Abstract
Background
The Asthma Impact on Quality of Life Scale (A-IQOLS) assesses the negative effect of asthma on quality of life (QoL) from the patient’s perspective, using dimensions of Flanagan’s Quality of Life Scale (QOLS), a measure of current QoL.
Objectives
To determine and compare the psychometric properties of the A-IQOLS and QOLS, including their sensitivities to differences and changes in asthma status.
Methods
In a test-retest design (3–5 week interval), adults with persistent asthma underwent spirometry and were administered the A-IQOLS, other asthma outcome measures (ACT, ASUI, Marks and Juniper AQLQs), and QOLS.
Results
Participants’ (n = 147) mean age was 49 yrs.; 76% were White; 12% Hispanic; 65% female. A-IQOLS and QOLS scores were significantly correlated with other asthma outcomes scores except FEV1, but shared relatively low common variance with these measures. A-IQOLS, but not QOLS, score changes were significantly correlated with changes in asthma outcomes. The A-IQOLS SEM = 0.27 implies that a within-person score change of ≥ ±0.73 constitutes a true change. The QOLS SEM = 0.43.
Conclusions
A-IQOLS provides a reliable, valid, and unique assessment of the patient-perceived negative effect of asthma on their QoL, suitable for use in asthma clinical research and potentially in clinical care. Further studies are needed in diverse patient populations. QOLS, a measure of current QoL, is less sensitive to disease status changes but may be useful in characterizing study populations, in treatment adherence research, and as a clinical and research tool in patients with multiple, severe, and/or life-limiting chronic conditions.
Keywords: Asthma, Quality of life, Measurement/Standardized measures, Clinical outcomes, Patient-centered outcomes
INTRODUCTION
The 2010 NIH Asthma Outcomes Workshop (AOW) reviewed existing instruments and procedures for measurement of all types of asthma outcomes measures. With respect to asthma-related quality of life (QoL),1 the AOW concluded that assessing disease impact on patients’ QoL remains an essential component of the asthma outcome measurement toolbox.2 However, it also concluded that no available “asthma-specific QoL” measures, even those in widespread use, actually assess the patient’s perception of the effect of asthma on their QoL.2 Instead, existing instruments measure the patient’s status in physical, mental, and social health domains as these relate to asthma. The conceptual frameworks of such measures consist of health domains -- symptom frequency and severity, how much asthma limits the individual’s activities (i.e., their functional status), and in some cases, negative emotions related to asthma such as concerns, fears, or embarrassment.
The AOW recognized that the content validity of a measure is fundamental, which means that, except in rare instances, the content of a measure should have a very direct, obvious relationship to its intended purpose and the construct it purports to measure.3 The fact that a health status measure is reliable, is logically correlated with other measures of asthma status, and contains items about the frequency and intensity of functional limitations, does not mean it is a valid measures of the patient’s perception of how or how much asthma affects their QoL -- a judgment that can only be made by the patient. The effects of asthma on QoL are very likely to be determined by factors in addition to symptoms and functional limitations, such as how important it is to the patient to engage in particular activities, how difficult for them to avoid things that trigger their asthma without having to forego valued activities, etc. Existing instruments may provide an assessment of an individual’s asthma and functional status. However, the fact that they do not assess the patient’s perception of how the disease affects their QoL is what led the AOW not to recommend any existing instrument as a core QoL measure for use in asthma clinical research.
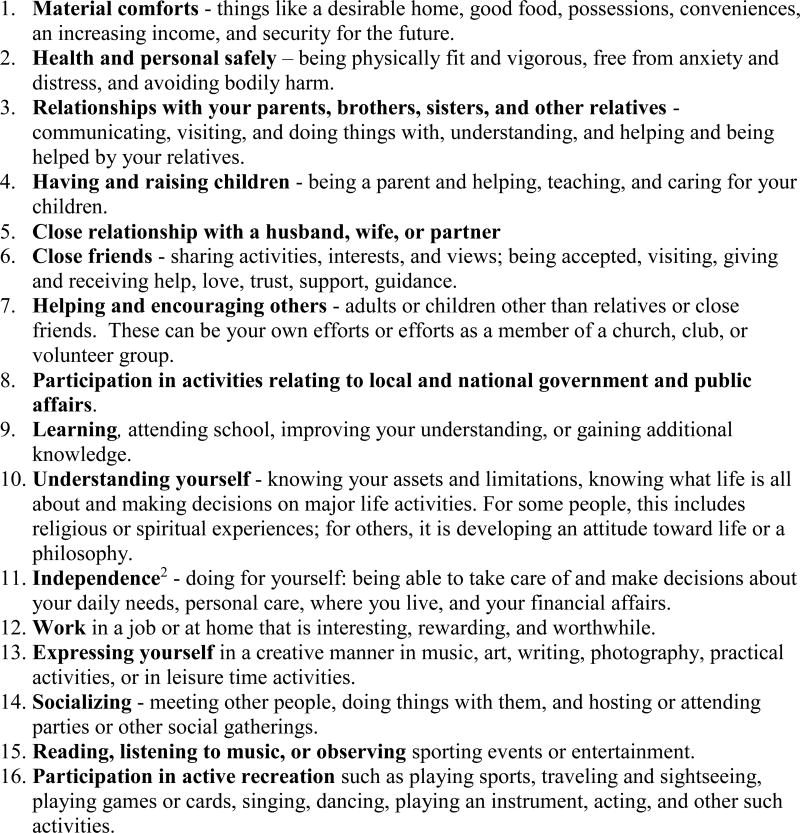
In the 1970s, by gathering and analyzing narrative reports from a large, diverse sample of individuals across the U.S. regarding events/experiences that significantly affected their quality of life (positively or negatively), eminent psychologist John C. Flanagan identified 15 dimensions that affect individuals’ quality of life (Figure 1).4 He developed a Quality of Life Scale (QOLS) on which individuals can rate the extent to which their needs and wants are being met on each dimension.5 In essence, he considered the quality of life of an individual as defined by how well that person felt that their needs and wants were being satisfied across all the dimensions of life. The QOLS, a generic measure that can be used with any individual, regardless of health status, does not ask the respondent to assess the contribution of any particular factor to their QoL.
Figure 1.
Flanagan’s Dimensions of Quality of Life.1
1Flanagan JC. A research approach to improving our quality of life. Am Psychol 1978;33:138.
2Added to the original Flanagan dimensions by Burckhardt CS, et al. Res Nurs Health. 1989;21:347–354.
We propose an approach to measuring an individual’s perception of the impact of a disease on their QoL that uses Flanagan’s quality of life dimensions. As an initial example of this approach, we created the Asthma Impact on Quality of Life Scale (A-IQOLS). Rather than asking how well the individual’s needs and wants are being satisfied, the A-IQOLS asks the individual to rate the negative effect of a disease and its treatment on each QoL dimension. Here we report the A-IQOLS’ development process and the methods and results of a test-retest study to determine its psychometric properties in patients with persistent asthma.
An alternative to the IQOLS approach would be to simply measure patients’ perception of their quality of life (e.g., using the QOLS), and then infer the impact of their disease based on temporal changes or between-group differences in QOLS scores. To compare these alternatives in asthma patients, and because both types of instruments could have potential uses in research and clinical practice, both were administered in this study. To assess the current relevance of the quality of life dimensions, we also obtained individuals’ ratings of the personal importance of each dimension.
METHODS
The research reported here was supported by Grant No. HL119845 (PI: Wilson) from the National Heart, Lung, and Blood Institute/NIH. The study is approved by the Sutter Health IRB (SHIRB No. 14-06-327).
Instrument Development and Pilot Testing
The development of the A-QOLS and the pilot testing of the A-QOLS, Flanagan’s Importance questionnaire, and his QOLS in asthma patients, are described in the Supplement. These measurement instruments, as used in the present study, are presented in Figure S1, followed by their Administration Instructions. The history of the development and use of the QOLS by Flanagan also is described in the Supplement, as are subsequent modifications made by other investigators. Key distinctions between these versions are described in order to clarify the rationale for using Flanagan’s own QOLS’s stem question and rating scale in the present study.
Test-Retest Study Sample
Eligibility
Inclusion criteria
Physician diagnosis of asthma
Ages 18–70 years (the upper limit was to reduce the likelihood that significant fixed airway obstruction would be observed upon assessment of patients’ lung function)
Current prescription for an asthma controller medication
Care received from a primary care provider in the large multi-specialty health care system within the preceding 24 mo.
