Abstract
Background
Ambulatory blood pressure (BP) monitoring (ABPM) is the reference standard for out-of-clinic BP measurement. Thresholds for identifying ambulatory hypertension (daytime systolic BP [SBP]/diastolic BP [DBP] ≥ 135/85 mmHg, 24-hour SBP/DBP ≥ 130/80 mmHg, and nighttime SBP/DBP ≥ 120/70 mmHg) have been derived from European, Asian and South American populations. We determined BP thresholds for ambulatory hypertension in a US population-based sample of African Americans.
Methods
We analyzed data from the Jackson Heart Study (JHS), a population-based cohort study comprised exclusively of African-American adults (n=5,306). Analyses were restricted to 1,016 participants who completed ABPM at baseline in 2000-2004. Mean systolic BP (SBP) and diastolic BP (DBP) levels were calculated for daytime (10:00am-8:00pm), 24-hour (all available readings) and nighttime (midnight-6:00am) periods, separately. Daytime, 24-hour, and nighttime BP thresholds for ambulatory hypertension were identified using regression- and outcome-derived approaches. The composite of a cardiovascular disease (CVD) or all-cause mortality event was used in the outcome-derived approach. For this latter approach, BP thresholds were identified only for SBP as clinic DBP was not associated with the outcome. Analyses were stratified by antihypertensive medication use.
Results
Among participants not taking antihypertensive medication, the regression-derived thresholds for daytime, 24-hour, and nighttime SBP/DBP corresponding to clinic SBP/DBP of 140/90 mmHg were 134/85 mmHg, 130/81 mmHg, and 123/73 mmHg, respectively. The outcome-derived thresholds for daytime, 24-hour, and nighttime SBP corresponding to a clinic SBP ≥ 140 mmHg were 138 mmHg, 134 mmHg, and 129 mmHg, respectively. Among participants taking antihypertensive medication, the regression-derived thresholds for daytime, 24-hour, and nighttime SBP/DBP corresponding to clinic SBP/DBP of 140/90 mmHg were 135/85 mmHg, 133/82 mmHg, and 128/76 mmHg, respectively. The corresponding outcome-derived thresholds for daytime, 24-hour, and nighttime SBP were 140 mmHg, 137 mmHg, and 133 mmHg, respectively, among those taking antihypertensive medication.
Conclusions
Based on the outcome-derived approach for SBP and regression-derived approach for DBP, the following definitions for daytime hypertension, 24-hour hypertension, and nighttime hypertension corresponding to clinic SBP/DBP ≥ 140/90 mmHg are proposed for African Americans: daytime SBP/DBP ≥ 140/85 mmHg, 24-hour SBP/DBP ≥ 135/80 mmHg, and nighttime SBP/DBP ≥ 130/75 mmHg, respectively.
Keywords: ambulatory blood pressure monitoring, African Americans
Introduction
The 2015 US Preventive Services Task Force (USPSTF) recommendation on screening for high blood pressure (BP) suggests using out-of-clinic BP measurements to confirm diagnoses of hypertension made in the clinic setting.1 Ambulatory BP monitoring (ABPM) is the most commonly recommended approach for out-of-office BP measurement.2,3 In addition to confirming the diagnosis of hypertension, ABPM can be used to determine BP control among individuals taking antihypertensive medication as well as identify BP phenotypes including masked and nocturnal hypertension.3,4 Several guidelines, scientific statements, and position papers have proposed BP thresholds for identifying ambulatory hypertension.3,5-8 These thresholds were primarily derived from population-based studies of European, Japanese, and South-American populations.
African Americans, a group with high risk for cardiovascular disease (CVD) outcomes, have higher mean daytime and nighttime ambulatory BP compared to whites.9-11 The applicability of ABPM thresholds derived in European, Japanese, and South-American populations to African Americans is unclear. In the current study, we used data from the Jackson Heart Study (JHS), a population-based cohort comprised exclusively of African American adults to determine ambulatory daytime, 24-hour and nighttime BP thresholds that correspond to different clinic BP thresholds. Additionally, we identified BP thresholds on ABPM that provide similar probability of CVD or all-cause mortality events as these clinic BP thresholds.
Methods
Study Population
The JHS is a population-based prospective cohort study designed to identify CVD risk factors among African Americans.12 The JHS enrolled 5,306 non-institutionalized African Americans, aged ≥21 years, between 2000 and 2004. Participants were recruited from the Atherosclerosis Risk in the Community (ARIC) site in Jackson, MS, and a representative sample of urban and rural Jackson, Mississippi metropolitan tri-county (Hinds, Madison and Rankin counties) residents, volunteers, randomly selected individuals, and secondary family members.12,13 The current analysis was restricted to 1,148 JHS participants who completed ABPM as part of their baseline study visit (Visit 1 2000-2004). Participants (n=132) who did not meet the International Database on ABPM in relation to Cardiovascular Outcomes (IDACO) criteria for valid ABPM (n=102; described below) or who were missing information on clinic BP or antihypertensive medication use (n=30) were excluded from the analyses. After these exclusions were applied, the final analytical sample size was 1,016 participants.
The institutional review boards of the University of Mississippi Medical Center, Jackson State University, and Tougaloo College approved the JHS protocol. The current analysis of JHS data was approved by the institutional review board at the University of Alabama at Birmingham. All participants provided written informed consent.
Data Collection
A detailed description of the methodology and data collection procedures for the baseline visit in the JHS have been described elsewhere.13-17 Briefly, data were collected during an in-home interview, clinic examination, and by ABPM. ABPM was an optional procedure that participants were invited to complete. Of relevance to the current analysis, during the in-home interview, self-reported information was collected on socio-demographics, health behaviors (e.g., alcohol consumption, current smoking), prior diagnoses of co-morbid conditions and antihypertensive medication use (see Supplemental Methods). During the clinic examination, trained technicians measured height, weight and BP, collected blood and urine samples, and conducted 2D echocardiography. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Using specimens collected during the study visit, low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol, serum creatinine, urine albumin and creatinine, fasting serum glucose, and glycated hemoglobin (HbA1c) were measured. Estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation18 and albumin-to-creatinine ratio was also calculated. Diabetes was defined by a fasting blood glucose ≥ 126 mg/dL, HbA1c ≥ 6.5% or a prior diagnosis of diabetes with use of glucose lowering medication.
