Abstract
Background
As predicted by self-medication theories that drinking is motivated by a desire to ameliorate emotional distress, some studies find internalizing symptoms (e.g., anxiety, depression) increase risk for adolescent drinking; however, such a risk effect has not been supported consistently. Our prior work examined externalizing symptoms as a potential moderator of the association between internalizing symptoms and adolescent alcohol use (AU) to explain some of the inconsistencies in the literature. We found that internalizing symptoms were protective against early adolescent AU particularly for youth elevated on externalizing symptoms (a two-way interaction). Our sample has now been followed for several additional assessments that extend into young adulthood, and the current study tests whether the protective effect of internalizing symptoms may change as youth age into young adulthood, and whether this age moderating effect varied across different clusters of internalizing symptoms (social anxiety, generalized anxiety, and depression). Internalizing symptoms were hypothesized to shift from a protective factor to a risk factor with age, particularly for youth elevated on externalizing symptoms.
Method
A community sample of 387 adolescents was followed for nine annual assessments (mean age =12.1 years at the first assessment and 55% female). Multilevel cross-lagged two-part zero-inflated poisson models were used to test hypotheses.
Results
The most robust moderating effects were for levels of alcohol use, such that the protective effect of all internalizing symptom clusters was most evident in the context of moderate to high levels of externalizing problems. A risk effect of internalizing symptoms was evident at low levels of externalizing symptoms. With age, the risk and protective effects of internalizing symptoms were evident at less extreme levels of externalizing behavior. With respect to alcohol-related problems, findings did not support age moderation for generalized anxiety or depression, but it was supported for social anxiety.
Conclusions
Findings highlight the importance of considering the role of emotional distress from a developmental perspective and in the context of externalizing behavior problems.
Keywords: alcohol, adolescents, internalizing, externalizing
Introduction
Internalizing symptoms (e.g., anxiety and depressive symptoms) have been considered a risk factor in the etiology of adolescent drinking. Yet empirical findings supporting this idea have been inconsistent, particularly with respect to early stages of adolescent alcohol use (Hussong et al., 2011; Colder et al., 2010). For example, consistent with self-medication and negative reinforcement theories that drinking is motivated by efforts to ameliorate emotional distress, some longitudinal studies find internalizing symptoms to be a risk factor for alcohol use (Kaplow et al., 2001; Parrish et al., 2016). Yet, findings from other longitudinal studies suggest that internalizing symptoms are negatively related to alcohol use (Colder et al., 2013; Kaplow et al., 2001; Fleming et al., 2008), perhaps because the fearfulness, social withdrawal, and avoidance that characterize internalizing psychopathology protect youth from selecting into peer groups that support drinking (Fite et al., 2006). Other research finds no association between internalizing problems and adolescent alcohol use after accounting for externalizing symptoms (Maslowsky et al., 2014; Miller-Johnson et al., 1998). Several adolescent preventive interventions target emotional distress (e.g., Botvin et al., 2001), and it is important to understand for whom or when such interventions may be most effective. In this paper we focus on three issues that might account for mixed findings regarding internalizing symptoms and adolescent drinking: (1) the co-occurrence of internalizing and externalizing problems, (2) age, and (3) heterogeneity of internalizing problems.
Co-Occurrence of Internalizing and Externalizing Symptoms
Internalizing and externalizing symptoms commonly co-occur (Achenbach and Rescorla, 2001), and the influence of internalizing symptoms on adolescent alcohol use may vary depending on whether they occur in the presence or absence of externalizing symptoms. Findings regarding the moderating role of externalizing symptoms on the association between internalizing symptoms and alcohol use are mixed with some longitudinal studies providing no support (e.g., Capaldi, 1992) and some studies finding exacerbating effects such that elevated symptoms in both domains is particularly risky (Hussong & Chassin, 1994; Miller-Johnson et al., 1998). Other longitudinal studies, including our own, have found that internalizing symptoms were protective against alcohol and other substance use (Colder et al., 2017, Colder et al., 2013; Mason et al., 2008; Scalco et al., 2014), with this protective effect most evident in the context of elevated externalizing symptoms. These inconsistent findings may be attributable to a few issues. In this study, we consider potential age differences and heterogeneity of internalizing symptoms.
Age
Alcohol use becomes increasingly normative with age (Miech et al., 2016) and beliefs and attitudes about drinking change during adolescence (Colder et al., 2014). Accordingly, psychological characteristics associated with adolescent alcohol use may differ depending on age. It has been posited that internalizing symptoms delay onset of adolescent alcohol use in part due to social withdrawal associated with internalizing symptoms which may then protect youth from engaging in social contexts that promote initiation (Hussong, 2000). However, as alcohol use becomes more normative, increased modeling of alcohol use by peers coupled with greater access to alcohol may result in increased risk for alcohol use by adolescents with elevated internalizing symptoms. Over time, regular drinking might come to serve a coping function for these youth (e.g., Stewart et al., 2006; Cooper et al., 1995). As such, one possibility is that internalizing symptoms are protective of alcohol use in early and middle adolescence, and emerge as a risk factor in late adolescence. Though several studies offer some support for such developmental differences (Colder and Chassin, 1999; Sartor et al., 2007), others have failed to replicate this pattern (Marmorstein, 2009; Marmorstein et al., 2010).
Age-related changes in the association between internalizing problems and alcohol use may depend on the co-occurrence of externalizing problems. That is, internalizing problems may be protective in the context of externalizing problems in early adolescence (Colder et al., 2013; Scalco et al., 2014), but may exacerbate risk for alcohol use in the presence of externalizing problems (a synergistic interaction) in late adolescence and young adulthood (Marmorstein, 2010). Examining developmental differences in the moderating role of externalizing symptoms on the association between internalizing symptoms and alcohol use requires a longitudinal sample that spans early adolescence to young adulthood with repeated assessments of mental health symptoms. To our knowledge, no study with these design features has examined this question. The current study uses a longitudinal design with repeated assessments of mental health symptoms and alcohol use to examine whether age enters into a three-way interaction with internalizing and externalizing symptoms to predict alcohol use.
In considering potential age differences, it may also be important to distinguish alcohol use from alcohol-related problems. Some research suggests that internalizing problems may be more strongly associated with problems rather than levels of use (e.g., Cooper et al., 1995). If this is true, then we might expect the proposed emergent risk effect of internalizing symptoms to be most evident when predicting alcohol-related problems.
Heterogeneity of Internalizing Problems
Anxiety and depression are common internalizing symptom clusters in adolescence (Achenbach & Rescorla, 2001), and it is possible that these subdomains of internalizing symptoms operate differently with externalizing problems across age (Hussong et al., 2011; Colder et al., 2010). Another goal of the current study was to examine clusters of internalizing symptoms, and test our moderational hypotheses separately for generalized anxiety, social anxiety, and depression symptoms.
During adolescence, separation anxiety declines substantially (Cohen et al., 1993), whereas both social and generalized anxiety decline slightly in early adolescence and then increase thereafter (Van Oort et al., 2009; La Greca, 1999). There is evidence that generalized anxiety symptoms are associated with escalation of alcohol use, but not initiation (Kaplow et al., 2001; Sartor et al., 2007; Sung et al., 2004), suggesting that generalized anxiety symptoms may become a risk factor after initial experimentation. The link between social anxiety and alcohol use may also depend on age. Studies of early and middle adolescent aged samples tend to show that social anxiety is unrelated to alcohol use, or associated with low levels of use (Frojd et al., 2011; Myers et al., 2003). Yet by late adolescence, social anxiety is a more robust risk factor for heavy alcohol use and alcohol-related problems (Buckner et al., 2008; Wu et al., 2010).