Exclusion criteria
Intermittent asthma (i.e., no routine use of asthma controller medications; seasonal asthma or daytime symptoms < 2times/week and nocturnal symptoms < 2 times/mo.)
Significant medical co-morbidities that could affect interpretation of the results, (e.g., COPD or another lung disease other than asthma)
Significant healthcare event such as chest or abdominal surgery in past 3 months, cataract or other major surgery in preceding month, or scheduled procedure prior to study follow-up.
Inability to complete basic requirements of the study protocol, including spirometry testing and questionnaires
Any circumstance preventing the patient from attending two clinic visits, one month apart.
Primary care physician’s determination that including the patient was inappropriate for any of the above reasons.
Recruitment
Patients potentially meeting the inclusion criteria were identified by querying electronic clinical and administrative records and randomly selected for recruitment using a disproportionate stratified sampling (SDS) methodology with stratification by race, ethnicity, sex, and treatment step of the patient’s current asthma controller regimen.12 Sampling probabilities were designed to achieve a distribution that: 1) corresponded to the sex and race distribution in the U.S. asthma population, and 2) ensured a more uniform distribution across asthma treatment steps (and, by inference, levels of asthma severity) than would have resulted from randomly sampling patients with persistent asthma, most of whom would have had mild or moderate disease. Potential participants were contacted by phone, screened, and (if eligible and interested) scheduled for an initial clinic visit.
Patient Assessment
At baseline, Informed consent and anthropometric measurements were obtained, pre-and post-bronchodilator spirometry performed and a questionnaire self-administered. Prebronchodilator spirometry and the questionnaire were repeated four weeks later (3–5 weeks depending on patients’ availability).
Importance of QoL dimensions
This measure asks respondents to rate how important each of the dimensions is to them on a scale from 1 = Not at all important to 5 = Very important.
Flanagan QOLS
The QOLS scale (Fig. S2) asks patients to rate how well their needs and wants are being satisfied on each quality of life dimension using a bidirectional scale from 1 = Not at all well satisfied to 5 = Very well satisfied.5
A-IQOLS
The A-IQOLS (Fig. S1) asks respondents to rate the negative effect of their asthma and its treatment, over the preceding 4 weeks, on each of 16 quality of life dimensions using a standard unidirectional scale ranging from 1 = No negative effect at all to 5 = Extremely negative effect.
Other standardized asthma outcome measures
Asthma control, symptoms and functional impairment were assessed using the Asthma Control Test (ACT),13 Asthma Symptom Utility index (ASUI),14 Marks Asthma Quality of Life Questionnaire (Marks AQLQ),15 and Juniper Mini Asthma Quality of Life Questionnaire (Mini-AQLQ)16 -- all widely used in asthma research. The Patient Health Questionnaire (PHQ-9)17 was used to assess depression.
Spirometry
Research coordinators, certified for occupational spirometry by NIOSH, used standardized research methods and equipment that met or exceeded American Thoracic Society standards.18 The percent predicted pre-bronchodilator FEV1 based on age-, sex- and race-specific norms,19 is considered a core physiological measure in asthma research.20
Statistical Analysis
Descriptive statistics were computed for patient demographic and clinical characteristics. The A-IQOLS and QOLS summary scores were the averages of their respective dimension ratings. Other standardized asthma outcome measures were scored and scaled using their published algorithms.13, 16, 21–25 Differences between the test and retest administrations on all measures were evaluated using t-tests (continuous variables) and chi-square tests (categorical variables). Associations between pairs of measures were assessed using Spearman or Pearson Rank-Order correlation coefficients, as appropriate to their distributional properties. The Importance questionnaire has no summary score; dimension importance ratings are considered individually.
Measurement reliability
Asthma being an inherently variable disease, it is not reasonable to assume that all changes that might be observed over a 3–5 weeks period are entirely due to errors of measurement and not to real changes in the underlying construct a given measure is designed to assess. However, the baseline and associated follow-up assessments were fairly uniformly distributed over all seasons of the year, and the 3–5 week test-retest interval, while arguably long enough to reduce recall influences, was short enough to minimize systematic seasonal changes in asthma status. It is expected that the observed variability in disease status would be typical of the variability that would occur in a clinical trial at a similar interval in the absence of any specific intervention.
Using the repeated assessments of each patient, a two-way, repeated-measures analysis of variance was used to calculate 1) the intraclass correlation coefficient (ICC), a relative reliability index, and 2) the within subject variance, whose square root is the estimated standard error of measurement (SEM), a less population-dependent reliability index that, unlike the ICC, can be interpreted on the original response scale. The repeatability coefficient is based on the SEM (CR = 2.77×SEM)26, and is the smallest within-person change that can be considered, with 95% confidence, to be a real change. The upper and lower bounds of the 95% limit of agreement (LOA) around the CR value, and their confidence intervals (CI), were also calculated.26, 27
Internal consistency reliability
Standardized coefficient alpha was used to estimate the internal consistency of the items of the A-IQOLS, QOLS, and other outcome measures.
Construct validity
The content validities of the QOLS and A-IQOLS were established by 1) the direct relevance of their root questions to the construct each is intended to measure, and 2) the original research that defined the quality of life dimensions to which the ratings are applied. The continued relevance of the dimension was evaluated by considering the present Importance ratings. Convergent validity was evaluated by examining the patterns and significance of the associations between the A-IQOLS and QOLS and other concurrently administered asthma outcome measures and their associations with each other. The squared correlations (R2) estimate the proportion of common variance between any two measures. Divergent validity, the amount of unique information provided by a measure, is estimated by 1-R2, the amount of independent variance between a pair of measures as well as variance due to measurement error.
A significance level of 0.05 was used throughout. To interpret the strength of correlation coefficients, we followed Evans (1996)28: 0.00–0.19 = very weak, 0.20–0.39 = weak, 0.40–0.59 = moderate, 0.60–0.79 = strong, 0.80–1.0 = very strong correlation. All statistical analyses were performed using SAS v 9.2 (SAS Institute, Inc., Cary, NC).
RESULTS
Study Population
Recruitment and Enrollment
Contact was attempted with 950 of the identified, potentially eligible patients, 153 of whom were screened, confirmed eligible, agreed to participate, and completed in-person consent and baseline assessment. Of these, 148 (97%) completed both the baseline (test) and follow-up (retest) assessments (STROBE diagram, Fig. S3). One was subsequently determined to have COPD, and hence was ineligible, resulting in an analysis sample with n = 147 patients.
Baseline characteristics
Participants’ mean (± SD) age was 49.1 (± 12.3) years; 64.6% were female, 75.5% White, 15.0% Black, and the remainder Asian or another race; 11.6% were Hispanic (Table 1). The sample was largely well educated and employed/retired, with moderate to high income. Just over half reported adult onset asthma, and 95.2% reported aeroallergens among their asthma triggers. Approximately three-fourths (76.2%) were never smokers and only 3.4% current smokers. In the year pre-enrollment, they averaged 0.4 (±0.8) exacerbations requiring an oral corticosteroid (OCS) and 1.58 (±1.95) asthma medical visits. A high proportion (82.3%) were either overweight (35.4%) or obese (46.9%), and nearly half (49.7% were at high risk for sleep apnea based on their Berlin scores. In 2010 the obesity rate was 38.8% in individuals with current asthma compared with 26.8% in those without.29 Obesity has been associated with adult asthma onset30 and obstructive sleep apnea.31 Since this sample has persistent, not just current, asthma, and obesity rates have continued to increase since 2010, the obesity and sleep apnea risk rates in this sample are not unreasonable.
Table 1.
