Abstract
Background
Common mental disorders are important contributors to the global burden of disease and cause negative effects on both the individual and society. Stress-related disorders influence the individual’s workability and cause early retirement pensions in Denmark. There is no clear evidence that mental health care alone will provide sufficient support for vocational recovery for this group. Integrated vocational and health care services have shown good effects on return to work in other similar welfare contexts.
The purpose of the Danish IBBIS (Integreret Behandlings- og BeskæftigelsesIndsats til Sygemeldte) study is to examine the efficacy of (1) a stepped mental health care intervention with individual stress coaching and/or group-based MBSR and (2) an integrated stepped mental health care with individual stress coaching and/or group-based MBSR and vocational rehabilitation intervention for people on sick leave because of exhaustion disorder, adjustment disorder or distress in Denmark.
Method/design
This three-armed, parallel-group, randomized superiority trial is set up to investigate the effectiveness of a stepped mental health care intervention and an integrated mental health care and vocational rehabilitation intervention for people on sick leave because of exhaustion disorder, adjustment disorder or distress in Denmark. The trial has an investigator-initiated multicenter design. Six hundred and three patients will be recruited from Danish vocational rehabilitation centers in four municipalities and randomly assigned into three groups: (1) IBBIS mental health care integrated with IBBIS vocational rehabilitation, (2) IBBIS mental health care and standard vocational rehabilitation, and (3) standard mental health care and standard vocational rehabilitation. The primary outcome is register-based return to work at 12 months. The secondary outcome measures are self-assessed level of depression (BDI), anxiety (BAI), distress symptoms (4DSQ), work- and social functioning (WSAS), and register-based recurrent sickness absence.
Discussion
This study will contribute with knowledge on the consequence of the current organizational separation of health care interventions and vocational rehabilitation regarding the individual’s process of returning to work after sick leave because of exhaustion disorder, adjustment disorder or distress. If the effect on return to work, symptom level, and recurrent sick leave is different in the intervention groups, this study can contribute with new knowledge on shared care models and the potential for preventing deterioration in stress symptoms, prolonged sick leave, and recurrent sick leave.
Trial registration
ClinicalTrials.gov, registration number: NCT02885519. Retrospectively registered on 15 August 2016). Participants have been included in the IBBIS trial for distress, adjustment disorder and exhaustion disorder since April 2016.
Electronic supplementary material
The online version of this article (doi:10.1186/s13063-017-2273-0) contains supplementary material, which is available to authorized users.
Keywords: Adjustment disorder, Exhaustion disorder, Distress, Return to work, Integrated services, Stress coaching, MBSR, Vocational rehabilitation, Prevention of recurrent sickness absence, RCT
Background
Stress-related disorders, like exhaustion disorder, adjustment disorder and distress, are frequent causes of sick leave in Denmark and other high-income countries [1–3]. Stress-related disorders are associated with individual suffering, and people who are on sick leave due to stress-related disorders often leave work with feelings of shame, anger, poor self-esteem, and physical symptoms of stress [4]. Though distress and exhaustion disorder are not considered clinical diagnoses, they are often used as sick leave causes by general practitioners in Denmark and other countries [5], and distress is a known risk factor for development of mental disorders like depression and anxiety [6, 7]. Long-term sick leave because of mental problems is a heavy burden on society [8]. Psychiatric disorders have an estimated financial burden on the Danish economy at 3.4% of the Danish gross domestic product [9]. Common mental disorders, like depression, anxiety, and adjustment disorder, cause the largest financial burden because of their high prevalence [9, 10]. Around 20% of people on sick leave because of adjustment disorders have relapses of psychological disorders and reoccurring sick leave [11] and anxiety disorders are the most common reasons for early retirement in Denmark [12].
Adjustment disorders, exhaustion disorder, and distress can be characterized as significant emotional and behavioral problems in response to one or more identified stressors. These stressors can be work-related factors like poor leadership, insecure working conditions, bullying or conflicts. Employees with impaired work functioning nonetheless most often express that a combination of social, economic, and work-related factors have caused their mental problems [13].
Though work can impose difficult and stressful challenges, it also seems to be pivotal for people [14]. Manifest benefits from work (e.g., income) and latent benefits from employment (e.g., daily structure, social contact, professional identity, status, and activity) make work attractive for the individual [15], and this applies to people with mental health problems as well [16]. Furthermore, long-term sick leave and unemployment is a known stressor and a risk factor for poor mental health for the individual [17, 18]. Whereas short-term sick leave can be necessary for the stressed person, it is highly relevant to help individuals return to work and prevent long-term sickness absence and deterioration in mental health [19]. The aim of the IBBIS intervention is to improve sick leave beneficiaries’ process of returning to employment after long-term sick leave due to adjustment disorders, distress, and exhaustion disorder.
Few return to work interventions for people on sick leave because of stress-related disorders have proven effective. In 2016, Nigatu and colleagues concluded from a meta-analysis of diverse return to work interventions (e.g., problem-solving therapy, cognitive behavioral therapy (CBT), workplace-directed interventions) for people with common mental disorders that no significant difference was found in return to work rates for the overall intervention group compared with control. The meta-analysis showed a small and significant reduction in sick leave duration in the pooled intervention group, where participants returned to work 13 days earlier than controls. Interventions that have proven effective in single studies are problem-solving therapy interventions, multidisciplinary interventions and/or Mindfulness-based Stress Reduction (MBSR) interventions [20].
Arends and colleagues’ earlier Cochrane Review regarding interventions specifically for people with adjustment disorders concluded that CBT did not improve part-time or full return to work compared to treatment as usual. Whereas problem-solving therapy did improve distress according to the Four-Dimensional Symptom Questionnaire (4DSQ) [5] after 3 months and improved partial return to work, it did not improve full return to work [2]. A Danish study by Netterstrøm and colleagues have shown good effect on stress symptoms and return to work with a combined intervention of workplace-oriented stress coaching and MBSR courses [21]. This study had a relatively small sample size and was conducted without a prior sample size calculation. Despite the large effect sizes, there is a risk of random type I error, and the result should be replicated in a larger population.
Return to work following sick leave is a multifaceted and complex process [22]. Personal, structural, and work-related factors probably also play an important role in the trajectory of return to work [23, 24]. Thus, the process of recovering from mental health problems and the process of vocational recovery are intertwined, as the reintegration in the workplace affects the individual’s mental health just as well as mental health affects work reintegration [25]. Most return to work interventions can be characterized as psychological interventions addressing the resilience of individuals undergoing stressful circumstances with a cognitive approach [20]. Work-related problems are addressed indirectly through the worker. Novel evidence-based interventions for people with common mental disorders directly addressing workplace accommodations are scarce. The intervention Individual Placement and Support (IPS) is an American intervention with a strong emphasis on integration of treatment and vocational support. IPS has shown to be superior compared with standard services in people with severe mental illness attaining and maintaining work in a Swedish randomized controlled trial (RCT) [26, 27], but there is not yet solid evidence on how IPS can best be modified to suit a target group with common mental disorders. Recently, a large Norwegian study tested integrated employment support designed with an emphasis on IPS principles and a work-directed therapy (“At work and Coping, AWaC”). The study showed positive results regarding faster return to work for people with common mental disorders [28].
Rehabilitation after stress-related disorders seems to be an issue that lies in the borderland between the health care sector and the employment sector. In Denmark, vocational rehabilitation and work-directed interventions are governed by the local public office called the job center. The job centers handle the benefit case closely together with the provision of rehabilitation services [29]. The Organization for Economic Co-operation and Development (OECD) suggests that there is an unfortunate lack of coordination between the health care system and social insurance offices in Scandinavian countries [9]. The lack of coordination causes conflicting requirements and goals and a feeling of confusion and uncertainty for the individual on sick leave at a time where the individual lacks control and certainty [22, 30]. Intervention models that genuinely integrate services from the health care sectors and the employment sector in Scandinavia have not yet, to the authors’ knowledge, been tested on a population with stress-related disorders.
The aim of the IBBIS trial for exhaustion disorder, adjustment disorder, and distress is to test the effect on return to work from stepped mental health care and integrated stepped mental health care and vocational rehabilitation. By integrating and coordinating the two types of interventions, we aim to reduce counterproductive aims and services in both sectors, conveying a higher degree of collaboration about the participants’ mental and vocational recovery.