Clinic BP measurement
Clinic BP was measured by trained staff using a random zero sphygmomanometer (Hawksley and Sons Ltd., Lancing, UK) during the baseline study visit. Each participant’s right arm circumference was measured to determine the appropriate cuff size. After participants had rested for at least 5 minutes in an upright position with their back and arms supported, feet flat on the floor and legs uncrossed, two BP measurements in the right arm, separated by one minute, were recorded. The mean of these clinic BP measurements was calculated. Quality control was conducted by the JHS Coordinating Center by monitoring digit preference for each staff member and by comparing the mean BP level measured within and between study staff. A BP comparability substudy was conducted in which BP was measured simultaneously, using a Y connector, by random zero sphygmomanometer and an Omron HEM-907XL device, a semi-automated device. As described in the Supplement (see Methods and Supplemental Figure 1) and in prior analyses of the JHS, the random-zero BP measurements were calibrated to the semi-automated device using robust regression.13,17 Elevated clinic BP was defined as mean clinic systolic BP (SBP) ≥ 140 mmHg or mean clinic diastolic BP (DBP) ≥ 90 mmHg.
ABPM
After completing the clinic examination, participants were given the opportunity to complete ABPM for 24 hours. Participants who consented were fitted with an ABPM device (Spacelabs 90207, Spacelabs, Redmond, WA) on their non-dominant arm. BP was recorded every 20 minutes. After 24 hours, the device was removed and data were downloaded onto a computer and processed with Medifacts International’s Medicom software (Rockville, MD). IDACO criteria were used to define a complete ABPM measurement, which is defined as ≥ 10 daytime (10:00 to 20:00) and ≥ 5 nighttime (00:00 to 06:00) SBP and DBP measurements.19 The mean SBP and DBP levels were calculated for the daytime, nighttime and 24-hour periods, separately.
CVD events and all-cause mortality
The adjudication procedures for CVD events and all-cause mortality have been described previously.20 Briefly, living participants or their proxies were contacted annually via telephone to assess potential CVD events and vital status. Hospital lists for discharges with specific diagnosis criteria were also obtained from the Jackson, Mississippi tri-county area hospitals. Death certificates were requested from the Mississippi State Department of Health for JHS participants as needed. When a CVD-related hospitalization or a death was identified, medical records were retrieved and abstracted. Trained clinicians adjudicated events following published guidelines using the information available about the circumstance surrounding an event.20 For the current analysis, definite or probable CVD events (i.e., coronary heart disease, nonfatal myocardial infarction or acute coronary heart disease death or stroke defined as non-carotid embolic or thrombotic brain infarction, brain hemorrhage or subarachnoid hemorrhage) and all-cause mortality were available through December 31, 2012.
Statistical Analyses
Characteristics of the participants included in the analytical sample (n=1,016), the sample who underwent ABPM but were excluded from the analysis (n=132), and non-ABPM sample (n=4,158) were calculated. All subsequent analyses were weighted to the age and sex distribution of African Americans adults using data from the 2010 US Census.21 Characteristics were calculated for the overall sample, and participants taking and not taking antihypertensive medication, separately. We used three approaches used in previous ABPM studies to identify thresholds for ambulatory hypertension: a distribution-derived approach, a regression-derived approach, and an outcome-derived approach.22-31 All of these analyses were conducted stratified by antihypertensive medication use. The three approaches described below for determining daytime BP thresholds were repeated for 24-hour, and separately, nighttime BP. All analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
Distribution-derived approach
The goal of the distribution-derived approach is to identify percentiles of the BP distribution on ABPM for a population.22,24,27,30-32 The distributions of clinic and daytime SBP, and separately clinic and daytime DBP, were calculated. The 90th, 95th and 99th percentiles of the daytime SBP and DBP distributions were identified using quantile regression. The 95% confidence interval was calculated by computing a Huber sandwich estimate using a local estimate of the sparsity function. The percentage of participants with clinic SBP ≥ 140 mmHg, and clinic DBP ≥ 90 mmHg was calculated for those with daytime SBP and DBP greater than or equal to these BP percentiles.
Regression-derived approach
The goal of the regression-derived approach is to identify the BP levels on ABPM that correspond to specific clinic BP levels.22,23,26,29 Using the intercept and beta coefficient from a linear regression model with clinic SBP as the outcome and daytime SBP as the independent variable, the level of daytime SBP and 95% confidence interval corresponding to clinic BP level of 140 mmHg were identified. Distribution curves were plotted to show the percentage of participants with clinic SBP at or above 140 mmHg and with daytime SBP at or above the thresholds from ABPM corresponding to clinic SBP of 140 mmHg. Daytime SBP levels corresponding to clinic SBP of 120 mmHg, 130 mmHg, and 160 mmHg were also determined. We used the same approach to determine daytime DBP levels corresponding with clinic DBP of 80 mmHg, 85 mmHg, and 100 mmHg.
Outcome-derived approach
The goal of the outcome-derived approach is to identify the threshold for ambulatory BP that corresponds to the same probability of an event associated with a clinic BP level (e.g., SBP of ≥ 140 mmHg).25,28 Higher clinic SBP was statistically significantly associated with the composite of CVD or all-cause mortality (p<0.001) but clinic DBP was not (p=0.121). Therefore, thresholds for ambulatory SBP but not DBP thresholds were calculated. Thresholds for daytime SBP yielding similar 5-year predicted probability of a CVD event or all-cause mortality associated with clinic SBP ≥ 140 mmHg were first calculated. To do this, we performed Cox regression with the composite outcome of CVD or mortality and clinic SBP as the independent variable. We identified the 5-year predicted probability of CVD or mortality for a clinic BP level of 140 mmHg. Next, we conducted a Cox regression model with the outcome of CVD/all-cause mortality and daytime SBP as the independent variable. From this latter model, we determined the daytime SBP value that corresponded to the 5-year predicted probability of the outcome for a clinic SBP level of 140 mmHg (i.e., from the first Cox model described above). A bootstrap with 1,000 data sets was used to calculate a 95% confidence interval for the daytime SBP yielding a similar 5-year predicted probability of the composite CVD/all-cause mortality outcome. Daytime SBP levels yielding similar 5-year predicted probability of an outcome associated with clinic SBP ≥ 120 mmHg, ≥ 130 mmHg, and ≥ 160 mmHg were also calculated.
Comparisons with recommended ambulatory BP thresholds
In scientific statements, guidelines and position papers, ambulatory hypertension has been defined as having daytime SBP/DBP ≥ 135/85 mmHg, 24-hour SBP/DBP ≥ 130/80 mmHg, and/or nighttime SBP/DBP ≥ 120/70 mmHg.3,5-8 We graphed the thresholds identified using the distribution-derived approach (95th percentile of BP), regression-derived approach (corresponding to clinic SBP/DBP of 140/90 mmHg), and outcome-derived approach (corresponding to clinic SBP of 140 mmHg) and contrasted them with these previously published thresholds.
