitalized adolescents and those treated in outpatient settings.
Acknowledgments
We thank Erika Sevetson, MS, health sciences librarian at the Alpert School of Medicine, Brown University, for assisting with the database searches and the following study authors who provided additional data: Bridgette M. Brawner, PhD, APRN; Larry K. Brown, MD; Briana A. Woods-Jaeger, PhD; Linda A. Teplin, PhD.
Funding Research reported in this paper was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under award number R01AA021355 to Lori A. J. Scott-Sheldon, PhD. Karlene Cunningham, PhD and David A. Martinez, PhD were supported by the Child/Adolescent Biobehavioral HIV Research Training Grant (T32 MH078788) from the National Institute of Mental Health. Karlene Cunningham, PhD was also supported by The Brown Initiative in HIV and AIDS Clinical Research for Minority Communities Training Grant (R25 MH83620). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References
References marked with an asterisk indicate studies included in the meta-analysis and references marked with a daggar indicate studies that are linked (i.e., provided details on the same sample) to the studies included in the meta-analysis.
- †.Abram KM, Teplin LA, McClelland GM, Dulcan MK. Comorbid psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry. 2003;60(11):1097–1108. doi: 10.1001/archpsyc.60.11.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Abrantes AM, Strong DR, Ramsey SE, Kazura AN, Brown RA. HIV-risk behaviors among psychiatrically hospitalized adolescents with and without comorbid SUD. Journal of Dual Diagnosis. 2006;2(3):85–100. doi: 10.1300/J374v02n03_08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-III. 3. Washington, DC: American Psychiatric Association; 1987. revised. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- *.Aruffo JF, Gottlieb A, Webb R, Neville B. Adolescent psychiatric inpatients: Alcohol use and HIV risk-taking behavior. Psychiatric Rehabilitation Journal. 1994;17(4):150–156. [Google Scholar]
- Berkson J. Limitations of the application of fourfold table analysis to hospital data. Biometrics. 1946;2(3):47–53. [PubMed] [Google Scholar]
- *.Bodison PR. An HIV/AIDS prevention study: A comparison of behavioral intentions between psychiatrically diagnosed and non-psychiatrically diagnosed adolescents. (PhD), Temple University; Ann Arbor: 1998. Retrieved from http://search.proquest.com/docview/304455837?accountid=9758 ProQuest Dissertations & Theses Full Text database. [Google Scholar]
- Bonar EE, Walton MA, Caldwell MT, Whiteside LK, Barry KL, Cunningham RM. Sexually Transmitted Infection History among Adolescents Presenting to the Emergency Department. Journal Of Emergency Medicine. 2015 doi: 10.1016/j.jemermed.2015.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonar EE, Whiteside LK, Walton MA, Zimmerman MA, Booth BM, Blow FC, Cunningham R. Prevalence and correlates of HIV risk among adolescents and young adults reporting drug use: Data from an urban Emergency Department in the U.S. Journal of HIV/AIDS & Social Services. 2014;28(2):625–630. [PMC free article] [PubMed] [Google Scholar]
- Booth RE, Zhang Y. Conduct disorder and HIV risk behaviors among runaway and homeless adolescents. Drug and alcohol dependence. 1997;48(2):69–76. doi: 10.1016/s0376-8716(97)00113-0. [DOI] [PubMed] [Google Scholar]
