Abstract
Background
This study examined whether a brief video intervention (Prevention of Postrape Stress; PPRS) delivered in the emergency department to recent sexual assault (SA) victims reduced alcohol and marijuana use at three points over the course of a six-month follow-up compared to treatment as usual (TAU) and an active control condition (Pleasant Imagery and Relaxation Information; PIRI). Prior assault history, minority status, and pre-SA substance use also were examined as moderators of intervention efficacy.
Methods
Women age 15 and older (N = 154) who participated in a post-SA medical forensic exam were randomly assigned to watch the PPRS video (n=54), the PIRI video (n=48), or receive TAU (n=52) and completed at least one follow-up assessment targeted at 1.5 (T1), 3 (T2), or 6 (T3) months following the exam.
Results
Regression analyses revealed that, relative to TAU, PPRS was associated with less frequent alcohol use at 6 months post-SA among women reporting pre-SA binge drinking and minority women. Relative to TAU, PPRS also was associated with fewer days of marijuana use at T1 among those who did not report pre-SA marijuana use and prior SA. Findings for pre-SA marijuana use were maintained at T3; however, findings for prior SA shifted such that PPRS was associated with fewer days of marijuana use at T3 for women with a prior SA.
Conclusions
PPRS may be effective at reducing substance use for some recent SA victims, including those with a prior SA history, a prior substance use history, and minority women.
Keywords: RCT, brief intervention, alcohol, marijuana, sexual assault
Introduction
Sexual assault (SA) is a public health concern, with recent national estimates indicating that 18% of women have experienced rape or attempted rape (Black et al., 2011). SA can have long-term negative physical and mental health consequences including alcohol and marijuana misuse (Bryan et al., 2016, Long and Ullman, 2016). Substance use can have unique consequences for SA victims including increasing sexual revictimization risk (Hannan et al., 2015) and can complicate the course of other associated mental health consequences like posttraumatic stress disorder (Kaysen et al., 2011).
Secondary Prevention of Drug and Alcohol Use for Recent Sexual Assault Victims
One way to attenuate the negative consequences of SA is to provide secondary prevention interventions to recent SA victims during the post-SA medical forensic exam (SAMFE) conducted at the emergency department (ED). Although two acute mental health prevention programs have targeted recent SA victims in the ED (Resnick et al., 2007a, Resnick et al., 2007b, Rothbaum et al., 2012), only Resnick and colleagues’ program targeted drug and alcohol use. This Prevention of Post-Rape Stress (PPRS) program included a video that presented recent SA victims with information about the SAMFE to help alleviate concerns about exam procedures along with psychoeducation and non-substance use coping strategies to reduce or prevent future substance use and mental health symptoms. A randomized controlled trial examining the efficacy of PPRS compared to treatment as usual (TAU) conducted among 268 recent SA victims indicated reduced frequency of post-rape marijuana use among women who reported recent pre-rape marijuana use (Resnick et al., 2007b). However, the video intervention was not compared to an active control condition (e.g., relaxation training) in that study.
Current Study
The current study examined changes in drug and alcohol use from pre-SA (assessed at baseline) to follow-up periods targeted at 6 weeks (Time 1; T1), 3 months (Time 2; T2), and 6 months (Time 3; T3) post-SA among recent SA victims who received medical care post assault and who were randomly assigned to one of three conditions: PPRS, Pleasant Imagery and Relaxation Information video (PIRI), and TAU. The current study examined the effects of a shortened version of the PPRS intervention (9 minutes; Miller et al., 2015), shown post-forensic exam, that provided modeling and instruction in coping strategies1. Specifically, PPRS targeted problematic avoidance by encouraging exposure to non-dangerous rape related cues and engagement in activities that do not involve substance use. The present study advances prior work by including an active control condition in addition to TAU. PIRI was chosen as an active control condition because it targeted acute peritraumatic distress, which might also reduce long-term symptomatology. We hypothesized that individuals in the PPRS condition would engage in less alcohol and marijuana use and abuse than those in the PIRI and TAU conditions. Based on prior work showing stronger effects for a video intervention among women with pre-assault substance use and heightened risk for pre-assault substance use among women with a prior history of assault (Resnick et al., 2007b), we hypothesized that individuals who reported pre-SA substance use and a previous SA history would benefit more from the PPRS condition. Given population-level differences in substance use and abuse by race/ethnicity (Grant et al., 2016, Hasin et al., 2015), minority status was explored as an additional moderator.
Materials and Methods
Participants
Girls and women age 15 years or older who were recent victims of SA (rape, suspected rape or attempted rape) and who participated in a SAMFE within 7 days of assault at one of two medical centers in a Midwestern metropolitan area were eligible for inclusion and assessed by medical personnel (N = 711; see Figure 1 for CONSORT diagram). A total of 466 were excluded for the following reasons: declined to participate (n = 209), did not meet inclusion criteria (n = 231), technical/logistical problems (n = 26). The 231 who did not meet inclusion criteria were non-English speaking or presented with serious injuries or medical issues, psychological distress, acute intoxication, or other factors that would preclude participating in informed consent procedures. Of the remaining 245, 233 completed the condition to which they were randomly assigned: PPRS (n = 77), PIRI (n = 77), and TAU (n = 79).
Figure 1.
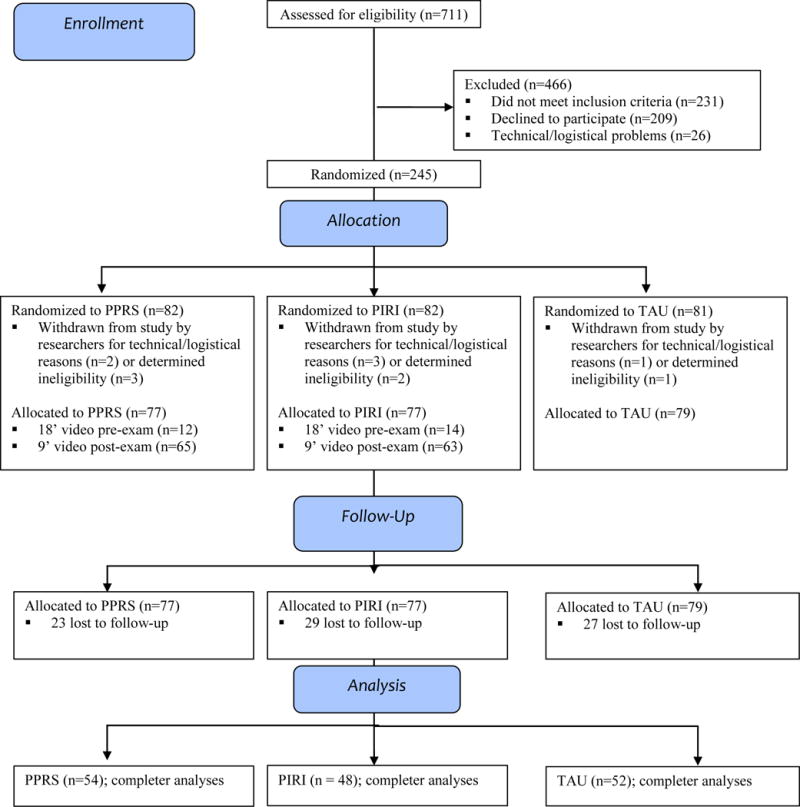
Participant Flow Diagram.