Results
Characteristics of the Jackson Heart Study participants included in the analytical sample (n=1,016), the sample who underwent ABPM but were excluded from the analysis (n=132), and non-ABPM sample (n=4,158) are shown in Supplemental Table 1. The mean age ± standard deviation of participants in the analytical sample weighted to the 2010 US African American adult population was 50.5 ± 11.2 years; 55.2% were female and 38.9% were taking antihypertensive medication (Table 1). Participants taking antihypertensive medication were older and more likely to be female, have less than a high school education, diabetes, eGFR < 60 ml/min/1.73 m2, urine albumin-to-creatinine ratio ≥ 30 mg/g, and not drink alcohol compared with those not taking antihypertensive medication. Additionally, mean BMI was higher while LDL-cholesterol was lower among those taking versus not taking antihypertensive medication. Clinic, daytime, nighttime and 24-hour SBP were each higher among participants taking versus not taking antihypertensive medication while no differences were present for DBP.
Table 1.
Characteristics of Jackson Heart Study participants with ambulatory blood pressure monitoring at baseline included in the current analysis.
| Overall | Taking Antihypertensive Medication | ||
|---|---|---|---|
| n=1,016 | No n=441 | Yes n=575 | |
| Demographic Characteristics | |||
| Age, years | 50.5 ± 11.2 | 47.1 ± 11.2 | 55.7 ± 9.7 |
| Female sex, % | 55.2% | 49.6% | 64.0% |
| Education < high school, % | 11.8% | 8.9% | 16.5% |
| Clinical Characteristics | |||
| Body mass index, kg/m2 | 31.2 ± 6.6 | 30.2 ± 7.6 | 32.6 ± 5.5 |
| Diabetes, % | 17.2% | 7.8% | 32.4% |
| LDL cholesterol, mg/dL | 124.7 ± 35.7 | 126.2 ± 43.3 | 122.2 ± 28.1 |
| HDL cholesterol, mg/dL | 51.0 ± 13.6 | 50.9 ± 15.1 | 51.1 ± 12.4 |
| Estimated glomerular filtration rate < 60 ml/min/1.73 m2, % | 4.7% | 1.1% | 10.2% |
| Albumin to creatinine ratio ≥ 30 mg/g, % | 9.5% | 5.3% | 16.6% |
| Health Behaviors | |||
| Alcohol use, % | |||
| Non-drinker | 51.3% | 45.6% | 60.4% |
| Moderate drinker | 43.5% | 48.6% | 35.5% |
| Heavy drinker | 5.1% | 5.8% | 4.1% |
| Current Smoking, % | 13.0% | 13.7% | 11.9% |
| Clinic blood pressure, mmHg | |||
| Clinic systolic blood pressure | 124.4 ± 14.8 | 121.6 ± 17.2 | 128.7 ± 11.9 |
| Clinic diastolic blood pressure | 76.1 ± 8.3 | 76.2 ± 9.6 | 75.8 ± 7.1 |
| Ambulatory blood pressure, mmHg | |||
| Daytime systolic ambulatory blood pressure | 127.2 ± 12.8 | 124.8 ± 13.6 | 130.9 ± 11.4 |
| Daytime diastolic ambulatory blood pressure | 79.5 ± 9.0 | 79.3 ± 9.9 | 79.9 ± 8.3 |
| 24-hour systolic ambulatory blood pressure | 123.5 ± 12.9 | 120.7 ± 13.6 | 127.9 ± 11.5 |
| 24-hour diastolic ambulatory blood pressure | 75.4 ± 8.7 | 74.8 ± 9.5 | 76.2 ± 8.0 |
| Nighttime systolic ambulatory blood pressure | 117.5 ± 14.6 | 114.2 ± 15.1 | 122.7 ± 13.1 |
| Nighttime diastolic ambulatory blood pressure | 68.8 ± 9.5 | 67.7 ± 10.4 | 70.5 ± 8.7 |
Characteristics are weighted to the age-sex distribution for the African American adult population using 2010 US census data. Unweighted characteristics for the overall sample (n=1,016) are reported in Supplemental Table 1.
Numbers in the table are percentages or mean ± standard deviation.
HDL: high-density lipoprotein cholesterol.
LDL: low-density lipoprotein cholesterol.
Distribution-derived Approach to Determine Ambulatory BP Thresholds
Among participants not taking antihypertensive medication, the 90th percentile, 95th percentile, and 99th percentile thresholds for daytime SBP were 138 mmHg, 144 mmHg, and 158 mmHg, respectively (Table 2). Among participants at or above the 90th percentile, 95th percentile, and 99th percentile thresholds for daytime SBP, 47.6%, 55.9%, and 100.0% had clinic SBP ≥ 140 mmHg, respectively. Among participants not taking antihypertensive medication, the 90th percentile, 95th percentile, and 99th percentile thresholds for daytime DBP was 91 mmHg, 94 mmHg, and 99 mmHg, respectively. Among participants at or above the 90th percentile, 95th percentile, and 99th percentile thresholds for daytime DBP, 24.9%, 27.8%, and 55.1% had clinic DBP ≥ 90 mmHg, respectively. The 90th, 95th, and 99th percentile thresholds for daytime, 24-hour, and nighttime SBP and DBP were higher for participants taking versus not taking antihypertensive medication.
Table 2.
Percentage of participants with elevated clinic systolic and diastolic blood pressure among those with ambulatory systolic and diastolic blood pressure at or above the 90th, 95th and 99th percentiles, stratified by antihypertensive medication use.
