Abstract
Background
The quality of perimortem care received by patients who died at our hospitals was unknown.
Objective
To describe the quality of hospital care experienced in the last week of life, as perceived by decedents' families.
Design
Telephone survey that included established measures and investigator-developed content.
Setting
Large, tertiary care center known for high-quality, cost-effective care.
Participants
Family members of 104 patients who died in-hospital (10% of annual deaths) over the course of 1 year.
Intervention
None.
Measurements
Participant perceptions of the decedent's care, including symptom management, personal care, communication, and care coordination.
Results
Decedents were mostly male (64%), white (96%), married (73%), and Christian (91%). Most survey participants were spouses of the decedent (68%); they were predominately white (98%), female (70%), and Christian (90%) and had a median age of 70 years (range, 35-91 years). Overall satisfaction was high. Pain, dyspnea, and anxiety or sadness were highly prevalent among decedents (73%, 73%, and 55%, respectively) but largely well managed. Most participants believed that decedents were treated respectfully and kindly by staff (87%) and that sufficient help was available to assist with medications and dressing changes (97%). Opportunities for improvement included management of decedents' anxiety or sadness (29%) and personal care (25%); emotional support of the family (57%); communication regarding decedents' illness (29%); and receiving contradictory or confusing information (33%).
Conclusions
Despite high satisfaction with care overall, we identified important unmet needs. Addressing these gaps will improve the care of dying patients.
Keywords: death, decedent, family caregivers, hospitals, quality of healthcare, terminal care
Introduction
Care of dying patients and their families is a critical component of excellent health care; this task is becoming increasingly challenging as the population ages and more Americans suffer and die of chronic disease (1-5). Demographic trends incited an urgent call for improvement in end-of-life care in the United States (US) in 2000 (6), and it is improving slowly, with fewer hospital days at the end of life and better use of hospice (4,7). Still, gaps remain, with more late referrals to hospice more intensive care unit (ICU) use, and more repeat hospitalizations in the last 90 days of life (6,7).
Gaps in quality of end-of-life care are most notable for those dying in the hospital (4,6). One-third of US deaths occur in the hospital (2,4,8), often with suboptimal symptom control (6,9) and medical care that is sometimes perceived to be “more” than patients and families desire (1). Compared with those receiving hospice care at home, people dying in the hospital receive inferior symptom management, poorer communication from health care professionals, less emotional support, and overall lower quality of care (9-12). Furthermore, escalating costs are a growing concern: one-quarter of Medicare spending goes toward caring for patients with severe chronic illness in their last year of life (4). The annual US death rate is rising (13) and the percentage of Americans who die in the hospital remains persistently high (2,4,8), despite most peoples' preference to die at home (14-17).
The Dartmouth Institute reported that chronically ill patients in their last 2 years of life were often better served by more cost-effective medical centers run by organized group practices or integrated hospital systems (1). Not only did more costly and aggressive care fail to improve performance on quality metrics, it often resulted in poorer quality care overall (1,4). In the context of the Dartmouth Atlas data, Mayo Clinic (Rochester, Minnesota) (MCR) received national acclaim for cost-effective end-of-life care and was cited as a benchmark for efficient, high-quality care (1). Despite this approbation, we have little data about the quality of perimortem care received by patients who died at our hospitals. Therefore, we sought to identify additional gaps in our practice that, when addressed, could further improve the end-of-life experience for patients and their families at our hospitals. The objectives of this study were to describe the quality of care experienced in the last week of life by patients who died in-hospital at a large tertiary academic medical center, as perceived retrospectively by decedents' family members, and to determine if any characteristics of the patient, family, or care delivery were associated with actionable gaps in the quality of that experience. These data will serve as a foundation from which improvements in the patient and family experience can be measured.
Patients and Methods
The Mayo Clinic Institutional Review Board approved this study. We conducted telephone surveys of families of 104 patients who died in-hospital at MCR from March 20, 2009 through March 19, 2010. “Family” was defined as the person closest to the decedent, regardless of whether that person was a relative or friend. We sought to study 10% of adult decedents over 1 year, basing our target number on an average of 1,000 annual in-hospital deaths. We recruited participants from 3 separate periods to account for potential seasonal variations.
Study Population
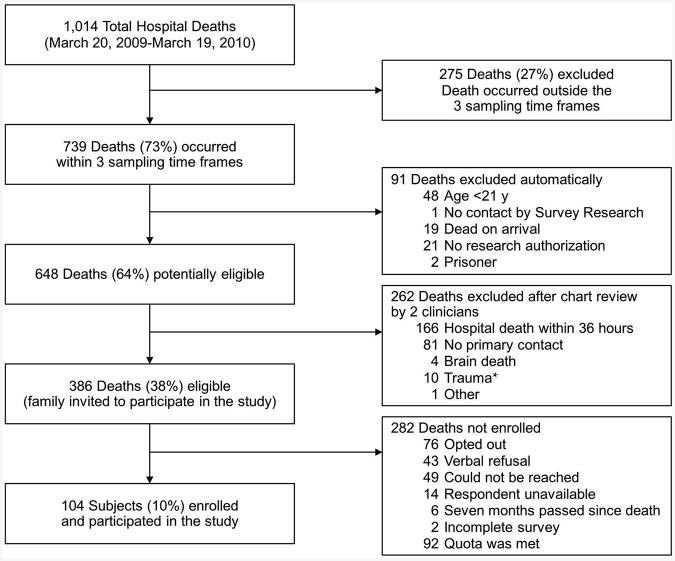
Mayo Clinic Survey Research Center (SRC) specialists screened hospital registration databases for deaths, automatically excluding decedents not meeting initial eligibility criteria (Figure). Two clinicians (E.C.C., A.M.D.) subsequently reviewed the electronic health records of potentially eligible patients, further excluding decedents meeting secondary exclusion criteria (Figure) and determining cause of death.