Methods/design
Aim
The aim of the randomized, three-armed, investigator-initiated, multicenter, parallel-group, superiority trial is to compare the effect on return to work of the following interventions: (1) IBBIS mental health care integrated with IBBIS vocational rehabilitation, (2) IBBIS mental health care and standard vocational rehabilitation or (3) standard mental health care and standard vocational rehabilitation. The primary hypothesis is that participants allocated to the IBBIS mental health care integrated with IBBIS vocational rehabilitation will have significantly faster return to work rates than people who are allocated to standard mental health care together with standard vocational rehabilitation. The secondary hypothesis is that IBBIS mental health care together with standard vocational rehabilitation will have a lesser but significant effect on return to work compared with standard mental health care together with standard vocational rehabilitation. The superiority of the IBBIS mental health care integrated with IBBIS vocational rehabilitation will also be tested by comparison with the IBBIS mental health care together with standard vocational rehabilitation intervention. The IBBIS vocational rehabilitation intervention alone will not be tested in this trial. We hypothesize that the superiority of the IBBIS interventions will be applicable for secondary outcomes and exploratory measures at 6-, 12-, and 24-month follow-ups so that (1) symptom level and presenteeism will be lower in participants allocated to IBBIS interventions and that (2) improvement in self-efficacy, quality of life, and functioning will be better in participants allocated to IBBIS interventions, and (3) satisfaction with services and number of weeks worked will be higher for participants allocated to IBBIS interventions.
The IBBIS trial is designed and reported in this article according to the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) 2013 Statement (SPIRIT checklist and elaborated SPIRIT figure is provided as Additional file 1) [31], and the final results will be published according to the Consolidated Standards of Reporting Trials (CONSORT) criteria for Randomized Trials of Nonpharmacologic Treatment [32]. There is a parallel trial in the IBBIS project with identical research design for participants with depression and anxiety (reference to parallel IBBIS trial if possible).
Setting
The interventions will be delivered by a cross-sector and multidisciplinary IBBIS team which is organized in collaboration between Mental Health Services in the Capital Region of Denmark and the following four municipalities: The City of Copenhagen, and the three suburban municipalities Gentofte, Gladsaxe, and Lyngby-Taarbæk. Participants are referred to the study by social security officers from job centers in the four municipalities, and the interventions are provided in locations other than the job centers and the mental health centers.
Participants
Eligible participants in this trial are adults who are on sick leave from work or unemployment and have received sick leave benefit for at least 4 weeks or have started a sick leave benefit case which is estimated to last for at least 8 weeks. Participants must meet the criteria for exhaustion disorders according to the National Board of Health and Welfare in Sweden [33], Adjustment disorder according to the International Classification of Mental and Behavioural Disorders, version 10 (ICD-10) [34] or distress according to the Four-Dimensional Symptom Questionnaire (4DSQ) [5]. Participants must also meet the following criteria to participate in the trial: be a resident of collaborating municipalities at baseline, be able to understand, speak and read Danish, be aged 18 years or older, and have given verbal and written consent to participate in the trial. Eligibility and determination of disorder are assessed by an IBBIS team member (nurse, physiotherapist, social worker, occupational therapist, psychologist or psychiatrist) who is trained to perform the assessment.
The IBBIS interventions are not designed to accommodate people in need of acute or highly specialized care. Thus, the potential participant will not be eligible if they meet the exclusion criteria: (1) the assessor determines the patients’ suicide risk to be high according to the MINI instrument [35] and the physician confirms this risk, (2) the patient meets the screening criteria for dementia according to The Mini-Mental State Examination (MMSE) screening instrument [36], (3) the patient abuses alcohol and/or other substances according to the assessor, (4) the patient has a severe, unstable, somatic condition (e.g., cancer, chronic obstructive pulmonary disease), (5) the patient needs secondary mental health care or (6) the patient is judged by job center staff to be at risk of displaying aggressive behavior. We wish to compare the IBBIS mental health care intervention alone with standard treatment. Thus, a potential participant will not be included in the study if they (7) do not accept to abstain from taking part in any psychotherapy or psychotherapy-like treatment outside the IBBIS intervention if they are allocated to IBBIS mental health care. Exclusion criteria 2–5 are only applied if the physician in the IBBIS team confirms the assessment and anticipates that the patient cannot benefit from the IBBIS interventions. In cases with high suicide risk, the participant will be referred to acute care services. People with alcohol and substance abuse problems will be offered referral to treatment if relevant.
Recruitment, data collection, and data management
Recruitment takes place in two steps. First, case managers from the four job centers can refer Danish-speaking, adult citizens on sick leave from either work or unemployment to a psychiatric assessment if either the case manager, the citizen or the individuals’ general practitioner suspects a mental health condition to have caused the sick leave. The referral and assessment are voluntary. The results of the assessment will be shared with the individual’s general practitioner (GP) and the job center. The psychiatric assessment is based on three sources of information about the participant:
- Personal interview conducted by a care manager/psychologist and supervised by psychiatrist, guided by the following instruments:
- ○ MINI International Neuropsychiatric Interview (MINI) [35]
- ○ Standardized Assessment of Personality – Abbreviated Scale (SAPAS) [37]
- ○ Attention deficit hyperactivity disorder (ADHD)-symptom checklist for adults (Adult Self-Report Scale, ASRS v1.1) [38]
- ○ If dementia is suspected: Mini-Mental State Examination (MMSE) [36]
Self-assessed symptoms: 4DSQ [5]
Sick leave note issued by the GP
Assessors are IBBIS team members who are specially trained to use the above-mentioned instruments. Trial eligibility will be evaluated after the psychiatric assessment, and subsequently, assessment data will constitute baseline data at the time − 1 (see Table 1). The assessment process should not take more than 3 weeks but can be prolonged if one or more of the three types of information are missing.
Table 1.
Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) figure: enrollment and data collection
| Baseline t-1 | Randomization t0 | 6-month follow-up t1 | 12-month follow-up, t2 | 24-month follow-up t3 | |
|---|---|---|---|---|---|
| Informed consent | X | ||||
| Case Report Form (CRF) from personal interviews | X | ||||
| Randomization database | X | ||||
| Registration sheets | X | X | Continuous registration | ||
| Self-assessment data | X | X | X | X | |
| Register data | X | X | X | X | |
Second, individuals who meet the aforementioned trial criteria at assessment, and subsequently consent to participate, will be randomly allocated to an intervention by the assessor at t0. The results of the psychiatric assessment will be utilized in the treatment plan if the participant is allocated to treatment in IBBIS. Participants will be followed up at 6, 12, and 24 months after allocation (see Fig. 1 for the flowchart of participant timeline). Participants will be prompted to fulfill self-assessment questionnaires at each follow-up time through up to five personal contacts.
Fig. 1.
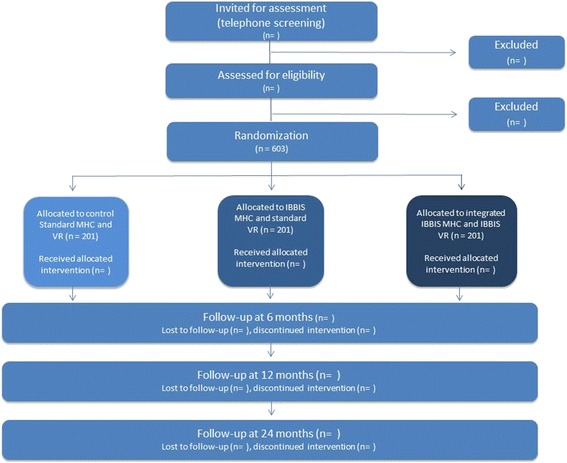
Flow chart for IBBIS participants
All electronic data (self-assessment, interview, and register data) are stored on secured servers at closed networks, and access to data is logged through unique login for an assigned list of IBBIS personnel. Physical data material (Case Report Forms with selected interview data) is stored in locked spaces, in locked facilities. Transfer of electronic data between staff members and other approved data managing institutions is carried out using only tunnel-encrypted e-mailing or encrypted UBS sticks.
Randomization
Participants will be allocated to receive one of the following interventions: (1) IBBIS mental health care and standard vocational rehabilitation, (2) IBBIS mental health care integrated with IBBIS vocational rehabilitation or (3) standard mental health care and standard vocational rehabilitation. The allocation ratio between the three arms is 1:1:1. A centralized randomization will take place according to a web-based, computer-generated, allocation sequence with varying block sizes kept unknown to the assessors. Odense Patient data Explorative Network (OPEN) is responsible for the randomization, administrative personnel in the IBBIS team perform the online randomization, and the IBBIS team leader will assign the participant to interventions and professionals.
We expect that service delivery can vary from municipality to municipality and the process of gaining a new job from unemployment will take longer time than returning to an existing job. Previous research has shown that diagnosis is a possible predictor of return to work [39]. Thus, the randomization is stratified according to (1) municipality, (2) employment status at baseline (on sick leave from work vs. on sick leave from unemployment), and (3) diagnosis (adjustment disorder vs. distress vs. exhaustion disorder).
