Abstract
Background and objective
Patients with anteromedial arthritis who require a knee replacement could receive either a unicompartmental knee replacement (UKR) or a total knee replacement (TKR). This review has been undertaken to identify economic evaluations comparing UKR and TKR, evaluate the approaches that were taken in the studies, assess the quality of reporting of these evaluations, and consider what they can tell us about the relative value for money of the procedures.
Methods
A search of MEDLINE, EMBASE and the Centre for Reviews and Dissemination National Health Service Economic Evaluation Database was undertaken in January 2016 to identify relevant studies. Study characteristics were described, the quality of reporting and methods assessed using the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist, and study findings summarised.
Results
Twelve studies satisfied the inclusion criteria. Five were within-study analyses, while another was based on a literature review. The remaining six studies were model-based analyses. All studies were informed by observational data. While methodological approaches varied, studies generally had either limited follow-up, did not fully account for baseline differences in patient characteristics or relied on previous research that did not. The quality of reporting was generally adequate across studies, except for considerations of the settings to which evaluations applied and the generalisability of the results to other decision-making contexts. In the short-term, UKR was generally associated with better health outcomes and lower costs than TKR. Initial cost savings associated with UKR seem to persist over patients’ lifetimes even after accounting for higher rates of revision. For older patients, initial health improvements also appear to be maintained, making UKR the dominant treatment choice. However, for younger patients findings for health outcomes and overall cost effectiveness are mixed, with the difference in health outcomes depending on the lifetime risk of revision and patient outcomes following revision.
Conclusions
UKR appears to be less costly than TKR. For older patients, UKR is also expected to lead to better health outcomes, making it the dominant choice; however, for younger patients health outcomes are more uncertain. Future research should better account for baseline differences in patient characteristics and consider how the relative value of UKR and TKR varies depending on patient and surgical factors.
Key Points for Decision Makers
| Twelve economic evaluations comparing unicompartmental knee replacement (UKR) with total knee replacement (TKR) were identified and analysed. |
| Model-based analysis best captured the different factors relevant to the choice between UKR and TKR. Studies were limited by either small sample sizes or not accounting for baseline differences in patient characteristics. |
| UKR appears to offer a less costly alternative to TKR, and also seems to lead to better health outcomes for older patients. Uncertainty surrounds the difference in health outcomes for younger patients, which depends on a patient’s lifetime risk of revision, and health outcomes following a revision. |
Introduction
For patients with end-stage osteoarthritis (OA) of the knee, total knee replacement (TKR) provides a highly effective treatment strategy associated with significant improvements in pain, function and quality of life [1, 2]. When compared with nonsurgical treatments, TKR has been found to be highly cost effective [3, 4]. However, for those patients with OA predominantly in only one compartment of the knee, unicompartmental knee replacement (UKR) offers an alternative approach, where only the diseased cartilage in an isolated part of the joint is replaced [5].
The choice between UKR and TKR is not clear-cut. While UKR is associated with a significantly reduced risk of postoperative complications and mortality as well as better functional and general health outcomes after 6 months, [6, 7] UKR is also associated with a higher rate of implant revision than TKR [6]. Although a primary UKR can be expected to be cheaper than a TKR, given a shorter hospital stay, the costs associated with revisions and any other differences in future healthcare utilisation could outweigh any short-term cost saving.
An economic evaluation can provide a means of informing the choice between UKR and TKR by providing a comparative analysis of the alternative courses of action in terms of both their costs and health outcomes [8]. For an economic evaluation of UKR and TKR to be useful, it needs to use appropriate methods so that its results are valid [8]. Given that evaluations address a question relevant to a place and setting, [9] decision makers also need to be able to consider whether the results apply to their decision-making context [8].
This review has been undertaken to identify economic evaluations comparing UKRs and TKRs, examine the approaches taken, assess the quality of these evaluations, and consider what they can tell us about the relative value for money of the procedures.
Methods
Eligibility Criteria
Economic evaluations including both UKR and TKR as treatment options for primary knee arthroplasty were eligible for this review. While primary UKR and TKR were required to be specified as treatment options, studies could also include additional treatment alternatives. No restrictions were imposed on the study populations.
Only full economic evaluations, in which both the costs and health outcomes of the alternative courses of action are estimated, [8] could be included. Any type of economic evaluation could have been undertaken, hence while costs were expected to be expressed in monetary terms, health outcomes could be measured in terms of a common unit of clinical effect (a cost-effectiveness analysis), a generic measure of health gain (a cost-utility analysis) or in monetary units (a cost-benefit analysis).
No restriction was placed on the date of publication but studies were required to be written in English. The review was conducted as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and the review protocol was registered prospectively with the PROSPERO database (registration number: CRD42015026664) [10].
Study Selection
Searches were undertaken in January 2016 of MEDLINE and EMBASE, using the OVID platform, and the Centre for Reviews and Dissemination National Health Service Economic Evaluation Database (NHS EED), which contains critical overviews of economic evaluations. The specific search terms used are detailed in the “Appendix”. Two of the authors (EB and SP) independently screened studies for inclusion based on their titles, with only those clearly not eligible being excluded, and then based on abstracts, with any discrepancies resolved by a third author (RPV). Two authors (EB and RPV) then screened the full texts of the remaining studies against the inclusion criteria and discrepancies were resolved through consensus discussion.
Analysis of Included Studies
Economic evaluations were grouped by the type of analytical frameworks used to inform decision making. A within-study analysis uses a single study as the vehicle for economic analysis, [11] with data collected within the study used to estimate costs and health outcomes. A literature review study identifies and compares estimates of health outcomes and costs from disparate research, while a model-based analysis defines a set of mathematical relationships to characterise the range of possible prognoses and the impact of the alternative interventions [8].