- †.Brakefield T, Wilson H, Donenberg G. Maternal models of risk: links between substance use and risky sexual behavior in African American female caregivers and daughters. J Adolesc. 2012;35(4):959–968. doi: 10.1016/j.adolescence.2012.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Brawner BM. Depression and HIV risk-related sexual behaviors among African American adolescent females (Doctoral dissertation) University of Pennsylvania; 2009. [Google Scholar]
- *.Brawner BM, Gomes MM, Jemmott LS, Deatrick JA, Coleman CL. Clinical depression and HIV risk-related sexual behaviors among African-American adolescent females: Unmasking the numbers. AIDS Care. 2012;24(5):618–625. doi: 10.1080/09540121.2011.630344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LK, Danovsky MB, Lourie KJ, DiClemente RJ, Ponton LE. Adolescents with psychiatric disorders and the risk of HIV. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(11):1609–1617. doi: 10.1016/S0890-8567(09)66573-4. [DOI] [PubMed] [Google Scholar]
- *.Brown LK, Hadley W, Donenberg GR, DiClemente RJ, Lescano C, Lang DM, Oster D, et al. Project STYLE: A Multisite RCT for HIV Prevention Among Youths in Mental Health Treatment. Psychiatric Services. 2014;65(3):338–344. doi: 10.1176/appi.ps.201300095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Brown LK, Hadley W, Stewart A, Lescano C, Whiteley L, Donenberg G, Project SSG, et al. Psychiatric disorders and sexual risk among adolescents in mental health treatment. Journal of Consulting and Clinical Psychology. 2010;78(4):590–597. doi: 10.1037/a0019632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Brown LK, Kessel SM, Lourie KJ, Ford HH. Influence of sexual abuse on HIV-related attitudes and behaviors in adolescent psychiatric inpatients. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(3):316–322. doi: 10.1097/00004583-199703000-00009. [DOI] [PubMed] [Google Scholar]
- *.Brown LK, Lourie KJ, Zlotnick C, Cohn J. Impact of sexual abuse on the HIV-risk-related behavior of adolescents in intensive psychiatric treatment. American Journal of Psychiatry. 2000;157(9):1413–1415. doi: 10.1176/appi.ajp.157.9.1413. [DOI] [PubMed] [Google Scholar]
- †.Brown LK, Nugent NR, Houck CD, Lescano CM, Whiteley LB, Barker D, Zlotnick C, et al. Safe Thinking and Affect Regulation (STAR): Human immunodeficiency virus prevention in alternative/therapeutic schools. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50(10):1065–1074. doi: 10.1016/j.jaac.2011.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Brown LK, Reynolds LA. A Pilot HIV Prevention Program for Adolescents in a Psychiatric Hospital. Psychiatric Services. 1997;48(4):531. doi: 10.1176/ps.48.4.531. [DOI] [PubMed] [Google Scholar]
- †.Brown RA, Ramsey SE, Strong DR, Myers MG, Kahler CW, Lejuez CW, Abrams DB, et al. Effects of motivational interviewing on smoking cessation in adolescents with psychiatric disorders. Tobacco control. 2003;12(Suppl 4):3–10. doi: 10.1136/tc.12.suppl_4.iv3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Bryant ES, Garrison CZ, Valois RF, Rivard JC, Hinkle KT. Suicidal behavior among youth with severe emotional disturbance. Journal of Child and Family Studies. 1995;4(4):429–443. [Google Scholar]
- Centers for Disease Control and Prevention. Sexual Risk Behavior: HIV, STD, & Teen Pregnancy Prevention. 2016 Retrieved from http://www.cdc.gov/healthyyouth/sexualbehaviors/index.htm.