Blinding
Due to the modalities of the IBBIS interventions, the participants and the professionals delivering the IBBIS interventions cannot be blinded to the group allocation. All outcomes are based on registries or self-assessed questionnaire data, and no assessor-based follow-up data will be obtained. Register data on employment status and income is created automatically through the national registries. Information on the participant’s sick leave benefit status is created through the job center management system, and benefits are granted and registered by the employment consultants in the IBBIS team.
Blinding of assessors is only relevant at the baseline interview, which takes place before group allocation. Referring personnel will likewise be blinded to the allocation sequence and block size to prevent them from anticipating the next group allocation. The researchers will be blinded to group allocation during the process of data analysis. Group allocation will be coded with names like X, Y, and Z to conceal the given intervention. The researcher will draw up conclusions at the 6- and 12-month follow-up based on the six scenarios where each group (X, Y or Z) has received IBBIS mental health care and standard vocational rehabilitation, integrated IBBIS mental health care and IBBIS vocational rehabilitation, and standard mental health care and vocational rehabilitation. After this, the blinding will be broken. The researcher performing analysis at 24-month follow-up will not be blind to group allocation, as any possible differences between groups will be revealed after 12-month follow-up.
Interventions and comparisons
The IBBIS intervention team is constituted by (1) three and a half full-time care managers who are nurses, occupational therapists, physiotherapists or social workers with mental health care experience and a minimum of 1 year certified training in CBT, (2) three and a half full-time employment consultants who are social insurance officers from the job centers, and (3) equivalent to 0.75 full-time psychiatrists (alternatively, general practitioner or psychologist). Care managers, psychiatrists, and psychologists are employed in the Mental Health Services, and employment consultants are employed in the job centers of the four municipalities. Care managers have a maximum momentary caseload of 25, and employment consultants have a maximum momentary caseload of 20. The IBBIS mental health care intervention is expected to have an average duration of 4 months, and the duration of the IBBIS vocational rehabilitation is expected to average 7 months.
The team delivers two separate interventions (1) IBBIS mental health care alone and (2) IBBIS mental health care integrated with IBBIS vocational rehabilitation. Both interventions are carried out with a great emphasis on participant involvement, shared decision-making, and involvement of the participants’ relatives. A fidelity scale (unpublished, available through the corresponding author) is developed and used for biannual fidelity reviews to ensure program adherence and continuous focus on program implementation and improvement. The fidelity reviews are based on observations and individual and group interviews of professionals, management, and participants, as well as a review of 10 participant cases. Once program fidelity is achieved future fidelity reviews will be conducted annually.
IBBIS mental health care and standard vocational rehabilitation
IBBIS mental health care is delivered as manualized stepped care. The participant will be offered treatment options according to a stepped care plan, offering the least invasive and least resource-demanding effective treatment first. Intervention modalities will be offered according to the stepped care plan, see Table 2. One or more of the following treatment options will be provided:
Care plan produced in collaboration with the care manager and participant and in accordance with treatment guidelines for the symptom severity and relevant step (step 1–3)
Regular monitoring by the care manager of progression in symptom level (according to 4DSQ) minimum every fortnight to ensure timely changes in the treatment plan and step if participants deteriorate [5] (steps 1–3)
Individual psychoeducation with a self-management approach by the care manager. The psychoeducation aims at providing general information about symptoms and coping strategies to normalize and provide help for self-help (steps 1–3)
Bibliotherapy: supplementary psychoeducational disease-specific written material which aims at providing general information about symptoms and coping strategies to normalize and provide help for self-help (steps 1–3)
Involvement of relatives by the care manager (steps 1–3)
Stress coaching conducted by the care manager inspired by the intervention in Netterstrøm (2013) [21]. The stress coaching intervention is a structured, seven-session individual intervention with focus on immediate stress reduction, identification of stressors, changing coping strategies and restoring balance (step 2)
An eight-session, group-based, Mindfulness-based Stress Reduction (MBSR) program [40] conducted by certified MBSR teachers (step 3)
Table 2.
Stepped care algorithm for adjustment disorder, exhaustion disorder, and distress
| Step | Disorder | Treatment |
|---|---|---|
| 1 | Mild stress disorder (4DSQ distress-subscale 10–20) for < 2 months or Moderate stress disorder (4DSQ distress-subscale > 20) for < 1 months or Adjustment disorder < 2 months |
Bibliotherapy Individual psychoeducation Monitoring by care manager Involvement of relatives |
| 2 | Moderate stress disorder (4DSQ distress-subscale > 20) for > 1 month or Mild stress disorder (4DSQ distress-subscale 10–20) for > 2 months or Adjustment disorder for > 2 months and 4DSQ 10–20 distress-subscale or Adjustment disorder for > 1 month and 4DSQ distress-subscale > 20 |
Stress coaching Bibliotherapy Individual psychoeducation Monitoring by care manager Involvement of relatives |
| 3 | Exhaustion disorder according to the National Board of Health and Welfare in Sweden | MBSR Stress coaching Bibliotherapy Individual psychoeducation Monitoring by care manager Involvement of relatives |
The psychiatrist and/or the psychologist of the IBBIS team are responsible for:
Supervision of care managers
Initiation of non-medical treatment (can be delegated to the care manager under supervision)
Collaboration with the participant’s GP and other possible treatment providers
Participants will receive standard vocational rehabilitation services from the local job center along with continuous control of the grounds for receiving sick leave benefit. The IBBIS team will not collaborate with job center personnel.
Integrated IBBIS mental health care and IBBIS vocational rehabilitation
The mental health care in intervention in the integrated intervention is identical with that which is described in the IBBIS mental health care above. The concurrent vocational rehabilitation in IBBIS is composed of the following elements, which are delivered to meet the participant’s individual needs for vocational recovery:
Vocational assessment of the participant’s work capacity and barriers in relation to work with focus on readiness for return to work [41], work role functioning [42], and return to work self-efficacy [43]
Vocational rehabilitation plan produced in collaboration with the participant and in compliance with the vocational rehabilitation manual
Problem-solving support in returning to a current workplace and preventing recurring sick leave inspired by Dutch guidelines and the intervention SHARP-at work. The support is focused on quick, stepwise return to work and problem-solving of issues related to the work-place which are barriers for return to work or impose risk factors for recurring sick-leave [44, 45]
Job-search support with a focus on the best possible job match inspired by Individual Placement and Support (IPS) in accordance with the slightly moderated IPS principles (1) focus on competitive employment, (2) integration of mental health and employment services, (3) strong attention to participant preferences, (4) counseling about benefit programs and supported work accommodations, (5) rapid job search, (6) systematic job development, and (7) time-unlimited support for work retention [46]
Case management according to Danish sick leave benefit legislation with continuous assessment of the justification of the type and duration of sick leave benefit
Coordination, where relevant, with other public authorities who provide social services
Involvement of relatives
Consistency between goals in treatment and vocational rehabilitation is crucial [22, 30]. Several integrational elements ensure coherence in the participants’ process of returning to work and recovering from mental problems in the integrated IBBIS intervention:
At least one meeting between the participant, the employment consultant, and the care manager where a joint plan for return to employment and the support from the IBBIS team is decided upon
Co-location of all team members
Multidisciplinary supervision of care managers and employment consultants together to enhance a continuous focus on the shared goals of the participants
The integrated services are based on the theoretical framework relational coordination by Jody Gittell in which timely and problem-solving communication between different professionals is created by focusing on shared goals, shared knowledge and mutual respect [47]. Unfortunately, it has not been possible to establish a shared electronic folder for IBBIS staff from different organizations to use due to separate secure IT systems and, hence, written communication across sectors and municipalities can only be shared through encrypted e-mails according to national guidelines to conform to the Act on the processing of Personal Data.
Training and supervision
Employment consultants and care managers have all attended a 4-week training course in April 2016; 1 week of joint training and 3 weeks of training in their monodisciplinary groups. Care managers are trained in all aspects of the IBBIS mental health care intervention with a special focus on psychiatric assessments and CBT. Likewise, employment consultants are trained in all aspects of the IBBIS vocational rehabilitation intervention with a special focus on the problem-solving method and job development. Care managers have weekly, case-based supervision and stress coaching supervision every fortnight, the employment consultants have weekly supervision, and the team has monthly, case-based, cross-disciplinary supervision.
Standard mental health care and standard vocational rehabilitation
Participants who will be allocated to the control group will receive standard health care by their GP and standard services in the job center. Adjustment disorder, exhaustion disorder, and distress are commonly used as reasons for sick leave by the GP, but are nonetheless not disorders that the public health care system is obliged to provide treatment for. A large number of private companies offer treatment of stress-related disorders in Denmark through an emerging market of insurance companies and out-of-pocket offers. These have been characterized as very diverse and lacking an evidence base [48].