The key characteristics of the included studies are summarised. The ages of the study populations and the interventions considered are noted, and the time horizon of analysis, over which costs and health outcomes where estimated, are recorded. The measures of overall health outcomes are detailed. The costing perspectives are also identified, with studies considering costs from a patient, hospital, payer, health system, government or societal perspective, and only those costs of relevance to the given perspective considered in an analysis.
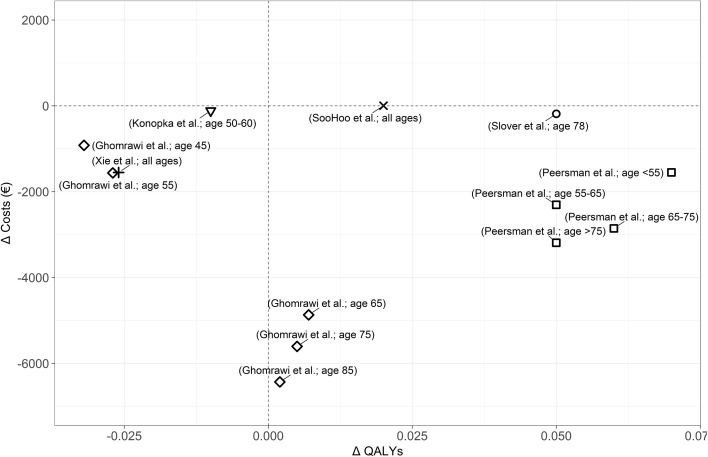
Subsequently, findings relating to UKR and TKR are compared. Estimates of the difference in costs and outcomes between UKR and TKR are summarised. The incremental cost-effectiveness ratio (ICER), given by the difference in cost divided by the difference in health outcome, is detailed for studies that express health outcomes in terms of quality-adjusted life-years (QALYs), which provide a generic measure of health capturing both quality and quantity of life. Where one alternative is both cost saving and health improving, it is considered to be the dominant treatment option. In addition, the difference in costs and QALYs associated with undertaking UKR rather than TKR are presented on a cost-effectiveness plane. For this figure, costs were transformed into 2015 Euros by first inflating costs in the original currency to 2015 prices using Consumer Price Index (CPI) indices and then converted to Euros using official exchange rates [12].
The methodological approaches of the studies are discussed. The specification of the decision problem, in terms of the choice of study population and treatment options, is assessed. The way in which estimates of effectiveness were derived are examined, with potential sources of bias identified. Factors relevant to the choice between UKR and TKR included in the studies are considered. In particular, attention is paid as to whether pain, function, or quality of life and risk of revision were assessed when summarising health outcomes, and whether the cost of the primary procedure and revision procedures were incorporated into the estimates of the overall costs.
The quality of reporting for each study is assessed using the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist, which represents a set of reporting standards for health economic studies [9]. For each study, items on the CHEERS checklist were assessed as having been satisfied, partially satisfied, not satisfied, or not applicable.
Results
Overview of Included Studies
Twelve studies were included in the review [13–24]. A flowchart of the screening process is provided in the Appendix, and the key characteristics of the included studies and the decision-making factors that they considered are detailed in Tables 1 and 2, respectively. Estimates of changes in costs and QALYs associated with the provision of UKR rather than TKR are presented on a cost-effectiveness plane (Fig. 1).
Table 1.
Overview of the included studies
| Author | Countrya | Interventions considered | Age limits for study population, years | Time horizona | Measure of health benefit | Costing perspectivea | Health outcomesb | Costsb | ICERb |
|---|---|---|---|---|---|---|---|---|---|
| Within-study analyses | |||||||||
| Koskinen et al. [15] | Finland | UKR vs. TKR | None | 15 years | Implant survival | Hospital | UKR had a 20 percentage point lower survival rate after 15 years | TKR had a lower cost (amount not specified) | NA |
| Manzotti et al. [16] | Italy | UKR vs. computer-assisted TKR | >60 | 3 years | Multiple outcomesc | Hospital | UKR resulted in superior results | UKR led to a cost saving of 3100 (Euros, year not specified) | NA |
| Robertsson et al. [19] | Sweden | UKR vs. TKR | None | 10 years | Implant survival | Hospital | UKR had a 4 percentage point lower survival rate after 10 years | UKR had a lower cost (amount not specified) | NA |
| Xie et al. [23] | Singapore | UKR vs. TKR | None | 2 years | QALYs | Societal, patient and government | UKR led to 0.026 fewer QALYS | UKR led to a cost saving of 1689, 1564 and 125 (US dollars, 2008) from a societal, patient and government perspective, respectively | TKR expected to cost 65245, 60382 and 4860 per QALY gained from a societal, patient and government perspective, respectively |
| Yang et al. [24] | Singapore | UKR vs. TKR | >50 | Six months | Multiple outcomesc | Hospital | UKR resulted in superior results | UKR expected to lead to a cost saving of 3300 (Singapore dollars, year not specified) | NA |
| Literature review | |||||||||
| Marcacci et al. [17] | Italy | KineSpring vs. UKR vs. TKR vs. HTO vs. conservative nonsurgical treatment | None | Lifetime | QALYs | Hospital | UKR and TKR assumed to result in equivalent outcomes | UKR led to a cost saving of 800 (Euros, year not specified) | UKR to be cost saving compared with TKR, with the same health outcomes |
| Decision model analyses | |||||||||
| Ghomrawi et al. [13] | US | UKR vs. TKR | Cohorts aged 45, 55, 65, 75, and 85 | Lifetime | QALYs | Societal | UKR to lead to 0.032 and 0.027 fewer QALYs for those aged 45 and 55 years, but 0.007, 0.005 and 0.002 more QALYs for those aged 65, 75 and 85 years | UKR to lead to a cost saving of 1000, 1700, 5300, 6100 and 7000 (US dollars, 2012) for those aged 45, 55, 65, 75 and 85 years, respectively | TKR to cost 30300 and 63000 per QALY gained for those aged 45 and 55 years. UKR expected to be dominant 65, 75 and 85 years |