Of the 233 participants, 154 (66%) completed one or more follow-up assessments (54 in PPRS, 48 in PIRI, 52 in TAU). Comparisons to nonparticipants indicated no differences on age or race [except that those who participated were more likely to indicate more than one race than nonparticipants (11.6% vs. 1.7%, χ2 (1, N = 407) = 14.2, p < .0005)]. Treatment groups also did not differ in terms of age, minority status, marital status, education, household income, student status, or employment status (see Table 1).
Table 1.
Prevalence of demographic characteristics and risk factors within study condition
| Overall % (n) | PPRS | PIRI | TAU | F/X2 (p) | |
|---|---|---|---|---|---|
| Age M (SD) | 27.5 (9.3) | 26.9 | 29.1 | 26.7 | 0.98 (.38) |
| Education | 5.35 (.25) | ||||
| Less than HS diploma | 22.7 (35) | 27.8 (15) | 22.9 (11) | 17.3 (9) | |
| HS diploma/some college | 68.2 (105) | 59.3 (32) | 66.7 (32) | 78.8 (41) | |
| College/graduate degree | 9.1 (14) | 13.0 (7) | 10.4 (5) | 3.8 (2) | |
| Marital status | 5.95 (.20) | ||||
| Married/cohabitating | 13.6 (21) | 16.7 (9) | 10.4 (5) | 13.5 (7) | |
| Single | 74.0 (114) | 72.2 (39) | 68.8 (33) | 80.8 (42) | |
| Divorce/separate/widow | 12.3 (19) | 11.1 (6) | 20.8 (10) | 5.8 (3) | |
| Household income | 3.91 (.42) | ||||
| <$25,000 | 83.9 (115) | 84.8 (39) | 78.3 (36) | 88.9 (40) | |
| $25,000–$50,000 | 12.4 (17) | 10.9 (5) | 19.6 (9) | 6.7 (3) | |
| >$50,000 | 3.6 (5) | 4.3 (2) | 2.2 (1) | 4.4 (2) | |
| Student (yes) | 13.6 (21) | 11.1 (6) | 10.4 (5) | 19.2 (10) | 2.10 (.35) |
| Employed (yes) | 34.4 (53) | 33.3 (18) | 35.4 (17) | 34.6 (18) | 0.05 (.98) |
| Minority status | 57.1 (88) | 66.7 (36) | 53.8 (28) | 50.0 (24) | 3.23 (.20) |
| Prior sexual assault | 61.7 (95) | 66.7 (36) | 57.7 (30) | 60.4 (29) | 0.95 (.62) |
| Past-year binge drinking | 44.2 (68) | 50.0 (27) | 48.1 (25) | 33.3 (25) | 3.58 (.17) |
| Past-year marijuana use | 46.8 (72) | 42.6 (23) | 51.9 (27) | 45.8 (22) | .95 (.62) |
Measures
Demographics
Participants provided self-report data on their age, race (White, Black or African American, Asian, American Indian/Alaskan Native, Hawaiian/Pacific Islander, Mixed Race, Other)/ethnicity (Hispanic/non-Hispanic), marital status, education, student/employment status, and household income.
Prior sexual assault
At the medical exam and at initial follow-up (T1), participants were asked whether, other than the incident that brought them to the hospital, anyone had ever used force or threat of force to have unwanted sexual contact with them. A “yes” response to either question was coded as 1.
Negative affect at ED visit
The negative affect subscale of the Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988) consists of 10 descriptors of negative affect (NA) “right now” (Watson et al., 1988). Items are rated on a 5-point scale ranging from 1 (“very slightly or not at all”) to 5 (“extremely”) yielding a total subscale score ranging from 10 to 50 (Watson et al., 1988). Watson and colleagues reported coefficient alpha of .85 for the NA subscale as measured “right now” as well as good discriminant validity based on low correlations between the NA and positive affect (PA) subscales. Coefficient alpha in the current study was .86 and .91 for pre and post-exam administrations, respectively. The PANAS was administered pre-exam as a measure of potential differences in distress across groups as well as post-exam as a validity check regarding intervention condition.
Alcohol use and problems
Two measures were used to assess alcohol use and abuse. First, at each follow-up, participants were asked how many days they drank alcohol during the past 14 days and how many drinks they consumed on average on days when they drank. Days of drinking and number of drinks per day were multiplied to yield alcohol use at each follow-up. Second, the 10-item Alcohol Use Disorders Identification Test (AUDIT) (Saunders et al., 1993) was used to assess drinking problems in the year prior to the rape at T1 or since the index SA at T3. If participants reported at least monthly binge drinking (four or more drinks on a single occasion) in the year prior to the rape on the AUDIT, they were coded as positive for pre-SA binge drinking. The AUDIT has good psychometric properties (de Meneses-Gaya et al., 2009); coefficient alphas in the current sample at T1 and T3 were .89 and .91, respectively.
Marijuana use and problems
Two measures were used to assess marijuana use and drug use problems. First, at T1, participants were asked whether they had ever used marijuana in the 12 months prior to the rape. At each follow-up, participants were asked the number of days they had used marijuana in the past 14 days. Second, the Drug Abuse Screening Test (DAST) (Skinner, 1982) was given to quantify drug use problems in the year prior to the rape at T1 and since the index assault at T3. The DAST has moderate to high levels of reliability, validity, sensitivity, and specificity (Yudko et al., 2007). Coefficient alphas in the current sample at T1 and T3 were .85 and .86, respectively.
Intervention Conditions
Prevention of Post-Rape Stress (PPRS) video intervention
This 9-minute2 video entitled Steps to Recovery included a female narrator providing information that could be used by victims to prevent future emotional problems and substance abuse, such as instructions for proper implementation of self-directed exposure exercises, methods to recognize and terminate inappropriate avoidance, and strategies to engage in activities that specifically did not involve alcohol or drug use and avoid situations or cues that have been triggers for use.