Figure.
Flowchart Detailing Inclusion and Exclusion Criteria for Participants Surveyed About the Quality of Death and Dying at Mayo Clinic (Rochester, Minnesota). * Trauma was defined as hospital death within 72 hours of a traumatic accident or act of violence.
The study participant was the primary contact listed in the decedent's record, unless he or she identified someone else. Potential participants were contacted 3 to 7 months following the death, after acute grief had diminished but before memory of the experience had faded (18). SRC staff mailed potential research participants an invitation. Eligible participants could opt out by mail, be unavailable by phone, or verbally refuse participation. Verbal consent for research participation was obtained before the interview. Permission to audio-record the interview was requested but did not affect participation. Unless otherwise noted, participants were asked to answer every question but any could be declined.
Survey Design
The survey assessed participants' perceptions of quality of care provided in the last week of life and included established measures and investigator-developed content. Survey design was based on a validated tool, the Toolkit After-Death Bereaved Family Member Interview (11,19), and incorporated 5 domains: 1) provide physical comfort and emotional support, 2) attend to emotional and spiritual needs of the family, 3) inform and promote shared decision-making, 4) focus on the individual, and 5) provide coordination of care. To create a comprehensive survey, the research team developed questions addressing issues identified by institutional stakeholders and by relevant literature. The final survey was piloted on 2 bereaved volunteers to ensure face validity and feasibility.
Data Management and Analysis
Descriptive statistics were used to summarize participant and decedent demographic and clinical data and to convey participants' perceptions of care quality. Because psychometric testing showed poor internal consistency within each domain, we evaluated outcomes by using individual variables. Because of high satisfaction overall and a resulting ceiling effect, we dichotomized all variables to reflect any level of dissatisfaction with the patient's care (eg, participants were either “always” satisfied or “usually, sometimes, or never” satisfied). Any degree of dissatisfaction became our dependent variable.
We considered the toolkit domains to be proxies for categories of care. Therefore, in subsequent inferential analyses, we identified 1 outcome variable per domain that was both clinically actionable and relevant and accompanied by at least a 25% rate of dissatisfaction. We used unadjusted logistic regression models to determine whether specific characteristics were independently associated with outcome variables. We chose these characteristics based on literature indicating that certain factors can result in increased suffering and risk of complicated grief (12,20-22) for the bereaved. We hypothesized that younger decedent age, being a spouse of the decedent, and death in the ICU would be associated with lower satisfaction. Additionally, we hypothesized that having the first and only encounter with MCR conclude in death might result in more dissatisfaction. Multivariable models were used when sample size allowed. All analyses were conducted using SAS (version 9.2; SAS Institute Inc).
Results
Patient Population
During the 1-year study period, 1,014 inpatient deaths occurred at MCR. Of those, 739 occurred within the sampling periods and 386 were study eligible. We enrolled 104 decedent-participant pairs (approximately 10% of inpatient deaths; Figure). Decedent demographic and clinical data are shown in Table 1. We did not identify significant differences between study decedents and eligible, nonparticipant decedents from the same time frame with regard to sex (36% vs 41% female, respectively; P =.28), mean age (67 years; P >.99), or race (96% white; P =.43).
Table 1. Decedent and Participant Characteristics (N=104).
