Abstract
Purpose
To study the ciliary neurotrophic factor (CNTF) concentration in the aqueous humor (AH), lacrimal fluid (LF), and blood serum (BS) in patients with age-related cataract and primary open-angle glaucoma (POAG).
Methods
CNTF concentrations were studied in 61 patients with age-related cataract, 55 patients with POAG combined with cataract, and 29 healthy controls (one eye in each person). Preliminary experiments permitted us to extend the minimum quantifiable value of the CNTF Quantikine enzyme-linked immunosorbent assay (ELISA) kit to 2.5 pg/ml.
Results
The levels of CNTF in LF and BS did not differ in patients with cataract and controls. The CNTF concentration (pg/ml) in patients with POAG and cataract was lower than in patients with cataract (p<0.001) in AH (39.9±26.2 versus 57.2±25.6) and in LF (25.7±14.9 versus 39.9±18.0). The differences were not statistically significant for the CNTF level in BS (5.45±4.72 versus 5.96±4.92) and the AH/LF ratio (1.69±1.05 versus 1.58±0.70). In the patients with POAG, the AH level of CNTF correlated with the visual field index (Pearson’s correlation coefficient r = 0.35, p = 0.01). A statistically significant decrease in the AH and LF concentrations of CNTF was observed in patients in all stages of POAG compared with the cataract group. This decrease was particularly prominent in patients with severe glaucoma. Compared to patients with combined early and moderate stages of disease patients with advanced glaucoma showed an insignificant reduction in the median CNTF concentration in AH and LF. The serum CNTF concentration did not show any dependence on the glaucoma stage. The CNTF concentration in the AH strongly correlated with the CNTF concentration in the LF (r=0.71, p<0.000). A formula was suggested to calculate the concentration of CNTF in AH based on the CNTF concentration in LF.
Conclusions
The CNTF concentration is reduced in the AH and LF of patients with POAG, especially in those with severe visual field loss. The CNTF concentration in AH and LF showed a strong correlation, and this phenomenon opens up new options for a noninvasive estimation of the CNTF concentration in AH. The CNTF concentration established in the AH, LF, and BS of patients with age-related cataract can serve as normative data for persons older than 50 years old.
Introduction
Neurotrophic factors are a class of regulatory proteins of the nervous tissue that promote proliferation, differentiation, survival, and functioning of neurons [1-3]. Neurotrophic factors are expected to play an important role in severe eye diseases, such as glaucoma, age-related macular degeneration, etc. Among these proteins, ciliary neurotrophic factor (CNTF) belonging to the neuropoietic cytokine family has attracted much attention [2,3].
CNTF is one of the most widespread cytokines in the nervous tissue [3]. The neuroprotective properties of CNTF have been demonstrated in animal models of the optic nerve or retinal damage [4-6]. Clinical trials of CNTF delivered by the intraocular encapsulated cell technology implant NT-501 (Neurotech Pharmaceuticals, Inc.) have been performed in severe eye diseases, such as age-related macular degeneration and retinitis pigmentosa [7-9]. CNTF was found in the inner and outer layers of the retina [5,10,11], the RPE [12], and the cells of the optic nerve head [13].
Analysis of the neurotrophic factors in the human eye may be of great importance for clarification of the pathogenesis of glaucoma and other ophthalmic diseases and evaluation of the efficacy of treatments that influence the concentrations of neurotrophic factors in the eye. However, in practice these studies are unrealizable outside planned surgical interventions. A single proteomics study reported the presence of the CNTF receptor (CNTFRα) in the aqueous humor (AH) of patients who underwent surgery for an uncomplicated cataract [14].
Scarce information, limited to a few biologic substances, exists on the interrelation of substance concentrations in lacrimal fluid (LF) and AH [15-20]. Previously, in a small group of patients operated for age-related cataract, a statistically significant correlation between AH and LF concentrations was shown for CNTF and brain-derived neurotrophic factor (BDNF) [21,22].
Therefore, we studied the CNTF levels in the LF, AH, and blood serum (BS) of patients with age-related cataract and primary open-angle glaucoma (POAG). The main purpose was to study CNTF levels in the AH of patients with POAG, while the secondary objective was to examine the interrelations between CNTF concentrations in LF and AH.
Methods
Subjects
We examined 116 patients (75 women, 41 men, age range 53-88 years) operated in The S. Fyodorov Eye Microsurgery Federal State Institution and 29 healthy volunteers (20 women, 9 men, age range 61-78 years) enrolled among persons undergoing routine periodic ophthalmic examination in the same Institution. All subjects were divided into three groups. Group 1 (the main or cataract and POAG group) consisted of 55 consecutive patients (55 eyes) with POAG, operated for age-related cataract. Group 2 (the comparison or cataract group) included 61 consecutive patients (61 eyes) without POAG, operated for age-related cataract. Group 3 (the control group) included 29 persons (29 eyes) without any ophthalmic diseases.
The inclusion criteria were age older than 50 years, axial length of the eye less than 26 mm, and amount of LF sufficient to measure CNTF levels. For patients with POAG, the inclusion criteria were uncomplicated phacoemulsification, open angles at gonioscopy, intraocular pressure (IOP) <26 mmHg preoperatively, and reliable repeated standard automated perimetry (Humphrey Field Analyzer II, Carl Zeiss Meditec Inc., Dublin, CA) using the Swedish Interactive Threshold Algorithm (SITA) Standard 24–2 program. In the comparison group, the inclusion criteria were uncomplicated age-related cataract, uneventful phacoemulsification, and postoperative best-corrected visual acuity not less than 20/40. Subjects in the cataract and control groups should have had IOP <21 mmHg, normal Humphrey visual fields, and normal appearance of the optic disc and retinal nerve fiber layer. In the patients, a thorough examination including perimetry and optical coherence tomography was performed (repeated) after the operation. The POAG stage was established according to Glaucoma Staging System suggested by Mills et al. [23].