Numerous studies provide evidence for an association between symptoms of depression and adolescent alcohol use (Armstrong and Costello, 2002; Hussong and Chassin, 1994; Sung et al., 2004;), even after controlling potential confounding factors such as externalizing problems (Marmorstein, 2010; Sung et al., 2004) or in combination with externalizing symptoms (Maslowsky and Schulenberg, 2013). However, there is limited evidence to support or refute potential age-related differences in the link between depression symptoms and adolescent alcohol use.
The Current Study
There is an implicit assumption made in the adolescent alcohol use literature that internalizing and externalizing problems represent two distinct pathways to drinking. However, evidence for an internalizing pathway in adolescence is equivocal, and limited research has explored co-occurring internalizing and externalizing symptoms in developmental pathways to alcohol use. We propose that whether internalizing symptoms operate as a risk or protective factor may depend on age and levels of externalizing symptoms. We are aware of no studies that span early adolescence to young adulthood with repeated assessments of mental health symptoms that have examined such a moderational question. We hypothesize that internalizing symptoms will serve a protective function (negatively associated with alcohol use) at high levels of externalizing problems based on our prior work with this sample. With increasing age, we expect that this effect of internalizing problems will shift to become a risk factor (positive association). We considered symptoms of generalized anxiety, depression, and social anxiety as separate clusters of internalizing psychopathology. Finally, we considered both alcohol use and alcohol-related problems because some research suggest that internalizing problems may be more strongly associated with problems.
Method
Sample
Data for this study were from a community sample of 387 adolescents and their caregivers recruited from households in Erie County, NY assessed annually for nine years. Recruitment occurred between April 2007 and February 2009. Adolescents were eligible for the study if they were between the ages of 11 and 12 at recruitment, and did not have any disabilities that would preclude them from either understanding or completing the assessment. For more information about recruitment procedures, eligibility criteria, and sample description see Trucco et al. (2014).
Average age at the first assessment was 12.1 years old. Average ages at subsequent assessments were 13.1, 14.1, 15.1, 16.1, 17.1, 18.4, 19.4, and 20.4 years old. The sample was approximately evenly split on gender (55% female at W1) and was predominantly non-Hispanic Caucasian (83.1%) or African American (9.1%). Median family income at first assessment was $70,000 and 6% of the families received public assistance income. These sample demographics compared well to demographics of families within our sampling frame, which was Erie County, NY (see Trucco et al., 2014).
Retention across waves of assessment was strong; after the first assessment, sample size varied between N=350 (90%) to N=373 (96%). We compared those present at all assessments and those missing data for at least one assessment on variables from our first assessment. Participants who completed all assessments did not significantly differ from those missing at least one assessment on minority status, gender, parental education, parental marital status, and lifetime alcohol and cigarette use (p-values = 0.63–0.99, φ = 0.001–0.020). There were also no differences on age, income, and internalizing and externalizing symptoms (p-values =0.68–0.97, d = 0.008–0.070). The lack of differences, small effect sizes, low rate of attrition, and our data analytic approach (multilevel modeling), which permitted inclusion of cases with missing data, suggest that missing data likely had a limited impact on our findings.
Procedures
Although there have been nine assessments, behavior problems were not measured at all assessments due to a lapse in funding. The current study only includes questionnaire data (externalizing and internalizing symptoms, and substance use) from seven assessments that allowed us to test prospective associations between symptoms and alcohol use outcomes (Waves 1–4, Waves 7–9). Wave 1–3 assessments were conducted in our research offices with the caregiver and adolescent. Families were compensated $75, $85 and $125 dollars for Waves 1–3, respectively.
Wave 4 consisted of a brief telephone administered audio-Computer Assisted Self Interview (CASI) of SU that took 10–15 minutes to complete. Parents provided consent over the phone and were given a phone number and PIN for their adolescent to use. Assent from the adolescent was obtained at the initiation of the audio-CASI survey. Adolescents received a $15 gift card for completing these assessments.
Wave 7–9 assessments followed procedures similar to those at Waves 1–3, however, we gave the participants the option to complete the survey remotely online (N=18 at Wave 7, N=40 at Wave 8, N=44 at Wave 9). Adolescents were compensated $125 for completing the full assessment (questionnaires and laboratory tasks) or $50 for completing only the questionnaires. Caregivers were compensated $40.
Measures
Alcohol Use
Alcohol use at Waves 1–4 was assessed with items taken from National Youth Survey (Elliott and Huizinga, 1983). Participants responded to two fill in the blank questions: (1) how many times in the past year they had used alcohol (frequency), and (2) how many drinks were typically consumed on days when alcohol was used (quantity). A drink was defined as a 12 oz. of beer, a 4 oz. glass of wine, a 12 oz. wine cooler, or a 1 ¼ oz. shot of hard liquor.
At Waves 7–9 participants were asked about frequency of alcohol use in the past year with nine response options that ranged from “not at all” to “everyday”. Quantity was assessed using a weekly drinking calendar that asked participants to report number of drinks consumed on each day of the week in a typical week from the past 90 days (Cahalan et al., 1969). Drinks per drinking day were computed from the calendar and then multiplied by the frequency item to create a quantity × frequency score for the past year.
As expected given the age of our participants, annual rates of alcohol use were quite low at the early waves, but then increased across assessments (see Table 1). This pattern was also true with respect to drinks consumed per year.
Table 1.
Descriptive statistics for alcohol use and problems.
| Wave | N | Age Mean (SE) | Percent using alcohol | Drinks per year1 Mean (SE) | Experienced at least one Drinking Problem2 | Number of Problems3 Mean (SE) |
|---|---|---|---|---|---|---|
| 1 | 387 | 12.09 (0.59) | 4% | 1.29 (0.76) | – | – |
| 2 | 373 | 13.13 (0.59) | 15% | 7.48 (13.17) | – | – |
| 3 | 369 | 14.11 (0.61) | 27% | 10.03 (22.98) | 77% | 6.45 (6.48) |
| 4 | 368 | 15.08 (0.61) | 35% | 14.43 (21.51) | – | – |
| 7 | 353 | 18.37 (0.66) | 81% | 196.46 (410.02) | 69% | 2.84 (1.98) |
| 8 | 352 | 19.40 (0.68) | 82% | 187.56 (296.81) | 80% | 7.80 (7.54) |
| 9 | 350 | 20.41 (0.66) | 87% | 198.65 (272.16) | 82% | 6.70 (7.36) |
Note:
Drinks per year are shown for those who drank at least once during the past year.
Problems were only assessed at Waves 3, 7, 8 and 9, and % who experienced at least one problem was calculated for those who drank at least once in the past year.
Mean number of problems are shown for those who experienced one of more drinking problems.
Alcohol Problems
Alcohol problems were not assessed at Waves 1–2 because of the young age of the sample, and expected low rates of endorsement. At Wave 3, adolescents who reported using alcohol in the past year were administered 13 questions about the frequency of alcohol problems during the past year (Windle and Windle, 1996). The number of items with positive responses (experiencing the problem at least once) were summed to form an alcohol problem score, and this sum score was used a covariate when predicting Wave 7 problems. At Waves 7–9, alcohol problems were assessed with the Young Adult Alcohol Consequences Questionnaire (YAACQ; Read et al., 2006). Participants who had any drinks during the past year, replied ‘yes’ or ‘no’ to 48 items that assessed drinking-related negative consequences and problems. The number of positively endorsed items were counted to form an alcohol problem score Waves 7–9. As shown in Table 1, for those who drank in the past year, the majority experienced at least one alcohol-related problem.