| Ambulatory SBP Threshold (95% CI), mmHg | % with elevated clinic SBP (≥140 mmHg) | Ambulatory DBP Threshold (95% CI), mmHg | % with elevated clinic DBP (≥90 mmHg) | ||
|---|---|---|---|---|---|
| Not taking antihypertensive medication | |||||
| Daytime SBP | Daytime DBP | ||||
| 90th percentile | 138 (135-140) | 47.6% | 90th percentile | 91 (90-92) | 24.9% |
| 95th percentile | 144 (137-151) | 55.9% | 95th percentile | 94 (93-95) | 27.8% |
| 99th percentile | 158 (134-182) | 100.0% | 99th percentile | 99 (98-99) | 55.1% |
| 24-hour SBP | 24-hour DBP | ||||
| 90th percentile | 133 (130-136) | 48.2% | 90th percentile | 86 (84-87) | 33.2% |
| 95th percentile | 140 (134-146) | 72.2% | 95th percentile | 88 (85-91) | 65.1% |
| 99th percentile | 152 (123-181) | 100.0% | 99th percentile | 95 (91-100) | 44.5% |
| Nighttime SBP | Nighttime DBP | ||||
| 90th percentile | 129 (125-133) | 41.7% | 90th percentile | 80 (77-83) | 32.0% |
| 95th percentile | 137 (132-142) | 50.6% | 95th percentile | 84 (81-88) | 51.5% |
| 99th percentile | 147 (113-181) | 83.7% | 99th percentile | 93 (89-97) | 53.8% |
| Taking antihypertensive medication | |||||
| Daytime SBP | Daytime DBP | ||||
| 90th percentile | 149 (145-152) | 41.1% | 90th percentile | 93 (92-93) | 7.8% |
| 95th percentile | 155 (150-159) | 40.7% | 95th percentile | 99 (98-100) | 0% |
| 99th percentile | 163 (153-173) | 48.0% | 99th percentile | 104 (102-106) | 0% |
| 24-hour SBP | 24-hour DBP | ||||
| 90th percentile | 146 (142-150) | 45.6% | 90th percentile | 90 (86-93) | 7.7% |
| 95th percentile | 152 (147-156) | 53.7% | 95th percentile | 95 (92-98) | 2.0% |
| 99th percentile | 164 (153-175) | 66.8% | 99th percentile | 103 (99-107) | 0% |
| Nighttime SBP | Nighttime DBP | ||||
| 90th percentile | 144 (140-148) | 49.0% | 90th percentile | 84 (80-88) | 4.7% |
| 95th percentile | 149 (141-157) | 48.3% | 95th percentile | 91 (87-94) | 4.1% |
| 99th percentile | 166 (153-178) | 42.1% | 99th percentile | 101 (96-106) | 0% |
Results are weighted to the age-sex distribution for the African American adult population using 2010 US census data.
CI: confidence interval.
DBP: diastolic blood pressure.
SBP: systolic blood pressure.
Regression-derived Approach to Determine Ambulatory BP Thresholds
Among participants not taking antihypertensive medication, daytime, 24-hour, and nighttime thresholds corresponding to clinic SBP/DBP of 140/90 mmHg were 134/85 mmHg, 130/81 mmHg, and 123/73 mmHg, respectively (Table 3). A higher percentage of participants had daytime SBP ≥ 134 mmHg, 24-hour SBP ≥ 130 mmHg, and nighttime SBP ≥ 123 mmHg than clinic SBP ≥ 140 mmHg (Figure 1). Also, a higher percentage of participants had daytime DBP ≥ 85 mmHg, 24-hour DBP ≥ 81 mmHg, and nighttime DBP ≥ 73 mmHg than clinic DBP ≥ 90 mmHg. Similar results were observed among participants taking antihypertensive medication (Supplemental Figure 2). Daytime, 24-hour, and nighttime thresholds corresponding to clinic SBP/DBP of 120/80 mmHg, 130/85 mmHg, and 160/100 mmHg among participants not taking antihypertensive medication are shown in Table 3 and Figure 2. Daytime, 24-hour, and nighttime SBP thresholds corresponding to clinic SBP of 120 mmHg, 130 mmHg, and 140 mmHg were higher among participants taking versus those not taking antihypertensive medication (Table 3 and Supplemental Figure 3). Among participants taking versus those not taking antihypertensive medication, SBP thresholds corresponding to clinic SBP of 160 mmHg were similar for the daytime and 24-hour period, and higher for the nighttime period. Daytime, 24-hour, and nighttime DBP thresholds were similar among participants taking versus not taking antihypertensive medication.
Table 3.
Daytime, 24-hour, and nighttime systolic and diastolic blood pressure thresholds corresponding to clinic systolic of 160, 140, 130 and 120 mm Hg and clinic diastolic blood pressure of 100, 90, 85 and 80 mm Hg among participants not taking and taking antihypertensive medication.
| Ambulatory blood pressure thresholds (95% CI) corresponding with specified clinic SBP/DBP levels, mmHg | ||||
|---|---|---|---|---|
| Not taking antihypertensive medication | Taking antihypertensive medication | |||
| Clinic SBP 160 mmHg | Clinic DBP 100 mmHg | Clinic SBP 160 mmHg | Clinic DBP 100 mmHg | |
| Daytime SBP/DBP | 144 (142-146) | 90 (88-92) | 143 (141-146) | 89 (87-92) |
| 24-hour SBP/DBP | 140 (138-142) | 86 (83-88) | 142 (139-144) | 86 (84-88) |
| Nighttime SBP/DBP | 133 (130-136) | 77 (74-79) | 137 (134-140) | 80 (77-82) |
| Clinic SBP 140 mmHg | Clinic DBP 90 mmHg | Clinic SBP 140 mmHg | Clinic DBP 90 mmHg | |
| Daytime SBP/DBP | 134 (133-135) | 85 (84-87) | 135 (134-137) | 85 (84-87) |
| 24-hour SBP/DBP | 130 (129-131) | 81 (80-82) | 133 (132-134) | 82 (80-83) |
| Nighttime SBP/DBP | 123 (121-125) | 73 (71-74) | 128 (126-129) | 76 (74-77) |
| Clinic SBP 130 mmHg | Clinic DBP 85 mmHg | Clinic SBP 130 mmHg | Clinic DBP 85 mmHg | |
| Daytime SBP/DBP | 129 (128-130) | 83 (82-84) | 131 (130-132) | 83 (82-85) |
| 24-hour SBP/DBP | 125 (124-126) | 79 (78-80) | 128 (127-129) | 80 (79-81) |
| Nighttime SBP/DBP | 118 (117-119) | 71 (70-72) | 123 (122-124) | 74 (73-75) |
| Clinic SBP 120 mmHg | Clinic DBP 80 mmHg | Clinic SBP 120 mmHg | Clinic DBP 80 mmHg | |
| Daytime SBP/DBP | 124 (123-125) | 81 (80-82) | 127 (126-129) | 82 (81-82) |
| 24-hour SBP/DBP | 120 (119-121) | 77 (76-77) | 124 (123-125) | 78 (77-79) |
| Nighttime SBP/DBP | 113 (112-114) | 69 (68-70) | 119 (117-120) | 72 (71-73) |
Results are weighted to the age-sex distribution for the African American adult population using 2010 US census data.
CI: confidence interval.
DBP: diastolic blood pressure.
SBP: systolic blood pressure.
Figure 1.
