Abstract
Autoimmune ophthalmopathy is one of the salient clinical features associated with Graves’ disease. Exophthalmos is one of the commonest manifestations of Graves’ associated ophthalmopathy. It is reported to regress after thyroidectomy favourably compared to radioiodine or antithyroid drug therapy. In this context, we present our experience based on a surgical series of Graves’ disease. This is a prospective study of 15 patients of Graves’ disease associated with ophthalmopathic exophthalmos. Preoperative and monthly postoperative evaluation of exophthalmos was done with Hertel’s exophthalmometer, apart from documenting lid, extra-ocular muscle and orbital involvement. The minimum follow-up of the cohort was 12 months. The female to male ratio was 12:3 and the mean age of the subjects was 33.4 years (18–55). Exophthalmos was bilateral in 13 and unilateral in 2 patients. All the 15 patients underwent total thyroidectomy without any major morbidity. Exophthalmos regressed in 12 patients at a mean follow-up of 15.6 ± 6.4 months (14–38) and was static in 3. None of the cases had worsened ophthalmopathy at the final follow-up. Mean regression of exophthalmos was 2.1 mm (1–5). The regression was statistically significant at P value = 0.035. Surgery has a positive impact on the regression of ophthalmopathic exophthalmos associated with Graves’ disease.
Keywords: Graves’ disease, Ophthalmopathy, Exophthalmos, Total thyroidectomy, Regression
Introduction
Graves’ disease (GD) is an organ-specific autoimmune thyroid disease and caused primarily by a thyroid-stimulating autoantibody (TSAb) acting on the TSH receptor of the thyrocyte membrane [1]. Worldwide, it is one of the commonest thyroid disorders in the community [2, 3]. The classical and often exclusive clinical features of GD are ophthalmopathy, pretibial myxoedema and acropachy [2]. Graves’ associated exophthalmos (GAE) is one of the striking and obvious manifestations of Graves’ associated ophthalmopathy (GAO). The primary mechanism of exophthalmos is increased volume of intraorbital fat and muscles [4]. The cornerstone (crucial component) in the management of GAE is achieving and maintaining euthyroidism. However, the natural history of GAO is variable with a course often independent of the clinical course of thyrotoxicosis [5]. Resolution rates of GAO have been reported to be better after thyroidectomy compared to radioiodine therapy and antithyroid drugs alone. But, the objective evidence for the favourable influence of surgery is scanty in the literature. In this context, we conducted a study on opthalmopathic outcome with specific emphasis on the objectively measurable component, i.e. GAE in a surgical series.
Material and Methods
This is a prospective observational study conducted in the endocrine surgery department of a tertiary-care teaching hospital in southern India. The duration of the study was 24 months between June 2012 and May 2014. The study complied with international ethical norms according to the Helsinki Declaration - Ethical Principles for Medical Research Involving Human Subjects [6]. All the patients were followed up for a minimum period of 12 months. Out of 64 surgically treated cases of Graves’ disease, 24 had GAO (37.5 %). All of them were initially evaluated, and GAO was graded according to the Mouritz clinical activity score (CAS). Ten patients had a CAS score <4 and 14 had a score >4. Only 15/24 (55.6 %) had measurable GAE. The study cohort included these 15 cases with GAE. GAE was measured with a Hertel exophthalmometer.
GAE was defined as exophthalmos with ≥1 mm visible upper sclera and/or ≥2 mm visible lower scleral conjunctiva in a case of GD. We excluded nine remaining cases of GAO with lid retraction, myopathy and periorbital inflammation but without exophthalmos. We also measured the palpebral fissure height (PFH) defined as distance between upper and lower eyelid margins on a straight forward stare as measured by a normal scale held close to the eyes. This PFH was measured before and after treatment at all follow-up intervals. All the patients were rendered euthyroid (clinically and biochemically) before surgery with titrated doses of antithyroid drugs and beta blockers. All the patients were advised local eye measures—cold compresses, sunglasses, lubricating eye drops and head-up reclined position while sleeping. Three of them needed analgesics and/or short-term oral prednisolone for pain and periorbital inflammation. None in the cohort required orbital decompression surgically. All the 15 cases in the cohort underwent total thyroidectomy by the same surgeon. The indications for surgery apart from GAO were large goitres in 11 cases, antithyroid drug intolerance in 2 and recurrence after radioiodine therapy in 2 cases. None of them suffered from hypoparathyroidism or recurrent laryngeal nerve palsy. Postoperatively, they were put on thyroxine replacement with an empirical dose of 100 μg/day and later titrated to serum thyroxine levels at 6–8 weekly intervals. Statistical analysis was done using SPSS software version 14.0. Descriptive statistics and chi-square test were employed to analyse the data. For analysing the impact of regression of GAE, Student’s t test was used to analyse paired mean samples of exophthalmic orbital measurements. A P value was considered significant at <0.05.
