Abstract
Objective
Qualitative interviews with 183 young adults (YA) in the follow up of the Multi-modal Treatment Study of Children with and without ADHD (MTA) provide rich information on beliefs and expectations regarding ADHD, life’s turning points, medication use, and substance use (SU).
Method
Participants from four MTA sites were sampled to include those with persistent and atypically high SU, and a local normative comparison group (LNCG). Respondents were encouraged to “tell their story” about their lives, using a semi-structured conversational interview format.
Results
Interviews were reliably coded for interview topics. ADHD youth more often desisted from SU because of seeing others going down wrong paths due to SU. Narratives revealed very diverse accounts and explanations for SU-ADHD influences.
Conclusions
Qualitative methods captured the perspectives of YAs regarding using substances. This information is essential for improving resilience models in drug prevention and treatment programs and for treatment development for this at-risk population.
Keywords: ADHD, MTA Study, Substance Use, Qualitative Research, Mixed Methods
Introduction
Research on Attention-Deficit Hyperactivity Disorder (ADHD)-related risk for substance use disorders (SUD) has relied primarily on clinical interviews, DSM-based mental health assessments, paper-and-pencil questionnaires about mediators and moderators, and studies testing biological mechanisms (neuroimaging and genetics). Combining quantitative and qualitative methods allow examination of specific malleable factors that contribute to SU onset, persistence, or desistence, changes in clinical course, and ultimate outcomes. Qualitative methods incorporating the beliefs and accounts of young adults (YAs) themselves can discover important setting and context-level influences for those with a variety of mental illnesses, capture the experiences and perspectives of the YAs, and identify triggers or turning points that often are missed in questionnaires (Capps & Ochs, 1995; Kleinman, 1988; Ochs & Capps, 1996; T.S. Weisner, 2002). Discovery of such patterns can lead to hypotheses that then can be tested using other methods.
Individual trajectories of SUD development among youth with ADHD have not been carefully examined. The role of key “turning points” during challenging developmental transitions (e.g., changes in life course related to cognitive, behavioral, or social-emotional events during adolescence and young adulthood) are not well understood. In this report, we describe qualitative interviews with 183 YAs participating in the 14- and 16-year follow up of the Multi-Modal Treatment Study of ADHD (MTA).
A recent comprehensive review of ADHD and SUD (Molina & Pelham Jr, 2014) concludes “Beliefs about the effects of alcohol and other drugs (expectancies) have received minimal research attention in the ADHD literature despite their well-documented contribution to alcohol use disorder.” (p.629). Qualitative methods can improve understanding of how and why YAs decide to start, persist or cease using substances, as they describe these processes from their point of view, and what these behavior changes mean for them. This is essential for improving resilience models in drug prevention and treatment programs (Johnston, O’Malley, & Bachman, 1999; Masten, Faden, Zucker, & Spear, 2008).
Qualitative and quantitative evidence show associations between ADHD and the Western social and cultural expectations for desiring more goods and experiences (Whybrow, 2006), the increased expectation of more intense, engaged, 24/7 work and activity (Martin, 2007), intentional work choices that have a better fit with behavioral, cognitive, and emotional tendencies in young adulthood (Lasky, et al, 2016), and changing cultural conceptions of conditions like ADHD or mania and their degree of “fit” with our economy and social values (Whybrow, 2006).
Integrating qualitative and quantitative data is important for developing interventions (Thomas S. Weisner, 2014; Thomas S. Weisner & Duncan, 2014). For example, youth beliefs regarding connections between SUD and ADHD medication are not well understood, though it is clear that YA, parents, and peers often have strong beliefs about connections (or lack thereof) between ADHD medication and SUD. The importance of further understanding these beliefs is highlighted by Molina and Pelham:
“Stimulant medication…, despite its well-documented acute effects on ADHD symptoms and impairment, has failed to demonstrate protective effects against substance use and disorder, as it has failed to demonstrate beneficial long-term effects in all of the key domains that mediate the development of SUD.”
(Molina & Pelham Jr, 2014) (pg. 629).
It is critical to understand the reasons that many young adults with ADHD who experience multiple risks do not develop SU problems; this may suggest unidentified resiliency and new pathways for intervention. For YAs with emotional or behavioral difficulties and delinquency histories, early achievement of stable, rewarding employment has been found to predict long-term successful adjustment (Sampson & Laub, 2003) including reduction in SUD; this factor could serve a similar role in young adults with ADHD, who, in general, have frequent job changes and underemployment (Barkley, Murphy, & Fischer, 2010; Weiss & Hechtman, 1993). Assuming family responsibilities, or changing beliefs about whether they still “have” ADHD in adulthood, also may shift SUD trajectories for some YAs.
The developmental stage of young adulthood (21–25 years), or “emerging adulthood” is precisely the period during which individuals confront a number of challenges, such as completing academic or vocational training, obtaining rewarding employment, family formation and residential changes, and developing independent living skills and resources. This is also a high-risk age for SU, which can have a substantial negative life impact for those who abuse or become dependent (Schulenberg, Sameroff, & Cicchetti, 2004).
In this report we describe the design, sample and methods for a qualitative-interview study of a subsample of YAs who participated in the larger MTA (which relied on traditional survey, interview, and paper-and-pencil measures) beginning at ages 7–9. The MTA sample is especially valuable because of its size and quantitative SU and diagnostic data across a 14–16 year time period. There are two sources for quantitative evidence in this report: (a) the ‘standard’ MTA assessments of SU, and ADHD medication use from the longitudinal study, and (b) the quantitative data yielded from the ordinal scale coding of the qualitative interviews. The qualitative data are narrative text excerpts from the interview. We describe (a) the sample; (b) the interview design and format; (c) interview administration; (d) topics covered and coding procedures; (e) description of MTA drug use and ADHD medication; (f) reliability of coding of interview excerpts; and (g) and analysis of SU beliefs comparing ADHD and a Local Normative Comparison Group (LNCG).