The exclusion criteria were any serious ophthalmic diseases (uveitis, degenerative diseases of the retina, corneal dystrophies, etc.), any ophthalmic surgery during the previous 3 months, and severe somatic pathology (diabetes mellitus, autoimmune or oncological diseases, etc.). Persons with initial or mild manifestations of somatic diseases, such as essential hypertension, ischemic heart disease or cardiac arrhythmias, etc., were not excluded.
The same surgeon operated on all patients. This study adhered to the tenets of the Declaration of Helsinki and had local ethics committee approval with written informed consent obtained from all subjects.
Specimens sampling and CNTF determination
In both groups of patients, AH and fasting venous blood were collected during the phacoemulsification. AH (100–120 µl) was taken immediately after entering the anterior chamber. LF was sampled on the day preceding the surgery to evade the influence of drugs instilled into the conjunctival fornix in the evening and morning before surgery. Similar to the patient groups, in the control group LF and blood were not collected on the same day.
In all subjects, a pipette was used to sample stimulated LF (secreted by the lacrimal gland in response to gentle touch of the cornea with the disposable tip of the pipette). A minimal sample of 100 µl was needed to measure CNTF in LF or AH. To obtain serum, blood samples collected in Gel/Clotting activator S-Monovette tubes (Sarstedt GmbH, Nümbrecht, Germany) were left at room temperature for 30 min and centrifuged at 1,500 ×g for 15 min. The BS, AH, and LF samples were stored at −25 °C in polypropylene tubes (Sarstedt GmbH, Nümbrecht, Germany) and analyzed within 3 months from sampling. The author who performed the CNTF analyses (TAD) was blinded to the patients’ details.
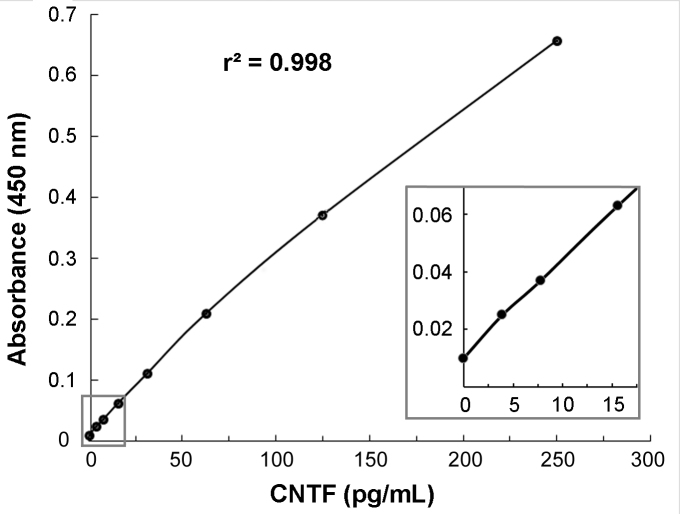
Upon thawing, the samples were centrifuged at 4,000 ×g for 15 min at 4 °C to ensure complete removal of the debris. The CNTF concentration was measured in biologic fluids using Human CNTF Quantikine enzyme-linked immunosorbent assay (ELISA) kits (R&D Systems, Inc., Minneapolis, MN) on a ChemWell 2910 automatic analyzer (Awareness Technology, Inc., Palm City, FL); the diluting solution of the kit was substituted to PBS (1X; 137 mM NaCl, 2.7 mM KCl, 10 mM NaPO4, 1.76 mM KPO4, pH 7.4) containing 1% bovine serum albumin (1% BSA in PBS). This solution was selected from six different diluents based on the optimal adjuvant properties and the lowest blank absorbance for CNTF measurements in diluted (1:3) AH and LF samples. The standard curve was created using calibrating solutions between 0 and 250 pg/ml (Figure 1). The minimum quantifiable value for the CNTF ELISA with the selected diluent was determined to be 2.5 pg/ml.
Figure 1.
Representative CNTF standard curve obtained using Human CNTF Quantikine ELISA kits with 1% BSA in PBS as diluent (calibrating solutions 0–250 pg/ml). The inset is an enlargement of the 0–17.5 pg/ml portion of the graph.
Statistical analysis
Statistical analysis was performed using R software package version 3.2.3 (The R Foundation for Statistical Computing, accessed February 12, 2017). The minimal required number of subjects in groups 1 and 2 was 51. It was calculated with the equation n1 = n2 = (Z1-α/2 + Z1-β)2 × (σ12 + σ22) / d2 [24], where σ1 and σ2 are standard deviations of CNTF levels in AH in groups 1 and 2 (27 and 23 pg/ml in the preliminary study, respectively), d is the minimal detectable difference (assumed 14 pg/ml), α was chosen to be 5%, and power (1-β) set at 80%.
The associations of the variables were analyzed with a simple linear regression. Pearson’s correlation coefficients (r) were calculated as well. The data sets were checked for outliers with Bonferroni adjustment of the p value for the largest absolute Studentized residual [25]; cases with Bonferroni-adjusted p value of less than 0.05 were excluded. The correlation coefficients were compared, and if appropriate, a common (weighted) correlation coefficient was calculated [26]. For the strength of the association for the absolute values of the correlation coefficient, 0.20–0.39 was regarded as weak, 0.40–0.59 as moderate, and 0.60–0.79 as strong [27].
Continuous variables were compared with Welch’s t test or the Mann–Whitney U test, as appropriate; comparisons in three or more groups were performed using the Kruskal–Wallis test and post hoc pairwise comparisons with p value adjustment for multiple comparisons. Categorical variables were compared with Fisher's exact test.
Summary statistics on the data sets of BS with a portion of observations (<25%) below the minimum quantifiable value (censored) were performed using the Kaplan–Meier method for groups of fewer than 50 cases; otherwise, the maximum likelihood estimation method was used [28,29]. The generalized Wilcoxon test or two-sample maximum likelihood estimation test was used for comparison of variables with censored values [28,29]. A p value of less than 0.05 was considered statistically significant.