GPs can, with supervision, offer up to seven therapy sessions to patients with social or psychological complaints. It is estimated that 89% of Danish GPs offer therapy to their patients and 49% of the GPs patients receiving therapy are registered with stress or adjustment disorder. The therapy is often very short term, as 36% of patients only receive one session and 73% receive three or fewer therapy session [49]. Local health authorities are not obliged to offer help to people who suffer from stress-related disorders, but two out of three municipalities in Denmark offer self-management courses [50] or stress management groups to people who can self-refer with mental problems.
The job centers offer a variety of courses and support and manage the sick leave benefit case according to government legislation, which requires regular follow-up every 4 weeks, reassessment of the sick leave diagnosis after 22 weeks, self-management courses and support to gradual return to work (in paid or unpaid jobs).
Collaboration between the job center and the health care system is minimal and conducted through standardized sick leave certificates from the GP to the job center. Representatives from the health care system (other than the individuals’ own health care providers) can be used in reassessment of the individuals’ sick leave case.
Outcomes
The primary outcome is time from baseline to the event return to work, within 12 months after baseline. Work is defined as having four consecutive weeks of working with a salary and with no concurrent vocational benefits. Benefit and income status is retrieved from the Danish DREAM database and the electronic income register [51]. The DREAM database is administered by Danish Agency for Labour Market and Recruitment and can be linked to a range of different registers, including the Danish Income Register. Returning to or achieving a flex-job, a type of subsidized work, is also defined as returning to work for participants who are entitled to flex-job when they enter the trial. The work-related, symptom-based and functional secondary outcomes are presented in Table 3. All explorative and safety measures are presented in Table 4.
Table 3.
Primary and secondary outcomes and data collection
| Data source | Outcome | Baseline | 6-month follow-up | 12-month follow-up | 24-month follow-up | |
|---|---|---|---|---|---|---|
| Primary | DREAM database | Time from baseline to RTW | X | |||
| Secondary | DREAM database | Proportion in ordinary work | X | |||
| DREAM database | Time from baseline to RTW | X | X | |||
| DREAM database | Time from the first day of RTW until possible recurrent sick leave | X | ||||
| Questionnaire | Difference in depressive symptoms measured by Beck Depression Inventory (BDI-II) [52] | X | X | |||
| Questionnaire | Difference in anxiety symptoms measured by Beck Anxiety Inventory (BAI) [55] | X | X | |||
| Questionnaire | Difference in stress symptoms measured by Cohen Perceived Stress 10-item Scale (PSS) [77] | X | X | |||
| Questionnaire | Social and work-related function measured by WSAS [57] | X | X |
RTW return to work, WSAS Work and Social Adjustment Scale
Table 4.
Explorative outcomes and safety measures
| Data source | Outcome | Baseline | Follow-up | ||
|---|---|---|---|---|---|
| 6 months | 12 months | 24 months | |||
| DREAM database | Weeks of work from baseline to current follow-up | X | X | ||
| Questionnaires | Symptoms of distress, anxiety, depression, and somatization by Four-Dimensional Symptom Questionnaire (4DSQ) [5] | X | X | X | X |
| Depressive symptoms measured by Beck Depression Inventory-II (BDI-II) [52] | X | X | X | ||
| Anxiety symptoms measured by Beck Anxiety Inventory (BAI) [55] | X | X | X | ||
| Stress-symptoms measured by Cohen Perceived Stress 10-item Scale (PSS) [77] | X | X | X | ||
| Social and work-related function measured by WSAS [57] | X | X | X | ||
| Burn-out symptoms measured by Karolinska Exhaustion Scale (KES) [58] | X | X | X | X | |
| Health-related quality of life measured by EQ-5D-5L [78] | X | X | X | X | |
| General quality of life measured by Flanagan’s QOLS [61] | X | X | X | X | |
| Self-efficacy concerning symptoms measured by IPQ subscale on personal control [62] | X | X | X | X | |
| Return to work self-efficacy measured by RTW-SE [63] | X | X | X | X | |
| General self-efficacy measured by General Self-efficacy Scale (GSS) [64] | X | X | X | X | |
| Client satisfaction with treatment measure measured by CSQ-8 [65] | X | ||||
| Presenteeism measured by Stanford Presenteeism Scale (SPS) [79] | X | X | X | ||
| Use of therapy and therapy-like services outside IBBIS | X | X | X | ||
CSQ-8 Client Satisfaction Questionnaire, EQ-5D-5L European Quality of Life Five Dimension Five Level version, IPQ Illness Perception Questionnaire-Revised, QOLS Quality of Life Scale, RTW-SE Return to Work Self-efficacy
The Beck Depression Inventory (BDI–II) consists of 21 items to assess the intensity of depression in clinical and normal patients. Each item is a list of four statements (0 to 3) arranged in increasing severity about a particular symptom of depression [52]. The Beck Anxiety Inventory (BAI) is a 21-item general questionnaire for anxiety, measuring symptoms during the last week rated on a four-point Likert-scale from 0 to 3 [53]. The BDI and BAI has shown excellent psychometric properties, with internal consistency around 0.9 [54, 55]. Cohen’s Perceived Stress Scale (PSS) is a global measure of perceived stress. The scale was originally a 14-item questionnaire, and it has later been moderated to a 10-item questionnaire which shows improved and satisfactory psychometric properties [56]. The Work and Social Adjustment Scale (WSAS) is a simple, reliable, five-item scale which measures functional impairment related to an identified problem [57], which is defined in this trial as “psychological symptoms.”
The Four-Dimensional Symptom Questionnaire (4DSQ) is a 50-item questionnaire designed to assess common psychological symptoms in the last week and has a special focus on distinguishing general distress from depression, anxiety, and somatization [5]. The Karolinska Exhaustion Scale (KES) 26-item version measures the degree of exhaustion disorder and the four inter-related dimensions of exhaustion disorder according to the Swedish National Board of Health and Welfare: lack of recovery, cognitive exhaustion, somatic symptoms, and emotional distress [58, 59]. The European Quality of Life Five Dimension Five Level version (EQ-5D-5L) is a measure of health status in five domains: mobility, self-care, usual activities, pain/discomfort and anxiety/depression and also includes a Visual Analogue Scale from 0 (worst imaginable health status) to 100 (best imaginable health status) [60]. Flanagan’s QOLS is a 16-item instrument that measures five conceptual domains of quality of life: material and physical wellbeing, relationships with other people, social, community and civic activities, personal development and fulfillment, recreation, and independence [61]. The six-item Personal Control subscale from the revised version of the Illness Perception Questionnaire (IPQ-R) is used to evaluate the participant’s self-efficacy regarding symptom management [62]. Return to work self-efficacy (RTW-SE) is an 11-item measure for self-efficacy beliefs regarding return to work where respondents are asked to respond to statements about their jobs, imagining that they would start working tomorrow in their present emotional state [63]. The General Self-Efficacy Scale is a 10-item psychometric scale that is designed to assess optimistic self-beliefs to cope with a variety of difficult demands in life [64]. The Client Satisfaction Questionnaire (CSQ-8) is an eight-item questionnaire which is used to measure the participants’ satisfaction with mental health care services and vocational rehabilitation [65]. Presenteeism refers to the state where a person attends work while being sick [66] and is used as a proxy measure for returning to work while having reduced workability.
Sample size and power calculation
The sample size of this trial is based on the primary outcome return to work rate (hazard ratio (HR)). There are to the authors’ knowledge no comparable Danish studies, and the sample size estimates are based on Dutch studies of comparable interventions for populations on sick leave with common mental disorders. The desired type II error risk is set at 10% (power = 90%). The mean number of days from baseline to return to work in the control group is conservatively estimated to be 210 days [67–69]. Due to multiple testing, as we will make comparisons between all three study arms, we Bonferroni correct the type I error risk (α) to 0.0167. An HR of 1.5 is estimated to be clinically relevant [70–72], and participants will be recruited through 639 days and followed for 365 additional days. With an allocation ratio of 1:1:1 we need 201 participants in each of the three arms to reject the null hypothesis that the return to work rate is equal in the control group, the IBBIS mental health care intervention, and the integrated IBBIS mental health care and IBBIS vocational rehabilitation intervention, respectively. If we fail to include 603 participants, the statistical power can be lowered to 80% and thus only 468 participants will be needed.
Power calculations (Tables 5 and 6) indicate that a sample size of 201 participants per group will be adequate to detect relevant significant differences in the secondary outcome measures with minimum 80% power.
Table 5.
