Abstract
Background
Patient navigation is an evidence-based intervention involving trained healthcare workers who assist patients in assessing and mitigating personal and environmental factors to promote healthy behaviors.
Objective
The purpose of this research is to systematically assess the efficacy of patient navigation and similar programs to improve diagnosis and treatment of diseases affecting medically underserved populations.
Methods
A systematic review was performed by searching PubMed, MEDLINE, PsychINFO, and CINAHL to identify potential studies. Eligible studies were those containing original peer-reviewed research reports in English on patient navigation, community health workers, vulnerable and underserved populations, and healthcare disparity. Specific outcomes regarding patient navigator included effect of the intervention on definitive diagnosis and effect on initiation of treatment were extracted from each study.
Results
The search produced 1,428 articles and 16 were included for review. All studies involved patient navigation in the field of Oncology in underserved populations. Timing of initial contact with a patient navigator after diagnostic or screening testing is correlated to the effectiveness of the navigator intervention. The majority of the studies reported significantly shorter time intervals to diagnosis and to treatment with patient navigation.
Conclusions
Patient navigation expedites oncologic diagnosis and treatment of patients in underserved populations. This intervention is more efficacious when utilized shortly after screening or diagnostic testing.
INTRODUCTION
Patient adherence to physician recommended follow-up and treatment plans is often a challenge. Martin et al reported in 2005 that up to 40% of patients did not comply with their recommended treatment plans. When a patient’s treatment plan is more complex or requires active lifestyle changes, that percentage of non-adherence can rise to as high as 70%. Such lack of patient compliance can lead to significant complications in the patient’s healthcare as well as increased medical expenses [1]. Reported factors that lead to non-adherence include confusion regarding the recommended follow-up or treatment plan, lack of consistency in the patient’s medical care, cultural or health beliefs that conflict with the plan, socioeconomic status, mistrust of the healthcare system, and a lack of social support for the patient [2]. All of these factors serve as potential barriers that doctors, nurses, and other providers must assist the patient in overcoming.
Patient navigation is an evidence-based intervention created to address non-adherence and help patients maneuver through personal and systematic barriers in order to achieve timely follow-up care for health conditions [3]. The role of a patient navigator is to assist patients in overcoming challenges that prevent adherence to their healthcare plan, allowing them to progress efficiently through their treatment. The original concept and development of this intervention stems from the findings of the American Cancer Society National Hearings on Cancer in the Poor in 1989. These hearings revealed a host of difficulties that underserved populations face in receiving timely and appropriate care. Based on these findings, Dr. Harold Freeman initiated the first patient navigation program in 1990 to promote timely cancer treatment in Harlem, New York [4]. Since that pilot program, treatment centers worldwide have been using patient navigators to improve the quality and timeliness of therapy in a multitude of cancer types. The purpose of this research is to systematically evaluate the efficacy of patient navigation in improving timely and appropriate diagnosis and treatment of disease in medically underserved populations. We hypothesize that patient navigation is effective in improving timely, appropriate follow-up care for diagnosis and treatment of chronic illness within underserved populations.
METHODS
This study was exempt from Institutional Review Board approval. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis [5] checklist was used to guide this systematic review. A specific outcome measure was not required for inclusion in this review. The specific inclusion criteria included: 1) articles pertaining to patient navigation in the healthcare setting, 2) articles reporting on the effect of navigation on definitive diagnosis, and 3) articles reporting on the effect of navigation on timely initiation of treatment, and 4) articles studying patient population designated as underserved. Exclusion criteria included: 1) single case reports or non-original research and 2) language other than English.