Results
Four samples of BS in the cataract group and one sample of BS in the control group were excluded from the study because of hemolysis. The CNTF concentration in LF was not examined in two patients in the cataract and POAG group due to technical errors. Twenty-two values in BS (11–24% in different groups) were below the validated assay range.
The mean age of the patients in the control group was statistically significantly lower than that in the cataract group. To compensate for the age difference, we formed a subgroup (the cataract subgroup) by excluding patients younger than 61 years and older than 75 years (two of five 75-year-old patients were also excluded). The CNTF concentrations in the LF and BS, as well as the age and gender characteristics of the cataract subgroup and controls, are presented in Table 1.
Table 1. Age and gender characteristics and CNTF concentrations (pg/ml) in the lacrimal fluid and blood serum of cataract patients and healthy controls.
| Variable | Cataract subgroup (n=33a) | Control group (n=29a) |
|---|---|---|
| Age | ||
| mean±SD |
67.8±4.0 |
67.5±4.7 |
| range |
61–75 |
61–78 |
| median (IQR) |
67.0 (65.0–71.0) |
66.0 (65.0–70.0) b |
| Sex | ||
| women, n (%) |
23 (70%) |
20 (69%) c |
| CNTF in lacrimal fluid | ||
| mean±SD |
41.5±19.0 |
40.1±12.1 |
| range |
4.6–92.4 |
16.8–66.8 |
| median (IQR) |
42.6 (28.2–52.5) |
40.2 (31.2–48.0) b |
| CNTF in blood serum | ||
| mean±SD |
5.87±4.95 |
5.78±2.80 |
| maximum |
26.50 |
12.10 |
| median (IQR) |
4.20 (2.60–6.60) |
4.90 (3.00–7.90) d |
| n / n censored | 32 / 6 | 28 / 5 |
The differences between cataract subgroup and control group are not significant (b Mann–Whitney U test, c Fisher's exact test; d two-sample maximum likelihood estimation test) SD – standard deviation; IQR – interquartile range; n censored - number of observations below the minimum quantifiable value 2.5 pg/ml a For CNTF in blood serum n is indicated in the last row.
According to the data shown in Table 1, the CNTF levels in the LF and BS of the patients with cataract did not differ from those in healthy controls. Thus, age-related cataract has little or no effect on the CNTF level in the LF and BS.
Next, we compared the main group (the cataract and POAG group) with the comparison (cataract) group. These two groups did not differ by gender: 32 (58%) versus 43 (70%) women (p=0.18). The age difference was also not statistically significant: 72.4±6.20 (range: 55–84) versus 69.8±8.80 (53–88) years (p=0.07). The data sets for the CNTF concentrations in the biologic fluids studied in both groups are presented in Table 2. The relationship between the CNTF concentrations in the AH and LF (the AH/LF ratio) is also shown in Table 2.
Table 2. CNTF concentrations in the biologic fluids (pg/ml) and the aqueous humor to lacrimal fluid ratio in cataract patients with and without POAG.
| Biologic fluid | Cataract and POAG group (n=55) | Cataract group (n=61a) | P |
|---|---|---|---|
| Aqueous humor | |||
| mean±SD |
39.9±26.2 |
57.2±25.6 |
<0.001 |
| range |
3.4–135.2 |
7.0–135.2 |
|
| median (IQR) |
36.6 (24.5–47.7) |
57.0 (38.0–72.8) |
|
| Lacrimal fluid | |||
| mean±SD |
25.7±14.9 b |
39.9±18.0 |
<0.001 |
| range |
3.2–84.4 |
4.6–92.4 |
|
| median (IQR) |
23.8 (17.6–31.4) |
38.4 (28.2–50.2) |
|
| Aqueous humor / lacrimal fluid ratio | |||
| mean±SD |
1.69±1.05 b |
1.58±0.70 |
NS |
| range |
0.45–6.88 |
0.33–4.33 |
|
| median (IQR) |
1.48 (1.15–1.82) |
1.47 (1.09–1.82) |
|
| Blood serum | |||
| mean±SD |
5.45±4.72 |
5.96±4.92 |
NS |
| maximum |
20.30 |
29.50 |
|
| median (IQR) |
4.12 (2.49–6.83) |
4.59 (2.82–7.47) |
|
| n / n censored | 55 / 10 | 57 / 7 | |
Statistical analysis was performed by Mann–Whitney U test; CNTF in blood serum was compared by the generalized Wilcoxon test POAG – primary open-angle glaucoma; SD – standard deviation; IQR – interquartile range; n censored - number of observations below the minimum quantifiable value 2.5 pg/ml; NS – non-significant a For blood serum n=57 b n=53 (two cases excluded with CNTF in lacrimal fluid not examined)
The CNTF levels varied in a relatively wide range in all biologic fluids studied. In both groups, the CNTF concentration was highest in the AH, somewhat lower in the LF, and much lower in the BS.
The CNTF levels in the AH and LF of the patients with glaucoma were statistically significantly lower than those in patients with cataract without POAG. The decrease in the CNTF concentration in the AH of the patients with POAG was proportional to the decrease in the Humphrey visual field index (VFI) indicative of glaucoma severity, showing a weak but statistically significant Pearson’s correlation: r=0.35, p=0.011 (Figure 2).
Figure 2.