| Konopka et al. [14] | US | UKR vs. TKR vs. HTO | 50–60 | Lifetime | QALYs | Health system | UKR to lead to 0.01 fewer QALYS | UKR to lead to a cost saving of 124 (US dollars, 2012) | TKR to cost 12400 per QALY gained |
| Peersman et al. [18] | Belgium | UKR vs. TKR | Cohorts aged <55, 55–65, 65–75, >75 | Lifetime | QALYs | Payer | UKR to lead to 0.07, 0.05, 0.06 and 0.05 more QALYs for those aged <55, 55–65, 65–75 and >75 years | UKR to lead to a cost saving of 1565, 2327, 2883 and 3220 (Euros, 2014) for those aged <55, 55–65, 65–75 and >75 years | UKR to be dominant for all age subgroups |
| Slover et al. [20] | US | UKR vs. TKR | 78 | Lifetime | QALYs | Payer | UKR to lead to 0.05 more QALYS | UKR to lead to a cost saving of 200 (US dollars, 2005) | UKR to be dominant |
| SooHoo et al. [21] | US | UKR vs. TKR | None | Lifetime | QALYs | Societal | UKR to lead to 0.02 more QALYS | UKR to lead to an increased cost of 5 (US dollars, 1998) | UKR to cost 277 per QALY gained |
| Willis-Owen et al. [22] | UK | UKR vs. TKR | None | 1 year | TKQ | Hospital | UKR led to a better TKQ score | UKR led to a cost saving of 1761 (British pounds, year not specified) | NA |
TKQ Total Knee Questionnaire, QALYs quality-adjusted life-years, HTO high tibial osteotomy, UKR unicompartmental knee replacement, TKR total knee replacement, ICER incremental cost-effectiveness ratio, NA not applicable
a Implied if not explicitly stated
b UKR compared with TKR
c Included functional outcomes, length of hospital stay, and surgical complications
Table 2.
Decision-making factors considered
| Author | Pain, function, or overall quality of life | Risk of revision | Cost of primary procedures | Cost of revisions |
|---|---|---|---|---|
| Within-study analysis | ||||
| Koskinen et al. [15] | ✘ | ✔ | ✔ | ✔ |
| Manzotti et al. [16] | ✔ | ✘ | ✔ | ✘ |
| Robertsson et al. [19] | ✘ | ✔ | ✔ | ✔ |
| Xie et al. [23] | ✔ | ✘ | ✔ | ✘ |
| Yang et al. [24] | ✔ | ✘ | ✔ | ✘ |
| Literature review | ||||
| Marcacci et al. [17] | ✔ | ✘ | ✔ | ✘ |
| Decision model | ||||
| Ghomrawi et al. [13] | ✔ | ✔ | ✔ | ✔ |
| Konopka et al. [14] | ✔ | ✔ | ✔ | ✔ |
| Peersman et al. [18] | ✔ | ✔ | ✔ | ✔ |
| Slover et al. [20] | ✔ | ✔ | ✔ | ✔ |
| SooHoo et al. [21] | ✔ | ✔ | ✔ | ✔ |
| Willis-Owen et al. [22] | ✔ | ✔ | ✔ | ✔ |
Fig. 1.
Cost-effectiveness plane with study findings. Only those studies that used QALYs as a health outcome are included. The horizontal axis represents the difference in expected QALYs following UKR and TKR (∆ QALYs = UKR QALYs−TKR QALYs); the vertical axis represents the difference in expected costs (∆ Costs = UKR cost–TKR cost). Study author and age group considered are in parentheses
Within-Study Analyses
Five publications used a within-study analysis as their framework of analysis [15, 16, 19, 23, 24]. Each of these studies was observational and compared the costs and health outcomes of patients who received UKR or TKR. The study populations were similar across studies and appropriate for those receiving the alternative procedures. To be a candidate for either UKR or TKR individuals are required to have OA in one compartment of the knee, to have previously failed nonsurgical treatment, and to have symptoms that had a substantial impact on their quality of life [25]; these were generally the characteristics of the patients described in the studies. While four studies imposed no age restriction for patients to be included in the study, one included only those older than 50 years of age, [24] while another assessed only those over 60 years of age [16].
Two studies considered multiple peri- and postoperative health outcomes for UKR and TKR up to 3 years following the procedures [16, 24]. Outcomes considered included blood loss during surgery, days required for independent ambulation, knee flexion, and knee-specific patient-reported outcome measures, such as the Knee Society score. In both studies, UKRs were matched with comparable TKRs. In one study, 34 UKRs were matched with 34 TKRs on the basis of preoperative arthritis severity, range of motion, age and sex [16], while in the other study, 50 UKRs were matched with 50 TKRs, but no details of the matching mechanism were provided [24]. Both studies found UKR to achieve better outcomes across all measures considered. In addition, taking a hospital perspective, the studies considered only the costs of primary procedures [16, 24], and found UKR to have a lower cost than TKR.
Another study compared quality of life associated with receiving UKR and TKR, measured using the Short-Form (SF)-36 questionnaire [23]. Scores recorded preoperatively and 6 and 24 months postoperatively were used to estimate individual’s QALYs over the 2 years following surgery. It was estimated that TKR would lead to a greater number of QALYs than UKR. The discrepancy with this finding compared with those of the previous studies that considered condition-specific measures of outcome is likely to be, at least in part, because this study did not appear to control for baseline differences between those receiving UKR and TKR. Only the costs of the primary procedures were considered in this analysis and, again, UKR was found to be cost saving compared with TKR. With this study considering costs from a government and societal perspective, excluding the costs of revision is likely inappropriate.