Pleasant Imagery and Relaxation Instruction (PIRI) video intervention
This 9 minute video included a female narrator providing instructions in diaphragmatic breathing, use of words such as relax paired with exhalation, instructions regarding muscle relaxation, and pleasant nature-related imagery and sounds. The original DVD was a commercial product entitled Relax ©, David Garrigus Productions, that was edited for content and length.
Treatment As Usual (TAU)
TAU involved completion of a SA examination performed by a Sexual Assault Nurse Examiner.
Procedures
The trial is registered at clinicaltrials.gov under the registration number NCT01430624 and includes protocol information, although full protocol is not publicly available. All procedures were approved by two University and two affiliated hospital Institutional Review Boards. Participants provided written informed consent at the time of the SAMFE which included access to medical records and self-report information. The study was designed as a parallel trial with an allocation ratio of 1:1:1. Initial sample size was determined via power analysis, and as many participants as possible were recruited before funding ended. A computerized random numbers generator was used to randomly assign participants to one of three conditions via a stratified blocked randomization procedure with variable block sizes of 9 or 12. Nurses who enrolled participants immediately after the study commenced (n = 28, 18%; henceforth referred to as phase 1) accessed videos for participants via a secure internet link and administered videos prior to the medical exam. Following an approved change of scope, those enrolled in phase 2 (n = 126) were administered videos on CDs following the medical exam that were stored in envelopes prepared by a study coordinator and labeled only with a participant subject number until opened by the nurse, who was blind to study condition to that point. Participants completed up to three structured telephone follow-up interviews targeted at 1.5, 3, and 6 months post-SA conducted by Counseling Psychology doctoral students who were blind to study condition. Phase 1 participants received $25 at the time of the exam but this was increased to $50 for phase 2 participants given the time required.
Data Analytic Plan
To examine whether intervention conditions had a main effect on alcohol or marijuana use at follow-up or interacted with minority status, prior SA history, or relevant past-year substance use (e.g., past year binge drinking for alcohol-related outcomes), separate multiple regression models predicting alcohol and marijuana use at each of the three follow-ups were conducted in Mplus version 7.4 (Muthén and Muthén, 2014). Alcohol use (days × drinks) was log-transformed due to skewness and kurtosis. Number of marijuana use days in the previous 2 weeks was treated as a count variable using Poisson models. AUDIT and DAST scores at T3 also served as outcomes. Predictors included two dummy coded variables reflecting the contrast between the PPRS and PIRI conditions as well as between the PPRS and TAU conditions, minority status, prior SA history, and relevant substance use in the year prior to the first assessment. Analyses were conducted in two steps: 1) main effects of each predictor controlling for the main effects of all other predictors; 2) interactions between the dummy coded intervention conditions and each of the other predictor variables (minority status, prior SA history, and past-year substance use) while controlling for all main effects. Although the primary question was whether the PPRS condition was more effective than PIRI or TAU, we also compared the PIRI and TAU conditions (data available upon request). Missing data were handled via Maximum Likelihood estimation with robust standard errors (MLR). Due to the large number of effects tested, a Bonferroni correction was applied such that only p-values of less than .0004 were considered significant (124 effects tested with an alpha of .05).
Results
Descriptive analyses
Recruitment occurred between May 2009 and December 2013. Of the 233 participants enrolled in the study at the ED, 66% (n = 154) completed the first follow-up interview approximately 2 months following the medical exam (M days = 56.95, SD = 24.87); 88% (n = 135) completed the second follow-up interview (Time 2) 3.5 months after the medical exam (M days = 107.63, SD = 25.17), and 79% (n = 121) completed the third follow-up interview (Time 3) 6.5 months after the medical exam (M days = 195.20, SD = 55.38). Those who completed at least one follow-up (n = 154) did not differ from study non-completers (n = 79) on study condition, χ2 (2) = 1.05, p = .59; age, F = .05, p = .83; or minority status, χ2 (2) = 1.19, p = .28). Nearly two-thirds had a prior SA history, 57% identified as racial/ethnic minority (30.5% Black, 8.4% Native American, 11.7% Mixed Race; 11% Hispanic), 44% reported monthly binge drinking in the previous year, and 47% reported marijuana use in the previous year.
Regression Models Predicting Alcohol Use at Each Follow-Up
Unstandardized coefficients for main effects models and interaction models predicting alcohol use (days × drinks) in the previous 2 weeks at each follow-up are presented in Table 2. Main effects models revealed no significant predictors of alcohol use at any time point. However, past-year binge drinking interacted with the PPRS v TAU comparison such that among women who reported past-year binge drinking, those in the PPRS condition had significantly lower log odds of T3 alcohol use compared to women in the TAU condition (p<.0004; Figure 2 Panel B). There was a trend for women in the PPRS condition to have lower log odds of T3 alcohol use compared to those in the PIRI condition among those who reported binge drinking (Figure 2 Panel A), as well as for minority women in the PPRS condition to have lower log odds of T3 alcohol use compared to minority women in the TAU condition (Figure 2 Panel C).
Table 2.