Baseline characteristics of test-retest study participants, n=147.
| Characteristic | N (%) or Mean ± SD (Range) |
|
|---|---|---|
| Age, years | 49.1 ± 12.3 (21–70) | |
| 18–44 years old | 51 (34.7) | |
| 45–59 years old | 61 (41.5) | |
| 60–70 years old | 35 (23.8) | |
| Sex | ||
| Female | 95 (64.6) | |
| Male | 52 (35.4) | |
| Race | ||
| White/Caucasian | 111 (75.5) | |
| Black/African American | 22 (15.0) | |
| Asian | 12 (8.2) | |
| American Indian/Alaska Native | 2 (1.4) | |
| Ethnicity | ||
| Hispanic | 17 (11.6) | |
| Non-Hispanic | 130 (88.4) | |
| Education | ||
| ≤ High school | 7 (4.8) | |
| Some college | 43 (29.3) | |
| College or above | 97 (66.0) | |
| Employment status | ||
| Employed | 109 (74.1) | |
| Unemployed | 9 (6.1) | |
| Homemaker/Student/Retired | 23 (15.6) | |
| Disabled, unable to work | 6 (4.1) | |
| Annual family income | ||
| <$75,000 | 35 (23.8) | |
| ≥$75,000 | 112 (76.2) | |
| Asthma onset age (self-report) | ||
| <5 years of age | 24 (16.3) | |
| 5 years of age - puberty† | 33 (22.4) | |
| Puberty - 17.9 years of age | 16 (10.9) | |
| ≥18 years of age | 74 (50.3) | |
| Aeroallergen(s) reported among asthma triggers‡ | ||
| Yes | 140 (95.2) | |
| No | 7 (4.8) | |
| Smoker | ||
| Current smoker | 5 (3.4) | |
| Ex-smoker | 30 (20.4) | |
| Never smoker | 112 (76.2) | |
| BMI, kg/m2 | 31.5 ± 7.9 (19.2–63.2) | |
| Normal weight (18.5 to 24.9 kg/m2) | 26 (17.7) | |
| Overweight (25 to 29.9 kg/m2) | 52 (35.4) | |
| Obese (≥30 kg/m2) | 69 (46.9) | |
| Berlin Questionnaire (Obstructive Sleep Apnea risk) | ||
| Low Risk | 74 (50.3) | |
| High Risk | 73 (49.7) | |
| No. asthma exacerbations requiring OCS§ (12 mos. preceding enrollment) | 0.4 ± 0.8 (0–5) | |
| 0 | 106 (72.1) | |
| 1 | 29 (19.7) | |
| >1 | 12 (8.2) | |
| No. asthma-related outpatient medical visits‖ (12 mos. preceding enrollment) | 1.58 ± 1.95 | |
| 0 | 47 (32.0) | |
| 1 | 48 (32.7) | |
| >1 | 52(35.4) | |
| Treatment step* | ||
| Step 2 | 15 (10.2) | |
| Step 3 | 23 (15.6) | |
| Step 4 | 61 (41.5) | |
| Step 5 | 47 (32.0) | |
| Step 6 | 1 (0.7) | |
Treatment step definitions available http://www.ncbi.nlm.nih.gov/books/NBK7222/. Step 2 = Low-dose inhaled corticosteroid (ICS) or alternative (Cromolyn, LTRA, Nedocromil, or Theophylline); Step 3 = Low-dose (ICS) + long-acting inhaled beta2-agonist (LABA), or Medium-dose ICS, or alternative (Low-dose (ICS) + either LTRA, Theophylline, or Zileuton); Step 4 = Medium-dose (ICS) + LABA or alternative (Medium-dose (ICS) + either LTRA, Theophylline, or Zileuton); Step 5 = High-dose (ICS) + LABA ± Omalizumab for patients who have allergies; Step 6 = High-dose (ICS) + LABA + oral corticosteroid ± Omalizumab for patients who have allergies.
Puberty was defined as starting at age 12 for girls, age 14 for boys.
Aeroallergens included pollen, house dust mites, cats, dogs, cockroaches, and molds.
OCS (oral corticosteroid) prescription of at least three days for an asthma-related diagnosis code: asthma (ICD9 493.x) cough (ICD9 786.2) bronchitis (ICD9 490), upper respiratory infection (ICD(465.9), bronchospasm (ICD9 519.11); or wheezing (ICD9 786.07), given that all patients had underlying asthma. Courses of OCS separated by >7 days were treated as separate exacerbations. See Asthma outcomes: Exacerbations. Fuhlbrigge, A., et al. J Allergy Clin Immunol, 2012:129(3);S34–S48.
Outpatient office and Urgent Care Clinic visits with asthma diagnosis code (ICD9 493.x) within 12 mos. preceding enrollment. Does not include hospital emergency department visits
Intentional oversampling of patients with more intense asthma regimens yielded a sample with 25.8% of patients at treatment step 2 or 3, 41.5% at step 4, and 32.7% at step 5 or 6 at baseline (Table 1). In the population of eligible patients with persistent asthma from which the sample was drawn, an estimated 55% were at step 2 or 3, 30% at step 4, and only 15% at step 5 or 6. Over-sampling patients with more intense regimens also tended to increase heterogeneity on other, associated disease parameters.
Clinical characteristics of the sample at baseline and follow-up (Table 2) show that lung function averaged in the normal range with no significant between-assessment difference. Based on ACT score, at baseline 54.4% of the enrolled patients had well controlled, 22.4% poorly controlled, and 23.1% very poorly controlled asthma, which can be compared with estimated proportions of 63%, 17%, and 20%, respectively, among all eligible patients. At follow-up, the proportion of patients with well-controlled asthma was significantly higher (by 8.2 percentage points), with a corresponding decrease in the proportions with poorly/very poorly controlled asthma. The mean ASUI score at baseline was 0.8, indicating a relatively low level of symptoms, which is consistent with mean scores on the Marks AQLQ (Mean = 13.9, between 0 = “Not at all” and 20 = “Mildly” affected on the Marks 0–80 scale)32 and Juniper Mini-AQLQ (Mean = 5.4; between 5 = “A Little of the Time”/”Some Limitation” and 6 = “Hardly Any of the Time”/”A Little Limitation”).16 All of these asthma status measures, as well as mean A-IQOLS scores, differed significantly, but by quite small amounts, between baseline and follow-up.
Table 2.
Comparison of clinical characteristics of participants at baseline (test) and follow-up (retest), n=147.
| Baseline | Follow-up | ||
|---|---|---|---|
| Clinical Characteristic | N (%) or Mean ± SD (Range) |
N (%) or Mean ± SD (Range) |
p |
| FEV1 Percent Predicted, pre-bronchodilator‡ | 87.8 ± 18.5 (37.0–151.0) | 87.1 ± 18.2 (38.0–131.0) | 0.27 |
| ACT | 19.0 ± 3.9 (10.0–25.0) | 19.8 ± 3.7 (9.0–25.0) | 0.003 |
| Well-controlled (20–25) | 80 (54.4) | 92 (62.6) | <0.0001 |
| Poorly controlled (16–19) | 33 (22.4) | 33 (22.4) | |
| Very poorly controlled (5–15) | 34 (23.1) | 22 (15.0) | |
| ASUI§ | 0.8 ± 0.2 (0.2–1.0) | 0.9 ± 0.1 (0.3–1.0) | 0.001 |
| Marks AQLQ‖ | 13.9 ± 12.1 (0–65) | 11.3 ± 11.0 (0–44) | <0.0001 |
| Juniper Mini-AQLQ: Total Score¶ | 5.4 ± 1.1 (2.9–6.9) | 5.7 ± 1.0 (2.9–7.0) | <0.0001 |
| Mini-AQLQ: Symptom Score** | 5.2 ± 1.2 (2.2–7.0) | 5.6 ± 1.1 (2.2–7.0) | <0.0001 |
| PHQ-9†† (Depression) | 4.1 ± 4.1 (0–20) | 3.1 ± 3.5 (0–15) | <0.0001 |
| No. asthma-related OCS prescriptions (4 wks. preceding enrollment)‡‡ | 0.03 ± 0.18 (0–1) | 0.04 ± 0.20 (0–1) | 0.76 |
| No. asthma-related medical visits§§ (4 wks. preceding enrollment) | 0.10 ± 0.29 (0–1) | 0.14 ± 0.46 (0–4) | 0.32 |
| A-IQOLS* | 1.35 ± 0.45 (1.00–3.94) | 1.25 ± 0.34 (1.00–3.00) | 0.002 |
| QOLS† | 3.73 ± 0.76 (1.18–4.94) | 3.63 ± 0.74 (1.19–5.00) | 0.06 |
Abbreviations: A-IQOLS, Asthma Impact on Quality of Life Scale; QOLS, Flanagan Quality of Life Scale; FEV1, forced expiratory volume in one second; ACT, Asthma Control Test; ASUI, Asthma Symptom Utility Index; Marks AQLQ Asthma Quality of Life Questionnaire; Mini-AQLQ, Juniper mini-Asthma Quality of Life Questionnaire, total score and symptom sub-scale; PHQ-9, Patient Health Questionnaire.