Results
Clinico-pathological and demographic details and follow-up durations are shown in Table 1. The F:M ratio was 12:3. The mean age of the cohort was 33.4 ± 8.3 years (18–55). The duration of disease as calculated from the history, referral notes and past records was 18.4 ± 12.6 months (3–48). Three of them had nodular goitre and 12 had diffuse hyperplastic goitre on clinical examination. The mean follow-up duration was 17.4 months (12–24). According to WHO grading, 4 patients had grade 1 goitre and 11 had grade 2 and 3 goitres. The mean exophthalmos was 22.1 ± 1.6 mm (19–25). 6/15 (33 %) had associated extra-thyroidal autoimmune disorders with the commonest manifestation being vitiligo. The chronology of ophthalmopathic manifestation in relation to hyperthyroidism was synchronous in 66 %, metachronous in 20 % and prechronous in 14 %. The mean preoperative PFH was 12.67 ± 1.3 mm (11–15).
Table 1.
Clinical and demographic profile of cohort
| S. no. | Sex | Age (years) | Duration of disease (months) | Onset of GAE | Type of GAE | Follow-up (months) |
|---|---|---|---|---|---|---|
| 1 | F | 25 | 8 | Synchronous | Bilateral | 38 |
| 2 | F | 19 | 14 | Synchronous | Unilateral | 36 |
| 3 | F | 31 | 10 | Synchronous | Bilateral | 36 |
| 4 | M | 42 | 24 | Prechronous | Bilateral | 32 |
| 5 | F | 50 | 12 | Synchronous | Bilateral | 32 |
| 6 | F | 38 | 3 | Metachronous | Bilateral | 30 |
| 7 | F | 18 | 12 | Synchronous | Bilateral | 27 |
| 8 | F | 55 | 36 | Synchronous | Bilateral | 26 |
| 9 | F | 44 | 40 | Synchronous | Unilateral | 24 |
| 10 | M | 48 | 24 | Prechronous | Bilateral | 24 |
| 11 | F | 23 | 8 | Synchronous | Bilateral | 21 |
| 12 | M | 21 | 12 | Synchronous | Bilateral | 18 |
| 13 | F | 34 | 18 | Synchronous | Unilateral | 16 |
| 14 | F | 41 | 20 | Prechronous | Bilateral | 15 |
| 15 | F | 29 | 4 | Synchronous | Bilateral | 14 |
Table 2 shows exophthalmopathic regression rates for GAE and PFH at follow-up after total thyroidectomy. The mean postoperative GAE and PFH at the last follow-up was 10.37 ± 0.6 mm (10–11) respectively. 11/15 (73 %) patients showed regression of the exophthalmos with resolution of photophobia, excess lacrimation and symptomatic relief (Fig. 1). Four patients had static exophthalmos but had symptomatic relief. Two patients had initial exacerbation with increased conjunctival injection and pain at 1 and 2 months respectively. They were treated with analgesics and diuretics. But, these exacerbations were self-limiting and not sight threatening. Three subjects had regression of unilateral exophthalmos (Figs. 2 and 3), till the end of the study period. None of the subjects required any corrective lid surgery or orbital decompression. Exophthalmos was measured at two monthly intervals and documented. On the average, regression of GAE and PFH was 2.1 ± 0.5 mm (1–5) and 2.2 ± 0.4 mm (1–4) respectively. The mean regression of GAE was statistically significant at P value = 0.035 on paired-samples t test. The mean regression of PFH was statistically significant at P value = 0.025 on t test.
Table 2.