Methods
Sample Selection
Participants in the present study were from the longitudinal follow-up of the MTA. Children with ADHD (N = 579) received a diagnosis of ADHD, Combined Type at study entry when they were 7.0–9.9 years old (grades 1–4) (Group, 1999a). Children were randomly assigned to one of four treatment groups: Medication Only (MedMgt), Behavioral Treatment Only (Beh), Combined Treatment (Comb), or Community-treated Comparison (CC). Study treatments are described in Wells et al. (2000), Greenhill et al. (1996), and the MTA Cooperative Group (1999b). Participants were assessed at completion of the 14-month treatment phase, at 24 and 36 months, and again at 6, 8, 10, 12, 14, and 16 years after randomization. The LNCG (N = 289) was recruited at the 24-month point from the same schools attended by the children with ADHD, selected not for ADHD but for demographic similarity (Molina et al., 2007). By the 16 year follow-up, MTA sample retention was 76% (72% of ADHD, 84% of LNCG); 81% of the MTA sample participated five or more times between the 24 month and 16 year follow-up assessments: 76% (441/579) of ADHD participants and 91% (264/289) of LNCG participants.
Participants in the Qualitative Interview Study
One hundred eighty-three participants from the ADHD and LNCG groups were recruited. To minimize subject burden and interview contamination, qualitative interviews were conducted either 1) more than two months before the 14 or 16 year assessment, or 2) more than two weeks after the 14- or 16-year assessment.
Recruitment aimed to fill four cells in a 2 (ADHD versus LNCG) × 2 (persistent substance user versus abstainer/experimenter) unbalanced design with the intention of oversampling participants with an ADHD history as well as participants with persistent SU into early adulthood. Participants were from four of the original seven MTA sites: University of California, Irvine (n = 53), Duke University Medical Center (n = 52), University of California, Berkeley (n = 52), and Montreal Children’s Hospital (n = 26). A total of 58 persistent substance users participated. The remaining ADHD participants were randomly selected from those not identified as persistent substance users, stratified by original treatment group assignment. The remaining LNCG participants were randomly selected from the available pool of participants not identified as persistent substance users. Only five potential qualitative interview study participants declined participation. Table 1 summarizes sex and race/ethnicity for ADHD and LNCG. The two samples are similar demographically.
Table 1.
MTA Qualitative Study sample demographics
| ADHD (n = 125) | LNCG* (n = 58) | Test statistic | p | |
|---|---|---|---|---|
| Age | 24.40 (1.18) | 23.74 (0.95) | t(181) = 3.75 | <.001 |
| Sex | ||||
| Male | 95 (76%) | 45 (77%) | χ2(1) = 0.06 | .81 |
| Female | 30 (24%) | 13(23%) | ||
| Race/ethnicity | χ2(5) = 5.00 | .42 | ||
| White | 90 (72%) | 49 (85%) | ||
| African-American | 12 (10%) | 2 (3%) | ||
| Asian | 1 (1%) | 1 (2%) | ||
| Mixed | 15 (12%) | 3 (5%) | ||
| Non-Black Hispanic | 5 (4%) | 2 (3%) | ||
| Other | 2 (2%) | 1 (2%) | ||
| Site (%) | ||||
| Berkeley | 36 (29%) | 16 (28%) | χ2(3) = 0.18 | .98 |
| Duke | 36 (29%) | 16 (28%) | ||
| Irvine | 35 (28%) | 18 (31%) | ||
| Montreal** | 18 (14%) | 8 (14%) | ||
LNCG = Local Normative Comparison Group sample
Note: Montreal’s N reflects their original sample, half the size of most MTA sites.
Persistent Drug Use and Use of ADHD Medication Scores
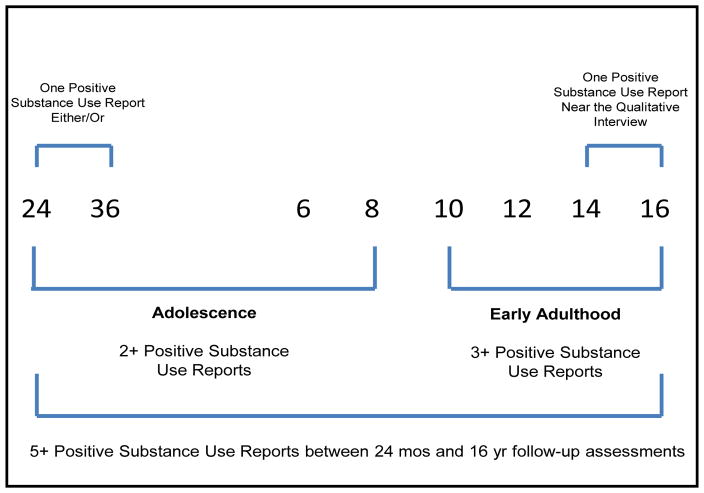
Persistent substance users were identified for the qualitative interview study by their positive SU self-report for any non-tobacco substance exceeding designated thresholds at five or more assessments between 24 months and 16 years. Use of alcohol, marijuana, other illicit drugs (e.g., cocaine), and misuse of prescription drugs was measured at these assessments with the Substance Use Questionnaire (SUQ) (Molina & Pelham Jr, 2003). Two of the five positive reports were required to occur in adolescence (between the 24-month and 8-year follow-ups) and three were required in adulthood (between 10 and 16 years) (Figure 1). Because of infrequently reported SU at the 24 and 36 month visits when the children were between the ages of 9 and 14 (Molina et al., 2007), report of SU at either or both of the 24 and 36 month assessments was counted as one positive report.