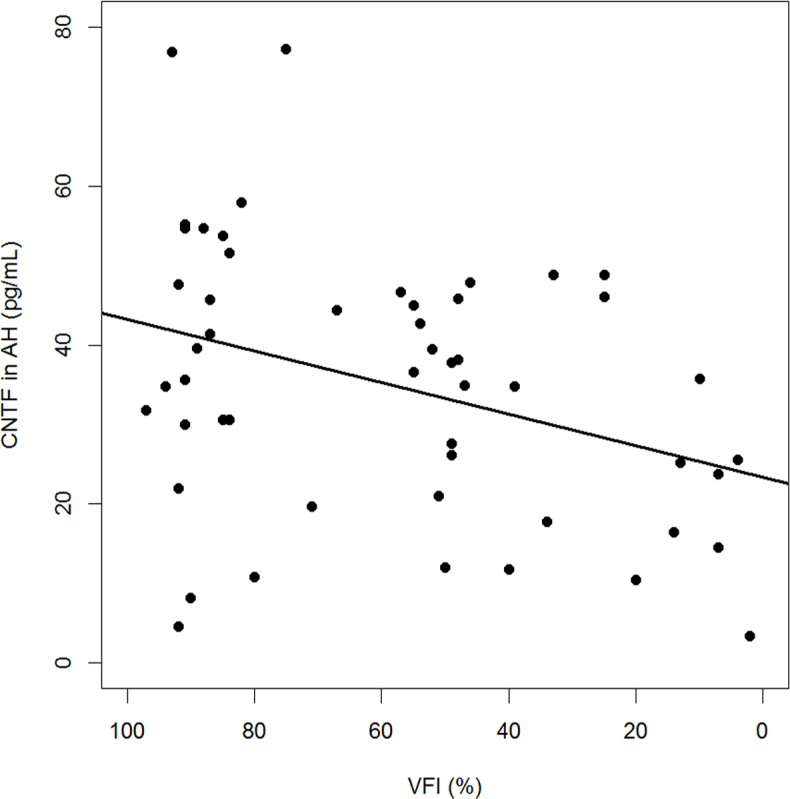
Plot of the CNTF concentration in aqueous humor versus the Humphrey visual field index. The solid line represents the linear regression fit. Note the reversed x-axis.
To study further the role of glaucoma progression, the CNTF concentrations were compared in patients with different POAG stages (due to the small number of cases, patients with early and moderate glaucoma were combined into one group). The detailed characteristics of patients with different POAG stages are presented in Table 3. The CNTF concentrations in the AH, LF, and BS did not show statistically significant correlations with the variables listed in Table 3 with only one exception: The CNTF level in the LF correlated statistically significantly with the IOP (Pearson’s r=0.39, p=0.005).
Table 3. Age and gender characteristics, IOP, medical, laser, and surgical treatment in the main group depending on the POAG stage.
| Variable | POAG stage |
P |
||
|---|---|---|---|---|
| 1/2. Early to moderate (n=21) | 3. Advanced (n=18) | 4. Severe (n=16) | ||
| Age | ||||
| mean±SD |
73.3±6.0 |
74.2±5.9 |
69.1±5.9 |
0.031 a |
| range |
55–83 |
60–84 |
58–79 |
|
| median (IQR) |
73.0 (71–78) |
75.5 (71–78) |
70.5 (64.8–74) |
|
| Sex | ||||
| Women, n (%) |
15 (71%) |
11 (61%) |
6 (37.5%) |
|
| IOP, mmHg | ||||
| mean±SD |
17.6±3.7 |
18.4±4.1 |
15.2±4.2 |
|
| range |
8–25 |
7–25 |
10–23 |
|
| median (IQR) |
17 (16–19) |
19 (17–20.5) |
14 (11–19) |
|
| Medications, n (%) | ||||
| β-blockers |
15 (71%) |
15 (83%) |
10 (63%) |
|
| Prostaglandin
analogs |
7 (33%) |
6 (33%) |
10 (63%) |
|
| Topical
carbonic
anhydrase
inhibitors |
8 (38%) |
5 (28%) |
2 (13%) |
|
| α2-adrenergic
agonists |
- |
4 (22%) |
1 (6%) |
0.044 b |
| Laser treatment and surgery | ||||
| SLT |
3 (14%) |
1 (6%) |
1 (6%) |
|
| NPDS |
7 (33%) |
7 (39%) |
6 (38%) |
|
| NPDS+deferr ed Nd:YAG goniopuncture | 3 (14%) | 5 (28%) | 4 (25%) | |
a Kruskal–Wallis test; b Fisher's exact test POAG – primary open-angle glaucoma; SD – standard deviation; IQR – interquartile range; IOP – intraocular pressure; SLT – selective laser trabeculoplasty; NPDS – nonpenetrating deep sclerectomy
Patients with different POAG stages had similar gender characteristics, IOP, and surgical treatment but differed statistically significantly by age and medical treatment with α2-adrenergic agonists. The CNTF changes depending on POAG stage are shown in Table 4. Means adjusted by age, gender, IOP, medical, laser, and surgical treatment are included in this table. A 72-year-old female patient with an IOP of 17 mmHg who received only β-blockers who did not have any laser or surgical treatment was taken as the standard.
Table 4. CNTF concentrations in the biologic fluids (pg/ml) and the aqueous humor to lacrimal fluid ratio in the main group depending on the POAG stage.