Search Strategy
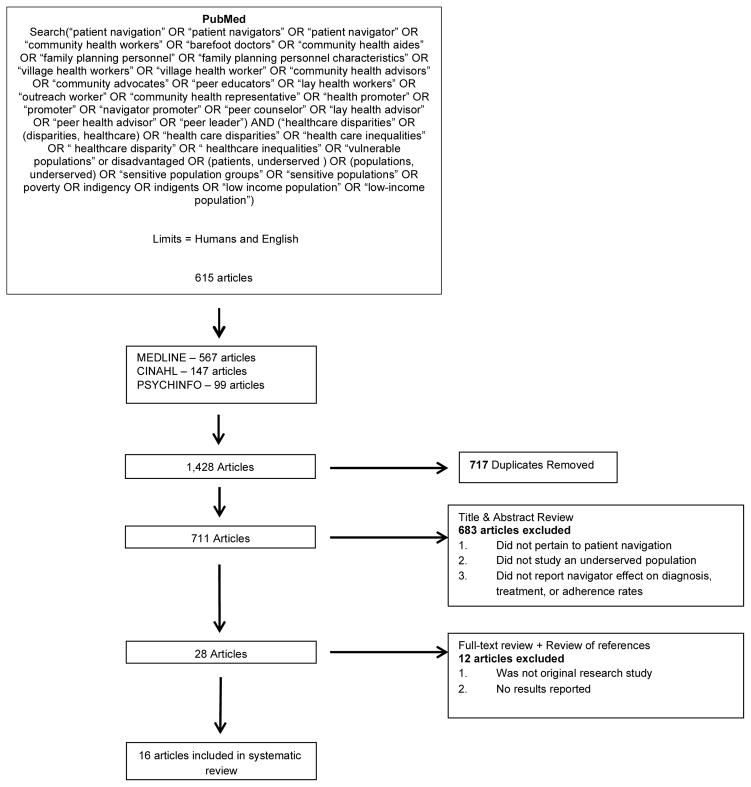
To perform a systematic literature review of patient navigation in the underserved, a search string was developed to include patient navigation or similar programs used in populations that are medically underserved. A search string was designed to include studies that addressed both (1) patient navigation and (2) medically underserved populations. See Figure 1 for the complete search string. A search strategy was developed using The National Library of Medicine’s (NLM) medical subject heading (MeSH) browser in expanded concept view to identify MeSH indexed search terms (http://www.nlm.nih.gov/mesh/MBrowser.html). In an attempt to capture articles pertaining to the study objective, MeSH terms associated with “patient navigation” were used to ensure that pertinent navigation studies were not excluded based on the title of the program. These included barefoot doctors, community health workers, community health aides, and health promoter. To identify all relevant articles related to “health disparity” the following words were also included: inequality, low-income, poverty, and indigent.
Figure 1.
Preferred reporting items for systematic review and meta-analysis algorithm
An initial search was performed in PubMed. [All Fields] was selected to ensure that articles that mentioned the pertinent terms in any form would be captured. The search was confined to English only papers. The same search string was then used to search MEDLINE, PsychINFO, Web of Science, and CINAHL, with duplicates from the four searches being removed. Title and abstract reviews were conducted to select articles that dealt with human subjects and any form of patient navigation and health disparity, eliminating case studies, literature reviews, or studies with no reported timing to diagnosis or treatment outcomes. The search was performed in August 2015. Figure 1 lists terms utilized in the search string as well as the algorithm for inclusion/exclusion.
Data Extraction
Article titles and abstracts were reviewed independently by 2 reviewers and were selected or removed based on the inclusion and exclusion criteria. In the event of disagreement over inclusion, the article was included for full text review to be more inclusive. The reviewers completed a full-text review of all eligible articles independently and the bibliographies of these articles were examined to identify additional articles. The two reviewers independently analyzed the articles and results were then organized into two tables focusing on the outcomes of (1) effect of navigation on obtaining a definitive diagnosis following screening test and (2) effect of navigation on obtaining treatment following diagnosis. The level of evidence of each article was also assessed according to the Oxford Centre for Evidence-based Medicine guidelines [6].