Possible range, 1-No negative effect at all to 5-Extremely negative effect.
Possible range, 1-Not at all well satisfied to 5-Very well satisfied.
Sample size, n=146.
Possible range, 0-Worst possible symptoms to 1-Best state/no symptoms. Sample size, n=146.
Possible range, 0-Less impact on functional status to 80-Very severe impact on functional status.
Possible range, 1-Totally limited to 7-Not at all limited
Possible range, 1-Symptoms all of the time to 7-Symptoms none of the time.
Possible range, 0-No symptoms to 27-Major depression, severe.
OCS (oral corticosteroid) prescription of at least 3 days for an asthma-related diagnosis code (asthma, ICD9 493.x; cough, ICD9 786.2; bronchitis, ICD9 490; upper respiratory infection, ICD(465.9; bronchospasm, ICD9 519.11; or wheezing, CD9 786.07) within 4 weeks preceding enrollment. Courses of OCS separated by >7 days were treated as separate exacerbations. See Asthma outcomes: Exacerbations. Fuhlbrigge, A., et al. J Allergy Clin Immunol, 2012:129(3);S34–S48. McNemar exact test.
Outpatient office and Urgent Care Clinic visits with asthma diagnosis code (ICD9 493.x) within 4 weeks preceding enrollment. Does not include hospital emergency department visits. McNemar exact test
To compare baseline and follow-up exacerbation and visit rates (Table 2), the 4 week period preceding each assessment was examined. In the relatively short period of 4 weeks, visits and exacerbations were relatively infrequent and the proportions of patients who had exacerbations and the proportion who had asthma visits did not differ significantly between baseline and follow-up (McNemar exact test, p = 1.0 and p = 0.82, respectively).
Importance of the Quality of Life dimensions
From 63% to 94% of patients rated 15 of the 16 dimensions, including Independence, as either Important/Very Important to them (Table S1). Only Participation in activities relating to local and national government and public affairs, was considered Important/Very Important by a significantly smaller proportion of individuals (26%). All individuals had dimensions they rated as Important/Very Important, but there was considerable individual variation in priorities. The pattern of what was typically more or less important (Table S1) was generally consistent with Flanagan’s earlier findings for 30-, 50-, and 70-year olds and for men and women in the general U.S. population.5 This indicates that these dimensions have lasting importance to individuals despite changes in American life in the intervening 40 years. Even Participation in government and civic affairs was considered Important/Very Important by more than one-third (35%) of older women.
Asthma Impact on Quality of Life Scale (A-IQOLS)
The mean baseline (test) and follow-up (retest) A-IQOLS summary scores were 1.35 ± 0.45 and 1.25 ± 0.34, respectively (Table 2), indicating, on average, a relatively low perceived negative impact of asthma on patients’ QoL. Individuals’ summary scores ranged from 1 – 3.9. The entire rating scale range (1–5) was used in patients’ ratings of impairment on the individual QoL dimensions. Ratings of 5 (Extremely Negative Effect) were given on seven of the 16 dimensions and ratings of either 4 or 5 on 13 of the 16 dimensions. Eleven patients (7.5%) reported a negative impact on one or more of nine different dimensions (material well-being, work, independence, relations with their spouse/partner, relations with other family members, having and raising children, helping others, governmental/civic activities, and personal/spiritual development and practices) that was equal to or greater than the impact they reported on health and safety, social activities, and active recreation, which are the dominant focus of other measures commonly referred to as asthma-related quality of life measures.
A-IQOLS scores differed by income level (p = 0.008) but not by age, sex, race, ethnicity, level of education, or employment status (Table S2). Lower income patients (< $75,000) felt that their asthma had a more negative effect on their quality of life than did those at higher income levels (A-IQOLS: Mn ± SD = 1.53 ± 0.50 versus Mn ± SD = 1.30 ± 0.42). However, the association with income was not significant after controlling for ACT score (p = 0.53), since poorer asthma control was more prevalent in the lower income patients. Patients at high risk for obstructive sleep apnea (OSA) had significantly higher A-IQOLS scores (i.e., greater negative effect of asthma) than did those at low OSA risk (p = 0.01). Smoking status and BMI were not associated with A-IQOLS scores.
Baseline mean A-IQOLS scores differed significantly by level of asthma control -- well-controlled (1.15), poorly controlled (1.45) and very poorly controlled asthma (1.73) (p < 0.0001). Asthma treatment “step” -- was marginally but not significantly associated with A-IQOLS score (p = 0.07). However, the mean score for those at step 6, which is characterized by a need for routine use of multiple asthma medications (high-dose ICS + LABA + oral corticosteroid ± Omalizumab), was considerably higher (1.78) than that of those at treatment steps 4 or 5 (1.34 and1.39), which also was higher than for those at steps 2 and 3 (1.25 and 1.24). Mean A-IQOLS scores differed significantly among these three groups (p = 0.02).
Reliability
The A-IQOLS intraclass correlation coefficient, ICC = 0.56 (Table 3). This value is similar to the ICCs of the other self-reported asthma outcome measures (Table S3). A higher ICC was observed for the PPFEV1 (ICC = 0.90), which would be expected for an objective, albeit effort-dependent and labile, clinical measure.
Table 3.
Relative and population-independent reliabilities of the A-IQOLS and Flanagan QOLS, n=147.
| Relative reliability |
Population- independent reliability | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline Mean ±SD |
Follow-up Mean ±SD |
r | ICC | Mean diff. (Bias) |
MeanAll (of B and F) |
Between subject SDdiff |
t | p | 95% LOA (95% CI) LB |
95% LOA (95% CI) UB |
WSV | SEM | SEM % |
CR | |
| A-IQOLS | 1.35 ±0.45 | 1.25 ±0.34 | 0.58 | 0.56 | −0.10 | 1.30 | 0.37 | −3.23 | <0.002 | −0.83 (−0.94, −0.73) | 0.63 (0.53, 0.74) | 0.07 | ±0.27 | 20.34 | ±0.73 |
| QOLS | 3.73 ±0.76 | 3.63 ±0.74 | 0.67 | 0.67 | −0.10 | 3.68 | 0.61 | −1.89 | 0.06 | −1.29 (−1.46, −1.12) | 1.10 (0.93, 1.27) | 0.19 | ±0.43 | 11.71 | ±1.19 |
Definitions: SD= Standard Deviation; r= Pearson’s correlation coefficient; ICC= Intraclass Correlation Coefficient; t= t-value from paired t-test; p= p-value for paired t-test; LOA= Limits of Agreement; CI= Confidence Interval; L/UB= Lower/Upper Bound; WSV = within subject variance from two-way repeated-measure analysis of variance; SEM (Standard Error of Measurement)= √WSV; SEM%= SEM/MeanAll X 100; CR1= Coefficient of Repeatability= 2.77 × SEM.
Vaz, Sharmila, Torbjörn Falkmer, Anne Elizabeth Passmore, Richard Parsons, and Pantelis Andreou. 2013. “The Case for Using the Repeatability Coefficient When Calculating Test-Retest Reliability.” PloS One 8 (9): e73990. doi:10.1371/journal.pone.0073990.
The standard error of measurement (SEM = square root of the within-subject variance) is a fundamental statistic by which to evaluate the reliability of a measure (Table 3). Unlike a dimensionless index such as ICC, the SEM is interpretable in the units of the score scale.33 The A-IQOLS’ SEM = ±0.27 scale score points. The estimated lower and upper bounds of the SEM limits of agreement (LOA) – the range that contains 95% of the differences between repeated measurements on the same individual – were −0.83 and 0.63, respectively. The A-IQOLS’ coefficient of repeatability (CR) = 2.77× SEM = ±0.73 units on the impact rating scale, indicating that, with 95% probability, a within-person change in A-IQOLS score of 0.73 units or more, in either direction, can be considered a true/real change in the perceived negative effect of asthma. SEM values of the other asthma outcome measures and PHQ-9 are provided in Table S4.