- Chen P, Jacobson KC. Developmental trajectories of substance use from early adolescence to young adulthood: gender and racial/ethnic differences. Journal of Adolescent Health. 2012;50(2):154–163. doi: 10.1016/j.jadohealth.2011.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML, Agocha VB, Sheldon MS. A motivational perspective on risky behaviors: The role of personality and affect regulatory processes. Journal of Personality. 2000;68(6):1059–1088. doi: 10.1111/1467-6494.00126. [DOI] [PubMed] [Google Scholar]
- Costello AJ, Edelbrock C, Dulcan MK, Kalas R, Klaric SH. Development and testing of the NIMH Diagnostic Interview Schedule for Children on a clinical population: Final Report. 1984. Retrieved from Rockville, MD. [Google Scholar]
- *.Cropsey KL, Weaver MF, Dupre MA. Predictors of involvement in the juvenile justice system among psychiatric hospitalized adolescents. Addictive Behaviors. 2008;33(7):942–948. doi: 10.1016/j.addbeh.2008.02.012. [DOI] [PubMed] [Google Scholar]
- Deas D. Adolescent substance abuse and psychiatric comorbidities. Journal of Clinical Psychiatry. 2006;67:18–23. [PubMed] [Google Scholar]
- *.Deas D, Randall CL, Roberts JS. Preventing HIV/AIDS: A brief intervention for adolescent substance abusers. Journal of Child & Adolescent Substance Abuse. 2000;10(2):23–32. [Google Scholar]
- DiClemente RJ, Ponton LE. HIV-related risk behaviors among psychiatrically hospitalized adolescents and school-based adolescents. American Journal of Psychiatry. 1993;150(2):324–325. doi: 10.1176/ajp.150.2.324. [DOI] [PubMed] [Google Scholar]
- †.Donenberg GR. Youths and HIV/AIDS: psychiatry’s role in a changing epidemic. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44(8):728–747. doi: 10.1097/01.chi.0000166381.68392.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Donenberg GR, Brown L, Hadley W, Kapungu C, Lescano C, DiClemente R. Family-Based HIV-Prevention for Adolescents with Psychiatric Disorders. In: Pequegnat W, Bell C, editors. Family and HIV/AIDS: Cultural and Contextual Issues in Prevention and Treatment. New York: Springer; 2012. pp. 261–278. [Google Scholar]
- *.Donenberg GR, Emerson E, Mackesy-Amiti ME. Sexual risk among African American girls: psychopathology and mother-daughter relationships. Journal of Consulting and Clinical Psychology. 2011;79(2):153–158. doi: 10.1037/a0022837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology & Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Fort G, Newman SC, Bland RC. Psychiatric comorbidity and treatment seeking: Sources of selection bias in the study of clinical populations. Journal of Nervous and Mental Disease. 1993;181(8):467–474. [PubMed] [Google Scholar]
- †.Elkington KS, Teplin LA, Mericle AA, Welty LJ, Romero EG, Abram KM. HIV/sexually transmitted infection risk behaviors in delinquent youth with psychiatric disorders: A longitudinal study. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(8):901–911. doi: 10.1097/CHI.0b013e318179962b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Emerson E, Donenberg GR, Wilson HW. Health-protective effects of attachment among African American girls in psychiatric care. Journal of Family Psychology. 2012;26(1):124–132. doi: 10.1037/a0026352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowkes FG, Fulton PM. Critical appraisal of published research: introductory guidelines. British Medical Journal. 1991;302(6785):1136–1140. doi: 10.1136/bmj.302.6785.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Gottlieb A, Aruffo JF, Webb R, Hardin B. Impact of peer-led AIDS education with adolescent medical and psychiatric inpatients. Journal of Adolescent Health. 1991;13(1):70. [Google Scholar]
- †.Hadley W, Barker DH, Lescano CM, Stewart AJ, Affleck K, Donenberg G, et al. Project Style Study, G. Associations Between Psychiatric Impairment and Sexual Risk Behavior Among Teens in Mental Health Treatment. Journal of HIV/AIDS & Social Services. 2013;13(2):198–213. doi: 10.1080/15381501.2013.789416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Hadley W, Brown LK, Lescano CM, Kell H, Spalding K, Diclemente R, et al. Project, S. S. G. Parent-adolescent sexual communication: associations of condom use with condom discussions. AIDS & Behavior. 2009;13(5):997–1004. doi: 10.1007/s10461-008-9468-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Hadley W, Hunter HL, Tolou-Shams M, Lescano C, Thompson A, Donenberg G, et al. Project, S. S. G. Monitoring challenges: a closer look at parental monitoring, maternal psychopathology, and adolescent sexual risk. Journal of Family Psychology. 2011;25(2):319–323. doi: 10.1037/a0023109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harbord RM, Higgins JPT. Meta-regression in Stata. Stata Journal. 2008;8(4):493–519. [Google Scholar]
- Heger JP, Brunner R, Parzer P, Fischer G, Resch F, Kaess M. Depression and Risk Behavior in Adolescence. Prax Kinderpsychol Kinderpsychiatr. 2014;63(3):177–199. [PubMed] [Google Scholar]
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- Huedo-Medina TB, Sanchez-Meca J, Marin-Martinez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychological Methods. 2006;11(2):193–206. doi: 10.1037/1082-989X.11.2.193. [DOI] [PubMed] [Google Scholar]
- Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975-2015: Overview, key findings on adolescent drug use. 2016 Retrieved from Ann Arbor: Retrieved from http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2015.pdf.