Figure 1.
Timeline of MTA follow-up assessments and substance use criteria for selection into qualitative interview study.’
Each positive SU report was based on developmentally specific thresholds selected for each type of substance and developmental period. These thresholds were chosen to reflect the well-established prognostic importance of early onset and the well-established escalation that occurs between childhood and adulthood (Chassin, Colder, Hussong, & Sher, 2015; Windle et al., 2008). For example, it has long been known that drinking more than a sip of alcohol before age ~15 is associated with later alcohol-related problems (Grant & Dawson, 1997; Odgers et al., 2008). However, because the majority of adolescents have consumed alcohol by high school graduation, a higher threshold of alcohol frequency is required to capture atypical drinking at older ages (coded as at least monthly alcohol use during the past six months). Given that SU peaks in early adulthood ((SAMHSA), 2012), weekly SU (e.g., weekly binge drinking or drunkenness, weekly marijuana use, etc.) was required for a positive SU report at the 12–16 year assessments. Thus, our developmentally specific thresholds for positive SU reports were the following: any SU by early adolescence, monthly SU in mid-to-late adolescence, and weekly SU in adulthood.
Substance Use Questionnaire (SUQ)
The SUQ (Molina & Pelham Jr, 2003) adapted for the MTA (Molina et al., 2007; Molina et al., 2013) includes questions about alcohol, tobacco, marijuana, other illicit drugs (e.g., cocaine), and misuse of prescription drugs. Items address lifetime use (e.g., “Have you ever had a drink of beer, wine, wine cooler, or liquor—not just a sip or a taste of someone else’s drink?), age of initial use (e.g., “How old were you the first time….”) and past six months frequency/quantity (e.g., “During the past 6 months, how often did you drink beer, wine, wine coolers, or liquor?” and “In the past 6 months, how many times did you drink five or more drinks?”). Response options for frequency items were typical of SU measures in longitudinal studies (e.g., 1=“Never” to 9=“More than twice a week”). The SUQ was modeled after similar SU measures in longitudinal or national survey studies of alcohol and other drug use that also rely on confidential self-report (Donovan, 1994; Jessor, Donovan, & Costa, 1989; National Household Survey on Drug Abuse, 1992; Winters & Fahnhorst, 2005).
Medication Use
The Services for Children and Adolescents-Parent Interview (SCAPI) obtained a detailed caregiver account of psychotropic medications through the 10-year assessment; after that medication use was collected from the Health Information Questionnaire self-report (Jensen et al., 2004). These data were used to estimate daily dose (in mg equivalents of methylphenidate) of stimulant medication and number of days treated between assessments, as well as cumulative total dose. An operational definition of adequate treatment developed by MTA investigators was medication on more than 50% of days since the prior assessment).
Interview Methods, Design and Format
Investigators developed a qualitative interview based on the Ecocultural Family Interview (EFI) (Duncan, Huston, & Weisner, 2007; T.S. Weisner, 2002; T. S. Weisner, 2011; T.S. Weisner, 2011; Thomas S Weisner & Fiese, 2011), a guided conversation with prompts. Topics are based on theory and on the particular focus of the study (in this study, ADHD, SU, life Turning Points and related topics). The EFI is a conversational interview, not a questionnaire or question-response survey using a Likert or yes-no question format. Following general guiding questions, the words, concepts, accounts, explanations, and narratives come from the participants. The explanations and accounts regarding, for example, SU or young adults’ turning points understandings of ADHD, are provided by the participants, not selected from a prepared checklist. Respondents are encouraged to “tell their story” about their lives and each topic (Table 2). The interview includes open-ended questions about SU, key transitions and life changes, and experiences regarding ADHD, medication and SU.
Table 2.
Interview Template: Topics Discussed and Prompts for Young Adult Ecocultural Family Interviews
| Topics Discussed | Sample Interviewer Prompts |
|---|---|
| General Overview | What’s going on in (school, family, work, or living situation) these days? Walk me through an average day for you. How satisfied are you with how things are going in life right now? What are things that are stressing you out these days? |
| Perceptions about the MTA Study and ADHD (if relevant) | What do you remember about being in the MTA study? What would you want the MTA team to know? What does “having ADHD” mean to you? How do you manage your ADHD? Was ADHD medication a good idea for you? (if relevant) What makes you similar and different from others (e.g., emotionally)? |
| Substance Use | Over your whole life, what kinds of illegal and legal drugs have you tried? How did things seem to start with (insert substance)? Is there a certain substance you like best? Why do you think that is? How did your use change, or not change, over time? In what ways, if any, did your use of an ADHD medication impact your use of (insert substance)? |
| Work | Can you describe your current job? What would you change about your work situation if you could? What kinds of difficulties are going on at work? |
| Future Plans/Goals | What are your hopes for the future (e.g., personal, work, family, friends, romantic relationships)? What are your fears about the future? What would you like to accomplish? What are your expectations about what might actually happen? |
| Family | Who are you closest to in your family? How have relationships changed as you’ve grown up? Has anyone had a big influence on you? Who are your role models? |
| Peers | Outside of family, do you have people you can really count on? Tell about your romantic relationships. What would you change about your social life if you could? |
| School | Is there anything you’d do differently as you progressed through school? What was your parent’s role in your schooling (now and in the past)? What advice would you give to teachers now if you could go back and talk to them? |
| Turning Points | What kinds of people/experiences really influenced you or your direction in life? Without this turning point, how would things be different for you? What situations or turning points would you really not want to change? Who/what are the greatest influences on you today? |
| Self-Knowledge and Identity | How would you describe yourself now compared to 4 to 5 years ago? What are some strengths and weaknesses you see in yourself? Thinking about ADHD, in what ways is that a part of you? Do you see yourself as a role model for any one or in any way? |
| Conclusion | What have we missed that’s important to you? What would you say to the leaders of this project about what’s important to you? What should we include in future interviews and make sure to discuss? |
The interview was piloted and refined with 16 young adults and their parents (not part of the study sample) (Murray, 2010). The team then designed a semi-structured script or template (the topics in Table 2) that was used to prompt MTA YAs throughout the interview.