Predictors of Days of Alcohol Use (Days × Drinks) at Each Time Point
| Main Effect Models | Interaction Models | |||||
|---|---|---|---|---|---|---|
| B (SE) | Beta | T | B (SE) | Beta | T | |
| Time 1 | R2 = .09 | R2 = .08 | ||||
|
| ||||||
| Past-year binge drinking | 0.14 (0.11) | 0.14 | 1.31 | 0.23 (0.17) | 0.22 | 1.37 |
| PIRI v PPRS | 0.07 (0.12) | 0.07 | 0.59 | 0.18 (0.26) | 0.17 | 0.69 |
| TAU v PPRS | 0.18 (0.11) | 0.17 | 1.68 | 0.10 (0.23) | 0.09 | 0.43 |
| Minority status | 0.02 (0.13) | 0.02 | 0.16 | 0.23 (0.16) | 0.23 | 1.51 |
| Prior SA | 0.03 (0.13) | 0.03 | 0.23 | 0.06 (0.16) | 0.06 | 0.37 |
| PIRI v PPRS × binge | – | – | – | −0.22 (0.26) | −0.17 | 0.85 |
| TAU v PPRS × binge | – | – | – | −0.06 (0.24) | −0.04 | −0.27 |
| PIRI v PPRS × minority | – | – | – | −0.14 (0.26) | −0.10 | −0.54 |
| TAU v PPRS × minority | – | – | – | −0.36 (0.24) | −0.24 | −1.48 |
| PIRI v PPRS × prior SA | – | – | – | 0.11 (0.26) | 0.09 | 0.43 |
| TAU v PPRS × prior SA | – | – | – | 0.28 (0.24) | 0.20 | 1.20 |
|
| ||||||
| Time 2 | R2 = .08 | R2 = .12 | ||||
|
| ||||||
| Past-year binge | 0.20 (0.11) | 0.21 | 1.78 | 0.08 (0.21) | 0.17 | 0.38 |
| PIRI v PPRS | 0.04 (0.11) | 0.04 | 0.31 | 0.06 (0.26) | 0.13 | 0.22 |
| TAU v PPRS | 0.10 (0.10) | 0.10 | 0.19 | −0.21 (0.27) | −0.46 | −0.77 |
| Minority status | 0.16 (0.11) | 0.16 | 0.31 | −0.04 (0.22) | −0.09 | −0.19 |
| Prior SA | 0.18 (0.13) | 0.19 | 0.90 | 0.07 (0.16) | 0.15 | 0.43 |
| PIRI v PPRS × binge | – | – | – | 0.16 (0.27) | 0.14 | 0.58 |
| TAU v PPRS × binge | – | – | – | 0.35 (0.28) | 0.28 | 1.26 |
| PIRI v PPRS × minority | – | – | – | −0.04 (0.28) | −0.03 | −0.14 |
| TAU v PPRS × minority | – | – | – | 0.36 (0.28) | 0.26 | 1.27 |
| PIRI v PPRS × prior SA | – | – | – | 0.004 (0.23) | 0.003 | 0.02 |
| TAU v PPRS × prior SA | – | – | – | 0.08 (0.27) | 0.07 | 0.31 |
|
| ||||||
| Time 3 | R2 = .09 | R2 = .21 | ||||
|
| ||||||
| Past-year binge | 0.17 (0.12) | 0.17 | 1.38 | −0.37 (0.17) | −0.36 | −2.19* |
| PIRI v PPRS | −0.002 (0.13) | −0.002 | −0.01 | −0.66 (0.26) | −0.64 | −2.53** |
| TAU v PPRS | 0.16 (0.12) | 0.16 | 1.42 | −0.96 (0.25) | −0.90 | −3.80**** |
| Minority status | −0.09 (0.13) | −0.08 | −0.66 | −0.27 (0.16) | −0.26 | −1.72 |
| Prior SA | −0.21 (0.16) | −0.20 | −1.35 | 0.18 (0.12) | 0.18 | 1.53 |
| PIRI v PPRS × binge | – | – | – | 0.65 (0.24) | 0.55 | 2.67** |
| TAU v PPRS × binge | – | – | – | 0.95 (0.26) | 0.71 | 3.69**** |
| PIRI v PPRS × minority | – | – | – | 0.14 (0.24) | 0.11 | 0.57 |
| TAU v PPRS × minority | – | – | – | 0.71 (0.29) | 0.45 | 2.48** |
| PIRI v PPRS × prior SA | – | – | – | 0.09 (0.22) | 0.08 | 0.42 |
| TAU v PPRS × prior SA | – | – | – | −0.21 (0.24) | −0.16 | −0.87 |
Note: The Prevention of Post-Rape Stress (PPRS) is the comparison condition (coded 0) in dummy variables in all analyses.
p<.05,
p<0.01,
p<0.001;
p<.0004
Figure 2.
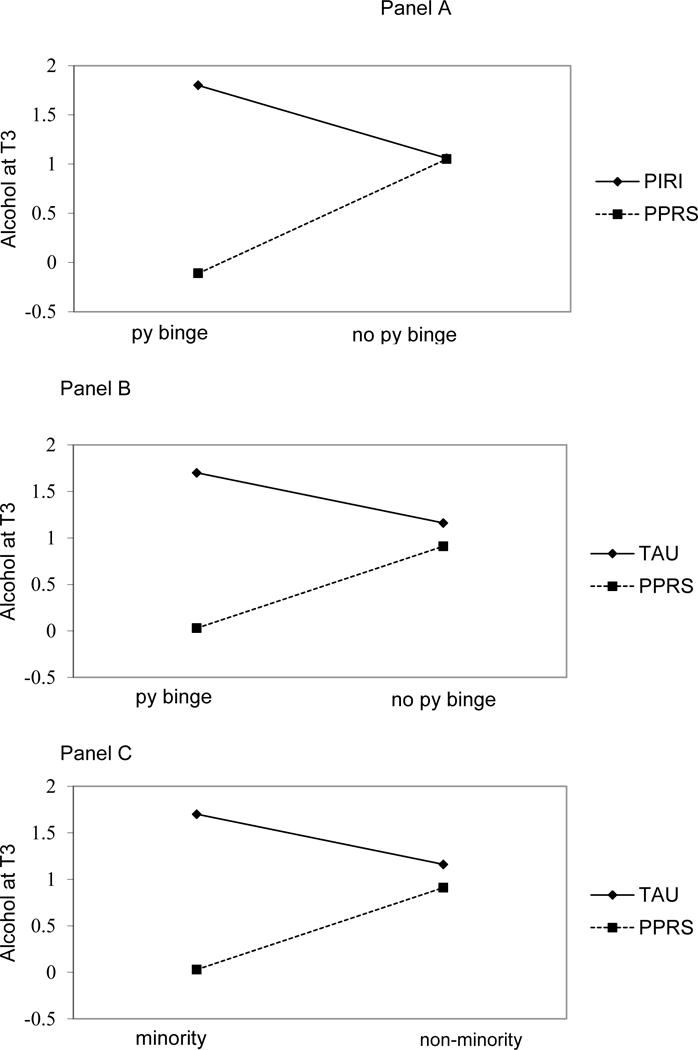
Panel A. Interaction between past year binge drinking and PPRS v PIRI on T3 alcohol use
Panel B. Interaction between past-year binge drinking and PPRS v TAU on T3 alcohol use
Panel C. Interaction between minority status and PPRS v TAU on T3 alcohol use
Regression Models Predicting AUDIT at Follow-Up
T1 AUDIT scores were the only significant predictor of T3 AUDIT scores (see Table 3). There were no significant main effects or interactions associated with the intervention conditions.
Table 3.