Bias Assessment
Articles were reviewed independently and scored based on accepted bias assessment tools. Randomized controlled studies were analyzed using the National Institute of Health Quality Assessment Tool for Controlled Intervention Studies. A score was obtained based on the 14-point questionnaire. The authors agreed on a score of 10 or above for a low risk of bias, 6–9 for a moderate risk of bias and 5 or less for high risk of bias. Retrospective studies were assessed using the Newcastle – Ottawa Scale. The authors agreed on a score of greater than 8 as a low risk for bias, 5–8 for moderate risk and less than 5 as high risk of bias. Studies that did not conform to these bias scales were not assessed.
RESULTS
Search Results
The initial search of all 4 databases yielded 1,428 articles. After the duplicates were removed, 711 articles remained. The titles and abstracts of these articles were scanned to determine if they met the study objectives; 683 articles were removed through this process. A full text review and scan of the references of the remaining twenty-eight articles were performed. Of the twenty-eight, sixteen met the inclusion criteria and were eligible for the systematic review. Of these studies, seven used a randomized trial design, five used a non-randomized design, two were observational, and two included multiple study sites that use different methods. There was a lack in consistency in outcome reporting and intervention conditions, thus a meta-analysis was not performed. The type of navigator in each study differed; seven of the studies recruited lay people to be trained in the role of a navigator, three employed nurses with oncology experience, and six studies used a team approach consisting of a lay person and a nurse or an individual with a master’s in social work (MSW). The studies were conducted from 1998–2011, and all were based in the United States. The participants in the studies included uninsured, non-English speaking, and underserved residents from urban or rural locations. The reported efficacy of navigation on diagnosis and treatment are recorded in Table 1 and Table 2, respectively, along with description of the study sample.
Table 1.
Effect of Patient Navigation on Diagnosis as Primary Outcome
| Author/Year | Level of Evidence | Sample | Cancer Type | Type of Navigator | Navigation Effective? | Bias Score and Risk Assessment | Average Time to Diagnosis |
|---|---|---|---|---|---|---|---|
| Percac-Lima (2015) | IIb | 369 women who were nonwhite, non-English speaking or had Medicaid or no insurance | 1 | Yes | 9 - Low | Not Reported | |
| Lee (2014) | IIb | 193 racial & ethnic minority participants | 2 | -- | Yes | 10 - Low | Not Reported |
| Freund (2014) | IIb | 10,521 mainly racial & ethnic minority and uninsured/publicly insured participants | 1, 2, 3, 4 | -- | Yes | Unable to Assess | Not Reported |
| Bensink (2014) | IIb | 4330 racial & ethnic minority/ low income participants | 1, 2, 3, 4 |
-- + |
Yes | Unable to Assess | Mean: 110 days PN vs 109 days control |
| Lee (2013) | IIb | 1,039 mainly low- income, non-English speaking, Hispanic women | 1 | -- | Yes | 11- Low | Median: 6.2 months PN vs 12 months control |
| Battaglia (2012) | IIb | 3,041 women mainly from racial & ethnic minority groups | 1, 3 | + | Yes | 8 - Low | Not Reported |
| Dudley (2012) | IIIb | 461 mainly low income women with lower education level | 1 |
-- + |
Yes | 8 - Low | Mean (Hispanic): 36.65 PN vs 52.96 control Mean (other minorities): 37.68 PN vs 70 control |
| Markossian (2012) | IIb | 897 low-income, racial & ethnic minority women | 1, 3 |
-- ** |
Yes | 9 - Low | Not Reported |
| Paskett (2012) | IIb | 862 participants from clinics serving mainly minority, low-income, and elderly patients. | 1, 2, 3 | + | Yes | 10 - Low | Not Reported |
| Raich (2012) | IIb | 993 mainly racial & ethnic minority and uninsured/publicly insured participants | 1, 2, 4 | -- | Yes | 10 - Low | Not Reported |
| Wells (2012) | IIb | 1,267 mainly racial & ethnic minority and uninsured/publicly insured participants | 1, 2 | -- | No | 11- Low | Mean: 61 days PN vs 42 days control |
| Ferrante (2008) | IIb | 105 non-English speaking Hispanic women | 1 | + | Yes | 11 - Low | Mean: 25.0 days PN vs 42.7 days control |
| Ell (2007) | IIb | 204 Hispanic women with low incomes and non-English speaking | 1 |
-- ** |
Yes | 10 - Low | Not Reported |
| Ell (2002) | IIb | 196 Hispanic women with low incomes | 3 |
-- ** |
Yes | 5 - Moderate | Not Reported |
| Ell (2002) | IIIb | 605 culturally diverse women with low incomes | 1 |
-- ** |
Yes | 8 - Low | Not reported |
Description of patient navigator effect on diagnosis. Lay navigator (--), professional health care workers (+), & MSW (**). Breast Cancer (1), Colorectal (2), Cervical (3), & Prostate (4).