| Characteristic | Value |
|---|---|
| Decedent Characteristics | |
| Age, y | |
| Mean | 67 |
| Median (range) | 70 (23-91) |
| Female sex, No. (%) | 37 (36) |
| Race/ethnicity, No. (%) | |
| White | 100 (96) |
| Asian | 2 (2) |
| Black | 1 (1) |
| Hispanic | 0 (0) |
| Other | 1 (1) |
| Highest level of education, No. (%) | |
| Less than high school | 11 (11) |
| High school | 44 (42) |
| Technical school or associate's degree | 14 (13) |
| Bachelor's degree or higher | 35 (34) |
| Religious affiliation, No. (%) (n=102) | |
| Christian | 93 (91) |
| Jewish | 0 (0) |
| None | 8 (8) |
| Other | 1 (1) |
| Marital status, No. (%) (n=103) | |
| Married | 76 (73) |
| Divorced | 11 (11) |
| Widowed | 10 (10) |
| Never married | 7 (7) |
| Clinical Features | |
| Cause of death, No. (%)a | |
| Malignant neoplasm | 37 (36) |
| Heart disease | 18 (17) |
| Infection | 15 (14) |
| Cerebrovascular disease | 10 (10) |
| Chronic lung disease | 5 (5) |
| Liver disease or cirrhosis | 4 (4) |
| Renal failure | 2 (2) |
| Peripheral vascular disease | 2 (2) |
| Progressive neurologic decline | 1 (1) |
| Otherb | 10 (10) |
| Overall condition during the last month of life, No. (%) (n=95)c | |
| Gradual decline | 41 (43) |
| Up and down decline | 8 (8) |
| Sudden decline | 46 (48) |
| Overall condition during the last 6 months of life, No. (%) (n=91)c | |
| Gradual decline | 56 (62) |
| Up and down decline | 22 (24) |
| Sudden decline | 13 (14) |
| Location of death, No. (%)a | |
| Intensive care unit | 58 (56) |
| General care unit | 46 (44) |
| Prior experience with medical center, No. (%)c | |
| All care | 34 (33) |
| Intermittent or specialty care | 40 (38) |
| First encounter | 30 (29) |
| Length of stay <7 days, No. (%)a | 54 (52) |
| Days in hospitala | |
| Mean | 13 |
| Median (range) | 8 (2-170) |
| Distance from medical centera | |
| Mean | 140 |
| Median (range) | 59 (1-1,716) |
| Participant Family Member Characteristics | |
| Female sex, No. (%) | 73 (70) |
| Age, y | |
| Mean | 62 |
| Median (range) | 70 (35-91) |
| Race/ethnicity, No. (%) (n=103) | |
| White | 101 (98) |
| Black | 2 (2) |
| Highest level of education, No. (%) (n=103) | |
| Less than high school | 3 (3) |
| High school | 42 (41) |
| Technical school or associate's degree | 19 (18) |
| Bachelor's degree or higher | 39 (38) |
| Religious affiliation (n=103) | |
| Christian | 93 (90) |
| None | 8 (8) |
| Other | 2 (2) |
| Relationship to decedent | |
| Life partner or spouse | 71 (68) |
| Child | 20 (19) |
| Biological parent | 5 (5) |
| Sibling | 3 (3) |
| Otherd | 5 (5) |
| Self-rated health now compared with 1 year ago | |
| Much better today | 6 (6) |
| Somewhat better | 10 (10) |
| About the same | 67 (66) |
| Somewhat worse | 16 (16) |
| Much worse | 3 (3) |
From chart review.
Diagnosis was not included in the list above or death resulted from multiple comorbid conditions.
From participant interview.
Includes in-laws, friends, and nieces or nephews.
Participant median age was 70 (range, 35-91 years). They were predominantly white (98%), female (70%), and Christian (90%). Fifty-three percent had a high school degree or less, and 68% were spouses of the decedent (Table 1).
Quality of Care in the Last Week of Life
Table 2 summarizes family perceptions of the quality of care provided. Most decedents were receiving pain medications, had difficulty breathing, and experienced feelings of anxiety and sadness, with 8% to 29% of participants reporting that symptoms were suboptimally managed. Participants reported that most decedents were treated with respect and kindness and that sufficient help was available to manage medications and dressing changes, but they also indicated that decedents' personal care needs were not always optimally addressed.
Table 2. Family Perceptions of the Quality of In-Hospital Care Provided in the Last Week of Life.
| Domain and Corresponding Survey Itemsa | No. (%)b |
|---|---|
| Physical Comfort and Emotional Support | |
| Painc | |
| Patient was receiving medication to treat pain | 63/86 (73) |
| Patient received too much medication for pain | 2/67 (3) |
| Patient received too little medication for pain | 8/67 (12) |
| Patient received right amount of medication for pain | 57/67 (85) |
| Difficulty breathingd | |
| Patient had trouble breathing | 63/86 (73) |
| Patients with difficulty breathing received insufficient help managing it | 5/64 (8) |
| Anxiety or sadness | |
| Patient experienced feelings of anxiety or sadness | 47/85 (55) |
| Patients with anxiety or sadness received inadequate help managing it | 11/38 (29) |
| Focus on the Individual | |
| Patient's personal care needs were not always taken care of as well as they should have been | 25/102 (25) |
| Patient was not always treated with respect by staff | 13/104 (13) |
| Patient was not always treated with kindness by staff | 14/104 (13) |
| There was not always enough help with medications and dressing changes | 3/104 (3) |
| Attend to Emotional and Spiritual Needs of the Family | |
| Family did not get enough support in dealing with feelings about patient's death | 8/103 (8) |
| Staff did not talk to loved ones about how they might feel after death when help was desired | 21/73 (29) |
| Staff did not suggest someone that the loved one could turn to if distressed | 54/94 (57) |
| Inform and Promote Shared Decision-Making | |
| Family sometimes had difficulty understanding what to expect from treatment | 11/97 (11) |
| Doctors sometimes provided either too much or too little information about the patient's medical condition | 17/98 (17) |
| Family desired but did not get sufficient information about the dying process | 18/102 (18) |
| Family desired but did not get sufficient information about what to do at the time of death | 18/98 (18) |
| Family desired but did not get sufficient information about medicines to manage pain or symptoms | 18/101 (18) |
| Family was not always kept informed about the patient's condition | 30/104 (29) |
| There were times that the staff did not know enough about the patient's medical history to provide the best possible care | 11/100 (11) |
| Provide Coordination of Care | |
| Doctors sometimes gave contradictory or confusing information about the patient's medical treatment | 32/98 (33) |
| There either was not always a doctor in charge of the patient's care or it was unclear which doctor was in charge of the patient's care | 20/99 (20) |
Items in boldface text were dependent variables in Table 3.