A-IQOLS internal consistency reliability
The standardized coefficient α for the A-IQOLS was high (α = 0.91 at baseline; α = 0.93 at follow-up), and comparable to those of the other self-reported measures on which these patients were assessed (Table S3). Coefficient alpha, an indicator of the cross-sectional inter-correlation among the items, is commonly reported for measurement tools. However, it is not informative regarding measurement reliability -- the ability of a measure to discriminate between individuals -- which information is provided by the SEM (and derivative CR). Alpha is most useful in item selection to achieve a reduction in the number of items, which was not the relevant for the A-IQOLS or QOLS.
A-IQOLS convergent and divergent validity
With the exception of PPFEV1, A-IQOLS scores were significantly correlated with all of the asthma status measures, and depression (PHQ-9 (all p-values < 0.0001), at both baseline and follow-up (Table 4). However, in nearly all cases, the shared or common variance (R2) between the A-IQOLS and the other measures was less than 40%. At baseline and follow-up, ACT and A-IQOLS scores were moderately correlated (r = −0.50 and r = .53). A-IQOLS scores also were moderately correlated with ASUI (symptom) scores (r = −0.51 and r = −0.52) and more highly correlated with Marks AQLQ scores (r = 0.74 and r = 0.72) than with the ACT (asthma control), ASUI (symptom), and Juniper AQLQ scores. Even so, the common variance between Marks AQLQ and A-IQOLS was only about 50% and for other measures even lower.
Table 4.
Correlations and shared variances between A-IQOLS, QOLS, and other clinical characteristics, at baseline and at follow-up, n=147.
| A-IQOLS (n=147) | QOLS (n=147) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||||||||
| Clinical Characteristic | r* | p | R2 | r* | p | R2 | r* | p | R2 | r* | p | R2 |
| A-IQOLS | - | - | - | - | - | - | −0.39 | <.0001 | 0.15 | −0.40 | <.0001 | 0.16 |
| FEV1 Percent Predicted, pre-bronchodilator† | 0.03 | 0.74 | <0.01 | −0.004 | 0.96 | <0.01 | 0.08 | 0.35 | 0.0060 | 0.14 | 0.09 | 0.02 |
| ACT | −0.50 | <.0001 | 0.25 | −0.53 | <.0001 | 0.28 | 0.24 | 0.004 | 0.06 | 0.26 | 0.002 | 0.07 |
| ASUI† | −0.51 | <.0001 | 0.26 | −0.52 | <.0001 | 0.27 | 0.32 | <.0001 | 0.10 | 0.26 | 0.001 | 0.07 |
| Marks AQLQ | 0.74 | <.0001 | 0.55 | 0.72 | <.0001 | 0.52 | −0.48 | <.0001 | 0.23 | −0.41 | <0.001 | 0.17 |
| Juniper Mini-AQLQ: Total Score | −0.63 | <.0001 | 0.39 | −0.65 | <.0001 | 0.42 | 0.41 | <.0001 | 0.16 | 0.32 | <.0001 | 0.10 |
| Symptom Score | −0.58 | <.0001 | 0.33 | −0.60 | <.0001 | 0.36 | 0.38 | <.0001 | 0.15 | 0.29 | 0.0003 | 0.09 |
| PHQ-9 | 0.45 | <.0001 | 0.20 | 0.53 | <.0001 | 0.28 | −0.52 | <.0001 | 0.27 | −0.54 | <.0001 | 0.30 |
| No. of exacerbations requiring OCS‡ | 0.10$ | 0.24 | 0.01 | 0.21$ | 0.01 | 0.04 | 0.08$ | 0.36 | 0.006 | −0.19$ | 0.02 | 0.04 |
| No. of asthma-related medical visits‖ | 0.15$ | 0.06 | 0.02 | 0.14$ | 0.10 | 0.02 | −0.04$ | 0.67 | 0.0001 | −0.05$ | 0.53 | <0.01 |
Abbreviations: A-IQOLS, Asthma Impact on Quality of Life Scale; QOLS, Flanagan Quality of Life Scale; FEV1, forced expiratory volume in one second; ACT, Asthma Control Test; ASUI, Asthma Symptom Utility Index; Marks AQLQ, Asthma Quality of Life Questionnaire; Mini-AQLQ, Juniper mini-Asthma Quality of Life Questionnaire, total score and symptom sub-scale; PHQ-9, Patient Health Questionnaire.
r=Pearson product-moment correlation
Sample size, n=146.
OCS (oral corticosteroid) prescription of at least 3 days for an asthma-related diagnosis code (asthma, ICD9 493.x; cough, ICD9 786.2; bronchitis, ICD9 490; upper respiratory infection, ICD(465.9; bronchospasm, ICD9 519.11; or wheezing, CD9 786.07) within 4 weeks prior to enrollment. Courses of OCS separated by >7 days were treated as separate exacerbations. See Asthma outcomes: Exacerbations. Fuhlbrigge, A., et al. J Allergy Clin Immunol, 2012:129(3);S34–S48.
Spearman Rank-Order Correlation.
Outpatient office visit or Urgent Care Clinic visit with asthma-related diagnosis code (ICD9 493.x) within 4 weeks preceding baseline and follow-up assessments. Does not include hospital emergency department visits.
At baseline neither the number of exacerbations requiring OCS use nor the number of medical visits in the preceding 4 weeks was significantly associated with A-IQOLS scores, but the follow-up correlation with exacerbations was significant (p = 0.01) (Table 4). Neither the number of exacerbations nor of visits in these brief time periods accounted for a meaningful proportion of the variance in A-IQOLS scores.
Depression (PHQ-9) was significantly correlated with patients’ evaluation of the negative impact of asthma on their quality of life (A-IQOLS scores). However, the correlation was not strong and the PHQ-9 and A-IQOLS shared only about one-fifth of their variance in common.
A-IQOLS’ sensitivity to changes in asthma status
Although small, baseline-to-follow-up changes in asthma status measures -- asthma control (ACT scores), asthma symptoms (ASUI scores), Marks and Juniper AQLQ scores, and number of asthma medical visits -- were significantly correlated with changes in A-IQOLS scores in the expected directions (Table 5). And while the A-IQOLS was significantly correlated with the number of exacerbations in the preceding 12 months (Table S2), the extremely small baseline to follow-up differences in the numbers of exacerbations and asthma-related medical visits in the relatively brief (one month) time periods preceding each assessment were not significantly associated with changes in A-IQOLS scores.
Table 5.
Correlations between baseline-to-follow-up changes in asthma status measures and changes in A-IQOLS and QOLS scores, with estimates of shared variance, n=147.
| Change in Characteristic |
Association with change in A-IQOLS Score |
Association with change in QOLS Score |
|||||
|---|---|---|---|---|---|---|---|
| Clinical Characteristics | Mean ± SD | r* | p | R2 | r* | p | R2 |
| FEV1 Percent Predicted, pre-bronchodilator† | −0.74 ± 8.06 | 0.10 | 0.22 | 0.01 | −0.08 | 0.32 | 0.01 |
| ACT | 0.79 ± 3.16 | −0.40 | <0.0001 | 0.16 | −0.07 | 0.40 | 0.005 |
| ASUI‡ | 0.04 ± 0.15 | −0.33 | <0.0001 | 0.11 | −0.02 | 0.77 | 0.001 |
| Marks AQLQ | −2.59 ± 7.02 | 0.52 | <0.0001 | 0.27 | −0.005 | 0.96 | <0.01 |
| Mini-AQLQ: Total Score | 0.28 ± 0.78 | −0.55 | <0.0001 | 0.30 | 0.07 | 0.38 | 0.01 |
| Mini-AQLQ: Symptom Score | 0.36 ± 0.93 | −0.45 | <0.0001 | 0.20 | 0.06 | 0.49 | 0.003 |
| PHQ-9 | −1.03 ± 2.96 | 0.20 | 0.01 | 0.04 | −0.16 | 0.053 | 0.03 |
| No. exacerbations requiring OCS§ | 0.01 ± 0.27 | 0.10‖ | 0.24 | 0.01 | 0.01‖ | 0.89 | <0.01 |
| No. asthma-related medical visits¶ | 0.04 ± 0.49 | 0.11‖ | 0.20 | 0.01 | −0.07‖ | 0.41 | <0.01 |
| A-IQOLS | −0.10 ± 0.37 | - | - | - | −0.15 | 0.07 | 0.02 |
| QOLS | −0.10 ± 0.61 | ||||||
Abbreviations: A-IQOLS, Asthma Impact on Quality of Life Scale; QOLS, Flanagan Quality of Life Scale; FEV1, forced expiratory volume in one second; ACT, Asthma Control Test; ASUI, Asthma Symptom Utility Index; Marks AQLQ, Asthma Quality of Life Questionnaire; Mini-AQLQ, Juniper mini-Asthma Quality of Life Questionnaire, total score and symptom sub-scale; PHQ-9, Patient Health Questionnaire.
r=Pearson product-moment correlation
Sample size, n=146.