Internalizing and Externalizing Symptoms
Mental health symptoms were assessed using the Youth Self Report (YSR; Achenbach and Rescorla, 2001) at Waves 1–3 and using the Adult Self-Report (ASR; Achenbach and Rescorla, 2003) at Wave 7 and 8 from the Achenbach System of Empirical Behavioral Assessment (ASEBA). Substance use items were removed to eliminate item overlap with our outcomes. We endeavored to form equivalent scales across adolescence and young adulthood by eliminating items that appeared only on the YSR or only on the ASR. With respect to externalizing symptoms, we included aggression and rule breaking scales and seven items of the YSR were not part of the ASR, and were removed, resulting in 21 total externalizing items at each assessment.
For the internalizing domain, we used the ASEBA Diagnostic Statistical Manual-V (DSM) – oriented scales. Both the generalized anxiety and affective scales of the YSR (Waves 1–3) included one item that was not part of the ASR scales. These two items were removed, resulting in 4 generalized anxiety and 11 depression items.
Social anxiety at Waves 1–3 was assessed using the social avoidance/distress (10 items) and fear of negative evaluation (8 items) subscales from the Social Anxiety Scale for Children and Adolescents-Revised (SASC-R, La Greca and Stone, 1993). At Waves 7 and 8, social anxiety was assessed using the Social Interaction Anxiety Scale (SIAS; Mattick and Clarke, 1998) and the Brief Fear of Negative Evaluation scale (BFNE-II; Carleton et. al., 2006).
Analytic Plan
Our longitudinal study spanned early adolescence to young adulthood, and this necessitated changing our measures to be developmentally appropriate. For externalizing, generalized anxiety, and depression symptoms, we were able to select equivalent items. For social anxiety our measures allowed for conceptual equivalence, but the items were different. In preliminary analysis, we used confirmatory factor analysis to evaluate the equivalence of our symptom measures across waves. Factor models were evaluated using the model χ2, Comparative Fit Index (CFI), Tucker-Lewis Index (TLI) and Root Mean Square Error of Approximation (RMSEA) (Hu & Bentler, 1999).
Random effects models with repeated measures nested within participants were used to test study hypotheses. Nested chi-square model tests were used to evaluate whether random effects improved model fit, and if supported, random effects were included in our final models. The data were organized to test cross-lagged effects controlling for prior levels of the outcome. For alcohol use, we were able to test five cross-lags (Wave 1 symptoms predicting Wave 2 alcohol use, Wave 2 symptoms predicting Wave 3 alcohol use, Wave 3 symptoms predicting Wave 4 alcohol use, Wave 7 symptoms predicting Wave 8 alcohol use, Wave 8 symptoms predicting Wave 9 alcohol use). For alcohol problems, we were able to test three cross-lags (Wave 3 symptoms predicting Wave 7 alcohol problems, Wave 7 symptoms predicting Wave 8 alcohol problems, Wave 8 symptoms predicting Wave 9 alcohol problems). Age, prior levels of the outcome, and mental health symptoms were included as level 1 time-varying covariates. Gender was included as a level 2 covariate. We formed three-way cross-product terms of interest (e.g., age × externalizing symptoms × internalizing symptoms) and relevant two-way interaction terms. We started with the full model including the three-way interaction terms of interest, and then trimmed out non-significant higher-order interaction terms. Predictor variables were standardized within age to facilitate interpretation of interaction effects (Hox, 2010). Separate models were run for each domain of internalizing problems (generalized anxiety, depression, and social anxiety). Because a four-year gap existed between the W3 predictor variables and W7 alcohol problems outcome, W3 predictors in the alcohol problems model were weighted to be 1/4th the effect of later cross-lags.
Our quantity by frequency variable and our problem alcohol variables were skewed with excess zeros, and therefore, we used a zero-inflated Poisson model with random effects to test our proposed interaction term. These models include a binomial part that describes the probability of drinking (or experiencing alcohol-related problems) during a given assessment, and for those who drank (or experienced a problem), the second part of the model describes how many drinks consumed (or how many problems experienced). Models were fit in SAS version 9.4 using Proc Nlmixed.
In the case of statistically significant interactions, we used procedures developed by Preacher et al. (2006) to determine regions where simple slopes of internalizing symptoms were statistically significant. We also plotted simple slopes of internalizing symptoms at the −2 to +2 standard deviations from the sample mean of externalizing symptoms at ages 12, 14, 17, and 19 years of age for descriptive purposes.
Results
Factor Analysis of Symptoms
For our measures of generalized anxiety, depression, and externalizing symptoms, we evaluated the equivalence of these measures across time using a longitudinal confirmatory factor model for each domain of symptoms. For generalized anxiety, the model included five latent variables (generalized anxiety at Waves 1–3, and at Waves 7–8) with the four anxiety items as indicators for each factor. The factors were allowed to covary. The model provided an adequate fit to the data (χ2(152) = 240.39 p > 0.05, CFI = 0.96, TLI = 0.95, RMSEA = 0.05.), and constraining the factor loadings to be equivalent over time resulted in a significant decrement in model fit (Δ χ2(11)=69.87, p<.001). This was due to one factor loading corresponding the item “too fearful/anxious” that varied across time. When this factor loading was allowed to vary, but the others were constrained to be equal over time, there was a non-significant change in the model χ2 (Δ χ2(8)=12.54, p=0.13). The standardized factor loadings for the “too fearful/anxious” item were all substantial (.54, .58, .64, .82, .87 at W1–3 and W7–8, respectively), but increased over time. This factor model supported partial invariance of generalized anxiety, and items were averaged to form scale scores at each wave. A similar model with five latent variables was specified for the 7 depression symptom items at each wave. This model provided an adequate fit to the data (χ2(265)=488.64, p<.05, CFI=.91, TLI=.89, RMSEA=.07), and constraining the factor loadings to be equal over time suggested a non-significant change in the model χ2 (Δ χ2(18)=22.61, p=0.21), supporting measurement equivalence over time. Items were averaged to form a depression scale score at each wave. For externalizing symptoms, the aggressive and rule breaking subscales were computed by averaging items, and the scale scores were used as indicators of the externalizing factor at each wave. This model fit the data well (χ2(25)=35.41, p>.05, CFI=.99, TLI=0.99, RMSEA=.05), and constraining the factor loadings to be equal over time did not result in a decrement in model fit (Δ χ2(4)=1.01, p=0.91).
Our social anxiety measures provided conceptual equivalence across developmental periods (social avoidance/distress and fear of negative evaluation), but unlike the YSR and ASR, the items were different. Accordingly, we formed social avoidance/distress and fear of negative evaluation scale scores at each wave by averaging items, and then standardized these scale scores. This allowed us to compare the association between each scale and the latent factor across developmental period. The model included five latent variables (Waves 1–3, and Waves 7–8) each with two indicators (social avoidance/distress and fear of negative evaluation). The factors were allowed to covary. The model fit the data well (χ2(19) = 94.79 p > 0.05, CFI = 0.96, TLI = 0.90, RMSEA = 0.07), and constraining the factor loadings to be equal over time resulted in a non-significant change in model fit χ2(Δ χ2(4)=2.11, p=0.72), supporting measurement invariance of social anxiety across time. Social avoidance/distress and fear of negative evaluation scales were averaged for form social anxiety scores at each assessment.