Some study participants did not answer every question, either because a prior question made that question irrelevant or because the participant declined to answer.
Some participants indicated that the decedent had not received pain medication but also answered questions about whether the amount of medication received was appropriate.
Some participants indicated that the decedent did not have breathing difficulty but also answered questions about whether the amount of breathing assistance received was appropriate.
Although participants believed that patients received sufficient help with emotional and spiritual needs, they perceived that their own emotional needs were insufficiently addressed: 57% reported that they were not directed to someone who could provide support when they were distressed and 29% reported that staff did not talk with family about how they might feel after the patient's death when they wanted the staff to do so. Twenty-nine percent reported that they were not always informed about the patient's condition. Thirty-three percent stated that doctors sometimes gave contradictory or confusing information, and 20% were unsure which doctor was directing the patient's care.
The 5 key outcome variables (1 per toolkit domain) included: 1) patient had feelings of anxiety or sadness and received inadequate help managing those feelings; 2) patient's personal care needs were not always taken care of as well as they should have been; 3) staff did not suggest someone that the family could turn to if distressed; 4) family was not always kept informed about the patient's condition; and 5) doctors gave contradictory or confusing information about the patient's medical treatment at least some of the time.
Table 3 shows the unadjusted logistic regression models testing whether specific demographic and clinical variables were independently associated with dichotomized versions of the 5 outcome variables. Family members of patients who received only subspecialty or intermittent care at the institution were significantly more likely to report feeling under-informed about the decedent's condition than families whose decedents were at the institution for the first time (odds ratio [OR], 3.3 [95% CI, 1.1-9.7]; P=.03). Families of older decedents were less likely to report receiving contradictory or confusing information than families of younger patients (OR, 0.4 [95% CI, 0.2-0.9]; P =.02), and spouses were marginally more likely to report contradictory or confusing information than other participants (adjusted model only; OR, 1.5 [95% CI, 0.5-4.8]; P =.046). When significant associations were identified, multivariable models were used; these showed similar results.
Table 3. Associations Between Decedent or Participant Characteristics and Perceptions of Inadequate Quality of Care During the Last Week of Life a.
| Characteristic of Decedent or Participant | Decedent Anxiety or Sadness (Less Help Than Needed) | Personal Needs (Decedent Needs Not Always Met) | Times of Distress (No Help or Suggestions for Family) | Regarding Decedent's Condition (Family Not Always Informed) | Regarding Medical Treatment (Received Confusing or Contradictory Information) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||||
| No. (%) | OR (95% CI) | No. (%) | OR (95% CI) | No. (%) | OR (95% CI) | No. (%) | OR (95% CI) | No. (%) | OR (95% CI) | |
| Age of decedent, y | ||||||||||
| <60 | 7/16 (43.8) | 1.0 | 9/39 (23.1) | 1.0 | 22/39 (56.4) | 1.0 | 13/40 (32.5) | 1.0 | 18/39 (46.2) | 1.0 |
| ≥60 | 4/21 (19.0) | 0.3 (0.1-1.3) | 16/63 (25.4) | 1.1 (0.4-2.9) | 32/55 (58.2) | 1.1 (0.5-2.5) | 17/64 (26.6) | 0.8 (0.3-1.8) | 14/59 (23.7) | 0.4 (0.2-0.9)b |
| Relationship to decedent | ||||||||||
| Child | 3/8 (37.5) | 1.0 | 6/19 (31.6) | 1.0 | 9/19 (47.4) | 1.0 | 7/19 (36.8) | 1.0 | 5/19 (26.3) | 1.0 |
| Spouse | 7/23 (30.4) | 0.7 (0.07-3.9) | 15/70 (21.4) | 0.6 (0.2-1.8) | 38/63 (60.3) | 1.7 (0.6-4.7) | 20/71 (28.2) | 0.7 (0.2-2.0) | 23/65 (35.4) | 1.5 (0.5-4.8)c |
| Other | 1/6 (16.7) | 0.3 (0.03-4.4) | 4/13 (30.8) | 1.0 (0.2-4.4) | 7/12 (58.3) | 1.6 (0.4-6.7) | 3/14 (21.4) | 0.5 (0.1-2.3) | 4/14 (28.6) | 1.1 (0.2-5.3) |
| Experience with Mayo Clinic | ||||||||||
| First time | 4/9 (44.4) | 1.0 | 5/29 (17.2) | 1.0 | 13/27 (48.1) | 1.0 | 6/30 (20.0) | 1.0 | 8/29 (27.6) | 1.0 |
| Specialty or intermittent | 3/15 (20.0) | 0.3 (0.1-1.9) | 13/39 (33.3) | 2.4 (0.7-7.7) | 23/36 (63.9) | 1.9 (0.7-5.3) | 18/40 (45.0) | 3.3 (1.1-9.7)d | 14/38 (36.8) | 1.5 (0.5-4.4) |
| Primary | 4/13 (30.8) | 0.6 (0.1-3.2) | 7/34 (20.6) | 1.2 (0.3-4.4) | 18/31 (58.1) | 1.5 (0.5-4.2) | 6/34 (17.6) | 0.9 (0.2-3.0) | 10/31 (32.3) | 1.3 (0.4-3.8) |
| Location of death | ||||||||||
| General care unit | 5/17 (29.4) | 1.0 | 13/45 (28.9) | 1.0 | 23/43 (53.5) | 1.0 | 14/46 (30.4) | 1.0 | 15/44 (34.1) | 1.0 |
| Intensive care unit | 6/20 (30.0) | 1.0 (0.3-4.2) | 12/57 (21.1) | 0.7 (0.3-1.6) | 31/51 (60.8) | 1.3 (0.6-3.1) | 16/58 (27.6) | 0.9 (0.4-2.0) | 17/54 (31.5) | 0.9 (0.4-2.1) |
Abbreviation: OR, odds ratio.