Power calculation for binary secondary outcomes
| Outcome | Expected proportion in control group | Clinically relevant proportion in intervention group | α | Power | Test | Reference |
|---|---|---|---|---|---|---|
| Proportion achieving > 4 four weeks of ordinary job | 0.65 | 0.80 | 0.0167 | 0.838 | χ2 test | [67–69, 80] |
| Proportion of > 4 weeks recurrent sick leave absence among participants who returned to work | 0.19 | 0.08 | 0.0167 | 0.801 | χ2 test | [11] |
Table 6.
Power calculation for linear secondary outcomes
| Outcome | δ clinically relevant difference in mean | σ expected standard deviation | α | Power | Test | Reference |
|---|---|---|---|---|---|---|
| Difference in depressive symptoms measured by Beck Depression Inventory (BDI) | 4 | 11 | 0.0167 | 0.893 | t test | [81–86] |
| Difference in anxiety symptoms measured by Beck Anxiety Inventory (BAI) | 4 | 12 | 0.0167 | 0.826 | t test | |
| Difference in stress symptoms measured by Cohen’s Perceived Stress Scale (PSS) | 5 | 8 | 0.0167 | 1.000 | t test | [87–89] |
| Social- and work-related function measured by WSAS | 4 | 10 | 0.0167 | 0.946 | t test | [90] |
WSAS Work and Social Adjustment Scale
All sample size and power calculations are conducted in the PS: Power and Sample Size Calculation software [73].
Statistical analysis plan
The primary objective of this superiority trial is to test if there is any difference in time from baseline to the event return to work between the three groups at 12-month follow-up time; the null hypothesis being that there is no difference. Because the primary outcome data is collected as register data, the data is expected to be complete. Kaplan-Meier survival curves will be computed, and the differences between the three intervention groups will be tested with a Cox proportional hazards regression analysis to estimate the treatment effect as HR with 95% confidence intervals. Cox regression analysis will also be used for the secondary outcomes at 24-month follow-up: “time from return to work to recurrent sick leave” for the subpopulation of individuals who have started working and “time from baseline to return to work.”
The continuous secondary outcomes at 6-month follow-up BDI, BAI, PSS, and WSAS are used with a repeated measurement design and the difference in the individuals’ scores between measurements will be analyzed by using linear mixed models with repeated measures and unstructured covariance matrix if possible. All participants will be included in the analysis according to the intention-to-treat principle. Missing data from the questionnaire-based instruments will be imputed with multiple imputations if we can assume that data are missing at random or missing completely at random. The effect of missing data will, furthermore, be assessed by sensitivity analyses. All statistical tests are two-sided. All exploratory continuous outcomes will be analyzed by the same method.
A non-parametric model will be used in situations where the scores are not normally distributed. The binary outcome proportion in ordinary work will be analyzed with logistic regression. All models will be adjusted for the stratification variables. We will assess the potential interaction between time and intervention for continuous secondary outcomes.
Discussion
This paper describes the study protocol of a randomized controlled trial comparing (1) IBBIS mental health care integrated with IBBIS vocational rehabilitation, (2) IBBIS mental health care and standard vocational rehabilitation, and (3) standard mental health care and standard vocational rehabilitation for people on sick leave because of distress, adjustment disorder or exhaustion disorder. Stress-related conditions are frequent causes of sick leave in Denmark with great costs for the individual and society. This trial will test two new targeted approaches to mental health care and vocational rehabilitation and the integration of these interventions to reduce the burden of these conditions.
This randomized controlled trial is designed with great emphasis on minimizing bias and reporting is done in accordance with SPIRIT guidelines [31]. The large sample size and, hence, high statistical power allows for detection of relevant differences in both primary and secondary outcomes. The randomization is in accordance with high methodological standards. There are nonetheless some methodological challenges.
Firstly, we expect that some contamination between the IBBIS mental health care intervention and the integrated IBBIS mental health care and IBBIS vocational rehabilitation intervention will occur because care managers might be inclined to provide IBBIS mental health care with an undesirable emphasis on vocational recovery because of their close collaboration with employment consultants regarding the participants in the integrated intervention. To minimize the risk of contamination for participants in the IBBIS mental health care and standard vocational rehabilitation intervention care managers are prompted to avoid collaboration with regular job center case managers about individual cases. Secondly, participants and professionals are not blinded to group allocation, and there is also a risk of both performance bias and subject-expectancy bias. These likely biases are difficult to prevent and will be included in the interpretation of the results.
Thirdly, implementation of structured interventions in multicenter designs have previously shown to be difficult; several context-factors affect the implementation of the intervention [74], and some variation in the delivered services between the Danish municipalities is expected [75]. We attempt to minimize the bias from the possibly skewed implementation by stratifying the randomization for municipality. To address the possible differences in effects between municipalities, we will, furthermore, conduct fidelity reviews to explicate differences in implementation.
Fourthly, multidisciplinary teams have previously shown difficult to establish [75], and the collaboration in integrated care can be difficult to implement as it has to be established and maintained at the macro, meso, and micro level in all municipalities [76]. Thus, we expect the teams to perform better at the end of the trial period than at the beginning, which can explain a missing or minimal effect from the interventions. This will be examined by analyzing the possible interaction between intervention and time.
Fifthly, standard mental health care and standard vocation rehabilitation for people with stress-related disorders are very scarcely described in Denmark. Thus, a limitation in the study design is the limited knowledge about the quality and quantity of the control intervention. To improve the possibilities for comparison between the three interventions three questions about the participants’ use of therapy and therapy-like services outside IBBIS have been added to the self-assessment scheme.
Sixthly, a limitation in the study design is the fact that we cannot measure the effect of the IBBIS vocational rehabilitation alone. Unfortunately, a four-armed design was not feasible regarding economy and sample size, and a 2 × 2 factor design is not suitable when the intervention components are expected to interact in synergy in the integrated intervention. We prioritize to test the efficacy of the IBBIS mental health care intervention as we expected improved treatment to be a necessity for improved return to work.
If this trial shows that the IBBIS mental health care intervention is superior to standard treatment, these positive results will support the further development of enhanced community-based mental health care for people on sick leave, and a wider implementation of treatment teams similar to IBBIS can be recommended. If this trial shows that integrated IBBIS mental health care and IBBIS vocational rehabilitation is superior to standard treatment or IBBIS mental health care alone, the positive results will support the assumption that integrated care is not only a perceived need from the target group, but also an effective way of supporting people in their vocational recovery. If the standard intervention is superior regarding return to work, we have further incentive to attempt to improve treatment and vocational care; it can be considered if return to work rates has reached a maximum.
This study can contribute with new knowledge on integrated vocational and health care interventions in welfare societies with separate health care and occupational sectors, and prevention of recurrent sickness absence among people with distress, adjustment disorder or exhaustion disorder.
Trial status
The IBBIS trial for distress, adjustment disorder, and exhaustion disorder was initiated in April 2016, and as of November 7, 2017, 426 participants have been recruited. This protocol is in version 2.0. Trial recruitment is expected to end on 31 December 2017.
Acknowledgements
The authors would like to thank Iris Arends, Ute Bültmann, and Jac J L van der Klink for giving permission to use the “Sharp at Work” manual for the vocational rehabilitation intervention. We thank Monique Loo, Bea Marie Kolbe Ebersbach, Bo Netterstrøm, and Bjarne Toftegård for the training of the IBBIS teams. We thank Lone Tonsgaard for the English revision of the manuscript.
Funding
The Danish Agency for Labour Market and Recruitment has sponsored the IBBIS project in a horizontal collaboration with the Mental Health Services in the Capital Region of Denmark. The four collaborating municipalities have partly financed the salary of the employment consultants. The Danish Agency for Labor Market and Recruitment has had a role in the design of the study (co-responsible for the selection of the target population and the design of selected interventions modalities). The funding agency will not take part of decisions regarding analysis, interpretation of the data or publication of results.
Availability of data and materials
Not applicable
Abbreviations
- 4DSQ
Four-Dimensional Symptom Questionnaire
- BAI
Beck Anxiety Inventory
- BDI-II
Beck Depression Inventory II
- CSQ-8
Client Satisfaction Questionnaire
- DREAM
Danish Register for Evaluation of Marginalization
- EQ-5D-5L
European Quality of Life Five Dimension, Five level version
- GP
General practitioner
- GSS
General Self-efficacy Scale
- IPQ-R
Illness Perception Questionnaire-Revised
- IPS
Individual Placement and Support
- KES
Karolinska Exhaustion Scale
- MINI
Mini International Neuropsychiatric Interview
- OPEN
Odense Patient data Explorative Network
- PSS
Cohen’s Perceived Stress Scale
- QOLS
Quality of Life Scale
- RTW-SE
Return to Work Self-efficacy
- SAPAS
Standardized Assessment of Personality: Abbreviated Scale
- SPS
Stanford Presenteeism Scale
- WSAS
Work and Social Adjustment Scale
Additional file
SPIRIT 2013 Checklist: recommended items to address in a clinical trial protocol and related documents*. (DOCX 44 kb)
Authors’ contributions
RP has drafted the manuscript and has participated in planning the intervention and design of the study. JPF, AH, and CH have participated in planning and designing the interventions and read and critically revised the manuscript. LFE developed the trial, participated in planning and designing the intervention and the study design and read and critically revised the manuscript. All authors read, improved, and approved the final manuscript.