Regression Models Predicting Alcohol Use
A random intercept was supported for the binomial, but not the continuous portion of all the alcohol use models. Results for generalized anxiety are presented in Table 2. Age did not enter into an interaction to predict probability of alcohol use, however, the two-way externalizing × internalizing symptom interaction term was supported. Generalized anxiety was negatively associated with probability of alcohol use at elevated levels of externalizing symptoms of use (0.40 standard deviations above the sample mean of externalizing symptoms). At extremely low levels of externalizing symptoms (3 standard deviations below the sample mean), generalized anxiety was positively associated with probability of alcohol use. The overall pattern suggested that the highest probability of drinking was evident for youth above the mean on externalizing symptoms and below the mean on generalized anxiety symptoms. This pattern was replicated in the depression symptoms model (see Table 3), such that depression was negatively associated with probability of alcohol use at high levels of externalizing (.82 standard deviations above the sample mean) and positively associated with probability drinking at extremely low levels of externalizing symptoms (3.2 standard deviations below the sample mean). Again, the highest probability of drinking was evident for youth low in depression symptoms and elevated on externalizing symptoms. There was no evidence that social anxiety entered into an interaction to predict probability of alcohol use (see Table 4). As a first-order effect, social anxiety was negatively associated with probability of alcohol use.
Table 2.
Unstandardized regression coefficients and random effect variance estimates for model with generalized anxiety symptoms.
| Predictor Variable | Drinks per Year Beta (SE) |
Drinking problems Beta (SE) |
|---|---|---|
| Binomial Model | ||
| Intercept | 0.49 (0.47) | −3.39 (0.74)*** |
| Age | 0.44 (0.03)*** | −0.04 (0.08) |
| Gender | 0.23 (0.09)** | 0.08 (0.17) |
| Prior alcohol use or problems | 8.16 (1.38)*** | 2.04 (0.54)*** |
| Gen. Anxiety | −0.12 (.09) | −0.04 (0.18) |
| Externalizing | 1.05 (0.11)*** | 0.09 (0.20) |
| Gen. Anxiety*Externalizing | −0.19 (0.06)** | |
| Gen. Anxiety*Age | ||
| Externalizing*Age | ||
| Gen. Anxiety*Externalizing*Age | ||
| Continuous Model | ||
| Intercept | 2.67 (0.02)*** | 2.77 (0.06)*** |
| Age | 0.32 (0.00)*** | −0.09 (0.01) *** |
| Gender | −0.23 (0.00)*** | 0.01 (0.02) |
| Prior alcohol use or problems | 0.23 (0.00)*** | 0.35 (0.01)*** |
| Gen. Anxiety | −0.19 (0.02)*** | −0.00 (0.02) |
| Externalizing | 0.10 (0.02)*** | 0.10 (0.02)*** |
| Gen. Anxiety*Externalizing | −0.15 (0.02)*** | −0.08 (0.01)*** |
| Gen. Anxiety*Age | 0.02 (0.00)*** | |
| Externalizing*Age | −0.01 (0.00)*** | |
| Gen. Anxiety*Externalizing*Age | 0.01 (0.00)*** | |
|
| ||
| Random Parameters | ||
| Intercept - Binomial Model | 2.50 (0.50)*** | |
| Intercept - Continuous Model | ||
Note.
p< .054.
p<.05.
p<.01.
p<.001. Gen. Anxiety= generalized anxiety.
Table 3.
Unstandardized regression coefficients and random effect variance estimates for model with depression symptoms.
| Predictor Variable | Drinks per Year Beta (SE) |
Drinking problems Beta (SE) |
|---|---|---|
| Binomial Model | ||
| Intercept | 0.49 (0.47) | −3.35 (0.74)*** |
| Age | 0.44 (0.03)*** | −0.04 (0.08) |
| Gender | 0.24 (0.09)** | 0.10 (0.17) |
| Prior alcohol use or problems | 8.15 (1.38)*** | 2.02 (0.55)*** |
| Depression | −0.12 (0.11) | −0.12 (0.20) |
| Externalizing | 1.05 (0.11)*** | 0.15 (0.22) |
| Depression*Externalizing | −0.15 (0.06)* | |
| Depression*Age | ||
| Externalizing*Age | ||
| Depression*Externalizing*Age | ||
| Continuous Model | ||
| Intercept | 2.69 (0.02)*** | 2.79 (0.06)*** |
| Age | 0.32 (0.00)*** | −0.09 (0.00)*** |
| Gender | −0.23 (0.00)*** | 0.02 (0.02) |
| Prior alcohol use or problems | 0.24 (0.00)*** | 0.36 (0.01)*** |
| Depress | −0.18 (0.02)*** | −0.04 (0.02) |
| Ext | 0.18 (0.02)*** | 0.15 (0.02)*** |
| Depress*Ext | −0.19 (0.02)*** | −0.07 (0.01)*** |
| Depress*Age | 0.02 (0.00)*** | |
| Ext*Age | −0.02 (0.00)*** | |
| Depress*Ext*Age | 0.02 (0.00)*** | |
|
| ||
| Random Parameters | ||
| Intercept - Binomial Model | 0.75 (0.18)*** | |
| Intercept - Continuous Model | ||
Note.
p<.05.
p<.01.
p<.001.
Table 4.
Unstandardized regression coefficients and variance estimates for model with social anxiety symptoms.
| Predictor Variable | Drinks per Year Beta (SE) |
Drinking problems Beta (SE) |
|---|---|---|
| Binomial Model | ||
| Intercept | 0.44 (0.46) | −3.40 (0.73)*** |
| Age | 0.41 (0.03)*** | −0.04 (0.08) |
| Gender | 0.24 (0.09)** | 0.08 (0.16) |
| Prior alcohol use or problems | 8.06 (1.35)*** | 2.04 (0.55)*** |
| Social Anxiety | −0.24 (0.09)** | −0.03 (0.16) |
| Externalizing | 0.58 (0.09)*** | 0.08 (0.18) |
| Social Anxiety*Externalizing | ||
| Social Anxiety*Age | ||
| Externalizing*Age | ||
| Social Anxiety*Externalizing*Age | ||
| Continuous Model | ||
| Intercept | 2.67 (0.02)*** | 2.68 (0.07)*** |
| Age | 0.32 (0.00)*** | −0.08 (0.01)*** |
| Gender | −0.22 (0.00)*** | 0.02 (0.02) |
| Prior alcohol use or problems | 0.24 (0.00)*** | 0.36 (0.01)*** |
| Social Anxiety | −0.20 (0.02)*** | 0.20 (0.07)** |
| Externalizing | −0.06 (0.01)*** | 0.11 (0.05)* |
| Social Anxiety*Externalizing | −0.16 (0.01)*** | 0.08 (0.04)* |
| Social Anxiety*Age | 0.01 (0.00)*** | −0.03 (0.01)** |
| Externalizing*Age | 0.01 (0.00)*** | −0.01 (0.01) |
| Social Anxiety*Externalizing*Age | 0.02 (0.00)*** | −0.02 (0.01)** |
|
| ||
| Random Parameters | ||
| Intercept - Binomial Model | 0.98 (0.22) *** | |
| Intercept - Continuous Model | ||
Note.
p<.05.
p<.01.
p<.001.