Sample size, n=146.
OCS (oral corticosteroid) prescription of at least 3 days for an asthma-related diagnosis code (asthma, ICD9 493.x; cough, ICD9 786.2; bronchitis, ICD9 490; upper respiratory infection, ICD(465.9; bronchospasm, ICD9 519.11; or wheezing, CD9 786.07) within 4 weeks preceding enrollment. Courses of OCS separated by >7 days were treated as separate exacerbations. See Asthma outcomes: Exacerbations. Fuhlbrigge, A., et al. J Allergy Clin Immunol, 2012:129(3);S34–S48.
Spearman Rank-Order Correlation.
Outpatient office visit or Urgent Care Clinic visit with asthma diagnosis code (ICD9 493.x) within 4 weeks preceding enrollment. Does not include hospital emergency department visits.
Changes in depression were significantly associated with changes in A-IQOLS scores (r = 0.20; p = 0.01).
Current Quality of Life (QOLS)
Participants’ mean QOLS summary scores were 3.7 ± 0.8 at baseline and 3.6 ± 0.7 at follow-up -- on average, they felt that their needs and wants were Well Satisfied or Very Well Satisfied (Table 2). The baseline to follow-up change in mean QOLS scores was borderline significant (p = 0.06). QOLS scores did not differ significantly by age, sex, race, level of education, or employment status (Table S1), but were significantly associated with ethnicity (lower in Hispanics than non-Hispanics; p = 0.03) and family income (lower in those with annual family income < $75,000; p = 0.01). Smoking status and BMI were not associated with QOLS scores. Patients at high risk for obstructive sleep apnea (OSA) had significantly lower QOLS scores than did those at low OSA risk (p = 0.002). Some high risk patients may have had OSA, especially given the high obesity rate, but some may have been reporting sleep problems largely or partially associated with asthma.
QOLS reliability
The QOLS’ within-subject ICC = 0.67 (Table 3), its standard error of measurement (SEM) = ±0.43, and its repeatability coefficient (CR) = ±1.19 (Table 3). One can be 95% confident that within-person QOLS score change of 1.2 units or more in either direction is a true/real change in how well the individual feels his/her needs and wants are being satisfied.
QOLS internal consistency reliability
The QOLS standardized coefficient α = 0.93 (Table S4). Again, alpha is not an indicator of measurement reliability.
QOLS convergent and divergent validity: correlations with health status measures
QOLs scores were not significantly correlated with the percent predicted FEV1 at either baseline or follow-up (Table 4) but were significantly correlated with the other asthma/health status measures and (at follow-up only) with the number of exacerbations requiring OCS use. As expected, the correlations between the asthma status measures and QOLS scores, and consequently their shared variances, were typically lower than the corresponding correlations between these measures and A-IQOLS scores, at both baseline and follow-up. Treatment step (2–6) and the number of asthma medical visits were not correlated with QOLS scores.
QOLS scores were significantly (p < 0.0001), but only weakly correlated28 with A-IQOLS scores (r = −0.39 at baseline), with only approximately 15% common variance.
The correlation between QOLS scores and depression (PHQ-9) and QOLS (r = −0.52 at baseline; p < 0.0001) was slightly greater than that between the PHQ-9 and A-IQOLS (r = 0.45), but this difference was not statistically significant.34
QOLS sensitivity to changes in asthma status
In contrast to the strong associations between changes in asthma status measures and changes in A-IQOLS scores between baseline and follow-up, changes in asthma status measure were not significantly correlated with changes in QOLS scores (Table 5). Similarly, the correlation between changes in A-IQOLS scores and changes in QOLS scores was very weak (r = −0.15) and not statistically significant (p = 0.07), at least for the relatively small changes observed between test and retest. Changes in depression (PHQ-9 scores), however, were significantly correlated with changes in QOLS scores (p = 0.053).
DISCUSSION
The A-IQOLS has strong content validity -- it directly queries the patient about the effects of their asthma on a comprehensive set of dimensions of individuals’ quality of life whose continued relevance is supported by the present results. Its scores proved to be reliable (i.e., to discriminate well between patients with differing asthma status, to have an appropriate-size SEM determined in a test-retest study), and to have strong convergent validity. Its scores and score changes were significantly correlated, in the expected directions, with scores and score changes in other asthma outcomes measures but not so highly correlated as to compromise its divergent/discriminant validity. The relatively low shared variances indicate that A-IQOLS scores provide unique information not provided by other asthma measures. Many of those measures, long included in the asthma outcome measurement toolbox, continue to be useful, but are not adequate proxies for a measure of the patient’s perception of how their asthma and its treatment are affecting their quality of life.
The relatively new Impact of Asthma on Quality of Life Scale (IAQLS)35 consists of items drawn from the National Institutes of Health’s Patient–Reported Outcome Measurement Information System (PROMIS®) database.36 PROMIS supports development of efficient, precise, valid, responsive adult and child reported measures of health status in specific health domains (http://www.nihpromis.org/about/missionvisiongoals), and addresses many limitations of existing generic and disease-specific health status measures. While the IAQLS may provide a better measure of asthma patients’ functional status, like earlier measures, it does not directly assess the patient’s perception of the impact of asthma on their life. Hence, contrary to its developer’s claim, it is not responsive to the central recommendation of the 2010 NIH AOW with regard to quality of life measures.
Potential research uses of the A-IQOLS
In asthma research the A-IQOLS may be used to characterize study populations at baseline. A-IQOLS scores, reflecting the patients’ perception of disease impact, also may have explanatory use in treatment adherence research. Importantly, a measure of patient perception of the effects of asthma and its treatment could provide an important secondary and, in some cases, potentially a primary outcome measure in trials of asthma therapy. In patients with moderately severe or severe asthma, where both the disease and its treatment may have significant negative effects, assessment of the patient’s perspective may be of even greater importance and may help ensure a more complete evaluation of therapeutic benefits than is provided by physiological, symptom, or functional status measures.
Potential research uses of the QOLS
The QOLS can be administered to any adult, regardless of health status. However, unlike other generic measures widely used in health research (e.g., the SF-1237 or the EuroQol-5D,38) which assess symptoms, mood, and functional limitations that have diverse etiology and high prevalence in the general population (e.g., pain), the QOLS measures the individual’s perception of their quality of life. The present study found that, while QOLS scores are reliable and are significantly correlated with A-IQOLS scores, the perceived negative effect of asthma on dimensions of an individual’s quality of life (A-IQOLS scores) shares only 15% variance with how well the individual feels their needs and wants are being satisfied (QOLS scores), and score changes in A-IQOLS and QOLS scores share only 2% common variance. Further, in asthma patients, QOLS scores are somewhat less strongly correlated with other asthma outcomes measures than are A-IQOLS scores. This suggests that, for many if not most asthma patients, their overall quality of life is less dependent on their asthma than on other factors. An individuals’ quality of life has many influences, historically and at any given point in time. A health problem is just one such potential influence. It appears that a measure, such as the A-IQOLS, which asks the patient to evaluate the impact of a specific disease on their quality of life, is a more direct, sensitive, and appropriate approach than inferring impact from changes or differences in a generic measure such as the QOLS. However, this does not mean that the QOLS has no appropriate clinical or behavioral research use. On the contrary, it is a reliable and valid measure and may be particularly useful as a generic QoL measure for characterizing and comparing study populations, as a measure of QoL when that construct is potentially a mediator or moderator of other outcomes, and as a primary or secondary outcome in studies of special populations such as those with multiple chronic diseases or diseases that are very severe and/or life-limiting.