Clinical course of exophthalmos in relation to thyroidectomy
| No. | Size of presurgery GAE (mm) | Size of postsurgery GAE (mm) | Regression of GAE (mm) | Size of presurgery PFH (mm) | Size of postsurgery PFH (mm) | Regression of PFH (mm) |
|---|---|---|---|---|---|---|
| 1 | 23 | 18 | 5 | 14 | 11 | 3 |
| 2 | 22 | 19 | 3 | 13 | 11 | 2 |
| 3 | 19 | 18 | 1 | 11 | 10 | 1 |
| 4 | 21 | 19 | 2 | 12 | 10 | 2 |
| 5 | 20 | 18 | 2 | 11 | 10 | 1 |
| 6 | 23 | 19 | 4 | 13 | 11 | 2 |
| 7 | 22 | 19 | 3 | 13 | 10 | 3 |
| 8 | 23 | 20 | 3 | 13 | 11 | 2 |
| 9 | 24 | 19 | 5 | 15 | 11 | 4 |
| 10 | 20 | 19 | 1 | 12 | 10 | 2 |
| 11 | 21 | 21 | 0 | 12 | 10 | 2 |
| 12 | 25 | 19 | 4 | 14 | 11 | 3 |
| 13 | 20 | 20 | 0 | 12 | 11 | 1 |
| 14 | 20 | 20 | 0 | 12 | 10 | 2 |
| 15 | 22 | 19 | 3 | 13 | 10 | 3 |
Fig. 1.
Bilateral regression of GAE at last follow-up of 30 months [Markers placed for PFH comparison before (left) and after (right) surgery.]
Fig. 2.
Right eye complete and left eye partial regression of GAE at 15 months follow-up [Markers placed for PFH comparison before (left) and after (right) surgery.]
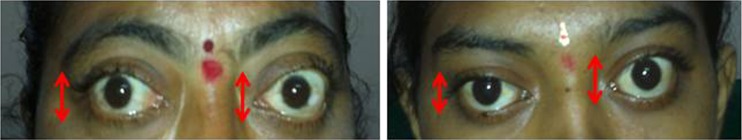
Fig. 3.
Regression of unilateral (left-sided) GAE at 12 months follow-up [Markers placed for PFH comparison before (left) and after (right) surgery.]
Discussion
Graves’ associated ophthalmopathy (GAO) is an autoimmune process with its own clinical course, apart from hyperthyroidism in Graves’ disease [7–9]. GAO can present in various forms such as extra-ocular myopathy, periorbital inflammation, exophthalmos, orbital pain or combination. Depending on the definition, clinical incidence is 10–50 % and radiological incidence based on sensitive orbital imaging is 80–90 % [4, 10]. Exophthalmos is mostly bilateral, though it occurs unilaterally in 10–20 % [11], due to accumulation of glycosaminoglycan and edema within these tissues. GAE is due to retro-orbital and periorbital deposition of glycosaminoglycans within a fibrinoid matrix and edema with or without pseudomuscular hypertrophy of extra-ocular muscles [12].
The natural history of ophthalmopathic exophthalmos is divided into progressive, plateau and resolution phases [13]. Occasionally, GAE can undergo gradual spontaneous resolution. These phases have variable duration and alter with thyroid functional status. Consequently, the natural history of GAE is unpredictable with significant individual variations in severity and duration [5]. In a 12-month follow-up study of GAO, two thirds of the patients had improvement and one third had no change or progression [7]. Despite the presence of scoring systems such as the Werner score, Mouritz score and others [14, 15], exophthalmos is the only reproducibly measurable component of GAO. The clinical activity score especially helps in prognostication of GAO and to an extent in deciding the treatment [15]. The natural course and chronology of the clinical presentation of GAO are extremely variable and unpredictable in an individual case [8]. In 35, 25 and 40 % of cases, GAO presents prechronously, synchronously and metachronously, respectively, compared to the thyrotoxic phase [9]. In our series, the GAO was synchronous in 73 % of cases. One of the reasons for the wide variability in distribution of chronology, natural history and severity could be the definitions used, design of the study and scanty prospective studies of the influence of thyroidectomy.