Associations were tested with logistic regression models.
P=.02 (unadjusted) and P=.004 (adjusted).
P=.046 in adjusted model (not significant unadjusted).
P=.03 (unadjusted) and P=.047 (adjusted).
Discussion
We sought to describe the quality of care experienced in the last week of life by patients who died in-hospital at a large tertiary medical center and to identify actionable gaps in the quality of that experience. We further wished to identify any patient or family characteristics that were associated with lower satisfaction with care. Participants were highly satisfied with the overall quality of care decedents received; they reported that symptoms were well managed overall and that their loved ones were treated with kindness, dignity, and respect. Nonetheless, an appreciable minority of participants reported unmet needs in key domains of clinical care, including symptom management, attention to personal care, communication, and coordination of care.
When we attempted to determine whether specific clinical or demographic characteristics influenced families' perception of care in 5 areas, we identified 3 significant associations, all pertaining to communication between the family and medical team. Surprisingly, families of patients who received only subspecialty or intermittent care were more likely to report being under-informed about the patient's condition. This may reflect the hazards in transitions of care as patients navigate among different providers and care systems (23). Such challenges may be heightened when patients, in distress and seeking a “miracle” (24), come to a tertiary care center with multiple subspecialty teams providing complex care. Consistent with other work, families perceived decedents to receive equally good care whether patients died in the ICU or on the general care unit (25).
Families of younger patients were more likely to report receiving confusing or contradictory information; spouses likewise had similar perceptions. These findings suggest that a loved one's death is even more stressful when decedents are younger (20) or when the bereaved is particularly close to the decedent (21,22). Certainly, difficult information is even more challenging to receive in the setting of intense emotions and anticipatory grief (26-28).
To isolate opportunities for improvement, we applied a rigorous standard to identify perceived gaps in care. First, a significant percentage of participants reported that decedents' personal care needs were not always optimally addressed. Personal care needs include self-care activities that may require assistance in the setting of illness, including toileting, oral care, bathing, and dressing—actions that healthy people complete largely by rote. Optimal maintenance of personal care is an important part of preserving dignity (29,30), deserves meticulous attention, and denotes a clear opportunity for improvement.
Second, participants noted challenges in care coordination, including communication missteps. Many reported being under informed about the patient's condition, receiving contradictory or confusing information, and not understanding which physician was directing care. In large academic medical centers, multiple physician teams often are involved in the care of each patient, which can result in communication gaps and misunderstandings (31,32).
Finally, participants did not always believe that their own distress as a family member was sufficiently addressed. They wanted more information about the dying process and tasks at the time of death than they received. For patients dying in the hospital and especially the ICU, the shift from aggressive, life-prolonging care to comfort-focused care of the dying can feel abrupt and surprising (33,34). However, after patients, families, and clinicians have accepted that death is unavoidable, families want anticipatory guidance when navigating the dying experience (33).
We identified deficits in basic services at an otherwise high-performing institution (1), consistent with other studies reporting suboptimal symptom management and lower satisfaction with patient-provider communication and coordination of care for patients who die in the hospital vs in hospice care (6,11). Such findings have changed little in the past decade or longer, despite increased availability of palliative care services (6). Similar to another recent study (35), we found that providers not only need to relieve symptoms, they also must be attuned to worsening clinical status, individual patient and family needs, and patient and family preferences regarding communication and medical decision-making.
Nearly 2 decades of work have gone into defining quality end-of-life care as care that ensures physical comfort and emotional support, promotes shared decision making, treats dying patients with respect, provides information and emotional support to families, and coordinates care across settings (5,11,36,37). Still, even in a top-ranked tertiary care center known for high-quality, cost-effective care (1,4), we face challenges and demonstrate deficits in care similar to those identified across the country. Thus, providing quality end-of-life care is not only a problem within individual hospitals, it is a complex problem within the US health care system.