| Biologic fluid | POAG stage |
P / Padj | ||
|---|---|---|---|---|
| 1/2. Early to moderate (n=21) | 3. Advanced (n=18) | 4. Severe (n=16) | ||
| Aqueous humor | ||||
| mean±SD |
44.6±25.9 |
45.2±31.6 |
27.7±14.6 |
NS / |
| mean (adjusted) |
45.3 |
42.7 |
28.2 |
0.028 b |
| range |
4.6–130 |
10.8–135.2 |
3.4–48.8 |
|
| median (IQR) |
41.4 (30.6–54.7) |
38.8 (26.6–46.4) |
25.4 (16–38.1) |
|
| Lacrimal fluid | ||||
| mean±SD |
28.5±14.6 a |
27.5±16.8 |
19.9±11.8 a |
0.041 c / |
| mean (adjusted) |
28.3 |
26.6 |
22.7 |
NS |
| range |
3.2–67.6 |
7.6–84.4 |
4.4–52.8 |
|
| median (IQR) |
28.5 (23.1–35.9) |
23.7 (20–26.3) |
20.0 (13.2–23.8) |
|
| Aqueous humor / lacrimal fluid ratio | ||||
| mean±SD |
1.89±1.47 a |
1.68±0.75 |
1.44±0.62 a |
NS / |
| mean (adjusted) |
1.91 d |
1.58 |
1.49 |
NS |
| range |
0.56–6.88 |
0.45–3.48 |
0.66–2.77 |
|
| median (IQR) |
1.50 (1.28–1.78) |
1.58 (1.28–1.93) |
1.26 (1.07–1.75) |
|
| Blood serum | ||||
| mean±SD |
4.60±2.24 |
6.32±4.01 |
5.78±2.76 |
NS / |
| mean (adjusted) |
3.21 |
5.19 |
4.21 |
NS |
| Maximum |
11.6 |
20.3 |
10.6 |
|
| median (IQR) |
3.90 (2.70–5.60) |
4.80 (3.80–6.60) |
4.50 (3.20–8.00) |
|
| n censored | 5 | 2 | 3 | |
Statistical analysis was performed by Kruskal–Wallis test with post hoc pairwise comparisons by Holm method; CNTF in blood serum was compared by the generalized Wilcoxon test SD – standard deviation; IQR – interquartile range; n censored - number of observations below the minimum quantifiable value 2.5 pg/ml; NS – non-significant; means are adjusted by age, sex, IOP, medical, laser, and surgical treatment; Padj – P for adjusted values a One case excluded with CNTF in lacrimal fluid not examined b Padj 1/2–4=0.010 c P1/2–4=0.017 d Without two extreme outliers, mean±SD=1.43±0.35, mean (adjusted)=1.45.
The adjusted CNTF values demonstrated mostly the same relationships as the unadjusted ones. The decrease in the CNTF levels in the AH and LF was particularly prominent in patients with severe glaucoma (the difference with early to moderate POAG was statistically significant for LF and with the adjustment, for AH). Compared to patients with early to moderate POAG, patients with advanced glaucoma showed an insignificant reduction in the median CNTF concentration in AH and LF.
When compared to the cataract group (see Table 2), patients in all stages of POAG demonstrated statistically significant decreases in AH and LF concentrations of CNTF (p<0.05; for the severe stage of the disease p<0.001, the Kruskal–Wallis test with post hoc pairwise comparisons with the Holm method). The CNTF concentration in serum did not show any dependence on glaucoma stage.
The CNTF level in the AH was statistically significantly correlated with the CNTF level in LF: The Pearson’s correlation coefficient was r=0.62 (95% confidence interval [95% CI]: 0.44–0.76, p<0.000) in the cataract group and r=0.72 (95% CI: 0.57–0.83, p<0.000) in the cataract and POAG group. These coefficients were not statistically significantly different; a common (weighted) correlation coefficient was 0.71 (95% CI: 0.60–0.79, p<0.000). In the cumulated group of patients with cataract and POAG and patients with cataract, a formula for estimating the concentration of CNTF in AH (y) depending on its concentration in LF (x) was derived with a simple linear regression:
y = 15.07 + 0.963 × x
(p<0.000; adjusted R2=0.527; standard error [SE] of intercept=3.28; SE of regression coefficient=0.087).
Discussion
In this work, we present new quantitative data on the concentrations of CNTF in human AH, LF, and BS. Due to the low level of CNTF in these biologic fluids, particularly in BS, assessing the CNTF concentrations using the existing ELISA kit with a low sensitivity (lower limit of quantitation 8 pg/ml) was a challenge. Our preliminary experiments permitted the introduction of some changes in the evaluation procedure and extended the minimum quantifiable value of CNTF to 2.5 pg/ml.
Limited information exists on CNTF concentration in BS. Some authors reported on the absence of CNTF in BS [8], while others found levels of about 1.9 pg/ml [30] or 9 pg/ml [31]. The present results fit within this concentration range. As for AH, previously a single proteomics study reported on the presence of the CNTF receptor (CNTFRα) in AH sampled during cataract surgery [14]; however, these data were not confirmed in other proteomics studies [32,33].
The present study was performed in patients with age-related cataract. Selecting this cohort of patients was motivated by the high prevalence of the disease, frequent need for surgical treatment, and its relatively benign course that is not accompanied by significant immune or inflammatory changes (largely because the lens is avascular and devoid of nerve elements). We did not find statistically significant differences in the CNTF concentrations in the LF and BS of the healthy controls and patients with cataract. These data confirmed our assumption that age-related cataract has little or no effect on the CNTF levels in the LF and BS. The strong correlation of CNTF levels in AH and LF found in the present study suggests that age-related cataract does not influence the CNTF level in AH. Thus, we assume that the new values of the CNTF levels in the AH and LF of patients with age-related cataract established in the present study can serve as normative data for healthy people older than 50 years of age.
The data for the CNTF level in the AH of patients with POAG provide new insight into pathogenesis of this potentially blinding disease. The present study shows that the CNTF concentration decreases in the AH of the patients with POAG, and this process goes in parallel with the disease progression (reduction in the VFI). The median CNTF level in AH showed a 27% decrease in early to moderate glaucoma, a 32% decrease in advanced glaucoma, and a 55% decrease in the severe stage of the disease. The relatively small reduction in the advanced stage compared to the combined early and moderate stage of the disease could be associated with the high variability of CNTF levels in AH, because the reduction in the median CNTF level in LF in the advanced stage is much more pronounced.
CNTF has been studied extensively in animals after optic nerve damage or in glaucoma models. Numerous studies have shown the neuroprotective effect of CNTF on retinal ganglion cells [4,34,35]. The level of CNTF increased in the first 4–8 weeks after major damage (crash, section, etc.) to the optic nerve [5,6]. In a mouse glaucoma model, CNTF also showed upregulation in the early terms of the disease but declined statistically significantly at the advanced stages (at the 30th week) [11]. The present results showing a prominent CNTF reduction in the severe stage of POAG are consistent with the latter data. We did not see CNTF upregulation in the patients in the present study even in the initial stages of the disease, apparently due to its long course.