The two remaining studies assessed the risk of revision following UKR and TKR over 10 and 15 years using data from national arthroplasty registers [15, 19]. One study did not control for differences in the baseline characteristics of those receiving UKR and TKR [15], while the other controlled for age, gender and year of operation [19]. Both found UKR to be associated with a greater risk of revision, however these estimates varied significantly. In one, UKR was expected to have a 4 percentage point lower survival rate after 10 years, [19] while in the other, UKR was estimated to have a 20 percentage point lower survival rate after 15 years [15]. Nonetheless, this use of revision rates as a health outcome may be misleading as revision of a UKR is more straightforward than revision of a TKR. As a result, UKRs are between four and six times more likely to be revised than a TKR, with the same functional outcome [26]. Both studies incorporated the cost of revision when estimating the costs of the alternative procedures. While the study that estimated a smaller difference in risk of revision found UKR to be cost saving compared with TKR, [19] the study that estimated a greater differential in revision rates found the costs of revisions to outweigh any initial savings associated with UKR [15].
The analyses were generally well-reported, with most items on the CHEERS checklist either partially or fully satisfied (see Sect. 6). The interventions being compared and the studies on which they were based were generally well reported, with the outcomes and costs described. However, no study discussed why the analysis used was sufficient to inform an economic evaluation of UKR and TKR. In addition, studies did not fully describe the setting to which the study applied, or discuss the generalisability of their findings.
Literature Review Study
One study was informed by a literature review from which estimates of health outcomes and costs were identified and compared [17]. Five alternative treatments were considered, with the KineSpring implant system (Moximed, Inc., Hayward, CA, USA), an extra-articular device designed to reduce the load on the knee joint [17], compared against UKR, TKR, high tibial osteotomy (HTO) and conservative nonsurgical treatment. The patient population to which the analysis applied was not described in detail. Nonetheless, the comparison of these alternative courses of action in this study is likely inappropriate. For example, candidates for UKR and TKR would be expected to have received and failed nonsurgical treatments [27]. Consequently, comparing the outcomes of these treatments is unlikely to be informative as it does not reflect the choice faced in reality.
In this study, UKR and TKR were grouped together as surgical procedures. It was assumed that both procedures would lead to the same health outcomes, in terms of QALYs. The effect of revisions on health outcomes was not considered. With only the costs of the primary procedures considered in this analysis, as with similar within-study analyses, UKR was estimated to be cost saving compared with TKR.
This study mostly partially satisfied items on the CHEERs checklist (see Sect. 6). The alternative treatments considered were well-described; however, the rationale for comparing them was not discussed. In addition, while the studies included in the analysis were reported, the process by which they were identified was not described in detail.
Model-Based Analyses
Six studies used decision-analytic models as the framework for analysis [13, 14, 18, 20–22]. Five of the studies compared UKR with TKR, [13, 18, 20–22], while one study also included HTO as a further treatment option [14]. While two studies did not specify any age restriction [21, 22], one study considered only those aged between 50 and 60 years [14], and another was based on those aged 78 years [20]. The remaining two studies estimated costs and health outcomes for a number of subgroups based on age [13, 18]. All of these model-based analyses incorporated each of the key decision-making factors relevant to the choice between UKR and TKR (see Table 2).
Two studies used decision trees [21, 22], in which branches represent possible future treatment pathways. Neither study imposed any age restriction on the study populations that they considered. In one study, a decision tree was only used to estimate costs; with the costs of revisions in the year after surgery incorporated, UKR was found to be cost saving compared with TKR. Meanwhile, health outcomes were measured postoperatively using the Total Knee Questionnaire (TKQ), with 20 UKRs matched with 20 TKRs on age and sex [22]. In line with the matched within-study analyses, UKR was found to lead to better postoperative scores than TKR. The other study used a decision tree to estimate costs and health outcomes, in terms of QALYs, over the remaining lifetimes of patients. As time is not explicitly modelled in decision trees, it was assumed that implant failure would occur for all patients 12 years following a UKR and 15 years following a TKR [21]. This is likely a significant oversimplification, with the risk of revision continuous over time and a proportion of patients who are likely to never require a revision. UKR was estimated to lead to a greater number of QALYs than TKR [21]. In addition, with all patients expected to require a revision, UKR was also expected to be marginally more costly than TKR [21]. UKR was expected to be cost effective, with the estimated health gain justifying the additional cost.
The four remaining model-based analyses were each informed by state-based Markov models [13, 14, 18, 20], which do allow time to be explicitly modelled. Across all of the Markov models, as time progresses patients could remain either unrevised or have a revision. Costs and health outcomes, in terms of QALYs, are estimated over the remaining lifetimes of patients. Two studies allowed for one revision following UKR and TKR [13, 20], one allowed for up to two revisions following both procedures [18], and no limit was placed on the number of revisions in another study [14]. In all cases, UKR was expected to be cost saving [13, 14, 18, 20]. Where health outcomes for patients aged 65 years and over were estimated [13, 18, 20], UKR was also expected to lead to better health outcomes than TKR, making it the dominant treatment option. However, findings for health outcomes and, in turn, cost effectiveness were mixed for younger patients. While, in one study, UKR was expected to lead to a gain in QALYs compared with TKR for those under 65 years of age [18], in another study TKR was expected to lead to better health outcomes for those between 50 and 60 years of age [14], while another study estimated that TKR would lead to better health outcomes for patients aged 45 and 55 years [13]. The contrasting estimates appear to be driven by both differences in estimates for the risk of revision and, in particular, the expected effect of revision on quality of life. While the study that found UKR to be health improving assumed that a revision of UKR would lead to quality of life equivalent to that following a primary TKR [13], the other studies expected that quality of life following revision of a UKR would either be equivalent to that following revision of a TKR [13] or between that of a primary TKR and revision of a TKR [14].