- †.Joppa MC, Rizzo CJ, Brown LK, Hadley W, Dattadeen JA, Donenberg G, DiClemente R. Internalizing Symptoms and Safe Sex Intentions among Adolescents in Mental Health Treatment: Personal Factors as Mediators. Child & Youth Services Review. 2014;46:177–185. doi: 10.1016/j.childyouth.2014.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Kapungu CT, Nappi CM, Thakral C, Miller SA, Devlin C, McBride C, Brown LK, et al. Recruiting and Retaining High-Risk Adolescents into Family-Based HIV Prevention Intervention Research. Journal of Child and Family Studies. 2012;21(4):578–588. [Google Scholar]
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Hawkins J, Zaza S, et al. Youth Risk Behavior Surveillance—United States, 2015. Morbidity and Mortality Weekly Report. 2016;65:1–174. doi: 10.15585/mmwr.ss6506a1. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Ryan ND, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatric Annals. 2002;32(9):509–515. [Google Scholar]
- Kuntsche E, Knibbe R, Engels R, Gmel G. Being Drunk to Have Fun or to Forget Problems? European Journal of Psychological Assessment. 2010;26(1):46–54. [Google Scholar]
- †.Lang DL, Rieckmann T, Diclemente RJ, Crosby RA, Brown LK, Donenberg GR. Multi-level factors associated with pregnancy among urban adolescent women seeking psychological services. Journal of Urban Health. 2013;90(2):212–223. doi: 10.1007/s11524-012-9768-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Lang DL, Sales JM, Salazar LF, DiClemente RJ, Crosby RA, Brown LK, Donenberg GR. Determinants of multimethod contraceptive use in a sample of adolescent women diagnosed with psychological disorders. Infectious Diseases in Obstetrics and Gynecology, 2011. 2011 doi: 10.1155/2011/510239. Retrieved from http://www.hindawi.com/journals/idog/ [DOI] [PMC free article] [PubMed]
- Langer LM, Tubman JG. Risky sexual behavior among substance-abusing adolescents: Psychosocial and contextual factors. American Journal of Orthopsychiatry. 1997;67(2):315. doi: 10.1037/h0080235. [DOI] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical Meta-Analysis. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Swendsen J, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W, Brown J, Simpson T, Handmaker N, Bien T, Luckie L. What works? A methodological analysis of alcohol treat outcomes literature. In: Hester R, Miller W, editors. Handbook of Alcoholism Treatment Approaches: Effectiveness Alternatives. Needham Heights, MA: Allyn & Bacon; 1995. pp. 12–44. [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- †.Nappi CM, Thakral C, Kapungu C, Donenberg GR, DiClemente R, Brown L. Parental monitoring as a moderator of the effect of family sexual communication on sexual risk behavior among adolescents in psychiatric care. AIDS & Behavior. 2009;13(5):1012–1020. doi: 10.1007/s10461-008-9495-9. [DOI] [PubMed] [Google Scholar]
- Nijjar R, Ellenbogen MA, Hodgins S. Personality, coping, risky behavior, and mental disorders in the offspring of parents with bipolar disorder: a comprehensive psychosocial assessment. Journal of Affective Disorders. 2014;166:315–323. doi: 10.1016/j.jad.2014.04.047. [DOI] [PubMed] [Google Scholar]
- Patrick ME, Maggs JL, Lefkowitz ES. Daily associations between drinking and sex among college students: A longitudinal measurement burst design. Journal of Research on Adolescence. 2015;25(2):377–386. doi: 10.1111/jora.12135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Ramsey SE, Strong DR, Stuart GL, Weinstock MC, Williams LA, Tarnoff G, Brown RA, et al. Substance use and diagnostic characteristics that differentiate smoking and nonsmoking adolescents in a psychiatric setting. Journal of Nervous & Mental Disease. 2003;191(11):759–762. doi: 10.1097/01.nmd.0000095130.33301.f9. [DOI] [PubMed] [Google Scholar]