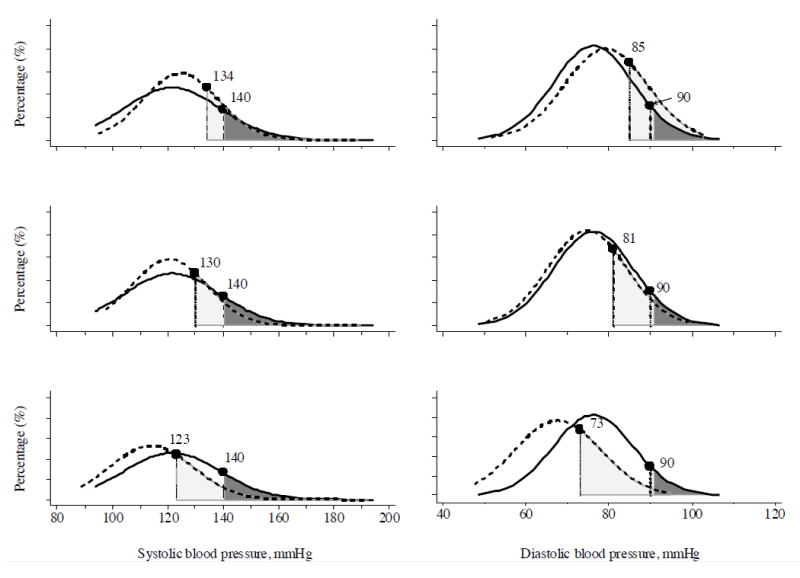
Daytime, 24-hour, and nighttime blood pressure thresholds corresponding to a clinic systolic blood pressure/diastolic blood pressure threshold of 140/90 mmHg determined using the regression-derived approach in participants not taking antihypertensive medication. Dash line represents the distribution of ambulatory blood pressure. Solid line represents the distribution of clinic blood pressure. Light gray shaded regions indicate the participants with daytime, 24-hour, and nighttime blood pressure at or above the thresholds corresponding to clinic systolic blood pressure/diastolic blood pressure of 140/90 mmHg. Dark gray shaded regions indicate the participants with clinic systolic blood pressure/diastolic blood pressure at or above the thresholds of 140/90 mmHg.
Figure 2.
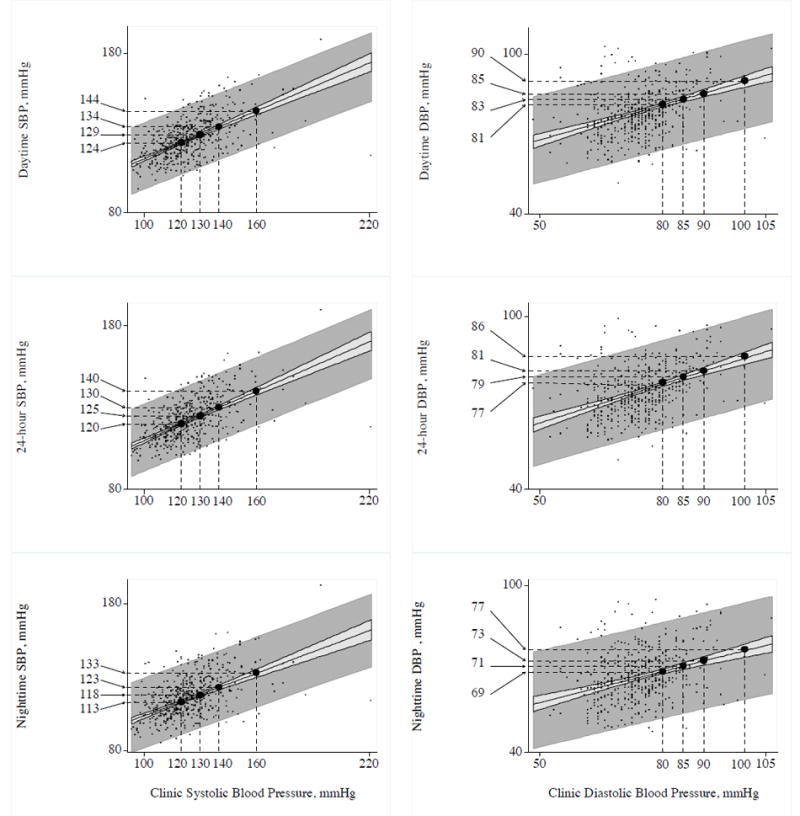
Daytime, 24-hour, and nighttime blood pressure thresholds corresponding to a clinic systolic blood pressure/diastolic blood pressure threshold of 120/80 mmHg, 130/85 mmHg, 140/90 mmHg, and 160/100 mmHg determined using the regression-derived approach in participants not taking antihypertensive medication. Light gray area represents 95% confidence interval bands. Dark gray area represents 95% prediction bands. DBP: diastolic blood pressure; SBP: systolic blood pressure.
Outcome-derived Approach to Determine Ambulatory BP Thresholds
There were 165 events (n=80 CVD events and n=85 deaths) over a median 10.8 years of follow-up. The 5-year predicted probability of a CVD or all-cause mortality event was higher at increasing levels of clinic SBP (Table 4). Among participants not taking antihypertensive medication, daytime, 24-hour, and nighttime SBP thresholds corresponding to clinic SBP of 140 mmHg were 138 mmHg, 134 mmHg, and 129 mmHg, respectively. Among participants taking antihypertensive medication, daytime, 24-hour, and nighttime SBP thresholds corresponding to clinic SBP of 140 mmHg were 140 mmHg, 137 mmHg, and 133 mmHg, respectively. Among participants taking versus not taking antihypertensive medication, daytime and 24-hour SBP thresholds were higher for clinic SBP thresholds of 160 mmHg and similar for clinic SBP thresholds of 120 mmHg and 130 mmHg. Finally, among participants taking versus not taking antihypertensive medication, nighttime SBP thresholds were higher for clinic SBP thresholds of 120 mmHg, 130 mmHg, and 160 mmHg.
Table 4.