Each of the models required estimates for risk of revision following UKR and TKR. National arthroplasty registries were used in four of the studies [13, 18, 20, 22]. In each of these it appears that the rates of revision for those receiving UKR and TKR were compared, with no adjustment made for differences in baseline characteristics. In the two other studies, estimates were derived by a literature review [14, 21].
The items on the CHEERS checklist were mostly either partially or fully satisfied. The model structures were typically described in detail, but the way in which model inputs were estimated was generally not fully explained. Meanwhile, although costs were reported in detail, the approaches used to estimate costs, in particular when provided by hospital administrators, were not fully described.
Discussion
A large proportion of individuals who require knee replacement are suitable for either TKR or UKR. Substantial uncertainty exists around the identification of patients for whom UKR or TKR is most appropriate, and significant variation has been observed in treatment choice [28, 29]. While both operations have been practiced for over 30 years, controversy remains over which is the most suitable intervention. UKR is associated with lower rates of early complications, morbidity and mortality, and superior patient-reported outcomes, but TKR is associated with a significantly lower risk of revision [6]. Economic evaluations provide a method of reducing any unwarranted variation in surgical choice by providing a systematic consideration of both the costs and health outcomes associated with each procedure.
This review identified 12 economic evaluations that have compared the costs and health outcomes of TKR and UKR. Five within-study analyses and one study based on a literature review provide a partial consideration of the costs and health outcomes associated with the procedures, with their focus generally either on perioperative and early postoperative outcomes or long-term revision rates. Six decision-analytic models provided a broader consideration of health outcomes and costs, incorporating each of the key factors for decision making. In particular, four studies that used state-based Markov models were able to consider costs and health outcomes over the remaining lifetimes of patients following UKR and TKR.
The studies included in this review differed in time horizons of analysis, study design, outcome measures and costing perspectives. While methodological approaches varied, studies generally had either limited follow-up, did not fully account for baseline differences in patient characteristics, or were informed by on previous research that did not. The quality of reporting was generally adequate across the included studies, except for considerations of the settings to which evaluations applied and the generalisability of the results to other decision-making contexts. This makes it difficult for decision makers to know whether results apply to their setting.
In the short-term, based on the economic evaluations considered in this study, UKR appears to be associated with better peri- and postoperative outcomes than TKR. Better early outcomes for UKR have also been observed for routine practice in the UK [6, 7], and are even more pronounced for UKRs performed by high-usage and high-volume surgeons [30]. Moreover, as would be expected given a lower length of stay, UKR is also estimated to offer an immediate cost saving compared with TKR.
This initial cost saving associated with UKR seems to be maintained over patients’ lifetimes, even after accounting for higher risk of revision. For older patients, initial health improvements also appear to be maintained, even after taking into account the higher risk of revision associated with UKR. However, for younger patients with a greater lifetime risk of revision, findings are mixed for health outcomes and the cost effectiveness of the procedures. Differences in both the estimates of revision risk and the consequences associated with revisions appear to drive this uncertainty. In particular, assumptions around quality of life following revision of a UKR appear to be key. Research findings are mixed as to how revision of a UKR compares with that of a primary TKR [31–33]. Additional research is required to better understand patients’ lifetime risk of revision and the consequences of revisions.
As well as age, a number of other patient characteristics have been found to be associated with differences in outcomes following knee replacement, such as sex, weight, and severity of symptoms [27, 34]. Surgical factors such as surgeon grade, their caseload, and the number of cases performed by the unit per year have also been found to be associated with implant survival [34, 35]. Differences in factors such as these could also influence the relative merits of the procedures, but none of the studies identified here considered how the cost effectiveness of UKR and TKR varies based on any factor other than age.
Further research is required to establish the cost effectiveness of UKR and TKR, and how this varies depending on patient and surgical factors. National registries, in particular, provide a rich source of information, capturing real-world outcomes with relatively long-term follow-up, which are of critical importance for these procedures. If based on such data, studies should utilise methods for addressing potential bias, such as regression analysis or matching estimators, to better estimate treatment effects [36]. In addition to the numerous sources of observational data, a large randomised controlled trial comparing UKR and TKR is currently underway [37]. While this study will provide valuable insight into the procedures by ascertaining more comprehensively their costs and health outcomes, data from observational studies will also be needed to better understand the long-term effects of the procedures.
Limitations of this Review
A systematic approach was taken to identify studies that have considered the costs and health outcomes associated with UKR and TKR; however, there does remain the possibility that relevant studies were not identified and included in the study. While MEDLINE, EMBASE and NHS EED were searched, searches of additional databases, such as the Health Economic Evaluations Database (HEED) may have returned more results. The search filter used was designed specifically for this study and has not previously been validated. In addition, while the terms used were chosen to find appropriate results from both databases, searching MEDLINE and EMBASE together using the OVID platform may have led to missing studies, given the distinct characteristics of these databases.
The descriptions of the included studies provide an objective overview of the economic evaluations that have been undertaken of UKR and TKR and their findings but the analysis of the methods used and quality of reporting is necessarily subjective. While an established checklist was used to consider the quality of reporting, categorising studies as satisfying, partially satisfying, or not satisfying particular items was necessarily based on the judgement of the authors of this study.
As well as comparing the approaches taken, the key findings of the studies have also been compared. Any such comparison should be treated with caution due to methodological limitations of the studies and the wide range of factors that limit the generalisability of results across economic evaluations [38]. In particular, cost estimates can vary across studies due to differences in costing perspectives of the studies and in health systems. In addition, converting costs from one currency to another adds further uncertainty [12]. However, a comparison of findings was still felt to be merited so as to provide a broad summary of the consistency in research findings and to provide an indication of the effect of differences in methodological approaches on results. Identifying such sources of variation across studies can help individual decision makers determine which studies best apply to their particular settings, and can guide future research [39].