Ecocultural Family Interview Administration
Following extensive training, Master’s-level, doctoral, or post-doctoral interviewers completed EFI interviews. To insure coverage of all intended domains, every topic was addressed with prompts as needed. YAs were assured that no information from their interview would be shared with other family members. IRB approvals and an NIH Certificate of Confidentiality strengthened the assurance of privacy. Interviews lasted 50 to 120+ minutes; most were 1.5 – 2 hours.
Interview Transcript Indexing and Coding
EFI interviews were digitally recorded, transcribed, and entered into the software system, Dedoose (Lieber & Weisner, 2010). Our initial reviews of the text, consultations with interviewers, consideration of the literature, and our clinical experience guided our iterative selection of topics to be coded. Seventeen main topics were coded: Substance Use, Possible Protective/Risk Factors; Stressors; Current Social Supports; Early Support and Stressors; Positive Social Involvement of Youth; Self-Knowledge and Goals; ADHD Effects and Perceptions; Memories of Prior Participation in MTA; Life Turning Points; School; Work; Future Plans; Parenting Memories; Relationships With Families and Friends; and Mentions of Emotional Functioning. Interview excerpts (a sentence, several sentences, up to a paragraph in which the content of the narrative is on that topic) were indexed (tagging of text by topics; e.g., marking excerpts in which reasons for SU desistance are discussed) and coded (on an ordinal scale from 0=unimportant to 8=very important). The ratings typically measure the perceived importance, extent, or severity of an item, e.g., importance of seeing the consequences of SU for others in sustaining desistance from SU.
Results
Rating and Coding Reliability
Lead rating coordinators at each site, along with the UCLA team leaders, did indexing, and established initial coding reliability. Interview excerpts across the sample, across sites, and across all topics were randomly selected for estimating reliability of coding. Other interviewer/raters coded these excerpts, which were then compared to lead rater scores. Raters were blind to scores of other raters and to sites from which excerpts came. All the individual topics and subtopics in Table 3 (nine coded SU topics) had Kappa coefficients >.70 and averaged .80.
Table 3.
Mean differences between ADHD and LNCG Youth for Nine Substance Use Topics
| ADHD Subjects | LNCG Subjects1 | Significance | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Substance Use - Nine Coded Topics | Number of Respondents Mentioning Topic (out of 125) | Average Number of Responses per person | Average score coded for this topic ( 0 – 8) | Median number of Responses | SD of number of coded Responses per person | Number of Respondents Mentioning Topic (out of 58) | Average Number of Responses per person | Average score coded for this topic (0 – 8) | Median number of Responses | SD of number of coded Responses per person | T- test Statistic | Degrees of Freedom | P Value |
| Relationship between emotional functioning and substance use initiation or maintenance. | 75 | 6.49 | 2.83 | 3 | 1.78 | 28 | 5.25 | 3.29 | 3 | 1.77 | −1.18 | 48.85 | 0.244 |
| Extent to which negative experience impacted substance use | 84 | 3.58 | 3.93 | 4 | 1.70 | 35 | 4.94 | 4.02 | 4 | 1.92 | −0.26 | 57.38 | 0.796 |
| YA’s opportunities for substance use | 106 | 4.65 | 5.15 | 5 | 0.69 | 49 | 5.51 | 5.01 | 5 | 1.07 | 0.84 | 67.08 | 0.405 |
| Extent of connection made between ADHD drugs and use of other substances (e.g. substituted for adhd drugs; led to other use; led to abstention; dual use) | 107 | 1.68 | 2.64 | 2 | 2.42 | -- | -- | -- | -- | -- | --2 | -- | -- |
| Extent to which people in his/her family influenced/impacted use/non-use. | 108 | 2.93 | 4.44 | 5 | 1.70 | 52 | 2.94 | 4.31 | 4 | 1.67 | 0.45 | 102.83 | 0.650 |
| Extent to which young adult perceives substance use as a negative experience | 110 | 5.19 | 3.83 | 4 | 1.59 | 50 | 5.56 | 3.79 | 4 | 1.34 | 0.17 | 111.15 | 0.867 |
| Extent to which seeing others go “down wrong path” influenced decisions about substance use | 65 | 1.89 | 4.99 | 5 | 1.95 | 35 | 1.86 | 3.85 | 4 | 1.88 | 2.86 | 72.09 | 0.006 |
| Extent to which substance use has a positive impact in other ways | 93 | 3.84 | 3.42 | 3 | 1.60 | 40 | 4.88 | 3.13 | 3 | 1.56 | 0.96 | 75.69 | 0.340 |
| Extent to which substance use has a positive impact on ADHD symptoms | 73 | 2.00 | 3.34 | 4 | 2.26 | -- | -- | -- | -- | -- | --2 | -- | -- |
LNCG = Local Normative Comparison Group
For the two topics out of nine that refer to how ADHD influences SU (“Extent of connection made between ADHD drugs and use of other substances (e.g. substituted for ADHD drugs; led to other use; led to abstention; dual use)”, and “Extent to which substance use has a positive impact on ADHD symptoms”) there is no meaningful t-test comparison to the LNCG sample.