The onset of GAO and thyrotoxicosis has a close temporal association presenting within 2 years of onset of each other in 80 % of cases [16]. In 70 % of cases GAO improves and 10 % exacerbates and 20 % remains static for a long time. Temporary measures such as diuretics, head-up posture at night, artificial tears, tinted lenses, eyelid taping and abstinence from smoking are employed to protect the cornea and provide symptomatic relief due to exophthalmos [17]. Therapy with orbital radiotherapy, oral steroids, parenteral steroids and immunosuppressive drugs was employed for severe proptosis with variable success [18, 19]. In severe sight-threatening cases with extreme proptosis, surgical orbital decompression may be required. None of our cases required any surgical orbital decompression during the study period.
The cornerstone in the management of GAO is achievement and maintenance of euthyroidism [20], though few studies show that treatment of hyperthyroidism has no effect [21]. The three principal options for ensuring euthyroidism are antithyroid drugs, radioiodine therapy and surgical thyroidectomy, of which the latter two are ablative therapies. Ablative therapies often constitute the definitive therapy for Graves’ disease [22], as the antithyroid drug treatment is associated with side effects, drug non-compliance and higher relapse rates [23]. Moreover, the ablative therapy destroys or removes the thyroid gland, thereby reducing autoimmunity, which could contribute to reversal of autoimmune manifestations. Amongst ablative therapies, radioiodine had more adverse influence on GAO compared to thyroidectomy [21].
GAE is an objectively and reproducibly measurable component of GAO with exophthalmometry. The most common method of its accurate measurement is by Hertel’s exophthalmometry [24]. The upper limits of exophthalmos vary between different ethnic groups with 18 mm for Asians, 20 mm for Caucasians and 22 mm for Africans [25, 26]. Vasanth kumar et al. [27] reported that the ethnic race of South Indians had a maximum PFH compared to Caucasians and Mongolians. Our study shows a mean PFH of 10.37 mm, after regression of GAE (from 12.67 mm). The improvement was statistically significant on t test at 0.04. Though specialized computerized protocols are available for accurate measurement of orbital dimensions, we employed simple objective clinical measurements for wider reproducibility at more clinical units doing similar work. Abrupt alteration in thyroid functional status can be complicated with exacerbation of GAO, often with loss of sight in severe cases [27]. Hypothyroidism is especially associated with exacerbation of ophthalmopathy [28]. In two of our cases, GAO had self-limiting mild exacerbation at 4 and 6 weeks respectively, in spite of maintaining postoperative euthyroidism. The cause of this exacerbation is difficult to explain, though it can be speculated to be part of the natural course of GAO.
Though achievement and maintenance of euthyroidism is an essential component of any management protocol, the natural course of GAO is independent of hyperthyroidism. Surgery has been reported to have a more favourable impact on GAO compared to radioiodine treatment in many studies [20]. Similarly, worsening or progression of GAO appears to be lower with thyroidectomy than medical or ablative therapies [29, 30]. They are mostly retrospective studies and based on scoring systems, which are largely subjective. Most of surgical series involved subtotal thyroidectomy and our study addresses total thyroidectomy. In the absence of a prospective randomized study, treatment of hyperthyroidism per se does not influence the course of GAO in the long run, but short-term impacts such as improvement or progression have been reported in many studies. Our study was prospectively conducted with a focused objective on exophthalmic regression. We have not evaluated the impact of thyroidectomy on the outcome of GAO with non-exophthalmic manifestation. In this study, regression of GAE was observed across all the age groups. The exact cause of this regression is as enigmatic as the etiology of GAO itself. One hypothesis is gradual reduction in levels of TSAb after ablative therapies of thyroidectomy and radioiodine treatment [29]. The strength of this study lies in its prospective design, its objective follow-up of exophthalmos, its design within a surgical series, total thyroidectomy as a surgical choice and scanty studies on this subject from South-Asian countries. The apparent drawbacks are a short-term follow-up, smaller cohort and lack of an intrastudy comparative group with other treatment modalities (radioiodine and antithyroid drugs). More studies with larger cohorts, randomization and a longer follow-up are needed to establish this phenomenon.
Conclusions
Graves’ disease associated exophthalmos regresses in 73 % of cases at 1 year with significant symptomatic relief, after thyroidectomy.
The regression of exophthalmos is statistically significant in responders.
Total thyroidectomy appears to be an ideal management for Graves’ disease associated with opthalmopathic exophthalmos forming additional indication for surgery in toxic goitres.
Acknowledgments
All the authors contributed to this manuscript intellectually, compiling data, drafting the manuscript and treating the subjects involved.