Conclusions
The economic evaluations of UKR and TKR that have been undertaken vary, with differences in study populations and methods of analysis. In the short-term, UKR appears to be both health improving and cost saving compared with TKR. This initial cost saving associated with UKR seems to persist, even after accounting for higher rates of revision over patients’ lifetimes. For older patients, UKR can also be expected to lead to better overall health outcomes, making it the dominant treatment choice. However, for younger patients, findings are mixed, with differences in estimates of the risk of revision and outcomes following revision leading to substantial differences in estimates of overall health outcomes.
To estimate all the costs and health outcomes associated with the choice between UKR and TKR, future research should incorporate long-term time horizons and estimates of effectiveness adjusted for baseline differences in patient characteristics. Further economic evaluations are required to better understand how the relative value of the procedures varies depending on patient and surgical factors.
Appendix
Search Terms
Search terms for Medline and Embase via Ovid SP
Exp Knee Joint/
Knee/
Knee.tw.
Arthroplasty, Replacement, Knee/
Knee Prosthesis/
(Knee arthroplast$ or knee replacement or knee prosthes$).tw.
(Uka or unicompartmental knee arthroplast$).tw.
Unicompartmental.tw.
Economics/
Exp “costs and cost analysis”/
Exp economics, hospital/
Economics, Medical/
Economics, Nursing/
Economics, Pharmaceutical/
(Economic$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab.
(Expenditure$ not energy).ti,ab.
Value for money.ti,ab.
Budget$.ti,ab.
1 or 2 or 3
4 or 5 or 6 or 7 or 8
9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
19 and 20 and 21
NHS EED, via The Cochrane Library
MeSH descriptor: [Arthroplasty, Replacement, Knee] explode all trees
MeSH descriptor: [Osteoarthritis, Knee] explode all trees
MeSH descriptor: [Knee Joint] explode all trees
Knee/
Knee prosthesis
Knee arthroplasty
Knee replacement
Uka
Unicompartmental
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9
Screening Results
Satisfaction of the CHEERS checklist
| Within-study analysis | Literature review | Decision model | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Koskinen et al. [14] | Manzotti et al. [15] | Robertsson et al. [18] | Willis-Owen et al.[21] | Xie et al. [22] | Yang et al. [23] | Marcacci et al. [16] | Ghomrawi et al. [12] | Konopka et al. [13] | Peersman et al. [17] | Slover et al. [19] | SooHoo et al. [20] | |
| Title | + | ± | ± | + | + | ± | ± | + | ± | + | + | + |
| Abstract | ± | ± | ± | ± | ± | ± | ± | ± | ± | + | ± | ± |
| Background and objectives | ± | ± | ± | ± | ± | ± | + | + | ± | + | + | ± |
| Target population and subgroups | ± | + | ± | ± | + | + | ± | ± | + | ± | + | ± |
| Setting and location | ± | − | ± | − | − | − | ± | − | − | ± | − | − |
| Study perspective | − | − | − | + | + | − | + | + | ± | + | − | + |
| Comparators | ± | + | + | + | + | + | + | ± | + | + | + | + |
| Time horizon | ± | ± | − | − | ± | ± | ± | + | ± | + | + | + |
| Discount rate | − | − | − | − | + | − | − | + | ± | + | + | + |
| Choice of health outcomes | ± | ± | ± | ± | ± | ± | ± | ± | + | ± | ± | ± |
| Measurement of effectiveness | ± | ± | ± | ± | ± | ± | ± | ± | ± | ± | ± | ± |
| Measurement and valuation of preference-based outcomes | NA | NA | NA | NA | + | NA | ± | + | ± | ± | + | ± |
| Estimating resources and costs | ± | ± | + | ± | + | − | ± | ± | + | ± | + | + |
| Currency, price date, conversion | + | ± | + | ± | + | ± | ± | + | + | + | + | + |
| Choice of model | NA | NA | NA | ± | NA | NA | NA | ± | + | ± | ± | ± |
| Model assumptions | NA | NA | NA | ± | NA | NA | NA | + | + | + | + | ± |
| Analytic methods | ± | ± | ± | ± | + | ± | ± | + | + | ± | ± | ± |
| Study parameters | ± | + | + | ± | + | + | ± | ± | + | ± | ± | ± |
| Incremental costs and outcomes | + | ± | + | + | + | ± | ± | + | + | ± | + | ± |
| Characterising uncertainty | − | ± | ± | ± | ± | − | − | ± | + | + | + | ± |
| Characterising heterogeneity | − | NA | − | − | − | − | − | + | NA | + | NA | NA |
| Discussion | ± | ± | ± | ± | ± | ± | ± | ± | ± | ± | ± | ± |
| Source of funding | − | − | ± | − | − | − | ± | + | + | ± | ± | + |
| Conflicts of interest | + | − | − | + | − | − | − | + | + | + | + | − |
CHEERS Consolidated Health Economic Evaluation Reporting Standards, NA not applicable, + satisfied, ± partially satisfied, − not satisfied
Compliance with Ethical Standards
David Murray and Hemant Pandit receive research funding in the form of grants paid to the Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS), University of Oxford, and the Oxford University Hospitals National Health Service Trust from Zimmer Biomet and Stryker, both of which are manufacturers of orthopaedic implants. David Murray receives royalties related to the Oxford UKR, and consultancy fees from Zimmer Biomet. Hemant Pandit receives consultancy fees from Zimmer Biomet. None of these companies were involved in the funding or conduct of this study. Thomas Hamilton, Rafael Pinedo-Villanueva, Alexander Liddle, Sunil Pai and Edward Burn have no potential conflicts of interest to declare.
Data availability statement
Data sharing is not applicable to this article as no datasets were generated during the study.