Strengths of our study include its representative sample (10%) of hospital deaths occurring in 1 year at a large academic medical center, with a mix of patients and illness severity on par with other US academic medical centers (1) and a mix of local and referral patients. Survey completion rate was high. Most survey participants resided within 140 miles of the medical center, thereby appropriately reflecting the sociocultural makeup of our region. Nonetheless, the homogeneity of local residents may limit generalizability of our findings when considering more ethnically and culturally diverse populations, such as that which might be found at a large urban center. One could argue, however, that the challenges of meeting the needs of dying patients and their families may be even greater in a more heterogenous population. We did not evaluate the influence of palliative care consultations because palliative care services were limited when these data were collected; other studies have demonstrated that increased palliative care involvement improves satisfaction with care (5,38-40). Interviewing participants retrospectively could be viewed as another limitation. Although the patient's perspective is preferred, we can learn much from family members as proxies, and most research evaluating care of dying patients has been conducted through after-death surveys of family (18,19). The 3- to 7-month pause between the patient's death and the interview may not reflect the just-in-time views of participants but honors their need to grieve acutely. This pause is a commonly accepted practice in studies of the dying experience (18,19), and our participants remembered the relevant events clearly and in detail (33). Finally, participants' perception of care may have been influenced by grief (27), but emotions and grief are inextricable from the dying process, one's perception of events, and one's ability to understand and interpret medical data. Our intent is to improve patients' and families' experience of care, which is linked to their feelings and perceptions.
Future research should address systems changes to improve the care of the dying in all settings, especially in hospitals, when transition to home is not possible. Our results highlight several opportunities for future interdisciplinary research, particularly in improving patient and family communication with providers, giving better attention to personal care needs, and providing emotional and spiritual support to family members and to patients. Our data identify a starting point for improvement efforts at our institution. Studies are currently underway to evaluate the impact of more robust, interdisciplinary interventions in palliative care and decedent affairs on the patient and family experience.
Conclusion
Despite high satisfaction with care overall, decedents' family members in a large tertiary referral hospital reported significant unmet needs and highlighted opportunities to improve the care of dying patients. Most of the deficits described are actionable and some straightforward solutions appear evident, including improving communication about patients' illness, prognoses, and treatment plans and providing families with increasing support as the illness course changes and it becomes clear that death is unavoidable. After it becomes apparent that the patient will die in the hospital, patients and families want help navigating the dying process, especially to know what to expect and what the ongoing care will entail. Although such solutions may appear self-evident and readily accessible, the deficits identified at our institution are pervasive within the health care system as a whole and may indicate the need for a multifaceted, systems-based solution.
Acknowledgments
We thank Dr Shiao Yen Khoo for her assistance with clarifying clinical data and Marguerite Robinson for her assistance with human subject issues, project organization, and grant management.
Funding: Research reported in this publication was supported by grants from the Mayo Clinic Program in Professionalism and Ethics, Saint Marys Hospital Sponsorship Research Committee, and Division of General Internal Medicine and was supported by CTSA Grant Number UL1 TR000135 from the National Center for Advancing Translational Science (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Abbreviations
- ICU
intensive care unit
- MCR
Mayo Clinic (Rochester, Minnesota)
- OR
odds ratio
- SRC
Mayo Clinic Survey Research Center
- US
United States
Footnotes
Conflict of interest: None.
References
- 1.Wennberg JE, Fisher ES, Goodman DC, Skinner JS. In: Tracking the care of patients with severe chronic illness: the Dartmouth Atlas of Health Care 2008. Bronner KK, editor. Lebanon (NH): Dartmouth Medical School; 2008. [PubMed] [Google Scholar]
- 2.Hall MJ, Levant S, DeFrances CJ. NCHS Data Brief. 118. 2013. Mar, Trends in inpatient hospital deaths: National Hospital Discharge Survey, 2000-2010; pp. 1–8. [PubMed] [Google Scholar]