Clinical use of the A-IQOLS and QOLS
The present study identified the minimal within-person score changes on the A-IQOLS and the QOLS that represent true change. This information is critical to their potential clinical use. They provide standardized measures of the patients’ perception of their QoL and of the negative effects of asthma on their QoL using a common conceptual framework. Both are brief, both can be completed on paper or electronically at home or in the clinic waiting room, and scoring is straightforward -- features that make their clinical use more feasible. For example, patients whose asthma is not as well controlled as it might be, but who feel asthma is having little negative effect (low A-IQOLS score), may be making personal choices about medication use or their activities that are satisfactory for them, and may not want or warrant escalation of treatment to improve asthma control. Other patients with poorly controlled asthma may regard their asthma as having only a small negative effect because other circumstances, situations, or health conditions are having a much greater negative effect. This circumstance, if revealed to clinicians by A-IQOLS and/or QOLS scores and ratings, and used in conjunction with other clinical information, may prove useful in clinical management. Given the current state of knowledge, choosing the appropriate response to a patient’s A-IQOLS or QOLS results would be a matter of clinician judgement. Further research is needed to determine whether the summary scores and/or the individual dimension ratings can play a useful role in informing clinical management decisions and care.
In both research and practice, a disease-specific instrument such as the A-IQOLS and a generic instrument such as the QOLS can be used separately or together. A disease-specific instrument appears most useful in patients with a single significant chronic disease or a small number of relatively distinct conditions. When rating the negative effect of a disease, it is to be expected that some patients will incorrectly attribute symptoms, functional limitations, and side effects to the disease when they actually result from another cause (e.g., shortness of breath may result from asthma and/or obesity and physical deconditioning). Conversely, patients may not recognize certain symptoms or side effects as being due to asthma or its treatment. However, such perceptions, accurate or not, may influence patients’ disease management. Further, this is not unique to the A-IQOLS. The same potential confusions exist in patient-reported symptoms, functional limitations, and medication side effects on asthma-related health status measures, and other self-report measures.
The QOLS may have an additional unique role to play in research and clinical practice involving patients with multiple chronic conditions (MCC) and/or a severe or life-limiting conditions. In such circumstances, the goals of medical treatment are appropriately aimed at maintaining, and if possible enhancing, the patient’s overall QoL. For that purpose, the QOLS has potential advantages over both disease-specific measures such as the A-IQOLS and generic measures such as the SF-12 or EuroQoL. Further, with disease progression may come a shift or narrowing in the areas of life that are most important to the individual, which the QOLS is uniquely able to accommodate. Further research is needed on the relative merits of the QOLS in patients with multiple, severe, and/or life-limiting conditions.
Limitations
The present study was intentionally broadly representative of asthma patients in its racial/ethnic and sex distribution, and heterogeneous in level of treatment intensity and asthma severity. It was not, however, designed to be representative in socioeconomic status, education, or source of health care. Participants also were drawn from a single health care system, although not a closed/single insurer system -- many PAMF patients also receive care from non-PAMF primary or specialty care providers.
More importantly, the sample size is too small to determine the psychometric properties of the A-IQOLS and QOLS in specific patient subgroups, e.g., those with very low levels of education, particular racial or ethnic groups, or those with severe asthma. However, several other clinical trials of asthma treatment are underway that will support key sub-group analyses (to determine the generalizability of use of the instruments) and will include analyses of follow-up data from clinical trials of asthma treatment (to determine sensitivity to treatment effects, which will further inform power and sample size estimates for future clinical trials.
Finally, the present sample is too small to properly assess the incremental value of weighting individuals’ responses on the A-IQOLS and/or QOLS scales by their personal Importance ratings when computing summary scores. Typically, such weighting strategies have not proven to be useful, have significant computational disadvantages in scoring,33 and require collection of additional information, such as on the present Importance scale, in order to calculate appropriate weights. It is likely that ratings on the A-IQOLS and QOLS already take into account the importance of dimensions to the individual. However, the issue of importance-weighting inevitably arises with regard to instruments of this type, and will be addressed in our analysis of data from other studies now underway.
Future directions
The A-IQOLS is a model for a potential family of IQOLS measures to assess the quality of life impact of other diseases, conditions, and treatments. Such measures are straightforward to create and are relevant to assessing the quality of life impact of virtually any health condition or treatment. They would utilize the same rating scale as the A-IQOLS, but the stem question would specify whatever disease or condition was of interest. The use of a common rating scale permits direct comparison of the negative effects of different diseases and treatments on quality of life and may also support cost benefit studies. For some purposes a bi-directional scale (both positive and negative effects) might also be used.
Conclusions
The Asthma Impact on Quality of Life Scale (A-IQOLS) is a reliable and valid measure of patients’ perception of the impact of asthma on their quality of life, providing unique information not provided by other asthma self-report measures that assess patient’s symptoms and functional status. Further study is needed to understand the performance of this measure in particular patient subgroups, its sensitivity to the effects of different therapeutic interventions, and its value in clinical care. The success of the IQOLS approach in asthma suggests that this type of measure may be useful in other diseases as well. The Flanagan QOLS is a reliable and valid measure of patients’ perception of whether their needs and wants are being satisfied and yields a score that represents their perceived quality of life. While less sensitive than the A-IQOLS to changes in asthma status, it has potential value in characterizing study populations and as an outcome measure in research involving persons with severe, multiple, or life-limiting conditions. Both the A-IQOLS and QOLS appear to be useful in clinical research and potentially useful in clinical care.
Supplementary Material
Clinical Implications.
The Asthma Impact on Quality of Life Scale assesses the negative impact of asthma on quality of life from the patient’s perspective, providing unique information for evaluating asthma outcomes in research and clinical settings.
Acknowledgments
The authors gratefully acknowledge the contributions of Nicholas Vesom to the conduct of the test-retest study, as well as the contributions of the study participants and staff of the Palo Alto Medical Foundation Mountain View’s Allergy and Pulmonology services where patient assessment occurred. We also acknowledge the expert review and helpful suggestions on this manuscript by Lauress L. Wise, PhD. Ultimately, responsibility for the research and for this report rests solely with the authors.
Funding: Supported by Grant No. HL119845 (PI: S. Wilson) from the National Heart, Lung and Blood Institute/NIH.
Abbreviations used
- ACT
Asthma Control Test
- A-IQOLS
Asthma Impact on Quality of Life Scale
- AOW
Asthma Outcomes Workshop
- ASUI
Asthma Symptom Utility Index
- BTR
Bronchial Thermoplasty Responder study
- COPD
Chronic Obstructive Pulmonary Disease
- CR
Repeatability Coefficient
- FEV1
Forced Expiratory Volume in 1 second
- IAQLS
Impact of Asthma on Quality of Life Scale
- ICC
Intraclass Correlation Coefficient
- LASST
Long-acting Beta Agonist Step Down Study
- LOA
Limit of Agreement
- Marks AQLQ
Marks Asthma Quality of Life Questionnaire
- Mini-AQLQ
Juniper Mini Asthma Quality of Life Questionnaire
- NIOSH
National Institute of Occupational Safety and Health
- OCS
Oral Corticosteroid
- OSA
Obstructive Sleep Apnea
- PHQ-9
Patient Health Questionnaire
- PROMIS
Patient Reported Outcomes Measurement Information System
- QoL
Quality of Life
- QOLS
Flanagan Quality of Life Scale
- SDS
Disproportionate Stratified Sampling
- SEM
Standard Error of Measurement
- STROBE
STrengthening the Reporting of OBservational studies in Epidemiology
- U.S.
United States
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Busse WW, Morgan WJ, Taggart V, Togias A. Asthma outcomes workshop: Overview. J Allergy Clin Immunol. 2012;129:S1–8. doi: 10.1016/j.jaci.2011.12.985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson SR, Rand CS, Cabana MD, Foggs MB, Halterman JS, Olson L, et al. Asthma outcomes: Quality of life. J Allergy Clin Immunol. 2012;129:S88–123. doi: 10.1016/j.jaci.2011.12.988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Streiner DL, Norman GR. Health Measurement Scales: A Practical Guide to Their Development and Use. 2. Oxford University Press; 1995. [Google Scholar]
- 4.Flanagan JC. A research approach to improving our quality of life. Am Psychol. 1978;33:138. [Google Scholar]
- 5.Flanagan JC. Measurement of quality of life: current state of the art. Arch Phys Med Rehabil. 1982;63:56–9. [PubMed] [Google Scholar]
- 6.Burckhardt CS, Woods SL, Schultz AA, Ziebarth DM. Quality of life of adults with chronic illness: a psychometric study. Res Nurs Health. 1989;12:347–54. doi: 10.1002/nur.4770120604. [DOI] [PubMed] [Google Scholar]
- 7.Wilson SR, Flanagan JC. Quality of Life as Perceived by 30 Year Old Army Veterans: Supplementary Report. [cited 2015 Aug 24];1974 Available from: http://eric.ed.gov/?id=ED114537.