Predictors of T3 Alcohol Use Problems on the Alcohol Use Disorders Identification Test
| Main Effects Models | Interaction Models | |||||
|---|---|---|---|---|---|---|
| B (SE) | Beta | T(p) | B (SE) | Beta | T(p) | |
| Time 3 | R2 = .11 | R2 = .14 | ||||
|
| ||||||
| PIRI v PPRS | 0.41 (1.92) | 0.02 | 0.21 (0.83) | 3.28 (2.63) | 0.19 | 1.25 |
| TAU v PPRS | 0.001 (2.20) | 0.001 | 0.001 (1.00) | −0.08 (2.47) | −0.004 | −0.03 |
| Minority status | 1.56 (1.65) | 0.09 | 0.94 (0.35) | 1.11 (3.30) | 0.07 | 0.34 |
| Prior SA | 1.17 (1.46) | 0.07 | 0.80 (0.42) | 3.21 (2.64) | 0.19 | 1.22 |
| T1 AUDIT | 0.32 (0.09) | 0.33 | 3.63**** | 0.35 (0.09) | 0.37 | 3.95**** |
| PIRI v PPRS × minority | – | – | – | −1.60 (3.85) | −0.08 | −0.42 |
| TAU v PPRS × minority | – | – | – | 3.62 (4.36) | 0.16 | 0.83 |
| PIRI v PPRS × prior SA | – | – | – | −3.21 (3.43) | −0.16 | −0.94 |
| TAU v PPRS × prior SA | – | – | – | −2.50 (3.72) | −0.12 | −0.67 |
Note: The Prevention of Post-Rape Stress (PPRS) is the comparison condition (coded 0) in dummy variables in all analyses.
p<.0004
Regression Models Predicting Marijuana Use at Each Follow-Up
Unstandardized coefficients for main effects models and interaction models predicting days of marijuana use in the previous 2 weeks at each follow-up are presented in Table 4. Main effects models revealed that past-year marijuana use was a significant positive predictor of past 2-week marijuana use frequency at each follow-up (ps<.0004). Interaction models revealed that past-year marijuana use interacted with the PIRI v PPRS comparison to predict marijuana use at T1 (p<.0004). Specifically, although those in the PPRS condition generally had lower marijuana use than those in the PIRI condition at T1, this difference was only statistically significant among those who did not report past-year marijuana use (See Figure 3 Panel A). Additionally, prior SA history interacted with the PIRI v PPRS comparison to predict marijuana use at T1 and T2 such that among those with a prior SA history the PPRS and PIRI conditions had a similar effect; however, among those without a prior SA history, those in the PPRS condition reported fewer days of marijuana use at T1 and T2 compared to those in the PIRI condition (T1 pattern depicted in Figure 3 Panel B).
Table 4.
Predictors of Days of Marijuana Use at Each Time Point
| Main Effect Models | Interaction Models | |||||
|---|---|---|---|---|---|---|
| B (SE) | Beta | T(p) | B (SE) | Beta | T(p) | |
| Time 1 | R2 = .19 | R2 = .22 | ||||
|
| ||||||
| Past-year marijuana | 1.84 (0.42) | 0.89 | 4.36**** | 1.79 (0.56) | 0.17 | 3.20*** |
| PIRI v PPRS | −0.03 (0.35) | −0.02 | −0.10 | −4.22 (0.97) | −1.26 | −4.74**** |
| TAU v PPRS | 0.38 (0.36) | 0.17 | 1.07 | 0.63 (0.84) | 0.05 | 0.75 |
| Minority status | 0.71 (0.31) | 0.34 | 2.32* | 0.72 (0.52) | 0.07 | 1.38 |
| Prior SA | 0.44 (0.32 | 0.21 | 1.37 | −0.09 (0.55) | −0.01 | −0.16 |
| PIRI v PPRS × marijuana | – | – | – | 7.14 (0.67) | 0.84 | 7.62**** |
| TAU v PPRS × marijuana | – | – | – | −0.56 (0.80) | −0.04 | −0.71 |
| PIRI v PPRS × minority | – | – | – | −0.41 (0.70) | −0.03 | 0.59 |
| TAU v PPRS × minority | – | – | – | 0.17 (0.72) | 0.01 | 0.23 |
| PIRI v PPRS × prior SA | – | – | – | 3.21 (0.86) | 0.24 | 3.74**** |
| TAU v PPRS × prior SA | – | – | – | −0.08 (0.68) | −0.01 | −0.12 |
|
| ||||||
| Time 2 | R2 = .19 | R2 = .22 | ||||
|
| ||||||
| Past-year marijuana | 1.70 (0.42) | 0.90 | 4.08**** | 1.31 (0.57) | 0.44 | 2.32* |
| PIRI v PPRS | −0.46 (0.35) | −0.23 | −1.32 | −3.30 (1.21) | −1.04 | −2.73** |
| TAU v PPRS | −0.55 (0.37) | −0.28 | −1.49 | −0.62 (1.04) | −0.20 | −0.60 |
| Minority status | 0.59 (0.32) | 0.31 | 1.82 | 0.78 (0.59) | 0.26 | 1.33 |
| Prior SA | 0.39 (0.35) | 0.20 | 1.13 | 0.27 (0.59) | 0.09 | 0.46 |
| PIRI v PPRS × marijuana | – | – | – | 1.01 (0.78) | 0.26 | 1.31 |
| TAU v PPRS × marijuana | – | – | – | 0.61 (0.86) | 0.14 | 0.71 |
| PIRI v PPRS × minority | – | – | – | −0.64 (0.78) | −0.17 | −0.83 |
| TAU v PPRS × minority | – | – | – | −0.08 (0.74) | −0.02 | −0.10 |
| PIRI v PPRS × prior SA | – | – | – | 2.69 (0.94) | 0.73 | 2.86** |
| TAU v PPRS × prior SA | – | – | – | −0.81 (0.81) | −0.22 | −0.10 |
|
| ||||||
| Time 3 | R2 = .22 | R2 = .29 | ||||
|
| ||||||
| Past-year marijuana | 3.39 (0.60) | 0.96 | 5.60**** | 4.11 (1.04) | 0.40 | 3.94**** |
| PIRI v PPRS | 0.72 (0.45) | 0.20 | −1.60 | 0.36 (1.60) | 0.03 | 0.22 |
| TAU v PPRS | 0.58 (0.51) | 0.16 | 1.15 | −8.92 (1.41) | −0.82 | −6.31**** |
| Minority status | 0.30 (0.36) | 0.08 | 0.83 | 0.92 (0.70) | 0.09 | 1.33 |
| Prior SA | 0.28 (0.38) | 0.08 | 0.73 | −0.87 (0.67) | −0.08 | −1.29 |
| PIRI v PPRS × marijuana | – | – | – | −1.91 (1.23) | −0.15 | −1.55 |
| TAU v PPRS × marijuana | – | – | – | 9.74 (1.12) | 0.67 | 8.68**** |
| PIRI v PPRS × minority | – | – | – | −0.77 (0.85) | −0.06 | −0.90 |
| TAU v PPRS × minority | – | – | – | −0.88 (0.93) | −0.06 | −0.94 |
| PIRI v PPRS × prior SA | – | – | – | −3.43 (0.92) | 0.27 | −3.75**** |
| TAU v PPRS × prior SA | – | – | – | 0.23 (0.92) | 0.02 | 0.25 |
Note: The Prevention of Post-Rape Stress (PPRS) is the comparison condition (coded 0) in dummy variables in all analyses.
p<0.05,
p<0.01,
p<0.001,
p<.0004
Figure 3.