With respect to the count portion of the alcohol use models, there was support for the proposed three-way interaction for each domain of internalizing symptoms (see Tables 2–4). Plots of the simple slopes of generalized anxiety at different ages are presented in Figure 1. Looking across Panels a-d of Figure 1 shows that levels of alcohol use increased with age. Across all ages, the general pattern was similar. Generalized anxiety was prospectively associated with increased drinking at low levels of externalizing symptoms, and with decreased drinking at high levels of externalizing symptoms. The highest level of drinking was observed at low levels of generalized anxiety and high levels of externalizing symptoms. The regions of significance (panels e-h of Figure 1) show that the moderating effect was evident at less extreme levels of externalizing symptoms at older ages. For example, at age 12 the positive effect of generalized anxiety was observed below −1.5 standard deviations from the sample mean of externalizing symptoms, and the negative effect was observed at values greater than −.75 standard deviations below the sample mean of externalizing symptoms. By age 19, these risk and protective effects hovered just below and above the sample mean of externalizing symptoms. This suggests that for most youth at age 12, generalized anxiety is protective against increases in levels of drinking. However, by age 19, the risk and protective effect of generalized anxiety is equally prevalent, and based on slight variations from normative levels of externalizing symptoms.
Figure 1.
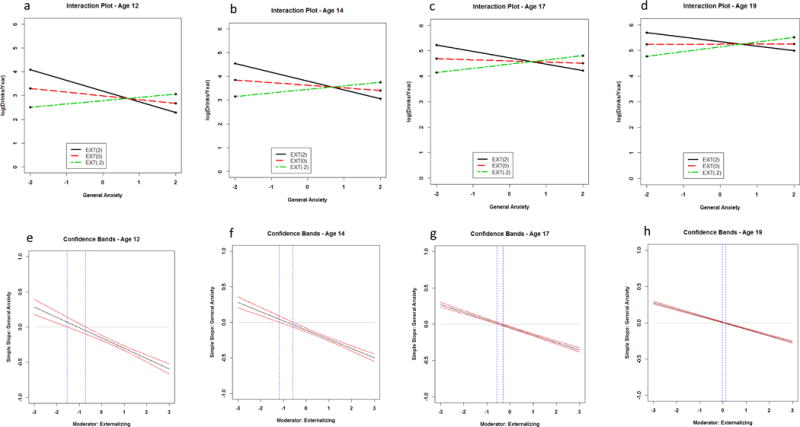
Panels a-d present simple slopes of generalized anxiety prospectively predicting number of drinks in the past year across levels of externalizing behavior (ext) and age. Numbers in parentheses in the legend correspond to standard deviations units from the sample mean of the observed externalizing symptom distribution. Panels e-h present 95% confidence bands for simple slopes of generalized anxiety predicting number of drinks in the past year across levels of externalizing problems and age. Vertical dashed lines indicate the point on the externalizing continuum that the confidence band does not include zero, and the simple slope becomes statistically significant (p < .05).
This pattern was similar for depression symptoms (see Figure 2). One notable difference was that the simple slopes of depression symptoms (both positive and negative slopes) were much flatter with age, suggesting that although externalizing behavior operated as a moderator, depression symptoms were less strongly related to levels of drinking in young adulthood.
Figure 2.
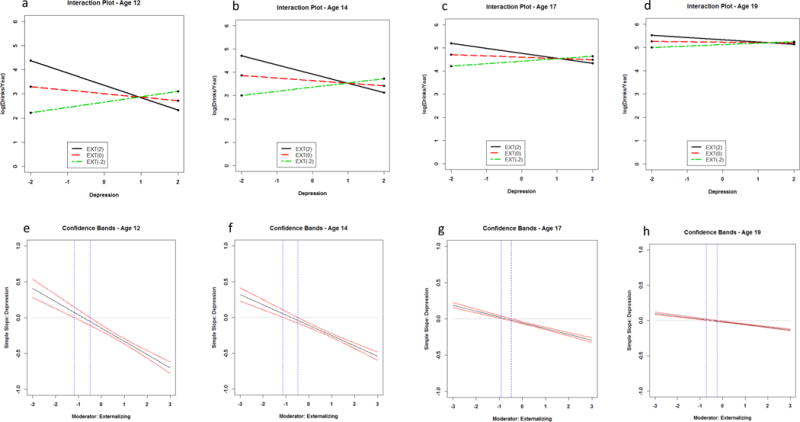
Panels a-d present simple slopes of depression prospectively predicting number of drinks in the past year across levels of externalizing behavior (ext) and age. Numbers in parentheses in the legend correspond to standard deviations units from the sample mean of the observed externalizing symptom distribution. Panels e-h present 95% confidence bands for simple slopes of depression predicting number of drinks in the past year across externalizing problems and age. Vertical dashed lines indicate the point on the externalizing continuum that the confidence band does not include zero, and the simple slope becomes statistically significant (p < .05).
The nature of the three-way interaction was similar for social anxiety at younger ages (see Figure 3). That is, social anxiety was prospectively associated with decreases in drinking at high levels of externalizing symptoms, and with increases in drinking at low levels of externalizing symptoms (panels a-d and e-h). However, at older ages (panels c-d and g-h), social anxiety was largely protective against drinking across the range of externalizing symptoms. In fact, the points of significance (vertical blue lines) occurred outside the range of our plots.
Figure 3.
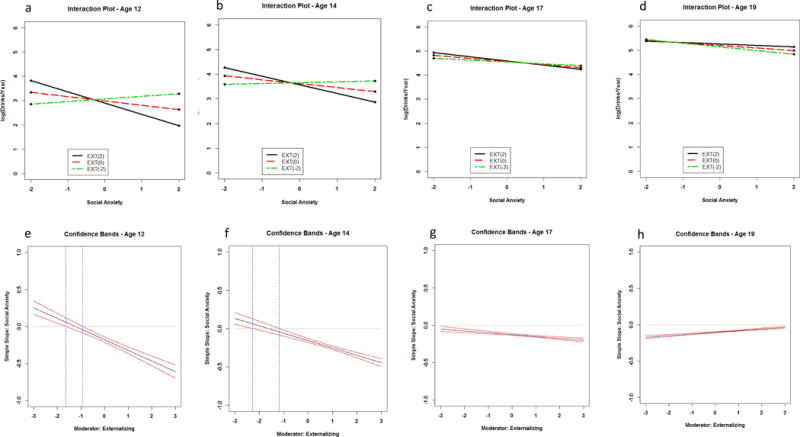
Panels a-d present simple slopes of social anxiety prospectively predicting number of drinks in the past year across levels of externalizing behavior (ext) and age. Numbers in parentheses in the legend correspond to standard deviations units from the sample mean of the observed externalizing symptom distribution. Panels e-h present 95% confidence bands for simple slopes of social anxiety predicting number of drinks in the past year across externalizing problems and age. Vertical dashed lines indicate the point on the externalizing continuum that the confidence band does not include zero, and the simple slope becomes statistically significant (p < .05).
Regression Models Predicting Alcohol Problems
Results from the final trimmed model with internalizing symptoms predicting alcohol problems are presented in Tables 2–4. The alcohol problems models did not support a random intercept for either the binomial or count portions of the model. Results from the binomial model showed no support for interaction terms. Furthermore, none of the symptom variables were prospectively associated with the probability of experiencing an alcohol-related problem. This was true across all internalizing domains.
Results in the count portion of the model supported a 3-way age interaction in the social anxiety model. As shown in panels a-b and c-d of Figure 4, at age 19, high levels of social anxiety were associated with increased problems at low levels of externalizing symptoms, and with decreased problems at high levels of externalizing symptoms. This pattern corresponds to what we observed for alcohol use. However, at age 17, the simple slopes of anxiety were not statistically significant within the range of our data.
Figure 4.
