Abstract
Regulatory approvals of non-vitamin K antagonist oral anticoagulants (NOACs) have been based on large randomized phase III trials evaluating dabigatran, rivaroxaban, apixaban, or edoxaban relative to warfarin for atrial fibrillation (AF). The results of the trials showed that all NOACs were at least non-inferior to warfarin in the prevention of stroke/thromboembolism and showed lower rates of intracranial bleeding than those associated with warfarin. However, the trials were designed differently, varied in the inclusion/exclusion criteria, and used either one dose or a low/high dose of the NOAC drug. Some of these differences have challenged the ability to directly compare various NOACs, and comparative data on effectiveness and intracranial bleeding are sparse in “real-world” patients. Real-world data complement data from large randomized phase III trials by providing new aspects of the “real-world” absolute risks of ischemic and hemorrhagic stroke associated with NOACs vs. warfarin. Moreover, “real-world” fragile patients might have been included (e.g., patients with increased risk of bleeding, liver disease, and chronic kidney disease), although these patients would be less represented in trials. This paper introduces recently published real-world data of NOACs and further suggests the recommended dosage of NOACs for Korean patients.
Keywords: Atrial fibrillation, Anticoagulants, Factor Xa inhibitors, Clinical trial
INTRODUCTION
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia, occurring in 1–2% of the general population, and its occurrence has increased rapidly in Korea.1),2) It is associated with a 5-fold increase in stroke risk, and one in 5 cases of stroke is attributed to this arrhythmia.3) Oral anticoagulant (OAC) treatment can prevent the majority of ischemic strokes in patients with AF and prolong life.4) It is superior to no treatment or aspirin in patients with different profiles for stroke risk.5) Non-vitamin K antagonist oral anticoagulants (NOACs) can have a considerable effect on standard stroke prevention and management in AF. Their predictable pharmacodynamics and kinetics as well as fewer drug-drug and drug-food interactions than those of warfarin can simplify their use by healthcare professionals and patients. Several major trials have shown that NOACs have on-par or better efficacy and safety than warfarin.6),7),8),9)
Regulatory approvals of NOACs were based on 4 large randomized phase III trials evaluating dabigatran (Pradaxa®; Boehringer Ingelheim Pharmaceuticals, Inc., Ridgefield, CT, USA), rivaroxaban (Xarelto®; Janssen Pharmaceuticals, Inc., Titusville, NJ, USA), apixaban (Eliquis®; Bristol-Myers Squibb Company, Princeton, NJ, USA), or edoxaban (Savaysa®; Daiichi Sankyo, Inc., Parsippany, NJ, USA) vs. warfarin (Coumadin®; Bristol-Myers Squibb Company) for AF.6),7),8),9) The results of the trials showed that all NOACs were at least non-inferior to warfarin in prevention of stroke/thromboembolism (TE). Intracranial bleeding was a safety outcome in the trials, and all NOACs were associated with lower rates of intracranial bleeding than was warfarin. However, the trials were designed differently, with variations in the inclusion/exclusion criteria and either one dose or a low/high dose of the NOAC drug. Some of these differences have challenged the ability to directly compare stroke/TE prophylaxis and risk of intracranial bleeding with dabigatran, rivaroxaban, or apixaban relative to warfarin. Importantly, results of randomized controlled trials are wholly convincing, but comparative data on effectiveness and intracranial bleeding are sparse in real-world patients. Recently, a considerable amount of real-world data on NOACs has been published (Table 1). Real-world data are complementary to those obtained from large randomized phase III trials, providing new information on the “real-world” absolute risks of ischemic and hemorrhagic stroke with NOACs vs. vitamin K antagonists (VKAs). Moreover, real-world fragile patients might have been included (e.g., patients with increased risk of bleeding, liver disease, and chronic kidney disease), although these patients would be less represented in the trials.10) This paper highlights recently published real-world data of NOACs and further recommends NOAC dosages for Korean patients.