Author’s contributions
Edward Burn, Alexander Liddle, Thomas Hamilton, Hemant Pandit, David Murray, and Rafael Pinedo-Villanueva made substantial contributions to the conception and design of the study. Edward Burn, Sunil Pai and Rafael Pinedo-Villanueva identified studies for inclusion in the review. Edward Burn and Rafael Pinedo-Villanueva drafted the manuscript, with Alexander Liddle, Thomas Hamilton, Sunil Pai, Hemant Pandit and David Murray revising it for important intellectual content. All authors read and approved the final manuscript.
Contributor Information
Edward Burn, Email: edward.burn@ndorms.ox.ac.uk.
Alexander D. Liddle, Email: a.liddle@ucl.ac.uk
Thomas W. Hamilton, Email: thomas.hamilton@ndorms.ox.ac.uk
Sunil Pai, Email: sunilkumarpai@doctors.org.uk.
Hemant G. Pandit, Email: hemant.pandit@ndorms.ox.ac.uk
David W. Murray, Email: david.murray@ndorms.ox.ac.uk
Rafael Pinedo-Villanueva, Email: rafael.pinedo@ndorms.ox.ac.uk.
References
- 1.Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster J-Y. Health-related quality of life in total hip and total knee arthroplasty. J Bone Jt Surg Am. 2004;86(5):963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Kane RL, Saleh KJ, Wilt TJ, Bershadsky B. The functional outcomes of total knee arthroplasty. J Bone Jt Surg. 2005;87(8):1719–1724. doi: 10.2106/JBJS.D.02714. [DOI] [PubMed] [Google Scholar]
- 3.Daigle ME, Weinstein AM, Katz JN, Losina E. The cost-effectiveness of total joint arthroplasty: a systematic review of published literature. Best Pract Res Clin Rheumatol. 2012;26(5):649–658. doi: 10.1016/j.berh.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nwachukwu BU, Bozic KJ, Schairer WW, Bernstein JL, Jevsevar DS, Marx RG, et al. Current status of cost utility analyses in total joint arthroplasty: a systematic review. Clin Orthop Relat Res. 2015;473(5):1815–1827. doi: 10.1007/s11999-014-3964-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ashraf ST, Ackroyd CE, Newman JH. Compartmental knee arthroplasty. Curr Orthop. 2003;17(2):134–143. doi: 10.1054/cuor.2002.0312. [DOI] [Google Scholar]
- 6.Liddle AD, Judge A, Pandit H, Murray DW. Adverse outcomes after total and unicompartmental knee replacement in 101 330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet. 2014;384(9952):1437–1445. doi: 10.1016/S0140-6736(14)60419-0. [DOI] [PubMed] [Google Scholar]
- 7.Liddle AD, Pandit H, Judge A, Murray DW. Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Jt J. 2015;97-B(6):793–801. doi: 10.1302/0301-620X.97B6.35155. [DOI] [PubMed] [Google Scholar]
- 8.Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW, Drummond MF, et al. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015. [Google Scholar]
- 9.Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS)–explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health. 2013;16(2):231–250. doi: 10.1016/j.jval.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG, Group Prisma Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sculpher MJ, Claxton K, Drummond M, McCabe C. Whither trial-based economic evaluation for health care decision making? Health Econ. 2006;15(7):677–687. doi: 10.1002/hec.1093. [DOI] [PubMed] [Google Scholar]
- 12.Gosden TB, Torgerson DJ. Converting international cost effectiveness data to UK prices. BMJ. 2002;325(7358):275–276. doi: 10.1136/bmj.325.7358.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghomrawi HM, Eggman AA, Pearle AD. Effect of age on cost-effectiveness of unicompartmental knee arthroplasty compared with total knee arthroplasty in the US. J Bone Jt Surg Am. 2015;97(5):396–402. doi: 10.2106/JBJS.N.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Konopka JF, Gomoll AH, Thornhill TS, Katz JN, Losina E. The cost-effectiveness of surgical treatment of medial unicompartmental knee osteoarthritis in younger patients: a computer model-based evaluation. J Bone Jt Surg Am. 2015;97(10):807–817. doi: 10.2106/JBJS.N.00925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koskinen E, Eskelinen A, Paavolainen P, Pulkkinen P, Remes V. Comparison of survival and cost-effectiveness between unicondylar arthroplasty and total knee arthroplasty in patients with primary osteoarthritis: a follow-up study of 50,493 knee replacements from the Finnish Arthroplasty Register. Acta Orthop. 2008;79(4):499–507. doi: 10.1080/17453670710015490. [DOI] [PubMed] [Google Scholar]
- 16.Manzotti A, Confalonieri N, Pullen C. Unicompartmental versus computer-assisted total knee replacement for medial compartment knee arthritis: a matched paired study. Int Orthop. 2007;31(3):315–319. doi: 10.1007/s00264-006-0184-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marcacci M, Zaffagnini S, Li CS, Bhandari M. Cost-effectiveness and Economic Impact of the KineSpring® Knee Implant System in the Treatment of Knee Osteoarthritis in Italy. J Long-Term Eff Med Implants. 2013;23(2):211–222. doi: 10.1615/JLongTermEffMedImplants.v23.i2-03.90. [DOI] [PubMed] [Google Scholar]
- 18.Peersman G, Jak W, Vandenlangenbergh T, Jans C, Cartier P, Fennema P. Cost-effectiveness of unicondylar versus total knee arthroplasty: a Markov model analysis. Knee. 2014;21:S37–S42. doi: 10.1016/S0968-0160(14)50008-7. [DOI] [PubMed] [Google Scholar]