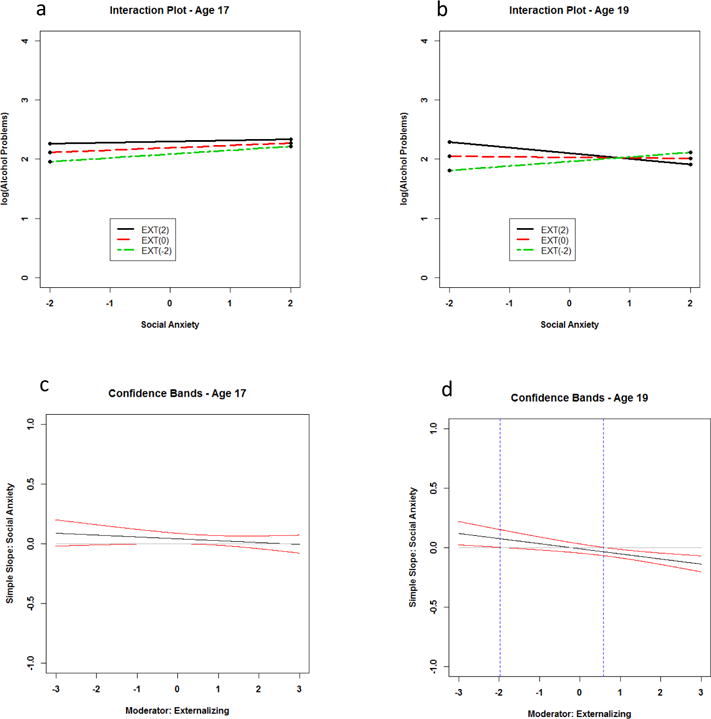
Panels a & b present simple slopes of social anxiety prospectively predicting number of alcohol problems in the past year across levels of externalizing behavior (ext) and age. Numbers in parentheses in the legend correspond to standard deviations units from the sample mean of the observed externalizing symptom distribution. Panels c & d present 95% confidence bands for simple slopes of social anxiety predicting number of alcohol problems in the past year across externalizing problems and age. Vertical dashed lines indicate the point on the externalizing continuum that the confidence band does not include zero, and the simple slope becomes statistically significant (p < .05).
Age did not enter into any interactions with generalized anxiety and depression to predict number of alcohol problems. However, a statistically significant two-way interaction with externalizing symptoms was supported for both generalized anxiety and depression (Tables 2 and 3). In both models, internalizing symptoms prospectively predicted increases in problems at low levels of externalizing symptoms (approximately 1 standard deviation below the sample mean of externalizing symptoms), and decreases in problems at high levels of externalizing symptoms (approximately .30 standard deviations above the mean of externalizing symptoms).
Discussion
The literature examining the association between internalizing symptoms and adolescent alcohol use has been inconsistent (Colder et al., 2010; Hussong et al., 2011). The goal of the current study was to shed light on these mixed findings by examining externalizing symptoms and age as potential moderators of the association between internalizing symptoms and alcohol involvement (probability of alcohol use, quantity and frequency of drinking and alcohol-related problems). We also considered different clusters of internalizing symptoms (generalized anxiety, depression, and social anxiety) with the idea that some of these clusters may be more strongly linked to alcohol involvement than others. A notable strength of our study is that it spanned early adolescence to young adulthood with repeated assessments of mental health symptoms and alcohol use/problems, and this allowed us to evaluate developmental differences that to our knowledge have not yet been tested.
The most consistent finding was support for a three-way age × externalizing symptoms × internalizing symptoms interaction term predicting levels of alcohol use for all three clusters of internalizing symptoms examined in this study. Contrary to our prediction, the nature of this interaction remained similar across developmental periods. Internalizing symptoms were protective at high levels of externalizing symptoms, and increased risk for drinking at low levels of externalizing symptoms. The highest level of drinking was evident among youth characterized by high levels of externalizing symptoms and low levels of internalizing symptoms, particularly at younger ages. With age, less extreme levels of externalizing symptoms were necessary to push internalizing symptoms to be a risk or protective factor, and the effect of elevated externalizing symptoms on promoting high levels of drinking diminished. This age-related pattern may reflect that alcohol use becomes more normative with age (Miech et al., 2016). In early adolescence, alcohol use is rare (see Table 1), and is a prominent feature of deviant peer groups that support drinking and provide access to alcohol (Dishion & Medici-Skaggs, 2000). Externalizing symptoms likely propel youth to select into deviant peer groups, and this may be more likely when internalizing symptoms are low and there is less fear and worry to curtail engagement in deviant behaviors (Scalco et al., 2014; Fite et al., 2006). At older ages, when drinking is less concentrated in deviant peer groups, externalizing symptoms are likely to play less of moderating role. Indeed, the pattern we observed suggests that although moderation by externalizing symptoms was still evident at older ages, the simple effects of internalizing symptoms tended to be less differentiated at older ages.
The age-related pattern for social anxiety predicting levels of alcohol use diverged somewhat. Social anxiety became more uniformly protective at older ages compared to generalized anxiety or depression symptoms. This was somewhat surprising because social anxiety is robustly associated with alcohol use in late adolescent and young adulthood (Buckner et al., 2008; Wu et al., 2010). We also found that high levels of social anxiety were associated with decreased probability of alcohol use, and this protective effect was evident regardless of age and levels of externalizing symptoms. Taken together, these findings suggest that socially anxious youth are unlikely to initiate drinking, perhaps because they avoid social situations where alcohol is likely to be available (Tomlinson et al., 2013), and when they drink, they are likely to consume lower levels of alcohol perhaps for fear of embarrassing themselves (fear of negative evaluations).
These findings suggest that internalizing symptoms can operate as a risk and protective factor for levels of consumption once youth decide to drink. Hussong et al. (2011) proposed that the role of internalizing symptoms in the etiology of adolescent alcohol use is likely characterized by several different mediational pathways, some of which might be risk enhancing and some of which might be protective. Youth drink for a variety of reasons including to enhance positive affect and to cope with emotional distress (Cooper et al., 1995). Drinking to cope with emotional distress may be a prominent feature of a risk pathway for youth characterized by high internalizing and low externalizing symptoms. In contrast, youth low in internalizing symptoms and high in externalizing symptoms are likely to be disinhibited and have trouble regulating their behavior (Hicks & Zucker, 2014), and this may lead to excessive drinking to enhance positive affect. However, high internalizing symptoms, when co-occurring with high levels of externalizing symptoms, may provide some protection for against excessive drinking associated with externalizing symptoms. Internalizing symptoms in this context may be associated with social withdrawal or fear and worry about the excessive drinking.
The general pattern of our findings did not suggest that internalizing symptoms emerged more strongly as a risk factor at older ages. A symptom pattern characterized by high externalizing symptoms and low internalizing symptoms at older ages was most strongly associated with increased levels of consumption when drinking occurred. It is possible that internalizing symptoms are more proximally associated with alcohol use than could be captured in our prospective models that included year lags (Hussong et al., 2001). Indeed, negative reinforcement models of addiction posit that the acute experience of emotional distress prompts drinking as a means of coping (Hussong et al., 2011), suggesting the link between emotional distress and alcohol use requires short time frames that might be best captured by ecological momentary and other more proximal assessment designs.