Frequency of Substance Use Topics and Codes
SU topics were extensively discussed in the interviews, totaling 3566 interview excerpts. One hundred eighty of 183 YAs had at least one such excerpt, averaging 19 excerpts/YA covering all SU topics coded. Nine SU topics were identified and coded (Table 3 column 1). For example (row 7 of Table 3), “Extent to which seeing others ‘go down wrong path’ influenced decisions about substance use” was described as a reason for desistance by 100/183 YAs (55%) (65/125 (52%) ADHD and 35/58 (60%) LNCG participants). Table 3 also shows the average number of responses and standard deviation for those who had at least one coded interview excerpt. YAs who talked about each SU topic typically offered 2 – 5 distinct codable excerpts.
ADHD vs. LNCG Group Differences Across Topics
ADHD youth were more likely to feel strongly that when they saw others going down the wrong path, this was more likely to have influenced them to desist from SU (t=2.86, p=0.006). No other coded excerpts (six of seven tests in Table 3) were significantly different comparing ADHD and LNCG Ss.
Connections between ADHD medication use and SU: Narrative data
ADHD Medication and SU
Many participants commented that ADHD medication use, never influenced their SU. Instead, they said that seeing peers with difficulties, their own choices, and other turning points in their lives influenced SU. These comments extend and support the quantitative finding that YA in the ADHD group saw others going down wrong paths and this led them to less SU, but the other influences were described similarly by ADHD and LNCG YAs. Many said that generalizations about SU and ADHD are difficult, since “everybody’s different” and everyone’s situations are different. Some said that medication affected them not through the direct effect of ADHD medication per se, but rather through feeling marked or labeled because of their ADHD diagnosis, as being “a person who needed to be medicated”. One woman who felt this way commented that “…It’s who people are, not medication or ADHD itself. You make your own decisions”. Another saw a connection, but not due to any effects of the ADHD medications, rather due to the “messages” she got from her parents and doctors implying her needing to be medicated, to the perception of themselves as a person who “needed to be medicated”, which made her want to fit in to a group of peers doing drugs. “…Yeah. I guess I never really felt like I fit in, so I think drugs kinda helped me to feel like I was fitting into a group - the druggie group”.
Other YAs commented that there was a connection between taking medication and having ADHD – but that this experience does not lead to SU: “…dealing with ADHD is hard enough; so why take drugs and have to deal with drugs too?”, as one YA said. Others argued that ADHD medication is a protective factor against SU because they just “hated taking any pills”.
“… you know what? I think it [ADHD meds] was the protective factor. I hate taking pills, and I was so terrible [about taking pills]. I would sneak around to [not] take my medicine. I would stick the pill in the side of the vent on the water fountain to keep from taking it. I was that bad. I hate taking medicine. I hate taking pills, so when I was approached by people, to take SU or whatever, there’s not even a second thought. I remember first time I ever went to a rock ‘n’ roll show, and one of the guys in one of the bands was trying to get me to take Ecstasy, and I was like -- “I hate taking pills. You can count me out.”
Others said the ADHD-SU connection was there but only in regard to the choice of which drugs to take, not about overall likelihood of SU, which would have happened anyway. Some viewed medication as a “good excuse” for SU: “why wouldn’t I then try anything [since I am taking Adderall anyway]?” On the other hand, another YA said Adderall does not count as a real drug because it does not “do” anything to you, while other drugs get you high, so for him, it did not influence SU.
“I don’t use my ADHD medication to get high or I don’t use my ADHD medication to feel all woozy or feel all cracked out…I don’t like that feeling.”
Reasons for a connection between medication use and SU
However, twenty participants (16%) in the ADHD sample did experience medication use as a risk for using other drugs. One YA commented that ADHD medication was an influence on him. “I’m surprised I’m not on more drugs, to be honest”. One recurring theme focuses on the recollection of just getting “used to the feeling” of doing drugs as a child. One YA wanted to counter “feeling like a drone” on ADHD meds by using other substances to feel good.
“ I think my personal opinion is pretty much if [you are] on drugs from a young age and they’re used to that feeling, after a while they want to find out – they want to pretty much feel normal. They don’t want to feel like a drone anymore so they’ll try pretty much anything to pretty much get a high, feel good or something. So maybe it will [increase] the chance of drug use down the road.
Some of these YAs said that ADHD diagnosis and medication use can just “provide me with an excuse” to do other substances.
“… as far as I’m concerned, saying something like that [that taking Adderall and having ADHD, leads to SU] [is like saying that] living with something like that is how addicts say they got a disease: ‘It’s not my fault, because I got a disease.’ I got ADHD real bad and they fed me full of amine compound and now I’m smoking meth, that’s my, you know, it’s an excuse.”
Fit with work life after high school; little or no connection with medication use
A number of YA described searching for work which fit their behavioral, cognitive, and emotional tendencies (work with their hands, active work such as in restaurants, work that kept them busy and therefore focused, work they cared about). Improved fit led to less of a need for drugs, or medication, or perhaps only limited drug use at occasional periods. One YA commented that
“I would say that there’s no relationship [between using or not using ADHD prescription medications, and SU]. You’re going to do what you’re going to do, whether you’re on medicine or not. I’ve been on both sides, I’ve taken the [ADHD] medicine, I’ve not taken the medicine [in the past]. And to me, it was kind of like, oh, I started [using substances] when I took the medicine, and I’m still [using] after the medicine. So the medicine didn’t affect me either way, it don’t bring me down from it or make me do SU any more [than I was going to use anyway].”