- Reyna VF, Farley F. Risk and rationality in adolescent decision-making: Implications for theory, practice, and public policy. Psychological Science in the Public Interest. 2006;7(1):1–44. doi: 10.1111/j.1529-1006.2006.00026.x. [DOI] [PubMed] [Google Scholar]
- †.Rickert VI, Jay MS, Gottlieb A. Effects of a peer-counseled AIDS education program on knowledge, attitudes, and satisfaction of adolescents. Journal of Adolescent Health. 1991;12(1):38–43. doi: 10.1016/0197-0070(91)90039-o. [DOI] [PubMed] [Google Scholar]
- *.Riggs PD, Mikulich-Gilbertson SK, Davies RD, Lohman M, Klein C, Stover SK. A randomized controlled trial of fluoxetine and cognitive behavioral therapy in adolescents with major depression, behavior problems, and substance use disorders. Archives of Pediatrics & Adolescent Medicine. 2007;161(11):1026. doi: 10.1001/archpedi.161.11.1026. [DOI] [PubMed] [Google Scholar]
- Schwab-Stone ME, Shaffer D, Dulcan MK, Jensen PS, Fisher P, Bird HR, Canino G, et al. Criterion validity of the NIMH diagnostic interview schedule for children version 2.3 (DISC-2.3) Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35(7):878–888. doi: 10.1097/00004583-199607000-00013. [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LAJ, Johnson BT. The sexual health of adolescents: Why, when, and how adolescents use contraceptives. In: Bromberg D, O’Donohue W, editors. Handbook of Child and Adolescent Sexuality: Developmental and Forensic Issues. Oxford: Academic Press; 2013. pp. 221–252. [Google Scholar]
- †.Seth P, Lang DL, Diclemente RJ, Braxton ND, Crosby RA, Brown LK, Donenberg GR, et al. Gender differences in sexual risk behaviours and sexually transmissible infections among adolescents in mental health treatment. Sexual Health. 2012;9(3):240–246. doi: 10.1071/SH10098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrier LA, Walls C, Lops C, Kendall AD, Blood EA. Substance use, sexual intercourse, and condom nonuse among depressed adolescents and young adults. Journal of Adolescent Health. 2012;50(3):264–270. doi: 10.1016/j.jadohealth.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J. Causal Considerations on Alcohol and HIV/AIDS - A Systematic Review. Alcohol and Alcoholism. 2010;45(2):159–166. doi: 10.1093/alcalc/agp091. [DOI] [PubMed] [Google Scholar]
- Smith MD. HIV risk in adolescents with severe mental illness: Literature review. Journal of Adolescent Health. 2001;29(5):320–329. doi: 10.1016/s1054-139x(01)00265-8. [DOI] [PubMed] [Google Scholar]
- †.Starr LR, Donenberg GR, Emerson E. Bidirectional linkages between psychological symptoms and sexual activities among African American adolescent girls in psychiatric care. Journal of Clinical Child and Adolescent Psychology. 2012;41(6):811–821. doi: 10.1080/15374416.2012.694607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele CM, Josephs RA. Alcohol myopia: Its prized and dangerous effects. American Psychologist. 1990;45(8):921. doi: 10.1037//0003-066x.45.8.921. [DOI] [PubMed] [Google Scholar]
- †.Stewart AJ, Theodore-Oklota C, Hadley W, Brown LK, Donenberg G, DiClemente R. Mania Symptoms and HIV-Risk Behavior among Adolescents in Mental Health Treatment. Journal of Clinical Child and Adolescent Psychology. 2012;41(6):803–810. doi: 10.1080/15374416.2012.675569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-48 (HHS Publication No (SMA) 14-4863) 2014 Retrieved from Rockville, MD. [Google Scholar]
- Tabrizi G, Vatankhah M, Tabrizi S. Study of personality disorders in AIDS patients with high risk behaviors. Scientific Journal of Iranian Blood Transfusion Organization. 2009;6(4):292–300. [Google Scholar]