Table 1. Comparison of NOACs.
| Author | Study design | Region | Enrollment period | Cohort size | Endpoints | NOACs analyzed |
|---|---|---|---|---|---|---|
| Laliberté et al.30) | RC | US | May 2011 to Jul 2012 | 30,479 | Effectiveness and bleeding | R vs. D |
| Bouillon et al.31) | RC | France | Jan 2011 to Nov 2012 | 17,410 | Effectiveness and bleeding | D, R, or W |
| Abraham et al.32) | RC | US | Nov 2010 to Sep 2013 | 219,027 | GI bleeding | D, R, or W |
| Maura et al.33) | RC | France | Jul to Nov 2012 | 32,807 | Effectiveness and bleeding | D, R, or W |
| Graham et al.17) | RC | US | Nov 2011 to Jun 2014 | 118,891 | Stroke, bleeding, and mortality | R vs. D |
| Noseworthy et al.11) | RC | US | Oct 2010 to Feb 2015 | 31,574 | Effectiveness and bleeding | D, R, or W |
| Deitelzweig et al.34) | RC | US | Jan 2012 to Mar 2014 | 74,730 | Bleeding-related hospital readmissions | D, R, or W |
| Coleman et al.35) | RC | US | Jan 2012 to Oct 2014 | 38,831 | Stroke, ICH | A, R, or W |
| Lip et al.36) | RC | US | Jan 2012 to Dec 2013 | 29,338 | Bleeding | A, D, R, or W |
| Halvorsen et al.37) | Registry | Norway | Jan 2013 to Jun 2015 | 32,675 | Bleeding | A, D, R, or W |
| Chan et al.15) | RC | Taiwan | Feb 2013 to Dec 2013 | 304,252 | Effectiveness and bleeding | D, R, or W |
| Larsen et al.12) | RC | Denmark | Aug 2011 to Oct 2015 | 61,678 | Effectiveness and bleeding | A, D, R, or W |
| Yao et al.38) | RC | US | Oct 2010 to Jun 2015 | 125,243 | Effectiveness and bleeding | A, D, R, or W |
| Lip et al.39) | RC | US | Jan 2012 to Dec 2014 | 33,262 | Major bleeding | A, D, R, or W |
| Gorst-Rasmussen et al.16) | Registry | Denmark | Feb 2012 to Jul 2014 | 22,358 | Effectiveness and bleeding | D, R, or W |
| Staerk et al.13) | Registry | Denmark | Aug 2011 to Dec 2015 | 54,312 | Effectiveness and ICH | A, D, R, or W |
| Lamberts et al.22) | Registry | Denmark | Aug 2011 to Dec 2015 | 54,312 | Bleeding and non-persistence | A, D, R, or W |
| Hohnloser et al.40) | Registry | Germany | Jan 2013 to Mar 2015 | 35,013 | Bleeding | A, D, R, or W |
| Hernandez and Zhang18) | RC | US | Nov 2011 to Dec 2013 | 17,507 | Effectiveness and bleeding | R vs. D |
A = apixaban; D = dabigatran; GI = gastrointestinal; ICH = intracranial hemorrhage; NOAC = non-vitamin K antagonist oral anticoagulant; R = rivaroxaban; RC = retrospective cohort; W = warfarin.
REAL-WORLD NOAC DATA: STROKE AND TE
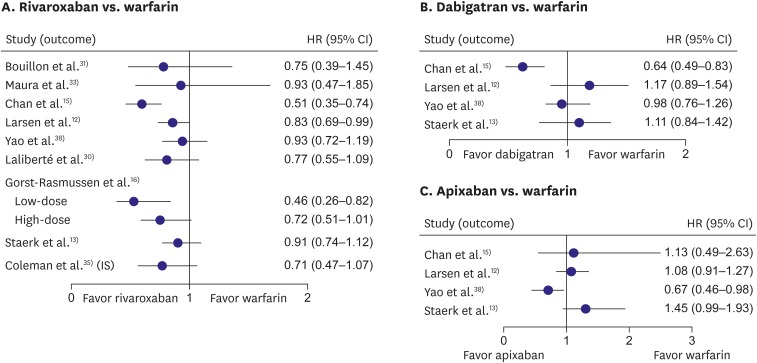
In cohorts of patients with non-valvular AF drawn from a large US database of commercial and Medicare supplement claims, dabigatran, rivaroxaban, and apixaban appeared to have similar effectiveness.11) In Danish nationwide registries, all NOACs appeared to be safe and effective alternatives to warfarin in a routine care setting.12) Recently, Staerk et al.13) reported that, in anticoagulant-naïve patients with AF, treatment with dabigatran, rivaroxaban, and apixaban was not associated with a significantly lower risk of stroke/TE than in patients administered anticoagulants (Figure 1).