Discussion
There were a wide range of beliefs regarding connections between SU, medication use, and ADHD symptoms, and many were novel and certainly not straightforward. These accounts included narratives about the importance of personal choice and responsibility, beliefs that individuals are so different and contexts so different that there is no pattern in these connections, beliefs that there is a kind of inevitability that SU will be a part of who they are as someone with ADHD, and the belief that ADHD can be used as a kind of “excuse” for SU. Other YAs experienced ADHD as being a marker for difference earlier in life, then leading to SU rather than the medications themselves being a gateway to SU. Some classified medications for ADHD being different from “party” drugs (since party drugs actually “do something” for example), so there are not connections between using the medications and SU, as well as the belief that only when there is concurrent use of medications along with other drugs would there be a “connection” between them, and finally the belief that SU is unconnected to ADHD medication because it’s already hard enough having ADHD, much less to add the hardships of drug use.
The qualitative narrative accounts expand the findings from quantitative measures by discovering some of the diverse ideas and explanatory models and beliefs of the YA themselves. Many young adults with ADHD who experience multiple risks do not develop problems with substance abuse or dependence, and their accounts suggest a number of shared beliefs associated with desistance, unidentified resiliency and new pathways for intervention. Further analyses of systematically selected cases looking across turning points, demographics, work and school experiences, romantic relationships, and their connections to SU will add value going forward to connect these ideas to other aspects of YA lives. Framing messages regarding SUD using the kinds of everyday perceptions and accounts in these YA narratives could improve interventions.
Clinical Implications
Our overall results indicate that the explanations given by individuals with ADHD for their SU decisions (initiating, persisting, desisting) generally do not differ from individuals without ADHD (leaving aside questions about medications or stigma and SU that were specific to the ADHD sample), nor are there consistent or strong relationships between previously prescribed stimulant medication and subsequent SU. Individuals with and without ADHD do note the strong importance and negative impact of the ready availability of illicit substances, the overall negative impact of SU experiences on themselves, as well as the positive impact of family members on their SU decisions.
However, the beliefs about connections among ADHD, medication, and SU actually differ widely; beliefs that there were straightforward direct connections were not typical. YAs have a complex belief system regarding what drugs are, as well as what ADHD in the past and now are, and such knowledge can lead to more effective intervention. Clinicians working with substance-abusing YA might use this knowledge to heighten their patients’ determination to abstain or desist from SU. More specifically to individuals with ADHD, our findings suggest that they may attribute greater importance to “seeing others go down the wrong path” than individuals without ADHD. Such findings, if replicated, might also be used during therapy to increase their motivation to abstain or desist from SU.
Acknowledgments
This study was supported by the National Institute on Drug Abuse (NIDA) to the following: Duke University: N01DA-8-5554, University of California, Berkeley: N01DA-8-5550, and University of California, Irvine: N01DA-8-551. Additional funding support provided by NIDA (K23DA032577 to J.T.M.). The Multimodal Treatment Study of Children with ADHD (MTA) was a National Institute of Mental Health (NIMH) cooperative agreement randomized clinical trial, continued under an NIMH contract as a follow-up study and finally under a National Institute on Drug Abuse (NIDA) contract. Collaborators from NIMH: Benedetto Vitiello, M.D. (Child & Adolescent Treatment and Preventive Interventions Research Branch), Joanne B. Severe, M.S. (Clinical Trials Operations and Biostatistics Unit, Division of Services and Intervention Research), Peter S. Jensen, M.D. (currently at the REACH Institute and the University of Arkansas of Medical Sciences), L. Eugene Arnold, M.D., M.Ed. (currently at Ohio State University), Kimberly Hoagwood, Ph.D. (currently at New York University); previous contributors from NIMH to the early phases: John Richters, Ph.D. (currently at National Institute of Nursing Research); Donald Vereen, M.D. (currently at NIDA). Principal investigators and co-investigators from the sites are: University of California, Berkeley/San Francisco: Stephen P. Hinshaw, Ph.D. (Berkeley), Glen R. Elliott, Ph.D., M.D. (San Francisco); Duke University: Karen C. Wells, Ph.D., Jeffery N. Epstein, Ph.D. (currently at Cincinnati Children’s Hospital Medical Center), Desiree Murray, Ph.D.; previous Duke contributors to early phases: C. Keith Conners, Ph.D. (former PI); John March, M.D., M.P.H.; University of California, Irvine: James Swanson, Ph.D., Timothy Wigal, Ph.D.; previous contributor from UCLA to the early phases: Dennis P. Cantwell, M.D. (deceased); New York University: Howard B. Abikoff, Ph.D.; Montreal Children’s Hospital/McGill University: Lily Hechtman, M.D.; New York State Psychiatric Institute/Columbia University/Mount Sinai Medical Center: Laurence L. Greenhill, M.D. (Columbia), Jeffrey H. Newcorn, M.D. (Mount Sinai School of Medicine). University of Pittsburgh: Brooke Molina, Ph.D., Betsy Hoza, Ph.D. (currently at University of Vermont), William E. Pelham, Ph.D. (PI for early phases, currently at Florida International University). Follow-up phase statistical collaborators: Robert D. Gibbons, Ph.D. (University of Illinois, Chicago); Sue Marcus, Ph.D. (Mt. Sinai College of Medicine); Kwan Hur, Ph.D. (University of Illinois, Chicago). Original study statistical and design consultant: Helena C. Kraemer, Ph.D. (Stanford University). Collaborator from the Office of Special Education Programs/US Department of Education: Thomas Hanley, Ed.D. Collaborator from Office of Juvenile Justice and Delinquency Prevention/Department of Justice: Karen Stern, Ph.D. Additional investigators involved in Qualitative Interview Sub-study: Thomas S. Weisner, Ph.D., Carol Fox Adams, Ph.D, Page Sorensen, M.A., & Jeffrey Good, Ph.D., UCLA.