Daytime, 24-hour, and nighttime systolic blood pressure thresholds yielding an equivalent 5-year predicted probability of the composite outcome of cardiovascular disease or all-cause mortality as clinic systolic blood pressure thresholds of 160 mmHg, 140 mmHg, 130 mmHg, and 120 mmHg.
| Clinic SBP threshold | 5-year predicted probability of CVD/all-cause mortality, % | Daytime SBP (95% CI), mmHg | 24-hour SBP (95% CI), mmHg | Nighttime SBP (95% CI), mmHg |
|---|---|---|---|---|
| Not taking antihypertensive medication | ||||
| 160 mmHg | 10.2 (4.4 - 21.1) | 148 (140 - 157) | 144 (136 - 152) | 140 (132 - 152) |
| 140 mmHg | 4.3 (2.0 - 8.3) | 138 (130 - 146) | 134 (126 - 142) | 129 (120 - 139) |
| 130 mmHg | 2.7 (1.3 - 5.4) | 133 (124 - 141) | 129 (121 - 137) | 123 (114 - 132) |
| 120 mmHg | 1.8 (0.8 - 3.7) | 128 (118 - 137) | 124 (116 - 133) | 117 (108 - 127) |
| Taking antihypertensive medication | ||||
| 160 mmHg | 9.0 (5.4 - 13.8) | 152 (143 - 166) | 148 (140 - 159) | 145 (136 - 156) |
| 140 mmHg | 5.9 (4.2 – 8.0) | 140 (129 - 151) | 137 (127 - 146) | 133 (123 - 142) |
| 130 mmHg | 4.8 (3.3 - 6.5) | 134 (120 - 144) | 131 (120 - 140) | 127 (116 - 137) |
| 120 mmHg | 3.8 (2.5 - 5.6) | 127 (109 - 138) | 125 (112 - 135) | 121 (107 - 131) |
Results are weighted to the age-sex distribution for the African American adult population using 2010 US census data.
BP: blood pressure.
CI: confidence interval.
CVD: cardiovascular disease.
SBP: systolic blood pressure.
Comparisons with Published Recommendations
Thresholds defined by the 95th percentile of the population distribution and the outcome-derived approach were higher than those from published recommendations3,5-8 for daytime BP, 24-hour BP, and nighttime BP among participants not taking and taking antihypertensive medication (Figure 3 and Supplemental Figure 4). Thresholds determined using the regression-derived approach were similar to published recommendations3,5-8 for daytime BP and 24-hour BP, and higher for nighttime BP among participants not taking and taking antihypertensive medication.
Figure 3.
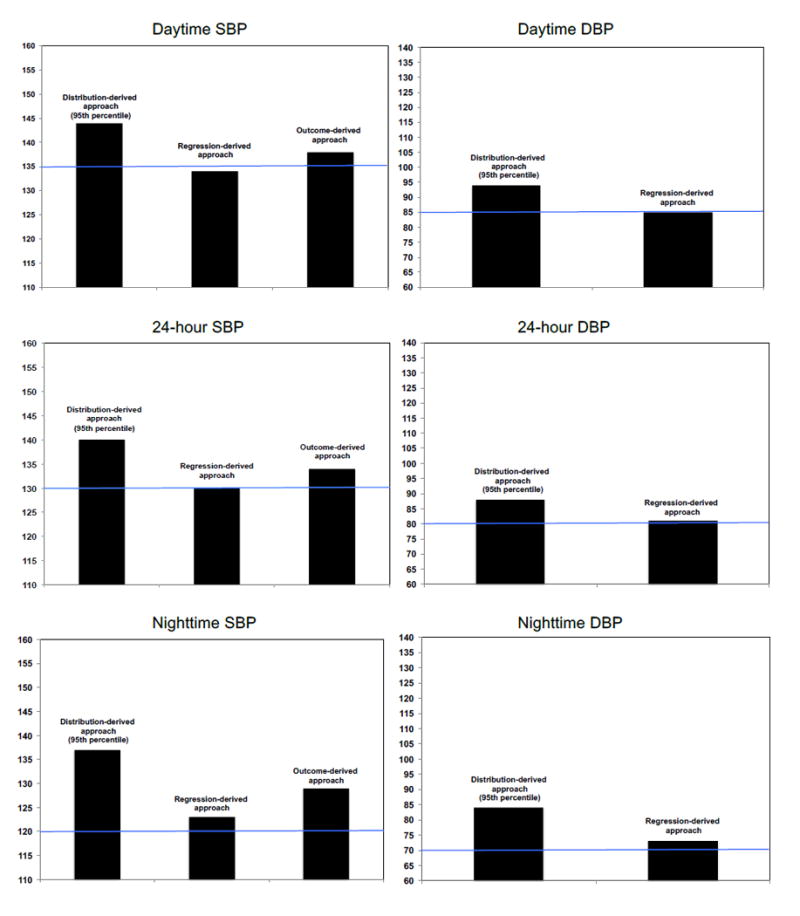
Daytime, 24-hour, and nighttime blood pressure thresholds among participants not taking antihypertensive medication compared to published recommendations3,5-8 of blood pressure thresholds for ambulatory hypertension: daytime systolic blood pressure/diastolic blood pressure ≥ 135/85 mmHg, 24-hour systolic blood pressure/diastolic blood pressure ≥ 130/80 mmHg, and nighttime systolic blood pressure/diastolic blood pressure ≥ 120/70 mmHg. Blue lines represent recommended systolic blood pressure and diastolic blood pressure thresholds. DBP: diastolic blood pressure; SBP: systolic blood pressure.
Discussion
In the current study, we identified BP thresholds for ambulatory hypertension in a US population-based sample of African Americans not taking and taking antihypertensive medication using the distribution-derived, regression-derived, and outcome-derived approaches. The ambulatory BP thresholds identified for African Americans were higher than those from published recommendations, which were based on data from European, Japanese and South American populations.3,5-8
Using the outcome-derived approach corresponding to a clinic SBP threshold of 140 mmHg, and regression-derived approach corresponding to a clinic DBP threshold of 90 mmHg, we recommend defining daytime hypertension as mean daytime SBP/DBP ≥ 140/85 mmHg, 24-hour hypertension as mean 24-hour SBP/DBP ≥ 135/80 mmHg, and nighttime hypertension as mean nighttime SBP/DBP ≥ 130/75 mmHg in African Americans. The use of these BP thresholds, which are higher than those from published recommendations, will lead to a lower prevalence of daytime, 24-hour and nighttime hypertension among African Americans. Consequently, the prevalence of white coat hypertension (i.e. clinic hypertension without ambulatory hypertension) will increase and masked hypertension (i.e. absence of clinic hypertension with ambulatory hypertension) will decrease.
An early method to derive ambulatory BP thresholds was the distribution-derived approach, commonly using the 95th percentile.22,24,27,30-32 In prior studies, thresholds using the distribution-derived approach have varied substantially from one another.24,27,30-32 These divergent findings likely reflect differences in population characteristics including the prevalence of clinic hypertension and whether the population was composed of individuals not taking and taking antihypertensive medication. Another issue with the distribution-derived approach is the assumption that a fixed percentage of the population have ambulatory hypertension. Given these limitations, the ambulatory BP thresholds we recommend do not take into consideration the thresholds determined using the distribution-derived approach.