Figure 1.
Comparison of each NOAC and warfarin in risk of stroke/TE in patients with AF.
AF = atrial fibrillation; CI = confidence interval; HR = hazard ratio; NOAC = non-vitamin K antagonist oral anticoagulant; TE = thromboembolism.
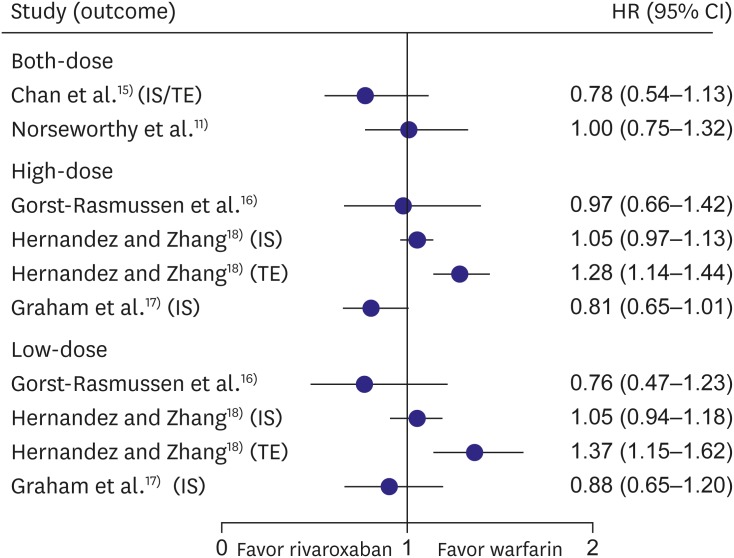
In a recent systematic review and meta-analysis, rivaroxaban was as effective as dabigatran, but was more effective than warfarin for the prevention of stroke/TE in patients with AF.14) Rivaroxaban was associated with a similar risk of stroke/TE to dabigatran11),15)16),17),18) (hazard ratio [HR], 1.02; 95% confidence interval [CI], 0.91–1.13; I2=70.2%, n=5), with a pooled rate for rivaroxaban at 0.3%/year vs. dabigatran at 0.3%/year (Figure 2).14) Noseworthy et al.11) reported that apixaban was as effective as rivaroxaban and dabigatran in the prevention of stroke/systemic embolism in patients with AF.
Figure 2.
Rivaroxaban compared with dabigatran in risk of stroke/TE in patients with AF.
AF = atrial fibrillation; CI = confidence interval; HR = hazard ratio; IS = ischemic stroke; TE = thromboembolism.
REAL-WORLD NOAC DATA: BLEEDING
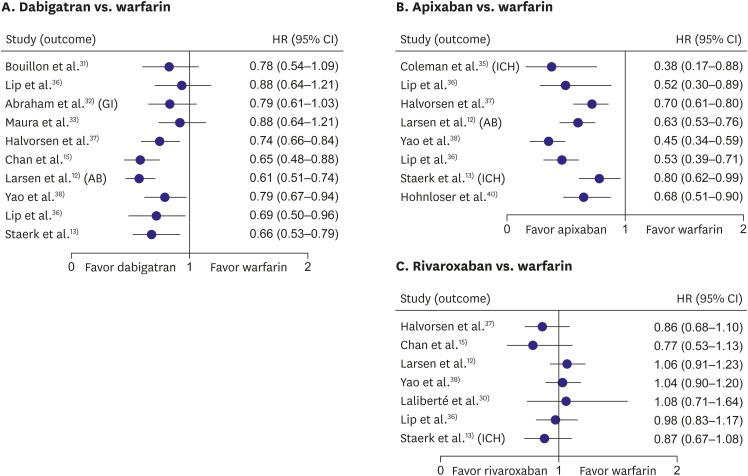
Each NOAC compared with warfarin in risk of major bleeding in patients with AF
Figure 3 shows the comparison of each NOAC with warfarin in risk of major bleeding in patients with AF. In the real-world study with elderly Medicare users of dabigatran,19) at the 150 mg twice-daily dose, the risk of intracranial bleeding and mortality in patients aged ≥65 was significantly reduced compared with that of warfarin. Similar observations were shown in real-world studies with elderly patients from other countries such as Canada.20) Carmo et al.21) published a meta-analysis of several observational trials of dabigatran. In total, 210,279 and 510,019 patients treated with dabigatran and warfarin, respectively, were included in the meta-analysis, which showed significant difference in mortality, intracranial hemorrhage, and major bleeding, in favor of dabigatran. Subgroup analysis showed greater benefits in the prevention of ischemic stroke with dabigatran than with warfarin in the elderly, but there was no significant benefit over warfarin for major bleeding related to age. The increased evidence of gastrointestinal bleeding with dabigatran 150 mg twice daily was in line with the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) trial, whereas dabigatran 110 mg twice daily showed no difference in gastrointestinal bleeding from warfarin.