Funding
The work reported was supported by cooperative agreement grants and contracts from the National Institute of Mental Health (NIMH) and the National Institute on Drug Abuse (NIDA) to the following: University of California–Berkeley: U01MH50461, N01MH12009, N01DA-8-5550; Duke University: U01MH50477, N01MH12012, N01DA-8-5554; University of California, Irvine: U01MH50440, N01MH12011, N01DA-8-5551; University of Pittsburgh: U01 MH50467, N01MH 12010, N01DA-8-5553; McGill University N01MH12008, N01DA-8-5548. Additional funding support provided by NIDA (K23DA032577) to J.T.M. The opinions and assertions contained in this report are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Health and Human Services, the National Institutes of Health or the National Institute of Mental Health.
Footnotes
Declaration of Interests
In the past 2 years: Dr. Jensen receives royalties from several publishing companies: Random House, Oxford, and APPI, Inc. He also is a part owner of a consulting company, CATCH Services, LLC. He is the CEO/President of a non-profit organization, the REACH Institute, but receives no compensation. Dr. Arnold has received research funding from Curemark, Forest, Lilly, Neuropharm, Novartis, Noven, Shire, and YoungLiving (as well as NIH and Autism Speaks) and has consulted with or been on advisory boards for Arbor, Gowlings, Neuropharm, Novartis, Noven, Organon, Otsuka, Pfizer, Roche, Seaside Therapeutics, Sigma Tau, Shire, Tris Pharma, and Waypoint and received travel support from Noven; Dr. Hechtman has received research funding, served on the advisory boards and has been speaker for Ely Lilly, GlaxoSmithKline, Ortho Janssen, Purdue, and Shire; and Dr. Wells receives royalty income from Multi-Health Systems. None of the other authors have any additional declarations.
Contributor Information
Dr. Thomas S. Weisner, Departments of Psychiatry & Anthropology, UCLA
Dr. Desiree W. Murray, Department of Psychiatry & Behavioral Sciences, Duke University Medical Center, Durham, NC, USA
Dr. Peter S. Jensen, Department of Psychiatry, University of Arkansas for Medical Sciences, Little Rock, AR, USA and the Reach Institute, New York, NY, USA
Dr. John T. Mitchell, Department of Psychiatry & Behavioral Sciences, Duke University Medical Center, Durham, NC, USA
Dr. James M. Swanson, School of Medicine, University of California, Irvine, CA, USA
Dr Stephen P. Hinshaw, Department of Psychology, University of California, Berkeley, CA, USA and the University of California, San Francisco, CA, USA
Dr. Karen Wells, Department of Psychiatry & Behavioral Sciences, Duke University Medical Center, Durham, NC, USA
Dr. Lily Hechtman, Division of Child Psychiatry, McGill University, Montreal Children’s Hospital, Montreal, Quebec, Canada
Dr. Brooke S. G. Molina, Departments of Psychiatry and Psychology, University of Pittsburgh, Pittsburgh, PA, USA
Dr. L. Eugene Arnold, Department of Psychiatry, Ohio State University, Columbus, OH, USA
Ms. Page Sorensen, Departments of Psychiatry & Anthropology, UCLA
References
- (SAMHSA), M. H. S. A. Mental Health Services Administration (SAMHSA)(2012) Results from the 2011 National Survey on drug use and health: summary of national findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2012. [Google Scholar]
- Barkley RA, Murphy KR, Fischer M. ADHD in adults: What the science says. Guilford Press; 2010. [Google Scholar]
- Capps L, Ochs E. Constructing Panic. The Discourse of Agoraphobia. Cambridge: Harvard University Press; 1995. [Google Scholar]
- Chassin L, Colder CR, Hussong A, Sher KJ. Substance use and substance use disorders. Developmental psychopathology 2015 [Google Scholar]
- Donovan J. The Teen Drinking Questionnaire. Pittsburgh: Pittsburgh Adolescent Alcohol Research Center, University of Pittsburgh; 1994. [Google Scholar]
- Duncan G, Huston A, Weisner T. Higher Ground: New Hope for working families and their children. New York: Russell Sage Foundation; 2007. [Google Scholar]
- Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: results from the National Longitudinal Alcohol Epidemiologic Survey. Journal of substance abuse. 1997;9:103–110. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Greenhill LL, Abikoff HB, Arnold LE, Cantwell DP, Conners CK, Elliott G, … Jensen PS. Medication treatment strategies in the MTA study: relevance to clinicians and researchers. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35(10):1304–1313. doi: 10.1097/00004583-199610000-00017. [DOI] [PubMed] [Google Scholar]
- Group MC. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Archives of general psychiatry. 1999a;56(12):1073. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- Group MC. Moderators and mediators of treatment response for children with attention-deficit/hyperactivity disorder: the Multimodal Treatment Study of children with Attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 1999b;56(12):1088. doi: 10.1001/archpsyc.56.12.1088. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Eaton Hoagwood K, Roper M, Arnold LE, Odbert C, Crowe M, … Hoza B. The services for children and adolescents–parent interview: Development and performance characteristics. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(11):1334–1344. doi: 10.1097/01.chi.0000139557.16830.4e. [DOI] [PubMed] [Google Scholar]
- Jessor R, Donovan J, Costa F. Health Behavrior Questionnaire. Boulder, CO: Institute of Behavioral Science, University of Colorado; 1989. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG. National Survey Results on Drug Use from the Monitoring the Future Study, 1975–1998. Volume II: College Students and Young Adults. ERIC; 1999. [Google Scholar]