Coping motives for drinking are often more strongly associated with alcohol problems than with alcohol use (Kuntsche et al., 2005), and we expected that the risk effect of internalizing symptoms would be more strongly linked to alcohol problems than to alcohol use, particularly at older ages when alcohol use disorder is most likely to emerge (Chassin et al., 2015). However, this was not supported. We did not assess problems until Wave 3 because we expected low endorsement of problems at our earlier waves when youth were early adolescence. The result was that analysis of alcohol-related problems was limited to 3 cross-lagged associations, and this likely limited our power to detect interactions predicting problems. Indeed, Monte Carlo simulations done in Mplus version 7.2 using results from our models suggested power to detect the three-way age × internalizing × externalizing interactions ranged from .25 to .81 for the alcohol problems regression models. Studies with more repeated assessments that extend further into young adulthood might be better suited to test our predictions for alcohol-related problems. Although we did find that social anxiety entered into a three-way interaction with age and externalizing symptoms to predict the number of alcohol problems, the nature of this interaction was similar to the one we observed for levels of use, and did not conform to our hypotheses.
Limitations
Results from this study should be understood within the context of certain limitations. First, our study included a community sample that was assessed from early to late adolescence, and may not generalize to high risk or clinical samples, or different aged samples. There is evidence that the co-occurrence of internalizing and externalizing problems may operate in a synergistic fashion in clinical samples (Miller-Johnson et al., 1998) and that internalizing problems more consistently predict SU later in adolescence (Sung et al., 2004) and in early adulthood (Hussong et al., 2011). This suggests that findings regarding interactive effects may depend on sample characteristics. Second, although we examined several facets of internalizing symptoms and our results suggest that they largely operated in a similar fashion, there are other domains of emotional distress to be considered such as post-traumatic stress symptoms (e.g., Read et al., 2013). It may also be useful to consider different facets of externalizing symptoms. Given the number of three-way interactions tested (12), we were reluctant to increase the number of statistical tests in our study. This may be useful direction for future research. Third, although we examined several aspects of alcohol involvement, internalizing symptoms have been linked to other drugs of abuse including marijuana, cigarette smoking, and other drugs (Chassin et al., 2015), and it would be useful to consider the proposed moderational model with respect to these other drugs. Finally, mental health symptoms and alcohol use were both assessed with self-reports, and some of our associations may have been inflated due to shared method variance.
Conclusions
Despite these limitations, our findings inform current developmental models of adolescent alcohol use (e.g., Zucker, 2006). There is currently no developmental model that accounts for the etiological role of internalizing problems in the initiation and escalation of adolescent SU. Our findings suggest that it would be fruitful for such a developmental model to consider the effect of internalizing problems in the context of co-occurring externalizing problems and age as our findings suggest that the moderating role of externalizing symptoms shifts across early adolescence into young adulthood. We observed some instances in which internalizing symptoms can increase risk for alcohol use consistent with coping theories of alcohol use, but these risk effects were conditioned on age and externalizing symptoms. This suggests that coping oriented interventions for unselected samples may not a wise use of resources.
Acknowledgments
The study was supported by NIDA Grant R01DA019631 awarded to C.R. Colder
References
- Achenbach TM, Rescorla LA. Youth Self-Report for Ages 11–18. ASEBA; Burlington, VT: 2001. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA Adult Forms and Profiles. University of Vermont; Burlington, VA: 2003. [Google Scholar]
- Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J Consult Clin Psych. 2002;70:1224. doi: 10.1037//0022-006x.70.6.1224. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Griffin KW, Diaz T, Ifill-Williams M. Preventing binge drinking during early adolescence: one- and two-year follow-up of a school-based preventive intervention. Psychol Addict Behav. 2001;15:360–365. doi: 10.1037//0893-164x.15.4.360. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, Lewinsohn PM. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. J Psychiat Res. 2008;42:230–239. doi: 10.1016/j.jpsychires.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carleton RN, McCreary DR, Norton PJ, Asmundson GJG. Brief Fear of Negative Evaluation Scale – Revised. Depression and Anxiety. 2006;23(5):297–303. doi: 10.1002/da.20142. [DOI] [PubMed] [Google Scholar]
- Cahalan D, Cisin IH, Crossley HM. American drinking practices: a national study of drinking behavior and attitudes. Monographs of the Rutgers Center of Alcohol Studies 1969 [Google Scholar]
- Capaldi DM. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: II. a 2-year follow-up at grade 8. Dev Psychopathol. 1992;4:125–144. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Chassin L, Colder CR, Hussong A, Sher K. Substance use and substance use disorders, in Developmental Psychopathology. In: Cichetti E, editor. Maladaptation and Psychopathology. 3rd. Vol. 3. J Wiley & Sons; New Jersey: 2015. pp. 833–897. [Google Scholar]
- Cohen P, Cohen J, Kasen S, Velez C, Hartmark C, Johnson J, Rojas M, Brook J, Streuning EL. An epidemiological study of disorders in late childhood and adolescence—I. age‐and gender‐specific prevalence. J Child Psychol Psyc. 1993;34:851–867. doi: 10.1111/j.1469-7610.1993.tb01094.x. [DOI] [PubMed] [Google Scholar]
- Colder CR, Chassin L. The psychosocial characteristics of alcohol users versus problem users: data from a study of adolescents at risk. Dev Psychopathol. 1999;11:321–348. doi: 10.1017/s0954579499002084. [DOI] [PubMed] [Google Scholar]
- Colder CR, Chassin L, Lee MR, Villalta IK. Developmental perspectives: affect and adolescent substance use. In: Kassel JD, editor. Substance Abuse and Emotion. American Psychological Association; Washington, DC: 2010. pp. 109–135. [Google Scholar]
- Colder CR, Frndak S, Lengua LJ, Read JP, Hawk LW, Wieczorek WF. Internalizing and externalizing problem behavior: a test of a latent variable interaction predicting trajectories of onset and escalation of adolescent drug use. J Abnorm Child Psych. 2017 doi: 10.1007/s10802-017-0277-6. epub ahead of print: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colder CR, O’Connor RM, Read JP, Eiden RD, Lengua LJ, Hawk LW, Wieczorek WF. Growth trajectories of alcohol information processing and associations with escalation of drinking in early adolescence. Psychol Addict Behav. 2014;28:659. doi: 10.1037/a0035271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colder CR, Scalco MD, Trucco EM, Read JP, Lengua LJ, Wieczorek WF, Hawk LW. Prospective associations of internalizing and externalizing problems and their co-occurrence with early adolescent substance use. J Abnorm Child Psych. 2013;41:667–77. doi: 10.1007/s10802-012-9701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: a motivational model of alcohol use. J Pers Soc Psychol. 1995;69:990. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Medici Skaggs N. An ecological analysis of monthly “bursts” in early adolescent substance use. App Dev Sci. 2000;4:89–97. [Google Scholar]
- Elliott DS, Huizinga D. Social class and delinquent behavior in a national youth panel: 1976–1980. Criminology. 1983;21:149–177. [Google Scholar]
- Fite PJ, Colder CR, O’Connor RM. Childhood behavior problems and peer selection and socialization: risk for adolescent alcohol use. Addict Behav. 2006;31:1454–1459. doi: 10.1016/j.addbeh.2005.09.015. [DOI] [PubMed] [Google Scholar]