Table 2.
Effect of Patient Navigation on Treatment as Primary Outcome
| Author/Year | Level of Evidence | Sample | Cancer Type | Navigator Type | Navigation Effective? | Bias Score and Risk Assessment | Average Time to Treatment |
|---|---|---|---|---|---|---|---|
| Ramirez (2014) | IIIb. | 109 Hispanic women with public or no insurance | 1 | -- | Yes | 8 - Low | Mean: 22.22 days PN vs 48.30 control |
| Freund (2014) | IIIb. | 10,521 mainly racial & ethnic minority and uninsured/publicly insured participants | 1, 2, 3, 4 | -- | Yes | Unable to Assess | Not Reported |
| Dudley (2012) | IIIb. | 461 mainly low income women with lower education level | 1 | + | Yes | 8 - Low | Mean: 57 days PN vs74 days control |
| Ell (2002) | IIIb. | 605 culturally diverse women with low incomes | 1 |
-- ** |
Yes | 8 - Low | Median: 24 days PN vs 29 days control |
Description of patient navigator effect on treatment. Lay navigator (--), professional health care workers (+), & MSW (**). Breast Cancer (1), Colorectal (2), Cervical (3), & Prostate (4).
Studies with Time to Diagnosis as the Primary Outcome
Fifteen of the articles included in the review assessed the effect of patient navigation on timely diagnostic resolution following an abnormal cancer screening. Twelve of fifteen studies had a low level of bias, with one study having a moderate level of bias and two studies unable to be assessed. The studies varied regarding the cancer type included in the trial; six of the articles addressed only patients with abnormal breast cancer screenings, one involved cervical cancer, one involved colorectal cancer, and the remaining seven included multiple types of cancer including breast, cervical, colorectal, and prostate cancers. Diagnostic resolution was defined as a patient obtaining follow-up testing that resulted in either a definitive diagnosis of cancer or no cancer [7,8]. A majority of the studies measured time to diagnosis as the date of the abnormal screening to the date diagnostic testing was complete [2,3,7,9–13]. Three of the studies placed more emphasis on adherence to follow-up appointments; however, these appointments usually resulted in diagnostic resolution as well [9,14,15].
As mentioned previously, the qualifications and characteristics of the navigators varied between studies. Some utilized lay navigators who had personal experience with the disease and represented the population they were serving (e.g. Hispanic women serving as navigators in an area where majority of the patients were also Hispanic). Others reported hiring professional health care workers or MSWs to perform navigation activities. Some studies included one or more navigators who were bilingual, commonly speaking English and Spanish. The structure of navigation also varied across studies. While some used a highly-structured guide or assessment tool for each patient encounter, others used a simple logging system to record barriers or problems addressed during a conversation with the patient. Though the execution of navigation differed between the articles, the basic services provided and challenges addressed were consistent. The articles cited obstacles such as transportation, lack of insurance, coordination of healthcare appointments, language barriers, and general misunderstanding of the follow-up process as difficulties that navigators helped patients overcome.