Compliance with Ethical Standards
Informed consent was taken from all the subjects included in the work.
Conflict of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Rees Smith B, MacLachlan SM, Furmaniak J. Autoantibodies to the thyrotropin receptor. Endocr Rev. 1988;9:106–121. doi: 10.1210/edrv-9-1-106. [DOI] [PubMed] [Google Scholar]
- 2.Tunbridge WM, Evered DC, Hall R, Appleton D, Brewis M, et al. The spectrum of thyroid disease in a community: the Whickham survey. Clin Endocrinol (Oxf) 1977;7:481–493. doi: 10.1111/j.1365-2265.1977.tb01340.x. [DOI] [PubMed] [Google Scholar]
- 3.Kochupillai N. Clinical endocrinology in India. Curr Sci. 2000;79:1061–1067. [Google Scholar]
- 4.Forbes G, Gorman CA, Gehring DG, et al. Computer analysis of orbital fat and muscle volumes in Graves’ ophthalmopathy. Am J Neuroradiol. 1983;4:737–742. [PMC free article] [PubMed] [Google Scholar]
- 5.Burch HB, Wartofsky L. Graves’ ophthalmopathy: current concepts regarding pathogenesis and management. Endocr Rev. 1993;14:747–793. doi: 10.1210/edrv-14-6-747. [DOI] [PubMed] [Google Scholar]
- 6.World Medical Organization Declaration of Helsinki. BMJ. 1996;313:1448–1449. [Google Scholar]
- 7.Perros P, Kendall-Taylor P, Crombie AL. Natural history of thyroid associated ophthalmopathy. Clin Endocrinol. 1995;42:45–50. doi: 10.1111/j.1365-2265.1995.tb02597.x. [DOI] [PubMed] [Google Scholar]
- 8.Bartley GB, Gorman CA, Garrity JA, et al. Long term follow-up of Graves ophthalmopathy in an incidence cohort. Ophthalmology. 1996;103:958–962. doi: 10.1016/S0161-6420(96)30579-4. [DOI] [PubMed] [Google Scholar]
- 9.Reed RR. In: Thyroid-associated ophthalmopathy: treatment. Thyroid disease: endocrinology, surgery, nuclear medicine and radiotherapy. 2. Falk SA, editor. Philadelphia: Lippincott-Raven Publishers; 1997. pp. 359–377. [Google Scholar]
- 10.Villadolid MC, Yokoyama N, Izumi M, et al. Untreated GD patients without clinical opthalmopathy demonstrate a high frequency of extraocular muscle (EOM) enlargement by magnetic resonance. J Clin Endocrinol Metab. 1995;80:2830–2833. doi: 10.1210/jcem.80.9.7673432. [DOI] [PubMed] [Google Scholar]
- 11.Wiersinga WM, Smit T, van der Garg R, Mouritis M, Koorneef L. Clinical presentation of Graves’ ophthalmopathy. Ophthalmic Res. 1989;21:73–82. doi: 10.1159/000266782. [DOI] [PubMed] [Google Scholar]
- 12.Riley FC. Orbital pathology in Graves’ disease. Mayo Clin Proc. 1972;47:975–979. [PubMed] [Google Scholar]
- 13.Rundle FF, Wilson CW. Development and course of exophthalmos and ophthalmoplegia in Graves’ disease with special reference to the effect of thyroidectomy. Clin Sci. 1945;5:177–194. [PubMed] [Google Scholar]
- 14.Werner SC. Modification of the classification of the eye changes of Graves’ disease: recommendations of the Ad Hoc Committee of the American Thyroid Association. J Clin Endocrinol Metab. 1977;44:203–244. doi: 10.1210/jcem-44-1-203. [DOI] [PubMed] [Google Scholar]
- 15.Mouritz MP, Koorneef L, Wiersinga WM, et al. Clinical criteria for the assessment of disease activity in Graves’ ophthalmopathy: a novel approach. Br J Ophthalmol. 1989;73:639. doi: 10.1136/bjo.73.8.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gorman CA. Temporal relationship between onset of Graves’ ophthalmopathy and diagnosis of thyrotoxicosis. Mayo Clin Proc. 1983;58:515–519. [PubMed] [Google Scholar]