It is not known whether CNTF deficiency in the AH of patients with POAG is the result or one of the causative factors of retinal ganglion cell death in POAG. In both cases, the CNTF supply to the eyes of patients with glaucoma seems beneficial and might promote survival of the retinal ganglion cells. Now, when modern methods offer possibilities for a continuous delivery of CNTF into the eye [7-9], the new data on CNTF deficiency in the AH of patients with POAG provide a basis for investigating such treatment methods in glaucoma.
Of special interest are the data on the similarity of the CNTF AH/LF ratio in patients with cataract with and without POAG. Studies have reported on different biologic substances in the LF, implying that the changes in the concentration in LF could be indicative of changes in the substances’ intraocular levels. For example, a decrease in the BDNF level in LF in glaucoma was regarded as a possible indicator of the BDNF decline in the eye [36], although such an assumption has not been justified. Therefore, the second objective of this study was to determine the interrelations between CNTF concentrations in the eye (in AH) and in LF. A strong correlation between CNTF levels in AH and LF was found, and it is the second important new result of this study. The formula established with a simple linear regression opens up new possibilities and is promising for indirect studies of CNTF concentrations in the AH of patients with different eye conditions. Certainly, such studies should be limited to groups of patients and not to individual subjects. In addition, it is quite possible that conditions other than POAG could influence the AH/LF ratios of neurotrophic factors; this issue needs further clarification and will be the subject of our future studies.
The correlations between the CNTF levels in AH and LF may actually be much stronger; they may be partially masked due to the sampling of AH and LF on different days. This suggestion was confirmed by data in studies that used same-day sampling of AH and LF and showed much stronger correlations for interleukins (IL-4, IL-6, IL-8, and IL-10) and matrix metallopeptidase 9 (MMP-9) in patients with choroidal melanoma [19,20].
The CNTF concentration in the AH was higher than in the LF. Other biologic substances could demonstrate different relations between AH and LF levels. For example, similar concentrations in AH and LF were found for proinflammatory cytokines (interleukins), and MMP-9 in patients with choroidal melanoma [19,20] and for uric acid [17]. The level of complement decay-accelerating factor (DAF) was reported to be almost 70 times higher in LF compared to that in AH [16], while the lactoferrin concentration was 30–40 times lower [18]. The AH/LF ratio for cystatin C [18] is the inverse compared to the AH/LF ratio for CNTF found in the present study. Some biologic substances identified in LF, such as epidermal growth factor (EGF), were not found in AH [15]. Possible reasons for these differences are not clear. If the substance is supplied to the LF from the AH, then the substance’s lipophilicity and molecular weight play an important role [37].
The primary place of origin of the substance may be relevant as well. In the case of CNTF, the present study data indirectly point to its intraocular origin, because the CNTF concentrations in AH and LF greatly exceed the concentration in BS. Numerous animal studies have shown the expression of CNTF in different cells and layers of the retina, as well as cells of the optic nerve head [5,10-13].
Several limitations may present in this study, including:
1. We studied CNTF levels in the AH of patients, although apparently CNTF in the vitreous plays major role in the survival of the retinal ganglion cells. It is not possible to sample vitreous during uncomplicated cataract surgery. Several studies suggest that the levels of cytokines in AH reflect the vitreous levels of these molecules [38,39], although for many proteins the levels in AH do not reflect those in the vitreous [40]. No data of this kind exist for CNTF. Still, a strong correlation of the CNTF concentration in AH and LF suggests a similar strong correlation of CNTF concentrations in AH and vitreous, although further study is needed.
2. In preliminary experiments, we extended the minimum quantifiable value of the Human CNTF Quantikine ELISA kit from 8.0 to 2.5 pg/ml. It was necessary to study the BS concentrations of CNTF. However, it practically did not influence the measurements of the CNTF concentrations in AH and LF because only 4% of the AH and LF samples had CNTF levels below 8.0 pg/ml. 3. The LF, AH, and BS were not sampled on the same day; therefore, the correlations established in the present study could be underestimated (partially masked). 4. We collected stimulated LF, which could influence CNTF levels. However, it was the only way to obtain a minimal amount of LF needed for examination, particularly in elderly patients. 5. We did not study CNTF in the AH of younger persons, because they usually have cataract of other types caused by trauma, diabetes, uveitis, etc., which obviously could affect the concentrations of neurotrophic factors. 6. Patients with IOP ≥ 26 mmHg were not included in the study, which could influence the IOP correlations with CNTF levels. However, the recruitment of such individuals is difficult, because usually the IOP in such patients is lowered by medications or surgery before phacoemulsification.
In conclusion, the CNTF concentration was decreased in the AH and LF of patients with POAG in particular with severe visual fields loss. These data could serve as an additional reason for investigating modern approaches to intraocular CNTF delivery in patients with glaucoma. The CNTF concentration in AH and LF showed a strong correlation. This phenomenon opens up new approaches for indirect studies of the CNTF level in the AH of patients with POAG and presumably with other ocular diseases, although further research is needed. The CNTF concentrations in AH, LF, and BS established in patients with age-related cataract can be regarded as normative data in persons older than 50 years old.
Acknowledgments
This study is a part of the research project of The S. Fyodorov Eye Microsurgery Federal State Institution, supported by the Ministry of Health of the Russian Federation. Partially supported by Russian Science Foundation grant # 14-25-00136 (development of the improved CNTF assay). The authors are named inventors of the Russian patent on methodology of indirect studies of CNTF contents in AH described in this manuscript. The authors thank Andrey V. Golovin, MD, PhD from The S. Fyodorov Eye Microsurgery Federal State Institution for his help with patient selection and performing cataract surgery and aqueous humor sampling in all patients. This work was presented in part at ARVO meeting 2017.