- 3.Goodman DC, Fisher ES, Wennberg JE, Skinner JS, Chasan-Taber S, Bronner KK. Tracking improvement in the care of chronically ill patients: a Dartmouth Atlas brief on medicare beneficiaries near the end of life. Lebanon (NH): Dartmouth Institute for Health Policy and Clinical Practice: a report of the Dartmouth Atlas Project; 2013. [PubMed] [Google Scholar]
- 4.Goodman DC, Esty AR, Fisher ES, Chang CH. In: Trends and variation in end-of-life care for Medicare beneficiaries with severe chronic illness. Bronner KK, editor. Lebanon (NH): Dartmouth Institute for Health Policy and Clinical Practice: a report of the Dartmouth Atlas Project; 2011. [PubMed] [Google Scholar]
- 5.Institute of Medicine: of the National Academies. Dying in America: improving quality and honoring individual preferences near the end of life. Washington (DC); The National Academies Press; 2015. [PubMed] [Google Scholar]
- 6.Teno JM, Freedman VA, Kasper JD, Gozalo P, Mor V. Is care for the dying improving in the United States? J Palliat Med. 2015 Aug;18(8):662–6. doi: 10.1089/jpm.2015.0039. Epub 2015 Apr 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Teno JM, Gozalo PL, Bynum JP, Leland NE, Miller SC, Morden NE, et al. Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013 Feb 6;309(5):470–7. doi: 10.1001/jama.2012.207624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Broad JB, Gott M, Kim H, Boyd M, Chen H, Connolly MJ. Where do people die? An international comparison of the percentage of deaths occurring in hospital and residential aged care settings in 45 populations, using published and available statistics. Int J Public Health. 2013 Apr;58(2):257–67. doi: 10.1007/s00038-012-0394-5. Erratum in: Int J Public Health. 2013 Apr;58(2):327. [DOI] [PubMed] [Google Scholar]
- 9.Addington-Hall JM, O'Callaghan AC. A comparison of the quality of care provided to cancer patients in the UK in the last three months of life in in-patient hospices compared with hospitals, from the perspective of bereaved relatives: results from a survey using the VOICES questionnaire. Palliat Med. 2009 Apr;23(3):190–7. doi: 10.1177/0269216309102525. Epub 2009 Feb 27. [DOI] [PubMed] [Google Scholar]
- 10.Mayland CR, Williams EM, Addington-Hall J, Cox TF, Ellershaw JE. Assessing the quality of care for dying patients from the bereaved relatives' perspective: further validation of “evaluating care and health outcomes: for the dying. J Pain Symptom Manage. 2014 Apr;47(4):687–96. doi: 10.1016/j.jpainsymman.2013.05.013. Epub 2013 Nov 5. [DOI] [PubMed] [Google Scholar]
- 11.Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004 Jan 7;291(1):88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 12.Wright AA, Keating NL, Balboni TA, Matulonis UA, Block SD, Prigerson HG. Place of death: correlations with quality of life of patients with cancer and predictors of bereaved caregivers' mental health. J Clin Oncol. 2010 Oct 10;28(29):4457–64. doi: 10.1200/JCO.2009.26.3863. Epub 2010 Sep 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dartmouth Institute for Health Policy and Clinical Practice. End of life care: inpatient days per decedent during the last six months of life, by gender and level of care intensity. Lebanon (NH): Dartmouth Institute for Health Policy and Clinical Practice: a report of the Dartmouth Atlas Project; 2012. [Google Scholar]
- 14.Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000 Nov 15;284(19):2476–82. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- 15.Fischer S, Min SJ, Cervantes L, Kutner J. Where do you want to spend your last days of life? Low concordance between preferred and actual site of death among hospitalized adults. J Hosp Med. 2013 Apr;8(4):178–83. doi: 10.1002/jhm.2018. Epub 2013 Feb 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Janssen DJ, Spruit MA, Schols JM, Wouters EF. Dynamic preferences for site of death among patients with advanced chronic obstructive pulmonary disease, chronic heart failure, or chronic renal failure. J Pain Symptom Manage. 2013 Dec;46(6):826–36. doi: 10.1016/j.jpainsymman.2013.01.007. Epub 2013 Apr 6. [DOI] [PubMed] [Google Scholar]
- 17.Kinoshita H, Maeda I, Morita T, Miyashita M, Yamagishi A, Shirahige Y, et al. Place of death and the differences in patient quality of death and dying and caregiver burden. J Clin Oncol. 2015 Feb 1;33(4):357–63. doi: 10.1200/JCO.2014.55.7355. Epub 2014 Dec 22. [DOI] [PubMed] [Google Scholar]
- 18.DiBiasio EL, Clark MA, Gozalo PL, Spence C, Casarett DJ, Teno JM. Timing of survey administration after hospice patient death: stability of bereaved respondents. J Pain Symptom Manage. 2015 Jul;50(1):17–27. doi: 10.1016/j.jpainsymman.2015.01.006. Epub 2015 Jan 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Teno JM, Clarridge B, Casey V, Edgman-Levitan S, Fowler J. Validation of toolkit after-death bereaved family member interview. J Pain Symptom Manage. 2001 Sep;22(3):752–8. doi: 10.1016/s0885-3924(01)00331-1. [DOI] [PubMed] [Google Scholar]