Figure 3.
Comparison of each NOAC and warfarin in risk of major bleeding in patients with AF.
AB = any bleeding; AF = atrial fibrillation; CI = confidence interval; HR = hazard ratio; ICH = intracranial hemorrhage; NOAC = non-vitamin K antagonist oral anticoagulant.
In Danish nationwide registries, both apixaban and dabigatran had significantly lower risks of death, any bleeding, or major bleeding than did warfarin.12),13) In patients with high stroke and bleeding risks, dabigatran was the only NOAC associated with persistence of a significant low risk of intracranial bleeding. Another study showed that apixaban had a lower adjusted major bleeding risk than those of rivaroxaban, dabigatran, and warfarin.22)
However, rivaroxaban was comparable to warfarin in major bleeding incidences, with an increased risk of gastrointestinal bleeding and decreased risk of intracranial hemorrhage.14)
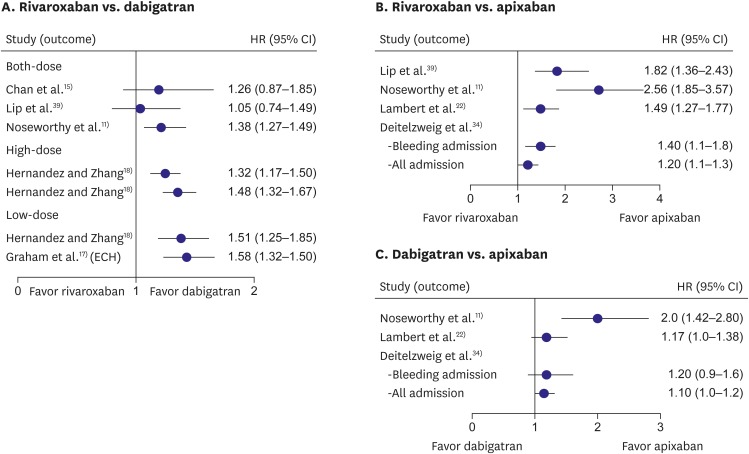
Comparison of NOACs in risk of major bleeding in patients with AF
Figure 4 shows the comparison of NOACs in risk of major bleeding in patients with AF. In a recent systematic review and meta-analysis, the major bleeding risk was significantly higher with rivaroxaban than it was with dabigatran (Figure 4A) or apixaban (Figure 4B), as were all-cause mortality and gastrointestinal bleeding. Rivaroxaban was associated with increased risk of all-cause mortality15),16),17),18) (HR, 1.23; 95% CI, 1.12–1.33), any bleeding16),17),18) (HR, 1.33; 95% CI, 1.17–1.49), and gastrointestinal bleeding15),17),18) (HR, 1.33; 95% CI, 1.18–1.48), but with similar risk of acute myocardial infarction15),17) (HR, 0.81; 95% CI, 0.43–1.19) and intracranial hemorrhage11),15),17),18) (HR, 1.22; 95% CI, 0.85–1.59) compared with dabigatran. Apixaban was comparable to dabigatran in major bleeding (Figure 4C).
Figure 4.
Comparison of NOACs in risk of major bleeding in patients with AF.
AF = atrial fibrillation; CI = confidence interval; ECH = extracranial hemorrhage; HR = hazard ratio; NOAC = non-vitamin K antagonist oral anticoagulant.
REAL-WORLD DATA FOR THE REDUCED DOSAGE OF NOAC
While NOACs do not require the meticulous dose adjustments required for warfarin, a clinical evaluation of appropriate (constant) doses is still necessary. A significant minority (approximately 1 in 8) of US patients in the community received NOAC doses inconsistent with labeling. NOAC over- and under-dosing are associated with an increased risk for adverse events.23) The efficacy and safety of reduced NOAC doses were reported in several studies. Recently, Nielsen et al.24) reported that, in the propensity weighted Danish nationwide study of reduced-dose NOAC regimens, apixaban 2.5 mg twice a day was associated with an increasing trend of ischemic stroke/systemic embolism rates compared with warfarin, while rivaroxaban 15 mg once a day and dabigatran 110 mg twice a day showed a trend of lower thromboembolic rates. The results were not significantly different. Rates of bleeding (the principal safety outcome) were significantly lower for dabigatran than for other agents, but did not significantly differ for apixaban and rivaroxaban compared with warfarin. Because the efficacy and safety were changed by reducing the dosage of NOAC, strict adherence to the dose reduction guideline is necessary.
Varying degrees of renal function require recommendations for reduced dosing regimens of these drugs; however, different cut-off values for age, body weight, or interacting drugs also require consideration for appropriate dose selection.25) Indeed, both age and chronic kidney disease in patients with AF intensify the risk of stroke and increase the risk of bleeding during antithrombotic treatment.26) In routine clinical practice, prescribed NOAC doses are often inconsistent with drug labeling. These prescribing patterns might be associated with worse safety profiles with no benefit in effectiveness in patients with severe kidney disease and worse effectiveness with no benefit in safety in apixaban-treated patients with normal or mildly impaired renal function.27)
RECOMMENDATION OF DOSE REGIMEN FOR KOREAN PATIENTS
Elderly patients with AF (such as those aged ≥80 years) and patients with impaired renal function were included in the landmark trials of NOACs, but these important subgroups comprised only a small proportion of the patient populations. For dabigatran, reduction of the daily recommended dose to 110 mg twice daily is indicated for patients aged ≥80 years. This dose can be reduced to 110 mg twice daily if the patient is aged 75–79 years and has other comorbidities that could affect bleeding risk such as previous gastritis, peptic ulcer disease, and moderate renal impairment. Indeed, label (or guideline) adherent use of dabigatran is clearly associated with better outcomes for stroke, major bleeding, and mortality.28),29) Insufficient published data for apixaban, edoxaban, and rivaroxaban indicate that further work is needed to clarify the bleeding risks of these NOACs in the elderly.
For Korean patients with AF, a reduced dosing regimen for dabigatran (110 mg twice a day) in patients aged ≥80 years or who have an estimated glomerular filtration rate (eGFR) of 30–50 mL/min; rivaroxaban (15 mg once daily) in patients aged ≥80 years or with an eGFR of 15–49 mL/min; apixaban (2.5 mg twice a day) if 2 of the 3 following criteria are present: age ≥80 years or an eGFR 15–29 mL/min or body weight ≤60 kg; or edoxaban (30 mg once daily) if eGFR is 15–50 mL/min are recommended (Table 2).
Table 2. Dose reduction of NOACs.
| Drug | Dose reduction criteria | Reduced dose | |
|---|---|---|---|
| Dabigatran | Patients aged ≥80 years or having eGFR of 30–50 mL/min | 110 mg twice daily | |
| Rivaroxaban | Patients aged ≥80 years or eGFR 15–49 mL/min | 15 mg once daily | |
| Apixaban | Two of three criteria: age ≥80 years, weight ≤60 kg, and Cr ≥1.5 mg/dL | 2.5 mg twice daily | |
| Edoxaban | ≥1 of 3 criteria | 30 mg once daily | |
| Concomitant use of potent P-glycoprotein inhibitors | |||
| Body weight ≤60 kg | |||
| CrCl 30–50 mL/min | |||
Cr = creatinine; CrCl = creatinine clearance; eGFR = estimated glomerular filtration rate; NOAC = non-vitamin K antagonist oral anticoagulant.
CONCLUSION
Real-world data is complementary to large randomized phase III trials by providing new information on the real-world absolute risks of ischemic and hemorrhagic stroke with NOACs vs. VKA. This paper highlighted recently published real-world data of NOACs and further recommended dosages for NOACs for Korean patients.
Footnotes
Funding: This study was supported by research grants from the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education, Science, and Technology (2017R1A2B3003303). In addition, grants were received from the Korean Healthcare Technology R&D project funded by the Ministry of Health and Welfare (HI16C0058 and HI15C1200).
Conflict of Interest: The author has no financial conflicts of interest.
- Conceptualization: Joung B.
- Data curation: Joung B.
- Formal analysis: Joung B.
- Funding acquisition: Joung B.
- Investigation: Joung B.
- Methodology: Joung B.
- Project administration: Joung B.
- Resources: Joung B.
- Software: Joung B.
- Supervision: Joung B.
- Validation: Joung B.
- Visualization: Joung B.
- Writing - original draft: Joung B.
- Writing - review & editing: Joung B.
References
- 1.Lee H, Kim TH, Baek YS, et al. The trends of atrial fibrillation-related hospital visit and cost, treatment pattern and mortality in Korea: 10-year nationwide sample cohort data. Korean Circ J. 2017;47:56–64. doi: 10.4070/kcj.2016.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee SR, Choi EK, Han KD, Cha MJ, Oh S. Trends in the incidence and prevalence of atrial fibrillation and estimated thromboembolic risk using the CHA2DS2-VASc score in the entire Korean population. Int J Cardiol. 2017;236:226–231. doi: 10.1016/j.ijcard.2017.02.039. [DOI] [PubMed] [Google Scholar]
- 3.Kim TH, Yang PS, Uhm JS, et al. CHA2DS2-VASc score (congestive heart failure, hypertension, age ≥75 [doubled], diabetes mellitus, prior stroke or transient ischemic attack [doubled], vascular disease, age 65–74, female) for stroke in Asian patients with atrial fibrillation: a Korean Nationwide Sample Cohort Study. Stroke. 2017;48:1524–1530. doi: 10.1161/STROKEAHA.117.016926. [DOI] [PubMed] [Google Scholar]
- 4.Gorst-Rasmussen A, Skjøth F, Larsen TB, Rasmussen LH, Lip GY, Lane DA. Dabigatran adherence in atrial fibrillation patients during the first year after diagnosis: a nationwide cohort study. J Thromb Haemost. 2015;13:495–504. doi: 10.1111/jth.12845. [DOI] [PubMed] [Google Scholar]
- 5.Hart RG, Pearce LA, Aguilar MI. Adjusted-dose warfarin versus aspirin for preventing stroke in patients with atrial fibrillation. Ann Intern Med. 2007;147:590–592. doi: 10.7326/0003-4819-147-8-200710160-00018. [DOI] [PubMed] [Google Scholar]
- 6.Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 7.Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–891. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]
- 8.Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–992. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- 9.Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–2104. doi: 10.1056/NEJMoa1310907. [DOI] [PubMed] [Google Scholar]
- 10.Tanislav C, Milde S, Schwartzkopff S, Misselwitz B, Sieweke N, Kaps M. Baseline characteristics in stroke patients with atrial fibrillation: clinical trials versus clinical practice. BMC Res Notes. 2015;8:262. doi: 10.1186/s13104-015-1237-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noseworthy PA, Yao X, Abraham NS, Sangaralingham LR, McBane RD, Shah ND. Direct comparison of dabigatran, rivaroxaban, and apixaban for effectiveness and safety in nonvalvular atrial fibrillation. Chest. 2016;150:1302–1312. doi: 10.1016/j.chest.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 12.Larsen TB, Skjøth F, Nielsen PB, Kjældgaard JN, Lip GY. Comparative effectiveness and safety of non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2016;353:i3189. doi: 10.1136/bmj.i3189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Staerk L, Fosbøl EL, Lip GY, et al. Ischaemic and haemorrhagic stroke associated with non-vitamin K antagonist oral anticoagulants and warfarin use in patients with atrial fibrillation: a nationwide cohort study. Eur Heart J. 2017;38:907–915. doi: 10.1093/eurheartj/ehw496. [DOI] [PubMed] [Google Scholar]
- 14.Bai Y, Deng H, Shantsila A, Lip GY. Rivaroxaban versus dabigatran or warfarin in real-world studies of stroke prevention in atrial fibrillation: systematic review and meta-analysis. Stroke. 2017;48:970–976. doi: 10.1161/STROKEAHA.116.016275. [DOI] [PubMed] [Google Scholar]
- 15.Chan YH, Kuo CT, Yeh YH, et al. Thromboembolic, bleeding, and mortality risks of rivaroxaban and dabigatran in Asians with nonvalvular atrial fibrillation. J Am Coll Cardiol. 2016;68:1389–1401. doi: 10.1016/j.jacc.2016.06.062. [DOI] [PubMed] [Google Scholar]
- 16.Gorst-Rasmussen A, Lip GY, Bjerregaard Larsen T. Rivaroxaban versus warfarin and dabigatran in atrial fibrillation: comparative effectiveness and safety in Danish routine care. Pharmacoepidemiol Drug Saf. 2016;25:1236–1244. doi: 10.1002/pds.4034. [DOI] [PubMed] [Google Scholar]
- 17.Graham DJ, Reichman ME, Wernecke M, et al. Stroke, bleeding, and mortality risks in elderly medicare beneficiaries treated with dabigatran or rivaroxaban for nonvalvular atrial fibrillation. JAMA Intern Med. 2016;176:1662–1671. doi: 10.1001/jamainternmed.2016.5954. [DOI] [PubMed] [Google Scholar]
- 18.Hernandez I, Zhang Y. Comparing stroke and bleeding with rivaroxaban and dabigatran in atrial fibrillation: analysis of the us medicare part d data. Am J Cardiovasc Drugs. 2017;17:37–47. doi: 10.1007/s40256-016-0189-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graham DJ, Reichman ME, Wernecke M, et al. Cardiovascular, bleeding, and mortality risks in elderly Medicare patients treated with dabigatran or warfarin for nonvalvular atrial fibrillation. Circulation. 2015;131:157–164. doi: 10.1161/CIRCULATIONAHA.114.012061. [DOI] [PubMed] [Google Scholar]
- 20.Avgil-Tsadok M, Jackevicius CA, Essebag V, et al. Dabigatran use in elderly patients with atrial fibrillation. Thromb Haemost. 2016;115:152–160. doi: 10.1160/TH15-03-0247. [DOI] [PubMed] [Google Scholar]
- 21.Carmo J, Moscoso Costa, F, Ferreira J, Mendes M. Dabigatran in real-world atrial fibrillation. Meta-analysis of observational comparison studies with vitamin K antagonists. Thromb Haemost. 2016;116:754–763. doi: 10.1160/TH16-03-0203. [DOI] [PubMed] [Google Scholar]
- 22.Lamberts M, Staerk L, Olesen JB, et al. Major bleeding complications and persistence with oral anticoagulation in non-valvular atrial fibrillation: contemporary findings in real-life danish patients. J Am Heart Assoc. 2017;6:e004517. doi: 10.1161/JAHA.116.004517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steinberg BA, Shrader P, Thomas L, et al. Off-label dosing of non-vitamin K antagonist oral anticoagulants and adverse outcomes: the ORBIT-AF II Registry. J Am Coll Cardiol. 2016;68:2597–2604. doi: 10.1016/j.jacc.2016.09.966. [DOI] [PubMed] [Google Scholar]
- 24.Nielsen PB, Skjøth F, Søgaard M, Kjældgaard JN, Lip GY, Larsen TB. Effectiveness and safety of reduced dose non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2017;356:j510. doi: 10.1136/bmj.j510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heidbuchel H, Verhamme P, Alings M, et al. Updated European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace. 2015;17:1467–1507. doi: 10.1093/europace/euv309. [DOI] [PubMed] [Google Scholar]
- 26.Olesen JB, Lip GY, Kamper AL, et al. Stroke and bleeding in atrial fibrillation with chronic kidney disease. N Engl J Med. 2012;367:625–635. doi: 10.1056/NEJMoa1105594. [DOI] [PubMed] [Google Scholar]
- 27.Yao X, Shah ND, Sangaralingham LR, Gersh BJ, Noseworthy PA. Non-vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. J Am Coll Cardiol. 2017;69:2779–2790. doi: 10.1016/j.jacc.2017.03.600. [DOI] [PubMed] [Google Scholar]
- 28.Lip GY, Clemens A, Noack H, Ferreira J, Connolly SJ, Yusuf S. Patient outcomes using the European label for dabigatran. A post-hoc analysis from the RE-LY database. Thromb Haemost. 2014;111:933–942. doi: 10.1160/TH13-09-0734. [DOI] [PubMed] [Google Scholar]