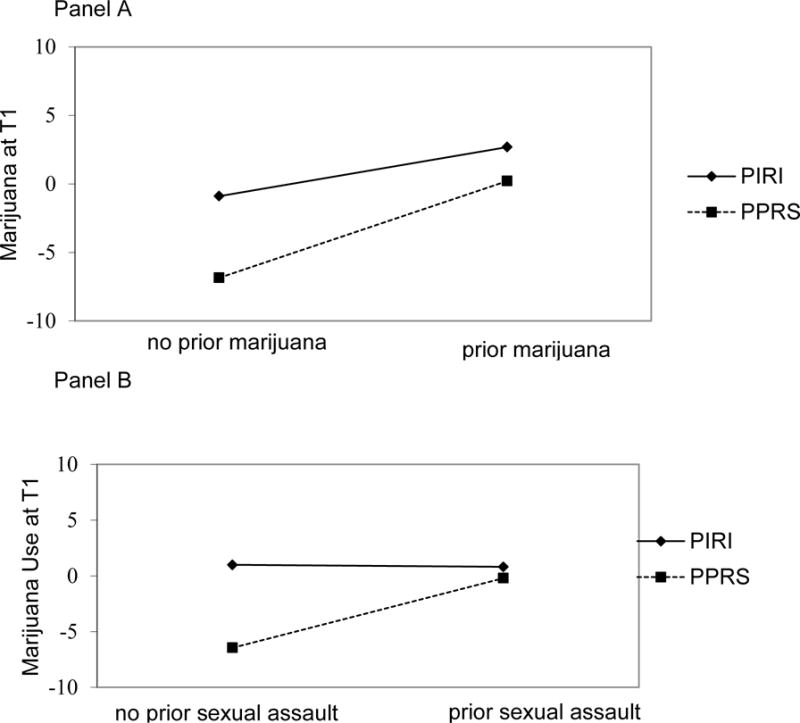
Panel A. Interaction between prior sexual assault and PIRI v PPRS on Days of Marijuana Use at T1.
Panel B. Interaction between past-year marijuana use and PIRI v PPRS on Days of Marijuana Use at T1.
Panel C. Panel B. Interaction between past-year marijuana use and TAU v PPRS on Days of Marijuana Use at T1.
At T3, the PPRS v TAU comparison interacted with pre-SA marijuana use such that among those who did not report past-year marijuana use, those in the PPRS condition reported fewer days of marijuana use compared to those in the TAU condition (p<.0004); among those who reported past-year marijuana use, intervention condition did not have an effect on marijuana use (see Figure 4 Panel A). The interaction pattern between the PPRS v PIRI comparison and prior SA that was observed at T1 and T2 shifted at T3 such that those in the PPRS condition who had a prior SA history reported fewer days of marijuana use at T3 compared to those in the PIRI condition who had a prior SA history (p<.0004; see Figure 4 Panel B). Among women who did not have a prior SA history, marijuana use frequency did not differ as a function of treatment condition.
Figure 4.
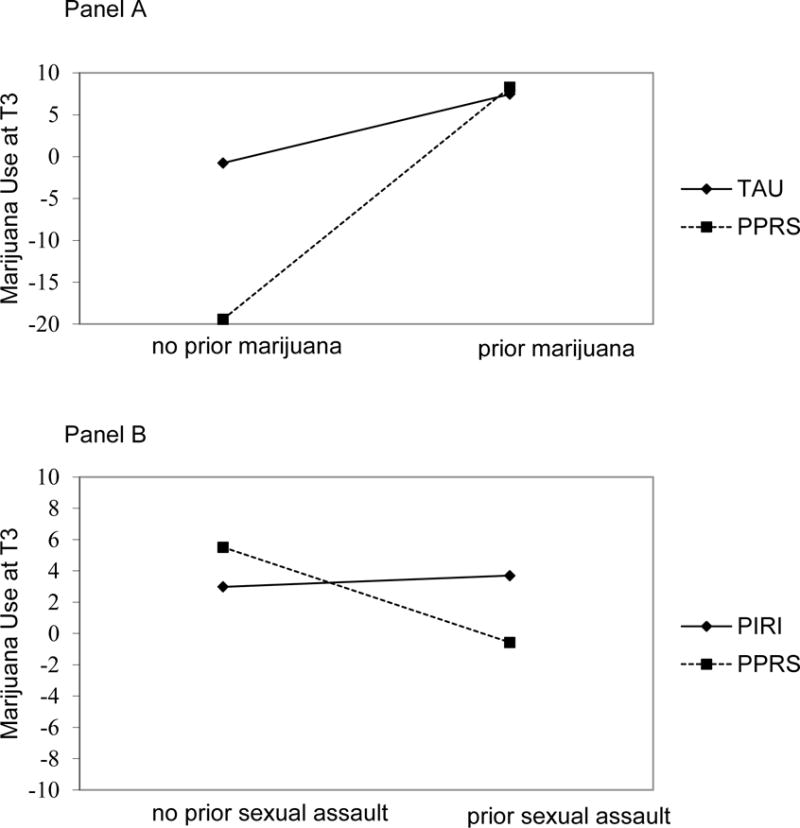
Interaction between prior sexual assault and PIRI v PPRS on Days of Marijuana Use at T3.
Regression Models Predicting DAST at Follow-Up
T1 DAST significantly predicted T3 DAST (p<.001). There also was a trend for the interaction between the TAU vs PPRS comparison and minority status to be associated with T3 DAST scores such that non-minority women in the PPRS condition had lower DAST scores than minority women in the PPRS and TAU and non-minority women in the TAU.
Discussion
The current study adds to the emerging literature concerning secondary prevention of substance use among recent SA victims using technology-based interventions that can be disseminated within EDs or other acute care settings (Resnick et al., 2007b). We extended previous findings comparing PPRS to TAU by also examining whether PPRS performed better than an active treatment comparison control that targeted peritraumatic distress by teaching relaxation, a technique that could have a broad impact on health. Our findings partially supported our hypotheses. There were no treatment condition main effects on substance use. However, we found several significant interactions suggesting that the PPRS video may be effective at reducing alcohol and marijuana use 6 months post-SA (T3) for some subgroups of women. Considering alcohol, PPRS resulted in less use than PIRI or TAU for women who engaged in past-year binge drinking. PPRS also resulted in less alcohol use than TAU for minority women. Patterns differed for marijuana use. PPRS resulted in less marijuana use days compared to TAU among those who reported no past-year pre-SA marijuana use. Taken together, these results indicated that brief mental health videos can have effects on substance use up to six months after a recent SA for some victims.