Ethics approval and consent to participate
The trial has been evaluated by the Regional Ethics Committees of the Capital Region (# H-16015724), but the trial was not judged to be a biomedical trial and the need for ethical approval was, therefore, not necessary. The protocol is registered on www.clinicaltrials.gov (# NCT02885519), and any changes in inclusion criteria or intervention will be submitted to the website. The Danish Data Protection Agency has approved the project (#RHP-2016-006), and it will be conducted in accordance with applicable regulations.
Every participant in the trial has been informed about the objective of the study, and the implications of participation by an IBBIS team member and has given oral and written consent to participate before enrollment. Participants will be informed about their rights to withdraw from the study at any point and without consequences for their future treatment. If withdrawing, participants can decide if their information, and how much of their information, can be used in the study.
Interventions similar to the IBBIS interventions have not previously shown adverse effects. Symptom severity and suicidal ideation are nonetheless monitored by care managers to make sure that deterioration in the participant’s condition can be accommodated. After the intervention phase has ended, we will evaluate on negative effects such as suicide, recurrent sick leave, death of any cause and symptom increase at 6-, 12-, and 24-month follow-up. Starting work will be stressful for some participants. If return to work takes place during the intervention period, this will be monitored closely by the involved IBBIS team member.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1186/s13063-017-2273-0) contains supplementary material, which is available to authorized users.
Contributor Information
Rie Poulsen, Email: rie.poulsen@regionh.dk.
Jonas Fisker, Email: Jonas.fisker@regionh.dk.
Andreas Hoff, Email: Andreas.hoff@regionh.dk.
Carsten Hjorthøj, Email: Carsten.hjorthoej@regionh.dk.
Lene Falgaard Eplov, Email: Lene.falgaard.eplov@regionh.dk.
References
- 1.Nielsen MBD, Bültmann U, Amby M, Christensen U, Diderichsen F, Rugulies R. Return to work among employees with common mental disorders: study design and baseline findings from a mixed-method follow-up study. Scand J Public Health. 2010;38:864–72. doi: 10.1177/1403494810384424. [DOI] [PubMed] [Google Scholar]
- 2.Arends I, Bruinvels DJ, Rebergen DS, Nieuwenhuijsen K, Madan I, Neumeyer-Gromen A, et al. Interventions to facilitate return to work in adults with adjustment disorders. Cochrane Database Syst Rev. 2012;12:CD006389. doi: 10.1002/14651858.CD006389.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Søgaard HJ, Bech P. Psychiatric disorders in long-term sickness absence—a population-based cross-sectional study. Scand J Public Health. 2009;37:682–9. doi: 10.1177/1403494809344357. [DOI] [PubMed] [Google Scholar]
- 4.Eriksson U, Starrin B, Janson S. Long-term sickness absence due to burnout: absentees’ experiences. Qual Health Res. 2008;18:620–32. doi: 10.1177/1049732308316024. [DOI] [PubMed] [Google Scholar]
- 5.Terluin B, van Marwijk HWJ, Adèr HJ, de Vet HCW, Penninx BWJH, Hermens MLM, et al. The Four-Dimensional Symptom Questionnaire (4DSQ): a validation study of a multidimensional self-report questionnaire to assess distress, depression, anxiety and somatization. BMC Psychiatry. 2006;6:34. doi: 10.1186/1471-244X-6-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang J. Work stress as a risk factor for major depressive episode(s) Psychol Med. 2005;35:865–71. doi: 10.1017/S0033291704003241. [DOI] [PubMed] [Google Scholar]
- 7.Wang JL, Lesage A, Schmitz N, Drapeau A. The relationship between work stress and mental disorders in men and women: findings from a population-based study. J Epidemiol Community Health. 2008;62:42–7. doi: 10.1136/jech.2006.050591. [DOI] [PubMed] [Google Scholar]
- 8.Henderson M, Glazier N, Elliott KH. Long term sickness absence: is caused by common conditions and needs managing. BMJ. 2005;330:802–3. doi: 10.1136/bmj.330.7495.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.OECD. Mental health and work: Denmark. OECD Publishing; 2013. http://dx.doi.org/10.1787/9789264188631-en.
- 10.Harvey SB, Henderson M, Lelliott P, Hotopf M. Mental health and employment: much work still to be done. Br J Psychiatry. 2009;194:201–3. doi: 10.1192/bjp.bp.108.055111. [DOI] [PubMed] [Google Scholar]
- 11.Koopmans PC, Bultmann U, Roelen CAM, Hoedeman R, van der Klink JJL, Groothoff JW. Recurrence of sickness absence due to common mental disorders. Int Arch Occup Environ Health. 2011;84:193–201. doi: 10.1007/s00420-010-0540-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flachs EM, Eriksen L, Koch MB, Ryd JT, Dibba E, Skov-Ettrup L, Juel K. Statens Institut for Folke- sundhed, Syddansk Universitet. Sygdomsbyrden i Danmark – sygdomme. København: Sundhedsstyrelsen; 2015.
- 13.Olsen IB, Overland S, Reme SE, Lovvik C. Exploring work-related causal attributions of common mental disorders. J Occup Rehabil. 2014;493–505. doi:10.1007/s10926-014-9556-z. [DOI] [PMC free article] [PubMed]
- 14.Hjarsbech PU, Nielsen MBD, Andersen MF, Rugulies R, Christensen U. Struggling at work—a qualitative study of working Danes with depressive symptoms. Disabil Rehabil. 2014;0:1–9. doi:10.3109/09638288.2014.973970. [DOI] [PubMed]
- 15.Ervasti H, Venetoklis T. Unemployment and Subjective Well-being: an empirical test of deprivation theory, incentive paradigm and financial strain approach. Acta Sociol. 2010;53:119–39. doi: 10.1177/0001699310365624. [DOI] [Google Scholar]
- 16.Grove B, Secker J, Seebohm P. New thinking about mental health and employment. Oxford: Radcliffe; 2005. [Google Scholar]
- 17.Wanberg CR. The individual experience of unemployment. Annu Rev Psychol. 2012;63:369–96. doi: 10.1146/annurev-psych-120710-100500. [DOI] [PubMed] [Google Scholar]
- 18.Paul KI, Moser K. Unemployment impairs mental health: meta-analyses. J Vocat Behav. 2009;74:264–82. doi: 10.1016/j.jvb.2009.01.001. [DOI] [Google Scholar]
- 19.Henderson M, Harvey SB, Overland S, Mykletun A, Hotopf M. Work and common psychiatric disorders. J R Soc Med. 2011;104:198–207. doi: 10.1258/jrsm.2011.100231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nigatu YT, Liu Y, Uppal M, McKinney S, Rao S, Gillis K, et al. Interventions for enhancing return to work in individuals with a common mental illness: systematic review and meta-analysis of randomized controlled trials. Psychol Med. 2016;1–12. doi:10.1017/S0033291716002269. [DOI] [PubMed]
- 21.Netterstrøm B, Friebel L, Ladegaard Y. Effects of a multidisciplinary stress treatment programme on patient return to work rate and symptom reduction: results from a randomised, wait-list controlled trial. Psychother Psychosom. 2013;82:177–86. doi: 10.1159/000346369. [DOI] [PubMed] [Google Scholar]
- 22.Andersen MF, Nielsen KM, Brinkmann S. Meta-synthesis of qualitative research on return to work among employees with common mental disorders. Scand J Work Environ Health. 2012;38:93–104. doi: 10.5271/sjweh.3257. [DOI] [PubMed] [Google Scholar]
- 23.Nielsen MBD, Bültmann U, Madsen IEH, Martin M, Christensen U, Diderichsen F, et al. Health, work, and personal-related predictors of time to return to work among employees with mental health problems. Disabil Rehabil. 2012;34:1311–6. doi: 10.3109/09638288.2011.641664. [DOI] [PubMed] [Google Scholar]
- 24.Hees HL, Koeter MWJ, Schene AH. Predictors of long-term return to work and symptom remission in sick-listed patients with major depression. J Clin Psychiatry. 2012;73:1048–55. doi: 10.4088/JCP.12m07699. [DOI] [PubMed] [Google Scholar]