- 17.Hegedus L, Brix TH, Vestergaard P. Relationship between cigarette smoking and Graves’ ophthalmopathy. J Endocrinol Investig. 2004;27:265–271. doi: 10.1007/BF03345276. [DOI] [PubMed] [Google Scholar]
- 18.Wiersinga W, Prummel MF. Therapeutic controversies. Retrobulbar radiation in Graves’ ophthalmopathy. J Clin Endocrinol Metab. 1995;80:345–347. doi: 10.1210/jcem.80.2.7852487. [DOI] [PubMed] [Google Scholar]
- 19.Prummel MF, Mouritz MP, Berghout A, et al. Prednisone and cyclosporine in the treatment of severe Graves’ ophthalmopathy. N Engl J Med. 1989;321:1353–1359. doi: 10.1056/NEJM198911163212002. [DOI] [PubMed] [Google Scholar]
- 20.Frilling A, Goretzki PE, Grussendorf M, Erbsloh M, Roher HD. The influence of surgery on endocrine ophthalmopathy. World J Surg. 1990;14:442–446. doi: 10.1007/BF01658552. [DOI] [PubMed] [Google Scholar]
- 21.Tallstedt L, Lundell G, Torring O, Wallin G, et al. Occurrence of ophthalmopathy after treatment for Graves’ hyperthyroidism. N Engl J Med. 1992;326:1733–1738. doi: 10.1056/NEJM199206253262603. [DOI] [PubMed] [Google Scholar]
- 22.Marushak D, Faurschon S, Blichet-Toft M. Regression of ophthalmopathy in Graves’ disease following thyroidectomy. Acta Ophthalmol (Copenh) 1984;82:767–779. doi: 10.1111/j.1755-3768.1984.tb05805.x. [DOI] [PubMed] [Google Scholar]
- 23.Laurberg P, Bulow Pedersen I, Pedersen KM, et al. Goiter size and outcome of medical treatment of Graves’ disease. Acta Endocrinol (Copenh) 1986;111:39–43. doi: 10.1530/acta.0.1110039. [DOI] [PubMed] [Google Scholar]
- 24.Mourits MP, Lombardo SH, van der Sluijs FA, Fenton S. Reliability of exophthalmos measurement and the exophthalmometry value distribution in a healthy Dutch population and in Graves’ patients. An exploratory study. Orbit. 2004;23:161–168. doi: 10.1080/01676830490504089. [DOI] [PubMed] [Google Scholar]
- 25.Amino N, Yuasa T, Yabu Y, et al. Exophthalmos in autoimmune thyroid disease. J Clin Endocrinol Metab. 1980;51:1232–1234. doi: 10.1210/jcem-51-6-1232. [DOI] [PubMed] [Google Scholar]
- 26.Migliori ME, Gladstone GJ. Determination of the normal range of exophthalmometric values for black and white adults. Am J Ophthalmol. 1984;98:438–442. doi: 10.1016/0002-9394(84)90127-2. [DOI] [PubMed] [Google Scholar]
- 27.Vasanthakumar P, Kumar P, Rao M. Anthropometric analysis of palpebral fissure dimensions and its position in South Indian ethnic adults. Oman Med J. 2013;28:26–32. doi: 10.5001/omj.2013.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stan MN, Durski JM, Brito JP, Bhagra S, Thapa P, Bahn RS. Cohort study on radioactive iodine-induced hypothyroidism: implications for Graves’ ophthalmopathy and optimal timing for thyroid hormone assessment. Thyroid. 2013;23:620–625. doi: 10.1089/thy.2012.0258. [DOI] [PubMed] [Google Scholar]
- 29.De Bellis A, Conzo G, Cennamo G, Pane E, Bellastella G, Colella C, et al. Time course of Graves’ ophthalmopathy after total thyroidectomy alone or followed by radioiodine therapy: a 2-year longitudinal study. Endocrine. 2012;41:320–326. doi: 10.1007/s12020-011-9559-x. [DOI] [PubMed] [Google Scholar]
- 30.Sisson JC, Schipper MJ, Nelson CC, Freitas JE, Frueh BR. Radioiodine therapy and Graves’ ophthalmopathy. J Nucl Med. 2008;49:923–930. doi: 10.2967/jnumed.107.049437. [DOI] [PubMed] [Google Scholar]