- Kleinman A. The Illness Narratives: Suffering, Healing, and the Human Condition. New York: Basic Books; 1988. [Google Scholar]
- Lieber E, Weisner TS. Meeting the practical challenges of mixed methods research. In: Tashakkori A, Teddlie C, editors. Handbook of Mixed Methods Research. Thousand Oaks, CA: Sage; 2010. pp. 559–579. [Google Scholar]
- Martin E. Bipolar expeditions: Mania and depression in American culture. Princeton University Press; 2007. [Google Scholar]
- Masten AS, Faden VB, Zucker RA, Spear LP. Underage drinking: A developmental framework. Pediatrics. 2008;121(Supplement 4):S235–S251. doi: 10.1542/peds.2007-2243A. [DOI] [PubMed] [Google Scholar]
- Molina BS, Flory K, Hinshaw SP, Greiner AR, Arnold LE, Swanson JM, … Hoza B. Delinquent behavior and emerging substance use in the MTA at 36 months: prevalence, course, and treatment effects. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(8):1028–1040. doi: 10.1097/chi.0b013e3180686d96. [DOI] [PubMed] [Google Scholar]
- Molina BS, Hinshaw SP, Arnold LE, Swanson JM, Pelham WE, Hechtman L, … Abikoff HB. Adolescent substance use in the multimodal treatment study of attention-deficit/hyperactivity disorder (ADHD)(MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(3):250–263. doi: 10.1016/j.jaac.2012.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BS, Pelham WE., Jr Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. Journal of abnormal psychology. 2003;112(3):497. doi: 10.1037/0021-843x.112.3.497. [DOI] [PubMed] [Google Scholar]
- Molina BS, Pelham WE., Jr Attention-Deficit/Hyperactivity Disorder and Risk of Substance Use Disorder: Developmental Considerations, Potential Pathways, and Opportunities for Research. Annual review of clinical psychology. 2014;10:607–639. doi: 10.1146/annurev-clinpsy-032813-153722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray DW. Mining the Meanings of ADHD, Treatment, and Substance Use/Abuse: The MTA Turning Points Study. Paper presented at the 57th Annual Meeting; October 26–31, 2010.2010. [Google Scholar]
- National Household Survey on Drug Abuse. Washington DC: 1992. [Google Scholar]
- Ochs E, Capps L. Narrating the Self. Annual Review of Anthropology. 1996;25:19–43. [Google Scholar]
- Odgers CL, Caspi A, Nagin DS, Piquero AR, Slutske WS, Milne BJ, … Moffitt TE. Is it important to prevent early exposure to drugs and alcohol among adolescents? Psychological Science. 2008;19(10):1037–1044. doi: 10.1111/j.1467-9280.2008.02196.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ, Laub JH. Life - Course Desisters? Trajectories Of Crime Among Delinquent Boys Followed To Age 70*. Criminology. 2003;41(3):555–592. [Google Scholar]
- Schulenberg JE, Sameroff AJ, Cicchetti D. The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Development and psychopathology. 2004;16(04):799–806. doi: 10.1017/s0954579404040015. [DOI] [PubMed] [Google Scholar]
- Weisner TS. Ecocultural understanding of children’s developmental pathways. Human Development. 2002;45(4):275–281. [Google Scholar]
- Weisner TS. The ecocultural family interview: New conceptualizations and uses for the study of illness. In: Bonichini S, Baroni MR, editors. Sviluppo e salute del bambino: Fattori individuali, sociali e culturali (In ricordo di Vanna Axia) Padova, Italia: Libraria Editrice Universitaria di Padova; 2011. pp. 166–173. [Google Scholar]
- Weisner TS. “If you work in this country you should not be poor, and your kids should be doing better”: Bringing mixed methods and theory in psychological anthropology to improve research in policy and practice. Ethos. 2011;39(4):455–476. [Google Scholar]
- Weisner TS. Why qualitative and ethnographic methods are essential for understanding family life. In: McHale SM, Amato P, Booth A, editors. Emerging Methods in Family Research. Springer; 2014. [Google Scholar]
- Weisner TS, Duncan G. The world isn’t linear or additive or decontextualized: Pluralism and mixed methods in understanding the effects of anti-poverty programs on children and parenting. In: Gershoff Mistry, Crosby, editors. Societal contexts of child development: Pathways of influence and implications for practice and policy. New York: Oxford University Press; 2014. [Google Scholar]
- Weisner TS, Fiese BH. Introduction to special section of the Journal of Family Psychology, advances in mixed methods in family psychology: integrative and applied solutions for family science. Journal of Family Psychology. 2011;25(6):795. doi: 10.1037/a0026203. [DOI] [PubMed] [Google Scholar]
- Weiss G, Hechtman LT. Hyperactive children grown up: ADHD in children, adolescents, and adults. Guilford Press; 1993. [Google Scholar]
- Wells KC, Pelham WE, Jr, Kotkin RA, Hoza B, Abikoff HB, Abramowitz A, … Del Carmen R. Psychosocial treatment strategies in the MTA study: rationale, methods, and critical issues in design and implementation. Journal of Abnormal Child Psychology. 2000;28(6):483–505. doi: 10.1023/a:1005174913412. [DOI] [PubMed] [Google Scholar]
- Whybrow PC. American mania: When more is not enough. WW Norton; 2006. [Google Scholar]
- Windle M, Spear LP, Fuligni AJ, Angold A, Brown JD, Pine D, … Dahl RE. Transitions into underage and problem drinking: developmental processes and mechanisms between 10 and 15 years of age. Pediatrics. 2008;121(Supplement 4):S273–S289. doi: 10.1542/peds.2007-2243C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters KC, Fahnhorst T. Recent Developments in Alcoholism. Springer; 2005. Assessment issues in adolescent drug abuse treatment research; pp. 407–425. [DOI] [PubMed] [Google Scholar]