Fourteen of the articles reported significant improvement in obtaining diagnostic resolution when a navigator was utilized [2,3,7–17]. The remaining article did not find the use of a patient navigator to be effective in improving the time from screening to diagnosis [18]. This outlying study reported a significant gap between the screening test and contact with the patient navigator. Over one-third of the patients in that study were not contacted by the navigator within the first month following the abnormal screening test [18]. This suggests that timeliness of initial contact by the navigator may influence the efficacy of such a program. Another study reported earlier diagnostic resolution with navigation; however, there was no significant difference in cancer stage at time of diagnosis between the navigator group and the control group in those patients that were actually diagnosed with cancer [17].
Studies with Time to Treatment as Primary Outcome
Four of the sixteen articles included in this review assessed the effect of a patient navigator on time from definitive diagnosis to initiation of appropriate treatment. All studies had a low risk of bias. Three of these studies only included patients diagnosed with breast cancer; the remaining study included patients who had been diagnosed with breast, cervical, colorectal, and prostate cancers. Two of the studies utilized a non-randomized design, one used an observational design, and one utilized multiple designs to accommodate the needs to each site in their study. These articles also had the same variation in the characteristics and qualifications of their navigators as the studies that focused on time to diagnosis. Each of the studies defined time to treatment initiation as the time from date of definitive diagnosis to the date that treatment was first received however the outcomes were reported through various methods [9,10,19,20]. Some of the articles reported an outcome of number of days to initiation of treatment whereas other described the proportion of patients receiving treatment within a defined period of time after diagnosis (i.e. −60 days, 90 days, or 365 days). Types of treatment that were included were radiation, chemotherapy, hormone therapy, and surgery [19]. All four articles saw a significant decrease in time to treatment initiation or improvement of adherence in the navigated patients over the standard of care. One study that did not employ a randomized controlled trial design utilized a sample of patients that were not enrolled into a patient navigation program as a control group to compare with those that were enrolled into patient navigation [9]. This observation pilot study followed these patients from a mammogram screening through diagnosis and even treatment. In spite of this study design and missing data on many patients, this study found that patients receiving navigation were treated on average 24 days after diagnosis compared with 29 days after diagnosis for those outside of the navigation program. [9] Another study that conducted a multi-site investigation with different study designs from each site examined the proportion of patients that received treatment within 60, 90, or 365 days. [10] There was no statistically significant difference between the navigation group and the control group in this study; however, this study was limited by lack of fidelity in the navigation intervention and variability in how the study was conducted at different sites. Ramirez et al described a non-randomized prospective study that found a significantly higher proportion of underserved Latinas receiving treatment at 30 days and 60 days after diagnosis [19]. Another study assessing navigation in Hispanic women conducted an observational study using a historical control from medical records of patients who did not undergo navigation compared with those prospectively enrolled in a navigation program [20]. In spite of this study design, this study found that patients receiving navigation initiated sooner than those receiving the standard of care. The majority of these studies were limited by lack of randomization in study group allocation with variability in outcome reporting; however, the evidence from these studies would support patient navigation in improving timing of treatment.
DISCUSSION
Patient compliance to care is a factor that limits the efficacy of all aspects of medicine. Within the medically underserved this problem is magnified. Patient navigation programs are designed to assist patients, specifically ones from underserved populations, in receiving and maintaining timely and adequate health care. The studies in this review assessed the efficacy of patient navigation in assisting the medically underserved in overcoming barriers to their care. Review of these articles yielded themes as to what makes a successful navigation program and which patients may benefit most from such programs. First, timeliness of navigation initiation plays a role in the success of a program. The timing of navigation is critical to promote positive health behaviors. Patients in the midst of a potential diagnosis of cancer or facing an ominous treatment regimen may be overwhelmed by the gravity of the situation which could lead to isolation, confusion, and frustration in taking the correct steps. Conversely, patients may also underestimate the seriousness of efficient diagnosis and treatment of malignant disease and may dismiss healthcare recommendations as time following screening elapses. The single non-efficacious program consistently took over 30 days to enroll patients into patient navigation. For these reasons, patient navigation should be initiated as soon as feasibly possible following cancer screening and/or cancer diagnosis. Timely initiation of navigation would make the patient-to-navigator relationship more meaningful, and increase the likelihood that the patient will receive diagnostic resolution and treatment within the necessary timeframe [18].