There was a complicated interaction trajectory found for treatment condition (PPRS vs. PIRI) and prior SA history on number of marijuana use days. At T1 and T2, PPRS and PIRI had similar effects on marijuana use for those who had a prior SA history. For those without a prior SA history, PPRS was more effective at reducing number of marijuana use days compared to PIRI at T1. However, at T3, among those with a prior SA history, those in the PPRS condition reported fewer days of marijuana use compared to those in the PIRI condition. This complicated pattern suggests that the compounding effects of sexual re-victimization may not be linearly related to subsequent substance use, and that the PPRS may be initially more effective at reducing substance use among those without a prior SA history. In the long-term, however, the PPRS appears to be more effective for those with a prior SA history. Data showing reciprocal associations between assault and substance use (Kilpatrick et al., 1997) highlight the possibility that women with a prior assault may have engaged in more marijuana use prior to the index rape and thus had more difficulty breaking this pattern of marijuana use relative to women without a prior assault who perhaps did not have the same substance use history. More research with larger samples is needed to replicate this differential trajectory based on SA history, examine possible interactions between prior use and prior assault on substance use trajectories, and determine why the PPRS is effective for some and not others at different time points.
Previous research found significant effects for PPRS in reducing marijuana use frequency among women with recent pre-rape marijuana use (Resnick et al., 2007b). The current study adds support for the use of the PPRS for those who engage in pre-SA alcohol use. However, the pattern of results differed for marijuana use such that the PPRS and PIRI were related to lower frequency of use compared to TAU at various time points among those who reported no use in the prior year rather than among pre-rape users. This is promising for primary prevention of marijuana use. However, it is unclear whether differences in findings may relate to differences in methods which included use of a broader time frame for prior use, screening by nurse examiners rather than on-call project assistants, and limited power to detect differences among those with prior use, given reduced sample size and evaluation of three treatment conditions.
Providing recent SA victims with skills, either related to relaxation (PIRI) or other coping (PPRS), may be beneficial using this universal approach, providing information to all. This universal approach also demonstrates feasibility of addressing substance use for recent SA victims within an ED setting. As we have previously reported (Resnick et al., 2012, 2013), a more targeted approach to intervention that includes additional treatment content for those with problem use would be beneficial, beyond the current universal approach that delivers similar content to all victims of SA. One possible approach would be to provide personalized feedback through motivational interviewing techniques. This approach has been implemented with a high-risk sample of college women under the age of 21 who engaged in heavy episodic drinking and found reductions in heavy episodic drinking among women with more severe sexual assault histories when both alcohol use and sexual assault risk were targeted using a web-based intervention (Gilmore, Lewis, and George, 2015). Future work could incorporate more personalized feedback interventions using both screening, brief intervention, and referral (SBIRT) techniques (Madras et al., 2009) and motivational interviewing techniques with the video components incorporated. This enhancement may increase the effect of the intervention and the universal approach could provide a warm hand off for more personalized interventions for individuals with more severe substance use problems.
There were no significant main effects or interactions with the treatment conditions on alcohol or drug abuse problems as assessed by standardized measures. Therefore, although video-based interventions may be effective at reducing non-problem alcohol and marijuana use for some, as noted above, more intensive interventions may be warranted for individuals with substance use disorders.
Findings indicated a trend for minority status to serve as a protective factor for alcohol use at T3 (in the PPRS condition specifically) but it was a significant risk factor for marijuana use frequency at T1 and T3 (in the PPRS condition specifically). Findings fit with national data suggesting that some racial/ethnic groups have lower risk for alcohol use disorders but increased risk for marijuana use disorders compared to whites (Grant et al., 2015, Hasin et al., 2015); thus, these somewhat oppositional findings may relate in part to baseline differences in substance use among minority and white participants. Taken as a whole, these data underline the importance of taking into consideration minority status, pre-SA substance use, and prior SA history when explaining substance use after an acute assault.
Strengths and Limitations
There are several strengths and limitations to the current study. First, it is a strength that the intervention was implemented within an ED setting and that a universal and automated standardized intervention was implemented by ED providers. However, pragmatic concerns arose that must be considered when interpreting the findings. For example, most participants received brief versions of the videos post-exam that retained key content and were more feasible to administer in this context than the full length videos shown pre-exam. Although there were no significant differences in distress between groups who received the brief and long versions of the video it may be important to note that all participants did not undergo the same procedure. Second, although it is a strength that the current study compared PPRS to both PIRI and TAU, the number of participants assigned to each condition ranged from 48 to 54. This sample size is relatively small to detect interaction effects, therefore, findings should be interpreted cautiously and larger studies should aim to replicate these findings. Third, the current study only included women because women are more likely to experience SA compared to men (Pimlott-Kubiak and Cortina, 2003); however, the results may not generalize to men or transgender individuals who are also at high risk of experiencing SA. Similarly, although the mean age and racial breakdown of the current sample is consistent with epidemiologic studies on rape victims presenting to the emergency department (Avegno et al., 2009), our sample was relatively low income, unemployed, single, and a majority had experienced a prior sexual assault; therefore it is unclear whether these findings would translate to rape victims with other demographic characteristics. Fourth, it is a strength that the current study examined recent SA victims as most research on SA and substance use focuses on a more distal analysis examining SA history and current use months or years after the SA. However, the exclusion criteria (e.g., not speaking English or presenting with serious injuries, psychological distress, acute intoxication) may have biased the sample towards including healthier individuals and impacted the results. Fifth, the analyses did not take into account other mental health symptoms including depression and posttraumatic stress symptoms. Future work with larger samples should examine substance use and mental health variables within the same model. A final limitation is that we included only participants who had at least one follow-up because we did not collect baseline substance use data; future studies should collect these data to conduct intent-to-treat analyses.
Conclusions
The current study adds to the literature on acute mental health treatments for recent SA victims. Although there were no main effects for the interventions, moderation analyses suggested that the PPRS may be effective at reducing substance use following an acute assault for some recent SA victims who are at particularly high risk for substance use, including those with a prior SA history, and those who reported binge drinking in the year prior to the SA. In addition, results indicated reduced marijuana use among those who did not report use in the year prior to rape.
Table 5.