- 20.Gamino LA, Sewell KW, Easterling LW. Scott and White Grief Study: phase 2: toward an adaptive model of grief. Death Stud. 2000 Oct-Nov;24(7):633–60. doi: 10.1080/07481180050132820. [DOI] [PubMed] [Google Scholar]
- 21.Bruinsma SM, Tiemeier HW, Verkroost-van Heemst J, van der Heide A, Rietjens JA. Risk factors for complicated grief in older adults. J Palliat Med. 2015 May;18(5):438–46. doi: 10.1089/jpm.2014.0366. Epub 2015 Feb 11. [DOI] [PubMed] [Google Scholar]
- 22.Newson RS, Boelen PA, Hek K, Hofman A, Tiemeier H. The prevalence and characteristics of complicated grief in older adults. J Affect Disord. 2011 Jul;132(1-2):231–8. doi: 10.1016/j.jad.2011.02.021. Epub 2011 Mar 12. [DOI] [PubMed] [Google Scholar]
- 23.Coleman EA, Roman SP. Family caregivers' experiences during transitions out of hospital. J Healthc Qual. 2015 Jan-Feb;37(1):12–21. doi: 10.1097/01.JHQ.0000460117.83437.b3. [DOI] [PubMed] [Google Scholar]
- 24.Chapple HS. No place for dying: hospitals and the ideology of rescue. Walnut Creek (CA): Left Coast Press; 2010. [Google Scholar]
- 25.Probst DR, Gustin JL, Goodman LF, Lorenz A, Wells-Di Gregorio SM. ICU versus non-ICU hospital death: family member complicated grief, posttraumatic stress, and depressive symptoms. J Palliat Med. 2016 Apr;19(4):387–93. doi: 10.1089/jpm.2015.0120. Epub 2016 Feb 1. [DOI] [PubMed] [Google Scholar]
- 26.Grassi L. Bereavement in families with relatives dying of cancer. Curr Opin Support Palliat Care. 2007 Apr;1(1):43–9. doi: 10.1097/SPC.0b013e32813a3276. [DOI] [PubMed] [Google Scholar]
- 27.Hudson PL, Thomas K, Trauer T, Remedios C, Clarke D. Psychological and social profile of family caregivers on commencement of palliative care. J Pain Symptom Manage. 2011 Mar;41(3):522–34. doi: 10.1016/j.jpainsymman.2010.05.006. Epub 2010 Dec 3. [DOI] [PubMed] [Google Scholar]
- 28.Back A, Arnold R, Tulsky J. Mastering communication with seriously ill patients: balancing honesty with empathy and hope. Cambridge (United Kingdom): Cambridge University Press; 2009. [Google Scholar]
- 29.Chochinov HM. Dignity-conserving care: a new model for palliative care: helping the patient feel valued. JAMA. 2002 May 1;287(17):2253–60. doi: 10.1001/jama.287.17.2253. [DOI] [PubMed] [Google Scholar]
- 30.Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Dignity in the terminally ill: a cross-sectional, cohort study. Lancet. 2002 Dec 21-28;360(9350):2026–30. doi: 10.1016/S0140-6736(02)12022-8. [DOI] [PubMed] [Google Scholar]
- 31.Hewett DG, Watson BM, Gallois C, Ward M, Leggett BA. Intergroup communication between hospital doctors: implications for quality of patient care. Soc Sci Med. 2009 Dec;69(12):1732–40. doi: 10.1016/j.socscimed.2009.09.048. Epub 2009 Oct 21. [DOI] [PubMed] [Google Scholar]
- 32.Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care. 2004 Oct;13(Suppl 1):i85–90. doi: 10.1136/qshc.2004.010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dose AM, Carey EC, Rhudy LM, Chiu Y, Frimannsdottir K, Ottenberg AL, et al. Dying in the hospital: perspectives of family members. J Palliat Care. 2015;31(1):13–20. doi: 10.1177/082585971503100103. [DOI] [PubMed] [Google Scholar]
- 34.Russ AJ, Kaufman SR. Family perceptions of prognosis, silence, and the “suddenness” of death. Cult Med Psychiatry. 2005 Mar;29(1):103–23. doi: 10.1007/s11013-005-4625-6. [DOI] [PubMed] [Google Scholar]
- 35.Witkamp FE, van Zuylen L, Borsboom G, van der Rijt CC, van der Heide A. Dying in the hospital: what happens and what matters, according to bereaved relatives. J Pain Symptom Manage. 2015 Feb;49(2):203–13. doi: 10.1016/j.jpainsymman.2014.06.013. Epub 2014 Aug 15. [DOI] [PubMed] [Google Scholar]
- 36.Singer PA, Martin DK, Kelner M. Quality end-of-life care: patients' perspectives. JAMA. 1999 Jan 13;281(2):163–8. doi: 10.1001/jama.281.2.163. [DOI] [PubMed] [Google Scholar]
- 37.Steinhauser KE, Clipp EC, McNeilly M, Christakis NA, McIntyre LM, Tulsky JA. In search of a good death: observations of patients, families, and providers. Ann Intern Med. 2000 May 16;132(10):825–32. doi: 10.7326/0003-4819-132-10-200005160-00011. [DOI] [PubMed] [Google Scholar]
- 38.Casarett D, Pickard A, Bailey FA, Ritchie C, Furman C, Rosenfeld K, et al. Do palliative consultations improve patient outcomes? J Am Geriatr Soc. 2008 Apr;56(4):593–9. doi: 10.1111/j.1532-5415.2007.01610.x. Epub 2008 Jan 16. [DOI] [PubMed] [Google Scholar]
- 39.Gade G, Venohr I, Conner D, McGrady K, Beane J, Richardson RH, et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008 Mar;11(2):180–90. doi: 10.1089/jpm.2007.0055. [DOI] [PubMed] [Google Scholar]
- 40.Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010 Aug 19;363(8):733–42. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]