There are several strengths of the current study. Few prior studies have conducted ABPM among African Americans, a population disproportionately affected by BP-related CVD compared with other racial/ethnic groups in the US. The relatively large sample size with ABPM in the Jackson Heart Study allowed us to determine ABPM thresholds among participants taking and not taking antihypertensive medication, separately, and for a wide range of clinic BP levels. Despite these strengths, the results should be interpreted in the context of possible limitations. Only a subset of JHS participants underwent ABPM. Further, two clinic BP readings were obtained for each participant. The BP thresholds may have differed if three or more BP measurements were obtained at the baseline visit or serial clinic BP measurements were averaged across multiple visits. Also, clinic BP was measured using a random-zero sphygmomanometer among JHS participants. However, these measurements were calibrated to an oscillometric device. Further, the ABPM cuff was placed on the participant’s non-dominant arm to minimize the effect of daily activities on BP measurement (e.g. writing, picking up objects, etc.) whereas clinic BP was measured in the right arm. Therefore, the current results may have been affected by inter-arm differences in BP measurements. Finally, data were only available for African Americans. ABPM thresholds for whites, Hispanics, and Asians in the US need to be identified among the same population to determine whether ambulatory BP thresholds differ by race/ethnicity.
In conclusion, the current study provides BP thresholds for identifying ambulatory hypertension in a US population-based sample of African Americans not taking and taking antihypertensive medication. The following ambulatory hypertension definitions corresponding to clinic SBP/DBP ≥ 140/90 mmHg are proposed: daytime hypertension defined as daytime SBP/DBP ≥ 140/85 mmHg, 24-hour hypertension defined as 24-hour SBP/DBP ≥ 135/80 mmHg, and nighttime hypertension defined as nighttime SBP/DBP ≥ 130/75 mmHg. These thresholds differ from previously published recommendations suggesting that there may be racial differences in thresholds for ambulatory BP.
Supplementary Material
Clinical Perspective.
What is new?
Ambulatory blood pressure (BP) monitoring (ABPM) is the most commonly recommended approach for out-of-office BP measurement.
Several guidelines, scientific statements, and position papers have proposed BP thresholds for identifying ambulatory hypertension on ABPM.
These thresholds were primarily derived from population-based studies of European, Japanese, and South-American populations.
We determined BP thresholds on ABPM for ambulatory hypertension in a US population-based sample of African Americans not taking and taking antihypertensive medication.
The ambulatory BP thresholds identified for African Americans were higher than those from published recommendations.
What are the clinical implications?
The use of these ABPM thresholds in African Americans will lead to a lower prevalence of daytime, 24-hour and nighttime hypertension, compared with using ABPM thresholds from published recommendations.
Therefore, these findings have important clinical implications for the diagnosis and treatment of hypertension in African Americans.
Acknowledgments
Role of Funding Sources: The Jackson Heart Study is supported and conducted in collaboration with Jackson State University (N01-HC-95170); University of Mississippi Medical Center (N01-HC-95171); and Touglaoo College (N01-HC-95172) and contracts HHSN268201300046C, HHSN268201300047C, HHSN268201300048C, HHSN268201300049C, HHSN268201300050C from the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute on Minority Health and Health Disparities (NIMHD) at the National Institutes of Health (NIH). This work was also supported by the NIH (HL047540, HL117323, HL117323-02S2, K24-HL125704) from the NHLBI, 5KL2TR001065 from the National Center for Advancing Translational Sciences, Bethesda, MD, and 15SFRN2390002 from the American Heart Association. The funding sources played no role in the design, conduct, analyses or reporting of the current study.
Footnotes
Disclosures: Dr. Paul Muntner received an institutional grant from Amgen Inc. Dr. Daichi Shimbo is a consultant for Abbott Vascular and Novartis Pharmaceuticals Corporation. Dr. Adam Bress received an institutional grant from Novartis. There are no other disclosures.
References
- 1.Siu AL. Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163:778–786. doi: 10.7326/M15-2223. [DOI] [PubMed] [Google Scholar]
- 2.Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Whitlock EP. Diagnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2015;162:192–204. doi: 10.7326/M14-1539. [DOI] [PubMed] [Google Scholar]
- 3.Shimbo D, Abdalla M, Falzon L, Townsend RR, Muntner P. Role of Ambulatory and Home Blood Pressure Monitoring in Clinical Practice: A Narrative Review. Ann Intern Med. 2015;163:691–700. doi: 10.7326/M15-1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. N Engl J Med. 2006;354:2368–2374. doi: 10.1056/NEJMra060433. [DOI] [PubMed] [Google Scholar]
- 5.Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Ryden L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 6.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111:697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 7.Pickering TG, White WB. ASH Position Paper: Home and ambulatory blood pressure monitoring. When and how to use self (home) and ambulatory blood pressure monitoring. J Clin Hypertens (Greenwich) 2008;10:850–855. doi: 10.1111/j.1751-7176.2008.00043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, vanMontfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y European Society of Hypertension Working Group on Blood Pressure M. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–1768. doi: 10.1097/HJH.0b013e328363e964. [DOI] [PubMed] [Google Scholar]
- 9.Muntner P, Lewis CE, Diaz KM, Carson AP, Kim Y, Calhoun D, Yano Y, Viera AJ, Shimbo D. Racial differences in abnormal ambulatory blood pressure monitoring measures: Results from the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Hypertens. 2015;28:640–648. doi: 10.1093/ajh/hpu193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knox SS, Hausdorff J, Markovitz JH. Coronary Artery Risk Development in Young Adults S. Reactivity as a predictor of subsequent blood pressure: racial differences in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Hypertension. 2002;40:914–919. doi: 10.1161/01.hyp.0000041417.94797.57. [DOI] [PubMed] [Google Scholar]
- 11.Profant J, Dimsdale JE. Race and diurnal blood pressure patterns. A review and meta-analysis. Hypertension. 1999;33:1099–1104. doi: 10.1161/01.hyp.33.5.1099. [DOI] [PubMed] [Google Scholar]
- 12.Sempos CT, Bild DE, Manolio TA. Overview of the Jackson Heart Study: a study of cardiovascular diseases in African American men and women. Am J Med Sci. 1999;317:142–146. doi: 10.1097/00000441-199903000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Abdalla M, Booth JN, 3rd, Seals SR, Spruill TM, Viera AJ, Diaz KM, Sims M, Muntner P, Shimbo D. Masked Hypertension and Incident Clinic Hypertension Among Blacks in the Jackson Heart Study. Hypertension. 2016;68:220–226. doi: 10.1161/HYPERTENSIONAHA.115.06904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. [March 8, 2017];Jackson Heart Study Protocol Manuals. April 2003 and September 2005. https://www.jacksonheartstudy.org/Research/Study-Design.