References
- 1.Skaper SD. The neurotrophin family of neurotrophic factors: an overview. Methods Mol Biol. 2012;846:1–12. doi: 10.1007/978-1-61779-536-7_1. [DOI] [PubMed] [Google Scholar]
- 2.Squire L, Berg D, Bloom F, du Lac S, Ghosh A, Spitzer N. Fundamental neuroscience. 3rd ed. Amsterdam etc.: Elsevier Academic Press; 2008. p.437–516. [Google Scholar]
- 3.Pasquin S, Sharma M, Gauchat JF. Ciliary neurotrophic factor (CNTF): New facets of an old molecule for treating neurodegenerative and metabolic syndrome pathologies. Cytokine Growth Factor Rev. 2015;26:507–15. doi: 10.1016/j.cytogfr.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 4.MacLaren RE, Buch PK, Smith AJ, Balaggan KS, MacNeil A, Taylor JS, Osborne NN, Ali RR. CNTF gene transfer protects ganglion cells in rat retinae undergoing focal injury and branch vessel occlusion. Exp Eye Res. 2006;83:1118–27. doi: 10.1016/j.exer.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 5.Valter K, Bisti S, Gargini C, Di Loreto S, Maccarone R, Cervetto L, Stone J. Time course of neurotrophic factor upregulation and retinal protection against light-induced damage after optic nerve section. Invest Ophthalmol Vis Sci. 2005;46:1748–54. doi: 10.1167/iovs.04-0657. [DOI] [PubMed] [Google Scholar]
- 6.Cai J, Cheng J, Huang X, Li Y, Ma X, Li Y, Wei R. Pathologic changes in chronic intraorbital optic nerve damage in rabbits. Brain Res. 2009;1267:103–15. doi: 10.1016/j.brainres.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 7.Zhang K, Hopkins JJ, Heier JS, Birch DG, Halperin LS, Albini TA, Brown DM, Jaffe GJ, Tao W, Williams GA. Ciliary neurotrophic factor delivered by encapsulated cell intraocular implants for treatment of geographic atrophy in age-related macular degeneration. Proc Natl Acad Sci USA. 2011;108:6241–5. doi: 10.1073/pnas.1018987108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kauper K, McGovern C, Sherman S, Heatherton P, Rapoza R, Stabila P, Dean B, Lee A, Borges S, Bouchard B, Tao W. Two-year intraocular delivery of ciliary neurotrophic factor by encapsulated cell technology implants in patients with chronic retinal degenerative diseases. Invest Ophthalmol Vis Sci. 2012;53:7484–91. doi: 10.1167/iovs.12-9970. [DOI] [PubMed] [Google Scholar]
- 9.Birch DG, Bennett LD, Duncan JL, Weleber RG, Pennesi ME. Long-term follow-up of patients with retinitis pigmentosa receiving intraocular ciliary neurotrophic factor implants. Am J Ophthalmol. 2016;170:10–4. doi: 10.1016/j.ajo.2016.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sarup V, Patil K, Sharma SC. Ciliary neurotrophic factor and its receptors are differentially expressed in the optic nerve transected adult rat retina. Brain Res. 2004;1013:152–8. doi: 10.1016/j.brainres.2004.03.030. [DOI] [PubMed] [Google Scholar]
- 11.Yu S, Tanabe T, Yoshimura N. A rat model of glaucoma induced by episcleral vein ligation. Exp Eye Res. 2006;83:758–70. doi: 10.1016/j.exer.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 12.Li R, Wen R, Banzon T, Maminishkis A, Miller SS. CNTF mediates neurotrophic factor secretion and fluid absorption in human retinal pigment epithelium. PLoS One. 2011;6:e23148. doi: 10.1371/journal.pone.0023148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu X, Clark AF, Wordinger RJ. Expression of ciliary neurotrophic factor (CNTF) and its tripartite receptor complex by cells of the human optic nerve head. Mol Vis. 2007;13:758–63. [PMC free article] [PubMed] [Google Scholar]
- 14.Chowdhury UR, Madden BJ, Charlesworth MC, Fautsch MP. Proteome analysis of human aqueous humor. Invest Ophthalmol Vis Sci. 2010;51:4921–31. doi: 10.1167/iovs.10-5531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ohashi Y, Motokura M, Kinoshita Y, Mano T, Watanabe H, Kinoshita S, Manabe R, Oshiden K, Yanaihara C. Presence of epidermal growth factor in human tears. Invest Ophthalmol Vis Sci. 1989;30:1879–82. [PubMed] [Google Scholar]
- 16.Lass JH, Walter EI, Burris TE, Grossniklaus HE, Roat MI, Skelnik DL, Needham L, Singer M, Medof ME. Expression of two molecular forms of the complement decay-accelerating factor in the eye and lacrimal gland. Invest Ophthalmol Vis Sci. 1990;31:1136–48. [PubMed] [Google Scholar]
- 17.Horwath-Winter J, Kirchengast S, Meinitzer A, Wachswender C, Faschinger C, Schmut O. Determination of uric acid concentrations in human tear fluid, aqueous humour and serum. Acta Ophthalmol. 2009;87:188–92. doi: 10.1111/j.1755-3768.2008.01215.x. [DOI] [PubMed] [Google Scholar]
- 18.Dikovskaya MA, Trunov AN, Chernykh VV, Korolenko TA. Cystatin C and lactoferrin concentrations in biological fluids as possible prognostic factors in eye tumor development. Int J Circumpolar Health. 2013;72:21087. doi: 10.3402/ijch.v72i0.21087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chernyavskaya MA, Efremov AV, Chernykh VV, Pustovetova MG. Content of matrix metalloproteinase-9 in the lacrimal and intraocular liquids in choroidal melanoma [in Russian]. Sibirskii Nauchnyi Med Zhurn 2015; 35:16–20.