- 29.Chan NC, Coppens M, Hirsh J, et al. Real-world variability in dabigatran levels in patients with atrial fibrillation. J Thromb Haemost. 2015;13:353–359. doi: 10.1111/jth.12823. [DOI] [PubMed] [Google Scholar]
- 30.Laliberté F, Cloutier M, Nelson WW, et al. Real-world comparative effectiveness and safety of rivaroxaban and warfarin in nonvalvular atrial fibrillation patients. Curr Med Res Opin. 2014;30:1317–1325. doi: 10.1185/03007995.2014.907140. [DOI] [PubMed] [Google Scholar]
- 31.Bouillon K, Bertrand M, Maura G, Blotière PO, Ricordeau P, Zureik M. Risk of bleeding and arterial thromboembolism in patients with non-valvular atrial fibrillation either maintained on a vitamin K antagonist or switched to a non-vitamin K-antagonist oral anticoagulant: a retrospective, matched-cohort study. Lancet Haematol. 2015;2:e150–e159. doi: 10.1016/S2352-3026(15)00027-7. [DOI] [PubMed] [Google Scholar]
- 32.Abraham NS, Singh S, Alexander GC, et al. Comparative risk of gastrointestinal bleeding with dabigatran, rivaroxaban, and warfarin: population based cohort study. BMJ. 2015;350:h1857. doi: 10.1136/bmj.h1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maura G, Blotière PO, Bouillon K, et al. Comparison of the short-term risk of bleeding and arterial thromboembolic events in nonvalvular atrial fibrillation patients newly treated with dabigatran or rivaroxaban versus vitamin K antagonists: a French nationwide propensity-matched cohort study. Circulation. 2015;132:1252–1260. doi: 10.1161/CIRCULATIONAHA.115.015710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Deitelzweig S, Bruno A, Trocio J, et al. An early evaluation of bleeding-related hospital readmissions among hospitalized patients with nonvalvular atrial fibrillation treated with direct oral anticoagulants. Curr Med Res Opin. 2016;32:573–582. doi: 10.1185/03007995.2015.1131676. [DOI] [PubMed] [Google Scholar]
- 35.Coleman CI, Antz M, Bowrin K, et al. Real-world evidence of stroke prevention in patients with nonvalvular atrial fibrillation in the United States: the REVISIT-US study. Curr Med Res Opin. 2016;32:2047–2053. doi: 10.1080/03007995.2016.1237937. [DOI] [PubMed] [Google Scholar]
- 36.Lip GY, Pan X, Kamble S, et al. Major bleeding risk among non-valvular atrial fibrillation patients initiated on apixaban, dabigatran, rivaroxaban or warfarin: a “real-world” observational study in the United States. Int J Clin Pract. 2016;70:752–763. doi: 10.1111/ijcp.12863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Halvorsen S, Ghanima W, Fride Tvete I, et al. A nationwide registry study to compare bleeding rates in patients with atrial fibrillation being prescribed oral anticoagulants. Eur Heart J Cardiovasc Pharmacother. 2017;3:28–36. doi: 10.1093/ehjcvp/pvw031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yao X, Abraham NS, Sangaralingham LR, et al. Effectiveness and safety of dabigatran, rivaroxaban, and apixaban versus warfarin in nonvalvular atrial fibrillation. J Am Heart Assoc. 2016;5:e003725. doi: 10.1161/JAHA.116.003725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lip GY, Keshishian A, Kamble S, et al. Real-world comparison of major bleeding risk among non-valvular atrial fibrillation patients initiated on apixaban, dabigatran, rivaroxaban, or warfarin. A propensity score matched analysis. Thromb Haemost. 2016;116:975–986. doi: 10.1160/TH16-05-0403. [DOI] [PubMed] [Google Scholar]
- 40.Hohnloser SH, Basic E, Nabauer M. Comparative risk of major bleeding with new oral anticoagulants (NOACs) and phenprocoumon in patients with atrial fibrillation: a post-marketing surveillance study. Clin Res Cardiol. 2017;106:618–628. doi: 10.1007/s00392-017-1098-x. [DOI] [PubMed] [Google Scholar]