- †.Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA. Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry. 2002;59(12):1133–1143. doi: 10.1001/archpsyc.59.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, Washburn JJ. Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. Psychiatric Services. 2005;56(7):823–828. doi: 10.1176/appi.ps.56.7.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Teplin LA, Mericle AA, McClelland GM, Abram KM. HIV and AIDS risk behaviors in juvenile detainees: implications for public health policy. American Journal of Public Health. 2003;93(6):906–912. doi: 10.2105/ajph.93.6.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Teplin LA, Welty LJ, Abram KM, Dulcan MK, Washburn JJ. Prevalence and persistence of psychiatric disorders in youth after detention: a prospective longitudinal study. Archives of General Psychiatry. 2012;69(10):1031–1043. doi: 10.1001/archgenpsychiatry.2011.2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Thurstone C, Riggs PD, Klein C, Mikulich-Gilbertson SK. A one-session human immunodeficiency virus risk-reduction intervention in adolescents with psychiatric and substance use disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(9):1179–1186. doi: 10.1097/chi.0b013e31809fe774. [DOI] [PubMed] [Google Scholar]
- †.Tolou-Shams M, Ewing SWF, Tarantino N, Brown LK. Crack and Cocaine Use Among Adolescents in Psychiatric Treatment: Associations with HIV Risk. Journal of Child & Adolescent Substance Abuse. 2010;19(2):122–134. doi: 10.1080/10678281003634926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tubman JG, Gil AG, Wagner EF, Artigues H. Patterns of sexual risk behaviors and psychiatric disorders in a community sample of young adults. Journal of Behavioral Medicine. 2003;26(5):473–500. doi: 10.1023/a:1025776102574. [DOI] [PubMed] [Google Scholar]
- †.Udell W, Donenberg G, Emerson E. The impact of mental health problems and religiosity on African-American girls’ HIV-risk. Cultural Diversity & Ethnic Minority Psychology. 2011;17(2):217–224. doi: 10.1037/a0023243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Valois RF, Bryant ES, Rivard JC, Hinkle KT. Sexual risk-taking behaviors among adolescents with severe emotional disturbance. Journal of Child and Family Studies. 1997;6(4):409–419. [Google Scholar]
- †.Weaver MF, Dupre MA, Cropsey KL, Koch JR, Sood BA, Wiley JL, Balster RL. Addiction epidemiology in adolescents receiving inpatient psychiatric treatment. Addictive Behaviors. 2007;32(12):3107–3113. doi: 10.1016/j.addbeh.2007.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Wilson HW, Donenberg GR, Emerson E. Childhood violence exposure and the development of sexual risk in low-income African American girls. Journal of Behavioral Medicine. 2014;37(6):1091–1101. doi: 10.1007/s10865-014-9560-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Wilson HW, Emerson E, Donenberg GR, Pettineo L. History of sexual abuse and development of sexual risk behavior in low-income, urban African American girls seeking mental health treatment. Women & Health. 2013;53(4):384–404. doi: 10.1080/03630242.2013.790337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Wilson HW, Woods BA, Emerson E, Donenberg GR. Patterns of Violence Exposure and Sexual Risk in Low-Income, Urban African American Girls. Psychology of Violence. 2012;2(2):194–207. doi: 10.1037/a0027265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †.Woods-Jaeger BA, Jaeger JA, Donenberg GR, Wilson HW. The relationship between substance use and sexual health among African-American female adolescents with a history of seeking mental health services. Womens Health Issues. 2013;23(6):e365–371. doi: 10.1016/j.whi.2013.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]