- Fleming CB, Mason WA, Mazza JJ, Abbott RD, Catalano RF. Latent growth modeling of the relationship between depressive symptoms and substance use during adolescence. Psychol Addict Behav. 2008;22:186. doi: 10.1037/0893-164X.22.2.186. [DOI] [PubMed] [Google Scholar]
- Fröjd S, Ranta K, Kaltiala-Heino R, Marttunen M. Associations of social phobia and general anxiety with alcohol and drug use in a community sample of adolescents. Alcohol Alcoholism. 2011;46:192–199. doi: 10.1093/alcalc/agq096. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Zucker RA. Alcoholism: A life span perspective on etiology and course. In: Lewis M, Rudolph K, editors. Handbook of Developmental Psychopathology. Springer; Boston, MA: 2014. pp. 583–599. [Google Scholar]
- Hox JJ. Multilevel Analysis: Techniques and Applications. 2nd. Routledge; New York: 2010. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Hussong AM. The settings of adolescent alcohol and drug use. J Youth Adolescence. 2000;29:107–119. [Google Scholar]
- Hussong AM, Chassin L. The stress-negative affect model of adolescent alcohol use: disaggregating negative affect. J Stud Alcohol. 1994;55:707–718. doi: 10.15288/jsa.1994.55.707. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Hicks RE, Levy SA, Curran PJ. Specifying the relations between affect and heavy alcohol use among young adults. J Abnorm Psychol. 2001;110:449. doi: 10.1037//0021-843x.110.3.449. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychol Addict Behav. 2011;25:390–404. doi: 10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplow JB, Curran PJ, Angold A, Costello EJ. The prospective relation between dimensions of anxiety and the initiation of adolescent alcohol use. J Clin Child Psychol. 2001;30:316–326. doi: 10.1207/S15374424JCCP3003_4. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clin Psychol Rev. 2005;25:841–861. doi: 10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- La Greca AM. The social anxiety scales for children and adolescents. BehavTherapist. 1999;22:133–136. [Google Scholar]
- La Greca AM, Stone WL. Social anxiety scale for children-revised: factor structure and concurrent validity. J Clin Child Psychol. 1993;22:17–27. [Google Scholar]
- Marmorstein NR. Longitudinal associations between alcohol problems and depressive symptoms: early adolescence through early adulthood. Alcohol Clin Exp Res. 2009;33:49–59. doi: 10.1111/j.1530-0277.2008.00810.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmorstein NR. Longitudinal associations between depressive symptoms and alcohol problems: the influence of comorbid delinquent behavior. Addict Behav. 2010;35:564–571. doi: 10.1016/j.addbeh.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmorstein NR, White HR, Loeber R, Stouthamer-Loeber M. Anxiety as a predictor of age at first use of substances and progression to substance use problems among boys. J Abnorm Child Psych. 2010;38:211–224. doi: 10.1007/s10802-009-9360-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslowsky J, Schulenberg JE. Interaction matters: quantifying conduct problem× depressive symptoms interaction and its association with adolescent alcohol, cigarette, and marijuana use in a national sample. Dev Psychopathol. 2013;25:1029–1043. doi: 10.1017/S0954579413000357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslowsky J, Schulenberg JE, Zucker R. Influence of conduct problems and depressive symptomatology on adolescent substance use: developmentally proximal versus distal effects. Dev Psychol. 2014;50:1179–1189. doi: 10.1037/a0035085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason WA, Hitchings JE, Spoth RL. The interaction of conduct problems and depressed mood in relation to adolescent substance involvement and peer substance use. Drug Alc Dep. 2008;96:233–248. doi: 10.1016/j.drugalcdep.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behav Res Ther. 1998;36:455–470. doi: 10.1016/s0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use: 1975–2015 Volume I, Secondary school students. Institute for Social Research, The University of Michigan; Ann Arbor, MI: 2016. [Google Scholar]
- Miller-Johnson S, Lochman JE, Coie JD, Terry R, Hyman C. Comorbidity of conduct and depressive problems at sixth grade: substance use outcomes across adolescence. J Abnorm Child Psych. 1998;26:221–232. doi: 10.1023/a:1022676302865. [DOI] [PubMed] [Google Scholar]
- Myers MG, Aarons GA, Tomlinson K, Stein MB. Social anxiety, negative affectivity, and substance use among high schools students. Psychol Addict Behav. 2003;17:277. doi: 10.1037/0893-164X.17.4.277. [DOI] [PubMed] [Google Scholar]
- Parrish KH, Atherton OE, Quintana A, Conger RD, Robins RW. Reciprocal relations between internalizing symptoms and frequency of alcohol use: findings from a longitudinal study of Mexican-origin youth. Psychol Addict Behav. 2016;30:203–208. doi: 10.1037/adb0000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. J Educ Behav Stat. 2006;31:437–448. [Google Scholar]
- Read JP, Kahler CW, Strong DS, Colder CR. Development and preliminary validation of the young adult alcohol consequences questionnaire. J Stud Alcohol. 2006;67:169–177. doi: 10.15288/jsa.2006.67.169. [DOI] [PubMed] [Google Scholar]
- Read JP, Wardell JD, Vermont LN, Colder CR, Ouimette P, White J. Transition and change: prospective effects of posttraumatic stress on smoking trajectories in the first year of college. Health Psychol. 2013;32:757. doi: 10.1037/a0029085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sartor CE, Lynskey MT, Heath AC, Jacob T, True W. The role of childhood risk factors in initiation of alcohol use and progression to alcohol dependence. Addiction. 2007;102:216–225. doi: 10.1111/j.1360-0443.2006.01661.x. [DOI] [PubMed] [Google Scholar]
- Scalco MD, Colder CR, Hawk LW, Read JP, Wieczorek WF, Lengua LJ. Internalizing and externalizing problem behavior and early adolescent substance use: a test of a latent variable interaction and conditional indirect effects. Psychol Addict Behav. 2014;28:828–840. doi: 10.1037/a0035805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SH, Morris E, Mellings T, Komar J. Relations of social anxiety variables to drinking motives, drinking quantity and frequency, and alcohol-related problems in undergraduates. J Ment Health. 2006;15:671–682. [Google Scholar]
- Sung M, Erkanli A, Angold A, Costello EJ. Effects of age at first substance use and psychiatric comorbidity on the development of substance use disorders. Drug Alcohol Depend. 2004;75:287–299. doi: 10.1016/j.drugalcdep.2004.03.013. [DOI] [PubMed] [Google Scholar]
- Tomlinson KL, Cummins KM, Brown SA. Social anxiety and onset of drinking in early adolescence. J Child Adoles Subst. 2013;22:163–177. doi: 10.1080/1067828X.2012.747994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trucco EM, Colder CR, Wieczorek WF, Lengua LJ, Hawk LW. Early adolescent alcohol use in context: how neighborhoods, parents, and peers impact youth. Dev Psychopathol. 2014;26:425–436. doi: 10.1017/S0954579414000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Oort FVA, Greaves‐Lord K, Verhulst FC, Ormel J, Huizink AC. The developmental course of anxiety symptoms during adolescence: the TRAILS study. J Child Psychol Psyc. 2009;50:1209–1217. doi: 10.1111/j.1469-7610.2009.02092.x. [DOI] [PubMed] [Google Scholar]
- Windle M, Windle RC. Coping strategies, drinking motives, and stressful life events among middle adolescents: associations with emotional and behavioral problems and with academic functioning. J Abnorm Psychol. 1996;105:551–560. doi: 10.1037//0021-843x.105.4.551. [DOI] [PubMed] [Google Scholar]
- Wu P, Goodwin RD, Fuller C, Liu X, Comer JS, Cohen P, Hoven CW. The relationship between anxiety disorders and substance use among adolescents in the community: specificity and gender differences. J Youth Adolescence. 2010;39:177–188. doi: 10.1007/s10964-008-9385-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker R. Developmental Psychopathology. 2nd. Kluwer Academic / Plenum Press Publishers; New York, NY: 2006. Alcoholism: a life span perspective on etiology and course; pp. 569–585. [Google Scholar]