- 20.Chernyavskaya MA, Efremov AV, Chernykh VV. Interrelation of cytokines in the lacrimal and intraocular fluid in melanoma of the choroid [in Russian]. Vestnik TGU 2015; 20:710–2.
- 21.Shpak AA, Guekht AB, Druzhkova TA, Kozlova KI, Golovin AV, Gulyaeva NV. Ciliary neurotrophic factor in patients with age-related cataract. Neurochem J. 2015;9:311–4. [Google Scholar]
- 22.Shpak AA, Guekht AB, Druzhkova TA, Kozlova KI, Golovin AV, Gulyaeva NV. Brain-derived neurotrophic factor in patients with age-related cataract. Neurochem J. 2016;10:240–3. [Google Scholar]
- 23.Mills RP, Budenz DL, Lee PP, Noecker RJ, Walt JG, Siegartel LR, Evans SJ, Doyle JJ. Categorizing the stage of glaucoma from pre-diagnosis to end-stage disease. Am J Ophthalmol. 2006;141:24–30. doi: 10.1016/j.ajo.2005.07.044. [DOI] [PubMed] [Google Scholar]
- 24.Riffenburgh RH. Statistics in Medicine. 2nd ed. Amsterdam, Netherlands: Elsevier Academic Press; 2005. p.121. [Google Scholar]
- 25.Fox J, Weisberg S. An R companion to applied regression. 2nd ed. Thousand Oaks (CA): SAGE Publications, Inc; 2010. p.285–328. [Google Scholar]
- 26.Zar JH. Biostatistical analysis. 5th ed. Upper Saddle River (NJ): Pearson Prentice-Hall; 2010. p.390–2. [Google Scholar]
- 27.Campbell MJ, Swinscow TDV. Statistics at square one. 11th ed. Chichester: John Wiley & Sons Ltd; 2009. p.123. [Google Scholar]
- 28.Huston C, Juarez-Colunga E. Guidelines for computing summary statistics for data-sets containing non-detects. Bulkley Valley Research Center. 2009. [Google Scholar]
- 29.Helsel DR. Statistics for censored environmental data using Minitab and R. 2nd ed. Hoboken, New Jersey: John Wiley & Sons Inc.; 2012. [Google Scholar]
- 30.Iłzecka J. Increased serum CNTF level in patients with amyotrophic lateral sclerosis. Eur Cytokine Netw. 2003;14:192–4. [PubMed] [Google Scholar]
- 31.Laaksovirta H, Soinila S, Hukkanen V, Röyttä M, Soilu-Hänninen M. Serum level of CNTF is elevated in patients with amyotrophic lateral sclerosis and correlates with site of disease onset. Eur J Neurol. 2008;15:355–9. doi: 10.1111/j.1468-1331.2008.02080.x. [DOI] [PubMed] [Google Scholar]
- 32.Pollreisz A, Funk M, Breitwieser FP, Parapatics K, Sacu S, Georgopoulos M, Dunavoelgyi R, Zlabinger GJ, Colinge J, Bennett KL, Schmidt-Erfurth U. Quantitative proteomics of aqueous and vitreous fluid from patients with idiopathic epiretinal membranes. Exp Eye Res. 2013;108:48–58. doi: 10.1016/j.exer.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 33.Kliuchnikova AA, Samokhina NI, Ilina IY, Karpov DS, Pyatnitskiy MA, Kuznetsova KG, Toropygin IY, Kochergin SA, Alekseev IB, Zgoda VG, Archakov AI, Moshkovskii SA. Human aqueous humor proteome in cataract, glaucoma, and pseudoexfoliation syndrome. Proteomics. 2016;16:1938–46. doi: 10.1002/pmic.201500423. [DOI] [PubMed] [Google Scholar]
- 34.Pease ME, Zack DJ, Berlinicke C, Bloom K, Cone F, Wang Y, Klein RL, Hauswirth WW, Quigley HA. Effect of CNTF on retinal ganglion cell survival in experimental glaucoma. Invest Ophthalmol Vis Sci. 2009;50:2194–200. doi: 10.1167/iovs.08-3013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Flachsbarth K, Kruszewski K, Jung G, Jankowiak W, Riecken K, Wagenfeld L, Richard G, Fehse B, Bartsch U. Neural stem cell-based intraocular administration of ciliary neurotrophic factor attenuates the loss of axotomized ganglion cells in adult mice. Invest Ophthalmol Vis Sci. 2014;55:7029–39. doi: 10.1167/iovs.14-15266. [DOI] [PubMed] [Google Scholar]
- 36.Shpak AA, Gavrilova NA, Lanevskaya NI, Degtyareva MV. Brain-derived neurotrophic factor in patients with primary glaucoma. Curr Eye Res. 2006;4:14–6. in Russian. [Google Scholar]
- 37.Zhang W, Prausnitz MR, Edwards A. Model of transient drug diffusion across cornea. J Control Release. 2004;99:241–58. doi: 10.1016/j.jconrel.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 38.Noma H, Funatsu H, Mimura T, Harino S, Hori S. Aqueous humor levels of vasoactive molecules correlate with vitreous levels and macular edema in central retinal vein occlusion. Eur J Ophthalmol. 2010;20:402–9. doi: 10.1177/112067211002000222. [DOI] [PubMed] [Google Scholar]
- 39.Kuiper J, Ten Dam-van Loon N, Domanian A, Schellekens P, Nierkens S, Radstake T, de Boer J. Correlation between measurement of IL-10 and IL-6 in paired aqueous humour and vitreous fluid in primary vitreoretinal lymphoma. Acta Ophthalmol. 2015;93:e680–1. doi: 10.1111/aos.12733. [DOI] [PubMed] [Google Scholar]
- 40.Ecker SM, Hines JC, Pfahler SM, Glaser BM. Aqueous cytokine and growth factor levels do not reliably reflect those levels found in the vitreous. Mol Vis. 2011;17:2856–63. [PMC free article] [PubMed] [Google Scholar]