- 8.Burckhardt CS, Archenholtz B, Bjelle A. Measuring the quality of life of women with rheumatoid arthritis or systemic lupus erythematosus: a Swedish version of the Quality of Life Scale (QOLS) Scand J Rheumatol. 1992;21:190–5. doi: 10.3109/03009749209099220. [DOI] [PubMed] [Google Scholar]
- 9.Anderson KL. The effect of chronic obstructive pulmonary disease on quality of life. Res Nurs Health. 1995;18:547–56. doi: 10.1002/nur.4770180610. [DOI] [PubMed] [Google Scholar]
- 10.Burckhardt CS, Anderson KL. The Quality of Life Scale (QOLS): reliability, validity, and utilization. Health Qual Life Outcomes. 2003;1:60. doi: 10.1186/1477-7525-1-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ma J, Strub P, Lavori PW, Buist AS, Camargo CA, Nadeau KC, et al. DASH for asthma: A pilot study of the DASH diet in not-well-controlled adult asthma. Contemp Clin Trials. 2013;35:55–67. doi: 10.1016/j.cct.2013.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007;120:S94–138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 13.Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, et al. Development of the asthma control test: A survey for assessing asthma control. J Allergy Clin Immunol. 2004;113:59–65. doi: 10.1016/j.jaci.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 14.Bime C, Wei CY, Holbrook JT, Sockrider MM, Revicki DA, Wise RA. Asthma Symptom Utility Index: Reliability, validity, responsiveness, and the minimal important difference in adult asthmatic patients. J Allergy Clin Immunol. 2012;130:1078–84. doi: 10.1016/j.jaci.2012.07.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marks GB, Dunn SM, Woolcock AJ. An evaluation of an asthma quality of life questionnaire as a measure of change in adults with asthma. J Clin Epidemiol. 1993;46:1103–11. doi: 10.1016/0895-4356(93)90109-e. [DOI] [PubMed] [Google Scholar]
- 16.Juniper E, Guyatt G, Cox F, Ferrie P, King D. Development and validation of the mini asthma quality of life questionnaire. Eur Respir J. 1999;14:32–8. doi: 10.1034/j.1399-3003.1999.14a08.x. [DOI] [PubMed] [Google Scholar]
- 17.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 18.Miller MR. Standardisation of spirometry. Eur Respir J. 2005;26:319–38. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 19.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–87. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 20.Tepper RS, Wise RS, Covar R, Irvin CG, Kercsmar CM, Kraft M, et al. Asthma outcomes: Pulmonary physiology. Stand Asthma Outcomes Clin Res Rep Asthma Outcomes Workshop. 2012;129:S65–87. doi: 10.1016/j.jaci.2011.12.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Juniper E, Guyatt G, Epstein R, Ferrie P, Jaeschke R, Hiller T. Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax. 1992;47:76–83. doi: 10.1136/thx.47.2.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Juniper E, Buist A, Cox F, Ferrie P, King D. Validation of a Standardized Version of the Asthma Quality of Life Questionnaire. CHEST J. 1999;115:1265. doi: 10.1378/chest.115.5.1265. [DOI] [PubMed] [Google Scholar]
- 23.Johnson JA, Coons SJ, Ergo A, Szava-Kovats G. Valuation of EuroQOL (EQ-5D) health states in an adult US sample. PharmacoEconomics. 1998;13:421–33. doi: 10.2165/00019053-199813040-00005. [DOI] [PubMed] [Google Scholar]
- 24.Marks G, Dunn S, Woolcock A. A scale for the measurement of quality of life in adults with asthma. J Clin Epidemiol. 1992;45:461–72. doi: 10.1016/0895-4356(92)90095-5. [DOI] [PubMed] [Google Scholar]
- 25.Revicki DA, Leidy NK, Brennan-Diemer F, Sorensen S, Togias A. Integrating patient preferences into health outcomes assessment: the multiattribute Asthma Symptom Utility Index. Chest. 1998;114:998–1007. doi: 10.1378/chest.114.4.998. [DOI] [PubMed] [Google Scholar]
- 26.Vaz S, Falkmer T, Passmore AE, Parsons R, Andreou P. The case for using the repeatability coefficient when calculating test-retest reliability. PloS One. 2013;8:e73990. doi: 10.1371/journal.pone.0073990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lexell JE, Downham DY. How to assess the reliability of measurements in rehabilitation. Am J Phys Med Rehabil Assoc Acad Physiatr. 2005;84:719–23. doi: 10.1097/01.phm.0000176452.17771.20. [DOI] [PubMed] [Google Scholar]
- 28.Evans JD. Straightforward statistics for the behavioral sciences. Brooks/Cole; 1996. [Google Scholar]
- 29.CDC - AsthmaStats - Asthma and Obesity. [cited 2016 Oct 17]; [Internet]. Available from: http://www.cdc.gov/asthma/asthma_stats/asthma_obesity.htm.
- 30.Camargo CA, Weiss ST, Zhang S, Willett WC, Speizer FE. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Arch Intern Med. 1999;159:2582–8. doi: 10.1001/archinte.159.21.2582. [DOI] [PubMed] [Google Scholar]
- 31.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 32.Katz PP, Eisner MD, Henke J, Shiboski S, Yelin EH, Blanc PD. The Marks Asthma Quality of Life Questionnaire: further validation and examination of responsiveness to change. J Clin Epidemiol. 1999;52:667–75. doi: 10.1016/s0895-4356(99)00026-8. [DOI] [PubMed] [Google Scholar]
- 33.Streiner DL, Norman GR, Cairney J. Health measurement scales : a practical guide to their development and use. Oxford: Oxford University Press; 2015. [Google Scholar]
- 34.Steiger JH. Tests for comparing elements of a correlation matrix. Psychol Bull. 1980;87:245. [Google Scholar]
- 35.Eberhart NK, Sherbourne CD, Edelen MO, Stucky BD, Sin NL, Lara M. Development of a measure of asthma-specific quality of life among adults. Qual Life Res. 2014;23:837–48. doi: 10.1007/s11136-013-0510-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.PROMIS. PROMIS Mission Vis. Goals. [cited 2015 Dec 21]; [Internet]. Available from: www.nihpromis.org.
- 37.Ware JE, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 38.Brooks R, Group E. EuroQol: the current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 39.Johns Hopkins University. Bethesda (MD): National Library of Medicine (US); 2000. [cited 2016 Apr 22]. Long-acting Beta Agonist Step Down Study (LASST) ClinicalTrials.gov [Internet]. Available from: http://clinicaltrials.gov/show/ NCT01437995 NLM Identifier: NCT01437995. [Google Scholar]
- 40.Johns Hopkins University. Bethesda (MD): National Library of Medicine (US); 2000. [cited 2016 Apr 22]. Effect of Positive Airway Pressure on Reducing Airway Reactivity in Patients With Asthma (CPAP) ClinicalTrials.gov [Internet]. Available from: http://clinicaltrials.gov/show/NCT01629823 NLM Identifier: NCT01629823. [Google Scholar]
- 41.Sarikonda K, Sheshadri A, Koch T, Kozlowski J, Wilson B, Schechtman K, et al. Predictors Of Bronchial Thermoplasty Response In Patients With Severe Refractory Asthma. Am J Respir Crit Care Med. 2014:A2429–A2429. [Google Scholar]
- 42.Washington University School of Medicine. Bethesda (MD): National Library of Medicine (US); 2000. [cited 2016 Apr 22]. A Prospective Observational Study of Biopredictors of Bronchial Thermoplasty Response in Patients With Severe Refractory Asthma (BTR Study) (BTR) ClinicalTrials.gov [Internet]. Available from: https://clinicaltrials.gov/show/NCT01185275 NLM Identifier: NCT01185275. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.