- 15.Carpenter MA, Crow R, Steffes M, Rock W, Heilbraun J, Evans G, Skelton T, Jensen R, Sarpong D. Laboratory, reading center, and coordinating center data management methods in the Jackson Heart Study. Am J Med Sci. 2004;328:131–144. doi: 10.1097/00000441-200409000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Taylor HA, Jr, Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ, Nelson C, Wyatt SB. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis. 2005;15:S6–4-17. [PubMed] [Google Scholar]
- 17.Diaz KM, Booth JN, 3rd, Seals SR, Abdalla M, Dubbert PM, Sims M, Ladapo JA, Redmond N, Muntner P, Shimbo D. Physical Activity and Incident Hypertension in African Americans: The Jackson Heart Study. Hypertension. 2017;69:421–427. doi: 10.1161/HYPERTENSIONAHA.116.08398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J, Ckd EPI. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thijs L, Hansen TW, Kikuya M, Bjorklund-Bodegard K, Li Y, Dolan E, Tikhonoff V, Seidlerova J, Kuznetsova T, Stolarz K, Bianchi M, Richart T, Casiglia E, Malyutina S, Filipovsky J, Kawecka-Jaszcz K, Nikitin Y, Ohkubo T, Sandoya E, Wang J, Torp-Pedersen C, Lind L, Ibsen H, Imai Y, Staessen JA, O’Brien E, Investigators I. The International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO): protocol and research perspectives. Blood Press Monit. 2007;12:255–262. doi: 10.1097/mbp.0b013e3280f813bc. [DOI] [PubMed] [Google Scholar]
- 20.Keku E, Rosamond W, Taylor HA, Jr, Garrison R, Wyatt SB, Richard M, Jenkins B, Reeves L, Sarpong D. Cardiovascular disease event classification in the Jackson Heart Study: methods and procedures. Ethn Dis. 2005;15:S6–62-70. [PubMed] [Google Scholar]
- 21.U.S. Census Bureau. [March 21, 2017];2010 Census, Current Population Survey, Annual Social and Economic Supplement. 2010 Mar; https://www.census.gov/population/race/data/ppl-ba10.html.
- 22.Hansen TW, Kikuya M, Thijs L, Li Y, Boggia J, Bjorklund-Bodegard K, Torp-Pedersen C, Jeppesen J, Ibsen H, Staessen JA. Diagnostic thresholds for ambulatory blood pressure moving lower: a review based on a meta-analysis-clinical implications. J Clin Hypertens (Greenwich) 2008;10:377–381. doi: 10.1111/j.1751-7176.2008.07681.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Head GA, Mihailidou AS, Duggan KA, Beilin LJ, Berry N, Brown MA, Bune AJ, Cowley D, Chalmers JP, Howe PR, Hodgson J, Ludbrook J, Mangoni AA, McGrath BP, Nelson MR, Sharman JE, Stowasser M Ambulatory Blood Pressure Working Group of the High Blood Pressure Research Council of A. Definition of ambulatory blood pressure targets for diagnosis and treatment of hypertension in relation to clinic blood pressure: prospective cohort study. BMJ. 2010;340:c1104. doi: 10.1136/bmj.c1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Imai Y, Nagai K, Sakuma M, Sakuma H, Nakatsuka H, Satoh H, Minami N, Munakata M, Hashimoto J, Yamagishi T, Watanable N, Yabe T, Nishiyama A, Abe K. Ambulatory blood pressure of adults in Ohasama, Japan. Hypertension. 1993;22:900–912. doi: 10.1161/01.hyp.22.6.900. [DOI] [PubMed] [Google Scholar]
- 25.Kikuya M, Hansen TW, Thijs L, Bjorklund-Bodegard K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Ibsen H, Imai Y, Staessen JA International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes I. Diagnostic thresholds for ambulatory blood pressure monitoring based on 10-year cardiovascular risk. Circulation. 2007;115:2145–2152. doi: 10.1161/CIRCULATIONAHA.106.662254. [DOI] [PubMed] [Google Scholar]
- 26.Mancia G, Sega R, Bravi C, De Vito G, Valagussa F, Cesana G, Zanchetti A. Ambulatory blood pressure normality: results from the PAMELA study. J Hypertens. 1995;13:1377–1390. [PubMed] [Google Scholar]
- 27.O’Brien E, Murphy J, Tyndall A, Atkins N, Mee F, McCarthy G, Staessen J, Cox J, O’Malley K. Twenty-four-hour ambulatory blood pressure in men and women aged 17 to 80 years: the Allied Irish Bank Study. J Hypertens. 1991;9:355–360. doi: 10.1097/00004872-199104000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Ohkubo T, Imai Y, Tsuji I, Nagai K, Ito S, Satoh H, Hisamichi S. Reference values for 24-hour ambulatory blood pressure monitoring based on a prognostic criterion: the Ohasama Study. Hypertension. 1998;32:255–259. doi: 10.1161/01.hyp.32.2.255. [DOI] [PubMed] [Google Scholar]
- 29.Schettini C, Bianchi M, Nieto F, Sandoya E, Senra H. Ambulatory blood pressure: normality and comparison with other measurements. Hypertension Working Group. Hypertension. 1999;34:818–825. doi: 10.1161/01.hyp.34.4.818. [DOI] [PubMed] [Google Scholar]
- 30.Staessen J, Bulpitt CJ, Fagard R, Mancia G, O’Brien ET, Thijs L, Vyncke G, Amery A. Reference values for ambulatory blood pressure: a population study. J Hypertens Suppl. 1991;9:S320–321. [PubMed] [Google Scholar]
- 31.Staessen JA, O’Brien ET, Amery AK, Atkins N, Baumgart P, De Cort P, Degaute JP, Dolenc P, De Gaudemaris R, Enstrom I, Fagard R, Gosse P, Gourlay S, Hayashi H, Imai Y, James G, Kawasaki T, Kuschnir E, Kuwajima I, Lindholm L, Liu L, Macor F, Mancia G, McGrath B, Middeke M, Ming J, Omboni S, Otsuka K, Palatini P, Parati G, Pieper C, Verdecchia P, Zachariah P, Zhang W. Ambulatory blood pressure in normotensive and hypertensive subjects: results from an international database. J Hypertens Suppl. 1994;12:S1–12. [PubMed] [Google Scholar]
- 32.Wiinberg N, Hoegholm A, Christensen HR, Bang LE, Mikkelsen KL, Nielsen PE, Svendsen TL, Kampmann JP, Madsen NH, Bentzon MW. 24-h ambulatory blood pressure in 352 normal Danish subjects, related to age and gender. Am J Hypertens. 1995;8:978–986. doi: 10.1016/0895-7061(95)00216-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