Predictors of T3 Drug Abuse Problems on the Drug Abuse Screening Test
| Main Effects Models | Interaction Models | |||||
|---|---|---|---|---|---|---|
| B (SE) | Beta | T(p) | B (SE) | Beta | T(p) | |
| Time 3 | R2 = .05 | R2 = .33 | ||||
|
| ||||||
| PIRI v PPRS | −0.73 (0.44) | −0.14 | −1.65 | −1.09 (0.74) | −0.21 | −1.46 |
| TAU v PPRS | 0.21 (0.54) | 0.10 | 0.38 | −0.90 (0.77) | −0.18 | −1.17 |
| Minority status | 0.09 (0.40) | 0.02 | 0.21 | −1.00 (0.70) | −0.20 | −1.43 |
| Prior SA | 0.43 (0.38) | 0.09 | 1.13 | 0.56 (0.67) | 0.11 | 0.56 |
| T1 DAST | 0.47 (0.11) | 0.49 | 4.43**** | 0.50 (0.10) | 0.52 | 4.96**** |
| PIRI v PPRS × minority | – | – | – | 0.54 (0.89) | 0.09 | 0.54 |
| TAU v PPRS × minority | – | – | – | 2.45 (0.97) | 0.38 | 2.52* |
| PIRI v PPRS × prior SA | – | – | – | −0.05 (0.82) | −0.01 | −0.06 |
| TAU v PPRS × prior SA | – | – | – | −0.37 (1.00) | −0.06 | −0.37 |
Note: The Prevention of Post-Rape Stress (PPRS) is the comparison condition (coded 0) in dummy variables in all analyses.
p<0.05,
p<.0004
Acknowledgments
The study was conducted with support from National Institute on Drug Abuse Grant DA023099. Manuscript preparation was supported by National Institutes of Health Grants MH107641, MH107641-02S1, DA036213, and T32-MH018869. Trial registered at clinicaltrials.gov under the registration number NCT01430624. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or other agencies.
Footnotes
DR. KATE WALSH (Orcid ID : 0000-0002-3996-2683)
The authors have no conflicts of interest to declare.
A small number of participants received a longer version of the video in the current study (see Methods).
A small proportion (n = 28; 18%) of participants received longer (18 minute) versions of the intervention and active control videos that were shown prior to the SAFME and included either the PPRS or PIRI video plus information about the exam. There were no differences among those who received the shorter and longer versions of the intervention and active control in pre-exam PANAS, F (1, 141) = 0.65, p = .42, post-exam PANAS, F (1, 141)= 0.01, p = .91), or assigned treatment condition, χ2 (df = 2) = 1.08, p = .58.
References
- Avegno J, Mills TJ, Mills LD. Sexual assault victims in the emergency department: analysis by demographic and event characteristics. The Journal of Emergency Medicine. 2009;37:328–334. doi: 10.1016/j.jemermed.2007.10.025. [DOI] [PubMed] [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, Stevens M. National intimate partner and sexual violence survey. Atlanta, GA: Centers for Disease Control and Prevention; 2011. p. 75. [Google Scholar]
- Bryan AE, Norris J, Abdallah DA, Stappenbeck CA, Morrison DM, Davis KC, George WH, Danube CL, Zawacki T. Longitudinal change in women’s sexual victimization experiences as a function of alcohol consumption and sexual victimization history: A latent transition analysis. Psychology of violence. 2016;6:271–279. doi: 10.1037/a0039411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Meneses-Gaya C, Zuardi AW, Loureiro SR, Crippa JAS. Alcohol Use Disorders Identification Test (AUDIT): An updated systematic review of psychometric properties. Psychology & Neuroscience. 2009;2:83–97. [Google Scholar]
- Gilmore AK, Lewis MA, George WH. A randomized controlled trial targeting alcohol use and sexual assault risk among college women at high risk for victimization. Behaviour research and therapy. 2015;74:38–49. doi: 10.1016/j.brat.2015.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA psychiatry. 2015;72:757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, Zhang H, Smith SM, Pickering RP, Huang B. Epidemiology of DSM-5 Drug Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions–III. JAMA psychiatry. 2016;73:39–47. doi: 10.1001/jamapsychiatry.2015.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannan SM, Orcutt HK, Miron LR, Thompson KL. Childhood sexual abuse and later alcohol-related problems investigating the roles of revictimization, PTSD, and drinking motivations among college women. Journal of interpersonal violence. 2015:1–21. doi: 10.1177/0886260515591276. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, Pickering RP, Ruan WJ, Smith SM. Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA psychiatry. 2015;72:1235–1242. doi: 10.1001/jamapsychiatry.2015.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen D, Atkins DC, Moore SA, Lindgren KP, Dillworth T, Simpson T. Alcohol Use, Problems, and the Course of Posttraumatic Stress Disorder: A Prospective Study of Female Crime Victims. Journal of Dual Diagnosis. 2011;7:262–279. doi: 10.1080/15504263.2011.620449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, Best CL. A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. Journal of consulting and clinical psychology. 1997;65:834–847. doi: 10.1037//0022-006x.65.5.834. [DOI] [PubMed] [Google Scholar]
- Long L, Ullman SE. Correlates of problem drinking and drug use in black sexual assault victims. Violence and victims. 2016;31:71–84. doi: 10.1891/0886-6708.VV-D-14-00024. [DOI] [PubMed] [Google Scholar]
- Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, Clark HW. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug and alcohol dependence. 2009;99:280–295. doi: 10.1016/j.drugalcdep.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus 7.3. Muthén, Muthén; 2014. p. 3463. [Google Scholar]
- Pimlott-Kubiak S, Cortina LM. Gender, victimization, and outcomes: reconceptualizing risk. Journal of consulting and clinical psychology. 2003;71:528–539. doi: 10.1037/0022-006x.71.3.528. [DOI] [PubMed] [Google Scholar]
- Resnick H, Acierno R, Waldrop AE, King L, King D, Danielson C, Ruggiero KJ, Kilpatrick D. Randomized controlled evaluation of an early intervention to prevent post-rape psychopathology. Behaviour research and therapy. 2007a;45:2432–2447. doi: 10.1016/j.brat.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick HS, Acierno R, Amstadter AB, Self-Brown S, Kilpatrick DG. An acute post-sexual assault intervention to prevent drug abuse: Updated findings. Addictive behaviors. 2007b;32:2032–2045. doi: 10.1016/j.addbeh.2007.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum BO, Kearns MC, Price M, Malcoun E, Davis M, Ressler KJ, Lang D, Houry D. Early intervention may prevent the development of posttraumatic stress disorder: a randomized pilot civilian study with modified prolonged exposure. Biological Psychiatry. 2012;72:957–963. doi: 10.1016/j.biopsych.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption‐II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Skinner HA. The drug abuse screening test. Addictive behaviors. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Yudko E, Lozhkina O, Fouts A. A comprehensive review of the psychometric properties of the Drug Abuse Screening Test. Journal of substance abuse treatment. 2007;32:189–198. doi: 10.1016/j.jsat.2006.08.002. [DOI] [PubMed] [Google Scholar]