- 25.Dunstan DA, MacEachen E. Bearing the brunt: co-workers’ experiences of work reintegration processes. J Occup Rehabil. 2013;23:44–54. doi: 10.1007/s10926-012-9380-2. [DOI] [PubMed] [Google Scholar]
- 26.Kinoshita Y, Ta F, Kinoshita K, Honyashiki M, Im O, Marshall M, et al. Supported employment for adults with severe mental illness. Cochrane Database Syst Rev. 2013;(9):CD008297. [DOI] [PMC free article] [PubMed]
- 27.Bejerholm U, Areberg C, Hofgren C, Sandlund M, Rinaldi M. Individual placement and support in Sweden—a randomized controlled trial. Nord J Psychiatry. 2015;69:57–66. doi: 10.3109/08039488.2014.929739. [DOI] [PubMed] [Google Scholar]
- 28.Reme SE, Grasdal AL, Løvvik C, Lie SA, Øverland S. Work-focused cognitive-behavioural therapy and individual job support to increase work participation in common mental disorders: a randomised controlled multicentre trial. Occup Environ Med. 2015;oemed-2014-102700. doi:10.1136/oemed-2014-102700. [DOI] [PMC free article] [PubMed]
- 29.Mehlsen L, Holt H, Bach HB, Thörnfeldt C. Ressourceforløb. Koordinerende sagsbehandleres og borgeres erfaringer. København: SFI Det Nationale Forskningscenter for Velfærd; 2015. [Google Scholar]
- 30.Mikkelsgård KA, Granerud A, Høye S. People with mental illness returning to work: a qualitative evaluation of a Norwegian project. Scand J Occup Ther. 2014;21:172–80. doi: 10.3109/11038128.2014.882981. [DOI] [PubMed] [Google Scholar]
- 31.Chan A-W, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 Statement: Defining Standard Protocol Items for Clinical Trials. Ann Intern Med. 2013;158:200. doi: 10.7326/0003-4819-158-3-201302050-00583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boutron I, Moher D, Altman D. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern. 2008;148(4):295–310. [DOI] [PubMed]
- 33.Besèr A, Sorjonen K, Wahlberg K, Peterson U, Nygren A, Asberg M. Construction and evaluation of a self rating scale for stress-induced exhaustion disorder, the Karolinska Exhaustion Disorder Scale. Scand J Psychol. 2014;55:72–82. doi: 10.1111/sjop.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Health Organization The ICD-10 Classification of Mental and Behavioural Disorders. Int Classif. 1992;10:1–267. [Google Scholar]
- 35.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 2):22–33. [PubMed] [Google Scholar]
- 36.Cole MG, McCusker J, Elie M, Dendukuri N, Latimer E, Belzile E. Systematic detection and multidisciplinary care of depression in older medical inpatients: a randomized trial. Can Med Assoc J. 2006;174:38–44. doi:10.1503/cmaj.050519. [DOI] [PMC free article] [PubMed]
- 37.Moran P, Leese M, Lee T, Walters P, Thornicroft G, Mann A. Standardised Assessment of Personality – Abbreviated Scale (SAPAS): preliminary validation of a brief screen for personality disorder. Br J Psychiatry. 2003;183:228–32. doi: 10.1192/bjp.183.3.228. [DOI] [PubMed] [Google Scholar]
- 38.Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245–56. doi: 10.1017/S0033291704002892. [DOI] [PubMed] [Google Scholar]
- 39.Nielsen MBD, Madsen IEH, Bültmann U, Christensen U, Diderichsen F, Rugulies R. Predictors of return to work in employees sick-listed with mental health problems: findings from a longitudinal study. Eur J Public Health. 2011;21:806–11. doi: 10.1093/eurpub/ckq171. [DOI] [PubMed] [Google Scholar]
- 40.Kabat-Zinn J. Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. 2nd edition. London: Piatkus; 2013.
- 41.Franche RL, Krause N. Readiness for return to work following injury or illness: conceptualizing the interpersonal impact of health care, workplace, and insurance factors. Handb Complex Occup Disabil Claims Early Risk Identification, Interv Prev. 2005;12:67–91. doi: 10.1023/a:1020270407044. [DOI] [PubMed] [Google Scholar]
- 42.Abma FI, Van Der Klink JJL, Bültmann U. The Work Role Functioning Questionnaire 2.0 (Dutch Version): examination of its reliability, validity and responsiveness in the general working population. J Occup Rehabil. 2013;23:135–47. doi: 10.1007/s10926-012-9379-8. [DOI] [PubMed] [Google Scholar]
- 43.Shaw WS, Reme SE, Linton SJ, Huang YH, Pransky G. 3rd place, PREMUS 1 best paper competition: development of the return-to-work self-efficacy (RTWSE-19) questionnaire – psychometric properties and predictive validity. Scand J Work Environ Health. 2011;37:109–19. doi: 10.5271/sjweh.3139. [DOI] [PubMed] [Google Scholar]
- 44.van der Klink JJ, Ausems CMM, Beijderwellen BD, Blonk R, Bruinvels DJ, Dogger J. Richtlijn: handelen van de bedrijfsarts bij werkenden met psychische problemen. Utrecht: Nederlands Vereniging voor Arbeids-en Bedrijfsgeneeskunde (NVAB); 2007. [Google Scholar]
- 45.Arends I, van der Klink JJL, van Rhenen W, de Boer MR, Bültmann U. Prevention of recurrent sickness absence in workers with common mental disorders: results of a cluster-randomised controlled trial. Occup Environ Med. 2014;71:21–9. doi: 10.1136/oemed-2013-101412. [DOI] [PubMed] [Google Scholar]
- 46.Burns T, Catty J, Becker T, Drake RE, Fioritti A, Knapp M, et al. The effectiveness of supported employment for people with severe mental illness: a randomised controlled trial. Lancet. 2007;370:1146–52. doi: 10.1016/S0140-6736(07)61516-5. [DOI] [PubMed] [Google Scholar]
- 47.Gittell JH, Weinberg D, Pfefferle S, Bishop C. Impact of relational coordination on job satisfaction and quality outcomes: A study of nursing homes. Hum Resour Manag J. 2008;18:154–70
- 48.Nielsen L, Curtis T, Grønbaek M, Nielsen NR. Forebyggelse og behandling af stress i Danmark. Copenhagen: Forebyggelse og behandling af stress i Danmark; 2007.
- 49.Region Sjælland. Samtaleterapi i almen praksis. En analyse i almen praksis. 2016.
- 50.Komiteen for Sundhedsoplysning. Lær at tackle status i Danmark. Patientuddannelse.info. 2017. http://patientuddannelse.info/om-laer-at-tackle/status-i-danmark.aspx.
- 51.Danish Agency for Labour Market and Recruitment. The DREAM database, statistics Denmark. DREAM databasen. 2016. http://www.dst.dk/da/TilSalg/Forskningsservice/Data/Andre_Styrelser.aspx. Accessed 21 Dec 2016.
- 52.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio: TX Psychol Corp; 1996. pp. 1–82. [Google Scholar]
- 53.Osman A, Hoffman J, Barrios FX, Kopper BA, Breitenstein JL, Hahn SK. Factor structure, reliability, and validity of the beck anxiety inventory in adolescent psychiatric inpatients. J Clin Psychol. 2002;58:443–56. doi: 10.1002/jclp.1154. [DOI] [PubMed] [Google Scholar]
- 54.Wang YP, Gorenstein C. Psychometric properties of the Beck Depression Inventory-II: a comprehensive review. Rev Bras Psiquiatr. 2013;35:416–31. doi: 10.1590/1516-4446-2012-1048. [DOI] [PubMed] [Google Scholar]
- 55.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–7. doi: 10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- 56.Lee E-H. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res (Korean Soc Nurs Sci) 2012;6:121–7. doi: 10.1016/j.anr.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 57.Mundt JC, Marks IM, Shear MK, Greist JH. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry. 2002;180:461–4. doi: 10.1192/bjp.180.5.461. [DOI] [PubMed] [Google Scholar]
- 58.Saboonchi F, Perski A, Grossi G. Validation of Karolinska Exhaustion Scale: psychometric properties of a measure of exhaustion syndrome. Scand J Caring Sci. 2013;27:1010–7. doi: 10.1111/j.1471-6712.2012.01089.x. [DOI] [PubMed] [Google Scholar]
- 59.The Swedish National Board of Health and Welfare. Exhaustion disorder. 2003.