Patients can be navigated through the healthcare system by a variety of different people. Physicians, nurses, case managers, social workers, and dedicated patient navigators can all provide the type of information and support that a patient navigation intervention is meant to provide. Professionals within busy multidisciplinary cancer centers may not have adequate time to assist patients as they navigate through cancer diagnosis and treatment. Healthcare providers may; however, take a more active role in navigation as threat of malignant disease is greater. The risk of malignant disease on screening testing may have an inverse relationship with patient navigation efficacy. When screening-testing results revealed a high risk for cancer, patient navigation was less effective as it is likely that key providers of care play an active role in expediting diagnostic evaluation and treatment. Stated another way, when a patient has objective findings on screening or diagnostic testing of either a high risk of malignancy or advanced stage disease, the medical provider and/or physician is more likely to play an active role in leading the patient through the healthcare process to obtain the appropriate diagnosis or treatment, somewhat limiting the utility of intervention by a patient navigator. The fear of a cancer diagnosis is also a strong motivator to overcoming significant barriers otherwise in place in this patient population. However, patients with low or moderate risk of a cancerous lesion on screening testing yielded the highest efficacy when navigated versus the control group [12,13]. This is proposed to be due to the perceived importance of definitive diagnostic evaluation. [12,13] A navigator may be able to emphasize the importance of definitive diagnostic evaluation in spite of low to moderate risk of disease, increasing their rates of adherence to care over control groups. While all patients from diverse backgrounds benefit from navigation compared with control groups in these studies, programs with limited resources may see the highest efficacy when targeting resources towards this specific patient group.
This review found that patient navigation is an efficacious intervention to improve adherence to receive timely medical care. This is an important issue within Oncology, as decreasing time to diagnosis and time to treatment has been shown to decrease mortality. Huo et al. found that delays in diagnosis among breast cancer patients correlated to increased likelihood of cancer metastasis and lower rates of disease-free survival [21]. Redaniel et al. describe that the patients receiving colorectal cancer screening sooner after diagnosis have higher survival rates [22]. Similarly, Dolly et al. found that a delay between diagnosis and treatment in endometrial cancer patients was correlated with a higher disease mortality [23]. Although disease survival and treatment outcomes were not consistently reported in the studies within this review, patient navigation expedites diagnosis and treatment in oncology patients and has the potential to impact survival in the treatment of cancer. Further studies to truly elucidate the time saved by navigation remain a priority to justify the monetary impact that navigation has on the healthcare system. The cost of navigation was underreported in the studies reviewed and this issue remains a concern when considering wide implementation of such interventions. In spite of demonstrating more expeditious diagnostic resolution following cancer screening with navigation, Bensink et al reported an increased cost of $275 per patient with patient navigation compared with control. The overall value and cost savings in patient navigation is likely understated as this study did note patient navigation contributed to significantly higher diagnostic resolution and probability of ever having diagnostic resolution [17].
There are limitations of this review as well as the articles included in the review. In spite of thorough search criteria, it is possible that relevant articles were excluded from this review. Publication bias is also a limitation as equivocal findings in intervention studies may not be reported or published. Outcome reporting bias is also a limitation of this review but using a protocol such that our hypothesis and methods were determined a priori to the knowledge of the results reduced this. Potential biases were reduced in our interpretation of the data by employing a systematic approach to our search strategy outlined above. Conclusions drawn from this systematic review are limited given that a meta-analysis could not be performed.
The care and support provided to patients at risk for having a cancer diagnosis is critical, as timing from an abnormal screening to diagnostic appointment can impact cancer status and ultimately survival. Although many different providers with varying levels of expertise and skills have provided navigation, there are many benefits that may come from nurses serving in this role. With nurses having extensive knowledge, skills, and clinical judgment, they’re able to assess a patient, provide supportive care, manage the complexity of care, integrate their care with other clinicians, and prepare and support patients throughout their care [24]. Nurses with oncology training, serving in the role of a patient navigator, may produce improved compliance rates among patients at risk for or diagnosed with cancer compared with non-nurse patient navigators. Skilled nursing staff does present a cost-barrier that utilizing other trained navigators, such as lay-people or nursing technicians, may mitigate. The appeal of navigating the cancer healthcare system with a person who has previously undergone similar experiences cannot be understated.
CONCLUSIONS
Patient navigation is useful in assisting in care delivery for the underserved. This review supports the use of navigation as an effective tool in increasing adherence to care in these populations. While certain populations may benefit more from navigation, it has been shown to work in diverse groups. In the future, it may be beneficial to investigate different delivery methods for patient navigation, the timing of intervention, and factors associated with successful patient navigators (i.e. the training and background of patient navigators). Further research into the use of navigation in the medically underserved will give more insight into potential uses.
Acknowledgments
This work was supported by National Center for Advancing Translational Sciences and the University of Kentucky Center for Clinical and Translational Science (UL1TR000117) (TS) and National Institute of Deafness and Other Communication Disorders (1K23DC014074)(MLB). MLB is a member of the Surgical Advisory Board of Med El Corporation.
Footnotes
The authors have no other financial relationships or conflicts of interest to disclose pertaining to the manuscript.
References
- 1.Martin LR, Williams SL, Haskard KB, DiMatteo MR. The challenge of patient adherence. Therapeutics and Clinical Risk Management. 2005;1(3):189–199. [PMC free article] [PubMed] [Google Scholar]
- 2.Ferrante JM, Chen P, Kim S. The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2008;85(1):114–124. doi: 10.1007/s11524-007-9228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Battaglia TA, Bak S, Heeren T, et al. Boston patient navigation research program: the impact of navigation on time to diagnostic resolution after abnormal cancer screening. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1645–1654. doi: 10.1158/1055-9965.EPI-12-0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freeman HP, Rodriguez RL. The history and principles of patient navigation. Cancer. 2011;117(15 0):3539–3542. doi: 10.1002/cncr.26262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic review sand meta-analyses: the PRISMA statement. British Medical Journal. 2009;338:b2535. [PMC free article] [PubMed] [Google Scholar]
- 6.Oxford Centre for Evidence-based Medicine – Levels of Evidence. Centre for Evidence-Based Medicine. Mar, 2009. Retrieved May 4, 2016. [Google Scholar]
- 7.Lee J, Fulp W, Wells KJ, Meade CD, Calcano E, Roetzheim R. Effect of patient navigation on time to diagnostic resolution among patients with colorectal cancer-related abnormalities. J Canc Educ. 2014;29:144–150. doi: 10.1007/s13187-013-0561-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Markossian TW, Darnell JS, Calhoun EA. Follow-up and timeliness after an abnormal cancer screening among underserved, urban women in a patient navigation program. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1691–1700. doi: 10.1158/1055-9965.EPI-12-0535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ell K, Padgett D, Vourlekis B, et al. Abnormal mammogram follow-up: a pilot study in women with low income. Cancer Practice. 2002;10(3):130–138. doi: 10.1046/j.1523-5394.2002.103009.x. [DOI] [PubMed] [Google Scholar]
- 10.Freund KM, Battaglia TA, Calhoun E, et al. Impact of patient navigation on timely cancer care: the patient navigation research program. JNCI. 2014;106(6) doi: 10.1093/jnci/dju115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee J, Fulp W, Wells KJ, Meade CD, Calcano E, Roetzheim R. Patient navigation and time to diagnostic resolution: results for a cluster randomized trial evaluating the efficacy of patient navigation among patients with breast cancer screening abnormalities, tampa, fl. PLoS ONE. 2013;8(9):e74542. doi: 10.1371/journal.pone.0074542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Percac-Lima S, Ashburner JM, McCarthy AM, Piawah S, Atlas SJ. Patient navigation to improve follow-up of abnormal mammograms among disadvantaged women. Journal of Women’s Health. 2015;24(2):138–143. doi: 10.1089/jwh.2014.4954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raich PC, Whitley EM, Thorland W, Valverde P, Fairclough D. Patient navigation improves cancer diagnostic resolution: an individually randomized clinical trial in an underserved population. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1629–1638. doi: 10.1158/1055-9965.EPI-12-0513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ell K, Vourlekis B, Muderspach L, et al. Abnormal cervical screen follow-up among low- income Latinas: project safe. Journal of Women’s Health & Gender-Based Medicine. 2002;11(7):639–651. doi: 10.1089/152460902760360586. [DOI] [PubMed] [Google Scholar]
- 15.Ell K, Vourlekis B, Lee P, Xie B. Patient navigation and case management following an abnormal mammogram: a randomized clinical trial. Preventative Medicine. 2007;44:26–33. doi: 10.1016/j.ypmed.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 16.Paskett E, Katz ML, Douglas MP, et al. The ohio patient navigation research program (opnrp): does the american cancer society patient navigation model improve time to resolution among patients with abnormal screening tests? Cancer Epidemiol Biomarkers Prev. 2012;21(10):1620–1628. doi: 10.1158/1055-9965.EPI-12-0523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bensink ME, Ramsey SD, Battaglia T, et al. Costs and outcomes evaluation of patient navigation after abnormal cancer screening. Cancer. 2014:570–578. doi: 10.1002/cncr.28438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wells KJ, Lee J, Calcano E, et al. A cluster randomized trial evaluating the efficacy of patient navigation in improving quality of diagnostic care for patients with breast or colorectal cancer abnormalities. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1664–1672. doi: 10.1158/1055-9965.EPI-12-0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramirez A, Perez-Stable E, Penedo F, et al. Reducing time-to-treatment in underserved Latinas with breast cancer. Cancer. 2014:752–760. doi: 10.1002/cncr.28450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dudley DJ, Drake J, Quinlan J, et al. Beneficial Effects of a combined navigator/promotora approach for hispanic women diagnosed with breast abnormalities. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1639–1644. doi: 10.1158/1055-9965.EPI-12-0538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huo Q, Cai C, Zhang Y, et al. Delay in diagnosis and treatment of symptomatic breast cancer in china. Ann Surg Oncol. 2015;22(3):883–8. doi: 10.1245/s10434-014-4076-9. [DOI] [PubMed] [Google Scholar]
- 22.Redaniel MT, Martin RM, Blazeby JM, Wade J, Jeffreys M. The association of time between diagnosis and major resection with poorer colorectal cancer survival: a retrospective cohort study. BMC Cancer. 2014;14:642. doi: 10.1186/1471-2407-14-642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dolly D, Mihai A, Rimel BJ, et al. A delay from diagnosis to treatment is associated with decreased overall survival for patients with endometrial cancer. Front Oncol. 2016;12(6):31. doi: 10.3389/fonc.2016.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gilbert JE, Green E, Lankshear S, et al. Nurses as patient navigators in cancer diagnosis: review, consultation and model design. European Journal of Cancer Care. 2011;20:228–236. doi: 10.1111/j.1365-2354.2010.01231.x. [DOI] [PubMed] [Google Scholar]