- 19.Robertsson O, Borgquist L, Knutson K, Lewold S, Lidgren L. Use of unicompartmental instead of tricompart-mental prostheses for unicompartmental arthrosis in the knee is a cost-effective alternative: 15,437 primary tricompartmental prostheses were compared with 10,624 primary medial or lateral unicompartmental prostheses. Acta Orthopaed. 1999;70(2):170–175. doi: 10.3109/17453679909011257. [DOI] [PubMed] [Google Scholar]
- 20.Slover J, Espehaug B, Havelin LI, Engesaeter LB, Furnes O, Tomek I, et al. Cost-effectiveness of unicompartmental and total knee arthroplasty in elderly low-demand patients. A Markov decision analysis. J Bone Jt Surg Am. 2006;88(11):2348–2355. doi: 10.2106/JBJS.E.01033. [DOI] [PubMed] [Google Scholar]
- 21.Soohoo NF, Sharifi H, Kominski G, Lieberman JR. Cost-effectiveness analysis of unicompartmental knee arthroplasty as an alternative to total knee arthroplasty for unicompartmental osteoarthritis. J Bone Jt Surg Am. 2006;88(9):1975–1982. doi: 10.2106/JBJS.E.00597. [DOI] [PubMed] [Google Scholar]
- 22.Willis-Owen CA, Brust K, Alsop H, Miraldo M, Cobb JP. Unicondylar knee arthroplasty in the UK National Health Service: an analysis of candidacy, outcome and cost efficacy. Knee. 2009;16(6):473–478. doi: 10.1016/j.knee.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 23.Xie F, Lo NN, Tarride JE, O’Reilly D, Goeree R, Lee HP. Total or partial knee replacement? Cost-utility analysis in patients with knee osteoarthritis based on a 2-year observational study. Eur J Health Econ. 2010;11(1):27–34. doi: 10.1007/s10198-009-0154-5. [DOI] [PubMed] [Google Scholar]
- 24.Yang KY, Wang MC, Yeo SJ, Lo NN. Minimally invasive unicondylar versus total condylar knee arthroplasty: early results of a matched-pair comparison. Singap Med J. 2003;44:559–562. [PubMed] [Google Scholar]
- 25.National Institute for Health and Care Excellence. Osteoarthritis: care and management. NICE guidelines [CG177]. London: National Institutes for Health and Care Excellence; 2014.
- 26.Goodfellow JW, O’Connor JJ, Murray DW. A critique of revision rate as an outcome measure: re-interpretation of knee joint registry data. J Bone Jt Surg Br. 2010;92(12):1628–1631. doi: 10.1302/0301-620X.92B12.25193. [DOI] [PubMed] [Google Scholar]
- 27.Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, et al. Knee replacement. Lancet. 2012;379(9823):1331–1340. doi: 10.1016/S0140-6736(11)60752-6. [DOI] [PubMed] [Google Scholar]
- 28.Beard DJ, Holt MD, Mullins MM, Malek S, Massa E, Price AJ. Decision making for knee replacement: variation in treatment choice for late stage medial compartment osteoarthritis. Knee. 2012;19(6):886–889. doi: 10.1016/j.knee.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 29.Williams DP, Blakey CM, Hadfield SG, Murray DW, Price AJ, Field RE. Long-term trends in the Oxford knee score following total knee replacement. Bone Jt J. 2013;95-B(1):45–51. doi: 10.1302/0301-620X.95B1.28573. [DOI] [PubMed] [Google Scholar]
- 30.Burn E, Sanchez-Santos MT, Pandit HG, Hamilton TW, Liddle AD, Murray DW, et al. Ten-year patient-reported outcomes following total and minimally invasive unicompartmental knee arthroplasty: a propensity score-matched cohort analysis. Knee Surg Sports Traumatol Arthrosc. Epub 29 Dec 2016. [DOI] [PMC free article] [PubMed]
- 31.Jones WH, Chan W, Harrison T, Smith TO, Masonda P, Walton NP. Revision of medial Oxford unicompartmental knee replacement to a total knee replacement: similar to a primary? Knee. 2012;19(4):339–343. doi: 10.1016/j.knee.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 32.Martin JG, Wallace DA, Woods DA, Carr AJ, Murray DW. Revision of unicondylar knee replacements to total knee replacement. Knee. 1995;2(2):121–125. doi: 10.1016/0968-0160(95)00017-J. [DOI] [Google Scholar]
- 33.Saldanha KA, Keys GW, Svard UC, White SH, Rao C. Revision of Oxford medial unicompartmental knee arthroplasty to total knee arthroplasty—results of a multicentre study. Knee. 2007;14(4):275–279. doi: 10.1016/j.knee.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 34.Liddle AD, Judge A, Pandit H, Murray DW. Determinants of revision and functional outcome following unicompartmental knee replacement. Osteoarthr Cartil. 2014;22(9):1241–1250. doi: 10.1016/j.joca.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liddle AD, Pandit H, Judge A, Murray DW. Effect of surgical caseload on revision rate following unicompartmental and total knee replacement. J Bone Jt Surg Am. 2016;98(1):1–8. doi: 10.2106/JBJS.N.00487. [DOI] [PubMed] [Google Scholar]
- 36.Jones AM, Rice N. Econometric evaluation of health policies. Oxford: Oxford University Press; 2012. [Google Scholar]
- 37.Beard D, Price A, Cook J, Fitzpatrick R, Carr A, Campbell M, et al. Total or Partial Knee Arthroplasty Trial-TOPKAT: study protocol for a randomised controlled trial. Trials. 2013;14:292. doi: 10.1186/1745-6215-14-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Anderson R. Systematic reviews of economic evaluations: utility or futility? Health Econ. 2010;19(3):350–364. doi: 10.1002/hec.1486. [DOI] [PubMed] [Google Scholar]
- 39.Pignone M, Saha S, Hoerger T, Lohr KN, Teutsch S, Mandelblatt J. Challenges in systematic reviews of economic analyses. Ann Intern Med. 2005;142((12_Part_2)):1073–1079. doi: 10.7326/0003-4819-142-12_Part_2-200506211-00007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated during the study.