- 60.Turner N, Campbell J, Peters TJ, Wiles N, Hollinghurst S. A comparison of four different approaches to measuring health utility in depressed patients. Health Qual Life Outcomes. 2013;11:81. doi: 10.1186/1477-7525-11-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Burckhardt CS, Anderson KL. The Quality of Life Scale (QOLS): reliability, validity, and utilization. Health Qual Life Outcomes. 2003;1:60. doi: 10.1186/1477-7525-1-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Moss-Morris R, Weinman J, Petrie KJ, Horne R, Cameron LD, Buick D. The revised Illness Perception Questionnaire (IPQ-R) Psychol Health. 2002;17:1–16. doi: 10.1080/08870440290001494. [DOI] [Google Scholar]
- 63.Lagerveld SE, Blonk RWB, Brenninkmeijer V, Schaufeli WB. Return to work among employees with mental health problems: development and validation of a self-efficacy questionnaire. Work Stress. 2010;24:359–75. doi: 10.1080/02678373.2010.532644. [DOI] [Google Scholar]
- 64.Schwarzer R, Jerusalem M. Generalized Self-Efficacy scale. In: Wright S, Johnston M, editors. Measures in health psychology: a user’s portfolio. Causal and control beliefs. Windsor: Generalized Self-Efficacy scale; 1995. p. 35–7.
- 65.Attkisson C, Zwick R. The Client Satisfaction Questionnaire: psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann. 1982;5:233–7. doi: 10.1016/0149-7189(82)90074-X. [DOI] [PubMed] [Google Scholar]
- 66.Johns G. Presenteeism in the workplace: a review and research agenda. J Organ Behav. 2010;31:519–42. doi: 10.1002/job.630. [DOI] [Google Scholar]
- 67.Van Oostrom SH, Van Mechelen W, Terluin B, De Vet HCW, Knol DL, Anema JR. A workplace intervention for sick-listed employees with distress: results of a randomised controlled trial. 2010. [DOI] [PubMed] [Google Scholar]
- 68.Vlasveld MC, van der Feltz-Cornelis CM, Ader HJ, Anema JR, Hoedeman R, van Mechelen W, et al. Collaborative care for sick-listed workers with major depressive disorder: a randomised controlled trial from the Netherlands Depression Initiative aimed at return to work and depressive symptoms. Occup Environ Med. 2013;70:223–30. doi: 10.1136/oemed-2012-100793. [DOI] [PubMed] [Google Scholar]
- 69.Lagerveld SE, Blonk RWB, Brenninkmeijer V, Wijngaards-de Meij L, Schaufeli WB. Work-focused treatment of common mental disorders and return to work: a comparative outcome study. J Occup Health Psychol. 2012;17:220–34. doi: 10.1037/a0027049. [DOI] [PubMed] [Google Scholar]
- 70.van Oostrom SH, Anema JR, Terluin B, de Vet HCW, Knol DL, van Mechelen W. Cost-effectiveness of a workplace intervention for sick-listed employees with common mental disorders: design of a randomized controlled trial. BMC Public Health. 2008;8:12. doi: 10.1186/1471-2458-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.van der Feltz-Cornelis CM, Hoedeman R, de Jong FJ, Meeuwissen JA, Drewes HW, van der Laan NC, et al. Faster return to work after psychiatric consultation for sicklisted employees with common mental disorders compared to care as usual. A randomized clinical trial. Neuropsychiatr Dis Treat. 2010;6:375–85. doi: 10.2147/NDT.S11832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Layard R, Clark D, Knapp M, Mayraz G. Cost-benefit analysis of psychological therapy. Natl Inst Econ Rev. 2007;202:90–8. doi: 10.1177/0027950107086171. [DOI] [Google Scholar]
- 73.Dupont WD, Plummer WD. Power and sample size calculations. A review and computer program. Control Clin Trials. 1990;11:116–28. doi: 10.1016/0197-2456(90)90005-M. [DOI] [PubMed] [Google Scholar]
- 74.Bonell C, Fletcher A, Morton M, Lorenc T, Moore L. Realist randomised controlled trials: a new approach to evaluating complex public health interventions. Soc Sci Med. 2012;75:2299–306. doi: 10.1016/j.socscimed.2012.08.032. [DOI] [PubMed] [Google Scholar]
- 75.Aust B, Nielsen MBD, Grundtvig G, Buchardt HL, Ferm L, Andersen I, et al. Implementation of the Danish return-to-work program: process evaluation of a trial in 21 Danish municipalities. Scand J Work Environ Health. 2015;41:529–41. doi: 10.5271/sjweh.3528. [DOI] [PubMed] [Google Scholar]
- 76.Valentijn PP, Boesveld IC, van der Klauw DM, Ruwaard D, Struijs JN, Molema JJW, et al. Towards a taxonomy for integrated care: a mixed-methods study. Int J Integr Care. 2015;15:e003. doi: 10.5334/ijic.1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cohen S, Williamson G. Perceived stress in a probability sample of the United States. Soc Psychol Health. 1988;13:31–67. [Google Scholar]
- 78.Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6D across seven patient groups. Health Econ. 2004;13:873–84. doi: 10.1002/hec.866. [DOI] [PubMed] [Google Scholar]
- 79.Koopman C, Pelletier KR, Murray JF, Sharda CE, Berger ML, Turpin RS, et al. Stanford presenteeism scale: health status and employee productivity. J Occup Environ Med. 2002;44:14–20. doi: 10.1097/00043764-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 80.Søgaard HJ, Bech P. The effect on length of sickness absence by recognition of undetected psychiatric disorder in long-term sickness absence. A randomized controlled trial. Scand J Public Health. 2009;37:864–71. doi: 10.1177/1403494809347551. [DOI] [PubMed] [Google Scholar]
- 81.König H-H, Born A, Heider D, Matschinger H, Heinrich S, Riedel-Heller SG, et al. Cost-effectiveness of a primary care model for anxiety disorders. Br J Psychiatry. 2009;195:308–17. doi: 10.1192/bjp.bp.108.058032. [DOI] [PubMed] [Google Scholar]
- 82.Proudfoot J, Ryden C, Everitt B, Shapiro DA, Goldberg D, Mann A, et al. Clinical efficacy of computerised cognitive-behavioural therapy for anxiety and depression in primary care: randomised controlled trial. Br J Psychiatry. 2004;185:46–54. doi: 10.1192/bjp.185.1.46. [DOI] [PubMed] [Google Scholar]
- 83.Proudfoot J, Goldberg D, Mann A, Everitt B, Marks I, Gray JA. Computerized, interactive, multimedia cognitive-behavioural program for anxiety and depression in general practice. Psychol Med. 2003;33:217–27. doi: 10.1017/S0033291702007225. [DOI] [PubMed] [Google Scholar]
- 84.Buszewicz M, Griffin M, McMahon EM, Beecham J, King M. Evaluation of a system of structured, pro-active care for chronic depression in primary care: a randomised controlled trial. BMC Psychiatry. 2010;10:61. doi: 10.1186/1471-244X-10-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mann A, Blizard R, Murray J, Smith J, Botega N, Macdonald E, et al. An evaluation of practice nurses working with general practitioners to treat people with depression. Br J Gen Pract. 1998;48:875–9. [PMC free article] [PubMed] [Google Scholar]
- 86.Muntingh ADT, van der Feltz-Cornelis CM, van Marwijk HWJ, Spinhoven P, Assendelft WJJ, de Waal MWM, et al. Collaborative stepped care for anxiety disorders in primary care: aims and design of a randomized controlled trial. BMC Health Serv Res. 2009;9:159. doi: 10.1186/1472-6963-9-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Willert MV, Thulstrup AM, Bonde JP. Effects of a stress management intervention on absenteeism and return to work--results from a randomized wait-list controlled trial. Scand J Work Environ Health. 2011;37:186–95. doi: 10.5271/sjweh.3130. [DOI] [PubMed] [Google Scholar]
- 88.Ejeby K, Savitskij R, Ost L-G, Ekbom A, Brandt L, Ramnerö J, et al. Symptom reduction due to psychosocial interventions is not accompanied by a reduction in sick leave: results from a randomized controlled trial in primary care. Scand J Prim Health Care. 2014;2013:1–6. doi: 10.3109/02813432.2014.909163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lengacher CA, Johnson-Mallard V, Post-White J, Moscoso MS, Jacobsen PB, Klein TW, et al. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psychooncology. 2009;18:1261–72. doi: 10.1002/pon.1529. [DOI] [PubMed] [Google Scholar]
- 90.Phillips R, Schneider J, Molosankwe I, Leese M, Foroushani PS, Grime P, et al. Randomized controlled trial of computerized cognitive behavioural therapy for depressive symptoms: effectiveness and costs of a workplace intervention. Psychol Med. 2014;44:741–52. doi: 10.1017/S0033291713001323. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable


